Abstract
Aim
To investigate the association between menstrual cycle regularity in healthcare providers and COVID‐19 pandemic‐related anxiety, depression, stress.
Methods
A cross‐sectional study was conducted by administrating online questionnaires to female healthcare workers in Turkey. Women aged 18–40 years with regular menstrual cycles for more than 1 year before the beginning of the pandemic were included in the study and they were divided into two groups according to menstrual cycle regularity during the pandemic. The questionnaires included sociodemographic characteristics, medical and reproductive history, lifestyle information of participants, COVID‐19 Stress Scales (CSS), and a short version of the Depression Anxiety Stress Scale (DASS‐21).
Results
A total of 952 women were included in the study, 679 had regular menstrual cycles, and 273 had irregular menstrual cycles. The prevalence of irregular menses among Turkish women healthcare workers aged 18–40 years was 28.7%. The CSS subdimensions and total scores were significantly higher in the irregular menstruation group than in women with regular menstruation (p < 0.001). The DASS‐21 depression, anxiety, and stress subdimensions were likewise significantly higher in women with irregular menstruation (p < 0.001). Besides, both the univariable and the multivariable logistic regression results showed the relationship between irregular menstruation and CSS total score.
Conclusion
The current study showed the association between the COVID‐19 pandemic‐induced anxiety, perceived stress, depressive symptoms, and increased prevalence of menstrual cycle irregularity among healthcare providers.
Keywords: anxiety, COVID‐19, depression, healthcare providers, menstrual cycle irregularity, stress
Introduction
Regular menstrual cycle is an indicator of the normally functioning hypothalamic–pituitary–gonadal (HPG) axis and a vital sign of women's health and well‐being.1 Menstrual cycle irregularities include the changes in a menstrual pattern in terms of frequency, regularity, duration, or intensity and also intermenstrual bleeding.2 Women with irregular menses tend to be at higher risk of developing cardiovascular disease, diabetes mellitus, chronic renal failure and also infertility, premature menopause, breast, and ovarian cancer later in life.3, 4, 5 The global prevalence of irregular menstruation varies between 5% and 34% during reproductive years and menstruation‐related problems constitute one of the most common reasons for admission to a gynecologist.6, 7 Menstrual patterns can be affected by a variety of factors, including structural entities, coagulopathy, ovulatory dysfunction, medication use, and modifiable factors (sudden weight loss, over‐exercising, obesity, smoking, psychological problems).8, 9 Menstrual cycle irregularities are not only related to future chronic health problems but also adversely affect the quality of life, work productivity and add a financial burden on health systems.10
In December 2019 severe acute respiratory tract infection, the coronavirus disease 19 (COVID‐19) originating at Wuhan city of China, has rapidly spread all over the world and led to a global risk to public health. World Health Organization declared the COVID‐19 outbreak as a pandemic on March 11, 2020.11 As of the time of writing, COVID‐19 had infected almost 100 million people and caused more than 2 million deaths worldwide. Turkey is one of the world's top 10 countries in the number of COVID‐19 cases with a confirmed 1.5 million infected cases as of January 2021.12 Widespread epidemics are not only associated with physical health concerns but also pose a significant threat to mental health.13 The reported prevalence of stress, anxiety, and depression in the general population during the COVID‐19 pandemic are 29.6%, 31.9%, and 33.7%, respectively.14
Healthcare providers are on the frontlines of this widespread outbreak and face an increased risk of becoming infected, experience a heavy workload, fatigue, stigma, and psychosocial stress. Previous studies have shown the harmful results of infectious disease outbreaks on healthcare workers' mental health.15, 16, 17 Also, some recent studies pointed out the COVID‐19 pandemic‐related mental health issues among health professionals. Demartini et al. reported higher levels of psychiatric symptoms in healthcare workers than in general public.18 A study from China by Song et al. detected depressive symptoms in 25% of participants among 14 825 enrolled doctors and nurses.19 Studies from Europe have also confirmed the impact of the pandemic on increased rates of depression, anxiety, and stress among healthcare providers.20, 21
The relation between psychological distress and menstrual cycle irregularities or the effect of the pandemic on mental health conditions of the general population and health workers has been previously discussed. However, there is no previous data of potential mental harmful effects of outbreak on menstrual cycle characteristics of healthcare professionals. The present study aimed to investigate the association between menstrual cycle regularity in healthcare providers and COVID‐19 pandemic‐related anxiety, depression, and stress.
Methods
Study design and participants
We conducted a cross‐sectional study by administrating online questionnaires to female healthcare workers in Turkey from November to December 2020. This survey was applied in primary, secondary, and tertiary care centers to healthcare workers including physicians, nurses, midwives, paramedical staff, support staff, and community workers. Surveys were administered through the online survey platform. Healthcare workers at various facilities in Istanbul were invited via the hospital communication platforms (i.e. occupational WhatsApp messaging groups) to participate in the survey. Participants completed the questionnaire which includes four sub‐instruments as follows: (1) sociodemographic characteristics, medical and reproductive history, and lifestyle information; (2) menstrual patterns of participants; (3) COVID‐19 Stress Scales (CSS); and (4) short version of the Depression Anxiety Stress Scale (DASS‐21). At the recruitment stage, 4000 potentially eligible individuals were invited to participate; 2794 of these individuals did not respond to the invitation while 1206 of them accepted to participate. Two hundred fifty‐six individuals were excluded, 226 did not meet the inclusion criteria, and 28 yielded a partial response. After removing ineligible participants, the final analysis was conducted with 952 participants (regular menstrual cycles n = 679, irregular menstrual cycles n = 273) (Figure 1).
Figure 1.
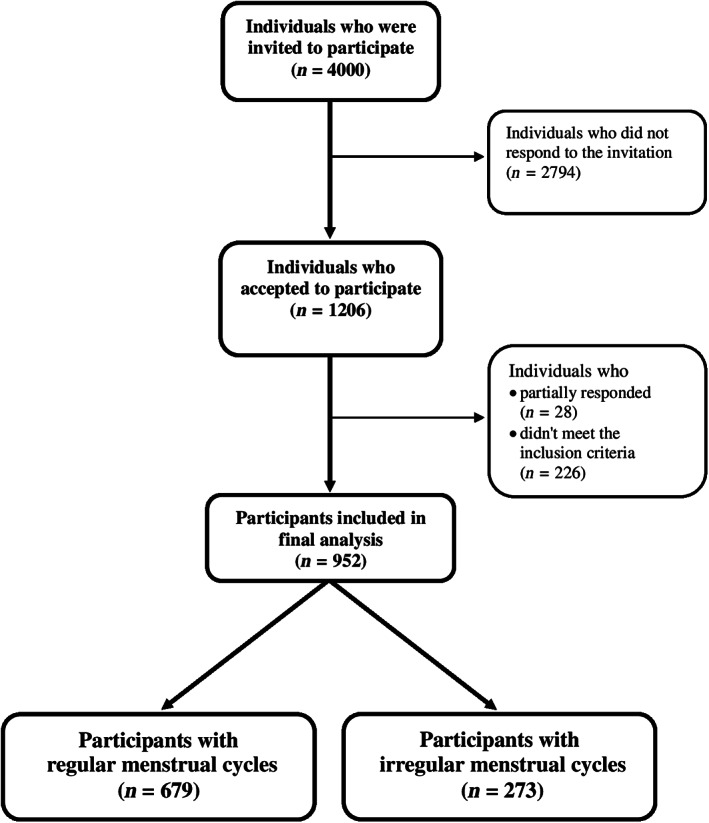
Flowchart of participants included in the study
The study was approved by the ethics committee of Bezmialem University Medical Faculty (BEAH 2020 21/401), and all participants provided informed consent online.
Women aged 18–40 years with regular menstrual cycles for more than 1 year before the beginning of the pandemic were included in the study. Women who were pregnant, postpartum or breastfeeding, taking hormone medication, or using any medication that could affect their menstrual patterns, had an intrauterine device, bleeding disorders, thyroid disease, hyperprolactinemia, chronic renal failure or cancer, undergone hysterectomy and/or oophorectomy, and diagnosed with major psychiatric disorder were not enrolled in the study.
Assessment of menstrual patterns
Women were asked about the characteristics of their last three menstrual cycles. The normal menstrual pattern was defined as a frequency of 24–38 days, 7–9 days variation between the shortest to longest cycles, duration of flow 8 days or less, and the blood loss 5–80 mL. Variations in any of these four parameters or intermenstrual bleeding were defined as irregular menstruation.22, 23
COVID‐19 Stress Scales
The scale was developed by Taylor et al.24 CSS aims to measure the stress and anxiety symptoms specific to the current outbreak. It consists of 36 items divided equally over six subscales (danger and contamination fears, socio‐economic consequences, fears of foreigners that they are spreading COVID‐19 [xenophobia], contamination, traumatic stress, compulsive checking). Each item scored on a scale ranging from 0 (never) to 4 (almost always). Higher scores indicate greater levels of pandemic‐related stress and anxiety.
Depression Anxiety and Stress Scale
The scale was developed by Lovibond et al. in 1995 as an instrument to measure depression, anxiety, and stress symptoms.25 The DASS‐21 has three subscales (depression, anxiety, and stress) each containing seven items. Items rated from 0 (did not apply to me at all) to 3 (applied to me most of the time). Higher scores indicate higher depression, anxiety, and stress levels. The validity and reliability of this scale for Turkish society had been established in a previous study.26
Statistical analysis
SPSS version 22 software for Windows was used for data analysis. Descriptive statistics were presented as frequencies (percentages) for categorical variables and mean ± SD for continuous variables. We used Pearson's chi‐square tests to compare categorical variables between groups. In the comparison of continuous variables, tests for sphericity and homogeneity of variance were performed on the data. Continuous variables that meet the assumptions of normality were analyzed with Student's t‐test. Variables found to be statistically significant by univariate analysis were also included in a multivariate logistic regression model to determine the predictors of “irregular menstrual cycles.” For all statistical tests, p < 0.05 was considered statistically significant.
Results
A total of 952 women were included in the study, 679 had regular menstrual cycles and 273 had irregular menstrual cycles. The prevalence of irregular menses among Turkish women healthcare workers aged 18–40 years was 28.7%.
Baseline sociodemographic and clinical characteristics of the groups are detailed in Table 1. There was no significant difference between groups regarding sociodemographic or clinical variables including age, body mass index, nulliparity, age at menarche, education status, professions, institution types, percentage of shift workers, income status, residency, smoking, alcohol use, caffeine intake, physical activity, and previous COVID‐19 positive diagnosis (p > 0.05).
Table 1.
Comparison of sociodemographic and clinical variables between groups
| Variable | Menstrual cycles | Statistic | df | p | |
|---|---|---|---|---|---|
| Regular (n = 679) | Irregular (n = 273) | ||||
| Age (years) | 29.48 ± 5.29 | 29.54 ± 5.94 | t = 0.158 | 950 | 0.875 |
| Body mass index (kg/m2) | 22.42 ± 3.85 | 22.82 ± 3.80 | t = −1.440 | 950 | 0.150 |
| Nulliparous | 150 (22.1%) | 26.4 (26.4%) | χ2 = 1.997 | 1 | 0.158 |
| Age at menarche (years) | 12.86 ± 1.25 | 12.99 ± 1.44 | t = −1.421 | 950 | 0.156 |
| Education | χ2 = 3.875 | 2 | 0.144 | ||
| High school | 75 (11.0%) | 24 (8.8%) | |||
| University | 309 (45.6%) | 143 (52.4%) | |||
| Postgraduate | 295 (43.4%) | 106 (38.8%) | |||
| Medical profession | χ2 = 2.079 | 2 | 0.354 | ||
| Nurse/midwives | 182 (26.8%) | 77 (28.2%) | |||
| Physician | 344 (50.7%) | 125 (45.8%) | |||
| Other | 153 (22.5%) | 71 (26.0%) | |||
| Institution type | χ2 = 5.337 | 2 | 0.069 | ||
| Primary Health Facility | 77 (11.3%) | 29 (10.6%) | |||
| Secondary Health Facility | 230 (33.9%) | 114 (41.8%) | |||
| Tertiary Referral Facility | 372 (54.8%) | 130 (47.6%) | |||
| Shift Worker | 296 (43.6%) | 134 (49.1%) | χ2 = 2.370 | 1 | 0.124 |
| Income status | χ2 = 2.547 | 2 | 0.280 | ||
| Income < expense | 115 (16.9%) | 47 (17.2%) | |||
| Income = expense | 232 (34.2%) | 107 (39.2%) | |||
| Income > expense | 332 (48.9%) | 119 (43.6%) | |||
| Residency | χ2 = 0.348 | 2 | 0.840 | ||
| Alone | 174 (25.6%) | 65 (23.8%) | |||
| Family (husband or parents) | 467 (68.8%) | 192 (70.3%) | |||
| Other (friends, dormitory etc.) | 38 (5.6%) | 16 (5.9%) | |||
| Current regular smokers | 167 (24.6%) | 82 (30.0%) | χ2 = 2.985 | 1 | 0.084 |
| Current alcohol users | 282 (41.5%) | 110 (40.3%) | χ2 = 0.123 | 1 | 0.725 |
| Caffeine consumption per day | χ2 = 0.997 | 2 | 0.607 | ||
| 0–1 cup | 241 (35.5%) | 97 (35.5%) | |||
| 2–3 cup | 311 (45.8%) | 132 (48.4%) | |||
| >3 cup | 127 (18.7%) | 44 (16.1%) | |||
| Weekly physical activity | χ2 = 5.943 | 3 | 0.114 | ||
| None | 299 (44.0%) | 144 (52.7%) | |||
| 1–3 h | 285 (42.0%) | 97 (35.5%) | |||
| 4–6 h | 62 (9.1%) | 21 (7.7%) | |||
| >6 h | 33 (4.9%) | 11 (4.0%) | |||
| Previous COVID‐19 positive diagnosis | 142 (20.9%) | 59 (21.6%) | χ2 = 0.057 | 1 | 0.811 |
Note: Values are expressed as n (%), mean ± SD. p < 0.05, statistically significant difference.
Table 2 shows the menstrual cycle characteristics of subjects. In this analysis, 10.7% (n = 102) of women reported short or long periods. A total of 12.9% (n = 123) women had a change in menstrual cycle length of longer than 9 days. Participants with prolonged menstrual flow made up 5.8% (n = 55) of the study sample. About 11% (n = 102) of the women reported experiencing light or heavy bleeding. Intermenstrual bleeding occurred in 6.5% (n = 62) patients. 76.9% (n = 732) of all women had kept track of their cycles with period tracking application on their smart devices (phone or tablet).
Table 2.
Menstrual characteristics of the participants
| Menstrual characteristics | Parameters | Number | Percentage (%) |
|---|---|---|---|
| Cycle length | <24 days | 80 | 8.4 |
| 24–38 days | 850 | 89.3 | |
| >38 days | 22 | 2.3 | |
| Cycle length variability | ≤9 days | 829 | 87.1 |
| >9 days | 123 | 12.9 | |
| Duration of flow | ≤8 days | 897 | 94.2 |
| >8 days | 55 | 5.8 | |
| Amount of blood loss | Light (<5 mL) | 24 | 2.5 |
| Moderate (5–80 mL) | 850 | 89.3 | |
| Heavy (>80 mL) | 78 | 8.2 | |
| Intermenstrual bleeding | Yes | 62 | 6.5 |
| No | 890 | 93.5 | |
| Use of period tracking application | Yes | 732 | 76.9 |
| No | 220 | 23.1 |
The comparison of psychometric measurement between study groups are presented in Table 3. The total CSS score was significantly higher in irregular menstruation group than in women with regular menstruation (t = −6.196, p < 0.001) and scores of its following subdimensions: danger (t = −3.794, p < 0.001), socioeconomic consequences (t = −6.375, p < 0.001), xenophobia (t = −4.990, p < 0.001), contamination (t = −3.838, p < 0.001), traumatic stress (t = −5.416, p < 0.001), and compulsive checking (t = −4.637, p < 0.001). The DASS‐21 depression, anxiety, and stress subdimensions were likewise significantly higher in women with irregular menstruation (p < 0.001).
Table 3.
Comparison of psychometric measurement of participants between study groups
| Variable | Menstrual cycles | Statistic | df | p * | |
|---|---|---|---|---|---|
| Regular (n = 679) | Irregular (n = 273) | ||||
| CSS | |||||
| Danger | 13.68 ± 4.74 | 15.01 ± 5.27 | t = −3.794 | 950 | <0.001 |
| Socioeconomic Consequences | 3.88 ± 4.01 | 6.55 ± 6.44 | t = −6.375 | 359 | <0.001 |
| Xenophobia | 8.45 ± 6.45 | 10.95 ± 7.19 | t = −4.990 | 457 | <0.001 |
| Contamination | 11.45 ± 6.15 | 13.14 ± 6.19 | t = −3.838 | 950 | <0.001 |
| Traumatic Stress | 5.32 ± 4.82 | 7.63 ± 6.33 | t = −5.416 | 404 | <0.001 |
| Compulsive Checking | 9.36 ± 4.91 | 11.12 ± 5.47 | t = −4.637 | 457 | <0.001 |
| CSS Total | 52.16 ± 23.18 | 64.43 ± 29.25 | t = −6.196 | 416 | <0.001 |
| DASS‐21 | |||||
| Anxiety | 4.25 ± 3.29 | 5.64 ± 4.04 | t = −5.070 | 423 | <0.001 |
| Depression | 6.52 ± 4.25 | 7.84 ± 4.69 | t = −4.023 | 460 | <0.001 |
| Stress | 6.77 ± 3.64 | 8.08 ± 4.17 | t = −4.541 | 447 | <0.001 |
Note: Values are expressed as mean ± SD.
Abbreviations: CSS, COVID‐19 Stress Scales; DASS‐21, Depression Anxiety Stress Scales‐21.
p < 0.05, statistically significant difference.
The univariable and multivariable logistic regression analysis was used to assess factors associated with irregular menstrual cycles (Table 4). Univariable logistic regression analysis revealed that the CSS total score (p < 0.001, odds ratio [OR] = 1.019, 95% confidence interval [CI] 1.013–1.025), DASS‐21 anxiety (p < 0.001, OR = 1.113, 95% Cl 1.070–1.157), depression (p < 0.001, OR = 1.069, 95% Cl 1.036–1.103), and stress (p < 0.001, OR = 1.092, 95% Cl 1.052–1.133) subdimensions were significant predictors of irregular menstruation. Multivariable regression analysis was conducted with variables that had significance in the univariate model. The multivariate model was significant (χ2 (5) = 53.714, p < 0.001), and the CSS total score was a significant predictor (p < 0.001, OR = 1.015, 95% Cl 1.009–1.022) for irregular menses.
Table 4.
Results of univariate and multivariate logistic regression analysis applied to determine the predictors of the irregular menstrual cycle
| Predictor | Univariate | Multivariate | ||
|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | |
| Age (1‐point increase) | 1.002 (0.977–1.028) | 0.875 | ||
| Shift worker | 1.247 (0.941–1.653) | 0.124 | ||
| Age at menarche (1‐point increase) | 1.080 (0.971–1.201) | 0.156 | ||
| Body mass index (1‐point increase) | 1.027 (0.991–1.064) | 0.151 | ||
| COVID‐19 Stress Scales total score (1‐point increase) | 1.019 (1.013–1.025) | <0.001 | 1.015 (1.009–1.022) | <0.001 |
| DASS‐21 Anxiety Score (1‐point increase) | 1.113 (1.070–1.157) | <0.001 | 1.039 (0.976–1.106) | 0.231 |
| DASS‐21 Depression Score (1‐point increase) | 1.069 (1.036–1.103) | <0.001 | 1.024 (0.973–1.078) | 0.356 |
| DASS‐21 Stress Score (1‐point increase) | 1.092 (1.052–1.133) | <0.001 | 0.996 (0.928–1.068) | 0.903 |
Abbreviation: DASS‐21, Depression Anxiety Stress Scales‐21.
Discussion
This study examined the psychological impact of the COVID‐19 outbreak on health professionals' menstrual cycle characteristics. Our findings indicate that perceived depression anxiety and stress during the pandemic were positively related to menstrual irregularities among healthcare workers. CSS subdimension and total scores and DASS‐21 scores for all subdimensions were significantly higher in the irregular menstruation group. Another notable finding in our study is that the CSS total score is an independent predictor for menstrual cycle irregularity in female healthcare workers.
Previous reports have shown the link between local or global crisis (wars, earthquakes) related to emotional, traumatic stress, and menstrual abnormalities.27, 28, 29, 30 The prevalence of irregular cycles among childbearing women was estimated to be about 16% in the Turkish population.31, 32 Whereas our results showed a much higher prevalence rate of 28.7% suffering from irregular periods among the adult women under pandemic conditions. There were two studies where the effect of the COVID‐19 pandemic on menstrual cycle characteristics was evaluated. In line with our results, the study from Turkey reported that 27.6% of women experienced irregular menses.33 Surprisingly, another study reported a significantly decreased menstrual regulation incidence during the pandemic with a rate of 10.5%.34 However, the sample size of these two studies was considerably smaller than ours.
Previous studies regarding the prevalence of irregular periods and their association with mental health issues are available in the literature. Some previous reports have documented positive relationships between perceived stress and irregular menstrual cycles35, 36, 37 and some others reported higher depressive symptoms in patients with irregular menses.38, 39 The results of studies by Nillni et al. and Jung et al. showed that women with irregular menstruation were more likely to report depressive symptoms and perceived stress.3, 9 Moreover, some studies evaluated the relation between psychological stress in the workplace and menstrual function and found significantly higher rates of cycle irregularity among women who are exposed to stress at work.40, 41, 42 One published data addresses the relationship between menstrual cycle irregularity and anxiety disorder. According to the results of this study, women with irregular cycles had less likely to have current anxiety disorder compared to those who reported regular cycles.43 In contrast, in the present study higher depression, anxiety, and stress levels were found to be associated with irregular menstruation. Additionally, our results revealed that pandemic‐linked anxiety and stress was a significant predictor of the irregular menstrual cycle. The close interaction between the hypothalamic–pituitary–adrenal (HPA) axis and the HPG axis has been claimed to be responsible for associations between irregular periods and psychological distress. The HPA axis plays a central role in the body's stress response. Exposure to physical, social, and environmental stressors causes the secretion of various hormones and dysregulation of HPA axis activity.44 This may result in the disruption of the normal functioning HPG axis via several mechanisms including: (1) the inhibition of hypothalamic GnRH release by CRH, endogen opioids, and glucocorticoids; (2) decreased pituitary response to GnRH, resulting in decreased luteinizing hormone (LH) secretion; (3) direct inhibitory effect of glucocorticoids upon the secretion of sex hormones; (4) glucocorticoid‐induced resistance to the gonadal steroids in target tissues; and (5) direct catecholaminergic inhibition on FSH, LH, and prolactin secretion.45, 46, 47
This study showed that the COVID‐19 pandemic‐induced psychological distress is related with menstrual cycle irregularities. Irregular cycles can also have long‐term consequences. Previous studies showed that menstrual cycle characteristics are closely linked with future reproductivity. A large prospective study with 391 320 participants found decreased fecundability ratios in women with longer cycle length, both shorter and longer bleeding duration.48 Another study observed a correlation among short cycle length, heavy menstrual bleeds, and lower fecundability ratios.49
Our study is limited by the inherent bias associated with self‐selecting web surveys. Another important point to note about was the nonresponse bias due to sampling in mental health studies. Individuals with higher levels of psychological distress may choose not to disclose their mental health problems to someone else. However, previous studies reported inconsistent results on the association between voluntary recruitment and the prevalence of mental disorders. In a recent study, Kawakami et al. reported that response rate does not strongly affect the prevalence estimates of mental disorders.50 While healthcare workers are on the frontline during the COVID‐19 pandemic and experience occupational exposures, we assume that they would intend to disclose their professional deformations and this results with low nonresponse bias. Additionally, retrospective recall of menstrual cycle characteristics may lead to misclassification of participants. However, earlier studies have reported that women recall their menstrual history.51, 52 Also, the majority of our study population was using a period tracking application, which may increase the accuracy and reliability of the data. Despite these weaknesses, our study also has several strengths. Until now, no previous study has investigated the mental health issues related to menstrual irregularities during the outbreak. Second, this study was conducted among a specific group of women, who experienced considerable psychological distress under the pandemic conditions of COVID‐19. Third, we applied a specific questionnaire that allows us to provide a multifactorial measure of COVID‐19‐related distress with five intercorrelated subscales. Another strength of this study was the large sample size of the cohort.
In summary, the current study showed the association between the COVID‐19 pandemic‐induced anxiety, perceived stress, depressive symptoms, and increased prevalence of menstrual cycle irregularity among healthcare providers. These results emphasize the need for interventions to improve the mental well‐being of healthcare professionals during an outbreak for their future reproductive health.
Conflict of interest
The authors declared no potential conflicts of interest.
Author Contributions
Taha Takmaz: Project development; Data Collection; Manuscript writing; Supervision. Ibrahim Gundogmus: Data analysis; Project development; Manuscript editing; Data Collection. Sabri Berkem Okten: Data Collection; Project development; Manuscript editing; Final proofreading. Anil Gunduz: Manuscript editing; Final proofreading; Data Collection.
Data availability statement
Data available on request due to privacy/ethical restrictions.
References
- 1.Wang YX, Arvizu M, Rich‐Edwards JW, Stuart JJ, Manson JE, Missmer SA, et al. Menstrual cycle regularity and length across the reproductive lifespan and risk of premature mortality: prospective cohort study. BMJ. 2020;371:m3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fraser IS, Critchley HO, Broder M, Munro MG. The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding. Semin Reprod Med. 2011;29:383–90. [DOI] [PubMed] [Google Scholar]
- 3.Nillni YI, Wesselink AK, Hatch EE, Mikkelsen EM, Gradus JL, Rothman KJ, et al. Mental health, psychotropic medication use, and menstrual cycle characteristics. Clin Epidemiol. 2018;28:1073–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terry KL, Willett WC, Rich‐Edwards JW, Hunter DJ, Michels KB. Menstrual cycle characteristics and incidence of premenopausal breast cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:1509–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cirillo PM, Wang ET, Cedars MI, Chen LM, Cohn BA. Irregular menses predicts ovarian cancer: prospective evidence from the Child Health and Development Studies. Int J Cancer. 2016;139:1009–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwak Y, Kim Y, Baek KA. Prevalence of irregular menstruation according to socioeconomic status: a population‐based nationwide cross‐sectional study. PLoS One. 2019;14:e0214071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ansong E, Arhin SK, Cai Y, Xu X, Wu X. Menstrual characteristics, disorders and associated risk factors among female international students in Zhejiang Province, China: a cross‐sectional survey. BMC Womens Health. 2019;19:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munro MG, Critchley HO, Broder MS, Fraser IS, FIGO Working Group on Menstrual Disorders . FIGO classification system (PALM‐COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113:3–13. [DOI] [PubMed] [Google Scholar]
- 9.Jung EK, Kim SW, Ock SM, Jung KI, Song CH. Prevalence and related factors of irregular menstrual cycles in Korean women: the 5th Korean National Health and Nutrition Examination Survey (KNHANES‐V, 2010‐2012). J Psychosom Obstet Gynaecol. 2018;39:196–202. [DOI] [PubMed] [Google Scholar]
- 10.Schoep ME, Nieboer TE, van der Zanden M, Braat DDM, Nap AW. The impact of menstrual symptoms on everyday life: a survey among 42,879 women. Am J Obstet Gynecol. 2019;220:569.e1–7. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization . Coronavirus disease (COVID‐19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 26 Sept 2020.
- 12. https://covid19.who.int
- 13.Bao Y, Sun Y, Meng S. 2019‐nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salari N, Hosseinian‐Far A, Jalali R, Vaisi‐Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: a systematic review and meta‐analysis. Global Health. 2020;16:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park JS, Lee EH, Park NR, Choi YH. Mental health of nurses working at a government‐designated hospital during a MERS‐CoV outbreak: a cross‐sectional study. Arch Psychiatr Nurs. 2018;32:2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.d'Ettorre G, Ceccarelli G, Santinelli L, Vassalini P, Innocenti GP, Alessandri F, et al. Post‐traumatic stress symptoms in healthcare workers dealing with the COVID‐19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18:601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demartini B, Nisticò V, D'Agostino A, Priori A, Gambini O. Early psychiatric impact of COVID‐19 pandemic on the general population and healthcare workers in Italy: a preliminary study. Front Psych. 2020;11:561345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossi R, Socci V, Pacitti F, di Lorenzo G, di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Netw Open. 2020;3:e2010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.González‐Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López‐Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID‐19) in Spain. Brain Behav Immun. 2020;87:172–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fraser IS, Critchley HO, Munro MG, Broder M. Can we achieve international agreement on terminologies and definitions used to describe abnormalities of menstrual bleeding? Hum Reprod. 2007;22:635–43. [DOI] [PubMed] [Google Scholar]
- 23.Fraser IS, Critchley HO, Munro MG, Broder M, Writing Group for this Menstrual Agreement Process . A process designed to lead to international agreement on terminologies and definitions used to describe abnormalities of menstrual bleeding. Fertil Steril. 2007;87:466–76. [DOI] [PubMed] [Google Scholar]
- 24.Taylor S, Landry C, Paluszek M, Fergus TA, McKay D, Asmundson GJ. Development and initial validation of the COVID stress scales. J Anxiety Disord. 2020;72:102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43. [DOI] [PubMed] [Google Scholar]
- 26.Saricam H. The psychometric properties of Turkish version of Depression Anxiety Stress Scale‐21 (DASS‐21) in health control and clinical samples. J Cognit Behav Psychother Res. 2018;7:19–30. [Google Scholar]
- 27.Whitacre FE. War amenorrhea. JAMA. 1944;124:399. [Google Scholar]
- 28.Hannoun AB, Nassar AH, Usta IM, Zreik TG, Abu Musa AA. Effect of war on the menstrual cycle. Obstet Gynecol. 2007;109:929–32. [DOI] [PubMed] [Google Scholar]
- 29.Pasternak A, Brooks PG. The long‐term effects of the Holocaust on the reproductive function of female survivors. J Minim Invasive Gynecol. 2007;14:211–7. [DOI] [PubMed] [Google Scholar]
- 30.Liu X, Yang Y, Yuan P, Zhang X, Han Y, Cao Y, et al. A study of the relationship between mental health and menstrual abnormalities in female middle school students from post‐earthquake Wenchuan. Biosci Trends. 2010;4:4–8. [PubMed] [Google Scholar]
- 31.Filippi V, Marshall T, Bulut A, Graham W, Yolsal N. Asking questions about women's reproductive health: validity and reliability of survey findings from Istanbul. Trop Med Int Health. 1997;2:47–56. [DOI] [PubMed] [Google Scholar]
- 32.Bulut A, Filippi V, Marshall T, Nalbnant H, Yolasal N, Graham W. Contraceptive choice and reproductive morbidity in Istanbul. Stud Fam Plann. 1997;28:35–43. [PubMed] [Google Scholar]
- 33.Yuksel B, Ozgor F. Effect of the COVID‐19 pandemic on female sexual behavior. Int J Gynaecol Obstet. 2020;150:98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aolymat I. A cross‐sectional study of the impact of COVID‐19 on domestic violence, menstruation, genital tract health, and contraception use among women in Jordan. Am J Trop Med Hyg. 2020;104:519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Toufexis D, Rivarola MA, Lara H, Viau V. Stress and the reproductive axis. J Neuroendocrinol. 2014;26:573–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palm‐Fischbacher S, Ehlert UJ. Dispositional resilience as a moderator of the relationship between chronic stress and irregular menstrual cycle. J Psychosom Obstet Gynaecol. 2014;35:42–50. [DOI] [PubMed] [Google Scholar]
- 37.Schliep KC, Mumford SL, Vladutiu CJ, Ahrens KA, Perkins NJ, Sjaarda LA, et al. Perceived stress, reproductive hormones, and ovulatory function: a prospective cohort study. Epidemiology. 2015;26:177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harlow BL, Cohen LS, Otto MW, Spiegelman D, Cramer DW. Early life menstrual characteristics and pregnancy experiences among women with and without major depression: the Harvard study of moods and cycles. J Affect Disord. 2004;79:167–76. [DOI] [PubMed] [Google Scholar]
- 39.Bleil ME, Bromberger JT, Latham MD, Adler NE, Pasch LA, Gregorich SE, et al. Disruptions in ovarian function are related to depression and cardiometabolic risk during premenopause. Menopause. 2013;20:631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fenster L, Waller K, Chen J, Hubbard AE, Windham GC, Elkin E, et al. Psychological stress in the workplace and menstrual function. Am J Epidemiol. 1999;149:127–34. [DOI] [PubMed] [Google Scholar]
- 41.Lin HT, Lin LC, Shiao JS. The impact of self‐perceived job stress on menstrual patterns among Taiwanese nurses. Ind Health. 2007;45:709–14. [DOI] [PubMed] [Google Scholar]
- 42.Nagma S, Kapoor G, Bharti R, Batra A, Batra A, Aggarwal A, et al. To evaluate the effect of perceived stress on menstrual function. J Clin Diagn Res. 2015;9:QC01–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barron ML, Flick LH, Cook CA, Homan SM, Campbell C. Associations between psychiatric disorders and menstrual cycle characteristics. Arch Psychiatr Nurs. 2008;22:254–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Young EA, Korszun A. The hypothalamic‐pituitary‐gonadal axis in mood disorders. Endocrinol Metab Clin North Am. 2002;31:63–78. [DOI] [PubMed] [Google Scholar]
- 45.Nicoletti I, Filipponi P, Sfrappini M, Fedeli L, Petrelli S, Gregorini G, et al. Catecholamines and pituitary function. I. Effects of catecholamine synthesis inhibition and subsequent catecholamine infusion on gonadotropin and prolactin serum levels in normal cycling women and in women with hyperprolactinemic amenorrhea. Horm Res. 1984;19:158–70. [DOI] [PubMed] [Google Scholar]
- 46.Schenker JG, Meirow D, Schenker E. Stress and human reproduction. Eur J Obstet Gynecol Reprod Biol. 1992;45:1–8. [DOI] [PubMed] [Google Scholar]
- 47.Johnson EO, Kamilaris TC, Chrousos GP, Gold PW. Mechanisms of stress: a dynamic overview of hormonal and behavioral homeostasis. Neurosci Biobehav Rev. 1992;16:115–30. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Q, Wang YY, Zhang Y, Zhang HG, Yang Y, He Y, et al. The influence of age at menarche, menstrual cycle length and bleeding duration on time to pregnancy: a large prospective cohort study among rural Chinese women. BJOG. 2017;124:1654–62. [DOI] [PubMed] [Google Scholar]
- 49.Wesselink AK, Wise LA, Hatch EE, Rothman KJ, Mikkelsen EM, Stanford JB, et al. Menstrual cycle characteristics and fecundability in a North American preconception cohort. Ann Epidemiol. 2016;26:482–487.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kawakami N, Yasuma N, Watanabe K, Ishikawa H, Tachimori H, Takeshima T, et al. Association of response rate and prevalence estimates of common mental disorders across 129 areas in a nationally representative survey of adults in Japan. Soc Psychiatry Psychiatr Epidemiol. 2020;55:1373–82. [DOI] [PubMed] [Google Scholar]
- 51.Must A, Phillips SM, Naumova EN, Blum M, Harris S, Dawson‐Hughes B. Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am J Epidemiol. 2002;155:672–9. [DOI] [PubMed] [Google Scholar]
- 52.Creinin MD, Keverline S, Meyn LA. How regular is regular? An analysis of menstrual cycle regularity. Contraception. 2004;70:289–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


