Abstract
Background
To combat the coronavirus disease 2019 pandemic, many countries, including Japan, implemented policies limiting social activities and encouraging preventive behaviors. This study examines the influence of such policies on the trends of 10 infectious pediatric diseases: pharyngoconjunctival fever; group A streptococcal pharyngitis; infectious gastroenteritis; chickenpox; erythema infectiosum; hand, foot, and mouth disease; herpangina; respiratory syncytial virus; exanthem subitum; and mumps.
Methods
The research adopted a retrospective cohort study design. We collected data from Japan's National Epidemiological Surveillance Program detailing the incidences of the 10 diseases per pediatric sentinel site for a period beginning at 9 weeks before government‐ordered school closures and ending at 9 weeks after the end of the state of emergency. We obtained corresponding data for the equivalent weeks in 2015–2019. We estimated the influence of the policies using a difference‐in‐differences regression model.
Results
For seven diseases (pharyngoconjunctival fever; group A streptococcal pharyngitis; infectious gastroenteritis; chickenpox; erythema infectiosum; hand, foot, and mouth disease; and herpangina), the incidence in 2020 decreased significantly during and after the school closures. Sensitivity analysis, in which the focus area was limited to the policy‐implementation period or existing trend patterns, replicated these significant decreases for one of the above mentioned seven diseases – infectious gastroenteritis.
Conclusions
Policies such as school closures and encouragement of preventive behaviors were associated with significant decreases in the incidences of most of the 10 diseases, which sensitivity analysis replicated in infectious gastroenteritis. To determine the long‐term effects of these policies, prospective cohort studies are needed.
Keywords: communicable disease, data collection, epidemiology, public policy, universal precaution
Coronavirus disease 2019 (COVID‐19) emerged in late 2019 and was declared a pandemic in March 2020. 1 , 2 To prevent the spread of COVID‐19, many national governments implemented policies limiting social activities. These measures included closures of schools and workplaces, placing restrictions on public transport and mass gatherings, and enforcing lockdowns. 3 Preventive behaviors were also encouraged, such as physical distancing; avoiding touching one's eyes, nose, and mouth; use of alcohol‐based hand sanitizers; washing hands; and wearing masks. 4 , 5 Several reports suggest that the implementation of these measures may be associated with a decline in the incidence of influenza in 2020. 6 , 7
In Japan, the government ordered the closure of all elementary, junior high, high, and special‐needs schools, declared a state of emergency, and sought to limit social activities and encourage preventive behaviors. 8 , 9 , 10 , 11 These policies may have impacted the prevalence of infectious pediatric diseases, as few have been reported. 12 In the present study we therefore aimed to examine the influence of the anti‐COVID‐19 policies on the prevalence of pediatric infections using an existing national infectious disease surveillance system.
Methods
The present research comprised a retrospective cohort study.
Setting and data source
The data for this study were obtained from the National Epidemiological Surveillance of Infectious Diseases (NESID) Program. 13 , 14 , 15 In Japan, based on the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases, the trends of a number of diseases are monitored. 16 Regarding pediatric infections, the NESID Program records the weekly incidences of 10 diseases by monitoring data from approximately 3,000 pediatric sentinel sites located across the country; these 10 diseases are: pharyngoconjunctival fever; group A streptococcal pharyngitis; infectious gastroenteritis; chickenpox; erythema infectiosum; hand, foot, and mouth disease; herpangina; respiratory syncytial virus (RSV); exanthem subitum; and mumps. 17
In Japan, most patients of pediatric hospitals and clinics are under 15 years old. 18 In January we therefore collected data of the total child population aged <15 years from the website of official statistics in Japan and used this information as the denominator. 19 The pediatric sentinel sites were chosen randomly as much as possible from hospitals and clinics with a pediatric department to monitor the cases of infections in each prefecture, considering the distribution of the population as well as hospitals and clinics with a pediatric department. The number of sentinel sites was decided based on the size of the population being served by each public health center. 20 For example, for a population size of <30 000, 30 000 ≤ 75 000, or ≥75 000, the number of sentinel sites was 1, 2, or 3+ (this number was determined by subtracting 75 000 from the size of the population and dividing the result by 50 000). We collected the data for the number of sentinel sites every week during the 2015–2019 observation period through annual reports. 13 In the sentinel sites, when the 10 diseases mentioned above are diagnosed, the numbers of cases are reported the following Monday. Respiratory syncytial virus and group A streptococcal pharyngitis require a positive diagnostic test for the diagnosis but others do not. 17 In weekly monitoring, each week commenced on a Monday and ended on the following Sunday; the first week of the year could commence in the previous year if the first day of the year was not a Monday. 21 One week was defined such that the first week of the year included at least 4 days of the new year. All weeks were numbered serially.
Exposures
The Japanese government began encouraging preventive behaviors on February 25, 2020 (the second day of week 9), and on March 2 (the first day of week 10) it ordered the closure of all elementary, junior high, high, and special‐needs schools until the end of the spring vacation. 8 , 11 Next, on April 7 (the second day of week 15), it declared a state of emergency and recommended limiting social activities. 9 During the state of emergency, the Japanese government modified the districts which required limiting social activities thrice, depending on the incidences. The government ended the state of emergency on May 25 (the first day of week 22). 10
Outcomes
For each of the 10 infectious pediatric diseases focused on in this research, we collected data regarding the cases per pediatric sentinel site from week 1 to week 30 for each year from 2015 to 2020. 14 , 15 , 22 In cases where we could not obtain data on the number of cases per pediatric sentinel site, we collected the data regarding the overall weekly number of cases and divided the number by the number of sentinel sites.
As we used data that were openly available online, no approval from an ethics committee was required.
Statistical analysis
Means and standard deviations were used to describe the number of the pediatric sentinel sites each week for each of the year‐based observation periods, and the total number of cases and estimated child population in Japan of each year were also reported. Each disease trend (cases per sentinel site) was described using line graphs. We estimated the influence of anti‐COVID‐19 policies, both school closures and encouragement of preventive behaviors, using a difference‐in‐differences regression model. 23 This model can be used to estimate a policy's effects, as it compares an intervention group's outcomes before and after the policy implementation, and also compares these outcomes with a control group's contemporaneous outcomes (which were not affected by the policy). 23 For the present analysis, we assumed parallel trends and same effects from other events except the effects of policy implementation on each trend during and after the period of the implementation and its corresponding period for each year. In the main analysis, we regarded the intervention period as 10–30 weeks – that is, from the start of school closures until after the schools reopened. To perform sensitivity analysis, we limited the intervention period to 10–21 weeks, which represented the period during which the policies for limiting social activities were implemented. We adjusted the intervention and its corresponding period (10–30/10–21 weeks every year from 2015–2020), the year of 2020, and anti‐COVID‐19 policies (10–30/10–21 weeks in 2020) as independent variables. The beta‐coefficients of 10–30/10–21 weeks every year from 2015–2020, the year of 2020, and anti‐COVID‐19 policies represent the risk difference of each independent variable. When the beta‐coefficients with 95% confidential interval were under 0 or above 0, we regarded it as a statistically significant decrease or increase, respectively. In cases where visual judgment of the line graphs helped detect several trend patterns for a disease, we estimated the influence of each pattern using a difference‐in‐differences regression model. We used Microsoft Excel® 2016 (Microsoft Corporation, Redmond, WA, USA) to develop the line graphs, and Stata® 14.2 (Stata Corp, College Station, TX, USA) for the other analyses.
Results
The mean numbers of pediatric sentinel sites during the observation period were 3,148.5 ± 37.5 in 2015, 3,159.5 ± 4.6 in 2016, 3,162.7 ± 5.3 in 2017, 3,157.9 ± 9.3 in 2018, and 3,157.6 ± 52.6 in 2019. The numbers for 2020 were not reported. The number of cases of the 10 diseases reported during the observation period is shown in Table 1. The total child population, those aged 0–14 years, in Japan is shown in Table S1.
Table 1.
The annual number of reported cases for the 10 target diseases during the observation period
| Disease name/year | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|---|
| Pharyngoconjunctival fever | 42 853 | 43 331 | 52 535 | 44 372 | 40 949 | 21 226 |
| Group A streptococcal pharyngitis | 255 406 | 249 252 | 234 348 | 230 083 | 216 000 | 152 618 |
| Infectious gastroenteritis | 618 169 | 565 980 | 559 651 | 505 412 | 537 136 | 276 308 |
| Chickenpox | 46 651 | 38 615 | 35 480 | 31 204 | 32 953 | 20 959 |
| Erythema infectiosum | 57 786 | 42 271 | 7,979 | 14 626 | 67 227 | 17 338 |
| Hand, foot, and mouth disease | 186 164 | 17 392 | 156 878 | 59 591 | 238 006 | 9,521 |
| Herpangina | 50 949 | 66 796 | 40 098 | 39 980 | 51 128 | 6,167 |
| RSV | 31 207 | 26 770 | 30 173 | 39 712 | 40 410 | 12 274 |
| Exanthem subitum | 49 256 | 45 225 | 44 148 | 42 318 | 38 446 | 34 843 |
| Mumps | 35 798 | 88 116 | 54 576 | 15 221 | 9,644 | 4,663 |
RSV, respiratory syncytial virus.
The trends for five diseases (pharyngoconjunctival fever; group A streptococcal pharyngitis; infectious gastroenteritis; chickenpox; and erythema infectiosum) are shown in Figure 1a–e. The trends for pharyngoconjunctival fever (Fig. 1a), group A streptococcal pharyngitis (Fig. 1b), infectious gastroenteritis (Fig. 1c), chickenpox (Fig. 1d), and erythema infectiosum (Fig. 1e) showed that their number of weekly cases in 2020 were the lowest across the 2015–2020 period, starting from late March (week 13), the middle of March (week 11), late February (week 9), the middle of March (week 12), and early May (week 19), respectively, to the end of the observation period after the school closure.
Fig. 1.
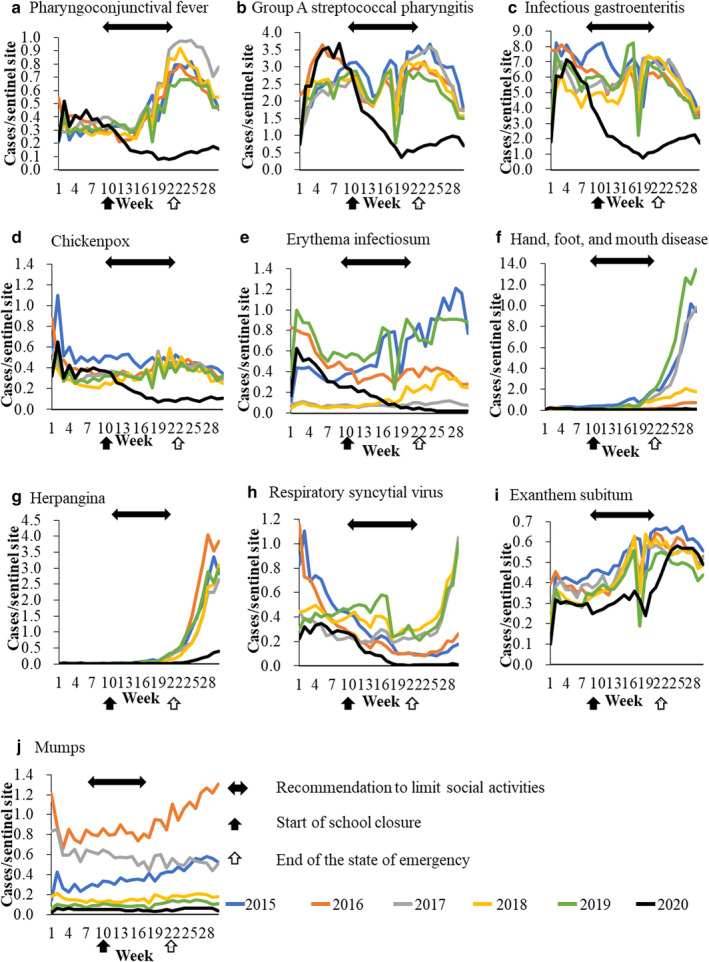
Trends for 10 infectious diseases: (a) pharyngoconjunctival fever; (b) group A streptococcal pharyngitis; (c) infectious gastroenteritis; (d) chickenpox; (e) erythema infectiosum; (f) hand, foot, and mouth disease; (g) herpangina; (h) respiratory syncytial virus; (i) exanthem subitum; (j) mumps. Blue line shows the trend for 2015, orange line for 2016, gray line for 2017, yellow line for 2018, green line for 2019, and black line for 2020.
The number of cases per week for hand, foot, and mouth disease (Fig. 1f) and herpangina (Fig. 1g) started to increase in April and May of every year during the observation period. The per week cases of these diseases in 2020 were the lowest for the entire 2015–2020 period, starting from late April (week 17) and March (week 12), respectively, to the end of the observation period after the school closure.
The trend for RSV over the period of 2015–2020 is shown in Figure 1h. When considering the trends for 2015–2019, two patterns were detected. In 2015 and 2016, the highest occurrences per week were detected in early January (week 1 or 2). In contrast, in 2017, 2018, and 2019, the highest occurrence in a week was detected in late July (week 30). From the middle of March (week 12) 2020 to the end of the observation period, the number of weekly cases was the lowest for the entire 2015–2020 period.
The trend for exanthem subitum is shown in Figure 1i. From early January (week 1) to early June (week 23) 2020, the number of cases per week was the lowest for the 2015–2020 period, with the exception of early February (week 7) and late April (week 18). After week 23, the number of weekly cases was no longer the lowest, unlike that for other diseases.
The trend for mumps is shown in Figure 1j. Overall, the number of cases each week in 2020 was the lowest across the 2015–2020 period.
The main analysis showed that, for seven of the 10 diseases (pharyngoconjunctival fever; group A streptococcal pharyngitis; infectious gastroenteritis; chickenpox; erythema infectiosum; hand, foot, and mouth disease; and herpangina), the number of weekly cases in 2020 was significantly lower during and after the school closures (Table 2). Sensitivity analysis replicated the significant findings from the main analysis for infectious gastroenteritis (Table S2). The results of hand, foot, and mouth disease and herpangina showed a significant increase, conflicting with those of the main analysis. The results of exanthem subitum showed significant decreases in the 2020 incidences, which were not noted as significant in the main analysis. Regarding RSV, over the course of the entire observation period, the number of weekly cases in 2020 did not differ significantly, including when sensitivity analysis was performed limiting the intervention period to 10–21 weeks. However, when considering the trend seen in the previous years (2017, 2018, and 2019 featuring peaks in July), the sensitivity analysis showed that, after the introduction of policies such as school closures and encouragement of preventive behaviors, the trend in 2020 showed a significant decrease in the number of cases each week while the results of the sensitivity analysis considering the other patterns (2015 and 2016 featuring peaks in January) showed a significant increase. One disease (mumps) did not show a significant decrease in either the main or the sensitivity analysis.
Table 2.
The effects of each independent variable on the number of cases per week per sentinel site in the main analysis
| Disease name | Independent variables | Crude beta‐coefficient | 95% CI | Adjusted beta‐coefficient | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Pharyngoconjunctival fever | 10–30 weeks in each year from 2015–2020 | 0.143 | 0.096 | ‐ | 0.189 | 0.216 | 0.171 | ‐ | 0.261 |
| 2020 | −0.249 | −0.305 | ‐ | −0.193 | 0.059 | 0.003 | ‐ | 0.114 | |
| anti‐COVID‐19 policies | −0.311 | −0.354 | ‐ | −0.268 | −0.440 | −0.515 | ‐ | −0.365 | |
| Group A streptococcal pharyngitis | 10–30 weeks in each year from 2015–2020 | −0.147 | −0.382 | ‐ | 0.089 | 0.183 | −0.035 | ‐ | 0.400 |
| 2020 | −0.891 | −1.294 | ‐ | −0.489 | 0.492 | −0.111 | ‐ | 1.096 | |
| anti‐COVID‐19 policies | −1.450 | −1.733 | ‐ | −1.167 | −1.977 | −2.646 | ‐ | −1.307 | |
| Infectious gastroenteritis | 10–30 weeks in each year from 2015–2020 | −0.999 | −1.495 | ‐ | −0.503 | −0.452 | −0.907 | ‐ | 0.003 |
| 2020 | −2.967 | −3.714 | ‐ | −2.220 | −0.667 | −1.772 | ‐ | 0.438 | |
| anti‐COVID‐19 policies | −4.069 | −4.408 | ‐ | −3.729 | −3.286 | −4.449 | ‐ | −2.123 | |
| Chickenpox | 10–30 weeks in each year from 2015–2020 | −0.052 | −0.100 | ‐ | −0.005 | −0.014 | −0.066 | ‐ | 0.038 |
| 2020 | −0.169 | −0.225 | ‐ | −0.114 | −0.007 | −0.090 | ‐ | 0.076 | |
| anti‐COVID‐19 policies | −0.243 | −0.284 | ‐ | −0.202 | −0.232 | −−0.324 | ‐ | −0.139 | |
| Erythema infectiosum | 10–30 weeks in each year from 2015–2020 | −0.003 | −0.094 | ‐ | 0.087 | 0.057 | −0.047 | ‐ | 0.160 |
| 2020 | −0.217 | −0.296 | ‐ | −0.137 | 0.036 | −0.091 | ‐ | 0.163 | |
| anti‐COVID‐19 policies | −0.308 | −0.366 | ‐ | −0.249 | −0.361 | −0.505 | ‐ | −0.217 | |
| Hand, foot, and mouth disease | 10–30 weeks in each year from 2015–2020 | 1.458 | 0.952 | ‐ | 1.964 | 1.761 | 1.169 | ‐ | 2.354 |
| 2020 | −1.287 | −1.720 | ‐ | −0.854 | −0.014 | −0.048 | ‐ | 0.021 | |
| Anti‐COVID‐19 policies | −1.234 | −1.644 | ‐ | −0.823 | −1.819 | −2.412 | ‐ | −1.226 | |
| Herpangina | 10–30 weeks in each year from 2015–2020 | 0.614 | 0.437 | ‐ | 0.792 | 0.725 | 0.518 | ‐ | 0.932 |
| 2020 | −0.461 | −0.619 | ‐ | −0.303 | 0.004 | −0.001 | ‐ | 0.008 | |
| Anti‐COVID‐19 policies | −0.414 | −0.568 | ‐ | −0.259 | −0.663 | −0.876 | ‐ | −0.450 | |
| RSV | 10–30 weeks in each year from 2015–2020 | −0.185 | −0.248 | −0.121 | −0.175 | −0.245 | ‐ | −0.104 | |
| 2020 | −0.226 | −0.283 | ‐ | −0.168 | −0.183 | −0.247 | ‐ | −0.119 | |
| Anti‐COVID‐19 policies | −0.293 | −0.340 | ‐ | −0.246 | −0.061 | −0.142 | ‐ | 0.021 | |
| Exanthem subitum | 10–30 weeks in each year from 2015–2020 | 0.157 | 0.130 | ‐ | 0.184 | 0.162 | 0.135 | ‐ | 0.189 |
| 2020 | −0.095 | −0.143 | ‐ | −0.047 | −0.076 | −0.123 | ‐ | −0.029 | |
| Anti‐COVID‐19 policies | −0.044 | −0.098 | ‐ | 0.011 | −0.027 | −0.099 | ‐ | 0.046 | |
| Mumps | 10–30 weeks in each year from 2015–2020 | 0.033 | −0.068 | ‐ | 0.135 | 0.040 | −0.071 | ‐ | 0.151 |
| 2020 | −0.380 | −0.432 | ‐ | −0.329 | −0.352 | −0.444 | ‐ | −0.260 | |
| Anti‐COVID‐19 policies | −0.359 | −0.410 | ‐ | −0.308 | −0.040 | −0.152 | ‐ | 0.071 | |
CI, confidential interval; RSV, respiratory syncytial virus.
Discussion
For most of the diseases analyzed, the number of cases per sentinel sites per week decreased during and after the implementation of policies enforcing school closures and encouraging preventive behaviors. For seven diseases, the effects of these policies were detected in the main analysis, and the results for one of these seven diseases were replicated in the sensitivity analysis.
A possible reason for the decreased incidences observed for most of the 10 diseases may be that, once the schools were closed, the children had fewer opportunities to come in contact with others. 24 Some children may also have adopted preventive behaviors. On the other hand, possible reasons for which significant decreases in six of the diseases (pharyngoconjunctival fever; group A streptococcal pharyngitis; chickenpox; erythema infectiosum; hand, foot, and mouth disease; and herpangina) were detected in the main analysis but not in the sensitivity analysis include a general improvement in precautionary behaviors and the small effect size and sample size. 10 For example, the number of chickenpox cases is controlled through mandatory vaccinations, and throughout the study period its weekly incidence was low. 25 The numbers of pharyngoconjunctival fever cases and erythema infectiosum cases also showed a level similar to that of chickenpox. The number of group A streptococcal pharyngitis cases was relatively high when compared to chickenpox. Despite this, no significant decrease was detected in the sensitivity analysis; this may be due to the small difference between the number of cases in 2020 and that in 2015–2019. The results of sensitivity analysis of hand, foot, and mouth disease and herpangina were unexpectedly different from those of the main analysis. This may be because the numbers of cases of these two diseases were as low as chickenpox in winter and early spring, the largest part of the sensitivity period. The effect size was so low that a random error was detected. Meanwhile, for pharyngoconjunctival fever, group A streptococcal pharyngitis, infectious gastroenteritis, chickenpox, and erythema infectiosum, the reduction in incidence was as expected. These results should be interpreted carefully if these statistical differences suggest significant clinical differences. Another possible reason for six diseases not being replicated in the sensitivity analysis may be the fact that some schools reopened gradually in Japan. 26 Some schools finished classes earlier than usual, and others rotated groups of children into the school at different times during the week. This may have contributed to fewer opportunities for children to indulge in physical contact over a longer period and the significant decreases in the main analysis. Unexpectedly, the incidence of RSV did not show a significant decrease in either the main analysis or the sensitivity analysis that focused on the period when social activities were restricted. On the other hand, the sensitivity analysis that focused on trend patterns in 2017–2019, which featured high incidences in July, showed that the introduction of policies such as school closures and encouragement of preventive behaviors brought about a significant decrease in the 2020 incidence of the mentioned diseases. The results obtained for the main analysis may therefore have considered the two trend patterns insufficiently. Exanthem subitum showed a different trend from the others. The number of cases reduced significantly during weeks 10–21 (from the start of the order to close all schools to the end of the state of emergency), but this was not shown in the main analysis. Exanthem subitum is mainly transmitted through saliva from parents rather than from social contact. 27 In addition, although exanthem subitum can cause fever, seizures, skin rash, and gastrointestinal and respiratory tract symptoms, these are relatively mild in most infants. 28 The lower number of cases of this disease might therefore have been a result of parents avoiding bringing their children to clinics, including pediatric sentinel sites, as a result of a fear of COVID‐19 infection. The number of mumps cases was not significantly lower in 2020. Mumps outbreaks occur occasionally, 29 and its vaccination is not mandatory in Japan. 25 The number of cases during the study years therefore varied, which may have made it difficult to estimate the effect size. Regarding the external validity of these findings, all data were obtained in Japan; thus, future research is required in this regard.
Some of these 10 diseases cause more severe symptoms in children than in adults, or can cause complications for the fetus through maternal infection. 30 , 31 , 32 , 33 For example, RSV affects younger infants more severely than older children, and hospitalization and mortality are high in infants aged <1 year. 30 Chickenpox and erythema infectiosum can also cause intrauterine death or, when maternal infection occurs, severe consequences to the fetus. 32 , 33 Thus, the influence of the anti‐COVID‐19 policies on reducing the incidences of these diseases may be beneficial in both the long term and short term. On the other hand, some diseases can cause more severe symptoms in adults than in children; for example, chickenpox can cause higher mortality in adults. 34 Prospective long‐term cohort studies will therefore be needed to examine the influences of the various policies on the prevalence of such diseases among adults.
There are several limitations to this study. First, there were selection biases. For example, decisions regarding the need for examination and diagnosis were taken by the children's respective pediatricians. Diseases like group A streptococcal pharyngitis and RSV, which are dependent on testing are largely affected by the requirement for personal protective equipment. Most physicians in clinics might opt against performing sampling. Therefore, the number of estimated cases may be lower than in reality. In addition, the COVID‐19 pandemic might have caused people to refrain from visiting clinics, including pediatric sentinel sites. However, the change in healthcare‐seeking behavior should not be related to decreases in diseases with symptoms severe enough to need hospitalization. Recently, a large Japanese cohort report revealed that the number of inpatients with pediatric infectious diseases decreased due to anti‐COVID‐19 policies; thus a true reduction in incidences was detected. 12 The reductions found in this paper were therefore not only due to changes in healthcare‐seeking behavior. Second, there is a measurement bias. The date of the end of spring vacation, which marked the end of government‐ordered school closures, differed across schools, and the state of emergency did not obligate complete school closures. In addition, the Japanese government did not implement policies for limiting social activities to all prefectures during the entire emergency period, and modified the districts that needed such policies three times. Therefore, not all schools were closed over the entire period of the government‐implemented policies and the policies' effect may be different in each school in each prefecture. In addition, there were no data measuring the effectiveness of the policy encouraging preventive behaviors. The COVID‐19 pandemic and the associated policies would have caused some school children and adolescents to adopt preventive behaviors; however, neonates, infants, preschool children, and other school children and adolescents would have been unable to adopt them. 35 , 36 Third, there were some issues related to the statistical analysis. The change in healthcare‐seeking behavior and the 6 day period preceding the school closures during which the Japanese government only encouraged preventive behaviors might have impacted the assumptions of the difference‐in‐differences regression model. However, the influence of the 6 day preventive‐behavior period may be small. We could also only obtain the data for the number of cases each week, could not determine the number of pediatric sentinel sites in 2020, and could not perform multilevel analysis. However, according to the implementation manual for the NESID Program, sentinel sites are chosen randomly as much as possible so that trends can be monitored. 20 To address this, we used the data for the number of weekly cases per pediatric sentinel site.
Conclusion
For seven of the 10 infectious pediatric diseases, the per week cases in 2020 significantly decreased during and after the implementation of preventive policies such as school closures, and was replicated by the sensitivity analysis for the 2020 incidence of infectious gastroenteritis. Prospective cohort studies with a long observation period will be needed to determine the long‐term influence of these policies.
Disclosure
Dr Miyakoshi received a grant from Chugai Pharmaceutical Co. Ltd; however, it was not associated with the submitted work. The other authors declare no conflict of interest.
Author contributions
S.Y.K. and Y.K. conceptualized and designed the study. S.Y.K. collected data. Y.K. supervised data collection. S.Y.K. conducted the initial analyses. Y.K. supervised analyses. S.Y.K. drafted the manuscript. S.Y.K., Y.K., K.T., C.M., and Y.Y. reviewed and revised the manuscript. All authors read and approved the final manuscript.
Supporting information
Table S1. The total child population (0–14 years old) in Japan.
Table S2. The effects of each independent variable on the number of cases per week per sentinel site in the sensitivity analysis.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1. World Health Organization . Coronavirus disease (COVID‐19) situation reports. [Cited 15 July 2020]. Available from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports/ [Google Scholar]
- 2. World Health Organization . Coronavirus disease (COVID‐19) pandemic. [Cited 4 September 2020]. Available from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019 [Google Scholar]
- 3. Islam N, Sharp SJ, Chowell G et al. Physical distancing interventions and incidence of coronavirus disease 2019: Natural experiment in 149 countries. BMJ 2020; 370: 2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . Coronavirus disease (COVID‐19) advice for the public. [Cited 4 September 2020]. Available from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/advice‐for‐public [Google Scholar]
- 5. Ministry of Health Labour and Welfare . Prevention measures against Coronavirus disease. 2019 (COVID‐19). [Cited 25 September 2020]. Available from: https://www.mhlw.go.jp/content/10900000/000607599.pdf [Google Scholar]
- 6. Itaya T, Furuse Y, Jindai K. Does COVID‐19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int. J. Infect. Dis. 2020; 97: 78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sakamoto H, Ishikane M, Ueda P. Seasonal influenza activity during the SARS‐CoV‐2 outbreak in Japan. JAMA 2020; 323(19): 1969–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ministry of Education, Culture, Sports and Technology J . [COVID‐19] Information about MEXT’s measures. [Cited 9 September 2020]. Available from: https://www.mext.go.jp/en/mext_00006.html [Google Scholar]
- 9. Looi MK. Covid‐19: Japan declares state of emergency as Tokyo cases soar. BMJ 2020; 9: m1447. [DOI] [PubMed] [Google Scholar]
- 10. Looi MK. Covid‐19: Japan ends state of emergency but warns of “new normal”. BMJ 2020; 369: m2100. [DOI] [PubMed] [Google Scholar]
- 11. Ministry of Health Labour and Welfare . Basic strategy against the Coronavirus Disease 2019. [Cited 25 September 2020]. Available from: https://www.mhlw.go.jp/content/10900000/000599698.pdf (Japanese) [Google Scholar]
- 12. Kishimoto K, Bun S, Takada D, Morishita T, Kunisawa S, Imanaka Y. Early impact of school closure and social distancing for COVID‐19 on the number of inpatients with childhood non‐COVID‐19 acute infections in Japan. medRxiv. 2020. [Cited 12 December 2020]; 2020.11.18.20233957. Available from: 10.1101/2020.11.18.20233957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Institute of Infectious Diseases . 2019 Annual report of the National Epidemiological Surveillance of Infectious Diseases Program [Internet]. [Cited 9 February 2021]. Available from: https://www.niid.go.jp/niid/ja/allarticles/surveillance/2270‐idwr/nenpou.html. (Japanese) [Google Scholar]
- 14. National Institute of Infectious Diseases . Weekly report of infectious diseases for 30 weeks of 2020; 2020. [Cited 4 September 2020]. Available from: https://www.niid.go.jp/niid/ja/data/9762‐idwr‐sokuho‐data‐j‐2030.html. Published 2020. (Japanese) [Google Scholar]
- 15. National Institute of Infectious Diseases . Weekly reports of infectious diseases for the 52 weeks of 2019; 2020. [Cited 23 July 2020]. Available from: https://www.niid.go.jp/niid/ja/data/9289‐idwr‐sokuho‐data‐j‐1952.html. Published 2020. (Japanese) [Google Scholar]
- 16. Japanese Law Translation : Act on the prevention of infectious diseases and medical care for patients with infectious diseases. [Cited 1 September 2020]. Available from: http://www.japaneselawtranslation.go.jp/law/detail/?vm=04&re=01&id=2830 [Google Scholar]
- 17. Ministry of Health Labour and Welfare . Requests for doctors' reports based on the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases. [Cited 15 July 2020]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/kekkaku‐kansenshou/kekkaku‐kansenshou11/01.html. (Japanese) [Google Scholar]
- 18. 17th meeting of examining health care plan in pediatric medicine. [Cited 25 November 2020]. Available from: https://www.mhlw.go.jp/content/10800000/000584472.pdf [Google Scholar]
- 19. Japan PS of OS of population estimates. [Cited 3 December 2020]. Available from: https://www.e‐stat.go.jp/en/stat‐search/files?page=1&layout=datalist&toukei=00200524&tstat=000000090001&cycle=1&tclass1=000001011678&tclass2val=0 [Google Scholar]
- 20. Implementation manual for the National Epidemiologic Surveillance of Infectious Disease Program. [Cited 2 December 2020]. Available from: https://www.mhlw.go.jp/file/06‐Seisakujouhou‐10900000‐Kenkoukyoku/0000196999.pdf. (Japanese) [Google Scholar]
- 21. National Institute of Infectious Diseases . Correspondence table of weekly reports. [Cited 16 July 2020]. Available from: https://www.niid.go.jp/niid/ja/calendar.html. (Japanese) [Google Scholar]
- 22. National Institute of Infectious Diseases . 2018 Annual report of the National Epidemiological Surveillance of Infectious Diseases Program. [Cited 20 July 2020]. Available from: https://www.niid.go.jp/niid/ja/allarticles/surveillance/2270‐idwr/nenpou/9203‐idwr‐nenpo2018.html. Published 2019. (Japanese) [Google Scholar]
- 23. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: The difference‐in‐differences approach. J. Am. Med. Assoc. 2014; 312: 2401–2. [DOI] [PubMed] [Google Scholar]
- 24. Litvinova M, Liu QH, Kulikov ES, Ajelli M. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc. Natl. Acad. Sci. USA 2019; 116(27): 13174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. e‐Gov . Enforcement order of Immunization act. [Cited 8 September 2020]. Available from: https://elaws.e‐gov.go.jp/search/elawsSearch/elaws_search/lsg0500/detail?lawId=323CO0000000197. Published 2020. [Google Scholar]
- 26. Ministry of Education, Culture, Sports S and T . Current situation regarding school reopening with COVID‐19. [Cited 25 November 2020]. Available from: https://www.mext.go.jp/content/20200603‐mxt_kouhou01‐000004520_4.pdf [Google Scholar]
- 27. Suga S, Yoshikawa T, Kajita Y, Ozaki T, Asano Y. Prospective study of persistence and excretion of human herpesvirus‐6 in patients with exanthem subitum and their parents. Pediatrics 1998; 102: 900–4. [DOI] [PubMed] [Google Scholar]
- 28. Agut H, Bonnafous P, Gautheret‐Dejean A. Human herpesviruses 6A, 6B, and 7. Microbiol. Spectr. 2016; 4(3): 1–18. [DOI] [PubMed] [Google Scholar]
- 29. Hviid A, Rubin S, Mühlemann K. Mumps. Lancet. 2008; 371: 932–44. [DOI] [PubMed] [Google Scholar]
- 30. Stein RT, Bont LJ, Zar H et al. Respiratory syncytial virus hospitalization and mortality: Systematic review and meta‐analysis. Pediatr. Pulmonol. 2017; 52: 556–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lynch JP, Kajon AE. Adenovirus: Epidemiology, global spread of novel serotypes, and advances in treatment and prevention. Semin. Respir. Crit. Care Med. 2016; 37: 586–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sauerbrei A, Pd O, Sauerbrei A. Varicella‐zoster virus infections in pregnancy. Intervirology. 1998; 41(4–5): 191–96. Available from: http://biomednet.com/karger [Cited 8 September 2020] [DOI] [PubMed] [Google Scholar]
- 33. Young NS, Brown KE. Parvovirus B19. N. Engl. J. Med. 2004; 350: 586–97. [DOI] [PubMed] [Google Scholar]
- 34. Rawson H, Crampin A, Noah N. Deaths from chickenpox in England and Wales 1995–7: Analysis of routine mortality data. BMJ 2001; 323(7321): 1091–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Walger P, Heininger U, Knuf M et al. Children and adolescents in the CoVid‐19 pandemic: Schools and daycare centers are to be opened again without restrictions. The protection of teachers, educators, carers and parents and the general hygiene rules do not conflict with this. GMS Hyg. Infect. Control 2020; 15: Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. World Health Organization . Advice on the use of masks for children in the community in the context of COVID‐19. [Cited 9 September 2020]. Available from: https://www.who.int/publications/i/item/WHO‐2019‐nCoV‐IPC_Masks‐Children‐2020.1 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The total child population (0–14 years old) in Japan.
Table S2. The effects of each independent variable on the number of cases per week per sentinel site in the sensitivity analysis.


