Abstract
Background
The coronavirus disease 2019 (COVID‐19) pandemic has highlighted the importance of using information and communication technology (ICT) to address daily and healthcare needs. The barriers for older adults in the United States to learn a new technology to go online during the pandemic remain to be studied.
Methods
Using data from the 2019–2020 National Health and Aging Trends Study (NHATS), a nationally representative survey of older Medicare beneficiaries aged 65 years and older in the United States, we used multivariable logistic regression models to identify sociodemographic and clinical factors associated with learning a new technology to go online during the COVID‐19 pandemic.
Results
Our sample represented 23,547,688 older adults nationally, of which the majority (60.2%) increased ICT use during the COVID‐19 pandemic. However, most older adults (71.8%) did not report learning a new technology to go online. Those who did not learn a new technology to go online had less of an increase in ICT use than those who learned either with help or by themselves (50.7% vs. 78.4% or 89.2% respectively, p < 0.01). The odds of learning a new technology decreased with increasing age (aOR [95%CI] = 0.96 [0.94–0.98]), being male (aOR [95%CI] = 0.56 [0.45–0.72]), having lower than high school educational attainment (aOR [95%CI] = 0.38 [0.29–0.50]), decreasing income levels (aORs ranged from 0.28 to 0.54), and self‐reported fair or poor general health (aOR [95%CI] = 0.65 [0.47–0.90]).
Conclusion
The identified sociodemographic and clinical factors could inform targeted intervention strategies to improve ICT use among older adults during the evolving COVID‐19 pandemic and in the future.
Keywords: barriers, COVID‐19, information and communication technology (ICT), learn a new technology, older adults
Key Points
Information and communication technology (ICT) use increased during the COVID‐19 pandemic.
Barriers to learn a new technology to go online were advanced age, male sex, low education and income, and poor health.
Why Does this Paper Matter?
Addressing these barriers are important as reliance on ICT is growing among older adults.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has accelerated the broader adoption of information and communication technology (ICT) in the United States to address daily and healthcare needs. While ICT has been rapidly adopted, older adults are usually slower to adopt a new technology as they may face more barriers to learn a new technology. 1 , 2 , 3 , 4 Previous research has shown that most older adults (77%) agreed that they need assistance when learning to use digital technology, compared to just 18% who were comfortable learning on their own. 5 , 6 Previous research also showed that older adults with advanced age, female sex, non‐white race, lower socioeconomic status, and singled or not partnered were less likely to use ICT. 7 , 8 , 9 , 10 , 11
Although previous research suggests that older adults face several unique challenges in ICT use, the barriers to learning a new technology during the COVID‐19 pandemic remain to be studied. To address this research gap, we utilized a nationally representative survey to assess changes in ICT use during the COVID‐19 pandemic and identify factors associated with learning a new technology to go online among older adults during the COVID‐19 pandemic. Our findings can enhance understanding of the barriers faced by older adults in learning and adopting a new technology and inform interventions to reduce disparities in ICT use.
METHODS
Data source and study population
Started in 2011, the National Health and Aging Trends Study (NHATS) is an annual, longitudinal, nationally representative survey of community‐dwelling Medicare beneficiaries aged 65 years and older. It is designed to study the health and wellbeing of older adults in the United States. Of the 4889 participants who completed the 2019 NHATS, 3255 participants also completed 2020 NHATS COVID‐19 Questionnaire. We identified 2909 participants who had non‐missing information on the main outcome of interest (i.e., learning a new technology) and sociodemographic and clinical factors (Figure S1).
Measures
In 2020, NHATS surveyed responders about their experience during the COVID‐19 pandemic. 12 COVID‐19 questionnaires were mailed from June to October, 2020, while most of the questionnaires were completed in July and August. 13
Learning a new technology to go online
Participants who responded yes to the question, “During the COVID‐19 outbreak, have you learned a new technology or program to go online? This includes learning to use a smartphone, computer or iPad or a program like Zoom or FaceTime,” were categorized as having learned a new technology to go online. How they learned a new technology (with help or by themselves) was based on their responses to the subsequent question, “Has anyone helped you with that or did you learn that on your own?”
Increase in ICT use
Participants were categorized as having an increase in ICT use during the COVID‐19 pandemic if they met any of the four criteria: (1) had a higher frequency of online shopping during than before the pandemic; (2) had a higher frequency of contacting family/friends virtually (email or videos) during than before the pandemic; (3) contacted health providers virtually during the pandemic but never did that before; and (4) conducted other activities (i.e., work for pay, volunteer, religious or other group activities like classes and clubs) online during the pandemic but never did that before. These criteria were based on questions 25–26, 33–34, 38, and 40–42 of the NHATS COVID‐19 survey. 12
Clinical factors
We used measures of overall self‐reported health (“poor,” “fair,” “good,” “very good,” or “excellent”) and a count of chronic conditions (heart diseases, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia/Alzheimer's disease, and cancer) based on self‐report of whether a doctor had ever told study participants they had each health condition. Participants were characterized as having probable depression if they scored ≥3 on the PHQ‐2 scale (range: 0–6) and as having probable anxiety if they scored ≥3 on the GAD‐2 scale (range: 0–6). 14 , 15 Participants were asked whether they received help with any of the following activities of daily living (ADLs): eating, getting cleaned up, using the toilet, dressing, walking around inside, and getting out of bed; and instrumental activities of daily living (IADL): laundry, shopping for groceries, making hot meals, handling bills and banking, and handling of prescribed medicines.
Sociodemographic factors
Sociodemographic factors included age, sex, race/ethnicity, marital status, educational attainment, and income quartile (quartile1 [Q1]: lower than $28,319; Q2: between $28,319 and $49,731; Q3: between $49,731–$89,037; Q4: higher than $89037).
Statistical analyses
We compared the characteristics and ICT use changes of the study population by whether participants learned a new technology, either with help or by themselves, to go online during the COVID‐19 pandemic using Rao–Scott Chi‐square test for categorical variables, and F‐test in linear regression for the continuous age variable. We used multivariable logistic regression to identify sociodemographic and clinical factors associated with learning a new technology either with help or by themselves to go online during the COVID‐19 pandemic. In a sensitivity analysis, we assessed the factors associated with learning a new technology with help and by themselves, respectively. All analyses were conducted using the survey procedures in SAS software (version 9.4TS1m6) and survey‐weighted statistics were reported.
RESULTS
Our sample represented 23,547,688 older adults nationally, of which the majority (87.1%) reported ICT use before the COVID‐19 pandemic. During the pandemic, 71.8% of the older adults did not learn a new technology to go online, while 17.4% learned with help, and 10.8% learned by themselves (Table 1). The prevalence of ICT use before the pandemic was lower among those who did not learn than those who did learn a new technology to go online during the pandemic (82.2% vs. 100%, p < 0.01). During the pandemic, 60.2% of participants showed an increase in ICT use. Not surprisingly, those who did not learn a new technology to go online showed less increase in ICT use than those who learned with help or by themselves (50.7% vs. 78.4% or 89.2%, p < 0.01). The magnitude of increase in the specific ICT usage types was also lower among those who did not learn a new technology than those who learned with help or by themselves (range: 12.3%–16.3% vs. 20.7%–42.3% or 30.4%–47.5%).
TABLE 1.
Information and communication technology (ICT) use overall and by mode of learning a new technology to go online during the pandemic
| Learn a new technology to go online during the pandemic | |||||
|---|---|---|---|---|---|
| Overall weighted = 100% (Weighted N = 23,547,688; Unweighted N = 2909) | No weighted = 71.8% (Weighted N = 16,776,060; Unweighted N = 2172) | With help weighted = 17.4% (Weighted N = 4,067,162; Unweighted N = 466) | By themselves weighted = 10.8% (Weighted N = 2,517,399; Unweighted N = 250) | p‐value | |
| Information and communication technology (ICT) use | |||||
| Any ICT use before the COVID‐19 pandemic (yes%) | 87.1 | 82.2 | 100 | 100 | <0.01 |
| Any ICT use during the COVID‐19 pandemic (yes%) | 89.1 | 84.5 | 100 | 100 | <0.01 |
| Increased any ICT use during the COVID‐19 pandemic (yes%) | 60.2 | 50.7 | 78.4 | 89.2 | <0.01 |
| Increase in virtual contact with friends/family (yes%) | 22.6 | 15.5 | 36.3 | 47.5 | |
| Increase in virtual contact with medical providers (yes%) | 22.4 | 16.3 | 36.2 | 38.9 | |
| Increase in online grocery (yes%) | 16.8 | 13.8 | 20.7 | 30.4 | 16.8 |
| Increase in other activities online (yes%) | 21.0 | 12.3 | 42.3 | 45.1 | 21.0 |
Note: There were 21 participants who answered they learned a new technology to go online during the pandemic but did not answer whether they learned with help or by themselves.
Abbreviations: COVID‐19, coronavirus disease 2019; ICT, Information and Communication Technology.
Those who did not learn a new technology to go online were older than those who learned with help or by themselves (77.8 vs. 76.4 or 74.7, p < 0.01, Table 2), while their differences in race/ethnicity and marital status were not statistically significant. Compared to those who learned a new technology to go online either with help or by themselves, those who did not learn were more likely to be male (47.2% vs. 38.2% or 43.3%, p < 0.01), have a high school or lower education level (41.7% vs. 18.6% or 14.0%, p < 0.01), and have lower income (e.g., income lower than $28,319: 26.6% vs. 13.3% or 8.9%). Income status also differed significantly across all income levels by the mode of learning a new technology to go online during the pandemic (p < 0.01). Additionally, compared to those who learned a new technology to go online either with help or by themselves, those who did not learn were also more likely to report poor or fair general health (20.6% vs. 12.9% or 7.8%, p < 0.01), probable depression (9.7% vs. 4.7% or 4.9%, p < 0.01) and received help for more than one ADLs (13.8% vs. 9.0% or 8.6%, p < 0.01). The differences were not significant in the number of chronic conditions, probable anxiety, and IADLs.
TABLE 2.
Characteristics of the study population overall and by mode of learning a new technology to go online during the pandemic
| Overall weighted = 100% (Weighted N = 23,547,688; Unweighted N = 2909) | Learn a new technology to go online during the pandemic | ||||
|---|---|---|---|---|---|
| No weighted = 71.8% | With help weighted = 17.4% | By themselves weighted = 10.8% | |||
| (Weighted N = 16,776,060; Unweighted N = 2172) | (Weighted N = 4,067,162; Unweighted N = 466) | (Weighted N = 2,517,399; Unweighted N = 250) | p‐value | ||
| Sociodemographic factors | |||||
| Age at interview (mean [standard error]) | 77.2 (0.1) | 77.8 (0.2) | 76.4 (0.3) | 74.7 (0.2) | <0.01 |
| Male (%) | 45.2 | 47.2 | 38.2 | 43.3 | <0.01 |
| Race/ethnicity (%) | 0.62 | ||||
| Non‐Hispanic whites | 86.2 | 85.9 | 86.2 | 88.7 | |
| Non‐Hispanic blacks | 6.1 | 6.2 | 5.7 | 6.8 | |
| Other | 3.1 | 3.2 | 3.7 | 1.1 | |
| Hispanic | 4.6 | 4.8 | 4.5 | 3.3 | |
| Married or with a partner (%) | 57.1 | 55.4 | 59.4 | 64.4 | 0.09 |
| Education (%) | <0.01 | ||||
| ≤High school | 34.7 | 41.7 | 18.6 | 14.0 | |
| >High school | 65.3 | 58.3 | 81.4 | 86.0 | |
| Income (%) | <0.01 | ||||
| Q1 (income <$28,319) | 22.4 | 26.6 | 13.3 | 8.9 | |
| Q2 ($28,319 ≤ income<$49,731) | 25.1 | 27.0 | 23.4 | 15.9 | |
| Q3 ($49,731 ≤ income<$89,037) | 26.0 | 26.0 | 24.4 | 28.0 | |
| Q4 (income ≥ $89,037) | 26.5 | 20.4 | 38.9 | 47.2 | |
| Clinical factors | |||||
| Self‐health rated (%) | <0.01 | ||||
| Excellent/very good/good | 82.2 | 79.4 | 87.1 | 92.2 | |
| Fair/poor | 17.8 | 20.6 | 12.9 | 7.8 | |
| Number of chronic conditions (%) | 0.38 | ||||
| 0 | 5.9 | 6.1 | 5.6 | 5.0 | |
| 1–2 | 45.1 | 43.6 | 48.6 | 50.0 | |
| 3+ | 48.9 | 50.3 | 45.8 | 45.0 | |
| Probable depression (%) | 8.3 | 9.7 | 4.7 | 4.9 | <0.01 |
| Probable anxiety (%) | 7.0 | 7.8 | 5.0 | 4.8 | 0.16 |
| Received assistance with ≥1 ADL (%) | 12.4 | 13.8 | 9.0 | 8.6 | <0.01 |
| Received assistance with ≥1 IADL (%) | 72.6 | 73.3 | 71.0 | 70.5 | 0.63 |
Note: There were 21 participants who answered they learned a new technology to go online during the pandemic but did not answer whether they learned with help or by themselves.
Abbreviation: ADL, activities of daily living.
The following sociodemographic factors were found to be significantly associated with decreasing odds of learning a new technology to go online (Figure 1): advanced age (adjusted OR [aOR] 0.96; 95%CI: 0.94–0.98), male sex (aOR 0.56; 95% CI: 0.45–0.72), having a high school or lower education level (aOR 0.38; 95%CI: 0.29–0.50), and having an income lower than $89,037 (aOR 0.28 (95%CI: 0.19–0.40), 0.44 (95%CI: 0.30–0.63), and 0.54 (95%CI: 0.39–0.73) for income levels lower than $28,319, between $28,319 and $49,731, between $49,731 and $89,037, respectively). In addition, poor/fair general health was associated with lower odds of learning a new technology to go online during the COVID‐19 pandemic (aOR 0.65; 95%CI: 0.47–0.90, Figure 1). Similar findings were obtained when comparing no learning and learned with help, and comparing no learning and learned by themselves, respectively (data not shown).
FIGURE 1.
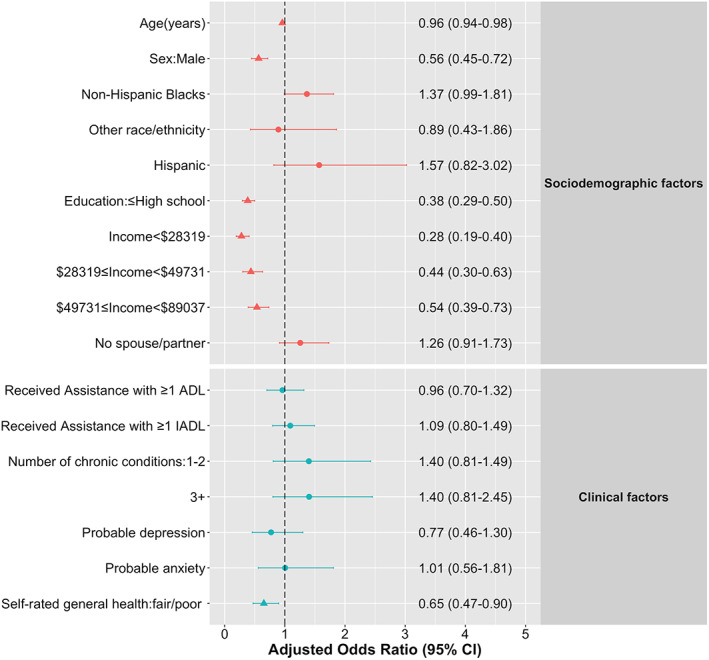
Sociodemographic and clinical factors associated with learning a new technology to go online during the coronavirus disease 2019 (COVID‐19) pandemic among older adults. Significant adjusted odds ratio (ORs) at p < 0.05 were shown in triangles. The reference groups, respectively, were female sex; non‐Hispanic white; education > high school; income ≥$89,037; married or with partner; received no assistance with activity of daily living (ADL); received no assistance with instrumental activities of daily living (IADL); have no chronic conditions; and self‐rated general health: excellent/very good/good
DISCUSSION
The COVID‐19 pandemic has highlighted the importance of using ICT to address daily and healthcare needs, as evidenced by a more than 50% increase in ICT use among older adults during the COVID‐19 pandemic observed in the current study. However, the growth of ICT use during the pandemic and the baseline ICT use before the pandemic were both lower among those who did not learn a new technology to go online, and the proportion of this segment of the older adults was sizable (e.g., 71.8%, equivalent to 25.8 million). Among those who learned a new technology to go online (28.2%), more than half learned with help instead of by themselves, which underscores previous research that older adults need assistance to learn a new technology to go online. 5 , 6 Furthermore, as previously reported, we found that older adults with advanced age, lower education, lower income, and poor/fair general health had reduced odds of learning a new technology to go online during the COVID‐19 pandemic. 7 , 11 Contrary to previous studies, 7 , 11 our analysis showed that males had lower odds of learning a new technology to go online than females. The discrepancies may reflect the differences between the outcomes defined, that is, learning vs. using ICT. It is likely that males already use ICT more than females before the pandemic, and thus did not learn a new technology during the pandemic. However, we did not find differences in ICT use before the pandemic by sex (p > 0.05, data not shown). Furthermore, differences in how the internet was used during COVID‐19 by males and females suggests that more research on sex differences in ICT use is warranted. 16
The strengths of this study include high generalizability because NHATS is representative of community‐dwelling Medicare beneficiaries aged 65 years and older in the United States. To our knowledge, this is the first study to assess barriers to learning a new technology to go online among the US older adults during the COVID‐19 pandemic. A limitation of the study is the potential selection bias as we only included individuals who responded to both 2019 NHATS and COVID‐19 questionnaires. Compared to those who only completed the 2019 NHATS, they were younger, more likely to be of non‐Hispanic white, married, with good self‐rated health and less likely to be depressed (data not shown). Therefore, the observed disparities in increasing ICT use among those did not learn a new technology during the pandemic is likely underestimated. Another limitation of the study is the short time between the beginning of the pandemic and NHATS data collection. We plan to conduct additional analyses to confirm the findings once more NHATS data become available.
This study highlighted clinical and sociodemographic characteristics associated with learning a new technology to go online among U.S. older adults. Addressing these barriers can potentially improve the wider adoption of ICT. Importantly, ICT use may be an indicator of how older adults will use technology for health focused or healthcare specific technologies. A recent study found that prior experience in using online communication technology to contact providers predict the use of patient portals. 17 Given the continued reliance on ICT in daily life and healthcare delivery, learning assistance targeting older adults with identified barriers will help address disparities in ICT use during the COVID‐19 pandemic and beyond.
CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
AUTHOR CONTRIBUTIONS
Study concept and design, data acquisition and analysis: W.L. and B.L.; initial manuscript draft: W.L.; result interpretation and revision of manuscript: B.L., K.A.O., Y.L., and W.L.
SPONSOR'S ROLE
The National Institute on Aging had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Supporting information
Figure S1. Flow chart of study population selection. Note: The selected study population was bold.
ACKNOWLEDGMENTS
This study is in part funded by a grant from the National Institute on Aging (5P30AG028741‐07) awarded to the Claude D Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai.
Li W, Ornstein KA, Li Y, Liu B. Barriers to learning a new technology to go online among older adults during the COVID‐19 pandemic. J Am Geriatr Soc. 2021;69(11):3051-3057. doi: 10.1111/jgs.17433
Funding information This study is in part funded by a grant from the National Institute on Aging (5P30AG028741‐07) awarded to the Claude D Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai. The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) and is conducted at the Johns Hopkins University.
REFERENCES
- 1. Reynolds AL. Age‐related differences in self‐efficacy and the use of e‐Health supports for exercise behavior in adults. Ph.D. Ann Arbor, University of Florida; 2013.
- 2. Van Jaarsveld GM. The effects of COVID‐19 among the elderly population: a case for closing the digital divide. Front Psychiatry. 2020;11:577427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hung LY, Lyons JG, Wu CH. Health information technology use among older adults in the United States, 2009‐2018. Curr Med Res Opin. 2020;36(5):789‐797. [DOI] [PubMed] [Google Scholar]
- 4. Kalicki AV, Moody KA, Franzosa E, Gliatto PM, Ornstein KA. Barriers to telehealth access among homebound older adults. J Am Geriatr Soc. 2021. Apr 13:10.1111/jgs.17163. doi: 10.1111/jgs.17163. Epub ahead of print. PMID: 33848360; PMCID: PMC8250614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reynolds A, Osborne TF. Promoting technology adoption and engagement in aging. In: Chau D, Osborne TF, eds. Springer Publishing Company:19‐38. [Google Scholar]
- 6. Pew Research Center . Older Adults and Technology Use. Published 2014. Accessed May, 2021. https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/
- 7. Gell NM, Rosenberg DE, Demiris G, LaCroix AZ, Patel KV. Patterns of technology use among older adults with and without disabilities. Gerontologist. 2013;55(3):412‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pew Research Center . Tech Adoption Climbs Among Older Adults. Published 2017. Accessed April, 2021. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/
- 9. Elliot AJ, Mooney CJ, Douthit KZ, Lynch MF. Predictors of older adults' technology use and its relationship to depressive symptoms and well‐being. J Gerontol B Psychol Sci Soc Sci. 2014;69(5):667‐677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Travers JL, Hirschman KB, Naylor MD. Adapting Andersen's expanded behavioral model of health services use to include older adults receiving long‐term services and supports. BMC Geriatr. 2020;20(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim J, Lee HY, Christensen MC, Merighi JR. Technology access and use, and their associations with social engagement among older adults: do women and men differ? J Gerontol B Psychol Sci Soc Sci. 2016;72(5):836‐845. [DOI] [PubMed] [Google Scholar]
- 12. National Health and Aging Trends Study . National Health and Aging Trends Study COVID‐19 Questionnaire. Published 2020. Accessed January, 2021. https://www.nhats.org/sites/default/files/2021-01/NHATS%20R10%20COVID-19%20Questionnaires.pdf
- 13. National Health and Aging Trends Study . COVID‐19 Supplement to the National Health and Aging Trends Study USER GUIDE. Published 2020. Accessed January, 2021. https://www.nhats.org/sites/default/files/inline-files/NHATS%20COVID-19%20User%20Guide%20Beta%20Release_0.pdf
- 14. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra‐brief screening scale for anxiety and depression: the PHQ‐4. Psychosomatics. 2009;50(6):613‐621. [DOI] [PubMed] [Google Scholar]
- 15. Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD‐7) in the general population. Med Care. 2008;46(3):266‐274. [DOI] [PubMed] [Google Scholar]
- 16. Campos‐Castillo C. Gender divides in engagement with COVID‐19 information on the internet among U.S. older adults. J Gerontol B Psychol Sci Soc Sci. 2020;76(3):e104‐e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hong YA, Jiang S, Liu PL. Use of patient portals of electronic health records remains low from 2014 to 2018: results from a national survey and policy implications. Am J Health Promot. 2020;34(6):677‐680. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Flow chart of study population selection. Note: The selected study population was bold.


