Abstract
Inhaled corticosteroid is not associated with a poor prognosis in COVID‐19
Keywords: coronavirus disease, COVID‐19, inhaled corticosteroid, prognosis, SARS‐CoV‐2
To the Editors:
The coronavirus disease 2019 (COVID‐19) pandemic is a worldwide tragedy. Inhaled corticosteroids (ICS) are often used to manage asthma or chronic obstructive pulmonary disease (COPD).1 However, the impact of prior ICS use in newly diagnosed COVID‐19 patients remains controversial.2
South Korea has a well‐established medical claims database with a single mandatory government health insurance system.3 We retrospectively analysed the association of ICS use with COVID‐19 prognosis using this database.
COVID‐19‐positive cases were diagnosed by reverse transcription‐PCR (RT‐PCR) from nasopharyngeal/oropharyngeal swab or sputum, and confirmed cases were isolated or admitted to hospital by the Korean government. We examined the complete South Korea data set on the use of ICS by COVID‐19 patient before and after diagnosis from 20 January 2019 to 15 May 2020.
The use of ICS is only approved for asthma and COPD treatment and comprehensively documented in the Korean medical claims database.1, 3, 4, 5, 6, 7 For this study, ICS use was defined as its use either alone or with a long‐acting β2‐agonist (LABA) during the year prior to the COVID‐19‐positive diagnosis. We evaluated comorbidities with the modified Charlson Comorbidity Index (mCCI), which did not include the pulmonary diseases to reflect the sole effect of ICS.8 Management of COVID‐19 was symptomatic treatment.
We used the Student's t‐test and chi‐square test for comparing continuous and categorical variables between groups, simple and multiple linear regression analyses for evaluating the influence of prior ICS use on hospital length of stay (LOS) of COVID‐19‐positive patients and similarly used univariable and multivariable logistic regression analyses for evaluating intensive care unit (ICU) admission and all‐cause mortality. A p‐value of <0.05 was considered statistically significant. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for statistical analysis.
A total of 6520 positive COVID‐19 patients were included in this study with a mean age of 47.9 years, of which 39.7% were male. The mean mCCI score was 0.9 points. The proportion of any prescription of ICS (±LABA) was 185/6520 (2.8%). The mean hospital LOS was 23 days, the ICU admission rate was 3.2% and overall mortality was 3.3%. The group of positive COVID‐19 patients who used ICS before diagnosis was on average older (53.7 ± 21.0 vs. 47.7 ± 19.1, p < 0.01) and their mCCI score was higher (2.1 vs. 0.9, p < 0.01) compared to the group of patients who had not used ICS in the year prior to diagnosis. There were no significant differences in sex and medical aid insurance (insurance for low socioeconomic status) between the two groups. Univariable analysis showed that the overall mortality was higher in the ICS group (9.7% vs. 3.1%, p < 0.01), while hospital LOS and ICU admission rates were not significantly different.
Multiple linear regression analysis was conducted to evaluate the contributing factors to hospital LOS. Age, sex, mCCI score, insurance type and the prior use of ICS were selected as predicting variables. No multi‐collinearity between variables was observed in the analysis. Older age (exponentiation of the β coefficient [exp(β)] = 1.14) and higher mCCI scores (exp(β) = 2.33) were significantly associated with a longer hospital LOS. Patients with medical aid insurance had a shorter hospital LOS than the National Health Insurance Group (exp(β) = 0.09). However, use of ICS before diagnosis was not associated with a longer hospital LOS (Table 1).
TABLE 1.
Clinical outcomes of COVID‐19 according to the use of ICS
| Variables | Hospital length of stay | ICU admission rate | Mortality | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Multiple linear | Multiple binary logistic | Multiple binary logistic | ||||||||||||||||
| Overall | Asthma | COPD | Overall | Asthma | COPD | Overall | Asthma | COPD | ||||||||||
| β | p‐Value | β | p‐Value | β | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | |
| Age | 0.18 | <0.01 | 0.11 | 0.16 | 0.06 | 0.76 | 1.05 (1.04–1.06) | <0.01 | 1.06 (1.01–1.11) | 0.02 | 0.94 (0.75–1.16) | 0.56 | 1.12 (1.11–1.14) | <0.01 | 1.17 (1.09–1.26) | <0.01 | 1.25 (1.01–1.55) | 0.04 |
| Male sex | −0.01 | 0.36 | 0.03 | 0.71 | −0.19 | 0.30 | 1.95 (1.47–2.60) | <0.01 | 1.38 (0.43–4.45) | 0.59 | — | — | 2.31 (1.69–3.16) | <0.01 | 2.56 (0.76–8.62) | 0.13 | 1.46 (0.13–16.3) | 0.76 |
| mCCI score | 0.08 | <0.01 | 0.02 | 0.77 | −0.07 | 0.89 | 1.20 (1.11–1.30) | <0.01 | 1.21 (0.79–1.86) | 0.39 | 1.50 (0.52–4.27) | 0.45 | 1.30 (1.20–1.41) | <0.01 | 1.02 (0.66–1.57) | 0.93 | 1.65 (0.91–2.97) | 0.10 |
| Medical aid | −0.05 | <0.01 | 0.09 | 0.19 | −0.23 | 0.27 | 0.61 (0.37–1.01) | 0.05 | 0.34 (0.04–3.00) | 0.33 | — | — | 1.54 (1.03–2.31) | 0.04 | 0.15 (0.02–1.53) | 0.11 | — | — |
| ICS (±LABA) | 0.00 | 0.77 | 0.09 | 0.17 | 0.30 | 0.11 | 0.66 (0.29–1.47) | 0.31 | 0.49 (0.14–1.70) | 0.26 | — | — | 1.40 (0.76–2.60) | 0.28 | 1.48 (0.45–4.85) | 0.52 | 4.93 (0.31–79.3) | 0.26 |
Abbreviations: COPD, chronic obstructive pulmonary disease; COVID‐19, coronavirus disease 2019; exp(β), exponentiation of the β coefficient; ICS, inhaled corticosteroid; ICU, intensive care unit; LABA, long‐acting β2‐agonist; mCCI, modified Charlson Comorbidity Index (scores excluding asthma or COPD).
Multivariable logistic regression analysis was used to examine the effects of age, sex, mCCI score, insurance type and use of ICS on ICU admission and all‐cause mortality. Older age (OR 1.05; 95% CI 1.04–1.06), male sex (OR 1.95; 95% CI 1.47–2.60) and higher mCCI scores (OR 1.20; 95% CI 1.11–1.30) were significantly associated with ICU admission rate, whereas the use of ICS (OR 0.66; 95% CI 0.29–1.47; p = 0.31) was not associated. While univariable analysis showed that all five factors were associated with mortality, adjusted multivariable analyses revealed that older age (OR 1.12; 95% CI 1.11–1.14), male sex (OR 2.31; 95% CI 1.69–3.16), higher mCCI scores (OR 1.30; 95% CI 1.20–1.41) and poor socioeconomic status (OR 1.54; 95% CI 1.03–2.31; p = 0.04) remained associated with all‐cause mortality. Unlike the other variables, the use of ICS was not associated with mortality (Table 1). The results were similar in the subgroup analysis of patients with the use of high‐dose ICS prior to COVID‐19 diagnosis.
The clinical role of ICS in COVID‐19 remains poorly understood. This nationwide retrospective population study examined the association between prior use of ICS and the prognosis of COVID‐19 patients. This study reports valuable findings regarding the use of ICS. Multivariable analysis revealed that hospital LOS, ICU admission and all‐cause mortality were not associated with the use of ICS and premorbid use of ICS does not seem to have a harmful effect in COVID‐19 patients.
Schultze et al.9 reported poor outcomes associated with ICS. However, the authors suggested that increased mortality observed in patients with high‐dose ICS use was possibly a result of unmeasured confounding due to disease severity. Wark et al. showed the reduced expression of angiotensin‐converting enzyme 2 (ACE2) receptor expression in asthma patients, which is a target of the COVID‐19 virus.10 Peters et al. showed supportive data of lower ACE2 receptor expression in patients with ICS use.11
This study was a nationwide population study that included detailed comorbidity and medication information, with no subjectively collected measures or missing data. Therefore, we were able to precisely determine the prevalence of ICS use prior to diagnosis, and evaluate the underlying respiratory diseases such as asthma or COPD, and other confounding demographic factors of confirmed COVID‐19‐positive cases.
There were several limitations to this study. First, data analysis in this study did not include lung function data, smoking status, BMI and symptomatic scores of COPD or asthma because of the nature of the medical claims data. This information is important when assessing the severity of asthma or COPD. Second, it did not include information of COVID‐19 patients who were still under treatment on 15 May 2020. A survival analysis was not performed in this study due to lack of the information about the timing of death. Although mortality data were available, the day of death was not included in the database. Third, this was a retrospective study to evaluate the effects of prior use of ICS itself on COVID‐19. However, using medical claims data was appropriate because of the comprehensive availability of information on medical utilization before the diagnosis of COVID‐19. Fourth, the use of ICS was defined as any ICS prescription within 1 year, including patients who were prescribed only one canister of ICS. However, we added a subgroup analysis of those patients with any ICS use within 3 months of COVID‐19 diagnosis and the results were similar. Fifth, we were unable to address the confounding influence of underlying asthma or COPD in the COVID‐19‐positive patients using ICS prior to diagnosis.
In conclusion, we should be careful with the withdrawal of ICS in COVID‐19‐positive patients, as this may lead to deterioration of underlying chronic lung disease. This study provides valuable evidence regarding the controversial issue of ICS during the COVID‐19 pandemic. In the adjusted analyses, we clarified that the prior use of ICS was not harmful in COVID‐19 patients. Older age, male sex, more comorbidities and poor socioeconomic status were significantly associated with all‐cause mortality. Based on our results, we suggest not withdrawing ICS medication in patients with asthma/COPD during the COVID‐19 pandemic.
AUTHOR CONTRIBUTIONS
Tai Joon An: Conceptualization; investigation; methodology; writing‐original draft; writing‐review & editing. Youlim Kim: Conceptualization; investigation; methodology; visualization; writing‐original draft; writing‐review & editing. Yong‐Bum Park: Conceptualization; investigation; methodology; supervision; validation; writing‐review & editing. Kyungjoo Kim: Data curation; formal analysis; investigation; methodology; resources; software; visualization. Do Yeon Cho: Data curation; formal analysis; resources; visualization. Kwang‐Ha Yoo: Conceptualization; investigation; methodology; project administration; supervision; validation. Chin Kook Rhee: Conceptualization; funding acquisition; investigation; methodology; project administration; supervision; validation; writing‐review & editing.
CONFLICT OF INTEREST
Chin Kook Rhee has received consulting/lecture fees from MSD, AstraZeneca, GSK, Novartis, Takeda, Mundipharma, Boehringer‐Ingelheim, Teva, Sanofi and Bayer. Other authors have no conflict of interest.
HUMAN ETHICS APPROVAL DECLARATION
This study was approved by the Institutional Review Board of the Catholic University of Korea Yeouido St. Mary's Hospital (approval no. SC20ZISE0067) and informed consent was waived due to the nature of the study.
Supporting information
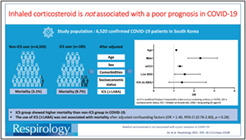
Visual abstract: Inhaled corticosteroid is not associated with a poor prognosis in COVID‐19
ACKNOWLEDGEMENTS
Research funding: This research was supported by a grant from the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HI18C0522).
An TJ, Kim Y, Park YB, et al. Inhaled corticosteroid is not associated with a poor prognosis in COVID‐19. Respirology. 2021;26:812–815. 10.1111/resp.14108
Associate Editor: Paul Thomas; Senior Editor: Paul King
Funding information Korea Health Industry Development Institute, Grant/Award Number: Korea Health Technology R&D Project; Ministry of Health & Welfare, Republic of Korea, Grant/Award Number: HI18C0522
REFERENCES
- 1.Lee J, Lee JH, Kim JA, Rhee CK. Trend of cost and utilization of COPD medication in Korea. Int J Chron Obstruct Pulmon Dis. 2017;12:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpin DMG, Singh D, Hadfield RM. Inhaled corticosteroids and COVID‐19: a systematic review and clinical perspective. Eur Respir J. 2020;55(5):2001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014;36:e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JY, Yoon HK, Lee JH, Yoo KH, Kim BY, Bae HW, et al. Nationwide use of inhaled corticosteroids by South Korean asthma patients: an examination of the Health Insurance Review and Service database. J Thorac Dis. 2018;10:5405–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim JA, Lim MK, Kim K, Park J, Rhee CK. Adherence to inhaled medications and its effect on healthcare utilization and costs among high‐grade chronic obstructive pulmonary disease patients. Clin Drug Investig. 2018;38:333–40. [DOI] [PubMed] [Google Scholar]
- 6.Choi JY, Yoon HK, Lee JH, Yoo KH, Kim BY, Bae HW, et al. Current status of asthma care in South Korea: nationwide the Health Insurance Review and Assessment Service database. J Thorac Dis. 2017;9:3208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhee CK, van Boven JFM, Yau Ming SW, Park HY, Kim DK, Park HS, et al. Does changing inhaler device impact real‐life asthma outcomes? Clinical and economic evaluation. J Allergy Clin Immunol Pract. 2019;7:934–42. [DOI] [PubMed] [Google Scholar]
- 8.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD‐10 version of the Charlson comorbidity index predicted in‐hospital mortality. J Clin Epidemiol. 2004;57:1288–94. [DOI] [PubMed] [Google Scholar]
- 9.Schultze A, Walker AJ, MacKenna B, Morton CE, Bhaskaran K, Brown JP, et al. Risk of COVID‐19‐related death among patients with chronic obstructive pulmonary disease or asthma prescribed inhaled corticosteroids: an observational cohort study using the OpenSAFELY platform. Lancet Respir Med. 2020;8:1106–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wark PAB, Pathinayake PS, Kaiko G, Nichol K, Ali A, Chen L, et al. ACE2 expression is elevated in airway epithelial cells from older and male healthy individuals but reduced in asthma. Respirology. 2021;26:442–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peters MC, Sajuthi S, Deford P, Christenson S, Rios CL, Montgomery MT, et al. COVID‐19‐related genes in sputum cells in asthma. Relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Visual abstract: Inhaled corticosteroid is not associated with a poor prognosis in COVID‐19


