1. INTRODUCTION
As the COVID‐19 pandemic has swept across the globe, the dominant narrative about overwhelmed inpatient settings obscured a more nuanced crisis—the rising prevalence of occult airway injuries among survivors. Up to 90% of patients admitted to intensive care units undergo intubation and invasive mechanical ventilation, often requiring tracheostomy. Resulting device‐related airway pressure injuries are disturbingly common, affecting over 50% of individuals. Endotracheal and tracheostomy tubes may cause a wide range of laryngotracheal injuries, from mucosal ulceration to destruction of cartilage or even transmural injury, causing stenosis—all with profound quality of life ramifications (Brodsky, Akst, et al., 2020; Brodsky et al., 2020). Nurses are uniquely positioned to expedite diagnosis and intervention, improving voice, swallowing and breathing.
2. FACTORS CONTRIBUTING TO THE DEVELOPMENT OF AIRWAY STENOSIS
Laryngotracheal stenosis (LTS), the most common long‐term complication of acute airway injury, involves a partial or complete narrowing of the airway lumen at the level of the larynx, subglottic space or trachea. The narrowest part of the normal adult airway is the subglottic space, which is the most common site of tracheal stenosis. Prior to the pandemic, up to 9% of patients requiring invasive mechanical ventilation experienced stenosis. In the COVID‐19 era, this rate has risen due to trauma associated with decreased visualisation when using personal protective gear, cuff overinflation and prolonged intubation (Hillel et al., 2016). COVID‐19 patients have a median ventilation duration of 17 days and a high frequency of re‐intubation. In addition, prone positioning, pressure of endotracheal tube cuff/tracheostomy tube and larger sizes of endotracheal tube can contribute to risk of stenosis (Hillel et al., 2016).
3. SIGNS, SYMPTOMS AND STAGING OF TRACHEAL STENOSIS
Many individuals are initially asymptomatic or have only mild symptoms for weeks to months, as the stenosis insidiously progresses. Inspiratory stridor is the most common presenting symptom, however, dyspnoea, dry cough, dysphagia, although some patients present with wheezing or a history of recurrent bronchitis (Shinn et al., 2019). Tracheal stenosis is often misdiagnosed given similar presentations to asthma and other respiratory‐related conditions. This possible confusion underscores the importance of obtaining a thorough medical history, including history of endotracheal intubation.
The severity of tracheal stenosis is determined via laryngoscopy and can be staged based on the length, location and extent of obstruction (Figure 1). Staging has implication for both management and prognosis. The McCaffrey staging system classifies stenosis based on length and location of the stenosis (Table 1). In contrast, the Cotton‐Meyer system of staging classifies stenosis severity based on the diameter of the remaining airway in correlation with the diameter of tracheal tubes, ranging from a Stage I classification for less than 70% obstruction to a Stage IV classification if there is 100% obstruction (Cotton, 1984; Myer et al., 1994) (Figure 2).
FIGURE 1.
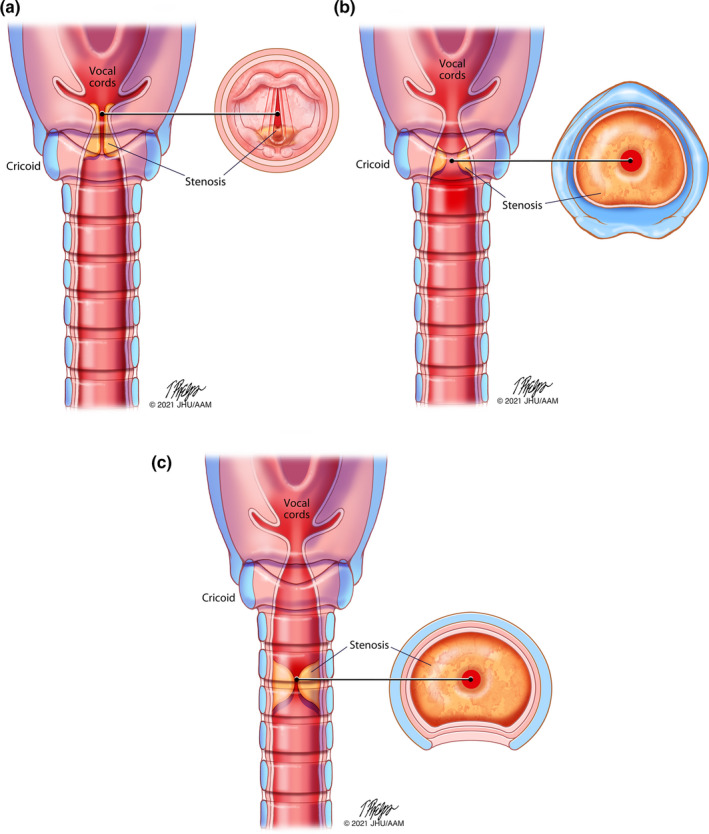
McCaffrey staging system. (a) Laryngeal stenosis. (b) Subglottic stenosis. (c) Tracheal stenosis
TABLE 1.
Tracheal stenosis grading systems
| Grading system | Stage I | Stage II | Stage III | Stage IV |
|---|---|---|---|---|
| McCaffrey | Subglottic or tracheal lesions <1 cm | Subglottic lesions >1 cm within cricoid ring and not extending to the glottis or trachea | Subglottic stenosis that extend into the upper trachea but does not involve the glottis | Glottic lesions with fixation/paralysis of the vocal cords |
| Meyers‐Cotton | Tracheal obstruction diameter: 0%−50% | Tracheal obstruction diameter: 51%–70% | Tracheal obstruction diameter: 71%–99% | No detectable lumen |
FIGURE 2.
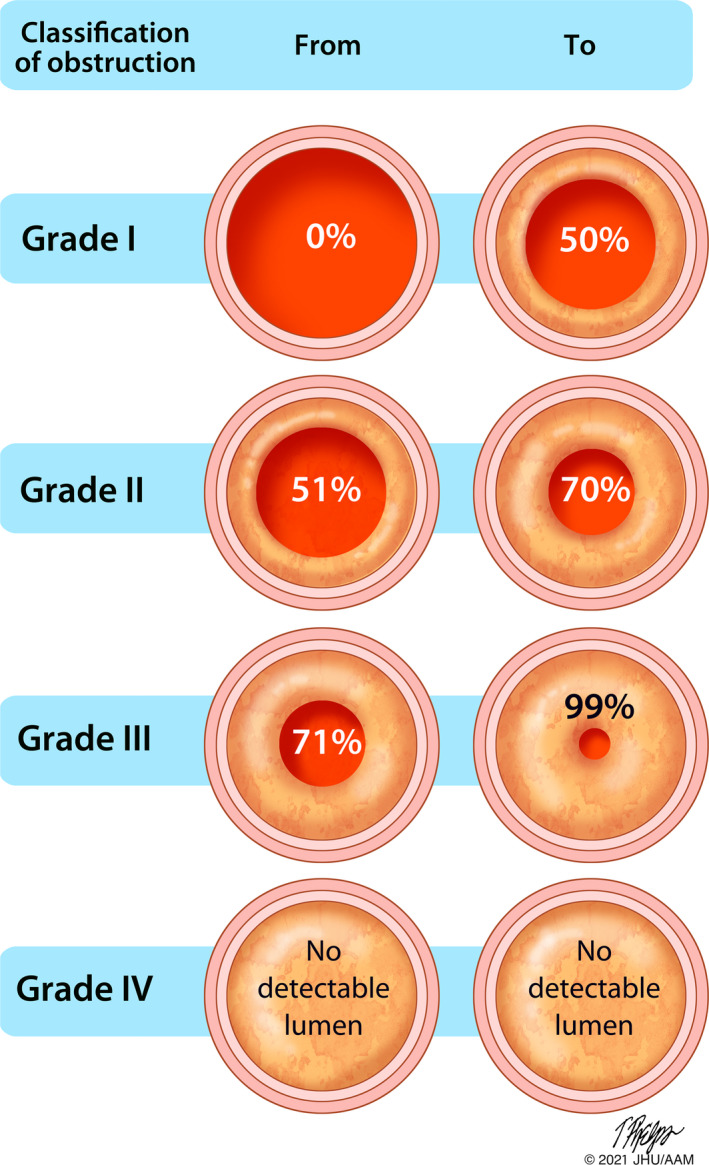
Cotton‐Meyer staging system
4. MEDICAL MANAGEMENT
The best studied approach to medical management of LTS is steroid injection. Protocols for serial steroid injections vary but most often involve multiple rounds of the synthetic glucocorticoid triamcinolone 40 mg/dl injected directly into the stenosis under direct visualisation, typically four injections spaced 3 to 6 weeks apart. These injections are usually performed while awake, using office‐based laryngoscopy, and are very well‐tolerated. This approach provides comparable improvements in peak expiratory flow compared to endoscopic dilation. Using steroidal injection as adjuvant therapy after dilation also can provide benefits, improving the inter‐dilation interval compared to dilation alone.
5. SURGICAL MANAGEMENT
Whereas steroid injections have a more preventative and temporising role in the management of LTS, surgery is the mainstay of treatment for severe cases. The two main types of surgery are categorised as endoscopic (focused largely on dilation with or without laser resection) and open (cricotracheal resection when stenosis involves cricoid cartilage, and tracheal resection with reconstruction when stenosis involves only a segment of the trachea). Endoscopic treatment is most commonly performed for idiopathic subglottic stenosis but may also have a role for post‐intubation stenosis and offers minimal morbidity with good functional outcomes—however, stenoses are often recurrent and repeated dilations may be required.
When injury extends beyond mucosal surfaces to include damage to the cartilage framework of the larynx or trachea—as is often the cause with intubation‐related LTS—open surgeries are often required. Surgical outcomes are more favourable for isolated tracheal resection, often involving distal stenoses; improvement is less consistent when cricotracheal resection is required, as with stenoses involving the larynx. Although open surgeries often allow for decannulation, repeated procedures may be necessary and voice may be negatively impacted. Furthermore, decannulation is not always achievable. As surgical management evolves, there may be a growing role for strategies that aim to modulate biology of the healing wound, such as endoscopic scar resection with skin‐graft resurfacing of the stenotic area and tissue engineering approaches to tracheal replacement and transplantation.
6. PSYCHOSOCIAL IMPACT OF EXPERIENCING LTS
LTS often has deleterious effects on physical, psychological and emotional quality of life, and treatment can help to alleviate these untoward effects. Online support groups exist, which can help reduce disease‐specific anxiety and inform treatment decision‐making. In addition to the anticipated rise in prevalence of LTS associated with the pandemic, patients who already had LTS before COVID‐19 are susceptible to amplified psychosocial stressors in relation to COVID‐19—they may struggle with access to necessary care, given constraints on resources; stenosis‐related cough and dyspnoea may cause them to be ostracised by individuals, healthcare professionals or members of the public, who mistakenly assume that individual with LTS have COVID‐19, and fears of contracting COVID‐19 themselves, which is a legitimate concern since COVID‐19 can make a baseline tenuous airway into an emergency. Finally, COVID‐19 has increased the stress experienced by healthcare providers taking care of patients with LTS, as airway procedures are often considered high risk for aerosol generation.
7. SAFE DISCHARGE, EDUCATION AND FOLLOW‐UP
Since the symptoms of stenosis are often subtle, patient and caregiver education regarding post‐intubation complications should include description of signs and symptoms of LTS. Discharge planning should include a plan for notifying healthcare professionals about changes in breathing patterns and dysphagia. Early recognition and treatment of tracheal stenosis may avert an acute respiratory event, shorten recovery, and improved clinical outcomes. If a patient is discharged home with a tracheostomy, they should be educated on symptoms of tracheal stenosis, often signalled by inability to pass suction catheter or difficulty with removal of secretions. In addition, proper tracheostomy tube care minimising internal irritation is crucial to preventing tracheal stenosis. If the patient has tracheal stenosis and is discharged to home/long‐term facilities, then follow‐up appointments instructions should address direct examinations to monitor for any progression of the stenosis, especially if the patient is has undergone tracheal reconstruction.
8. CONSIDERATIONS IN THE COMMUNITY SETTING
Advanced practice nurses have a vital role in identifying and evaluating LTS that was not detected during an inpatient stay. For example, the history taken on any patient who required mechanical ventilation should include number of intubations, duration of intubation(s), prior airway surgery and family history of airway pathologies. Progressive symptoms of dyspnoea, stridor (or other noisy breathing) and/or respiratory distress requires evaluation in an emergency department. A chest CT scan evaluates expiration and inspiration, providing information on airway dynamics and structural abnormalities. Direct visualisation of the airway with awake flexible laryngoscopy allows evaluation of the upper airway, and a bronchoscopy allows evaluation for subglottic abnormalities and dynamic airway collapse. If imaging and direct visualisation are unrevealing, pulmonary function testing can help differentiate upper versus lower airway conditions.
9. AIRWAY ASSESSMENT IN EMERGENCY DEPARTMENT AND OPERATING ROOM
Certified registered nurse anaesthetists and other professionals involved in performing intubation of patients should inquire about history of difficult airway, prior intubations and symptoms of LTS. These considerations apply to patients being evaluated in emergency department who may require intubation and patients being brought to operating room for elective procedures. Other preoperative considerations include recent respiratory tract infections, exercise tolerance and neck mobility. Decisions regarding preferred airway technique (direct laryngoscope, videolaryngoscope or fiberoptic bronchoscope) and size of endotracheal tube should be made in collaboration with an interprofessional team that understands the location and severity of stenosis.
10. PREVENTION OF TRACHEAL STENOSIS IN ACUTE CARE SETTINGS
Acute care nurse practitioners and critical care clinical nurse specialists should routinely verify appropriate endotracheal tube placement using radiographic or ultrasound imaging. Patient transport and repositioning may inadvertently lead to tube malposition. Appropriate endotracheal tube placement is defined radiographically as 3–5 cm above the bifurcation carina. Best practice guidelines also recommend that endotracheal/tracheostomy tube cuff pressure be maintained between 20 and 30 cm H20 to minimise aspiration of secretions; cuff pressures <30 cm H2O reduce risk of luminal mucosal hypoperfusion, thereby avoiding mucosal necrosis, scarring and subsequent stenosis.
11. CONCLUSION
Acquired airway injuries are a defining feature of COVID‐19 survivorship, and the extent of this hidden epidemic is only just beginning to come to light, as unprecedented numbers of intensive care survivors enter the community. Vigilance regarding predisposing history and signs and symptoms is critical. As frontline professionals, nurses have a vital role in the prevention, early detection and management of these injuries, and in doing so can greatly improve quality of life for patients.
CONFLICTS OF INTEREST
No conflicts of interest.
ACKNOWLEDGEMENTS
We want to thank Dr. Sandra Panchalingam for her editorial support.
Allgood, S. , Peters, J. , Benson, A. , Maragos, C. , McIltrot, K. , Slater, T. , Akst, L. , Best, S. R. , Galiatsatos, P. , Brodsky, M. B. , Brenner, M. J. , & Pandian, V. (2021). Acquired laryngeal and subglottic stenosis following COVID‐19—Preparing for the coming deluge. Journal of Clinical Nursing, 00, 1–5. 10.1111/jocn.15992
Funding information
Financial support for this editorial was provided by R01 NIH 5‐R017433 (Martin B Brodsky, Vinciya Pandian) on laryngeal injury post‐extubation in intensive care unit settings.
REFERENCES
- Brodsky, M. B. , Akst, L. M. , Jedlanek, E. , Pandian, V. , Blackford, B. , Price, C. , Cole, G. , Mendez‐Tellez, P. A. , Hillel, A. T. , Best, S. R. , & Levy, M. J. (2020). Laryngeal injury and upper airway symptoms after endotracheal intubation during surgery: A systematic review and meta‐analysis. Anesthesia and Analgesia, 132(4), 1023–1032. 10.1213/ANE.0000000000005276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodsky, M. B. , Pandian, V. , & Needham, D. M. (2020). Understanding variable prevalences of acute laryngeal injury post‐extubation. Critical Care Medicine, 48(5), e430–e431. 10.1097/CCM.0000000000004245 [DOI] [PubMed] [Google Scholar]
- Cotton, R. T. (1984). Pediatric laryngotracheal stenosis. Journal of Pediatric Surgery, 19(6), 699–704. 10.1016/s0022-3468(84)80355-3 [DOI] [PubMed] [Google Scholar]
- Hillel, A. T. , Karatayli‐Ozgursoy, S. , Samad, I. , Best, S. R. A. , Pandian, V. , Giraldez, L. , Gross, J. , Wootten, C. , Gelbard, A. , Akst, L. M. , & Johns, M. M. (2016). Predictors of posterior glottic stenosis: A multi‐institutional case‐control study. The Annals of Otology, Rhinology, and Laryngology, 125(3), 257–263. 10.1177/0003489415608867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer, C. M. 3rd , O'Connor, D. M. , & Cotton, R. T. (1994). Proposed grading system for subglottic stenosis based on endotracheal tube sizes. The Annals of Otology, Rhinology, and Laryngology, 103(4 Pt 1), 319–323. 10.1177/000348949410300410 [DOI] [PubMed] [Google Scholar]
- Shinn, J. R. , Kimura, K. S. , Campbell, B. R. , Sun Lowery, A. , Wootten, C. T. , Garrett, C. G. , Francis, D. O. , Hillel, A. T. , Du, L. , Casey, J. D. , Ely, E. W. , & Gelbard, A. (2019). Incidence and outcomes of acute laryngeal injury after prolonged mechanical ventilation. Critical Care Medicine, 47(12), 1699–1706. 10.1097/CCM.0000000000004015 [DOI] [PMC free article] [PubMed] [Google Scholar]


