BACKGROUND
It is estimated that 1.9 million older adults are completely homebound with many more requiring the assistance of others to leave their home.1 Many of these patients are best served with home‐based medical care, and yet medical trainees receive limited training to provide care in the home environment. Incorporating house calls into residency training is integral to teaching resident physicians about the care of homebound older adults.2, 3
Although the COVID‐19 pandemic has shifted medical education online, it remains important that we provide opportunities for trainees to build longitudinal primary care relationships, learn geriatric care in the home environment, and receive feedback from attending preceptors directly observing their clinical care. The Johns Hopkins Home‐based Medicine (JHOME) program provides home‐based primary care to older adults in Baltimore, Maryland, and is a unique opportunity for longitudinal training in this setting. Internal medicine residents in the general internal medicine (GIM) track of the Johns Hopkins Bayview (JHB) Internal Medicine Residency Program follow a panel of 4–5 homebound older adult patients during their second and third years of residency and see them at home every 3 months during their community‐based practice rotation. Typically, attending preceptors and residents see patients in the home together, allowing preceptors to directly observe the visit and provide feedback. In response to the COVID‐19 pandemic, the JHOME team adapted house call education to limit the number of visitors in the home while still preserving opportunities for practice‐based learning. Following 9 months of piloting several visit approaches, we surveyed residents to gather their perspectives and plan for future education.
METHODS
A voluntary, anonymous online survey was sent to the 15 second‐ and third‐year GIM residents at JHB. The survey consisted of Likert scale (strongly agree, agree, neither agree or disagree, disagree, and strongly disagree) and open‐ended questions specifically focused on the experience of residents during the first 9 months of the pandemic.
The objective of the survey was to better understand the facilitators and barriers to learning in the home environment via three visit types that utilized a secure video conferencing software: (1) resident leading the visit on video with the attending preceptor in the home, (2) resident in the home with the attending preceptor observing on video, or (3) resident observing a resident colleague lead a visit on video. There was one open‐ended question about the overall JHOME experience.
This study was designated as exempt by the Johns Hopkins Institutional Review Board.
RESULTS
Fifteen residents were surveyed, 100% responded to the survey. Sixty percent of the residents were in their first year of house calls and had not conducted visits prior to the pandemic. All residents reported they had the opportunity to try out the three approaches to visits during the pandemic. The majority of residents agreed or strongly agreed that they enjoyed each of the approaches to house calls. The most popular approach was being present in the home with the attending preceptor on video, with 14 of 15 residents who agreed or strongly agreed they enjoyed this approach. The least popular approach was observing resident colleagues lead visits. Ten of fifteen residents agreed or strongly agreed that they enjoyed this approach. When asked to choose their preferred approach, most residents (58%) preferred being in‐person with the attending preceptor on video. In addition, residents identified positive and negative factors for each hybrid approach (Figure 1).
FIGURE 1.
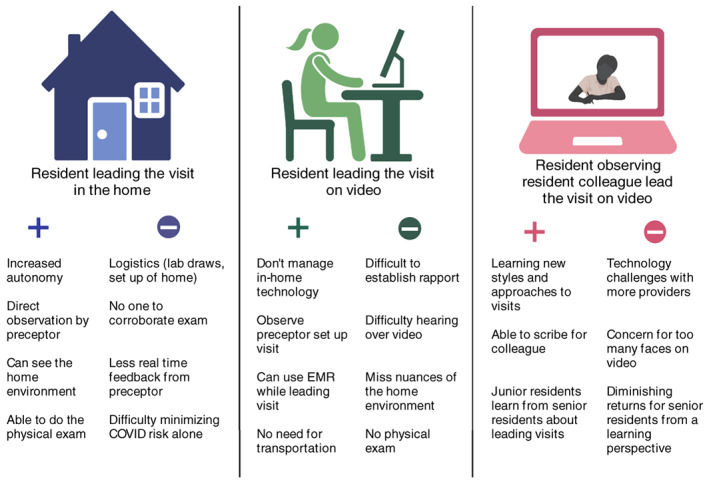
Resident perceptions of hybrid approaches to house calls
DISCUSSION
The pandemic has forced innovation in medical education across settings.4 We found that within our JHOME program, the visit adjustments made during the pandemic expanded opportunities for direct observation and experiential learning for residents in the home setting. Residents who performed a house call on their own with the attending observing on video were able to experience a house call as it might be for a practicing house call doctor, while still having opportunity for direct observation. The residents identified autonomy as one of the positive aspects of this approach, and this may also be one of the reasons they chose this as the preferred approach out of the three options. An additional benefit of this strategy has been increasing the number of house calls an attending can precept in a half‐day session since they tune in to the visit remotely although residents travel to the house call. Although we plan to return to attending‐resident joint in‐person visits with the easing of the pandemic and the roll out of vaccination, we anticipate the benefits of hybrid approaches may lead to care delivery innovations that have long‐term implications. We hope that changes to telemedicine requirements, which allowed for this innovative teaching strategy during the COVID public health emergency, will be permanently adopted. We plan to continue educational opportunities to allow residents to perform solo house calls for their longitudinal patients with a preceptor and possibly a colleague or other learner observing on video.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Drs. Robertson, Colburn, Schuchman, and Cudjoe were involved in the study concept and design, acquisition of data, and preparation of manuscript.
SPONSOR'S ROLE
None.
Robertson ML, Schuchman M, Cudjoe TKM, Colburn J. Innovative educational approaches to house calls in the time of COVID‐19. J Am Geriatr Soc. 2021;69(8):E20–E22. 10.1111/jgs.17331
Contributor Information
Mariah Lyn Robertson, Email: mdewsna1@jhmi.edu, @MLRobertsonMD.
Jessica Colburn, Email: jcolbur1@jh.edu.
REFERENCES
- 1.Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175(7):1180‐1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayashi JL, Christmas C, Durso SC. Educational outcomes from a novel house call curriculum for internal medicine residents: report of a 3‐year experience. J Am Geriatr Soc. 2011;59(7):1340‐1349. [DOI] [PubMed] [Google Scholar]
- 3.Hayashi JL, Phillips KA, Arbaje A, Sridharan A, Gajadhar R, Sisson SD. A curriculum to teach internal medicine residents to perform house calls for older adults. J Am Geriatr Soc. 2007;55(8):1287‐1294. [DOI] [PubMed] [Google Scholar]
- 4.Lucey CR, Johnston SC. The transformational effects of COVID‐19 on medical education. JAMA. 2020;324(11):1033‐1034. [DOI] [PubMed] [Google Scholar]


