Abstract
COVID‐19‐associated discrimination (CAD) is an important issue that may adversely affect frontline nurses’ work effectiveness and well‐being. This study examined the relationships between frontline nurses’ perceptions of COVID‐19‐associated discrimination and their resilience, mental health, and professional‐turnover intention. This cross‐sectional descriptive study involved 259 frontline nurses in the Central Philippines and used four online self‐report measures. The results revealed that frontline nurses perceived a moderate level of COVID‐19‐associated discrimination. Frontline nurses who perceived a higher level of discrimination during the coronavirus pandemic reported poorer mental health and higher professional‐turnover intention. Resilience acted as a mediator and reduced the effects of COVID‐19‐associated discrimination on nurses’ mental health and their professional‐turnover intention. Proactive measures to reduce the negative consequences of discrimination during the pandemic, and efforts to foster resilience in nurses who are in the forefront of the fight against the highly transmissible virus, should be given high priority by hospital and nursing administrators to better support nurses’ mental health and foster retention.
Keywords: COVID‐19, discrimination, mental health, nursing, resilience, turnover intention
Introduction
Discriminatory acts or behaviours against healthcare workers who support the fight against the virus have spiked at alarming rates since the onset of the pandemic. COVID‐19‐associated discrimination is defined as ‘a form of discrimination towards individuals who share social or behavioural characteristics with COVID‐19 patients but may not necessarily carry the virus’ (Liu et al. 2020; p. 482). Discrimination occurs most often during infectious disease outbreaks, including the current pandemic, as a result of extreme fear and misinformation (Ransing et al. 2020; Schoch‐Spana et al. 2010). COVID‐19‐associated discrimination was initially observed online against the Chinese people and later extended to other people of Asian origin (Budhwani & Sun 2020). Evidence have shown a substantial increase of racist attitudes, bullying, discriminatory behaviours, and hateful acts against these individuals, which were later extended to those who were afflicted or had recovered from the disease, their family members, and healthcare personnel (Abuhammad et al. 2021; Islam et al. 2020). Among these groups, reports suggest an increased likelihood of experiencing COVID‐19‐associated discrimination, social exclusion and/or rejection, and stigma among healthcare workers (Dye et al. 2020).
Reports worldwide have shown an increase in the number of healthcare workers, including nurses, who are experiencing discrimination, threatening gestures, and harassment since the onset of the pandemic (Ransing et al. 2020). As well, empirical evidence has shown an increasing number of healthcare personnel reporting being threatened, stigmatized, and socially discriminated against since the onset of the coronavirus outbreak (Cassiani‐Miranda et al. 2021; Sotgiu & Dobler 2020). A report from Jordan estimated that about 21% of healthcare workers (HCWs) experienced moderate levels of social discrimination, while 25% experienced a higher level of social discrimination (Dalky et al. 2020). In India, a much higher percentage (50%) of HCWs reported increased apprehension due to stigma from the community where they lived, while 70% reported experiencing rude and threatening behaviours from the community (Yadav et al. 2020). In research spanning multiple countries, Dye et al. (2020) found that discrimination, bullying, and stigma against HCWs during the pandemic varied according to region of the world. In particular, HCWs in Asia, Africa, North America, and Oceania experienced a higher level of social discrimination that those in Latin America and Europe. Among HCWs, a greater extent of COVID‐19‐associated discrimination was observed in those with lower qualifications, particularly among those who worked in quarantine hospitals (Mostafa et al. 2020), those who did not receive COVID‐19‐related training, and those with pre‐existing mental health issues (Teksin et al. 2020).
As the largest group of healthcare personnel who are on the frontlines in the fight against the coronavirus, nurses are most at risk of experiencing discriminatory acts or behaviours from the public. Constant exposure to these behaviours along with other pandemic‐related stressors may have an adverse impact on nurses’ mental health and well‐being and work outcomes. Available evidence has suggested that constant exposure to threats, bullying, stigmatization, and discriminatory acts from the public may potentially and negatively affect nurses’ clinical performance and work satisfaction (Ramaci et al. 2020; Teksin et al. 2020). A growing number of studies have strongly linked increased perceptions of discrimination during the pandemic to poorer mental health, reduced psychological well‐being, increased frustration and loneliness, a higher level of job burnout, and psychological and emotional trauma in frontline nurses (Kwaghe et al. 2020; Ransing et al. 2020; Zandifar et al. 2020). Collectively, these conditions could potentially drive nurses to leave their jobs and/or the profession, further aggravating the looming nursing shortage and negatively affecting patients’ quality of care and the overall delivery of healthcare services.
Considering the untoward effects of discriminatory acts against frontline nurses and other members of the healthcare team during the pandemic, it is imperative that measures be initiated to minimize or reduce the work‐ and health‐related outcomes of such acts. Hospital and nursing administrators play an essential role in ensuring that nurses are equipped with the necessary resources to effectively handle the psychological and mental health burden resulting from discrimination. The vital role of resilience during crises, emergency and disaster events, and other traumatic situations had been clearly established in the literature (Cooper et al. 2021). Resilience refers to an individual’s capabilities to rebound from traumatic events and has long been recognized as a protective factor for mental health. Previous outbreaks of illnesses and diseases, including Ebola, SARS, H1N1, and MERS, have identified the protective effects of resilience against various psychological and mental ill effects in nurses who were directly involved in the care of infected patients (De Brier et al. 2020; Schreiber et al. 2019). During the height of the coronavirus outbreak, when psychological and mental health burdens were high, resilience allowed nurses to rebound successfully (Sumner & Kinsella 2021), resulting in sustained clinical performance and improved mental health (Labrague 2021; Zhang et al. 2021). Moreover, resilience served as an important mediator to significantly decrease the negative effects of the ongoing pandemic on nurses’ emotional, psychological, and mental health (Lorente et al. 2021; Serrão et al. 2021). Therefore, resilience may also act as a mediator to reduce the effect of discrimination related to COVID‐19 on nurses’ health and work productivity. However, the mechanism explaining how resilience might reduce the effects of COVID‐19‐associated discrimination on nurses’ mental health and work outcomes remains unexplored. Consequently, this study assessed the influence of COVID‐19‐associated discrimination on frontline nurses’ mental health and their intention to quit the nursing profession with resilience acting as a mediator.
Methods
Design, sample, and setting
This cross‐sectional study used an online survey to collect data from clinical nurses in the Central Philippines. Licensed‐registered nurses with at least 6 months of work experience in their current unit and who were directly involved in the care of coronavirus patients were eligible for the study. The sample size was determined using G*Power software, with an effect size of 0.05, an alpha value of 0.05, and statistical power of 80%, resulting in 220 nurses. The online survey was sent to 300 nurses, of which 259 (86% response rate) completed the survey.
Instruments
The COVID‐19‐Associated Discrimination scale (CAD; Liu et al. 2020) was utilized to examine nurses’ experiences of discriminatory behaviour from the public since the onset of the pandemic. The scale contained four items answerable by a response of ‘yes’, ‘no’, or ‘unsure’. A ‘yes’ response was coded as 1, while ‘no’ and ‘unsure’ were assigned 0. Nurses responded to questions asking whether they had experienced the following due to people thinking they might have the coronavirus: (a) treated with less courtesy and respect than others, (b) received poorer service at restaurants or stores, (c) people acted afraid of them, and (d) threatened or harassed. The scales’ predictive validity and internal consistency were found to be acceptable in previous research (Liu et al. 2020).
Resilience was examined using the Brief Resilient Coping Skills (BRCS; Smith et al. 2008). The BRCS contained four items answerable by a five‐point Likert scale ranging from 0 (does not describe me at all) to 5 (describes me very well). Higher mean scores represent greater resilience. This scale has been widely used to examine resilience levels both in nursing and non‐nursing populations. Research before and during the pandemic has shown an acceptable predictive validity and reliability with Cronbach’s alpha values ranging from 0.84 to 0.93 (Labrague and De los Santos, 2020, 2021).
The Mental Health Inventory (MHI; Veit & Ware 1983) was used to determine frontline nurses’ mental health status during the coronavirus pandemic. The scale consisted of 5 items which asked about nurses’ feelings during the previous months utilizing a six‐point Likert scale from 0 (none of the time) to 5 (all of the time), with higher scores indicating poorer mental health. This scale has been used to examine mental health status in the nursing population and the general public and has shown excellent criterion and predictive validity and internal consistency (Berwick et al. 1991).
Turnover intention was assessed using a single item measure answerable by a five‐point Likert scale ranging from 0 (strongly disagree) to 5 (strongly agree). Nurses responded to the item, ‘Given the current situation, I am more likely to leave my profession’. This single item measure of turnover intention has been previously used to examine professional‐turnover intention before and during the pandemic and has shown excellent criterion validity and reliability (Labrague and De los Santos, 2020, 2021).
The Cronbach’s alpha values of the multi‐items scales were 0.91 (Mental Health Inventory), 0.85 (COVID‐19‐Associated Discrimination scale), and 0.85 (Brief Resilient Coping Skills).
Data collection and ethical review
Samar State University Institutional Research Ethics Review Committee (IRERC) (IRERC EA0012‐I) provided ethical approval for the study. After obtaining ethical clearance, the official email addresses and/or the official social media accounts of nurses in the region were secured. Given the current restrictions due to the pandemic regarding the in‐person collection of research data, an online questionnaire administered via Google Forms was used to collect the data. The first page of the survey provided a description of the study and a statement seeking participants’ informed consent. Nurses who agreed to partake in the study were asked to press the ‘yes’ button and were then directed to the survey questionnaire, while those who opted not to participate were asked to press the ‘no’ button and were directed to the exit page. Weekly reminders were sent to potential participants’ email addresses asking them to complete the survey. To ensure participants’ confidentiality, nurses were not required to enter personal information. Data were collected from November 2020 to December 2020.
Data analysis
Prior to data analysis, data were inspected for missing values. The Statistical Package for Social Sciences (SPSS) version 23 was used to analyse the data, and inferential and descriptive statistics were calculated. The direct and indirect effect of discrimination on nurses’ mental health and professional‐turnover intention was calculated using multiple linear regressions. The three‐step approach described by Sobel was adhered to when examining the mediating effects of resilience on the relationships between discrimination and nurses’ mental health and professional‐turnover intention.
Results
A total of 259 frontline nurses responded to our online questionnaire. The mean age and years of nursing experience were 34.86 and 10.67 years, respectively. Most participants were female, unmarried, worked fulltime, and held BSN degrees and staff nurse positions (Table 1).
Table 1.
Nurse characteristics (n = 259)
| Variables | Category | n | % | Mean | SD | Test statistic | P value |
|---|---|---|---|---|---|---|---|
| Age † | 34.861 | 8.832 | −0.133 | 0.032 | |||
| Years of experience in nursing † | 10.671 | 7.532 | −0.112 | 0.032 | |||
| Years of experience in the organization † | 6.065 | 5.580 | −0.066 | 0.290 | |||
| Gender ‡ | Male | 66 | 25.5 | 2.311 | 0.494 | −0.908 | 0.365 |
| Female | 193 | 74.5 | 2.376 | 0.505 | |||
| Marital status ‡ | Married | 112 | 43.2 | 2.330 | 0.505 | −0.802 | 0.424 |
| Unmarried | 147 | 56.8 | 2.381 | 0.501 | |||
| Education ‡ | BSN | 205 | 79.2 | 2.356 | 0.510 | −0.185 | 0.848 |
| MSN | 54 | 20.8 | 2.370 | 0.478 | |||
| Job status ‡ | Fulltime | 234 | 90.3 | 2.370 | 0.509 | 1.038 | 0.249 |
| Part time | 25 | 9.7 | 2.260 | 0.436 | |||
| Job role ‡ | Staff nurse | 180 | 69.5 | 2.389 | 0.525 | 1.445 | 0.125 |
| Nurse manager | 79 | 30.5 | 2.291 | 0.443 | |||
| Facility size § | Small | 90 | 34.7 | 2.339 | 0.473 | 0.822 | 0.441 |
| Medium | 74 | 28.6 | 2.318 | 0.494 | |||
| Large | 95 | 36.7 | 2.411 | 0.536 | |||
| Attendance in COVID‐19‐related trainings ‡ | Yes | 138 | 53.3 | 2.348 | 0.522 | −0.386 | 0.700 |
| No | 121 | 46.7 | 2.372 | 0.481 |
Pearson r correlation coefficient.
Independent t‐test.
ANOVA.
The CAD composite score was 2.359 of a possible score of 4. The composite scores representing mental health (1.012 of 5) and resilience (4.353 of 5) were above the midpoint, while the composite score of the professional‐turnover intention measure was below the midpoint (1.931 of 5). Fewer than 50% of the four CAD items received ‘yes’ responses. Among the four CAD items, 32.4% (n = 84) of frontline nurses reported that people around them felt afraid of them and thought that they had COVID‐19 infections, while 21.6% (n = 56) reported being treated with less respect and courtesy than others. Some frontline nurses reported receiving poor service at stores or restaurants (n = 26, 10%) and being threatened or harassed (n = 20, 32.4%) (Table 2).
Table 2.
Responses on the CAD scale
| CAD items | Yes response | % | No response | % |
|---|---|---|---|---|
| 1. Thinking that I may have a COVID‐19 infection, I was treated with less courtesy and respect than others | 56 | 21.6 | 203 | 78.4 |
| 2. Thinking that I may have a COVID‐19 infection, I often receive poorer service at restaurants or stores | 26 | 10.0 | 233 | 90.0 |
| 3. Thinking that I may have a COVID‐19 infection, people act as if they were afraid of me | 84 | 32.4 | 175 | 67.6 |
| 4. Thinking that I may have a COVID‐19 infection, I am often threatened or harassed | 20 | 7.7 | 239 | 92.3 |
The pearson correlation coefficients showed significant and positive correlation between COVID‐19‐associated discrimination and mental health (r = 0.236, P < 0.001), a negative correlation with psychological resilience (r = −0.140, P < 0.01), and a significant and positive correlation with professional‐turnover intention (r = 0.123, P < 0.01). Moreover, psychological resilience had a significant and negative correlations with mental health (r = −0.462, P < 0.001) and professional‐turnover intention (r = −0.178, P < 0.001) (Table 3).
Table 3.
Correlations between study variables
| Variables | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. COVID‐19‐associated discrimination | 2.359 | 0.502 | ||||
| 2. Mental health | 1.012 | 0.930 | 0.236** | |||
| 3. Professional turnover intention | 1.931 | 1.065 | 0.123* | 0.110 | ||
| 4. Resilience | 4.353 | 0.564 | −0.140* | −0.462** | −0.178** | 1 |
p < 0.01.
p < 0.001.
Table 4 shows the regression analyses to determine the mediating effects of resilience on the relationships between COVID‐19‐associated discrimination and frontline nurses’ mental health and professional‐turnover intention. Figure 1 shows the final models. First, regression analyses identified that higher CAD scores were associated with higher scores on the mental health measure (β = 0.236, P < 0.001) and higher scores on the professional‐turnover intention measure (β = 0.123, P = 0.048). Second, increased scores on the psychological resilience measure were associated with decreased scores on the mental health measure (β = −0.462, P < 0.001) and a lower score on the professional‐turnover intention measure (β = −0.182, P = 0.004). Finally, psychological resilience partially mediated the relationship between COVID‐19‐related discrimination and mental health (β = 0.175, P = 0.002) and fully mediated the relationship between COVID‐19‐related discrimination and professional‐turnover intention (β = 0.100, P = 0.107). In other words, resilience reduced the negative effects of COVID‐19‐related discrimination and resulted in improved mental health and reduced professional‐turnover intention. The Sobel test results on the mediating effects of resilience on the relationship between (a) COVID‐19‐related discrimination and mental health (z = 2.179, P = 0.02) and (b) COVID‐19‐related discrimination and professional‐turnover intention (z = 1.780, P = 0.07) were significant.
Table 4.
Mediating effects of resilience on the relationship between COVID‐19‐associated discrimination and nurse outcomes
| Model | B | SE | β | t | p | 95.0% CI | |
|---|---|---|---|---|---|---|---|
| LB | UB | ||||||
| Direct effects | |||||||
| COVID‐19‐associated discrimination → mental health | 0.218 | 0.056 | 0.236 | 3.892 | 0.001 | 0.108 | 0.329 |
| COVID‐19‐associated discrimination → professional turnover intention | 0.130 | 0.066 | 0.123 | 1.985 | 0.048 | 0.001 | 0.260 |
| COVID‐19‐associated discrimination → Resilience | −0.079 | 0.035 | −0.140 | −2.264 | 0.024 | −0.147 | −0.010 |
| Resilience → Mental Health | −0.761 | 0.091 | −0.462 | 8.355 | 0.001 | −0.941 | −0.582 |
| Resilience → professional turnover intention | −0.336 | 0.116 | −0.182 | −2.903 | 0.004 | −0.565 | −0.108 |
| Indirect effects | |||||||
| COVID‐19‐associated discrimination → resilience → Mental Health | 0.162 | 0.051 | 0.175 | 3.182 | 0.002 | 0.062 | 0.262 |
| COVID‐19‐associated discrimination → resilience → professional turnover intention | 0.106 | 0.066 | 0.100 | 1.617 | 0.107 | −0.023 | 0.235 |
Fig. 1.
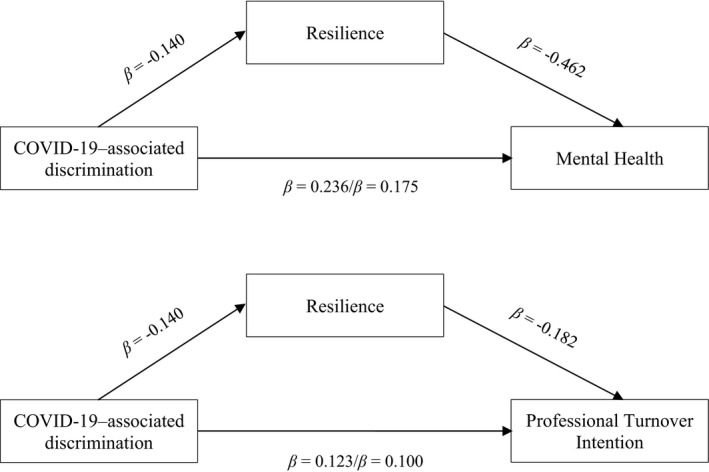
Final models
Discussion
As one of the first studies to determine the consequences of COVID‐19‐associated discrimination on frontline nurses, this research yielded valuable results that may guide nursing managers in formulating measures to reduce the occurrence of discrimination towards nurses and its accompanying consequences. Overall, the hypothesized models were supported by the study findings.
The mean CAD score suggests that frontline nurses perceived a moderate level of discrimination during the coronavirus pandemic. This result provided support to a handful of evidence describing the magnitude of stigma, discrimination and rejection experienced by nurses and other HCWs around the world during the coronavirus pandemic (Abuhammad et al. 2021; Sotgiu & Dobler 2020). For instance, in Jordan about 21% of HCWs reported a medium degree of social discrimination while 25% reported a higher level of social discrimination due to coronavirus (Dalky et al. 2020). Moreover, these study results are in accordance with anecdotal and media reports in which HCWs including nurses, as well as those infected with the virus, were stigmatized and socially discriminated against by the public (Islam et al. 2020; Ransing et al. 2020). A multi‐country study showed that individuals employed in hospitals had higher odds of being mistreated, harassed, and bullied during the pandemic relative to other groups of individuals in a community (Dye et al. 2020). This result is congruent with evidence from previous pandemics, including the EBOLA, H1N1, SARS, and MERS outbreaks, which also identified considerable levels of stigma and discrimination towards infected and recovered patients as well as nurses caring for these patients (Almutairi et al. 2018; Wester & Giesecke 2019).
In the present study, a significant percentage of frontline nurses (32.4%) reported that people around them were afraid of them and thought they were infected with COVID‐19, while 21.6% reported being mistreated and disrespected. This result is in accordance with earlier research in which HCWs in COVID‐19 designated hospital facilities perceived higher levels of discriminatory behaviours from the public and the community (Duy et al. 2020; Mostafa et al. 2020). Due to fear of being infected, 47% of the respondents in Taylor’s (2020) study expressed not wanting to be around HCWs treating COVID‐19 patients, while 34% reported they would refrain from visiting HCWs for medical reasons for fear of contracting the virus. In one study, 69.5% of HCWs reported rude and threatening behaviours against them by the public, while 30% reported receiving derogatory remarks (Yadav et al. 2020). Such displays of discriminatory behaviour from the public against nurses may be due to nurses’ high level of involvement in the management and care of suspected and/or infected patients, which puts them at higher risk of contracting the virus compared to other community members (Dye et al. 2020). Further, negative behaviours from the public towards frontline nurses and other health personnel could be a result of their fear of the virus since it is relatively new, potentially more transmissible compared to previous diseases, and little is known regarding its treatment. As noted in previous pandemics, when there is a potentially deadly disease and illness without a known treatment or cure, the risk for stigmatization and discriminatory behaviours towards the affected individual as well as those caring for the patient is relatively high (Almutairi et al. 2018; Wong & Sam 2011).
Regression analyses identified a direct influence of COVID‐19‐associated discrimination on frontline nurses’ mental health. In other words, a higher perception of discrimination by nurses’ was associated with poorer mental health. This study finding is consistent with earlier reports linking a higher perception of stigma and discrimination by frontline healthcare personnel to increased emotional exhaustion, fatigue (Ramaci et al. 2020), and psychological trauma (Zandifar et al. 2020). In Vietnam, a higher level of perceived discrimination was strongly tied to greater mental health issues including psychological distress, anxiety, and extreme sadness (Duy et al. 2020), while in India, a significant increase in stress levels were noted among allied health staff who perceived a higher level of COVID‐19‐associated discrimination (Uvais et al. 2020).
The direct influence of COVID‐19‐associated discrimination on frontline nurses’ professional‐turnover intention is a novel and important finding of this study. This result suggests that a higher perception of discrimination by frontline nurses may potentially drive them away from the nursing profession. This study is the first to confirm such a relationship, although a few studies during the pandemic have shown the negative effects of COVID‐19‐associated discrimination and stigma on nurses’ job satisfaction and work impairment (Ramaci et al. 2020). This result is alarming considering the increasing shortage of qualified nurses in the country, as well as the increasing number of nurses being infected or placed under quarantine (Department of Health 2020). Ignoring this situation may result in nurse turnover, potentially affecting overall healthcare service delivery. As such, tangible strategies to reduce the impact of stigmatization and discrimination among frontline nurses should be formulated to better support their mental health and increase their retention.
A key finding of this study was the mediating effect of psychological resilience on the relationships between COVID‐19‐associated discrimination and professional‐turnover intention and mental health. In other words, psychological resilience reduced the negative effects of COVID‐19‐associated discrimination and resulted in improved mental health and reduced professional‐turnover intention. While resilience has been previously reported as having mediating effects between pandemic‐related stressors and emotional distress (Lorente et al. 2021), depression and burnout (Serrão et al. 2021) and social support and mental health (Hou et al. 2021) during the COVID‐19 outbreak among healthcare workers, this is the first study to report such mediating effects and, thus to contribute additional knowledge regarding the importance of harnessing resilience in nursing staff during the pandemic. Resilience, or an individual’s capabilities to rebound from traumatic events, has long been recognized as a major protective factor that safeguards nurses’ mental and psychological health (Cooper et al. 2021). Evidence also suggested that when nurses were equipped with adequate levels of psychological resilience, they were more likely to sustain their clinical performance, remain satisfied and engaged in their jobs, and remain committed to their organization (Yu et al. 2019). Reports during the initial wave of the pandemic showed a similar pattern, namely that resilient nurses exhibited more sustained psychological, emotional, mental, and physiological well‐being despite the threats and the burden of the pandemic (Labrague 2021; Labrague and De los Santos, 2020, 2021; Zhang et al. 2021). This result is valuable in light of the numerous reports of frontline nurses being discriminated against, bullied, threatened, and socially excluded (Bagcchi 2020; Sotgiu & Dobler 2020), along with the increasing number of frontline nurses suffering from mental health issues (Kwaghe et al. 2020), and the growing number of nursing staff who have left their jobs and/or intending to leave their jobs and profession during the pandemic (Labrague and De los Santos, 2020, 2021). This result, therefore, underscores the need to proactively provide resilience‐enhancing measures, particularly for those nurses and other HCWs who are in the frontline battle against the highly transmissible virus, to better support their mental health and enhance their retention in the organization.
Limitations of the Study
This study has some shortcomings. First, given the nature of the research design employed, establishing causality between study variables may not be possible. Second, our participants were located in only one region of the country; hence, the generalizability of the findings may be limited. As such, future studies should consider other nurses located in other parts of the country. The partial mediating effect of resilience suggests that other potential factors (e.g. self‐efficacy, coping abilities, sense of coherence) might not have been accounted for in this study. Further, we recommend that future studies utilizing qualitative methods be conducted to explore the experiences of discrimination among frontline nurses during the pandemic.
Conclusions
In accordance with media reports and empirical evidence, nurses who are in the forefront of the battle against the coronavirus infection experience a significant level of social discrimination. An increased perception of COVID‐19‐associated discrimination was associated with poorer mental health and increased professional‐turnover intention. Further, this study identified resilience as a protective factor against the negative consequences of the public’s discriminatory behaviours against frontline nurses, resulting in improved mental health and reduced professional‐turnover intention. Organizational strategies to reduce the impact of discrimination during the pandemic against frontline nurses should be prioritized and should harness nurses’ resilience through theory‐driven strategies, adequate organizational support, and supportive leadership.
Relevance for Clinical Practice
Discrimination related to COVID‐19 is an issue that requires involvement from the different sectors of the government. Since discrimination against frontline nurses during any disease outbreak is driven by fear and misinformation about the disease (Schoch‐Spana et al. 2010) among the general public, health officials and local government officers should implement campaigns to raise the public’s awareness and correct misinformation regarding the disease, provide education about protective measures, and convey the importance of frontline nurses in the battle against the virus. At the hospital level, a wide‐range of measures can be implemented by the institution and by nursing administrators to reduce the effects of the public’s discriminatory behaviours against frontline nurses. Adequate organizational and social support must be provided, as well as a non‐discriminating and supportive work environment.
Mental health professionals, including mental health nurses play an important role to address COVID‐19‐associated discrimination and its accompanying mental health consequences. By recommending trustworthy sources of information related to COVID‐19 to the public, conducting research to determine public perceptions of the pandemic, implementing stigma/discrimination reduction strategies, and offering mental health support to other healthcare workers on the frontline, mental health nurses can help curtail the negative effects of stigma and discrimination during the pandemic (Prasad et al. 2020; Usher et al. 2020). By ensuring access to mental health professionals (e.g. mental health nurses) and/or mental health services to address the mental health issues of frontline nurses, the untoward effects of COVID‐19‐associated discrimination can be greatly reduced (Chen et al. 2021; Viswanathan et al. 2020). Further, nurse staffing levels should be increased to accommodate growing patient admissions and a more flexible schedule and adequate rest periods should be provided to further support the mental health of frontline nurses (Kang et al. 2020; Digby et al. 2021).
Hospitals should consider implementing proactive strategies to enhance resilience in frontline nurses through relevant training and education, theory‐driven resilience‐enhancing interventions (e.g. resiliency programme, mindfulness, self‐care resilience programme, and hardiness training), hospital policies supporting nurses’ work‐life balance and well‐being, and supportive leadership (Cooper et al. 2021; Goh et al. 2021). Collectively undertaking these measures could ultimately reduce the negative effects of the public’s discriminatory behaviours on nurses’ overall mental health and well‐being, resulting in increased professional and organizational retention.
Research Fund
This study is non‐funded.
Ethical Approval
Samar State University Institutional Research Ethics Review Committee (IRERC) (IRERC EA‐0012‐I).
Acknowledgement
The authors would like to acknowledge and thanks all nurses who participated in the study.
Declaration of conflict of interest: All authors declare that there is no conflict of interest.
References
- Abuhammad, S. , Alzoubi, K.H. & Khabour, O. (2021). Fear of COVID‐19 and stigmatization towards infected people among Jordanian people. International Journal of Clinical Practice, 75 (4), e13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almutairi, A.F. , Adlan, A.A. , Balkhy, H.H. , Abbas, O.A. & Clark, A.M. (2018). “It feels like I’m the dirtiest person in the world”.: Exploring the experiences of healthcare providers who survived MERS‐CoV in Saudi Arabia. Journal of Infection and Public Health, 11 (2), 187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagcchi, S. (2020). Stigma during the COVID‐19 pandemic. The Lancet. Infectious Diseases, 20 (7), 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick, D.M. , Murphy, J.M. , Goldman, P.A. , Ware, J.E. Jr , Barsky, A.J. & Weinstein, M.C. (1991). Performance of a five‐item mental health screening test. Medical Care, 29, 169–176. [DOI] [PubMed] [Google Scholar]
- Budhwani, H. & Sun, R. (2020). Creating COVID‐19 stigma by referencing the novel coronavirus as the “Chinese virus” on Twitter: Quantitative analysis of social media data. Journal of Medical Internet Research, 22 (5), e19301. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassiani‐Miranda, C.A. , Álvarez‐Solorza, I. , Campo‐Arias, A. , Arismendy‐López, Y.A. , Tirado‐Otálvaro, A.F. , Bustamante‐Montes, L.P. & Toxqui‐Tlachino, M.J.G. (2021). Factors associated with the stigma‐discrimination complex towards healthcare workers among university students during the coronavirus pandemic in Mexico. medRxiv.
- Chen, R. , Sun, C. , Chen, J.J. et al. (2021). A large‐scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID‐19 pandemic. International Journal of Mental Health Nursing, 30 (1), 102–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, A.L. , Brown, J.A. & Leslie, G.D. (2021). Nurse resilience for clinical practice: An integrative review. Journal of Advanced Nursing, 77 (6), 2623–2640. Ahead of Print [DOI] [PubMed] [Google Scholar]
- Dalky, H.F. , Abu‐Hassan, H.H. , Dalky, A.F. & Al‐Delaimy, W. (2020). Assessment of mental health stigma components of mental health knowledge, attitudes and behaviors among jordanian healthcare providers. Community Mental Health Journal, 56 (3), 524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health (2020). Updates on novel coronavirus disease (COVID‐19). Department of Health. [Cited February 23, 2021]. Available from: URL: https://www.doh.gov.ph/2019‐nCoV
- De Brier, N. , Stroobants, S. , Vandekerckhove, P. & De Buck, E. (2020). Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID‐19): A rapid systematic review. PLoS One, 15 (12), e0244052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digby, R. , Winton‐Brown, T. , Finlayson, F. , Dobson, H. & Bucknall, T. (2021). Hospital staff well‐being during the first wave of COVID‐19: Staff perspectives. International Journal of Mental Health Nursing, 30 (2), 440–450. [DOI] [PubMed] [Google Scholar]
- Do Duy, C. , Nong, V.M. , Van, A.N. , Thu, T.D. , Do Thu, N. & Quang, T.N. (2020). COVID‐19 related stigma and its association with mental health of health‐care workers after quarantined in Vietnam. Psychiatry and Clinical Neurosciences. 74 (10), 566–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye, T.D. , Alcantara, L. , Siddiqi, S. et al. (2020). Risk of COVID‐19‐related bullying, harassment and stigma among healthcare workers: An analytical cross‐sectional global study. British Medical Journal Open, 10 (12), e046620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh, Y.S. , Ow Yong, Q.Y.J. , Chen, T.H.M. , Ho, S.H.C. , Chee, Y.I.C. & Chee, T.T. (2021). The impact of COVID‐19 on nurses working in a University Health System in Singapore: A qualitative descriptive study. International Journal of Mental Health Nursing, 30 (3), 643–652. [DOI] [PubMed] [Google Scholar]
- Hou, W.K. , Tong, H. , Liang, L.i. et al. (2021). Probable anxiety and components of psychological resilience amid COVID‐19: A population‐based study. Journal of Affective Disorders, 282, 594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam, M.S. , Sarkar, T. , Khan, S.H. et al. (2020). COVID‐19–related infodemic and its impact on public health: A global social media analysis. The American Journal of Tropical Medicine and Hygiene, 103 (4), 1621–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, L. , Ma, S. , Chen, M. et al. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross‐sectional study. Brain, Behavior, and Immunity, 87, 11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwaghe, A.V. , Ilesanmi, O.S. , Amede, P.O. , Okediran, J.O. , Utulu, R. & Balogun, M.S. (2020). Stigmatization, psychological and emotional trauma among frontline health care workers treated for COVID‐19 in Lagos State, Nigeria: A qualitative study. Researchsquare. 10.21203/rs.3.rs-53453/v1 [DOI] [PMC free article] [PubMed]
- Labrague, L. (2021). Psychological resilience, coping behaviors, and social support among healthcare workers during the COVID‐19 pandemic: A systematic review of quantitative studies. Journal of Nursing Management. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L.J. & De los Santos, J.A.A. (2020). COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management, 28 (7), 1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L.J. & De los Santos, J.A.A. (2021). Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nursing, 38 (3), 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y. , Finch, B.K. , Brenneke, S.G. , Thomas, K. & Le, P.D. (2020). Perceived discrimination and mental distress amid the COVID‐19 pandemic: Evidence from the understanding America study. American Journal of Preventive Medicine, 59 (4), 481–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorente, L. , Vera, M. & Peiró, T. (2021). Nurses´ stressors and psychological distress during the COVID‐19 pandemic: The mediating role of coping and resilience. Journal of Advanced Nursing, 77 (3), 1335–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostafa, A. , Sabry, W. & Mostafa, N.S. (2020). COVID‐19‐related stigmatization among a sample of Egyptian healthcare workers. PLoS One, 15 (12), e0244172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad, S.K. , Karahda, A. , Singh, P. & Gupta, R. (2020). Role of mental health professionals in dealing with the stigma attached to COVID‐19. General Psychiatry, 33 (5), e100298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaci, T. , Barattucci, M. , Ledda, C. & Rapisarda, V. (2020). Social stigma during COVID‐19 and its impact on HCWs outcomes. Sustainability, 12 (9), 3834. [Google Scholar]
- Ransing, R. , Ramalho, R. , de Filippis, R. et al. (2020). Infectious disease outbreak related stigma and discrimination during the COVID‐19 pandemic: Drivers, facilitators, manifestations, and outcomes across the world. Brain, Behavior, and Immunity, 89, 555–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoch‐Spana, M. , Bouri, N. , Rambhia, K.J. & Norwood, A. (2010). Stigma, health disparities, and the 2009 H1N1 influenza pandemic: How to protect Latino farmworkers in future health emergencies. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 8 (3), 243–254. [DOI] [PubMed] [Google Scholar]
- Schreiber, M. , Cates, D.S. , Formanski, S. & King, M. (2019). Maximizing the resilience of healthcare workers in multi‐hazard events: Lessons from the 2014–2015 Ebola response in Africa. Military Medicine, 184 (Supplement_1), 114–120. [DOI] [PubMed] [Google Scholar]
- Serrão, C. , Duarte, I. , Castro, L. & Teixeira, A. (2021). Burnout and depression in Portuguese healthcare workers during the COVID‐19 pandemic—The mediating role of psychological resilience. International Journal of Environmental Research and Public Health, 18 (2), 636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, B.W. , Dalen, J. , Wiggins, K. , Tooley, E. , Christopher, P. & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15 (3), 194–200. [DOI] [PubMed] [Google Scholar]
- Sotgiu, G. & Dobler, C.C. (2020). Social stigma in the time of coronavirus disease 2019. European Respiratory Journal, 56, 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner, R.C. & Kinsella, E.L. (2021). Grace under pressure: Resilience, burnout, and wellbeing in frontline workers in the United Kingdom and Republic of Ireland during the SARS‐CoV‐2 pandemic. Frontiers in Psychology, 11, 3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. , Landry, C.A. , Rachor, G.S. , Paluszek, M.M. & Asmundson, G.J. (2020). Fear and avoidance of healthcare workers: An important, under‐recognized form of stigmatization during the COVID‐19 pandemic. Journal of Anxiety Disorders, 75, 102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teksin, G. , Uluyol, O.B. , Onur, O.S. , Teksin, M.G. & Ozdemir, H.M. (2020). Stigma‐related factors and their effects on health‐care workers during COVID‐19 pandemics in Turkey: A multicenter study. The Medical Bulletin of Sisli Etfal Hospital, 54 (3), 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K. , Durkin, J. & Bhullar, N. (2020). The COVID‐19 pandemic and mental health impacts. International Journal of Mental Health Nursing, 29 (3), 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uvais, N.A. , Aziz, F. & Hafeeq, B. (2020). COVID‐19‐related stigma and perceived stress among dialysis staff. Journal of Nephrology, 33, 1121–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veit, C.T. & Ware, J.E. (1983). The structure of psychological distress and well‐being in general populations. Journal of Consulting and Clinical Psychology, 51 (5), 730–742. [DOI] [PubMed] [Google Scholar]
- Viswanathan, R. , Myers, M.F. & Fanous, A.H. (2020). Support groups and individual mental health care via video conferencing for frontline clinicians during the COVID‐19 pandemic. Psychosomatics, 61 (5), 538–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, L.P. & Sam, I.C. (2011). Knowledge and attitudes in regard to pandemic influenza A (H1N1) in a multiethnic community of Malaysia. International Journal of Behavioral Medicine, 18 (2), 112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wester, M. & Giesecke, J. (2019). Ebola and healthcare worker stigma. Scandinavian Journal of Public Health, 47 (2), 99–104. [DOI] [PubMed] [Google Scholar]
- Yadav, K. , Laskar, A.R. & Rasania, S.K. (2020). A study on stigma and apprehensions related to COVID‐19 among healthcare professionals in Delhi. International Journal of Community Medicine and Public Health, 7 (11), 4547–4553. [Google Scholar]
- Yu, F. , Raphael, D. , Mackay, L. , Smith, M. & King, A. (2019). Personal and work‐related factors associated with nurse resilience: A systematic review. International Journal of Nursing Studies, 93, 129–140. [DOI] [PubMed] [Google Scholar]
- Zandifar, A. , Badrfam, R. , Khonsari, N.M. , Mohammadi, M.R. , Asayesh, H. & Qorbani, M. (2020). Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID‐19 patients. Iranian Journal of Psychiatry, 15 (4), 340–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X. , Jiang, X. , Ni, P. et al. (2021). Association between resilience and burnout of front‐line nurses at the peak of the COVID‐19 pandemic: Positive and negative affect as mediators in Wuhan. International Journal of Mental Health Nursing, 30 (4), 939–954. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]


