Abstract
Aims and objectives
To synthesise evidence regarding vaccination intention, identify factors contributing to vaccine hesitancy among healthcare professionals and the general populations globally.
Background
As COVID‐19 vaccine becomes available worldwide, attention is being directed to community vaccine uptake, to achieve population‐wide immunity. A number of factors have been reported to influence vaccine intention.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines, a systematic search of COVID‐19 vaccination intention related literature published on or before 31 December 2020 from seven databases was undertaken.
Results
Thirty articles were included in this systematic review. Overall COVID‐19 vaccination intention during the first year of the pandemic ranged from 27.7% to 93.3%. Findings highlighted that socio‐demographic differences, perceptions of risk and susceptibility to COVID‐19 and vaccine attributes influenced vaccination intention. Healthcare professionals particularly, nurses have higher vaccine hesitancy reportedly due to concerns regarding vaccine safety and efficacy and mistrust of health authorities. Negative information about COVID‐19 vaccines in the social media and low confidence in the health system were associated with lower acceptability among the community. Interestingly, cumulative increase in COVID‐19 caseloads of countries over time was not associated with vaccination intention.
Conclusions
The significant variability in vaccine intention rates worldwide would hamper efforts to achieve immunity against COVID‐19. Nurses’ concerns about vaccine safety and efficacy need to be addressed to increase vaccine acceptance and maximise their influence on vaccination decision in the community. As misinformation through social media negatively impacts vaccination uptake, authoritative and reliable information on vaccine attributes, disease risks and vaccination benefits are needed.
Relevance to clinical practice
Concerns about vaccine safety and efficacy including misinformation are important contributors to vaccine hesitancy. Addressing these factors, particularly among nurses who are considered trusted influencers of vaccination decisions in the community is an important strategy for pandemic preparedness.
Keywords: coronavirus, COVID‐19, vaccination, vaccine acceptance, vaccine hesitancy, vaccine uptake
What does this paper contribute to the wider global clinical community?
COVID‐19 vaccine intention in the first year of the pandemic was 27.7% to 93.3%. The low rate in some countries would hamper efforts to achieve herd immunity.
Nurses and nursing assistants were found to have higher vaccine hesitancy than other healthcare professionals.
Media misinformation, particularly from social media, remains a challenge to vaccination uptake.
1. INTRODUCTION
The emergence of SARS‐CoV‐2 in the latter part of 2019 is perhaps the biggest health threat in living memory. This novel coronavirus that causes COVID‐19, remains a significant threat to life (Fauci et al., 2020). The rapid spread of this disease has caused substantial burden on morbidity and mortality, particularly among older people, causing a need to quarantine and physical distance to reduce transmission. In addition, restriction measures have contributed to a major global economic downturn (Mehta, 2020). The cataclysmic impact of the COVID‐19 pandemic on health and economy globally has contributed to an unprecedented pace in COVID‐19 vaccine development to gain herd immunity.
Effective vaccine development usually takes an average of 10 years, but in the case of COVID‐19 vaccines, 10 were developed and were being tested in clinical trials by June 2020. Of these, two received Emergency Use Authorization in December 2020 to be rolled out before the end of 2020 (Mullard, 2020). Despite this unprecedented success in vaccine development, convincing the population to accept vaccination against COVID‐19 remains a major challenge (World Health Organization, 2021). Vaccination intention can be broadly defined to include willingness to be vaccinated, vaccine acceptability including desirability, vaccine demand and positive attitudes towards the given vaccine, which is contrasted to vaccine resistance, the refusal to be vaccinated (Gates et al., 2021). Of most concern to public health is the issue of vaccine hesitancy, which can be defined as indecision, reluctance or concerns regarding vaccination for oneself or loved ones or delay in the uptake of vaccines (Dubé et al., 2013). This indecision or reluctance towards COVID‐19 vaccination can severely jeopardise herd immunity, which is the indirect protection conferred on vulnerable populations when a sufficiently large number of individuals who are immune to the disease within a population (Randolph & Barreiro, 2020). Therefore, as the race to COVID‐19 vaccine development is reaching the finish line, attention is now focused on community vaccine uptake, to achieve population‐wide immunity. Pivotal in this effort is vaccine acceptance among healthcare professionals, particularly nurses, who are at the frontline of health care to promote vaccine acceptance by the public.
A range of factors are known to influence vaccination intention, which include personal socio‐demographic characteristics, individual beliefs and experiences, to broader external or organisational factors (Dube et al., 2015). Among parents from minority populations, willingness to have their children vaccinated has been influenced by concerns regarding the threat of the infection, perceived susceptibility of their children and confidence of vaccine effectiveness (Frew et al., 2011). In relation to COVID‐19 vaccine uptake intention, there have been several studies published in 2020 alone, focusing on the general public, healthcare workers, as well as on specific at‐risk groups. The aim of this review was to assess intention to receive a COVID‐19 vaccine, and to identify factors shown to be associated with vaccine acceptability. Additionally, this review also aimed to examine if the vaccination intention among nurses and other healthcare professionals were significantly different from that of the community in general. Findings from this review will contribute to understanding the challenges related to vaccine hesitancy across all population groups, and explore strategies to overcome these challenges.
2. METHODS
This review was designed to explore COVID‐19 vaccination intention of any people 18 years and above, and factors that influence uptake intention. This review was undertaken using the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines (see Supporting Information; Liberati et al., 2009) and followed a pre‐defined protocol (PROSPERO #CRD42020224269).
2.1. Search terms and strategies
The search strategy for this study was tailored to each database according to the indexing terms, including Medical Subject Headings (MeSH), truncations and Boolean operators. A combination of terms for the concepts of COVID‐19 (SARS‐CoV‐2, novel coronavirus, coronavirus), vaccine (vaccination, inoculation and immunisation) and intention (attitude, acceptance, barriers, hesitancy, perception, refusal, uptake, utilisation and willingness) were used. In total, seven databases were searched CINAHL, Cochrane Library, Google Scholar, ProQuest, PsycINFO, PubMed and Scopus. Database searches commenced from 17 December 2020, and the date of the last search was performed on 31 December 2020. The reference lists of included studies were also reviewed for inclusion, as well as recent citations of the included studies. Any alerts of studies published before 31 December 2020 were included.
2.2. Inclusion and exclusion criteria
Studies that aimed to investigate attitude and perceptions of people towards COVID‐19 vaccine were included. These included studies that used cross‐sectional, observational or qualitative approaches that focused on COVID‐19 vaccination intention. In addition to the three key concepts (COVID‐19, vaccine and intention), all population groups were included. Studies published in languages other than English and Arabic were excluded from this review. Pre‐print references with no evidence of acceptance by peer‐reviewed journals up to 31 December 2020 were excluded from this review.
2.3. Screening
All records retrieved from the seven databases that met the inclusion criteria were downloaded using the reference management software, EndNote Version X9.0. Following removal of duplicate references, two authors (DM and YS) screened to exclude irrelevant records, firstly by title and then by abstract. Upon completion of this process, the full text of the remaining references was sourced and screened for inclusion in this systematic review (Figure 1).
FIGURE 1.
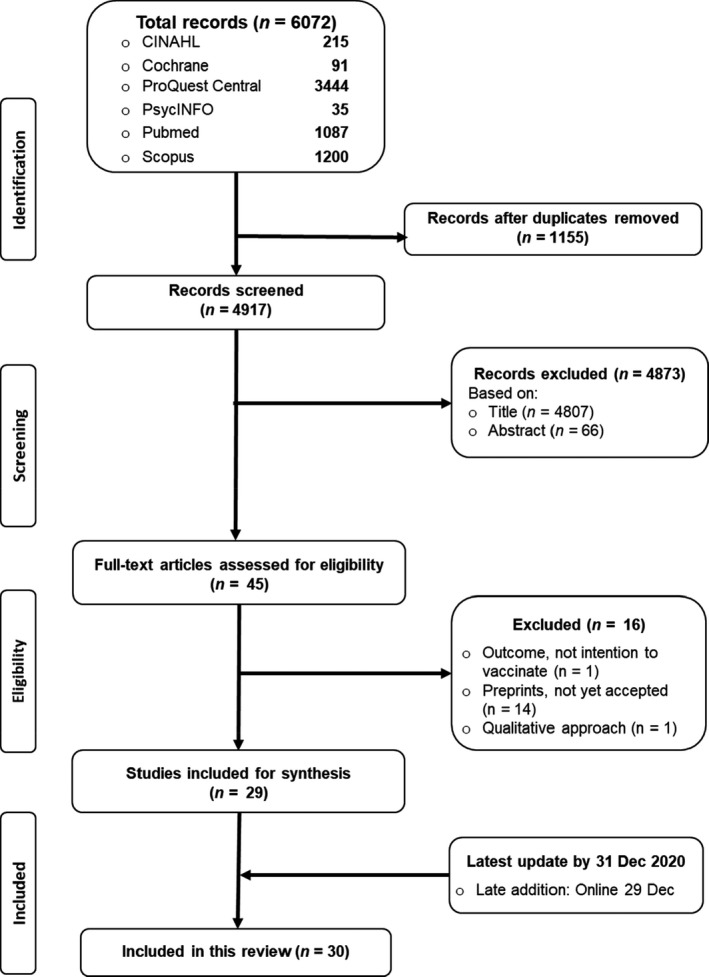
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow chart for the systematic review
2.4. Data extraction
We developed and pilot tested a data extraction form, which was tested by three authors (BE, JM and YS). Following testing and agreement of the included fields (author, year, country, aim, study design, sample size, key measures, results and comments), the same three authors undertook data extraction for all 30 studies. Data were also sourced from the Worldometer (COVID‐19 Coronavirus Pandemic 2020, 2020), from March to December 2020, to extract the ‘total COVID‐19 cases per 1 million population’ daily information of the relevant country, at the commencement and completion of data collection for each of the studies.
2.4.1. Risk of bias
The Joanna Briggs Institute critical appraisal tools for quasi‐experimental design (The Joanna Briggs Institute, 2017) were used to conduct quality assessment and to assess for risk of bias. Each study was assessed independently by two authors (RA and DM). In cases of disagreement on any of the criteria, the assessment of a third author (BE) was sought. The results of the quality assessments of all 30 studies are summarised in Table 1. The assessment score of each study was aggregated, using quality appraisal categories previously reported (Goldsmith et al., 2007; Villarosa et al., 2019). In total, 16 of 30 (54%) studies were rated to be above 80% (high quality), 10 of 30 (33%) studies were within the range of 60%–79% (moderate quality), and 3 of 30 (13%) studies were appraised as poor quality (30%–59%).
TABLE 1.
Summary of included studies published in 2020 on COVID‐19 vaccination intention
| Author, year and country | Aim/research question and study design | Sample and key measures | Results | Comments | |
|---|---|---|---|---|---|
| 1 |
Al‐Mohaithef and Padhi (2020) Saudi Arabia |
Aim To assess the prevalence of COVID‐19 vaccine acceptance and their determinants among people in Saudi Arabia Study design Cross‐sectional study of participants from Saudi Arabia recruited through social media and snowball sampling |
Sample size n = 992 (no specified date of recruitment but stated that it was during the lockdown period)
Key measures
|
|
|
| 2 |
Barello et al. (2020) Italy (69% from Lombardy and Lazio) |
Aim To explore students’ attitudes towards a future vaccine to prevent COVID‐19 To evaluate the impact of healthcare versus non‐healthcare curricula on the intention to vaccinate Study design Cross‐sectional study of Italian university students recruited through university mailing lists |
Sample size N = 934 (81% response rate) n = 551 healthcare students n = 383 non‐healthcare students Key measures Intention to vaccinate |
|
|
| 3 |
Bertin et al. (2020) France |
Aim To explore the relationship between COVID‐19 conspiracy beliefs and attitudes towards vaccines science To examine the relationship of conspiracy beliefs with the intention to be vaccinated against COVID‐19 Study design Two cross‐sectional studies Participants: In Study 1: Social media users; French participants In Study 2: undergraduate university students and social media users (France) |
Sample size Study 1: n = 409 (recruited 2 days after official lockdown in France to 27 March 2020) Study 2: n = 396 (not reported when recruitment occurred, but indicated it was post‐Study 1) Key measures Study 1:
Study 2:
|
Study 1:
Study 2:
|
Limitations:
Strength:
|
| 4 |
Bogart et al. (2020) USA |
Aim To examine relationships between mistrust with COVID‐19 vaccine and antiretroviral (ART) adherence among HIV‐positive Black Americans Study design Cross‐sectional study of participants from a parent study of Black Americans living with HIV in the community |
Sample size n = 103 (recruited between May and July 2020)
Key measures
|
|
|
| 5 |
Dodd et al. (2020) Australia |
Aim To examine actions or intentions towards flu vaccine and a potential COVID‐19 vaccine Study design Cross‐sectional online survey in Australia |
Sample size n = 4,362 Australians (April 17–21, 4 weeks after lockdown measures)
Key measures
|
|
|
| 6 |
Dong et al. (2020) China |
Aim To examine how factors related to vaccine characteristics, their social normative influence and convenience of vaccination can affect the public's preference for the uptake of the COVID‐19 vaccine in China Study design Cross‐sectional online survey to general Chinese population via WJX (survey company) |
Sample size n = 1,236
Key measures
|
|
|
| 7 |
Dror et al. (2020) Israel |
Aim To examine acceptance of COVID‐19 vaccine among health care workers and the general public in Israel population Study design Cross‐sectional survey |
Sample size n = 1,941
Key measures
|
|
|
| 8 |
Fisher et al. (2020) USA |
Aim To assess intent to be vaccinated against COVID‐19 among a representative sample of adults in the United States and identify predictors of and reasons for vaccine hesitancy Study design Cross‐sectional survey via Amerispeak survey company |
Sample size n = 991 (16–20 April 2020)
Key measures
|
|
|
| 9 |
Freeman et al. (2020) United Kingdom |
Aim To estimate provisional willingness to receive a COVID‐19 vaccine To identify predictive socio‐demographic factors Study design Cross‐sectional survey via market research company |
Sample size n = 5,114 adults (18+ years old) was conducted from 24 September to 17 October 2020 Key measures Intent to be vaccinated against COVID‐19; a yes or no question |
|
|
| 10 |
Gagneux‐Brunon et al. (2020) France |
Aim To determine COVID‐19, 24 vaccine acceptance rate of healthcare workers in France Study design Cross‐sectional online survey |
Sample size n = 2,047 (26 March–2 July 2020) Key measures The intention to get vaccinated against COVID‐19 if the vaccine was available |
|
|
| 11 |
Goldman et al. (2020) United States, Canada, Israel, Japan, Spain, and Switzerland |
Aim To investigate predictors associated with global caregivers’ intent to vaccinate their children against COVID‐19, when the vaccine becomes available Study design Cross‐sectional survey of caregivers arriving with their children to 16 Paediatric Emergency Departments (ED) across six countries (United States, Canada, Israel, Japan, Spain, and Switzerland) |
Sample size n = 1,541 (26 March–31 May 2020) Key measures The intention to vaccinate their children against COVID‐19 |
|
|
| 12 |
Graffigna et al. (2020) Italy |
Aim To understand how adult citizens’ health engagement, perceived COVID‐19 susceptibility and severity, and general vaccine‐related attitudes affect the willingness to vaccinate against COVID‐19 Study design Cross‐sectional survey of Italian adult citizens (18 years old and above) using online survey panel provider Norstat Italia srl |
Sample size n = 1,004 (early days of reopening after the lockdown/phase 2) Key measures Health engagement Vaccine attitude (VAs) Perceived severity and susceptibility to COVID‐19 Willingness to vaccinate (5‐point Likert Scale) |
|
|
| 13 |
Grech et al. (2020) Malta |
Aim To examine the degree of COVID‐19 vaccine hesitancy among GPs and GP trainees in Malta Study design Cross‐sectional mail‐out survey to medical doctors listed on the ‘Malta College of Family Doctors’ register |
Sample size n = 123 (recruited between 25 and 29 September 2020)
Key measures
A 5‐item scale on the likelihood of taking the COVID‐19 vaccine |
|
|
| 14 |
Grüner and Krüger (2020) Germany |
Aim To assess psychosocial predictors of COVID−19 vaccine uptake intention Study design Cross‐sectional online survey administered by the survey research firm Qualtrics |
Sample size
n = 2,077 (18 May to 2 August 2020) recruited from universities in Germany
Key measures
|
|
|
| 15 |
Guidry et al. (2020) USA |
Aim To assess the psychosocial predictors of COVID‐19 vaccine uptake intention under Emergency Use Authorisation (EUA) Study design Cross‐sectional online survey of adults administered by the survey research firm Qualtrics |
Sample size n = 788 in July 2020
Key measures
|
|
|
| 16 |
Harapan et al. (2020) Indonesia |
Aim To assess the acceptance of a 50%–95% efficacious COVID‐19 vaccine when available Study design Cross‐sectional online survey using Google Forms distributed on the WhatsApp communication platform |
Sample size Adult population (n = 1,359) collected between 25 March and 6 April 2020
Key measures
|
|
|
| 17 |
Head et al. (2020) USA |
Aims
Study design Cross‐sectional online survey facilitated by market research firm, Dynata, data collected 4–11 May 2020 |
Sample size Adult population (n = 3,159)
Key measures
|
|
|
| 18 |
Kabamba Nzaji et al. (2020) Republic of Congo |
Aim To assess the acceptability of COVID‐19 vaccine among healthcare workers (HCWs) Study design Cross‐sectional survey—self‐administered |
Sample size Healthcare workers (n = 613) collected between 20 March and 30 April 2020 (from 23 hospitals in Congo)
Key measures
|
|
|
| 19 |
Kreps et al. (2020) USA |
Aim To examine factors associated with likelihood of receiving hypothetical COVID‐19 vaccine (Vaccine A, B, or none) Study design Cross‐sectional online survey, recruited from contacting 3,708 US adults through the Lucid platform |
Sample size Adult population (n = 1,971) collected on 9 July 2020
Key measures
|
|
|
| 20 |
La Vecchia et al. (2020) Italy |
Aim To examine intention to be vaccinated against COVID‐19 Study design Cross‐sectional online survey, recruited using Computer Assisted Web Interviews (CAWI) |
Sample size National survey of Italian population (n = 1,055) recruited between 16 and 28 September 2020
Key measures
|
|
|
| 21 |
Lazarus et al. (2020) Total: 19 countries (China, Nigeria, South Korea, India, Poland, Mexico, South Africa, Germany, Canada, Ecuador, France, Russia, Italy, United Kingdom, Brazil, Sweden, Spain, Singapore, United States of America) |
Aim To determine potential acceptance of COVID‐19 vaccination Study design Cross‐sectional survey of vaccine acceptance across 19 countries (recruitment procedure not reported). No report of any translation of questionnaire procedure |
Sample size Survey of 19 countries (n = 13,426) recruited between June 2020 Key measures Age category, sex, income level, education level, vaccination acceptance level, acceptance level with employer's recommendation |
|
|
| 22 |
Malik et al. (2020) USA |
Aim
Study design Cross‐sectional online survey via CloudResearch, an online survey platform |
Sample size n = 672 USA adults surveyed in May 2020
Key measures
|
|
|
| 23 |
Palamenghi et al. (2020) Italy |
Aim To understand citizens’ perceptions and behaviours about preventive behaviours and willingness to vaccinate for COVID‐19 Study design Two cross‐sectional online surveys through Norstat Italia, srl (professional survey company) |
Sample size Sample 1: n = 968 Italian citizens, surveyed during the early days after the initial spread of the SARS‐COV‐2 virus in Italy Sample 2: n = 1,004 Italian citizens, surveyed during the early days of the Italian reopening after lockdown
Key measures
|
|
|
| 24 |
Pogue et al. (2020) USA |
Aim To understand the attitudes towards and obstacles facing COVID‐19 vaccination Research design Cross‐sectional online survey administered by Qualtrics |
Sample Online survey of n = 316 adults Date of survey unclear but likely August–September 2020
Key measures
|
|
|
| 25 |
Reiter et al. (2020) USA |
Aim To determine acceptability of a COVID‐19 vaccine Research design Cross‐sectional online survey administered through survey company, SSRS |
Sample: Convenience sample of n = 2,006 US adults in May 2020 Key measures COVID‐19 vaccination willingness (5‐point Likert ranging from definitely not/definitely will) Knowledge, Attitudes, Beliefs: 14‐items Self‐efficacy: 2‐items Demographic and Health‐Related Characteristics: gender, age, race/ethnicity, marital status, education level, household income, political leaning, religiosity, sexual identity, urbanicity, region of residence, health insurance, underlying medical condition, ever tested for/history of COVID |
|
|
| 26 |
Sherman et al. (2020) UK |
Aim To investigate factors associated with intention to be vaccinated against COVID‐19 Research design Cross‐sectional online survey administered through survey company, Prolific |
Sample: Convenience sample of n = 1,500 UK adults recruited between 14 and 17 July 2020 Key measures Personal and clinical characteristics: sex, age, religion, highest qualification, employment, key worker, household income, vulnerable others in home, influenza vaccination previous winter general beliefs and attitudes relating to vaccination, COVID‐19 illness, COVID‐19 vaccination vaccination intention (when a vaccine becomes available) (primary outcome) |
|
|
| 27 |
Szilagyi et al. (2020) USA |
Aim To track the likelihood of COVID‐19 vaccine uptake, from March to December 2020 Research design Longitudinal online survey recruited using address‐based sampling |
Sample Beginning 10 March 2020, the entire ‘Understanding America Study (UAS) panel with approximately 9,000 US non‐institutionalised adults were invited to participate in biweekly tracking surveys about COVID‐19; consenting respondents are invited on a rolling basis (590 invited daily) to complete the survey Key measures Age, sex, age, ethnicity, highest educational qualification, likelihood of vaccine uptake |
|
|
| 28 |
Wang et al. (2020) Hong Kong, China |
Aim To examine the impact of the COVID‐19 pandemic on change of influenza vaccination acceptance and identify factors associated with acceptance of potential COVID‐19 vaccination Research design Cross‐sectional online survey |
Sample N = 806 nurses recruited by email through membership of Association of Hong Kong Nursing Staff between 26 February and 31 March 2020 Key measures vaccination‐related intentions and behaviours (previous seasonal influenza vaccination; intention to accept seasonal influenza vaccination in current year; intention to accept COVID‐19 vaccination when available) work‐related factors (high‐risk and non‐risk setting; public/private sector; encountered suspected/confirmed COVID‐19; perception of likelihood of being infected) demographics (age, gender, having chronic condition) |
|
|
| 29 |
Williams et al. (2020) UK |
Aim (a) To identify and understand the barriers and facilitators to receiving a future COVID‐19 vaccine; (b) to provide recommendations for the design of interventions aimed at maximising uptake of the vaccine among the public Study design Cross‐sectional online survey |
Sample N = 527 UK adults recruited between 1 and 10 April 2020. Participants were recruited through two ongoing projects examining vaccination behaviour more broadly Key measures Perceptions of COVID‐19 COVID‐19 vaccination intention Influence of COVID‐19 on future vaccination behaviour |
|
|
| 30 |
Zhang et al. (2020) China |
Aim To investigate parental acceptability of free COVID‐19 vaccination for children under the age of 18 years Study design Secondary analysis of cross‐sectional closed online survey |
Sample N = 1,052 parents of at least one child <18 years of age Key measures Sociodemographic characteristics: parental history of seasonal influenza vaccination, and whether they had a family member with a history of COVID‐19 Parental acceptability of free COVID‐19 vaccination for children under 18 years Perceptions related to COVID‐19 vaccination Influence of social media |
|
|
2.5. Data analysis
Characteristics of all studies were summarised, including country of study, sample, period of data collection, levels of COVID‐19 vaccination intention and key factors influencing this intention. Due to the heterogeneity in measurement of vaccination intention, synthesis of this outcome measure was included in the results section. The process of grouping similar textual description and similar data types were undertaken to provide a valid and meaningful narrative that address the review aims. COVID‐19 spread in each country, as indicated by the total confirmed COVID‐19 cases per 1 million population, retrieved from the Worldometer live update (COVID‐19 Coronavirus Pandemic 2020). A mean value of total COVID‐19 cases at two time points was used, at commencement and at completion of data collection in each study.
3. RESULTS
3.1. Characteristics of included studies
Data collection in 14 of the 30 included studies was administered by a commercial survey panel provider (Dong et al., 2020; Fisher et al., 2020; Freeman et al., 2020; Graffigna et al., 2020; Grüner & Krüger, 2020; Guidry et al., 2020; Head et al., 2020; Kreps et al., 2020; La Vecchia et al., 2020; Malik et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Reiter et al., 2020). Following the completion of the search and screening process, 30 studies met the criteria for inclusion in this review (Figure 1) and are summarised in Table 1. None of these were published in Arabic. Of the 30 studies, nine were undertaken in the United States (Bogart et al., 2020; Fisher et al., 2020; Guidry et al., 2020; Head et al., 2020; Kreps et al., 2020; Malik et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Szilagyi et al., 2020), four in Italy (Barello et al., 2020; Graffigna et al., 2020; La Vecchia et al., 2020; Palamenghi et al., 2020), three in the United Kingdom (Freeman et al., 2020; Sherman et al., 2020; Williams et al., 2020), two in France (Bertin et al., 2020; Gagneux‐Brunon et al., 2020), two in mainland China (Dong et al., 2020; Zhang et al., 2020) and one each from Australia (Dodd et al., 2020), Congo (Kabamba Nzaji et al., 2020), Germany (Grüner & Krüger, 2020), Hong Kong (Wang et al., 2020), Indonesia (Harapan et al., 2020), Israel (Dror et al., 2020), Malta (Grech et al., 2020) and Saudi Arabia (Al‐Mohaithef & Padhi, 2020). Two studies surveyed respondents across six (Goldman et al., 2020) to 19 countries (Lazarus et al., 2020). Except for one study that surveyed respondents at 16‐time points (Szilagyi et al., 2020), the remaining 29 studies used a cross‐sectional survey design. Time periods of surveys varied from early during the COVID‐19 pandemic up to April 2020 (Bertin et al., 2020; Dodd et al., 2020; Dror et al., 2020; Fisher et al., 2020; Harapan et al., 2020; Kabamba Nzaji et al., 2020; Wang et al., 2020; Williams et al., 2020), from May to August 2020 (Bogart et al., 2020; Dong et al., 2020; Gagneux‐Brunon et al., 2020; Grüner & Krüger, 2020; Guidry et al., 2020; Head et al., 2020; Kreps et al., 2020; Lazarus et al., 2020; Malik et al., 2020; Reiter et al., 2020; Sherman et al., 2020), and from September to December (Freeman et al., 2020; Grech et al., 2020; La Vecchia et al., 2020; Pogue et al., 2020; Zhang et al., 2020). Four studies did not include the time period of data collection (Al‐Mohaithef & Padhi, 2020; Barello et al., 2020; Graffigna et al., 2020; Palamenghi et al., 2020).
Two‐thirds (20 of 30) of the included studies focused on the general public living in each of the respective countries (Al‐Mohaithef & Padhi, 2020; Bertin et al., 2020; Dodd et al., 2020; Dong et al., 2020; Fisher et al., 2020; Freeman et al., 2020; Graffigna et al., 2020; Guidry et al., 2020; Harapan et al., 2020; Head et al., 2020; Kabamba Nzaji et al., 2020; Kreps et al., 2020; La Vecchia et al., 2020; Lazarus et al., 2020; Malik et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Sherman et al., 2020; Szilagyi et al., 2020). Three focused on students in higher education (Barello et al., 2020; Bertin et al., 2020; Grüner & Krüger, 2020), and two collected data exclusively from parents or caregivers, and focused on their intended uptake of vaccine for their children against COVID‐19 (Goldman et al., 2020; Zhang et al., 2020). One on HIV‐positive Black Americans (Bogart et al., 2020), and another on older adults or patients with chronic respiratory disease (Williams et al., 2020).
3.2. COVID‐19 vaccination intention and variability in intention assessment
Except for one study that assessed preference for the types of hypothetical COVID‐19 vaccines (Dong et al., 2020), the remaining 29 studies measured vaccination intention using a range of approaches. Six studies used a two (e.g. ‘Yes’ or ‘No’) category response format (Dror et al., 2020; Gagneux‐Brunon et al., 2020; Goldman et al., 2020; Grüner & Krüger, 2020; Harapan et al., 2020; Kabamba Nzaji et al., 2020), five studies used a three (e.g. ‘Yes’, ‘No’ or ‘Unsure’) category response format (Al‐Mohaithef & Padhi, 2020; Barello et al., 2020; Dodd et al., 2020; Fisher et al., 2020; Wang et al., 2020), and one study used a four (‘Yes’, ‘Probably Yes’, ‘Probably No’, ‘No’) category response format (La Vecchia et al., 2020). The remaining 17 studies used a 5‐ to 11‐point Likert response format.
In total, 11 studies that used the 5‐point Likert response format, eight collapsed the first two positive categories of a 5‐point Likert response format to indicate vaccination intention (Grech et al., 2020; Lazarus et al., 2020; Malik et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Szilagyi et al., 2020; Zhang et al., 2020), two computed an average score to indicate vaccination intention percentages (Bogart et al., 2020; Freeman et al., 2020), and one reported the scores of all five categories (Graffigna et al., 2020). Two studies that used a 6‐point Likert response format also did not collapse category scores and reported scores for all six categories (Guidry et al., 2020; Williams et al., 2020), and three studies used a 7‐point Likert response format and computed an average score to indicate vaccination intention percentages (Bertin et al., 2020; Head et al., 2020; Kreps et al., 2020). One study used an 11‐point Likert scale and aggregated the first 3 categories to indicate vaccination intention (Sherman et al., 2020).
Overall vaccination intention percentages for COVID‐19 ranged from as low as 27.7% (Kabamba Nzaji et al., 2020) to 93.3% (Harapan et al., 2020). In the one USA study that examined national trends in acceptability of COVID‐19 vaccine from April to November 2020, there was an overall decline in vaccination intention over time, from 74% to 56% (Szilagyi et al., 2020).
3.3. Factors influencing COVID‐19 vaccination intention
Studies included in this review also identified factors influencing COVID‐19 vaccine uptake intention, which were categorised into five categories: (a) socio‐demographic differences; (b) health literacy and COVID‐19 information sources; (c) perceived risk or perceived susceptibility of COVID‐19; (d) vaccine attributes, and speed of vaccine development; and (e) regional increase in cumulative COVID‐19 caseloads over time.
3.3.1. Socio‐demographic differences in vaccination intention
Of the 30 studies, 12 found that those in older age groups were more likely to express willingness to be vaccinated against COVID‐19 (Al‐Mohaithef & Padhi, 2020; Fisher et al., 2020; Freeman et al., 2020; Gagneux‐Brunon et al., 2020; Grech et al., 2020; Kabamba Nzaji et al., 2020; La Vecchia et al., 2020; Lazarus et al., 2020; Malik et al., 2020; Palamenghi et al., 2020; Sherman et al., 2020; Szilagyi et al., 2020), in contrast, three studies found higher vaccine acceptance among those in the younger age group (Guidry et al., 2020; Harapan et al., 2020; Kreps et al., 2020). In relation to gender, 11 studies found that men were more likely to express acceptance of COVID‐19 vaccine compared to women (Dror et al., 2020; Freeman et al., 2020; Gagneux‐Brunon et al., 2020; Grüner & Krüger, 2020; Guidry et al., 2020; Kabamba Nzaji et al., 2020; Kreps et al., 2020; Malik et al., 2020; Reiter et al., 2020; Szilagyi et al., 2020; Wang et al., 2020). This was also the case if fathers were the designated respondents to a caregiver survey, about their intention to accept COVID‐19 vaccine for their child (Goldman et al., 2020). Among racial and ethnic groups, lower COVID‐19 vaccination intention was reported among Black Americans and those of ethnic minority backgrounds (Fisher et al., 2020; Freeman et al., 2020; Guidry et al., 2020; Kreps et al., 2020; Malik et al., 2020; Reiter et al., 2020; Szilagyi et al., 2020). In contrast, two USA studies reported that those of Asian descent had higher intention to COVID‐19 vaccination compared to other racial and ethnic minority groups (Malik et al., 2020; Szilagyi et al., 2020). In another study that sampled populations from 19 countries (Lazarus et al., 2020), respondents living in China reported the highest positive COVID‐19 acceptance percentage (88.6%).
Among studies that assessed educational attainment, 10 reported COVID‐19 vaccination intention was lower among those with lower education levels (Al‐Mohaithef & Padhi, 2020; Dodd et al., 2020; Fisher et al., 2020; Freeman et al., 2020; Guidry et al., 2020; Head et al., 2020; Kreps et al., 2020; La Vecchia et al., 2020; Malik et al., 2020; Szilagyi et al., 2020). Political affiliations were also found to be associated with vaccination intention in three studies, with higher acceptance of COVID‐19 vaccine among those with moderate or liberal political leanings (Head et al., 2020; Kreps et al., 2020; Reiter et al., 2020), although one study did not show any group difference between vaccine uptake and political affiliation (Guidry et al., 2020).
3.3.2. Healthcare workers, nurses and vaccination intention
Nine of the 30 studies included or exclusively focused on healthcare workers (HCWs). Of these, two reported no difference between those in healthcare and the non‐healthcare groups (Barello et al., 2020; Grüner & Krüger, 2020). Although one study reported lower intent to be vaccinated among HCWs compared to the general public (Head et al., 2020), another study reported higher vaccination intention among HCWs (Harapan et al., 2020). Within HCW groups, physicians were consistently reported to have higher intention to be vaccinated against COVID‐19 compared to trainees or other HCWs, including nurses (Dror et al., 2020; Gagneux‐Brunon et al., 2020; Grech et al., 2020; Kabamba Nzaji et al., 2020). In the study that exclusively surveyed nurses, only 40% reported an intention to accept COVID‐19 vaccination (Wang et al., 2020).
3.3.3. Beliefs and COVID‐19 information sources related to vaccination intention
While inadequate health literacy has been shown to be related to COVID‐19 vaccination hesitancy (Dodd et al., 2020; Sherman et al., 2020), high exposure to negative information about COVID‐19 vaccines in the media, particularly social media, was associated with lower acceptability of COVID‐19 vaccination (Bertin et al., 2020; Grüner & Krüger, 2020; Malik et al., 2020; Zhang et al., 2020). Specifically, those with conspiracy beliefs about the vaccine (Bertin et al., 2020; Freeman et al., 2020), and those who reported vaccine mistrust (Bogart et al., 2020; Guidry et al., 2020), expressed reluctance to be vaccinated against COVID‐19.
In contrast, those with high trust in their nation's health system (Al‐Mohaithef & Padhi, 2020), or trust in health‐related information from government bodies (Grüner & Krüger, 2020; Lazarus et al., 2020), were more likely to report willingness to be vaccinated. One USA study reported that endorsements from the Centers for Disease Control and Prevention and World Health Organization were associated with higher vaccination intention (Kreps et al., 2020). Trust in information from scientific research (Palamenghi et al., 2020) and recommendation from their healthcare provider were also associated with willingness to vaccinate against COVID‐19 (Head et al., 2020; Reiter et al., 2020).
Although one study reported that HCWs had higher acceptance of the COVID‐19 vaccine (Harapan et al., 2020), other studies did not find higher vaccination intention among those working in the healthcare industry (Barello et al., 2020; Grüner & Krüger, 2020; Kabamba Nzaji et al., 2020). Of concern, certain health professional groups, including nurses and assistant nurses, consistently reported lower COVID‐19 vaccine acceptance, when compared to the adult population, or other health professional groups (Dror et al., 2020; Gagneux‐Brunon et al., 2020; Kabamba Nzaji et al., 2020; Wang et al., 2020). Two studies showed that medical doctors were more likely to express willingness to be vaccinated against COVID‐19 compared to medical trainees or other HCWs (Grech et al., 2020; Kabamba Nzaji et al., 2020).
3.3.4. Perceived risk and susceptibility to COVID‐19 and vaccination intention, including among vulnerable groups and HCWs
Vaccine acceptance was higher among those who perceived themselves to be at greater risk or threat (e.g. HCWs who were exposed to COVID‐19 patients) of acquiring the infection (Al‐Mohaithef & Padhi, 2020; Dror et al., 2020; Grüner & Krüger, 2020; Harapan et al., 2020; Reiter et al., 2020; Wang et al., 2020; Williams et al., 2020). Additionally, those who perceived themselves to be vulnerable or at greater susceptibility to COVID‐19 (e.g. older age groups or those with chronic health conditions), were also more likely to indicate increased vaccine acceptance (Guidry et al., 2020; Head et al., 2020; Malik et al., 2020; Sherman et al., 2020; Wang et al., 2020). Seven studies included vaccine intention among HCWs (Dror et al., 2020; Gagneux‐Brunon et al., 2020; Harapan et al., 2020; Head et al., 2020; Kabamba Nzaji et al., 2020; Wang et al., 2020) which ranged from 28% to 96%. Nurses were shown to have lower vaccine intention (28%–65%) in half of these studies (Dror et al., 2020; Gagneux‐Brunon et al., 2020; Wang et al., 2020) because of lower perception of personal risk, concerns regarding the vaccine and time constraints.
3.3.5. Vaccine attributes, speed of vaccine development and vaccination intention
Seven studies reported higher acceptance of the COVID‐19 vaccine if respondents had had influenza vaccine in the past (Dror et al., 2020; Fisher et al., 2020; Gagneux‐Brunon et al., 2020; Goldman et al., 2020; Grech et al., 2020; Sherman et al., 2020; Wang et al., 2020). Among those from healthcare backgrounds, two studies reported that they were more likely to receive the influenza vaccine than the COVID‐19 vaccine (Dror et al., 2020; Grüner & Krüger, 2020); however, there was no group difference in COVID‐19 vaccination intention between healthcare professionals and the general population (Grüner & Krüger, 2020). In two studies, concerns about vaccine novelty and the speed of COVID‐19 vaccine development were reasons given for vaccine hesitancy (Freeman et al., 2020; Goldman et al., 2020).
In relation to personal preference of hypothetical types of available COVID‐19 vaccines and vaccination intention, respondents from eight studies indicated effectiveness of vaccine was an important factor influencing vaccine selection or vaccination intention (Dong et al., 2020; Freeman et al., 2020; Harapan et al., 2020; Kreps et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Wang et al., 2020), as was a vaccine with long duration of disease protection (Dong et al., 2020; Kreps et al., 2020; Pogue et al., 2020). Vaccine safety, that is a vaccine with no or few adverse effects, was also a strong determinant influencing willingness to be vaccinated (Dong et al., 2020; Freeman et al., 2020; Kreps et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Sherman et al., 2020; Wang et al., 2020). Furthermore, COVID‐19 vaccines that were developed or manufactured in America or Europe received higher preference ratings compared to those developed in China or Russia (Dong et al., 2020; Kreps et al., 2020; Pogue et al., 2020). Interestingly, in one study, cost of the vaccine was found to be the least important factor in respondents’ vaccine selection (Dong et al., 2020).
3.3.6. Regional increase in cumulative COVID‐19 caseloads over time and vaccination intention
Figure 2 plots the estimated cumulative mean caseloads of COVID‐19 cases per 1 million people in the country retrieved from the Worldometer live update (COVID‐19 Coronavirus Pandemic 2020, 2020), on the day when survey data were collected, against the overall reported COVID‐19 vaccination intention in 23 studies included in this review. Studies that (a) did not specify a data collection period (Al‐Mohaithef & Padhi, 2020; Barello et al., 2020; Graffigna et al., 2020; Palamenghi et al., 2020); (b) included multiple countries (Goldman et al., 2020; Lazarus et al., 2020); and (c) recorded trend over time in a single country (Szilagyi et al., 2020); were excluded in this plot (Figure 2). The time series pattern showed low estimated R of −0.00042, indicating no relationship between cumulative increase in COVID‐19 caseloads and respondents’ vaccination intention. The same and consistent pattern was also found in the study by Lazarus et al. (2020), which collected data from 19 countries in June 2020. Low correlation (R = −.0004) was found between vaccination intention in each country and the cumulative mean COVID‐19 caseloads per 1 million people during the period of data collection in June 2020.
FIGURE 2.
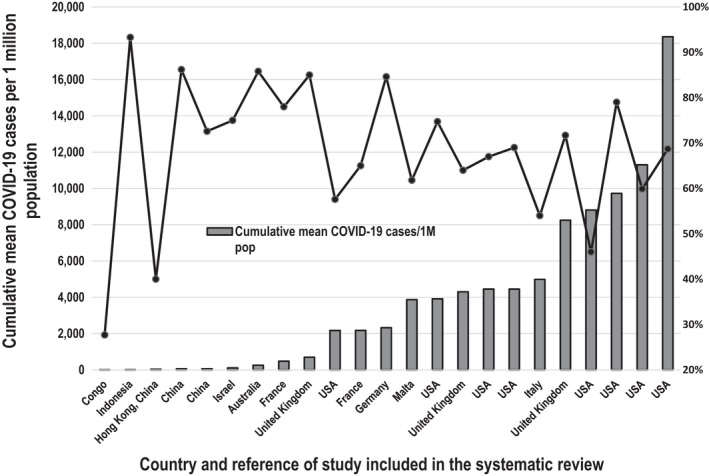
Cumulative mean number of COVID‐19 cases per 1 million population and overall percentages vaccination intention
4. DISCUSSION
As world leaders and public health officials focus on securing sufficient COVID‐19 vaccines and an effective vaccine roll‐out strategy for their population, this review underscores another urgent challenge—to address the variability in COVID‐19 acceptance across socio‐demographic groups, and addressing barriers to vaccine acceptance. Findings of this review on COVID‐19 vaccination intention are consistent with previously reported seasonal influenza vaccination uptake which showed that being older, ethnically White, and having higher educational attainment were associated with higher vaccine acceptance (Okoli et al., 2019). Similarly, the finding that men were more receptive to the COVID‐19 vaccine is consistent with previous investigation on gender differences and vaccine uptake (Flanagan et al., 2017). Some of the reasons postulated were lower level of social support for women and being less open to healthcare recommendations and preventive measures (Jiménez‐García et al., 2010). In contrast to those who underestimated the severity of the disease or showed mistrust in authorities, those who had previously received vaccination for seasonal influenza, and/or expressed higher concern and belief in their susceptibility to the disease were understandably more willing to vaccinate against COVID‐19 (Graffigna et al., 2020).
Vaccine attributes were also found to be crucial in the decision to vaccinate, including effectiveness of the vaccine, long duration of protective effects and optimum safety profile which were also consistent with previous findings, for example, in the study conducted on the H1N1 vaccine during the 2009 influenza A pandemic (Frew et al., 2011). Confidence in the quality of the vaccine was reported to be strengthened by recommendations from reliable sources such as nurses and physicians highlighting the role of HCWs in building public trust. Another important factor that influenced vaccine hesitancy found in this review was the speed of vaccine development which was not surprising considering the novelty of the COVID‐19 virus and the new technologies used, raising uncertainties about the adequacy of research and testing, adversely impacting on perceived efficacy and safety of vaccines (Freeman et al., 2020).
Of concern, this review also highlighted a decline in vaccination intention over a 10‐month span in 2020, which was borne out in two studies, one conducted in the USA (Szilagyi et al., 2020) and the other in Italy (Palamenghi et al., 2020). This decline occurred during a period when confirmed COVID‐19 cases in both countries were consistently among the 10 highest in the world (COVID‐19 Coronavirus Pandemic, 2020, 2020). Nevertheless, this trend is consistent with findings of another study conducted during the 2009–2010 H1N1 pandemic (Gidengil et al., 2012). Postulated reasons for this paradoxical trend of decline in vaccination intention over time could be (a) an overestimation of perceived risk in an unusual event (COVID‐19 pandemic), which declines as more comprehensive understanding of the threat emerges (Gidengil et al., 2012); (b) messaging fatigue, a status of weariness and desensitisation, due to repeated exposure to information about COVID‐19 (Koh et al., 2020); and (c) infodemic, an oversupply of information making it difficult to distinguish between reliable information and misinformation (Zarocostas, 2020). Findings from this review support a need to address the issue of potential ‘crisis of public confidence’ against COVID‐19 vaccination, and to address specific concerns of subpopulation groups, with vaccination messages that are group‐ and context‐specific, to restore confidence in COVID‐19 vaccines (Larson et al., 2011). Although the WHO has established a new information platform to share information tailored for specific target groups since the declaration of the COVID‐19 pandemic (Zarocostas, 2020), findings from this review indicate more work is needed. This need is particularly important, as it has been shown empirically, that undecided or vaccine hesitant groups were more likely to be influenced by the views from minority but well‐organised anti‐vaccination groups, compared to those from pro‐vaccination groups (Johnson et al., 2020). One strategy that has been promoted is psychological inoculation, also known as pre‐bunking, an approach of presenting anti‐conspiracy arguments to counter misinformation about COVID‐19 vaccination, before the general public is exposed to misinformation on vaccination conspiracy theories (van der Linden et al., 2020). Nevertheless, the effectiveness of this strategy against COVID‐19 vaccination intention has yet to be reported.
In addition to highlighting the issues of vaccine intention in different population groups, this review has also highlighted the need for standardisation in measuring vaccine uptake. Differences in terminology used to refer to vaccine intention, heterogeneity in measurement of vaccine acceptance and collapsing responses often into dichotomous categories limit the capacity to undertake precise quantitative comparisons among studies that measured the same construct of vaccination intention. A standardised measure of this construct will enhance accuracy to identify target areas to improve vaccination uptake.
4.1. Limitations
We only included full‐text articles of studies published up until December 2020 and we excluded pre‐print articles that had not yet been peer reviewed. Given the very high rate of COVID‐19 research publications—estimated at 137 publications per day compared to 6 papers per day during the 2009/2010 H1N1 pandemic (Yeo‐Teh & Tang, 2021), it may be that including papers available in pre‐print but not peer‐reviewed at the time of our search may have resulted in different conclusions being drawn. We also only included papers published in English because of the lack of resources to undertake translation which may limit the generalisability of these findings.
5. CONCLUSIONS
This review identified significant variability in vaccine intention rates across countries, ranging from 27.7% to 93.3%, which in some countries would hamper efforts to achieve herd immunity. Nevertheless, factors shown to be associated with vaccine acceptability included being older, male, having higher levels of education, previous receipt of influenza vaccination, perceiving oneself to be at greater risk of exposure or greater susceptibility to COVID‐19, and having high levels of trust in health‐related information from government bodies and healthcare providers. In contrast, high exposure to negative information about COVID‐19 vaccines, particularly in social media, and certain health professional groups including nurses and nursing assistants were associated with lower vaccine acceptability. This review did not support COVID‐19 caseload as a factor associated with vaccination intention rather, it has highlighted a decline in vaccination intention during a period when COVID‐19 have been increasing. More research is needed to understand why nurses have lower rates of vaccine acceptability particularly as they are at higher risk of exposure to COVID‐19 and will be prioritised to receive the vaccine. Addressing methodological issues of measuring vaccine acceptance would be an important step towards an improved evaluation of vaccine intention. Intensive population education programs, in concert with vaccination promotion efforts from health, social and political organisations to address the barriers reported in this review are needed to improve vaccination acceptance.
6. RELEVANCE TO CLINICAL PRACTICE
An important finding of this review was the number of studies showing lower vaccine acceptance among healthcare professionals, particularly among nurses. This is consistent with previous studies that showed that nurses had more concerns with vaccine efficacy and safety, and mistrust in health authorities (Wilson et al., 2020). Given that nurses are considered the most trusted professionals in the community (Milton, 2018), more focus should be given to address their vaccine hesitancy concerns, to enable them to provide informed and authoritative recommendations to the public.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTION
Study conception and design: RA and DM; Data, investigation and methodology: RA, DM, ARV and YS; Data extraction: BE, JM and YS; Performance of the data analysis: YS, BE, JM, ARV, DM and RA; Manuscript draft: RA, DM, YS, BE, JM and ARV; Critical revisions to the paper for important intellectual content: RA, DM, YS, BE, JM and ARV; Supervision of the conduct of the research and the research team: YS.
Supporting information
Supplementary Material
Al‐Amer, R. , Maneze, D. , Everett, B. , Montayre, J. , Villarosa, A. R. , Dwekat, E. , & Salamonson, Y. (2022). COVID‐19 vaccination intention in the first year of the pandemic: A systematic review. Journal of Clinical Nursing, 31, 62–86. 10.1111/jocn.15951
DATA AVAILABILITY STATEMENT
Data are in the table and figures included in the article (Table 1).
REFERENCES
- Al‐Mohaithef, M. , & Padhi, B. K. (2020). Determinants of COVID‐19 vaccine acceptance in Saudi Arabia: A web‐based national survey. Journal of Multidisciplinary Healthcare, 13, 1657–1663. 10.2147/JMDH.S276771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello, S. , Nania, T. , Dellafiore, F. , Graffigna, G. , & Caruso, R. (2020). ‘Vaccine hesitancy’ among university students in Italy during the COVID‐19 pandemic. European Journal of Epidemiology, 35(8), 781–783. 10.1007/s10654-020-00670-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertin, P. , Nera, K. , & Delouvée, S. (2020). Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: A conceptual replication‐extension in the COVID‐19 pandemic context [Article]. Frontiers in Psychology, 11, Article 565128. 10.3389/fpsyg.2020.565128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart, L. M. , Ojikutu, B. O. , Tyagi, K. , Klein, D. J. , Mutchler, M. G. , Dong, L. , Lawrence, S. J. , Thomas, D. , & Kellman, S. (2020). COVID‐19 related medical mistrust, health impacts, and potential vaccine hesitancy among black Americans living with HIV. Journal of Acquired Immune Deficiency Syndromes, 86(2), 200–207. 10.1097/QAI.0000000000002570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd, R. H. , Cvejic, E. , Bonner, C. , Pickles, K. , McCaffery, K. J. , Ayre, J. , Batcup, C. , Copp, T. , Cornell, S. , Dakin, T. , Isautier, J. M. , Nickel, B. , & Sydney Health Literacy Lab, C.‐G. (2020). Willingness to vaccinate against COVID‐19 in Australia. The Lancet Infectious Diseases. 10.1016/S1473-3099(20)30559-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, D. , Xu, R. H. , Wong, E. L. Y. , Hung, C. T. , Feng, D. , Feng, Z. , Yeoh, E. K. , & Wong, S. Y. S. (2020). Public preference for COVID‐19 vaccines in China: A discrete choice experiment. Health Expectations, 23(6), 1543–1578. 10.1111/hex.13140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dror, A. A. , Eisenbach, N. , Taiber, S. , Morozov, N. G. , Mizrachi, M. , Zigron, A. , Srouji, S. , & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID‐19. European Journal of Epidemiology, 35(8), 775–779. 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé, E. , Laberge, C. , Guay, M. , Bramadat, P. , Roy, R. , & Bettinger, J. A. (2013). Vaccine hesitancy: An overview. Human Vaccines & Immunotherapeutics, 9(8), 1763–1773. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube, E. , Vivion, M. , & MacDonald, N. E. (2015). Vaccine hesitancy, vaccine refusal and the anti‐vaccine movement: Influence, impact and implications. Expert Review of Vaccines, 14(1), 99–117. 10.1586/14760584.2015.964212 [DOI] [PubMed] [Google Scholar]
- Fauci, A. S. , Lane, H. C. , & Redfield, R. R. (2020). Covid‐19—Navigating the uncharted. New England Jouranl of Medicine, 382. 10.1056/nejme2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, K. A. , Bloomstone, S. J. , Walder, J. , Crawford, S. , Fouayzi, H. , & Mazor, K. M. (2020). Attitudes toward a potential SARS‐CoV‐2 vaccine: A survey of U.S. adults. Annals of Internal Medicine, 173(12), 964–973. 10.7326/m20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan, K. L. , Fink, A. L. , Plebanski, M. , & Klein, S. L. (2017). Sex and gender differences in the outcomes of vaccination over the life course. Annual Review of Cell and Developmental Biology, 33(1), 577–599. 10.1146/annurev-cellbio-100616-060718 [DOI] [PubMed] [Google Scholar]
- Freeman, D. , Loe, B. S. , Chadwick, A. , Vaccari, C. , Waite, F. , Rosebrock, L. , Jenner, L. , Petit, A. , Lewandowsky, S. , Vanderslott, S. , Innocenti, S. , Larkin, M. , Giubilini, A. , Yu, L. M. , McShane, H. , Pollard, A. J. , & Lambe, S. (2020). COVID‐19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (OCEANS) II. Psychological Medicine, 1–34. 10.1017/s0033291720005188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frew, P. M. , Hixson, B. , del Rio, C. , Esteves‐Jaramillo, A. , & Omer, S. B. (2011). Acceptance of pandemic 2009 Influenza A (H1N1) vaccine in a minority population: Determinants and potential points of intervention. Pediatrics, 127(Suppl. 1), S113. 10.1542/peds.2010-1722Q [DOI] [PubMed] [Google Scholar]
- Gagneux‐Brunon, A. , Detoc, M. , Bruel, S. , Tardy, B. , Rozaire, O. , Frappe, P. , & Botelho‐Nevers, E. (2020). Intention to get vaccinations against COVID‐19 in French healthcare workers during the first pandemic wave: A cross sectional survey. Journal of Hospital Infection. 10.1016/j.jhin.2020.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates, A. , Gates, M. , Rahman, S. , Guitard, S. , MacGregor, T. , Pillay, J. , Ismail, S. J. , Tunis, M. C. , Young, K. , Hardy, K. , Featherstone, R. , & Hartling, L. (2021). A systematic review of factors that influence the acceptability of vaccines among Canadians. Vaccine, 39(2), 222–236. 10.1016/j.vaccine.2020.10.038 [DOI] [PubMed] [Google Scholar]
- Gidengil, C. A. , Parker, A. M. , & Zikmund‐Fisher, B. J. (2012). Trends in risk perceptions and vaccination intentions: A longitudinal study of the first year of the H1N1 pandemic. American Journal of Public Health, 102(4), 672–679. 10.2105/AJPH.2011.300407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D. , Yan, T. D. , Seiler, M. , Parra Cotanda, C. , Brown, J. C. , Klein, E. J. , Hoeffe, J. , Gelernter, R. , Hall, J. E. , Davis, A. L. , Griffiths, M. A. , Mater, A. , Manzano, S. , Gualco, G. , Shimizu, N. , Hurt, T. L. , Ahmed, S. , Hansen, M. , Sheridan, D. , … For the International Covid‐Parental Attitude Study Group . (2020). Caregiver willingness to vaccinate their children against COVID‐19: Cross sectional survey. Vaccine, 38(48), 7668–7673. 10.1016/j.vaccine.2020.09.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith, M. R. , Bankhead, C. R. , & Austoker, J. (2007). Synthesising quantitative and qualitative research in evidence‐based patient information. Journal of Epidemiology and Community Health, 61(3), 262–270. 10.1136/jech.2006.046110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graffigna, G. , Palamenghi, L. , Boccia, S. , & Barello, S. (2020). Relationship between citizens’ health engagement and intention to take the covid‐19 vaccine in Italy: A mediation analysis. Vaccines, 8(4), 1–11. 10.3390/vaccines8040576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, V. , Bonnici, J. , & Zammit, D. (2020). Vaccine hesitancy in Maltese family physicians and their trainees vis‐à‐vis influenza and novel COVID‐19 vaccination. Early Human Development. 10.1016/j.earlhumdev.2020.105259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grüner, S. , & Krüger, F. (2020). The intention to be vaccinated against COVID‐19: Stated preferences before vaccines were available. Applied Economics Letters. 10.1080/13504851.2020.1854445 [DOI] [Google Scholar]
- Guidry, J. P. D. , Laestadius, L. I. , Vraga, E. K. , Miller, C. A. , Perrin, P. B. , Burton, C. W. , Ryan, M. , Fuemmeler, B. F. , & Carlyle, K. E. (2020). Willingness to get the COVID‐19 vaccine with and without emergency use authorization. American Journal of Infection Control. 10.1016/j.ajic.2020.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harapan, H. , Wagner, A. L. , Yufika, A. , Winardi, W. , Anwar, S. , Gan, A. K. , Setiawan, A. M. , Rajamoorthy, Y. , Sofyan, H. , & Mudatsir, M. (2020). Acceptance of a COVID‐19 vaccine in Southeast Asia: A cross‐sectional study in Indonesia. Frontiers in Public Health. 10.3389/fpubh.2020.00381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head, K. J. , Kasting, M. L. , Sturm, L. A. , Hartsock, J. A. , & Zimet, G. D. (2020). A national survey assessing SARS‐CoV‐2 vaccination intentions: Implications for future public health communication efforts. Science Communication, 42(5), 698–723. 10.1177/1075547020960463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez‐García, R. , Hernández‐Barrera, V. , de Andres, A. L. , Jimenez‐Trujillo, I. , Esteban‐Hernández, J. , & Carrasco‐Garrido, P. J. V. (2010). Gender influence in influenza vaccine uptake in Spain: Time trends analysis (1995–2006). Vaccine, 28(38), 6169–6175. 10.1016/j.vaccine.2010.07.029 [DOI] [PubMed] [Google Scholar]
- Johnson, N. F. , Velásquez, N. , Restrepo, N. J. , Leahy, R. , Gabriel, N. , El Oud, S. , Zheng, M. , Manrique, P. , Wuchty, S. , & Lupu, Y. (2020). The online competition between pro‐ and anti‐vaccination views. Nature, 582(7811), 230–233. 10.1038/s41586-020-2281-1 [DOI] [PubMed] [Google Scholar]
- Kabamba Nzaji, M. , Kabamba Ngombe, L. , Ngoie Mwamba, G. , Banza Ndala, D. B. , Mbidi Miema, J. , Luhata Lungoyo, C. , Lora Mwimba, B. , Cikomola Mwana Bene, A. , & Mukamba Musenga, E. (2020). Acceptability of vaccination against COVID‐19 among healthcare workers in the Democratic Republic of the Congo. Pragmatic and Observational Research, 11, 103–109. 10.2147/por.S271096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh, P.‐K.‐K. , Chan, L. L. , & Tan, E.‐K. (2020). Messaging fatigue and desensitisation to information during pandemic. Archives of Medical Research, 51(7), 716–717. 10.1016/j.arcmed.2020.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreps, S. , Prasad, S. , Brownstein, J. S. , Hswen, Y. , Garibaldi, B. T. , Zhang, B. , & Kriner, D. L. (2020). Factors associated with US adults’ likelihood of accepting COVID‐19 vaccination. JAMA Network Open, 3(10), e2025594. 10.1001/jamanetworkopen.2020.25594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Vecchia, C. , Negri, E. , Alicandro, G. , & Scarpino, V. (2020). Attitudes towards influenza vaccine and a potential COVID‐19 vaccine in Italy and differences across occupational groups, September 2020. La Medicina Del Lavoro, 111(6), 445–448. 10.23749/mdl.v111i6.10813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson, H. J. , Cooper, L. Z. , Eskola, J. , Katz, S. L. , & Ratzan, S. (2011). Addressing the vaccine confidence gap. The Lancet, 378(9790), 526–535. 10.1016/S0140-6736(11)60678-8 [DOI] [PubMed] [Google Scholar]
- Lazarus, J. V. , Ratzan, S. C. , Palayew, A. , Gostin, L. O. , Larson, H. J. , Rabin, K. , Kimball, S. , & El‐Mohandes, A. (2020). A global survey of potential acceptance of a COVID‐19 vaccine. Nature Medicine, 27(2), 225–228. 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati, A. , Altman, D. G. , Tetzlaff, J. , Mulrow, C. , Gøtzsche, P. C. , Ioannidis, J. P. , Clarke, M. , Devereaux, P. J. , Kleijnen, J. , & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: Explanation and elaboration. Journal of Clinical Epidemiology, 62(10), e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- Malik, A. A. , McFadden, S. M. , Elharake, J. , & Omer, S. B. (2020). Determinants of COVID‐19 vaccine acceptance in the US. EClinicalMedicine, 26, 100495. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, V. (2020). The new proxemics: COVID‐19, social distancing, and sociable space. Journal of Urban Design, 25(6), 669–674. 10.1080/13574809.2020.1785283 [DOI] [Google Scholar]
- Milton, C. L. (2018). Will nursing continue as the most trusted profession? An ethical overview. Nursing Science Quarterly, 31(1), 15–16. 10.1177/0894318417741099 [DOI] [PubMed] [Google Scholar]
- Mullard, A. (2020). COVID‐19 vaccine development pipeline gears up. The Lancet, 395(10239), 1751–1752. 10.1016/S0140-6736(20)31252-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okoli, G. N. , Abou‐Setta, A. M. , Neilson, C. J. , Chit, A. , Thommes, E. , & Mahmud, S. M. (2019). Determinants of seasonal influenza vaccine uptake among the elderly in the United States: A systematic review and meta‐Analysis. Gerontology and Geriatric Medicine, 5, 2333721419870345. 10.1177/2333721419870345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamenghi, L. , Barello, S. , Boccia, S. , & Graffigna, G. (2020). Mistrust in biomedical research and vaccine hesitancy: The forefront challenge in the battle against COVID‐19 in Italy. European Journal of Epidemiology, 35(8), 785–788. 10.1007/s10654-020-00675-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogue, K. , Jensen, J. L. , Stancil, C. K. , Ferguson, D. G. , Hughes, S. J. , Mello, E. J. , Burgess, R. , Berges, B. K. , Quaye, A. , & Poole, B. D. (2020). Influences on attitudes regarding potential Covid‐19 vaccination in the United States. Vaccines, 8(4), 1–14. 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph, H. E. , & Barreiro, L. B. (2020). Herd Immunity: Understanding COVID‐19. Immunity, 52(5), 737–741. 10.1016/j.immuni.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, P. L. , Pennell, M. L. , & Katz, M. L. (2020). Acceptability of a COVID‐19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine, 38(42), 6500–6507. 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman, S. M. , Smith, L. E. , Sim, J. , Amlôt, R. , Cutts, M. , Dasch, H. , Rubin, G. J. , & Sevdalis, N. (2020). COVID‐19 vaccination intention in the UK: Results from the COVID‐19 vaccination acceptability study (CoVAccS), a nationally representative cross‐sectional survey. Human Vaccines and Immunotherapeutics, 17(6), 1612–1621. 10.1080/21645515.2020.1846397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi, P. G. , Thomas, K. , Shah, M. D. , Vizueta, N. , Cui, Y. , Vangala, S. , & Kapteyn, A. (2020). National trends in the US public’s likelihood of getting a COVID‐19 vaccine—April 1 to December 8, 2020. JAMA Network Open, 325(4), 396. 10.1001/jama.2020.26419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joanna Briggs Institute . (2017). Checklist for quasi‐experimental studies (non‐randomized experimental studies). Retrieved from https://joannabriggs.org/sites/default/files/2020‐08/Checklist_for_Quasi‐Experimental_Appraisal_Tool.pdf
- van der Linden, S. , Roozenbeek, J. , & Compton, J. (2020). Inoculating against fake news about COVID‐19. Frontiers in Psychology, 11, Article 566790. 10.3389/fpsyg.2020.566790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarosa, A. R. , Maneze, D. , Ramjan, L. M. , Srinivas, R. , Camilleri, M. , & George, A. (2019). The effectiveness of guideline implementation strategies in the dental setting: A systematic review. Implementation Science, 14(1), 106. 10.1186/s13012-019-0954-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, K. , Wong, E. L. Y. , Ho, K. F. , Cheung, A. W. L. , Chan, E. Y. Y. , Yeoh, E. K. , & Wong, S. Y. S. (2020). Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross‐sectional survey. Vaccine, 38(45), 7049–7056. 10.1016/j.vaccine.2020.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, L. , Gallant, A. J. , Rasmussen, S. , Brown Nicholls, L. A. , Cogan, N. , Deakin, K. , Young, D. , & Flowers, P. (2020). Towards intervention development to increase the uptake of COVID‐19 vaccination among those at high risk: Outlining evidence‐based and theoretically informed future intervention content. British Journal of Health Psychology, 25(4), 1039–1054. 10.1111/bjhp.12468 [DOI] [PubMed] [Google Scholar]
- Wilson, R. , Zaytseva, A. , Bocquier, A. , Nokri, A. , Fressard, L. , Chamboredon, P. , Carbonaro, C. , Bernardi, S. , Dubé, E. , & Verger, P. (2020). Vaccine hesitancy and self‐vaccination behaviors among nurses in southeastern France. Vaccine, 38(5), 1144–1151. 10.1016/j.vaccine.2019.11.018 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2021). Ten threats to global health in 2019. Retrieved from https://www.who.int/news‐room/spotlight/ten‐threats‐to‐global‐health‐in‐2019 [Google Scholar]
- Worldometer . (2020). COVID‐19 Coronavirus Pandemic 2020. Retrieved from https://www.worldometers.info/coronavirus/
- Yeo‐Teh, N. S. L. , & Tang, B. L. (2021). An alarming retraction rate for scientific publications on coronavirus disease 2019 (COVID‐19). Accountability in Research, 28(1), 47–53. 10.1080/08989621.2020.1782203 [DOI] [PubMed] [Google Scholar]
- Zarocostas, J. (2020). How to fight an infodemic. The Lancet, 395(10225), 676. 10.1016/S0140-6736(20)30461-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, K. C. , Fang, Y. , Cao, H. , Chen, H. , Hu, T. , Chen, Y. Q. , Zhou, X. , & Wang, Z. (2020). Parental acceptability of COVID‐19 vaccination for children under the age of 18 years in China: Cross‐sectional online survey. JMIR Pediatrics and Parenting. 10.2196/24827 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data are in the table and figures included in the article (Table 1).


