Abstract
Objectives
The aim of this study was to assess acceptance of COVID‐19 vaccination and the willingness to pay (WTP) for it, and investigate associated factors among pregnant women in Vietnam.
Methods
Cross‐sectional survey of pregnant women in two obstetric hospitals in Hanoi and Ca Mau provinces, Vietnam. Data on acceptance and WTP for COVID‐19, demographic characteristics, maternal characteristics, and risk perceptions toward COVID‐19 were collected. Multivariate logistic and linear regression models were performed to identify factors associated with the acceptance and WTP for the vaccine.
Results
Of 651 pregnant women, 60.4% accepted to receive the vaccine, and 82.6% of the total pregnant women were willing to pay for a COVID‐19 vaccine with the mean amount of WTP of USD 15.2 (SD ± 27.4). The most common reason for refusing vaccination was “Worry about the safety of the vaccine” (66.9%) in Hanoi and “The preventive effect of COVID‐19 is low” (45.2%) in Ca Mau. A higher income, having children, self‐perceived risk of COVID‐19 infection, and perceived risk to friends were associated with a higher likelihood of acceptance and WTP for the vaccine.
Conclusions
Implementing COVID‐19 vaccination and resource mobilisation among pregnant women in Vietnam is feasible, although communication programmes to improve risk perception and awareness about vaccine should be developed for facilitating acceptance of the vaccine.
Keywords: acceptance, COVID‐19, pregnant women, vaccine, willingness to pay
INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is a global threat and has been crippling health systems worldwide. As of 11 July 2021, the cumulative number of confirmed cases had reached approximately 185 million, with more than 3.08 million deaths, and the majority of health care services globally have been disrupted due to COVID‐19 [1, 2, 3]. Pregnant women are among vulnerable populations to the current pandemic given the associations with a higher rate of hospitalisations, mechanical ventilation, and death [4, 5, 6, 7]. Disruptions of essential health services for women and children, including reproductive, maternal, newborn services due to the COVID‐19 pandemic, are increasingly threatening the health of pregnant women [3, 8].
In the worldwide response to the pandemic, over 5000 clinical trials to examine drug interventions’ safety and efficacy have been registered [9]. Yet, no specific therapeutics have been found to be highly effective in the treatment of COVID‐19 [2]; thus, developing vaccines against COVID‐19 has been accelerated to mitigate the pandemic. As of 18 February 2021, at least seven vaccines had been officially launched for limited use in several countries, and over 60 vaccine candidates were undergoing clinical trials [10]. Successful universal vaccination is expected to pave the way to ending COVID‐19 if vaccine uptake is sufficient and variants are not too problematic. Thus, hesitancy in receiving the vaccines is a significant challenge in combating the pandemic. Vaccination strategies need to address issues regarding vaccine acceptance and affordability to reach high coverage. It is crucial to examine acceptance and willingness to pay (WTP) for COVID‐19 vaccines as well as their associated determinants among different population groups. Assessment of acceptance and WTP for COVID‐19 vaccines benefits organisations and pharmaceutical manufacturers in determining the potential market and pricing strategy for vaccines. Moreover, this evidence assists health care decision‐makers in formulating optimal allocation and payment strategies among various groups.
Globally, pregnant women have not been listed in recommended groups for receiving the first supply of COVID‐19 vaccines [2, 11]; primarily because pregnant and lactating women were excluded from clinical trials for COVID‐19 vaccines. Thus, the safety and efficacy of the vaccines for this population and their foetuses remain unknown [12, 13]. However, recent preliminary evidence shows that immunity has been equivalently produced between pregnant and lactating women [13], and antibodies could be passed to the newborn when the mother got the vaccine before birth [14], suggesting that pregnant women are eligible for the vaccination. Currently, getting vaccinated for COVID‐19 is a personal choice of pregnant women according to their preferences and their consideration of the benefits and drawbacks of receiving vaccines. A systematic review showed that among pregnant individuals, vaccine uptake was influenced by healthcare professional recommendation, safety and efficacy of vaccines, perceptions of vaccine utility, and the belief in the risk of infection [15].
Studies on acceptance and WTP for COVID‐19 vaccines have been scarce, and most of them have been conducted in the general population with hypothetical COVID‐19 vaccines [16, 17, 18, 19]. Three previous nationwide online studies in China showed a high demand for hypothetical COVID‐19 vaccination of the general Chinese population with the amount willing to pay ranging from USD 28 to USD 149 [20, 21, 22]. In South America, WTP for vaccines in Chile and Ecuador was USD 184.72 and ranged from USD 76.9 to USD 102.5 respectively [23, 24]. A study in Indonesia reported a high rate of WTP for the COVID‐19 vaccine, with a mean WTP of USD 57.2 [16], while in Malaysia the mean WTP for COVID‐19 vaccine was USD 30.66 per dose [19]. However, evidence on the acceptance and WTP for COVID‐19 vaccine in pregnant women is insufficient, implying the need for further study to fulfil this knowledge gap.
As of 11 July 2021, Vietnam had undergone four waves of COVID‐19 pandemic with 28,470 confirmed cases and 105 deaths recorded among approximately 96.5 million people [25]. Although Vietnam has successfully implemented COVID‐19 prevention measures such as social distancing, contact tracing and face mask‐wearing in the first three waves, these measures seem to be insufficient as the rate of infection in the community is increasing rapidly. During the fourth wave of the pandemic, the number of infections in Vietnam has been accelerating with 24,932 cases (87.6% of total cases) since 27 April 2021 due to the Delta variant [25]. So far, the Vietnamese healthcare system has not yet witnessed an acute shortage of hospital beds, healthcare staff, and other medical equipment [26]; however, with a significant increase in the number of cases, and if mass vaccination is not implemented to achieve herd immunity soon, Vietnam's health system may face collapse. The pandemic negatively affects people's lives and income, which may impact on demand for and affordability of COVID‐19 vaccines [27]. Accelerating vaccination has become the top priority of the Vietnam Government to return to a “new normal life”.
Vietnam initiated a vaccination campaign with imported vaccines on 8 March 2021. Two other COVID‐19 vaccines developed by domestic manufacturers are undergoing phase II clinical trials and are expected to be introduced in late 2021 or early 2022. However, vaccine supply remains a roadblock to Vietnam's national free vaccination programme. In anticipation of a shortage amidst the pandemic, the Vietnamese government issued Resolution 21/NQ‐CP, identifying eleven groups of individuals that will be prioritised for the free vaccines. At first, vaccine is administered freely to frontline health workers, the elderly, and those at high risk of exposure to COVID‐19. Vietnamese pregnant women are not prioritised to get vaccines at this phase. Due to insufficient financing sources and fiscal capacity, the Vietnamese government may be unable to fully subsidise vaccines for all populations in the long run. Therefore, in addition to providing free vaccines, the Government has proposed to deploy on‐demand vaccination services to mobilise financial resources from the community [28]. Understanding the demand of different sub‐populations, including pregnant women, is important to propose financial mechanisms and vaccination strategies to increase vaccination coverage. Our study was conducted to assess the acceptance of COVID‐19 vaccination and WTP for it among pregnant women in Vietnam. We also aimed to investigate factors associated with acceptance and WTP for COVID‐19 vaccines since they are vital for manufacturers, organisations, and the government to effectively design vaccination programmes and pricing strategies for this vulnerable population.
METHODS
Study setting and participants
This was a cross‐sectional study on pregnant women from January to February 2021, at Hanoi Obstetrics & Gynecology Hospital, a central hospital located in the north of Vietnam, and Ca Mau Obstetrics & Pediatrics, a provincial hospital in the south of Vietnam. When potential participants visited the hospitals, well‐trained researchers approached pregnant women, briefly informed them about the study, and requested participation. Eligibility criteria for participating were: (1) aged over 18 years; (2) being pregnant or had just given birth; (3) providing written informed consent to participate. Twenty‐four pregnant women were excluded from the recruitment process; they suffered from serious illnesses or could not answer the questionnaire (for instance, inability to read/write or having a cognitive impairment which might influence the ability for responding to questions). At the end of the data collection period, a total of 651 pregnant women had taken part. The protocol of this study was approved by the Ethical Review Board of Hanoi Obstetrics & Gynecology Hospital on 6 January 2021 (Code: 07 QĐ/PS‐TTĐT CĐT).
Measurement and instrument
An online questionnaire on SurveyMonkey's platform was designed since it was time‐saving, and no resources for data entry were needed. The survey link was sent to participants by the research team, and the participants answered the questionnaire via their smartphones or tablets. The researchers stayed in the same room with participants to answer their questions or clarify unclear terminology. The survey had four components: (1) socio‐demographic information; (2) maternal characteristics; (3) affected by COVID‐19 pandemic; (4) willingness to receive and pay for COVID vaccine.
Outcome variables
The primary outcomes were the acceptance to receive the COVID‐19 vaccine, willingness to pay for the vaccine and the amount of money participants were willing to pay (hereby we named it “amount of WTP”). To measure the outcomes, we asked them the following questions: “Do you want to get a COVID‐19 vaccine?” and “Are you willing to pay for a COVID‐19 vaccine for yourself and your household members?” We asked this question because pregnant women might perceive that they were not eligible for the vaccination but they were willing to pay for other family members to be vaccinated. Those who answered “No” were asked to provide their reasons. Meanwhile, pregnant women answering “Yes” were then asked the amount of money they would be willing to pay for the COVID vaccination by asking “How much do you want to pay for a COVID vaccination?”. The price was converted to USD (USD 1 ~ VND 23.000).
Predictor variables
Demographic information
Social‐demographic characteristics included in this study were: age; monthly household income; living area (urban, rural/mountain); education (high school and below, college, university/postgraduate); occupation (white‐collar, blue‐collar/farmer, unemployment, others); living arrangements (parents, parents in law, partner/children); health insurance status (none, social health insurance, private health insurance, both types). People reported their living areas based on the administrative classification of the Vietnamese Government.
Maternal characteristics
Participants were asked to report the number of children in their family, number of pregnancies, number of comorbidities (e.g. diabetes, hypertension, or other diseases which pregnant women suffered from during the pregnancy), and ever having any complications in the period of pregnancy.
Effect of COVID‐19 epidemic during antenatal care
Fear of COVID‐19 scale (FCV‐19S) was used to assess pregnant women's fear of COVID‐19. Participants indicated their level of agreement with seven questions using a five‐point Likert scale with 1 = “Strongly disagree”, 2 = “Disagree”, 3 = “Neutral”, 4 = “Agree” and 5 = “Strongly agree”. The scores were calculated by summing scores of all items, and the total score ranged from 7 to 35 with a higher score corresponding to a higher level of fear of COVID‐19 [29]. Cronbach's alpha of this instrument in this study was 0.87. Participants also rated the risk of COVID‐19 acquisition for themselves, their husband/partner, family members, friends, and colleagues by answering the question “How would you rate your risk of COVID‐19?” or “How would you rate your husband/family members’/friends/colleagues’ risk of COVID‐19?” The response options ranged from 0 = “No risk”, 1 = “Low risk”, 2 = “High risk”, 3 = “Very high risk”, 4 = “Unknow” and 5 = “Not apply”. Participants also reported the effect of COVID‐19 during antenatal care and childbirth (i.e. Childbirth before the COVID 19/Childbirth during COVID 19 but not being affected/being affected by COVID 19).
Data analysis
STATA version 16.0 was used to analyse the data. Chi‐squared (χ 2), Fisher's exact and Mann‐Whitney tests were performed to examine the differences in acceptance of, WTP and maximum amount WTP for COVID‐19 vaccine according to socio‐demographic and maternal characteristics and perceived risk of COVID‐19.
Multivariate logistic regression models were conducted to assess factors associated with acceptance (Yes = 1/No = 0, model 1) and willingness to pay (Yes = 1/No = 0, model 2) for the COVID‐19 vaccine. Regarding the maximum amount of WTP for the COVID‐19, due to its non‐normal distribution, the data were transformed into logarithmic form. Factors associated with the amount they were WTP for COVID‐19 vaccine were identified by using the multivariate linear regression model in Model 3. Independent variables for three models included social‐demographic characteristics (age, monthly household income, living area, education, occupation, person living with and health insurance status), maternal characteristic (number of children in their family, number of pregnancies, number of comorbidities, maternity problems), effect of epidemic COVID‐19 during antenatal care (fear of COVID‐19, risk of COVID‐19). Variance Inflation Factor (VIF) analysis was performed to examine collinearity of the independent variables, with a value of 10 being considered the threshold. In this study, we did not find any VIF values exceeding 10, suggesting no collinearity in our models. Forward stepwise selection strategies with a p‐value below 0.2 of the log‐likelihood tests had been used with the regression models to produce the adjusted models. A p‐value below 0.05 was considered statistically significant.
RESULTS
Respondent's characteristics
Among 651 respondents, the majority were living in the urban area (66.4%) and living with husband and children (61.8%). Their mean age was 29.4 years (SD = 5.0). 44.4% held a bachelor's degree or above and 47.2% were white‐collar. A total of 67.8% of respondents had social health insurance. The average monthly household income was USD 662.6 (SD = 530.5). The monthly household income of individuals in Hanoi was USD 787.1 (SD = 560.9), while the monthly household income of women in Ca Mau was USD 296.2 (SD = 75.3). The difference was statistically significant (p < 0.05).
Respondents’ acceptance to and willingness to pay for COVID‐19 vaccine
Significant differences in willingness to receive COVID vaccine were observed between respondents in Hanoi and Ca Mau (p < 0.01), whereby 67.8% (95% CI = 63.2%–71.6%) of women in Hanoi were willing to get the vaccine, whereas in Ca Mau only 39.9% (95% CI = 32.8%–47.4%) were. The majority of respondents (82.6%, 95% CI = 79.5%–85.4%) were willing to pay for the COVID vaccine with a mean amount of WTP of USD 15.2 (SD = 27.4, 95% CI = 13.1–17.3); however, there were notable differences in WTP for the vaccine between Hanoi (mean = 16.2 ± 31.5 USD, 95% CI = 13.3–19.0) and Ca Mau (mean = 12.4 ± 8.5 USD, 95% CI = 11.1–13.7; p < 0.01) (Table 1). Figure 1 illustrates the cumulative percentage of women's willingness to pay for COVID vaccine. Less than 35% and 50% of participants were willing to pay 15.2 USD and 4.5 USD for the vaccine respectively.
TABLE 1.
Acceptance and willingness to pay for COVID‐19 vaccine regarding study sites
| Characteristics | Hanoi (n = 478) | Ca Mau (n = 173) | Total (n = 651) | p‐Value | |||
|---|---|---|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | n (%) | 95% CI | ||
| Acceptance to COVID‐19 vaccine | |||||||
| Yes | 324 (67.8) | 63.2–71.6 | 69 (39.9) | 32.8–47.4 | 393 (60.4) | 56.5–64.1 | <0.001 |
| No | 154 (32.2) | 28.4–36.8 | 104 (60.1) | 52.6–67.2 | 258 (39.6) | 35.9–43.5 | |
| Willingness to pay for COVID‐19 vaccine | |||||||
| Yes | 385 (80.5) | 77.0–84.1 | 153 (88.4) | 82.7–92.4 | 538 (82.6) | 79.5–85.4 | 0.019 |
| No | 93 (19.5) | 15.9–23.0 | 20 (11.6) | 7.6–17.3 | 113 (17.4) | 14.6–20.5 | |
| Amount of willingness to pay | |||||||
| Mean (US$) | 16.2 | 13.3–19.0 | 12.4 | 11.1–13.7 | 15.2 | 13.1–17.3 | <0.001 |
| SD | 31.5 | 8.5 | 27.4 | ||||
| Median (US$) | 1.5 | 8.7 | 4.3 | ||||
| 25th quartile (US$) | 0.04 | 6.5 | 0.04 | ||||
| 75th quartile (US$) | 21.7 | 21.7 | 21.7 | ||||
FIGURE 1.
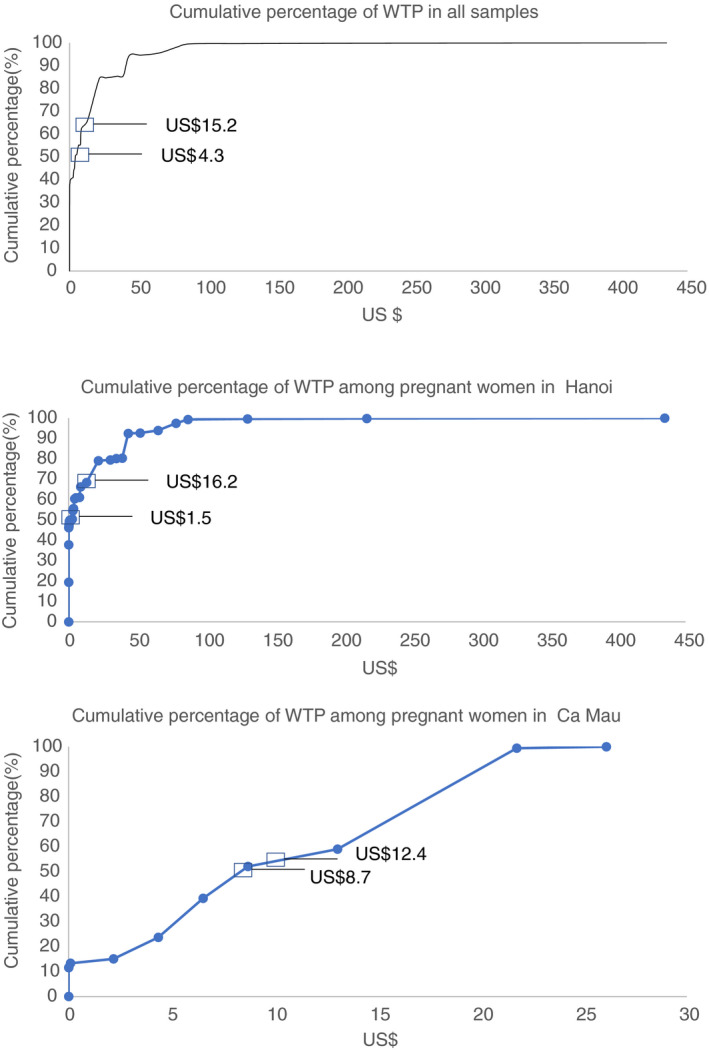
Cumulative percentage of women's willingness to pay for COVID vaccine according to study sites
Figure 2 shows the reason for unwillingness to pay and to receive the COVID‐19 vaccine. In terms of unwillingness to receive the vaccine, the most common reason among respondents in Hanoi was “Worry about safety of the vaccine” (66.9%, 95% CI = 58.9%–74.2%), while in Ca Mau, the most common reason was “The preventive effect of COVID‐19 is low” (45.2%, 95% CI = 35.4%–55.3%). The most common reason for not being willing to pay for the vaccine was “The COVID‐19 vaccine should be provided freely” in both study sites with 59.1% (95% CI = 48.5%–69.2%) in Hanoi and 90.0% (95% CI = 68.3%–98.8%) in Ca Mau (p < 0.05).
FIGURE 2.
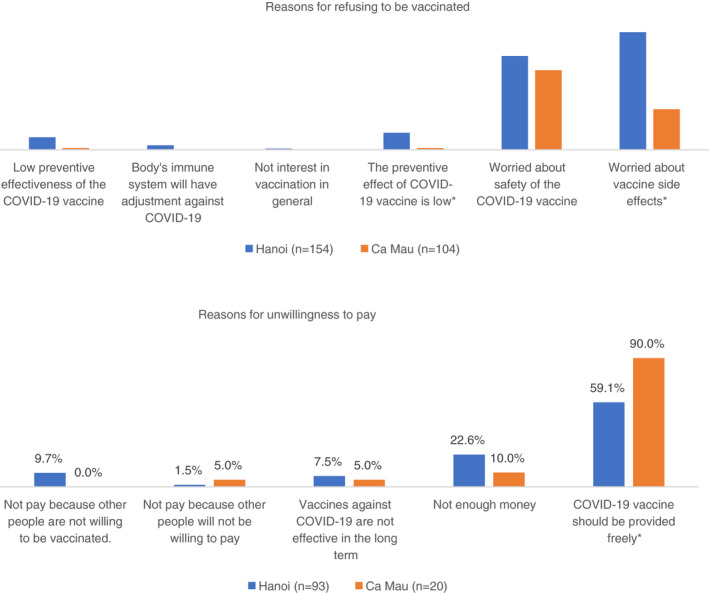
Bivariate analysis in reasons refusing to pay for and receive COVID‐19 vaccine by study sites. Note: *p < 0.05
Associated factors with acceptance to and willingness to pay for COVID‐19 vaccine
Regarding acceptance, pregnant women living in rural/mountainous areas (48.4%), those with high school education or below (51.6%), and those with private health insurance (31.5%) were more likely to refuse vaccination (p < 0.01, Table 2). White‐collar workers were more likely to accept to be immunised (67.1%) and pay for the vaccine (87.3%) than other groups. Pregnant women living with husband and children were less likely to be willing to pay (92.2%) for the vaccine (p < 0.1). Those willing to be vaccinated and pay for it had significantly higher monthly household income than those not willing be vaccinated and to pay (p < 0.01).
TABLE 2.
Acceptance and willingness to pay for COVID‐19 vaccine regarding sociodemographic characteristics
| Characteristics | Total | Acceptance of vaccination | Willingness to pay for vaccine | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | OR (95% CI) | Yes | No | OR (95% CI) | ||
| n (%) | n (%) | n (%) | n (%) | ||||
| Total | 651 | 393 (60.4) | 258 (39.6) | 538 (82.6) | 113 (17.4) | ||
| Living location | |||||||
| Urban | 432 | 287 (66.4) | 145 (33.6) | 1 | 358 (82.9) | 74 (17.1) | 1 |
| Rural/mountain | 219 | 106 (48.4) | 113 (51.6) | 0.47* (0.34–0.66) | 180 (82.2) | 39 (17.8) | 0.95 (0.62–1.46) |
| Education | |||||||
| High school and below | 246 | 127 (51.6) | 119 (48.4) | 1 | 198 (80.5) | 48 (19.5) | 1 |
| College | 115 | 78 (67.8) | 37 (32.2) | 1.98* (1.24–3.14) | 92 (80.0) | 23 (20.0) | 0.97 (0.56–1.69) |
| University or above | 288 | 188 (65.3) | 100 (34.7) | 1.76* (1.24–2.50) | 246 (85.4) | 42 (14.6) | 1.42 (0.90–2.24) |
| Occupation | |||||||
| White‐collar | 307 | 206 (67.1) | 101 (32.9) | 1 | 268 (87.3) | 39 (12.7) | 1 |
| Blue‐collar/farmer | 87 | 45 (51.7) | 42 (48.3) | 0.53* (0.32–0.85) | 65 (74.7) | 22 (25.3) | 0.43* (0.24–0.77) |
| Unemployment | 173 | 92 (53.2) | 81 (46.8) | 0.56* (0.38–0.82) | 142 (82.1) | 31 (17.9) | 0.67 (0.40–1.11) |
| Others | 84 | 50 (59.5) | 34 (40.5) | 0.74 (0.45–1.21) | 63 (75.0) | 21 (25.0) | 0.42* (0.23–0.75) |
| Living with parents | |||||||
| No | 598 | 365 (61.0) | 233 (39.0) | 1 | 490 (81.9) | 108 (18.1) | 1 |
| Yes | 51 | 28 (54.9) | 23 (45.1) | 0.78 (0.44–1.38) | 47 (92.2) | 4 (7.8) | 2.59 (0.91–7.34) |
| Living with parents in law | |||||||
| No | 386 | 240 (62.2) | 146 (37.8) | 1 | 314 (81.4) | 72 (18.7) | 1 |
| Yes | 263 | 153 (38.9) | 110 (43.0) | 0.85 (0.61–1.17) | 223 (84.8) | 40 (15.2) | 1.28 (0.84–1.95) |
| Living with husband and/or children | |||||||
| No | 248 | 144 (58.1) | 104 (41.9) | 1 | 219 (88.3) | 29 (11.7) | 1 |
| Yes | 401 | 249 (62.1) | 152 (37.9) | 1.18 (0.86–1.63) | 318 (79.3) | 83 (20.7) | 0.51 (0.32–0.80) |
| Health insurance | |||||||
| Do not have | 24 | 17 (70.8) | 7 (29.2) | 1 | 20 (83.3) | 4 (16.7) | 1 |
| Social health insurance | 385 | 264 (68.6) | 121 (31.4) | 0.90 (0.36–2.22) | 313 (81.3) | 72 (18.7) | 0.87 (0.29–2.62) |
| Private health insurance | 127 | 40 (31.5) | 87 (68.5) | 0.19* (0.07–0.49) | 115 (90.6) | 12 (9.4) | 1.92 (0.56–6.54) |
| Both types | 32 | 20 (62.5) | 12 (37.5) | 0.69 (0.22–2.13) | 27 (84.4) | 5 (15.6) | 1.08 (0.26–4.54) |
| Mean (SD) | Mean (SD) | p‐Value | Mean (SD) | Mean (SD) | p‐Value | ||
| Age (unit: year) | 651 | 29.3 (4.9) | 29.6 (5.3) | 0.99 (0.96–1.02) | 29.3 (5.0) | 29.6 (5.4) | 0.99 (0.95–1.03) |
| Monthly household income (unit: hundred USD) | 651 | 7.0 (5.4) | 6.0 (5.0) | 1.04* (1.00–1.07) | 6.8 (5.5) | 5.6 (4.2) | 1.06* (1.01–1.12) |
p < 0.05.
Table 3 shows that multiparous women were more likely to be willing to pay for the vaccine (p < 0.05). Otherwise, the differences in acceptance and willingness to pay for COVID‐19 were not significant across groups (p > 0.05).
TABLE 3.
Acceptance and willingness to pay for COVID‐19 vaccine regarding maternal characteristics
| Characteristics | Total | Acceptance of vaccination | Willingness to pay | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | OR (95% CI) | Yes | No | OR (95% CI) | ||
| n (%) | n (%) | n (%) | n (%) | ||||
| Number of children in the family | |||||||
| None | 164 | 99 (60.4) | 65 (39.6) | 1 | 137 (83.5) | 27 (16.5) | 1 |
| One child | 290 | 163 (56.2) | 127 (43.8) | 0.84 (0.57–1.24) | 244 (84.1) | 46 (15.9) | 1.05 (0.62–1.76) |
| Two children or more | 191 | 128 (67.0) | 63 (33.0) | 1.33 (0.86–2.06) | 152 (79.6) | 39 (20.4) | 0.77 (0.45–1.32) |
| Number of pregnancies | |||||||
| Once | 272 | 159 (58.5) | 113 (41.5) | 1 | 236 (86.8) | 36 (13.2) | 1 |
| Twice | 268 | 156 (58.2) | 112 (41.8) | 0.99 (0.70–1.39) | 218 (81.3) | 50 (18.9) | 0.67 (0.42–1.06) |
| Three times and more | 106 | 73 (68.9) | 33 (31.1) | 1.57 (0.98–2.53) | 80 (75.5) | 26 (24.5) | 0.47* (0.27–0.83) |
| Ever having complications of pregnancy | |||||||
| No | 498 | 294 (59.0) | 204 (41.0) | 1 | 412 (82.7) | 86 (17.3) | 1 |
| Yes | 149 | 96 (64.4) | 53 (35.6) | 1.26 (0.86–1.84) | 123 (82.6) | 26 (17.5) | 0.99 (0.61–1.60) |
| Number of comorbidities | |||||||
| None | 415 | 241 (58.1) | 174 (41.9) | 1 | 347 (83.6) | 68 (16.4) | 1 |
| One comorbidity | 138 | 90 (265.2) | 48 (34.8) | 1.35 (0.91–2.02) | 115 (83.3) | 23 (16.7) | 0.98 (0.58–1.64) |
| Two comorbidities or more | 60 | 37 (61.7) | 23 (38.3) | 1.16 (0.67–2.02) | 51 (85.0) | 9 (15.0) | 1.11 (0.52–2.36) |
p<0.05.
Table 4 depicts that acceptance and willingness to pay for COVID‐19 vaccine were not related to the influence of COVID‐19 during antenatal care (p > 0.05). However, the proportion of women accepting to be vaccinated was higher in those rating that self, husband/partner, family members, friends and colleagues were at risk of COVID‐19 infection than in women perceiving no risk (p < 0.01). The percentage of pregnant women being willing to pay for the vaccine were also significantly higher among those rating friends and colleagues at risk of COVID‐19 infection than those perceiving no risk (p < 0.05). Women who were not willing to pay had significantly higher fear of COVID‐19 score than those who were willing to pay (p < 0.05).
TABLE 4.
Acceptance and willingness to pay for COVID‐19 vaccine regarding COVID‐19 related characteristics
| Characteristics | Total | Acceptance of vaccination | Willingness to pay | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | OR (95% CI) | Yes | No | OR (95% CI) | ||
| n (%) | n (%) | n (%) | n (%) | ||||
| Being affected by COVID‐19 during antenatal care | |||||||
| Childbirth before the COVID 19 | 57 | 29 (50.9) | 28 (49.1) | 1 | 48 (84.2) | 9 (15.8) | 1 |
| Childbirth during COVID 19 but not being affected | 523 | 316 (60.4) | 207 (39.6) | 1.47 (0.85–2.55) | 434 (83.0) | 89 (17.0) | 0.91 (0.43–1.93) |
| Being affected by COVID 19 | 66 | 45 (68.2) | 21 (31.8) | 2.11* (1.02–4.40) | 51 (77.3) | 15 (22.7) | 0.60 (0.24–1.48) |
| Self‐perceived risk of COVID‐19 | |||||||
| No | 259 | 120 (46.3) | 139 (53.7) | 1 | 215 (83.0) | 44 (17.0) | 1 |
| Unknown | 75 | 51 (68.0) | 24 (32.0) | 2.44* (1.42–4.20) | 59 (78.7) | 16 (21.3) | 0.77 (0.41–1.46) |
| Yes | 316 | 222 (70.3) | 94 (29.7) | 2.71* (1.93–3.82) | 264 (83.5) | 52 (16.5) | 1.06 (0.69–1.65) |
| Risk of husband in COVID‐19 acquisition | |||||||
| No | 247 | 113 (45.8) | 134 (54.2) | 1 | 210 (85.0) | 37 (15.0) | 1 |
| Unknown | 63 | 40 (63.5) | 23 (36.5) | 2.04* (1.16–3.62) | 47 (74.6) | 16 (25.4) | 0.53 (0.27–1.03) |
| Yes | 338 | 239 (61.0) | 99 (38.7) | 2.84* (2.01–4.00) | 280 (82.8) | 58 (17.2) | 0.87 (0.56–1.37) |
| Risk of family members in COVID‐19 acquisition | |||||||
| No | 247 | 113 (45.8) | 134 (54.3) | 1 | 208 (84.2) | 39 (15.8) | 1 |
| Unknown | 65 | 43 (66.2) | 22 (33.9) | 2.30* (1.30–4.07) | 50 (76.9) | 15 (23.1) | 0.64 (0.33–1.25) |
| Yes | 337 | 237 (70.3) | 100 (29.7) | 2.79* (1.98–3.92) | 280 (83.1) | 57 (16.9) | 0.94 (0.61–1.47) |
| Risk of friends in COVID‐19 acquisition | |||||||
| No | 126 | 36 (28.6) | 90 (71.4) | 1 | 112 (88.9) | 14 (11.1) | 1 |
| Unknown | 189 | 119 (63.0) | 70 (37.0) | 4.14* (2.55–6.71) | 147 (77.8) | 42 (22.2) | 0.47* (0.25–0.89) |
| Yes | 334 | 237 (71.0) | 97 (29.0) | 5.94* (3.79–9.32) | 278 (83.2) | 56 (16.7) | 0.66 (0.36–1.22) |
| Risk of colleagues in COVID‐19 acquisition | |||||||
| No | 133 | 42 (31.6) | 91 (68.4) | 1 | 118 (88.7) | 15 (11.3) | 1 |
| Unknown | 188 | 118 (62.8) | 70 (37.2) | 3.57* (2.23–5.70) | 145 (77.1) | 43 (22.9) | 0.46* (0.25–0.85) |
| Yes | 327 | 231 (70.6) | 96 (29.4) | 5.09* (3.30–7.86) | 273 (83.5) | 54 (16.5) | 0.69 (0.38–1.25) |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Fear of COVID‐19 | 651 | 21.2 (4.5) | 21.1 (4.0) | 1.00 (0.97–1.04) | 21.0 (4.2) | 21.9 (4.6) | 0.95 (0.91–1.00) |
p < 0.05.
Results of Multivariate logistic regression for acceptance of vaccination and WTP for COVID‐19, and Multivariate linear regression for the log of the amount of WTP are presented in Table 5. Living in Ca Mau province [Odds ratio (OR) = 0.32, 95% CI = (0.15; 0.69)], living with husband and children [OR = 0.5, 95% CI = (0.28; 0.9)], and having private health insurance [OR = 0.46, 95% CI = (0.26; 0.82)] were negatively associated with the willingness to receive the vaccine. Meanwhile, respondents’ friends have risk of COVID‐19 [OR = 2.85, 95% CI = (1.6; 5.07)] were positively associated with the willingness to receive.
TABLE 5.
Results of multivariate logistic regression for acceptance of vaccination and WTP for COVID‐19, and Multivariate linear regression for the log of the amount of WTP
| Characteristics | Acceptance of vaccination | WTP for COVID‐19 vaccine | Log of the amount of WTP | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | Coef. | 95% CI | |
| Individual characteristic | ||||||
| Province (Ca Mau vs. Hanoi‐ref) | 0.32** | 0.15; 0.69 | 11.88** | 2.57; 54.91 | 1.28** | 0.45; 2.11 |
| Occupation (vs. white‐collar‐ref) | ||||||
| Blue‐collar/farmer | 0.30** | 0.14; 0.65 | ||||
| Others | 0.41* | 0.21; 0.81 | ||||
| Living with | ||||||
| Parents in law (yes vs. no‐ref) | 0.67 | 0.39; 1.15 | ||||
| Husband and/or children (yes vs. no‐ref) | 0.50* | 0.28; 0.90 | 0.52* | 0.28; 0.95 | ||
| Monthly income (hundred USD) | 1.09* | 1.02; 1.16 | ||||
| Health insurance (vs. none) | ||||||
| Private health insurance | 0.46** | 0.26; 0.82 | ||||
| Both 2 types | 0.51 | 0.22; 1.19 | 0.95 | −0.21; 2.12 | ||
| Maternal characteristics | ||||||
| Number of children in the family (vs. none) | ||||||
| One child | 0.67 | 0.44; 1.01 | 1.83* | 1.02; 3.30 | 0.57* | 0.06; 1.08 |
| Ever having complications (yes vs. no‐ref) | 0.57 | −0.02; 1.15 | ||||
| Number of pregnancies (vs. once) | ||||||
| Twice | 0.62 | 0.35; 1.09 | ||||
| Number of comorbidities (vs. none) | ||||||
| One comorbidity | 0.43 | −0.16; 1.02 | ||||
| COVID 19 pandemic | ||||||
| Fear of COVID‐19 (per score) | −0.10** | −0.16; −0.04 | ||||
| Risk of COVID 19 | ||||||
| Self‐perceived risk of COVID‐19 (vs. no risk) | ||||||
| Have risk | 3.17* | 1.23; 8.16 | ||||
| Husband/partner had risk of COVID‐19 (vs. no) | ||||||
| Yes | 0.40 | 0.15; 1.10 | ||||
| Friends had risk of COVID‐19 (vs. no) | ||||||
| Unknown | 3.38** | 1.72; 6.66 | 1.10* | 0.26; 1.94 | ||
| Yes | 2.85** | 1.60; 5.07 | 1.57* | 0.04; 3.09 | ||
| Colleagues had risk of COVID 19 (vs. no) | ||||||
| Yes | −1.44* | −2.84; −0.05 | ||||
| Pseudo‐R2/adjusted R2 | 0.1387 | 0.1211 | 0.0889 | |||
| Akaike information criterion (AIC) | 572.03 | 376.68 | 1935.13 | |||
| Bayesian information criterion (BIC) | 613.76 | 418.41 | 1975.24 | |||
p < 0.01
p < 0.05.
Regarding factors associated with WTP, living in Ca Mau province [OR = 11.88, 95% CI = (2.57; 54.91)], having a child [OR = 1.83, 95% CI = (1.02; 3.3)] and perceiving themselves to be at higher risk of having COVID‐19 [OR = 3.17, 95% CI = (1.23; 8.16)] or higher monthly household income [OR = 1.09, 95% CI = (1.02; 1.16)] were positively associated with WTP for COVID‐19 vaccine. Blue‐collar workers/Farmers or other occupations were less willing to pay for vaccine than white‐collar workers by a factor of 0.30–0.41.
Regarding the maximum amount of WTP, respondents living in Ca Mau [Coefficient (Coef.) = 1.28, 95% CI = (0.45; 2.11)] were willing to pay 128% more for the vaccine than those in Hanoi. Having a child [Coef. = 0.57, 95% CI = (0.06; 1.08)] or friends at risk of COVID‐19 [Coef. = 1.57, 95% CI = (0.04; 3.09)] were also positively related to the amount of WTP. Participants who were more fearful of COVID‐19 than the mean will pay 1% less for the vaccine [Coef. = −0.10, 95% CI = (−0.16; −0.04)]; and those whose colleagues were not at risk of COVID‐19 were willing to pay less for the vaccine than those whose colleagues were at risk [Coef. = −1.44, 95% CI = (−2.84; −0.05)] (Table 5).
DISCUSSION
This study highlights a high acceptance rate, a significant percentage of pregnant women WTP and at a moderate price for the COVID‐19 vaccine. Moreover, our regression models indicated factors associated with acceptance of the COVID‐19 vaccine, WTP and amount of WTP for the vaccine with respect to socioeconomic characteristics, history of maternity care, perceived fear and risk of having COVID‐19. Our results might contribute as a reliable source for pricing strategy and planning vaccination programme purposes.
We found that 60.4% of respondents were willing to receive the COVID‐19 vaccine; that percentage might reach the herd immunity threshold based on the transmissibility of COVID‐19 [16]. This finding was relatively similar to the willingness to obtain influenza vaccination among Vietnamese women of reproductive age (64.3%) [30]. However, compared to previous studies on acceptance of the COVID‐19 vaccine, our finding was lower than those of general population‐based studies in Indonesia (from 67% to 93.3% according to different COVID‐19 vaccine effectiveness scenarios) [31], China (77.4%) [21] and Ecuador (97%) [24]. There are two possible explanations for these discrepancies. First, within the context of Vietnam, strict adherence to precautions effectively mitigates virus transmission, leading to a moderate impact of the pandemic on the Vietnamese people's health and health system [26, 32]. Vaccination to end the pandemic in Vietnam might not be expected as much as in countries that are hard‐hit by the pandemic such as Indonesia, China and Ecuador. Second, safety and efficacy of the available vaccines were less certain for pregnant women than the general population since clinical trials of available COVID‐19 vaccines excluded this vulnerable group [12]. Indeed, our data also disclosed primary reasons for unwillingness to receive COVID‐19 vaccines among our respondents were concerns about the side effects and the safety of COVID‐19 vaccines.
The vast majority of respondents were willing to pay for the COVID‐19 vaccine (82.6%) with a mean WTP of USD 15.2 per dose or USD 30.3 for a two‐dose regime. That amount was over 1.7 times higher than the mean WTP for flu vaccine among Vietnamese women of childbearing age (USD 8.5) [30], reflecting a greater perceived benefit of health gained from preventing COVID‐19 than seasonal flu. However, our result was significantly lower than the amount of WTP for the COVID‐19 vaccines in previous studies conducted in Indonesia (USD 57.2) [16], Malaysia (USD 30.66) [19], China (ranging from USD 28 to USD 149) [20, 21, 22], and Ecuador (up to USD 102.5) [24]. Besides the perception of the risk and severity of the disease, which varied across countries, we suppose another possible reason was that our study was performed when several COVID‐19 vaccines were officially launched to market and information on prices of those vaccines were available while previous studies were conducted with hypothetical COVID‐19 vaccines. The amount of WTP for the vaccine in this study was, therefore, close to the prices of available vaccines in the market. However, the rate of willingness to pay (82.6%) was higher than the vaccination acceptance rate (60.4%), perhaps because women might not be willing to get vaccinated, but might be willing to pay for other people (e.g. husband, child or parents) to be vaccinated.
Our study echoed previous findings when showing that higher income was associated with a higher likelihood of willingness to pay for vaccine [16, 20, 23, 33]. We also found that white‐collar workers (or office workers) were more likely to pay for the vaccine than pregnant women with other jobs such as blue‐collar workers or others, which might be because white‐collar jobs generate higher income. Interestingly, pregnant women in Ca Mau in the south were less likely to receive the vaccine but more likely to pay for the vaccine than women in Hanoi in the north. Women in Ca Mau had a lower level of education than those in Hanoi; hence, it may be more difficult for them to accept a new public good such as vaccines [34] whose efficacy and safety in pregnant women were uncertain [12]. However, regarding WTP for the vaccine, the reason might be related to the cultural differences: northern people are cautious when paying for any goods, especially for one that is not already on the market, southerners are more open to paying for a commodity. This result suggested the importance of contextualisation when developing strategies for resource mobilisation for the COVID‐19 vaccine.
Self‐perceived risk of COVID‐19 was related to willingness to pay for the vaccine. This result is similar to a previous study where perceived risk or susceptibility was associated with acceptance and willingness to pay for the COVID‐19 vaccine [16, 31]. In addition, we found that women who perceived the risk of COVID‐19 in their friends were more likely to receive the vaccine and pay more for vaccine than others. This could be explained by the fact that they could not control the risks of their friends; and with that uncertainty, they were willing to get vaccinated, which could help them prevent the risk from their friends. Meanwhile, those perceiving risk of COVID‐19 in their colleagues showed a lower amount they were WTP for vaccination. We observed that in this case, pregnant women were more likely to transfer the responsibility of vaccine payment to their employers because they believed that the employers should demonstrate responsibility for the care and prevention of COVID‐19 infection to employees. Notably, in our result, a higher level of fear was associated with a lower amount of WTP, which could be because people with greater fear also have greater doubts about vaccine efficacy and safety, and in turn, had a lower amount of WTP for the vaccine.
Several implications would be proposed according to our findings. First, a vaccine safety communication plan should be developed to reassure pregnant women about the safety of available vaccines to increase their likelihood of willing to receive the vaccine. Second, as the most common reason for unwillingness to pay for COVID‐19 vaccine of rural and mountainous respondents was a financial hardship, the government should grant subsidies to them to increase vaccine coverage. Moreover, domestic subsidies should also be considered to provide free‐of‐charge vaccine for low‐income groups while allowing people with high‐come accessing vaccine via the private sector. Third, the policymakers could consider contextual factors when implementing COVID‐19 vaccination programmes given the socio‐cultural differences across regions in Vietnam.
Several limitations of this study should be noted. First, the convenient sampling technique in this study could produce sampling bias; thus one should be cautious when generalising our findings to other settings. Second, because our study asked the WTP of pregnant women for a hypothetical vaccine, the WTP might be lower or higher for the actual vaccine. Third, the cross‐sectional design limited our capacity to establish causal relationships between WTP and associated factors. Finally, our results limited only in pregnant women; thus, our findings could not be used to generalise to other women's groups.
CONCLUSION
Among pregnant women in Vietnam the willingness to receive and pay for COVID‐19 vaccine is high, suggesting that implementing vaccination for them is feasible. However, WTP should not be a barrier to quick and effective rollout of COVID‐19 vaccination programmes. For individuals who already show vaccine hesitancy, payment for COVID‐19 vaccines may cause another barrier to adequate coverage. Contextualised communication programmes to improve risk perception and awareness about vaccine safety and efficacy should be developed to facilitate acceptance of the vaccine.
ACKNOWLEDGEMENTS
We would like to acknowledge all pregnant women who supported this research.
Nguyen LH, Hoang MT, Nguyen LD, Ninh LT, Nguyen HTT, Nguyen AD, et al. Acceptance and willingness to pay for COVID‐19 vaccines among pregnant women in Vietnam. Trop Med Int Health. 2021;26:1303–1313. 10.1111/tmi.13666
Sustainable Development Goals: Good health and wellbeing, Reduced Inequality.
Nguyen and Hoang contributed equally.
REFERENCES
- 1. World Health Organization WHO coronavirus disease (COVID‐19) dashboard 2021. https://covid19.who.int/. Accessed 11 July, 2021.
- 2. Strategic Advisory Group of Experts (SAGE) . Background paper on Covid‐19 disease and vaccines 2020. https://apps.who.int/iris/bitstream/handle/10665/338095/WHO‐2019‐nCoV‐vaccines‐SAGE_background‐2020.1‐eng.pdf. Accessed 11 July, 2021.
- 3. World Health Organization . Pulse survey on continuity of essential health services during the COVID‐19 pandemic: interim report, 27 August 2020. https://www.who.int/publications/i/item/WHO‐2019‐nCoV‐EHS_continuity‐survey‐2020.1. Accessed 11 July, 2021.
- 4. Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, et al. Characteristics of women of reproductive age with laboratory‐confirmed SARS‐CoV‐2 infection by pregnancy status – United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jering KS, Claggett BL, Cunningham JW, Rosenthal N, Vardeny O, Greene MF, et al. Clinical characteristics and outcomes of hospitalized women giving birth with and without COVID‐19. JAMA Intern Med. 2021;181(5):714–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lokken EM, Huebner EM, Taylor GG, Hendrickson S, Vanderhoeven J, Kachikis A, et al. Disease severity, pregnancy outcomes and maternal deaths among pregnant patients with SARS‐CoV‐2 infection in Washington State. Am J Obstet Gynecol. 2021;225(1):77.e1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kumar R, Yeni CM, Utami NA, Masand R, Asrani RK, Patel SK, et al. SARS‐CoV‐2 infection during pregnancy and pregnancy‐related conditions: concerns, challenges, management and mitigation strategies–a narrative review. J Infect Public Health. 2021;14(7):863–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fahriani M, Anwar S, Yufika A, Bakhtiar B, Wardani E, Winardi W, et al. Disruption of childhood vaccination during the COVID‐19 pandemic in Indonesia. Narra J. 2021;1(1):e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang X, Guan Y. COVID‐19 drug repurposing: a review of computational screening methods, clinical trials, and protein interaction assays. Med Res Rev. 2021;41(1):5–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization . COVID‐19 vaccines 2021. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/covid‐19‐vaccines. Accessed 11 July, 2021.
- 11. US Centers for Disease Control and Prevention . Vaccination considerations for people who are pregnant or breastfeeding 2021. https://www.cdc.gov/coronavirus/2019‐ncov/vaccines/recommendations/pregnancy.html. Accessed 11 July, 2021.
- 12. Stafford IA, Parchem JG, Sibai BM. The coronavirus disease 2019 vaccine in pregnancy: risks, benefits, and recommendations. Am J Obstet Gynecol. 2021;224(5):484–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gray KJ, Bordt EA, Atyeo C, Deriso E, Akinwunmi B, Young N, et al. COVID‐19 vaccine response in pregnant and lactating women: a cohort study. medRxiv. 2021. [DOI] [PMC free article] [PubMed]
- 14. Gilbert P, Rudnick C. Newborn antibodies to SARS‐CoV‐2 detected in cord blood after maternal vaccination. medRxiv. 2021:2021.02.03.21250579. [DOI] [PMC free article] [PubMed]
- 15. Kilich E, Dada S, Francis MR, Tazare J, Chico RM, Paterson P, et al. Factors that influence vaccination decision‐making among pregnant women: a systematic review and meta‐analysis. PLoS One. 2020;15(7):e0234827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Willingness‐to‐pay for a COVID‐19 vaccine and its associated determinants in Indonesia. Hum Vaccines Immunother. 2020;16(12):3074–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID‐19 vaccine in Southeast Asia: a cross‐sectional study in Indonesia. Front Public Health. 2020;8(381). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vo NX, Huyen Nguyen TT, Van Nguyen P, Tran QV, Vo TQ. Using contingent valuation method to estimate adults’ willingness to pay for a future coronavirus 2019 vaccination. Value Health Reg Issues. 2021;24:240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wong LP, Alias H, Wong P‐F, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID‐19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID‐19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12):e0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhang Y, Luo X, Ma ZF. Willingness of the general population to accept and pay for COVID‐19 vaccination during the early stages of COVID‐19 pandemic: a nationally representative survey in mainland China. Hum Vaccin Immunother. 2021;17(6):1622–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang J, Lyu Y, Zhang H, Jing R, Lai X, Feng H, et al. Willingness to pay and financing preferences for COVID‐19 vaccination in China. Vaccine. 2021;39(14):1968–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. García LY, Cerda AA. Contingent assessment of the COVID‐19 vaccine. Vaccine. 2020;38(34):5424–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sarasty O, Carpio CE, Hudson D, Guerrero‐Ochoa PA, Borja I. The demand for a COVID‐19 vaccine in Ecuador. Vaccine. 2020;38(51):8090–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Health VMo . Acute respiratory infection COVID‐19 portal Hanoi: Ministry of Health; 2021. https://ncov.moh.gov.vn/. Accessed 11 July, 2021.
- 26. Tran BX, Hoang MT, Pham HQ, Hoang CL, Le HT, Latkin CA, et al. The operational readiness capacities of the grassroots health system in responses to epidemics: implications for COVID‐19 control in Vietnam. J Glob Health. 2020;10(1):011006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dang AK, Le XTT, Le HT, Tran BX, Do TTT, Phan HTB, et al. Evidence of COVID‐19 impacts on occupations during the first Vietnamese national Lockdown. J. Glob. Health. 2020;86(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Health VMo . COVID‐19 vaccine in Vietnam: there will be both expanded immunization and on‐demand services Hanoi: Ministry of Health; 2021. https://ncov.moh.gov.vn/web/guest/‐/6847912‐95. Accessed 11 July, 2021.
- 29. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID‐19 scale: development and initial validation. Int J Ment Health Addict. 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Le XTT, Nguyen HT, Le HT, Do TTT, Nguyen TH, Vu LG, et al. Rural‐urban differences in preferences for influenza vaccination among women of childbearing age: implications for local vaccination service implementation in Vietnam. Trop Med Int Health. 2021;26(2):228–36. [DOI] [PubMed] [Google Scholar]
- 31. Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID‐19 vaccine in Southeast Asia: a cross‐sectional study in Indonesia. Front Public Health. 2020;8:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, et al. The impact of COVID‐19 pandemic on physical and mental health of Asians: a study of seven middle‐income countries in Asia. PLoS One. 2021;16(2):e0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cerda AA, García LY. Willingness to pay for a COVID‐19 vaccine. Appl Health Econ Health Policy. 2021;19(3):343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID‐19 vaccine. Nat Med. 2021;27(2):225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


