Abstract
Background
Understanding the physical and mental changes in community‐dwelling elderly people is very important during the coronavirus disease 2019 (COVID‐19) pandemic when considering preventive measures. The purpose of this study was to clarify the changes of physical function and anxiety for activities of daily living in community‐dwelling older adults, focusing on locomotor function during the COVID‐19 pandemic.
Methods
The study participants were 127 older people who participated in successive surveys, in the summers of 2019 and again in 2020, after the state of emergency. The Locomo 25 questionnaire, Geriatric Depression Scale‐15 (GDS‐15) questionnaire, medical history, and number of people living together were self‐reported. The Locomo 25 covers six aspects of physical pain, movement‐related difficulty, usual care, daily activity, social activities, and anxiety.
Results
The paired samples t‐test revealed that Locomo 25 total scores in 2020 were significantly higher than those in 2019. The GDS‐15 score showed no significant difference. The comparison of scores for each item of the Locomo 25 revealed significantly higher scores in 2020 on Q21 (‘difficult to perform sports activity’, P = 0.0021), Q22 (‘restricted from meeting own friends’, P < 0.001), Q23 (‘restricted from joining social activities’, P < 0.001), Q24 (‘anxious about falling in own house’, P = 0.0023), and Q25 (‘anxious about being unable to walk in the future’, P = 0.0016).
Conclusions
About 2 months after declaration of the first state of emergency due to the COVID‐19 pandemic in Japan, social activity was severely restricted. Older adults showed almost no changes in body pain and locomotive disabilities, but increases in their anxieties about walking ability and falling were remarkable.
Keywords: anxiety, COVID‐19, fear of falling, Locomo 25, older adults
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic, which began in 2019, has significantly changed people's lives and behaviours. In January 2020, the first infected person was confirmed in Japan. After that, the number of infected people increased, and an emergency declaration was issued on April 7, 2020. Although restrictions on going out were not as strong as those in the EU lockdown, recommended infection control measures in Japan included cancelling some events, refraining from going out unnecessarily, school closures, recommendations for telework, keeping physical distance as much as possible, wearing a mask, washing hands, gargling, etc. After that, people were recommended to continue the above new lifestyle even after the state of emergency was lifted on May 25, 2020. A second state of emergency was subsequently issued in January 2021, and a third state of emergency was issued in April 2021, with the above restrictions reinstituted.
Mortality from coronavirus infection in healthy adults has been reported to be about 2–3%, and is about three times higher in the elderly.1 Scientists have speculated that older people are at increased risk of being more seriously affected by COVID‐19 infection because viral infection can exacerbate symptoms from existing diseases. Furthermore, pandemic stress can also increase mental illness in older people with a weakened immune system.2
Under these circumstances, the total physical activity time in the elderly living in the community in Japan decreased significantly in April 2020 compared to January 2020.3 Numerous studies abroad have also shown that people's physical activity during the COVID‐19 pandemic is decreasing, and sitting time is increasing.4, 5 Physical activity is one of the key behavioural factors that has a positive impact on health outcomes, including reduced risk of chronic illness, increased cognitive function, and improved mental health.6, 7 In addition, restrictions on going out have weakened social connections, which are deeply linked to the nervous system, endocrine system, and immune system. The feeling of loneliness caused by social isolation causes mood and cognitive decline, alters the regulation of inflammatory responses in the body, damages the immune system, and impairs concentration and sleep habits.8
Understanding the physical and mental changes in the elderly living in the community is very important in such a situation when considering preventive measures. However, most reports have described abstract anxiety feelings in young people, and few reports have described self‐evaluated motor function in elderly people.
We have been conducting health classes and physical fitness tests for older adults living in Kaizuka City in Osaka Prefecture. In general, older adults who attend the event are healthy and are very active in promoting their own health. However, this pandemic has forced many, including these people, to refrain from social activities. Therefore, the purpose of this study was to clarify the changes in physical function and anxiety for activities of daily living in community‐dwelling older adults, focusing on locomotor function during restrictions on going out during the COVID‐19 pandemic.
METHODS
Study design and participants
The study was conducted in Kaizuka City, Osaka Prefecture, Japan, between 2019 and 2020 for community‐dwelling Japanese aged 60 and older. Kaizuka City is located about 30 km south of the centre of Osaka City, close to Kansai International Airport, and is a rural area with an ageing rate of 24.9%. All participants took part in the annual health check co‐sponsored by Osaka Kawasaki Rehabilitation University and the Kaizuka City Elderly Care Division. Surveys in the summer of 2019 assessed the elderly in the community who participated in a health check, which is an event to measure athletic ability and body composition, and to answer a questionnaire about their locomotive function. The survey in the summer of 2020 (after the first state of emergency was lifted) assessed the older adults in the community who were sent a questionnaire about their locomotive function in July and responded by mid‐August. The 2019 survey included 272 participants. In the 2020 survey, 504 people who had participated in the previous health check were mailed questionnaires, and 283 of these people returned their answers. We analysed 127 of the 195 people who participated in both 2019 and 2020, excluding 68 people (14 who were under the age of 60 years, and 54 who did not answer the questionnaire completely; Fig. 1).
Figure 1.
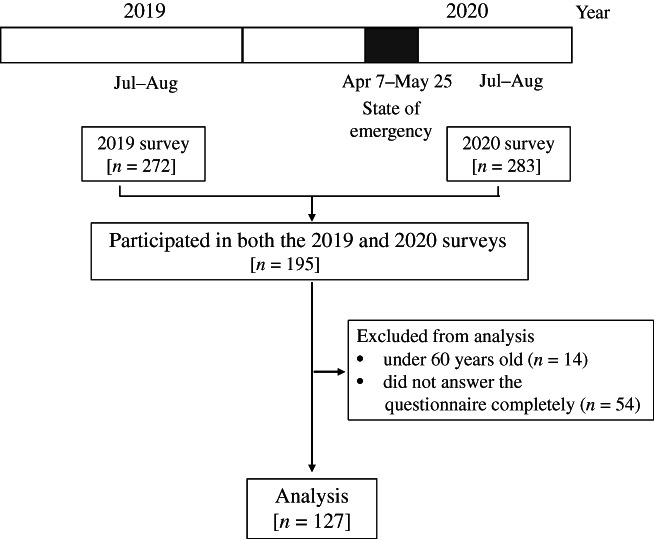
Flow chart showing the survey periods and the participants recruited in the study.
This study was approved by the Ethics Committee of Osaka Kawasaki Rehabilitation University (Reference No. OKRU20‐A013) and performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants before the study began.
Questionnaires
The questionnaires included the Locomo 25 questionnaire, Geriatric Depression Scale‐15 (GDS‐15), and queries about medical history (Alzheimer's disease, cerebrovascular dementia, stroke, Parkinson's disease, hypertension, diabetes mellitus, hyperlipidaemia, respiratory disease, osteoporosis, osteoarthritis, fractures after age 60 years, depression) and the number of people living together at the time of the investigation. Locomo 25 is a self‐administered questionnaire proposed by the Japanese Orthopaedic Association that subjectively screens for locomotive syndrome. The questionnaire contains 25 questions aimed at explaining the six aspects of physical pain (Q1–Q4), movement‐related difficulty (Q5–Q7), usual care (Q8–Q11, Q14), daily activity (Q12, Q13, Q15–Q17, Q19, Q20), social activities (Q18, Q21–Q23), and anxiety (Q24, Q25), with 0 (no impairment) to 4 (severe impairment) points for each.9, 10 Higher scores indicate worse locomotive function. The GDS‐15, which is a commonly used instrument for depression screening in the general geriatric population, was used to assess depression status.11
Statistical analysis
The paired samples t‐test was performed to compare variables between survey years. All statistical tests were two‐tailed, and P values <0.05 were considered to indicate statistical significance. All statistical analyses were conducted using JMP11 Statistics software (SAS Institute, Cary, NC).
RESULTS
Characteristics of the study participants
Table 1 shows the characteristics of the study participants. The paired samples t‐test revealed a significant difference in the Locomo 25 total scores between 2019 and 2020 (P < 0.001). The Locomo 25 total scores in 2020 were significantly higher than those in 2019. The GDS‐15 score showed no significant difference (Table 1).
Table 1.
Characteristics of the study participants
| Survey year | 2019 | 2020 | P |
|---|---|---|---|
| N (% men) | 127 (26.8%) | ||
| Age (years) | 73.65 (6.01) | 74.52 (6.00) | <0.0001 |
| Locomo 25 score (points) | 7.47 (8.19) | 10.27 (1.00) | <0.0001 |
| GDS‐15 score (points) | 3.22 (2.97) | 2.99 (2.44) | 0.2204 |
| Living alone | 28 (22.0%) | ||
| Medical history | |||
| Alzheimer's disease | 0 (0%) | ||
| Cerebrovascular dementia | 1 (0.8%) | ||
| Stroke | 5 (3.9%) | ||
| Parkinson's disease | 0 (0%) | ||
| Hypertension | 51 (40.2%) | ||
| Diabetes mellitus | 14 (11.0%) | ||
| Hyperlipidaemia | 31 (24.4%) | ||
| Respiratory disease | 9 (7.1%) | ||
| Osteoporosis | 28 (22.0%) | ||
| Osteoarthritis | 19 (15.0%) | ||
| Fractures after age 60 years | 20 (15.7%) | ||
| Depression | 7 (5.5%) | ||
Data are presented as means (standard deviation) or as prevalence (percentage). The paired samples t‐test was used to compare variables between survey years. GDS‐15, Geriatric Depression Scale‐15.
Comparison of scores for each item of the Locomo 25 between 2019 and 2020
Table 2 shows the comparison of scores for each item of the Locomo 25 between 2019 and 2020. The paired samples t‐test revealed significantly higher scores in 2020 than 2019 on Q21 (‘difficult to perform sports activity’, P = 0.0021), Q22 (‘restricted from meeting own friends’, P < 0.001), Q23 (‘restricted from joining social activities’, P < 0.001), Q24 (‘anxious about falling in own house’, P = 0.0023), and Q25 (‘anxious about being unable to walk in the future’, P = 0.0016).
Table 2.
Comparison of scores for each item in Locomo 25 between survey years
| Survey year | 2019 | 2020 | P |
|---|---|---|---|
| Q1. Did you have any pain (including numbness) in your neck or upper limbs (shoulder, arm, or hand)? | |||
| 0.72 (0.89) | 0.72 (0.87) | 0.9297 | |
| Q2. Did you have any pain in your lower back or buttocks? | |||
| 0.71 (0.80) | 0.75 (0.84) | 0.5605 | |
| Q3. Did you have any pain (including numbness) in your lower limbs (hip, thigh, knee, calf, shin, ankle, or foot)? | |||
| 0.65 (0.86) | 0.76 (0.96) | 0.1362 | |
| Q4. To what extent has it been painful to move your body in daily life? | |||
| 0.43 (0.61) | 0.51 (0.71) | 0.1664 | |
| Q5. To what extent has it been difficult to get up from a bed or lie down? | |||
| 0.12 (0.32) | 0.15 (0.40) | 0.3478 | |
| Q6. To what extent has it been difficult to stand up from a chair? | |||
| 0.11 (0.31) | 0.13 (0.36) | 0.5337 | |
| Q7. To what extent has it been difficult to walk inside the house? | |||
| 0.05 (0.21) | 0.09 (0.28) | 0.0585 | |
| Q8. To what extent has it been difficult to put on and take off a shirt? | |||
| 0.02 (0.15) | 0.03 (0.18) | 0.7070 | |
| Q9. To what extent has it been difficult to put on and take off trousers and pants? | |||
| 0.08 (0.27) | 0.13 (0.36) | 0.1091 | |
| Q10. To what extent has it been difficult to use the toilet? | |||
| 0.02 (0.15) | 0.05 (0.21) | 0.3192 | |
| Q11. To what extent has it been difficult to wash your body in the bath? | |||
| 0.02 (0.12) | 0.04 (0.20) | 0.2585 | |
| Q12. To what extent has it been difficult to go up and down stairs? | |||
| 0.48 (0.76) | 0.42 (0.74) | 0.2498 | |
| Q13. To what extent has it been difficult to walk briskly? | |||
| 0.51 (0.81) | 0.57 (0.87) | 0.2780 | |
| Q14. To what extent has it been difficult to keep yourself neat? | |||
| 0.04 (0.20) | 0.05 (0.25) | 0.7643 | |
| Q15. How far can you keep walking without rest? (please select the closest answer) | |||
| 0.68 (1.04) | 0.61 (0.92) | 0.3678 | |
| Q16. To what extent has it been difficult to go out to visit neighbours? | |||
| 0.06 (0.33) | 0.06 (0.33) | 1.0000 | |
| Q17. To what extent has it been difficult to carry objects weighing approximately 2 kg (2 standard milk bottles or 2 PET bottles each containing 1 l)? | |||
| 0.31 (0.71) | 0.42 (0.86) | 0.0576 | |
| Q18. To what extent has it been difficult to go out using public transportation? | |||
| 0.13 (0.40) | 0.15 (0.47) | 0.5337 | |
| Q19. To what extent have simple tasks and housework (preparing meals, cleaning up, etc.) been difficult? | |||
| 0.07 (0.29) | 0.11 (0.36) | 0.2267 | |
| Q20. To what extent have load‐bearing tasks and housework (cleaning the yard, carrying heavy bedding, etc.) been difficult? | |||
| 0.31 (0.61) | 0.37 (0.76) | 0.3036 | |
| Q21. To what extent has it been difficult to perform sports activity (jogging, swimming, gate ball, dancing, etc.)? | |||
| 0.55 (0.91) | 0.79 (1.09) | 0.0021 | |
| Q22. Have you been restricted from meeting your friends? | |||
| 0.24 (0.61) | 1.11 (1.18) | <0.0001 | |
| Q23. Have you been restricted from joining social activities (meeting friends, playing sports, engaging in activities and hobbies, etc.)? | |||
| 0.50 (0.96) | 1.43 (1.42) | <0.0001 | |
| Q24. Have you ever felt anxious about falls in your house? | |||
| 0.24 (0.44) | 0.39 (0.66) | 0.0023 | |
| Q25. Have you ever felt anxious about being unable to walk in the future? | |||
| 0.46 (0.70) | 0.66 (0.83) | 0.0016 | |
Data are presented as means (standard deviation). The paired samples t‐test was used to compare variables between survey years.
DISCUSSION
In this study, we investigated the mental and physical changes related to activities of daily living in community‐dwelling older adults before (2019) and during the COVID‐19 pandemic (2020) using the Locomo 25 questionnaire. As a result, Locomo 25 items Q21–Q25 each showed a significant increase in 2020 compared to 2019. Regarding Q21, ‘difficult to perform sports activity’, Q22, ‘restricted from meeting own friends’, and Q23, ‘restricted from joining social activities’, we presume that the participants in 2020 experienced a decline in social participation due to restrictions on going out because of the state of emergency.
Furthermore, we observed a significant increase in the anxiety‐related items Q24, ‘anxious about falling in own house’, and Q25, ‘anxious about being unable to walk in the future’, in 2020. An increase in the Q24 score indicates that the fear of falling (FOF) in the house has increased during the COVID‐19 pandemic. Falls and fractures are the third leading cause of becoming bedridden in the elderly. The underlying cause is often an overestimation of the older person's own motor function. On the other hand, the amount of physical activity may decrease due to excessive FOF, resulting in a fall. Older adults with FOF have reduced activity due to a combination of reduced range of activity, decreased activity frequency,12 and less frequent outdoor activities,13 leading to a poor quality of life.14, 15 FOF may be associated with decreased physical and social activity, along with physical conditions such as dizziness, other illnesses,16 gait function and imbalance, as well as fracture experience, rather than direct fall experience.17, 18, 19 The increase in FOF may be due to physical and psychological changes caused by deterioration of physical and social activities during the COVID‐19 pandemic. FOF is associated with frailty, sarcopenia, and impaired cognitive function.16, 20, 21, 22 Maintenance of daily physical activity prevents anxiety, including FOF, and prevents deterioration of physical function.23 Therefore, maintaining physical activity and psychological care is important for preventing frailty syndrome and disease onset due to the COVID‐19 pandemic.
An increase in the score on item Q25, ‘anxious about being unable to walk in the future’, indicates that the COVID‐19 pandemic increased anxiety about future walking. More than half of the participants in other studies on the impact among the elderly of COVID‐19 reported exacerbated depression and increased loneliness associated with anxiety.24, 25 These results reflect the relationship between a sedentary lifestyle and anxiety26, 27 and depression.28 On the other hand, a significant correlation is present between frailty and subjective, self‐judged weakness in the leg muscles by older community‐living Japanese during the COVID‐19 pandemic.29, 30 This result indicates that the evaluation of self‐weakness by older participants is highly reliable. We speculate that uncertainty associated with the self‐restraint restriction period due to the COVID‐19 pandemic may have led to a loss in confidence in the walking function of the elderly. In addition, we speculate that the increase in the score for ‘difficulty walking in the house’ (Q7) is also behind the increase in the score for these types of anxiety.
In conclusion, about 2 months after the declaration of the first state of emergency due to the COVID‐19 pandemic in Japan, older adults showed almost no changes in body pain and locomotive disabilities, but the increases in their anxieties about walking ability and falling were remarkable.
LIMITATIONS
The present study has a number of limitations. First, there is a bias in the selection of subjects. The subjects of this research were those who participated in the health check so far and are highly conscious of their health. Second, the present results are only based on individual subjective assessments, as Locomo 25 is a self‐administered questionnaire. In the future, investigation of objective indicators will be necessary. Third, because the details of the behavioural regulation imposed by the declaration of emergency due to the COVID‐19 pandemic are unique to Japan, careful interpretation of these results is required.
AUTHOR CONTRIBUTIONS
The present work was carried out in collaboration among all authors. M.N. wrote the manuscript; M.I., H.N., M.H., R.I., and F.T. contributed to the study design and management; M.T. contributed to the discussions.
ETHICAL STANDARDS
The Ethics Committee of Osaka Kawasaki Rehabilitation University approved the study protocol (Reference No. OKRU20‐A013). All participants provided written informed consent.
ACKNOWLEDGMENTS
The authors thank Ms. Kaori Hamamura, Ms. Hiroko Fujiwara, and Mr. Hiroshi Tousuji of the Kaizuka City Office, Welfare Department Elderly Care section; Ms. Ritsuko Tanaka; and the many students at Osaka Kawasaki Rehabilitation University for their assistance with examinations and measurements. This research was supported by Joint Research Funds of Osaka Kawasaki Rehabilitation University in 2018, 2019, and 2020 and by JSPS KAKENHI (Grant Number; 18K10800). The funders had no role in the design of the study, the collection, analysis, and interpretation of the data, or the writing of the manuscript.
Disclosure: The authors declare no conflicts of interest.
References
- 1.Banerjee D. The COVID‐19 outbreak: crucial role the psychiatrists can play. Asian J Psychiatr 2020; 50: 102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of the COVID‐19 pandemic on Alzheimer's disease and related dementias. Am J Geriatr Psychiatry 2020; 28: 712–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamada M, Kimura Y, Ishiyama Det al. Effect of the COVID‐19 epidemic on physical activity in community‐dwelling older adults in Japan: a cross‐sectional online survey. J Nutr Health Aging 2020; 24: 948–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castañeda‐Babarro A, Arbillaga‐Etxarri A, Gutiérrez‐Santamaría B, Coca A. Physical activity change during COVID‐19 confinement. Int J Environ Res Public Health 2020; 17: 6878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallè F, Sabella EA, Ferracuti Set al. Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of CoViD‐19 pandemic. Int J Environ Res Public Health 2020; 17: 6171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blondell SJ, Hammersley‐Mather R, Veerman JL. Does physical activity prevent cognitive decline and dementia? A systematic review and meta‐analysis of longitudinal studies. BMC Public Health 2014; 14: 510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feter N, Caputo EL, Smith ECet al. Association between physical activity and subjective memory decline triggered by the COVID‐19 pandemic: findings from the PAMPA cohort. Prev Med 2021; 145: 106415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Santini ZI, Jose PE, York Cornwell Eet al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 2020; 5: e62–e70. [DOI] [PubMed] [Google Scholar]
- 9.Seichi A, Hoshino Y, Doi T, Akai M, Tobimatsu Y, Iwaya T. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25‐question Geriatric Locomotive Function Scale. J Orthop Sci 2012; 17: 163–172. [DOI] [PubMed] [Google Scholar]
- 10.Wang C, Ikemoto T, Hirasawa A, Arai YC, Kikuchi S, Deie M. Assessment of locomotive syndrome among older individuals: a confirmatory factor analysis of the 25‐question Geriatric Locomotive Function Scale. Peer J 2020; 8: e9026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shiekh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, ed. Clinical Gerontology: A Gutide to Assessnment and Intervention. New York: Haworth Press; 1986; 165–173. [Google Scholar]
- 12.Bertera EM, Bertera RL. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health Soc Work 2008; 33: 54–62. [DOI] [PubMed] [Google Scholar]
- 13.Spaltenstein J, Bula C, Santos‐Eggimann B, Krief H, Seematter‐Bagnoud Let al. Factors associated with going outdoors frequently: a cross‐sectional study among Swiss community‐dwelling older adults. BMJ Open 2020; 10: e034248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howland J, Peterson EW, Levin WC, Fried L, Pordon D, Bak S. Fear of falling among the community‐dwelling elderly. J Aging Health 1993; 5: 229–243. [DOI] [PubMed] [Google Scholar]
- 15.Akosile CO, Igwemmadu CK, Okoye ECet al. Physical activity level, fear of falling and quality of life: a comparison between community‐dwelling and assisted‐living older adults. BMC Geriatr 2021; 21: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health 1994; 84: 565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DIet al. Fear of falling and fall‐related efficacy in relationship to functioning among community‐living elders. J Gerontol 1994; 49: M140–M147. [DOI] [PubMed] [Google Scholar]
- 18.Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A. Covariates of fear of falling and associated activity curtailment. Gerontologist 1998; 38: 549–555. [DOI] [PubMed] [Google Scholar]
- 19.Legters K. Fear of falling. Phys Ther 2002; 82: 264–272. [PubMed] [Google Scholar]
- 20.Merchant RA, Chen MZ, Wong BLLet al. Relationship between fear of falling, fear‐related activity restriction, frailty, and sarcopenia. J Am Geriatr Soc 2020; 68: 2602–2608. [DOI] [PubMed] [Google Scholar]
- 21.Esbrí‐Víctor M, Huedo‐Rodenas I, López‐Utiel Met al. Frailty and fear of falling: the FISTAC study. J Frailty Aging 2017; 6: 136–140. [DOI] [PubMed] [Google Scholar]
- 22.Vo THM, Nakamura K, Seino K, Nguyen HTL, Van Vo TV. Fear of falling and cognitive impairment in elderly with different social support levels: findings from a community survey in Central Vietnam. BMC Geriatr 2020; 20: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levinger P, Panisset M, Dunn Jet al. Exercise interveNtion outdoor proJect in the cOmmunitY for older people – results from the ENJOY Seniors Exercise Park project translation research in the community. BMC Geriatr 2020; 20: 446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kotwal AA, Holt‐Lunstad J, Newmark RLet al. Social isolation and loneliness among San Francisco Bay Area older adults during the COVID‐19 shelter‐in‐place orders. J Am Geriatr Soc 2020; 23: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grolli RE, Mingoti MED, Bertollo AGet al. Impact of COVID‐19 in the mental health in elderly: psychological and biological updates. Mol Neurobiol 2021; 58: 1905–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vancampfort D, Stubbs B, Herring MP, Hallgren M, Koyanagi Aet al. Sedentary behavior and anxiety: association and influential factors among 42,469 community‐dwelling adults in six low‐ and middle‐income countries. Gen Hosp Psychiatry 2018; 50: 26–32. [DOI] [PubMed] [Google Scholar]
- 27.Vancampfort D, Stubbs B, Smith Let al. Correlates of sedentary behavior among community‐dwelling adults with anxiety in six low‐ and middle‐income countries. Psychiatry Res 2019; 273: 501–508. [DOI] [PubMed] [Google Scholar]
- 28.Andrade‐Gómez E, Martínez‐Gómez D, Rodríguez‐Artalejo F, García‐Esquinas Eet al. Sedentary behaviors, physical activity, and changes in depression and psychological distress symptoms in older adults. Depress Anxiety 2018; 35: 884–897. [DOI] [PubMed] [Google Scholar]
- 29.Suzuki Y, Maeda N, Hirado D, Shirakawa T, Urabe Y. Physical activity changes and its risk factors among community‐dwelling Japanese older adults during the COVID‐19 epidemic: associations with subjective well‐being and health‐related quality of life. Int J Environ Res Public Health 2020; 17: 6591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takashima R, Onishi R, Saeki K, Hirano M. Perception of COVID‐19 restrictions on daily life among Japanese older adults: a qualitative focus group study. Healthcare 2020; 8: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]


