Abstract
Background
Individuals aged 65 and older face unique barriers to adoption of telehealth, and the coronavirus disease 2019 pandemic has provided a “natural experiment” in how to meet the health needs of older patients remotely. Physician perspectives on practical considerations surrounding telehealth adoption, motivations of use, and reasons for nonuse are necessary to inform the future of healthcare delivery. The objective is to understand the experiences of physicians using telemedicine for older patients.
Methods
From September to November 2020, we conducted 30‐min semi‐structured interviews using purposeful sampling to identify and enroll participants from diverse settings. We included 48 U.S.‐based physicians (geriatrician, n = 18, primary care, n = 15, emergency, n = 15) from all geographic regions, rural–urban and academic/community settings. Audio‐recorded interviews were professionally transcribed and analyzed using framework analysis. Major themes and subthemes were identified.
Results
Participants had a median (interquartile range) age of 37.5 (34–44.5), 27 (56%) were women. Five major themes emerged: (1) telehealth uptake was rapid and iterative, (2) telehealth improved the safety of medical care, (3) use cases were specialty‐specific (for geriatricians and primary care physicians telehealth substituted for in‐person visits; for emergency physicians it primarily supplemented in‐person visits), (4) physicians altered clinical care to overcome older patient barriers to telehealth use, and (5) telehealth use among physicians declined in mid‐April 2020, due primarily to patient needs and administrator preferences, not physician factors.
Conclusion
In this qualitative analysis, physicians reported a rapid, iterative uptake of telehealth and attenuation of use as coronavirus disease 2019 prevalence declined. Physician experiences during the pandemic can inform interventions and policies to help buoy telehealth for ongoing healthcare delivery and ensure its accessibility for older Americans.
Keywords: COVID‐19, older adults, qualitative methods, telehealth, telemedicine
Key Points
Physicians expressed that telemedicine was essential to provide medical care to older adults during the COVID‐19 pandemic.
Physicians reported assessing older patients' telehealth capacity, altering care delivery, and engaging in team‐based care to overcome older patients' barriers to telehealth use.
Physicians suggested telemedicine would remain an important means of care delivery due to enhanced convenience, staffing flexibility, efficiency, and reduced travel burden.
Why Does this Paper Matter?
Specialty‐dependent and physician‐level factors associated with telehealth adoption and use identified in this study should be considered in the development of interventions and policies aimed at supporting telemedicine for healthcare delivery.
INTRODUCTION
In March 2020, many U.S. physician offices were closed, hospitals reduced nonessential healthcare services, 1 and emergency department (ED) patient volumes plummeted. 2 The abrupt reduction in in‐person healthcare services during the coronavirus disease 2019 (COVID‐19) pandemic resulted in an unplanned and unexpected boon for telehealth, 3 , 4 , 5 whereby the growth of telemedicine offset two‐thirds of the decline in in‐person visit volume. 5 Older adults are disproportionally affected by COVID‐19 6 and may face the greatest challenges with telehealth, yet little is known about how physicians commonly caring for these patients—geriatricians, primary care physicians (PCPs), and emergency medicine (EM) physicians—met their health needs when in‐person visits declined.
Older adults face unique barriers to adoption of telehealth including access, design challenges, privacy and trust concerns, and cost. 7 In 2018, 38% of older Americans were not ready for video visits, and only 80% could handle a telephone visit due to inexperience with technology, physical disability, dementia, or difficulty hearing or communicating. 8 However, older adult technology use has increased in recent years 9 ; older adults who own smartphones doubled between 2011 and 2016 from 35% to 77%, and 67% reported using the internet in 2016. 10 Younger, wealthier, and healthier older persons are more likely to use technology. 10 , 11 Computer and internet adoption by older adults is also influenced by perceived usefulness, ease of use, and self‐efficacy. 12 , 13 Technology training programs can increase adoption among older adults by addressing self‐perceived capacity and motivations to use technology. 14 With growing technology use among geriatric patients, researchers and clinicians have called for a digital transformation of the healthcare delivery system.
Previous studies on telehealth adoption among older adults have focused on the effectiveness of home telehealth programs in chronic disease management. 15 , 16 , 17 The widespread adoption of telehealth during the COVID‐19 pandemic by clinicians and patients provides an opportunity to understand use patterns and barriers and facilitators to using telehealth among older patients. 18 Physicians caring for geriatric patients had valuable experiences relating to the adoption of telehealth during the pandemic and their perspectives could elucidate how to achieve a digital transformation without exacerbating existing inequities. 19
The purpose of our study was to interview a diverse sample of U.S. physicians representing multiple frontline specialties, geographic regions, and practice settings, as previously published work on telehealth primarily reports on outcomes at large medical centers in younger patients. 20 , 21 , 22 , 23 , 24 Interviews focused on the (1) practical considerations surrounding the adoption of telehealth during the pandemic, (2) factors influencing their decision to adopt telehealth, and (3) specialty‐specific and individual experiences with telehealth use and its evolution over time.
METHODS
Study design
We conducted semi‐structured interviews with U.S. geriatricians, primary care, and EM physicians between September and November 2020. We explored physicians' views on the practical considerations, motivations of use, and experiences providing care remotely through telehealth to older patients during COVID‐19. We performed a qualitative study because hypothesis‐forming research is a useful first step to understand physician experiences and perspectives on telehealth for older adults, which is still an emerging research area. Our findings can guide future larger‐scale and quantitative work in this area. Consistent with the American Telemedicine Association's definition, we defined telehealth as remote communication with patients, including via telephone calls, video visits, home monitoring with wearables, app‐based management, or web portals to ensure all telehealth modalities were included in the study. We followed the consolidated criteria for reporting qualitative research 25 in drafting this manuscript. The principal investigator's institutional review board approved the study.
Conceptual framework
We apply a socio‐technical approach, which has been successfully used to address other safety and quality challenges, to evaluate the design, implementation, and impact of telehealth (Figure 1). This approach addresses barriers, additional areas for research, and regulatory changes to ensure applications are evidence‐based, safe, and effective. We explored how physicians reacted to new restrictions and disincentives to in‐person visits and also explored system‐level and contextual factors thought to impact the quality, safety, and value of telehealth on individuals and communities using Sittig's sociotechnical model for studying health information technology in complex adaptive healthcare systems. 26 This eight‐dimensional model addresses the socio‐technical challenges involved in development, implementation, and use of technology within healthcare.
FIGURE 1.
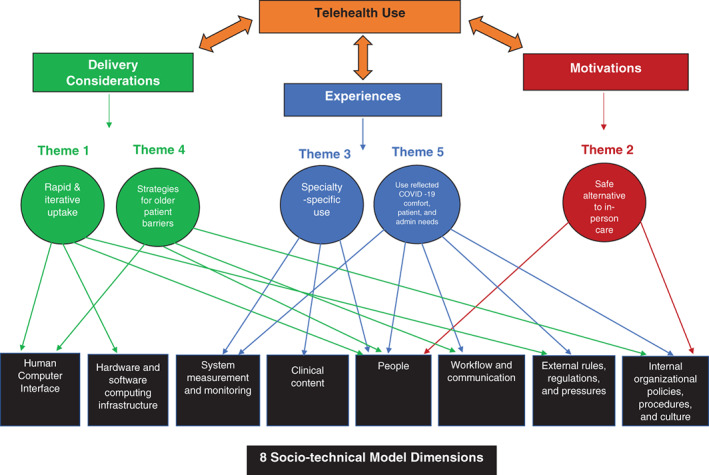
Overlap between study themes, interview guide domains, and domains of the sociotechnical model for studying health information technology in complex adaptive healthcare systems
Study population
Study eligible physicians were licensed to practice in the United States in geriatrics, primary care (internal medicine or family practice), or EM. Because we sought to understand physician experiences caring for older adult patients during the COVID‐19 pandemic, eligible physicians must have cared for patients 65 years of age and older (with or without COVID‐19) in‐person and/or via telehealth during the pandemic. In order to assess motivators and contextual factors for not adopting telehealth, study eligibility was not restricted to physicians who used telehealth during the pandemic.
Participant recruitment
We solicited participants through two social media platforms (Twitter, Facebook), which 75%–90% of U.S. physicians use, 27 , 28 and two specialty society listservs (Academy for Geriatric Emergency Medicine, 158 members, and the American Geriatric Society Member Forum, 7600 members). We posted study information once per site or listserv. Because specialty, practice location (metropolitan, suburban, or rural), and type of practice (academic or community) might influence perspectives about telehealth, we aimed to recruit 12–18 physicians in each specialty stratified by practice location and type. For qualitative research, sample sizes as small as 6–12 interviews in a homogenous group have been shown to be adequate to achieve thematic saturation. 29 We used U.S. Department of Agriculture Rural–Urban Continuum Codes 30 to group practice settings into metropolitan, suburban, or rural categories.
Interview content
The study authors composed the interview guide, which contained semi‐structured questions with follow‐up questions and probes to further explore participants' responses (Text S1). The interview guide was pilot tested within the research group. Although the precise content of the interviews varied according to specialty, we asked participants questions in the following domains:
Delivery considerations: (1) ability to carry out patient communication, disease monitoring, and treatment via telehealth during COVID‐19; (2) actions taken to adapt clinical practice to remote setting; (3) timing of telehealth adoption or plans for adoption;
Motivations of use: (1) receptivity to and concerns about telehealth adoption; (2) perceived adverse effects and challenges with initiating or continuing healthcare provision using telehealth;
Experiences: (1) specialty‐specific or other contextual factors influencing use/nonuse; (2) trajectories of use (evolution), including reasons for adopting, not adopting, continuing, or stopping telehealth usage.
Interview procedures
After obtaining informed consent, we conducted 30‐min remote interviews with participants. Participants first answered questions about their demographic and practice characteristics (years in practice, practice location, volume, patient demographics). Two individuals facilitated the interviews; the principal investigator (EG) has postdoctoral training in qualitative methods and the trained research coordinator (FJ) has three years of work experience with qualitative research. Interviews were audio‐recorded, transcribed, and de‐identified. Transcripts were corrected against the audio recording for accuracy. Interviewers completed a written debriefing after each interview to collect observations related to the tenor of the interview and emerging themes.
Analysis
We used the principles of applied thematic analysis to guide the analysis, 31 including the following steps carried out by a team of 11 individuals inclusive of two interviewers. (1) We familiarized ourselves with the data through reading and rereading the transcripts and noting initial observations. (2) We developed a set of codes based on interview questions: deductive codes (a priori from the research agenda) and inductive codes (new or emergent information learned from participants) were used. Major topics and subtopics were coded independently by two study personnel in rotating pairs, then reconciled through team discussion. We used NVivo (Version 12) 32 to organize the coded data. (3) We used framework analysis—a qualitative analysis technique, in which investigators summarize content within categories into charts after transcription 32 , 33 , 34 to iteratively search for common themes and subthemes across participants and interviews. (4) We reviewed themes in relation to the coded extracts and entire dataset and selected representative quotes to illustrate the themes. (5) We recorded coding definitions and decisions as well as ideas about emerging themes in an ongoing audit trail. 31 (6) We prepared the analytic narrative and contextualized it using the existing literature.
RESULTS
We recruited 48 geriatricians (n = 18), PCPs (n = 15), and EM physicians (n = 15) to participate in interviews (Table 1). Interviews lasted a mean of 30 min. Only one‐third (29%) of physicians reported using video visits before March 2020; however, most (58%) had previously used some form of telehealth. Two EM physicians reported not using telehealth during the pandemic. Median telehealth visits during the pandemic varied widely by specialty, with PCPs reporting the most (500 visits). Five major themes emerged relating to delivery considerations (Table S1), motivations for telehealth use (Table S2), and telehealth experiences (Table S3).
TABLE 1.
Characteristics and telehealth use for total sample and by physician specialty
| No, (%) or mean (SD) | ||||
|---|---|---|---|---|
| Total (N = 48) | Geriatrics a (N = 18) | Primary care b (N = 15) | Emergency medicine c (N = 15) | |
| Age | ||||
| 25–44 | 36 (75) | 11 (61) | 13 (87) | 12 (80) |
| 45–64 | 7 (15) | 3 (17) | 1 (7) | 3 (20) |
| 65 and over | 5 (10) | 4 (22) | 1 (7) | 0 (0) |
| Age, Median (IQR) | 37.5 (34–44.5) | 40 (35–63) | 35 (34–43) | 37 (34–43) |
| Sex | ||||
| Male | 21 (44) | 10 (56) | 3 (20) | 8 (53) |
| Female | 27 (56) | 8 (44) | 12 (80) | 7 (47) |
| Years in practice | ||||
| 0–10 | 33 (69) | 10 (56) | 11(73) | 11 (73) |
| 11–21 | 9 (19) | 2 (11) | 3 (20) | 4 (27) |
| 22–32 | 2 (4) | 2 (11) | 1 (7) | 0 (0) |
| 33 years or more | 4 (8) | 4 (22) | 0 (0) | 0 (0) |
| Years in practice, median (IQR) | 7 (3.8–13) | 9 (4–27) | 6 (3.5–11) | 7 (3–11) |
| Region | ||||
| Northeast | 19 (40) | 6 (33) | 4 (27) | 9 (60) |
| Midwest | 10 (21) | 3 (17) | 3 (20) | 4 (27) |
| South | 9 (19) | 5 (28) | 3 (20) | 1 (7) |
| West | 10 (21) | 4 (22) | 5 (33) | 1 (7) |
| Practice setting | ||||
| Metro | 26 (54) | 12 (67) | 7 (47) | 7 (47) |
| Suburban | 18 (38) | 4 (22) | 8 (53) | 6 (40) |
| Rural | 4 (8) | 2 (11) | 0 (0) | 2 (13) |
| Practice type | ||||
| Academic | 24 (50) | 9 (50) | 5 (33) | 10 (67) |
| Community | 24 (50) | 9 (50) | 10 (67) | 5 (33) |
| Before telehealth use | ||||
| Video‐visit only | 8 (17) | 2 (11) | 3 (17) | 3 (17) |
| Non‐video visit only | 14 (29) | 5 (28) | 6 (40) | 3 (17) |
| Video and non‐video visits | 6 (13) | 2 (11) | 1 (7) | 3 (17) |
| No telehealth | 20 (42) | 9 (50) | 5 (33) | 6 (40) |
| Telehealth patients seen d , median (IQR) | 224 (64–640) | 250 (64–640) | 500 (200–960) | 100 (35–400) |
Note: Not all percentages add to 100% due to rounding. Missing data for Telehealth Patients Seen for three geriatricians and two PCPs.
Abbreviation: IQR, Interquartile range.
Some geriatricians reported a secondary specialty: Hospice and Palliative Medicine (n = 1); Sleep Medicine (n = 1).
PCPs were boarded in Internal Medicine (n = 12) or Family Medicine (n = 3). Some PCPs reported a secondary specialty: Clinical Information (n = 1); Geriatrics (n = 2); Pediatrics (n = 1); Sports Medicine (n = 1).
Some emergency medicine physicians reported a secondary specialty: Clinical Informatics (n = 1); Internal Medicine (n = 1).
Estimated pandemic period was 32 weeks between March 13 and October 16, 2020.
Theme 1: Telehealth uptake was rapid, disorganized, and iterative
Although most physicians had made phone calls or used other Web‐based modes to communicate with patients before the pandemic, few reported any use of video visits before COVID‐19. Although some physician practices and hospital systems had already initiated audiovisual visits, most described a rapid, unanticipated, and chaotic adoption of audiovisual telehealth platforms as a reaction to COVID‐19 and subsequent relaxation of telehealth regulations and telehealth payment parity. Many physicians' organizations underwent extensive iterative improvements to platforms, equipment, and scheduling schema after telehealth initiation.
Most physicians reported being comfortable using telehealth after an initial learning curve. Younger physicians were more likely to describe themselves as tech‐savvy, whereas some older physicians described being hesitant to use telehealth technology at first. However, all physicians, regardless of their age or perceived technology savviness, noted that they were able to use the technology after receiving training. Many physicians reported little or no dedicated training on telehealth. Training likely facilitates adoption, as one participant noted, “we certainly have plenty of patients and a couple of doctors, frankly, who just did not take to it at first, but we've been able to bring it along with some coaching and hand holding” (Participant 9, Geriatrician, South, Community).
Theme 2: Physicians embraced telehealth use as a safe work‐around during COVID‐19
Physicians saw telehealth as a tool to protect themselves from COVID‐19 exposure as well as reducing risk of contracting the disease for older adult patients. This concern was especially true among physicians working in facilities because “people who work between facilities are the people who bring the disease into the nursing home” (Participant 19, Geriatrician, Northeast, Community). Physicians noted other motivators included reduced travel burdens with telehealth and improved access to care for older patients with mobility or transportation issues.
Geriatricians and PCPs reported that due to office closures in Spring 2020 they quickly restructured their practices to meet virtually with patients via telephone or video visits. Although some practices offered respiratory clinics or outdoor COVID‐19 evaluations, most PCPs and geriatricians chose to evaluate patients with COVID‐19 symptoms via telehealth or send them to EDs for in‐person evaluation. EM physicians reported using telehealth in two main settings. Thirteen EM interviewees used telephone calls or audiovisual communication via iPads or laptops with patients in the ED, while 11 described using telephone calls, video visits, and chat‐based visits via apps for non‐ED patients in outpatient settings.
Theme 3: Use cases and the mix of telehealth and in‐person visits were physician‐ and specialty‐specific
Physicians described needing to make decisions on the mix of telehealth and in‐person visits to offer by April 2020. Most geriatricians described a preference for telehealth for Medicare Annual Wellness Visits, for patients in facilities, for those with chronic care conditions, for medication reconciliation, and completing follow‐up appointments. They expressed that in‐person visits were preferable during the pandemic for older adults with cognitive impairment, little family support, or those lacking equipment or broadband due to the difficulties these patient populations experienced with accessing video visits independently.
“I think some of the older folks are actually going to want to continue to use virtual. […] if we're only doing the Medicare [Annual] Wellness Visit, then we should do it virtually. It is easier on them; it is a better use of all of our resources and time.” (Participant 32, PCP, South, Community)
PCPs preferred telehealth to avoid “contaminating” the office, for mental health and medication refill needs, certifying home health and durable medical equipment, and to avoid office closures if staff had an exposure. Although they worried about missing diagnoses and falling behind on health maintenance, physicians in our sample were unaware of any adverse events related to telehealth. Many geriatricians and PCPs noted that they were initially surprised with how much could be accomplished remotely with history taking, and exams adapted for virtual modalities. Physicians reported guiding older patients through self‐exams, enlisting caregivers to assist, and having patients provide vitals through remote monitoring devices.
EM physicians treating patients in the ED often described themselves as nonusers of telehealth but noted using phone calls to connect with patients' families during hospital visitor restrictions. They used a variety of video‐enabled devices, apps, and phone calls to reduce exposure time. Most acknowledged that critical patients often still needed hands‐on care. EM physicians who engaged with older adults via text‐based visits reported filling a gap in primary care services during the pandemic.
“I think especially once you use [the chat platform] a couple of times […] it becomes very easy for [older patients] and very convenient for them, especially with older adults that have transportation issues. […] There's a lot of benefit for older adults using telemedicine for [medication refills].” (Participant 34, EM, Midwest, Academic)
Some participants with personal vulnerabilities to COVID‐19 (e.g., being peripartum, older, or having a chronic condition) stated that telehealth enabled them to continue to practice medicine through low‐contact clinical roles, including moonlighting with telehealth vendors, temporarily switching to occupational medicine for the health system, doing virtual Medicare Annual Wellness Visits, or serving as medical directors for home health and facilities. For instance, one geriatrician said she had retired, but decided to return to conduct Medicare Annual Wellness Visit exams entirely virtually to assist with the pandemic response. Another EM physician temporarily practiced occupational health via telehealth after hospital policy for redeployment of pregnant employees.
Theme 4: Physician reported challenges to using telehealth with older adult patients and strategies to overcome barriers
Most physicians reported challenges to using video visits with older patients; however, some physicians noted that patient barriers were not strictly due to age but rather limited technology comfort or knowledge due to cognitive or sensory impairments, low socioeconomic status, or lacking internet access. As one physician stated, “the digital divide, it's far less age and far more technical literacy for one reason or another” (Participant 22, PCP, West, Community).
To engage older adults in telehealth visits, physicians reported a variety of strategies. These included calling patients before visits to assess telehealth capability, using phone calls when patients were unable to use audiovisual platforms, delivering tablets to patients who lacked a computer or smartphone device, and employing the help of caregivers to facilitate video visits with older patients who lacked the devices or technology literacy. To enhance understandability and rapport with older patients, physicians said they slowed their speaking speed, connected hearing impaired patients with Bluetooth‐enabled headphone devices, and used chat features to circumvent audio communication issues. Some physicians also addressed patient concerns surrounding the quality of telemedicine and privacy and security considerations. A few physicians used a team‐based approach involving social workers and/or caregivers to improve remote cognitive assessments.
Theme 5: Telehealth use declined due to decreasing prevalence of COVID‐19, patient needs, administrator requests, and physician preferences
Physicians relayed that their use of telehealth with older patients decreased as perceived COVID‐19 risk declined and protective equipment availability and safety protocols improved. Additional motivators to increase in‐person visits included missing in‐person interactions with patients, medicolegal concerns with telehealth, and for some, that telehealth technology was cumbersome and inefficient. Many reduced the number of telehealth visits offered due to patient preferences for in‐person visits, patients' inability to access telehealth visits, or a medical concern requiring in‐person visits. Support from organizational leadership determined the extent of continued telehealth use. Although many physicians described administrators, who encouraged telehealth adoption to protect employees, seven physicians stated their administrators discouraged telehealth use due to insufficient funding or reimbursement for telehealth or fears of patient dissatisfaction. Many physicians reported they hoped to continue telemedicine even after cases declined. One physician reported that she “still tr[ies] to encourage everyone to do virtual if they can, because there's still risk” (Participant 44, Geriatrician, West, Community).
DISCUSSION
In this study of U.S. geriatricians, PCPs, and EM physicians, we identified five themes relating to telehealth initiation and use in response to COVID‐19. Interviews revealed several unique considerations related to motivators of telehealth adoption. Notably, physicians described how patients and administrators often influenced the mix of telehealth and in‐person visits provided. Pay parity with in‐person visits, improved reimbursement for phone calls, and patient requests for telemedicine could address physician‐identified administrator concerns. 35
The medical staff shortages during the COVID‐19 pandemic and the impact of the pandemic on office closures and revenue 36 reveal the need for ongoing support of telehealth‐related infrastructure to enable flexible employment options for clinicians. Physicians noted telehealth could address physician shortages related to health conditions or early retirement. Interviewees reported transitioning to telehealth work due to pregnancy, medical conditions, or older age, and identified several advantages of telehealth related to their own safety, in some cases allowing them to remain in the healthcare workforce. Investment in telehealth would prepare the workforce for future pandemics 4 and could be a tool to reduce physician shortages unrelated to the pandemic, 37 particularly in long‐term care and rural settings, provided patients' needs are met and reimbursement is competitive with in‐person visits. Parity laws have been passed in the majority of U.S. states, which means private payors need to reimburse telehealth like in‐person visits, and this could improve sustainability of telehealth. 35 Additionally, many governors' plan to use coronavirus relief funds to expand broadband access, which could enhance access.
Recent studies have found that enhanced reimbursement for telehealth 38 and safety restrictions since the start of COVID‐19 increased uptake of telehealth, 37 , 39 and that telehealth benefits include convenience for patients and clinicians, 40 expanded opportunities for medical care for those with transportation barriers, 41 and potential for decreased healthcare costs. 42 Further, although telehealth use declined after peaking the week of April 15, 2020, 5 physicians identified promising examples of how telehealth can fill existing gaps in medical care beyond the scope of the COVID‐19 pandemic. Similar to other studies, physicians in our study reported that video and telephone visits were suitable for Medicare Annual Wellness Visits, those living in congregate care settings, 43 , 44 mental health appointments, 45 medication refills, 46 and involving caregivers in medical care discussions. 47 Additionally, our data also support prior findings that many face‐to‐face clinical visits are unnecessary and telehealth improves medical staff efficiency and safety. 48 Although our interviewees interacted with older patients daily who have lower digital literacy, 8 they still identified telehealth as a beneficial tool to facilitate patient care. Our study supports the existing literature on physician experiences and satisfaction with telehealth 49 and adds the physician perspective of the impact of COVID‐19 on telehealth use, especially for reaching older adults.
Telehealth is an important part of healthcare delivery, and older adults have unique needs and limitations that should be addressed in medical training. We suggest core competencies for providing medical care to older patients via telehealth informed by this research in Table S4. Additional research is also needed to identify suitable assessments for cognition and other geriatric syndromes via telehealth. Although our physicians did not report adverse events related to televisits, it is likely that they are underreported, and further study of favorable and unfavorable patient outcomes related to telehealth is important.
Our study has several limitations. Our data reflect perspectives of physicians only, which may differ from experiences of other stakeholders, such as patients, nurses, and administrators. As physicians are often leaders in care transformation as practice owners and hospital administrators, they are an important stakeholder group in telehealth. Recruitment methods may have introduced bias as our sample skewed toward younger physicians, and results may not be generalizable to older physicians or those who are less comfortable with technology. Because most of the older physicians included in our sample were geriatricians, the results may not reflect views of older EM physicians or PCPs. However, we found themes were similar among younger and older interviewees. The use of the AGEM listserv may also have resulted in inclusion of academic over community‐based EM physicians. The results reflect an early period of the COVID‐19 pandemic; as physicians gained more experience with the disease, facilitators, barriers, and motivations of use may change. Regulatory and payment considerations play a major role in telehealth adoption, but were not the focus of this work.
As frontline clinicians, geriatricians, PCPs, and EM physicians described varied adoption of telehealth in response to the COVID‐19 pandemic and all reported increased telehealth use. Sustained telehealth use was influenced by contextual factors including patient and administrator preferences and perspectives. Our results highlight promising areas where telehealth can facilitate care delivery; however, investments in infrastructure, payment policies, and training are needed to ensure telehealth viability, after COVID‐19.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Study concept and design: Elizabeth M. Goldberg, Kate Guthrie, Roland C. Merchant. Acquisition of data: Elizabeth M. Goldberg, Frances N. Jiménez. Analysis and interpretation of data: Elizabeth M. Goldberg, Frances N. Jiménez, Kevin Chen, Daniel H. Strauss, Melinda Li, Maria Zou, Natalie M. Davoodi. Preparation of manuscript: Elizabeth M. Goldberg, Frances N. Jiménez.
SPONSOR'S ROLE
The sponsor was not involved in any aspect of study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, or preparation of manuscript.
Supporting information
Table S1: Summary of themes, subthemes and illustrative quotes aligned with delivery considerations domain.
Table S2: Summary of themes, subthemes and illustrative quotes aligned with motivations of use domain.
Table S3: Summary of themes, subthemes and illustrative quotes aligned with experiences domain.
Table S4: Comparison of AAMC telehealth competencies for experienced faculty physicians (3–5 years post residency) and proposed older adult‐specific additions based on findings.
Text S1: Semi‐structured interview protocol.
ACKNOWLEDGMENTS
We thank Selena Evora at the Rhode Island Hospital, Providence, RI for her contribution to this article in developing included tables. This study was supported by grant K76 AG‐059983 from the National Institute on Aging.
Goldberg EM, Jiménez FN, Chen K, et al. Telehealth was beneficial during COVID‐19 for older Americans: A qualitative study with physicians. J Am Geriatr Soc. 2021;69(11):3034-3043. 10.1111/jgs.17370
Funding information National Institute on Aging, Grant/Award Number: K76 AG‐059983
REFERENCES
- 1. American Hospital Association . Hospitals and Health Systems Face Unprecedented Financial Pressure Due to COVID‐19; 2020. https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf. Accessed February 22, 2021.
- 2. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 pandemic on emergency department visits—United States, January1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Betancourt JA, Rosenberg MA, Zevallos A, Brown JR, Mileski M. The impact of COVID‐19 on telemedicine utilization across multiple service lines in the United States. Healthcare (Basel). 2020;8:380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID‐19). J Telemed Telecare. 2020;26:309‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID‐19 pandemic in the US. JAMA Intern Med. 2021;181:388‐391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . Q&A on coronaviruses (COVID‐19); 2020. https://www.who.int/news-room/q-a-detail/q-a-coronaviruses. Accessed February 4, 2021.
- 7. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180:1386‐1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine Unreadiness among older adults in the United States during the COVID‐19 pandemic. JAMA Intern Med. 2020;180:1389‐1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brahmandam S, Holland WC, Mangipudi SA, et al. Willingness and ability of older adults in the emergency department to provide clinical information using a tablet computer. J Am Geriatr Soc. 2016;64:2362‐2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anderson M, Perrin A. Tech Adoption Climbs Among Older Adults; updated May 17, 2017. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/. Accessed June 6, 2021.
- 11. Cresci MK, Yarandi HN, Morrell RW. Pro‐nets versus no‐nets: differences in urban older Adults' predilections for internet use. Educ Gerontol. 2010;36:500‐520. [Google Scholar]
- 12. Heinz M, Martin P, Margrett JA, et al. Perceptions of technology among older adults. J Gerontol Nurs. 2013;39:42‐51. [DOI] [PubMed] [Google Scholar]
- 13. Adams N, Stubbs D, Woods V. Psychological barriers to internet usage among older adults in the UK. Med Inform Internet Med. 2005;30:3‐17. [DOI] [PubMed] [Google Scholar]
- 14. Fischer SH, David D, Crotty BH, Dierks M, Safran C. Acceptance and use of health information technology by community‐dwelling elders. Int J Med Inform. 2014;83:624‐635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hawley CE, Genovese N, Owsiany MT, et al. Rapid integration of home telehealth visits amidst COVID‐19: what do older adults need to succeed? J Am Geriatr Soc. 2020;68:2431‐2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hersh WR, Wallace JA, Patterson PK, et al. Telemedicine for the Medicare population: pediatric, obstetric, and clinician‐indirect home interventions. Evid Rep Technol Assess (Summ). 2001;24 Suppl:1‐32. [PMC free article] [PubMed] [Google Scholar]
- 17. Radhakrishnan K, Xie B, Berkley A, Kim M. Barriers and facilitators for sustainability of tele‐homecare programs: a systematic review. Health Serv Res. 2016;51:48‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keesara S, Jonas A, Schulman K. Covid‐19 and health Care's digital revolution. N Engl J Med. 2020;382:e82. [DOI] [PubMed] [Google Scholar]
- 19. Nouri S, Khoong Elaine C, Lyles Courtney R, Karliner L. Addressing equity in telemedicine for chronic disease management during the COVID‐19 pandemic. NEJM Catal. 2000;1. [Google Scholar]
- 20. Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID‐19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27:1132‐1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dewar S, Lee PG, Suh TT, Min L. Uptake of virtual visits in a geriatric primary care clinic during the COVID‐19 pandemic. J Am Geriatr Soc. 2020;68:1392‐1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khairat S, Pillai M, Edson B, Gianforcaro R. Evaluating the telehealth experience of patients with COVID‐19 symptoms: recommendations on best practices. J Patient Exp. 2020;7:665‐672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID‐19 pandemic. JAMA Netw Open. 2020;3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Srinivasan M, Asch S, Villendrer S, et al. Qualitative assessment of rapid system transformation to primary care video visits at an Academic Medical Center. Ann Intern Med. 2020;173:527‐535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349‐357. [DOI] [PubMed] [Google Scholar]
- 26. Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(Suppl 3):i68‐i74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16:e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Surani Z, Hirani R, Elias A, et al. Social media usage among health care providers. BMC Res Notes. 2017;10:654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18:59‐82. [Google Scholar]
- 30. U.S. Department of Agriculture . Rural‐Urban Continuum Codes; 2020. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx#.U0VBhleG-Hs. Accessed May 14, 2020.
- 31. Curry L Sr, Wetle T. Improving Aging and Public Health Research: Qualitative and Mixed Methods. Washington, DC: American Public Health Association and the Gerontological Society of America; 2006. [Google Scholar]
- 32. NVivo; 2020. https://www.qsrinternational.com/nvivo/home.
- 33. Ward DJ, Furber C, Tierney S, Swallow V. Using framework analysis in nursing research: a worked example. J Adv Nurs. 2013;69:2423‐2431. [DOI] [PubMed] [Google Scholar]
- 34. Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res. 2011;18:52‐62. [DOI] [PubMed] [Google Scholar]
- 35. eVisit. Private Payors & Telemedicine; 2021. https://evisit.com/resources/telemedicine-private-payers-issues/. Accessed June 21, 2021.
- 36. Goldhill O. 'People Are Going to Die': Hospitals in half the States Are Facing a Massive Staffing Shortage as Covid‐19 Surges. Boston, MA: STAT; 2020. [Google Scholar]
- 37. Kichloo A, Albosta M, Dettloff K, et al. Telemedicine, the current COVID‐19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8:e000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lepkowsky CM. Telehealth reimbursement allows access to mental health care during COVID‐19. Am J Geriatr Psychiatry. 2020;28:898‐899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID‐19 pandemic—United States, January–march 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1595‐1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Powell RE, Stone D, Hollander JE. Patient and health system experience with implementation of an Enterprise‐wide telehealth scheduled video visit program: mixed‐methods study. JMIR Med Inform. 2018;6:e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jacobs JC, Hu J, Slightam C, Gregory A, Zulman DM. Virtual savings: patient‐reported time and money savings from a VA National Telehealth Tablet Initiative. Telemed e‐Health. 2020;26:1178‐1183. [DOI] [PubMed] [Google Scholar]
- 42. de la Torre‐Díez I, López‐Coronado M, Vaca C, Aguado JS, de Castro C. Cost‐utility and cost‐effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J e‐Health: Off J Am Telemed Assoc. 2015;21:81‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Harris DA, Archbald‐Pannone L, Kaur J, et al. Rapid telehealth‐centered response to COVID‐19 outbreaks in Postacute and long‐term care facilities. Telemed J E Health. 2021;27:102‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gray LC, Edirippulige S, Smith AC, et al. Telehealth for nursing homes: the utilization of specialist services for residential care. J Telemed Telecare. 2012;18:142‐146. [DOI] [PubMed] [Google Scholar]
- 45. Langarizadeh M, Tabatabaei MS, Tavakol K, Naghipour M, Rostami A, Moghbeli F. Telemental health care, an effective alternative to conventional mental care: a systematic review. Acta Inform Med. 2017;25:240‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ebbert JO, Ramar P, Tulledge‐Scheitel SM, et al. Patient preferences for telehealth services in a large multispecialty practice. J Telemed Telecare. 2021. 10.1177/1357633x20980302. [DOI] [PubMed] [Google Scholar]
- 47. Chi N‐C, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015;21:37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Berwick DM. Choices for the “new Normal”. JAMA. 2020;323:2125‐2126. [DOI] [PubMed] [Google Scholar]
- 49. Miner H, Fatehi A, Ring D, Reichenberg JS. Clinician telemedicine perceptions during the COVID‐19 pandemic. Telemed J Health. 2021;27(5):508‐512. 10.1089/tmj.2020.0295. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Summary of themes, subthemes and illustrative quotes aligned with delivery considerations domain.
Table S2: Summary of themes, subthemes and illustrative quotes aligned with motivations of use domain.
Table S3: Summary of themes, subthemes and illustrative quotes aligned with experiences domain.
Table S4: Comparison of AAMC telehealth competencies for experienced faculty physicians (3–5 years post residency) and proposed older adult‐specific additions based on findings.
Text S1: Semi‐structured interview protocol.


