Abstract
COVID‐19 significantly affects patients' mental health, triggering a wide range of psychological disorders, including anxiety. The aim of this study was to investigate the effect of mandala colouring on the anxiety of hospitalized COVID‐19 patients. In this randomized controlled clinical trial, 70 hospitalized patients with COVID‐19 were randomly divided between the intervention and control groups. Standard care was provided for both groups. The intervention group spent 30 min/day for six consecutive days performing mandala colouring. Patient anxiety was measured prior and subsequent to the intervention in both groups using the Spielberger State‐Trait Anxiety Inventory. Data were analysed using SPSS software version 25. The mean anxiety score was not significantly different between the two groups before the intervention (P = 0.08). Subsequent to the intervention, the mean anxiety score in the intervention and control groups was 44.05 ± 4.67 and 67.85 ± 6.25, respectively, indicating a statistically significant (P = 0.0001) decrease in the anxiety measured among the intervention group as compared with that of the control group. The results of this study show that 30 min of mandala colouring daily is an effective strategy for reducing anxiety in hospitalized COVID‐19 patients. Mandala colouring can complement routine treatment and provides a non‐pharmaceutical option for decreasing patient anxiety.
Keywords: anxiety, art therapy, colouring, COVID‐19, mandala
INTRODUCTION
As an emerging disease, coronavirus disease 2019 (COVID‐19) has widespread effects on people's physical and mental health (Usher et al. 2020b). Commonly experienced negative emotions include helplessness, confusion, fear, anxiety, depression, and guilt (Usher et al. 2020a; Usher et al. 2020c). Anxiety disorders are a pressing mental health concern (Abbing et al. 2018). Feelings of anxiety are an expected response to stressful situations (Roy et al. 2020). They can be characterized by unpleasant feelings such as panic and fear (Gençdoğan et al. 2018). The experience of anxiety can lead to a series of physiological changes that can weaken the immune system(Liu et al. 2020) and ultimately threaten a patient's health(Curran et al. 2017). Anxiety has also been associated with depression, suicidality, and self‐harming behaviour (Holmes et al. 2020). In a meta‐analysis, Deng et al. reported a prevalence of anxiety in COVID‐19 patients of 47%(Deng et al. 2020). For many patients diagnosed with COVID‐19, a fear of the unknown nature of the disease and quarantine restrictions can lead to anxiety (Liu et al. 2020). Furthermore, the physical and social isolation of patients with COVID‐19 has been shown to contribute to anxiety and sleep disorders (Rajeswari & SanjeevaReddy 2020). Many studies have highlighted the high prevalence of psychiatric disorders among COVID‐19 survivors, demonstrating the importance of prevention, screening, and treatment for these diagnoses (Duan & Zhu 2020; Epstein et al. 2020; Paz et al. 2020).
Various pharmacologic and non‐pharmacologic methods may be used to manage anxiety. Although symptoms of anxiety in patients with COVID‐19 are typically mild in the early stages of the disease, they can suddenly worsen (Liu et al. 2020; Rajeswari & SanjeevaReddy 2020). The use of benzodiazepines or other pharmacologic agents to treat anxiety introduces an increased risk of respiratory depression and side effects causing clinical deterioration. As a result, non‐pharmaceutical interventions, such as art therapy, may be safer alternatives (Liu et al. 2020). There is a close relationship between art, healing, and well‐being which has been acknowledged around the world. Since the mid‐twentieth century, art has been an important tool for the diagnosis and treatment of mental illnesses (Gençdoğan et al. 2018). According to art psychotherapists, mandala colouring is a psychotherapy technique which can provide psychological support and healing(Elkis‐Abuhoff et al. 2009; Gençdoğan et al. 2018). In a study investigating the relationship between consciousness, the unconscious, and reality, it was noted that mandala colouring could be used as an effective method for treating some diseases (Gençdoğan et al. 2018). The mandala is a product of creative imagination, in which deep religious, philosophical, psychological, and aesthetic concepts are mingled(Gençdoğan et al. 2018; Kim et al. 2018). Mandalas include art forms created using a circular framework. In Sanskrit, the word mandala means ‘the whole world’ or ‘the circle of healing’, reflecting the order and unity of the universe(Elkis‐Abuhoff et al. 2009). This concept refers individuals to their essence and guides them to be honest with themselves to achieve a peaceful spirit (Kim et al. 2018). This circular art has been traditionally used for meditation in various Eastern cultures(Malchiodi 1993) and is a symbol of psychological integrity(Elkis‐Abuhoff et al. 2009).
A systematic review by Abbing et al. showed that art therapy had a positive effect on reducing anxiety in patients(Abbing et al. 2018). The results of another study by Flett et al. also revealed that daily mandala colouring improved psychological symptoms(Flett et al. 2017). Other studies have demonstrated that mandala colouring can decrease anxiety(Carsley et al. 2015). Mandala colouring is a safe and accessible activity that does not require any special skills or training and can be used as a complementary strategy for anxiety reduction. To date, there are no published studies investigating the effects of mandala colouring on anxiety in patients with COVID‐19. Considering the relatively high prevalence of anxiety in this patient population and its devastating effects on the patient's physical and mental health, this study aimed to investigate the effect of this mandala colouring on anxiety levels in hospitalized COVID‐19 patients.
METHODS
Study design
This study was a randomized controlled clinical trial performed from May 20, 2020 to November 30, 2020 on 70 patients hospitalized with COVID‐19 on the internal medicine and infectious disease wards of the Amir Al‐Momenin Hospital of Arak, affiliated with Arak University of Medical Sciences.
Participants
The eligible study population included all patients between 18 and 65 years of age diagnosed with COVID‐19 who were admitted for greater than 24 hours during the dates of study. There could be no documented history of diagnosis or treatment for mental illnesses/anxiety disorder. The selected participants were clinically stable, without dyspnoea or hypoxia, and were not at the end‐stage of the disease(Elkis‐Abuhoff et al. 2009; Jodaki et al. 2021; Kim et al. 2018). Exclusion criteria were lack of capacity, deterioration of the patient's condition (decline in consciousness or haemodynamic instability), transfer to the ICU, or discharge(Curran et al. 2017; Elkis‐Abuhoff et al. 2009; Jodaki et al. 2021).
Sample Size
The sample size was determined based on Koo et al. (2020) using the following formula:
Considering α = 0.05, β = 0.2, S1 = 6.8, S2 = 11.8, and the statistical power of 0.8, the sample size per each group was determined n = 35 (Figure 1).
Randomization
Patients were enrolled using a convenience sampling method. They were randomly divided between the intervention and control groups using a block randomization design. For this study, ten blocks were considered; half of which were coded ‘C’, and the other half were coded ‘E’, which were then assigned to the control and intervention groups, respectively. The codes were non‐repeatedly placed in each block, and the blocks were randomly selected without any substitution.
Outcome assessment
The tools used in this study included two questionnaires. The first one was a demographic questionnaire to collect information such as age, gender, marital status, education level, employment status, and length of hospitalization. These data were collected through either medical record review or direct patient interview. The second questionnaire was the Spielberger State‐Trait Anxiety Inventory (STAI). This instrument, developed by Spielberger in 1983, includes independent self‐assessment scales for measuring overt (state) and covert anxiety (trait) (Jodaki et al. 2021). This study focussed on the overt anxiety scale, which consists of 20 items that assess a person's feelings based on a 4‐point Likert scale (very low, low, high, and very high). The total score of the STAI can range from 20 to 80. In the overt anxiety scale, scores are interpreted using the following categories: 20–31 (mild); 32–42 (mild/moderate); 43–53 (moderate/severe); 54–64 (relatively severe); 65–75 (severe); and ≥76 (very severe) (Jodaki et al. 2021). Standardization and intercultural matching of the STAI questionnaire in Iran were performed by Roohy et al. (2005), reporting a reliability of 0.90 (Roohy et al. 2005). The reliability of this tool was confirmed, delivering a Cronbach's alpha coefficient of 92%.
Intervention
On the second hospital day or later, patients were eligible for recruitment and assignment to the control and intervention groups. Demographic information was collected through medical record review and patient interviews for patients in both groups. Subsequently, the STAI questionnaire was administered. In the control group, patients received routine care. In the intervention group, patients received routine care and performed mandala colouring for 30 min/day in the evenings for six consecutive days. On the evening of the 6th day of the intervention, the STAI questionnaire was again administered to patients in both groups.(Gençdoğan et al. 2018; Noor et al. 2017; Yakar et al. 2021). The evening time was chosen for performing the intervention to avoid interference with clinical nursing tasks (medication administration and other therapeutic interventions). Six preselected mandala drawings were separately printed on A4 (21.0 cm × 29.7 cm) sheets. A new drawing was given to each patient daily. Various designs were used for the six days of the intervention. At the beginning of the study, a pack of six coloured pencils (yellow, blue, green, red, purple, and brown) was provided. Each patient was advised to colour in relative silence (Angellim et al. 2020.; Gençdoğan et al. 2018; Yakar et al. 2021). For illiterate patients, the researcher read the questions to the patient and then recorded their responses.
Data analysis
In this study, the data were analysed using SPSS (version 25) software. Quantitative variables were described using mean and standard deviation, and qualitative variables were presented by frequency and percentage. For inferential analysis of qualitative variables, the Chi‐square and Fisher's exact tests were applied. The distribution of quantitative variables was assessed by the Kolmogorov–Smirnov test. The independent (or paired) samples Student’s t test or its non‐parametric equivalents (the Mann–Whitney or Wilcoxon tests) were used accordingly. To control the confounding effects of baseline parameters, the covariance test was used. A P‐value of <0.05 was considered statistically significant.
Ethical considerations
This study was approved by the Corona Research Center of the Research Committee of Arak University of Medical Sciences (registration code: 3634) and the Ethics Committee of the university (ethics code: IR.ARAKMU.REC.1399.089). After obtaining the required permissions from the Vice Chancellor for Research, the study was performed at the Amir Al‐Momenin Hospital of Arak. The study's protocol was registered at the Iranian Registry for Clinical Trials (trial code: IRCT20180519039711N6) and is available online. Before starting the study, the patients were advised regarding the method and purpose of the study and informed consent acquired.
Results
Thirty‐two (45.7%) of the participants were female, and 38 (54.3%) were male. The mean age was 39 ± 7.9 years, and the mean duration of hospitalization due to COVID‐19 at the onset of study participation was 8.4 ± 5.2 days. Other demographic and clinical data are presented in Table 1, indicating no statistically significant differences between the intervention and control groups.
Table 1.
Comparison of demographic and clinical characteristics of patients in the control and intervention groups
| Control group | Intervention group | Significance | |||
|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | ||
| Gender | |||||
| Female | 13 | 37.1 | 19 | 54.3 |
X2=2.072 P = 0.230 |
| Male | 22 | 62.9 | 16 | 45.7 | |
| Marital status | |||||
| Single | 8 | 22.9 | 6 | 17.1 |
Fisher exact=2.826 P = 0.460 |
| Married | 23 | 65.7 | 28 | 80 | |
| Divorced | 2 | 5.7 | 1 | 2.9 | |
| Widowed | 2 | 5.7 | 0 | 0 | |
| Educational level | |||||
| Illiterate | 5 | 14.3 | 5 | 14.3 |
Fisher exact=1.865 P = 0.117 |
| High school | 10 | 28.6 | 9 | 25.7 | |
| Diploma | 11 | 31.3 | 10 | 28.6 | |
| Superior diploma | 1 | 2.9 | 2 | 5.7 | |
| Undergraduate | 7 | 20 | 8 | 22.8 | |
| Master | 1 | 2.9 | 1 | 2.9 | |
| Occupation | |||||
| Employee | 12 | 34.2 | 9 | 25.8 |
Fisher exact=4.638 P = 0.467 |
| Self‐employed | 13 | 37.1 | 11 | 31.3 | |
| Unemployed | 1 | 2.9 | 0 | 0 | |
| Retired | 1 | 2.9 | 1 | 2.9 | |
| Homemaker | 8 | 22.9 | 14 | 40 | |
| Mean (SD) | Mean (SD) | ||
|---|---|---|---|
| Age (years) | 40.42 (8.59) | 37.65 (6.92) |
T = 1.468 P = 0.142 |
| Duration of hospitalization (days) | 8.37 (4.26) | 9.42 (5.94) |
Mann–Whitney u = 492.5 P = 0.157 |
SD, Standard deviation.
Our findings demonstrate that the mean anxiety score was not significantly different between the two groups prior to the intervention. However, this score significantly increased in the control group while decreasing in the intervention group at the end of the study period (Table 2).
Table 2.
Comparison of the mean anxiety scores of COVID‐19 patients before and after the intervention in the two studied groups
| Group | Before | After | P‐Value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Anxiety Score on STAI | Intervention | 58.68 | 2.97 | 44.05 | 4.67 | 0.0001 |
| Control | 57.43 | 4.44 | 67.85 | 6.25 | 0.0001 | |
| P‐value | 0.08 | 0.0001* | ||||
SD, Standard deviation; *ANCOVA.
To control for the confounding effect of the baseline anxiety score, analysis of covariance (ANCOVA) was performed, resulting in the adjusted mean baseline scores of 56.94 ± 0.56 and 55.96 ± 0.56 in the control and intervention groups, respectively (P > 0.05, Table 3).
Table 3.
Estimated marginal means of baseline anxiety after ANCOVA
| Group | Mean | Std. Error | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Control | 56.949a | .564 | 49.824 | 61.074 |
| Intervention | 55.965a | .564 | 46.840 | 57.091 |
Abbreviation: Std. Error, standard error.
This demonstrates no statistically significant difference in the distribution of various anxiety severities between the intervention and control groups at the baseline (P = 0.08), with all patients scoring within the mild and moderate anxiety ranges. After the intervention, there was a statistically significant difference in the distribution of anxiety severity between the two groups (P < 0.0001). According to the Wilcoxon test, anxiety levels increased in a statistically significant fashion in the control group (P < 0.0001). Four patients in the control group, who had mild anxiety at the baseline, progressed to the moderate level, and one patient who had moderate anxiety entered into the severe range. Conversely, patients in the intervention group recorded a statistically significant decrease in anxiety (P = 0.008). In this group, three patients who had severe anxiety fell into a lower category. Out of 26 patients who had moderate anxiety, seven entered the mild range, indicating an improvement in their anxiety. According to the Wilcoxon test, changes in anxiety levels in both groups were statistically significant after the intervention (P < 0.003) (Table 4).
Table 4.
Distribution of anxiety scores before and after intervention
| Variable | Group |
Before intervention N (%) |
After intervention N (%) |
P‐value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Mild | Moderate | Severe | No | Mild | Moderate | Severe | |||
| Anxiety Score | Intervention | 0 | 6 (17.1) | 26 (74.3) | 3 (8.6) | 0 | 16 (45.8) | 19 (54.2) | 0 | 0.008 |
| Control | 0 | 6 (17.1) | 27 (77.2) | 2 (5.7) | 0 | 2 (5.7) | 30 (85.7) | 3(8.6) | 0.003 | |
|
X2=15.96 P‐value <0.08 |
Fisher exact=0.699 P‐Value <0.003 |
|||||||||
N = Number.
DISCUSSION
The present study shows that patients hospitalized with COVID‐19 had mild to moderate levels of anxiety at baseline. Other studies have demonstrated anxiety among this population, especially when receiving treatment in isolation (Liu et al. 2020). The results of one study by Zandifar et al. showed severe and very severe anxiety levels in all patients hospitalized with COVID‐19 (Zandifar et al. 2020). In one study examining the prevalence and risk of depression/anxiety among patients hospitalized with COVID‐19, a high level of anxiety was most notably documented in patients who had lost relatives due to the disease (Nie et al. 2021). In another study, 36% of 44 patients hospitalized with COVID‐19 exhibited symptoms of severe anxiety (Parker et al. 2020).
The results of our study show an increase in measured anxiety among the control group consistent with previously documented results (Mazza et al. 2020; Nie et al. 2021; Parker et al. 2020; Sun et al. 2021). Fear, denial, and stigma usually occur during the early stages of disease (Sun et al. 2021; Zhou 2020). Numerous factors, including fear of permanent disability or death, uncertainty about the diagnosis and treatment, isolation from family and friends, guilt regarding the possibility of infecting family members, changes in diet, sleep disturbances, and physical symptoms have been noted to contribute to the development and persistence of anxiety(Sun et al. 2021; Zandifar et al. 2020).
Given the increased prevalence and risk of anxiety among patients hospitalized with COVID‐19, psychological counselling and art therapy are useful non‐pharmacologic interventions to alleviate these feelings(Sun et al. 2021; Zandifar et al. 2020). A review by Abbing et al. showed that various types of art therapy methods could reduce anxiety in adults (Abbing et al. 2018). In another study by Yakar et al., mandala colouring significantly reduced distress and anxiety in cancer patients (Yakar et al. 2021). In the present study, hospitalized COVID‐19 patients with mild to moderate anxiety who performed 30 min daily of mandala colouring showed a significant reduction in these symptoms. Artistic and structural efforts that are based on Yogi's theory, such as mandala colouring, have been shown to be effective in reducing anxiety and stress, as well as in processing complex personal, negative emotions, and promoting general well‐being (Duong et al. 2018). McMahon declared that mandala colouring was not only one of the most effective methods in counselling groups, but also a calming tool for reducing anxiety, developing relationships, and nurturing a creative space for expressing one's feelings (McMahon et al. 2007). Previous studies have shown that mandala colouring has a significant impact on reducing anxiety(Amelia et al. 2020; Koo et al. 2020; Lee 2018; Salazar 2019). A study by Curry & Kasser showed significantly lower levels of anxiety in a group of students who painted mandalas (Curry & Kasser 2005). The anxiety‐reducing effects of mandala colouring appear to be stronger than that of painting (Lee 2018) (37). Mandal colouring may be an effective intervention for other populations, including those with long‐term anxiety (Curry & Kasser 2005).
LIMITATIONS
Many factors, including economic, cultural, and social differences, contribute to the development of anxiety and vary between different sample populations. These were not examined or controlled for in this study. Furthermore, the lack of accurate information about the origin of anxiety, as well as an unclear relationship between COVID‐19 disease and the development of anxiety, makes the results less generalizable. Some of these limitations may be overcome by performing future studies with higher sample sizes.
CONCLUSION
Mandala colouring was effective in reducing measured anxiety in patients hospitalized due to COVID‐19. Based on the findings of this study, physicians and nurses may consider offering mandala colouring as a complementary treatment option along with routine therapies. It is a safe, cheap, and accessible alternative therapeutic strategy to reduce anxiety among patients hospitalized with COVID‐19. Future research may focus on comparing the effects of mandala colouring with pharmacologic therapy for anxiety in patients hospitalized with COVID‐19.
RELEVANCE TO CLINICAL PRACTICE
Mandala colouring can complement routine treatment and provides a non‐pharmaceutical option for decreasing patient anxiety. Physicians and nurses may consider offering mandala colouring as a complementary treatment option along with routine therapies. It is a safe, cheap, and accessible alternative therapeutic strategy to reduce anxiety among patients hospitalized with COVID‐19.
Funding information
This study was supported by Arak University of Medical Sciences, Arak, Iran (No 3634).
Figure 1.
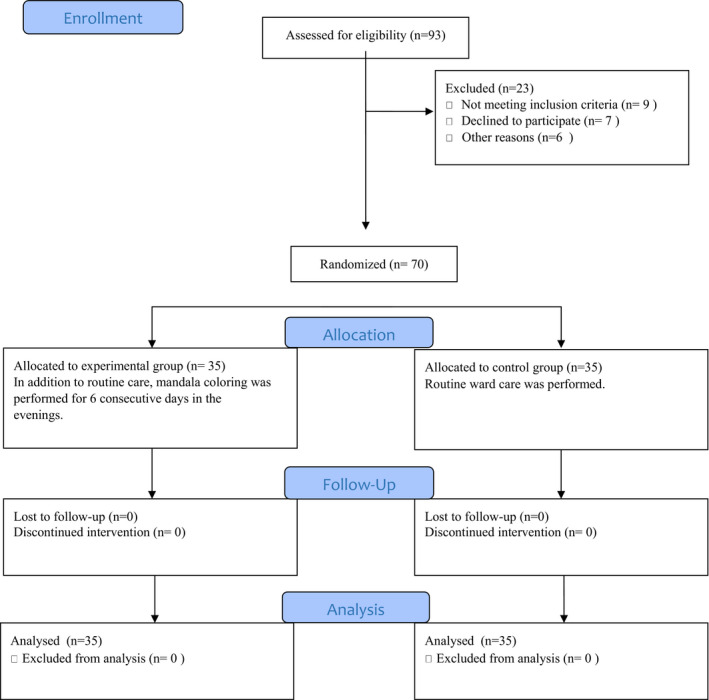
The CONSORT follows diagram of the patients' recruitment.
Acknowledgements
The authors would like to appreciate the patients and colleagues in Amir Al‐Momenin hospital in Arak city, as well as the assistant of the Vice Chancellor for Research and Technology of Arak University of Medical Sciences.
Authorship statement: FK, MR, MG, EH, NM, and FR involved in study conception and design, data collection, data interpretation, and critical revision of the paper; MT, SM, FR, and MG involved in study conception and design; MG, MR, and MG involved in study conception and design, and critical revision of the paper; FK, MG, SM, MT, FR, and MR involved in study conception and design, data analysis (Statistics specialist) and interpretation, manuscript preparation, and critical revision of the paper. All the authors read and approved the final manuscript for submission.
Declaration of conflict of interest: The authors report no declaration of interest.
References
- Abbing, A., Ponstein, A., van Hooren, S. , de Sonneville, L. , Swaab, H. & Baars, E. (2018). The effectiveness of art therapy for anxiety in adults: A systematic review of randomised and non‐randomised controlled trials. PLoS One, 13, e0208716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amelia, G., Satiadarma, M.P. & Wati, L. (2020) The Effects of Drawing and Coloring Mandala on Anxiety among Pregnant Women in Their Third Trimester. In The 2nd Tarumanagara International Conference on the Applications of Social Sciences and Humanities (TICASH 2020). Atlantis Press, pp. 997–1002. [Google Scholar]
- Angellim, C., Satiadarma, M.P. & Subroto, U. (2020). Mandala drawing for reducing test anxiety in college student. In The 2nd Tarumanagara International Conference on the Applications of Social Sciences and Humanities (TICASH 2020) (pp. 451–456). Atlantis Press; [Google Scholar]
- Carsley, D., Heath, N.L. & Fajnerova, S. (2015). Effectiveness of a classroom mindfulness coloring activity for test anxiety in children. Journal of Applied School Psychology, 31, 239–255. [Google Scholar]
- Curran, L., Sharpe, L. & Butow, P. (2017). Anxiety in the context of cancer: A systematic review and development of an integrated model. Clinical Psychology Review, 56, 40–54. [DOI] [PubMed] [Google Scholar]
- Curry, N.A. & Kasser, T. (2005). Can coloring mandalas reduce anxiety? Art Therapy, 22, 81–85. [Google Scholar]
- Deng, J., Zhou, F., Hou, W.et al. (2020). The prevalence of depression, anxiety, and sleep disturbances in COVID‐19 patients: A meta‐analysis. Annals of the New York Academy of Sciences, 1486 (1), 90–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, L. & Zhu, G. (2020). Psychological interventions for people affected by the COVID‐19 epidemic. The Lancet Psychiatry, 7, 300–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong, K., Stargell, N.A. & Mauk, G.W. (2018). Effectiveness of coloring mandala designs to reduce anxiety in graduate counseling students. Journal of Creativity in Mental Health, 13, 318–330. [Google Scholar]
- Elkis‐Abuhoff, D., Gaydos, M., Goldblatt, R., Chen, M. & Rose, S. (2009). Mandala drawings as an assessment tool for women with breast cancer. The Arts in Psychotherapy, 36, 231–238. [Google Scholar]
- Epstein, D., Andrawis, W., Lipsky, A.M., Ziad, H.A. & Matan, M. (2020). Anxiety and suicidality in a hospitalized patient with COVID‐19 infection. European Journal of Case Reports in Internal Medicine, 7(5), 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flett, J.A.M., Lie, C., Riordan, B.C., Thompson, L.M., Conner, T.S. & Hayne, H. (2017). Sharpen your pencils: Preliminary evidence that adult coloring reduces depressive symptoms and anxiety. Creativity Research Journal, 29, 409–416. [Google Scholar]
- Gençdoğan, B., Çetinkaya, S.K. & Gümüş, E. (2018). Effects of coloring mandalas on test anxiety. İnönü Üniversitesi Eğitim Fakültesi Dergisi, 19, 221–229. [Google Scholar]
- Holmes, E.A., O'Connor, R.C., Perry, V.H.et al. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7 (6), 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jodaki, K., Mousavi, M.‐S., Mokhtari, R., Asayesh, H., Vandali, V. & Golitaleb, M. (2021). Effect of Rosa damascene aromatherapy on anxiety and sleep quality in cardiac patients: A randomized controlled trial. Complementary Therapies in Clinical Practice, 42, 101299. [DOI] [PubMed] [Google Scholar]
- Kim, H., Kim, S., Choe, K. & Kim, J.‐S. (2018). Effects of mandala art therapy on subjective well‐being, resilience, and hope in psychiatric inpatients. Archives of Psychiatric Nursing, 32, 167–173. [DOI] [PubMed] [Google Scholar]
- Koo, M., Chen, H.‐P. & Yeh, Y.‐C. (2020). Coloring activities for anxiety reduction and mood improvement in Taiwanese community‐dwelling older adults: A randomized controlled study. Evidence‐Based Complementary and Alternative Medicine, 200, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, S.‐L. (2018). Why color mandalas? A study of anxiety‐reducing mechanisms. Art Therapy, 35, 35–41. [Google Scholar]
- Liu, K., Chen, Y., Wu, D., Lin, R., Wang, Z. & Pan, L. (2020). Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID‐19. Complementary Therapies in Clinical Practice, 39, 101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malchiodi, C.A. (1993). Art Therapy: Journal of the American Art Therapy Association—The First 10 Years. Taylor & Francis. [Google Scholar]
- Mazza, M.G., de Lorenzo, R. , Conte, C.et al. (2020). Anxiety and depression in COVID‐19 survivors: Role of inflammatory and clinical predictors. Brain, Behavior, and Immunity, 89, 594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon, C., McDermott, P., Horsfall, D., Selvarajah, J., King, A. & Vail, A. (2007). The reproducibility of transcranial Doppler middle cerebral artery velocity measurements: implications for clinical practice. British Journal of Neurosurgery, 21, 21–27. [DOI] [PubMed] [Google Scholar]
- Nie, X.‐D., Wang, Q., Wang, M.‐N.et al. (2021). Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. International Journal of Psychiatry in Clinical Practice, 25(2), 109–114. [DOI] [PubMed] [Google Scholar]
- Noor, S.M., Saleem, T., Azmat, J. & Arouj, K. (2017). Mandala‐coloring as a therapeutic intervention for anxiety reduction in university students. Pakistan Armed Forces Medical Journal, 67, 904–907. [Google Scholar]
- Parker, C., Shalev, D., Hsu, I.et al. (2020). Depression, anxiety, and acute stress disorder among patients hospitalized with COVID‐19: A prospective cohort study. Psychosomatics, 62 (2), 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz, C., Mascialino, G., Adana‐Díaz, L.et al. (2020). Behavioral and sociodemographic predictors of anxiety and depression in patients under epidemiological surveillance for COVID‐19 in Ecuador. PLoS One, 15, e0240008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajeswari, S. & Sanjeevareddy, N. (2020). Efficacy of progressive muscle relaxation on pregnancy outcome among anxious Indian primi mothers. Iranian journal of nursing and midwifery research, 25, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roohy, G., Rahmany, A., Abdollahy, A. & Ghr, M. (2005). The effect of music on anxiety level of patients and some of physiological responses before abdominal surgery. Journal of Gorgan University of Medical Sciences, 7, 75–78. [Google Scholar]
- Roy, D., Tripathy, S., Kar, S.K., Sharma, N., Verma, S.K. & Kaushal, V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID‐19 pandemic. Asian Journal of Psychiatry, 51, 102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar, L. R. (2019). Exploring the effect of coloring mandalas on students’ math anxiety in business statistics courses. Business, Management and Education, 17, 134–151. [Google Scholar]
- Sun, N., Wei, L., Wang, H.et al. (2021). Qualitative study of the psychological experience of COVID‐19 patients during hospitalization. Journal of Affective Disorders, 278, 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K., Bhullar, N., Durkin, J., Gyamfi, N. & Jackson, D. (2020a). Family violence and COVID‐19: Increased vulnerability and reduced options for support. Wiley Online Library. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K., Durkin, J. & Bhullar, N. (2020b). The COVID‐19 pandemic and mental health impacts. International Journal of Mental Health Nursing, 29, 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K., Jackson, D., Durkin, J., Gyamfi, N. & Bhullar, N. (2020c). Pandemic‐related behaviours and psychological outcomes; A rapid literature review to explain COVID‐19 behaviours. International Journal of Mental Health Nursing, 29, 1018–1034. [DOI] [PubMed] [Google Scholar]
- Yakar, H.K., Yilmaz, B., Ozkol, O., Gevher, F. & Celik, E. (2021). Effects of art‐based mandala intervention on distress and anxiety in cancer patients. Complementary Therapies in Clinical Practice, 43, 101331. [DOI] [PubMed] [Google Scholar]
- Zandifar, A., Badrfam, R., Yazdani, S.et al. (2020). Prevalence and severity of depression, anxiety, stress and perceived stress in hospitalized patients with COVID‐19. Journal of Diabetes & Metabolic Disorders, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, X. (2020). Psychological crisis interventions in Sichuan Province during the 2019 novel coronavirus outbreak. Psychiatry Research, 286, 112895. [DOI] [PMC free article] [PubMed] [Google Scholar]


