Abstract
Background/Objectives
Transitional care management (TCM) visits delivered following hospitalization have been associated with reductions in mortality, readmissions, and total costs; however, uptake remains low. We sought to describe trends in TCM visit delivery during the COVID‐19 pandemic.
Design
Cross‐sectional study of ambulatory electronic health records from December 30, 2019 and January 3, 2021.
Setting
United States.
Participants
Forty four thousand six hundred and eighty‐one patients receiving transitional care management services.
Measurements
Weekly rates of in‐person and telehealth TCM visits before COVID‐19 was declared a national emergency (December 30, 2019 to March 15, 2020), during the initial pandemic period (March 16, 2020 to April 12, 2020) and later period (April 12, 2020 to January 3, 2021). Characteristics of patients receiving in‐person and telehealth TCM visits were compared.
Results
A total of 44,681 TCM visits occurred during the study period with the majority of patients receiving TCM visits age 65 years and older (68.0%) and female (55.0%) Prior to the COVID‐19 pandemic, nearly all TCM visits were conducted in‐person. In the initial pandemic, there was an immediate decline in overall TCM visits and a rise in telehealth TCM visits, accounting for 15.4% of TCM visits during this period. In the later pandemic, the average weekly number of TCM visits was 841 and 14.0% were telehealth. During the initial and later pandemic periods, 73.3% and 33.6% of COVID‐19‐related TCM visits were conducted by telehealth, respectively. Across periods, patterns of telehealth use for TCM visits were similar for younger and older adults.
Conclusion
The study findings highlight a novel and sustained shift to providing TCM services via telehealth during the COVID‐19 pandemic, which may reduce barriers to accessing a high‐value service for older adults during a vulnerable transition period. Further investigations comparing outcomes of in‐person and telehealth TCM visits are needed to inform innovation in ambulatory post‐discharge care.
Keywords: COVID‐19, hospitalization, medicare, transitional care management
Key Points
During the COVID‐19 pandemic, 15% of post‐discharge transitional care management (TCM) visits shifted to telehealth.
Older adults were as likely to receive telehealth TCM visits as younger adults.
Why Does This Paper Matter?
Delivering TCM services via telehealth appears feasible and may reduce logistical barriers for older adults to access this high‐value service during the vulnerable post‐discharge period, particularly following hospitalizations related to COVID‐19.
INTRODUCTION
The post‐hospitalization period is a vulnerable time during which patients face elevated risk of adverse events, lapses in care, and rehospitalization. 1 , 2 This risk is particularly pronounced for older adults with multiple chronic conditions. In an effort to improve post‐hospitalization care, Medicare provides enhanced reimbursement to clinicians for outpatient care delivered in the 30 days following discharge from a hospital, observation, skilled nursing facility, or acute rehabilitation facility stay through transitional care management (TCM) services. 3 Use of TCM has been associated with reductions in mortality, readmissions, and total costs 4 and has also been adopted by some commercial insurers. Despite this, TCM services remain greatly underutilized. 5 , 6
Hypothesized barriers include insufficient reimbursement, administrative complexity of TCM billing requirements, and difficulty in arranging for patients to be seen for a face‐to‐face visit after recovering from acute illness. To qualify for TCM reimbursement, a care team member must contact the patient or their caregiver within 2 days after discharge and a face‐to‐face visit with a clinician must occur within 7 days of discharge for patients with highly complex conditions and within 14 days for patients with moderately complex conditions. Although Medicare has permitted TCM visits to be conducted by telehealth since 2014, 7 telehealth TCM programs have not been previously described. In response to the coronavirus diseases 2019 (COVID‐19) pandemic, national adoption of telehealth services has grown dramatically. 8 To understand how this practice shift has impacted delivery of TCM, we examined trends in the TCM visits among a national sample of electronic health records (EHRs).
METHODS
We examined the HealthJump database to identify outpatient TCM visits occurring between December 30, 2019 and January 3, 2021. The HealthJump database consists of ambulatory health records aggregated from multiple national EHR platforms and standardized to facilitate interoperability. The HealthJump database contains EHR data from millions of patients regardless of payer, the database includes EHRs from all regions of the US but representation of patients from the New England and West North Central census regions is limited. This database has been made available for research through the COVID‐19 Research Database Consortium. 9 We identified TCM visits by Common Procedural Terminology codes 99495 and 99496 and telehealth visits via modifier codes GT, GQ, or 95.
We examined weekly rates of in‐person and telehealth TCM visits, focusing on three periods: before COVID‐19 was declared a national emergency (December 30, 2019 to March 15, 2020), during the initial pandemic period (March 16, 2020 to April 12, 2020) and later period (April 12, 2020 to January 3, 2021). We examined TCM visits among adults younger than age 65, ages 65 to 74, ages 75 to 84, and age 85 and above. For each age group, we examined overall and COVID‐related TCM visits, identified by the presence of a primary or secondary International Classification of Diseases, 10th Revision, Clinical Modification diagnosis code for COVID‐19 (U071 or U072). We compared characteristics of individuals receiving in‐person and telehealth TCM services using chi 2 tests, where p < 0.05 was considered statistically significant. All analyses were conducted using Stata, version 16.1 (StataCorp LLC). The study was classified as exempt by the Beth Israel Deaconess Medical Center Institutional Review Board and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
RESULTS
A total of 44,681 TCM visits occurred during the study period and the majority of patients receiving TCM visits were age 65 years and older (68.0%) and female (55.0%) (Table 1). There was substantial geographic variation in telehealth TCM use and a greater proportion of telehealth TCM visits were by female patients (59.6% vs 54.4% of in‐person visits, p < 0.001). Use of telehealth TCM visits was similar across age strata, including the oldest old, with telehealth accounting for 11.3% of TCM visits by adults younger than 65 years of age, 10.6% of TCM visits by adults age 65–74 years, 10.4% of TCM visits by adults age 75–84, and 11.2% of TCM visits by adults age 85 years and older (p = 0.08).
TABLE 1.
Characteristics of individuals receiving transitional care management visits, December 30, 2019 to January 3, 2021
| Health jump population a | Overall TCM visits, no. (%) | COVID‐19‐related TCM visits, no. (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Telehealth | In‐person | p‐Value | Total | Telehealth | In‐person | p‐Value | ||
| Total | 7,107,330 | 44,681 | 4865 | 39,816 | 1228 | 419 | 809 | ||
| Gender | |||||||||
| Male | 2,976,080 (41.9) | 20,116 (45) | 1976 (40.6) | 18,140 (45.6) | <0.001 | 586 (47.7) | 189 (45.1) | 397 (49.1) | 0.18 |
| Female | 3,698,360 (52.0) | 24,559 (55) | 2888 (59.4) | 21,671 (54.4) | 607 (47.5) | 172 (43.4) | 435 (49.3) | ||
| Unknown | 432,890 (6.1) | <10 | <10 | <10 | 0 | 0 | 0 | ||
| Age, years | |||||||||
| <65 | 4,451,311 (62.6) | 14,317 (33.8) | 1622 (35.1) | 12,695 (33.7) | 0.08 | 495 (42.0) | 162 (40.1) | 333 (43.0) | 0.66 |
| 65–74 | 2,604,726 (36.6) | 11,260 (26.6) | 1199 (26.0) | 10,061 (26.7) | 322 (27.3) | 115 (28.5) | 207 (26.7) | ||
| 75–84 | 10,673 (25.2) | 1111 (24.1) | 9562 (25.4) | 258 (21.9) | 94 (23.3) | 164 (21.2) | |||
| ≥85 | 6076 (14.4) | 683 (14.8) | 5393 (14.3) | 103 (8.7) | 33 (8.2) | 70 (9.0) | |||
| Unknown | 51,293 (0.7) | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Race | |||||||||
| White | 941,435 (13.2) | 26,597 (59.5) | 2499 (51.4) | 24,098 (60.5) | <0.001 | 693 (56.4) | 222 (53.0) | 471 (58.2) | 0.18 |
| Black | 320,152 (4.5) | 4794 (10.7) | 556 (11.4) | 4238 (10.6) | 192 (15.6) | 75 (17.9) | 117 (14.5) | ||
| Asian | 29,483 (0.4) | 265 (0.6) | 28 (0.6) | 237 (0.6) | 12 (1.0) | <10 | <10 | ||
| Other | 7604 (0.1) | 176 (0.4) | <10 | 168 (0.4) | <10 (<1.0) | <10 | <10 | ||
| Unknown | 5,808,656 (81.7) | 12,849 (28.8) | 1774 (36.5) | 11,075 (27.8) | 327 (26.6) | 115 (27.4) | 212 (26.2) | ||
| Ethnicity | |||||||||
| Hispanic | 289,540 (4.1) | 7358 (16.5) | 1144 (23.5) | 6214 (15.6) | <0.001 | 305 (24.8) | 123 (29.4) | 182 (22.5) | 0.28 |
| Non‐Hispanic | 1,566,167 (22.0) | 25,003 (56.0) | 2504 (51.5) | 22,499 (56.5) | 592 (48.2) | 217 (51.8) | 375 (46.4) | ||
| Unknown | 5,251,623(73.9) | 12,320 (27.6) | 1217 (25.0) | 11,103 (27.9) | 331 (27.0) | 79 (18.9) | 252 (31.1) | ||
| Census division | |||||||||
| East North Central | 1,327,042(18.7) | 1006 (2.3) | 53 (1.1) | 953 (2.4) | <0.001 | 19 (1.5) | <10 | 14 (1.7) | <0.001 |
| East South Central | 438,166 (6.2) | 3674 (8.2) | 227 (4.7) | 3447 (8.7) | 117 (9.5) | 18 (4.3) | 99 (12.2) | ||
| Middle Atlantic | 519,955 (7.3) | 7267 (16.3) | 850 (17.5) | 6417 (16.1) | 159 (12.9) | 67 (16.0) | 92 (11.4) | ||
| Mountain | 977,681(13.8) | 3947 (8.8) | 433 (8.9) | 3514 (8.8) | 112 (9.1) | 28 (6.7) | 84 (10.4) | ||
| New England | 8093 (0.1) | 13 (<0.1) | 0 | 13 (<0.1) | 0 | 0 | 0 | ||
| Pacific | 1,068,598 (15.0) | 4341 (9.7) | 554 (11.4) | 3787 (9.5) | 111 (9.0) | 32 (7.6) | 79 (9.8) | ||
| South Atlantic | 2,026,219 (28.5) | 15,246(34.1) | 1870 (38.4) | 13,376 (33.6) | 364 (29.6) | 152 (36.3) | 212 (26.2) | ||
| West North Central | 60,712 (0.9) | 4385 (9.8) | 247 (5.1) | 4138 (10.4) | 130 (10.6) | 27 (6.4) | 103 (12.7) | ||
| West South Central | 351,152 (4.9) | 4800 (10.7) | 631 (13.0) | 4169 (10.5) | 216 (17.6) | 90 (21.5) | 126 (15.6) | ||
| Unknown | 329,712 (4.6) | <10 | 0 | <10 | 0 | 0 | 0 | ||
Note: Individuals may have contributed more than 1 TCM visit during study period. Other reported races include American Indian, Alaska Native, and Pacific Islander and are grouped due to low sample size. Categories with fewer than 10 observations are listed as <10 to preserve confidentiality.
Abbreviation: TCM, transitional care management.
Substrata of older adult categories not available for overall HealthJump population due to data use restrictions, thus N for >65 years of age sub‐group provided for overall population.
Prior to the COVID‐19 epidemic, the average number of weekly TCM visits was 927, nearly all of which were conducted in‐person (Figure 1). In the initial pandemic, there was an immediate decline in overall TCM visits and a rise in telehealth TCM visits, accounting for 15.4% of TCM visits during this period. In the later pandemic, the average weekly number of TCM visits was 841 and 14.0% were telehealth. Older adults accounted for 70.4% of telehealth TCM visits during the initial pandemic period and 66.4% of telehealth TCM visits during the late pandemic period.
FIGURE 1.
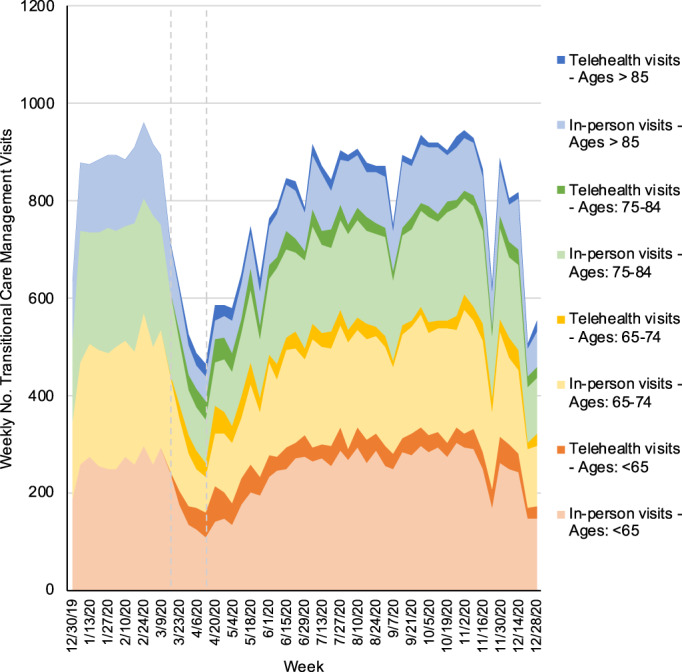
Trends in in‐person and telehealth transitional care management visits per week, December 30, 2019 to January 3, 2021. Note: The dotted vertical lines indicate the beginning of the early pandemic period (March 16, 2020) and later pandemic period (April 13, 2020). Older adults defined as individuals age 65 years of age and older while younger adults include those younger than 65 years of age [Color figure can be viewed at wileyonlinelibrary.com]
COVID‐19‐related TCM visits grew during the initial and later pandemic periods, with peaks in April, August, and December 2020 corresponding to peaks in national COVID cases (Figure 2). During the initial and later pandemic periods, 73.3% and 33.6% of COVID‐19‐related TCM visits were conducted by telehealth, respectively. Older adults accounted for 63.4% of COVID‐related telehealth TCM visits during the initial pandemic period and 61.3% of COVID‐related telehealth TCM visits during the late pandemic period. Use of telehealth for COVID‐19‐related TCM visits was similar across age strata, including the oldest old, with telehealth accounting for 32.7% of visits by adults younger than 65 years of age, 35.7% of visits by adults age 65–74 years, 36.4% of visits by adults age 75–84, and 32.0% of visits by adults age 85 years and older (p = 0.66).
FIGURE 2.
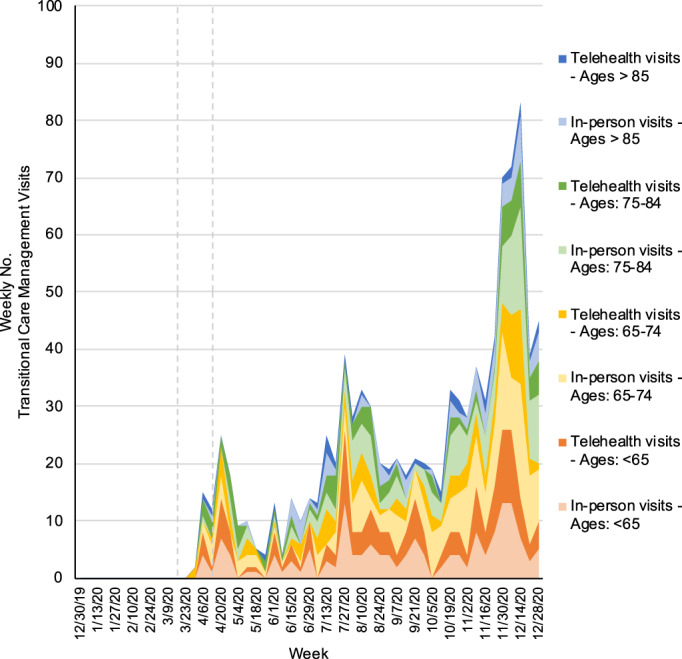
Trends in in‐person and telehealth COVID‐19‐related transitional care management visits per week, December 30, 2019 to January 3, 2021. Note: The dotted vertical lines indicate the beginning of the early pandemic period (March 16, 2020) and later pandemic period (April 13, 2020). Older adults defined as individuals age 65 years of age and older while younger adults include those younger than 65 years of age [Color figure can be viewed at wileyonlinelibrary.com]
DISCUSSION
During COVID‐19 pandemic, there was an initial decline in overall TCM visits, which have since recovered, with 14% shifting to telehealth, including one‐third of COVID‐19‐related TCM visits. These findings highlight a new and sustained shift to providing TCM services via telehealth during the COVID‐19 pandemic with similar patterns of telehealth use among younger and older adults.
Our findings build on prior studies documenting the uptake of telehealth during the COVID‐19 pandemic. 8 , 10 , 11 Past studies, included a variety of visit types, have documented higher rates of telehealth use, ranging from 20% to 40% of ambulatory visits. This difference likely reflects different timeframes, as prior studies examined only the first half of 2020, during which time restrictions on ambulatory visits placed in response to the initial pandemic response, were more common. Furthermore, prior studies of telehealth use for general outpatient care have shown that older adults were less likely to complete telehealth visits compared to younger adults 10 , 11 although the current study documents similar use of telehealth across ages for TCM visits specifically.
Why might older adults use of telehealth differ for TCM compared with other outpatient visits? During recovery from acute illness, older adults may face transport, mobility, and care coordination barriers in arranging follow‐up care. Despite the fact that the post‐hospitalization period is a highly vulnerable time during which patients face decreased function and increased risk for preventable adverse events, 12 , 13 patients without specific concerns may not feel it necessary to seek care or may not feel able to overcome these barriers. Delivering post‐discharge TCM visits through telehealth reduces the logistical barrier of requiring patients to physically return to a clinic setting while still recovering from acute illness. This option may be a promising alternative, particularly for frail patients, those with impaired mobility or limited access to transport. Many integral parts of post‐discharge visits are amenable to telehealth, including medication reconciliation and coordination of specialist and home services. However, in some circumstances, particularly if patients report worsening of symptoms, telehealth visits may be a poor substitute for in person evaluations. Furthermore, more than one‐third of older adults are estimated to be unready to engage in telemedicine, 14 thus identifying patients preferred care pathway and developing infrastructure for older adults to access telehealth in the post‐discharge period is vital. It is unlikely that all or even most TCM visits should be converted to telehealth, but the current study provides a useful starting point for clinics and health systems seeking to target telehealth initiatives beyond the COVID‐19 pandemic, particularly if telehealth provides an option for patients who otherwise would receive no post‐discharge follow‐up.
This study did not assess outcomes following TCM visits and may not generalize to other ambulatory settings. Additionally, as HealthJump is a primarily outpatient EHR dataset, we were unable to identify hospitalizations for which TCM visits did not occur though prior research has clearly documented an underuse of these services prior to the COVID pandemic. 5 , 6 Some patients may receive post‐hospitalization care that is not billed under TCM and our study was not able to assess the frequency of telehealth use for these types of visits.
Further study will be necessary to determine if telehealth TCM visits are associated with the same improvements in clinical outcomes and cost savings as in‐person visits, whether differences in outcomes exist between visits delivered by video or phone, and older adults' perspectives on the acceptability of telehealth TCM visits. If telehealth TCM visits are found to be as beneficial as in‐person TCM visits or beneficial in specific circumstances, this practice innovation may substantially reduce patient barriers to accessing care and increase use of a high‐value service while also providing enhanced reimbursement to primary care clinicians. Ultimately, it is likely that a mix of telehealth and in‐person options for post‐discharge care may be best suited to meet patient needs, in which case, sustained adoption of telehealth TCM services will require further Medicare policy changes to maintain and increase ambulatory practice incentives to deliver telehealth and to facilitate telehealth infrastructure for older adults in the home.
CONFLICT OF INTEREST
Dr. Anderson reports grant funding from the National Institute on Aging and American College of Cardiology outside of the submitted work. Dr. Herzig reports grant funding from the Agency for Healthcare Research and Quality outside of the submitted work.
AUTHOR CONTRIBUTIONS
Dr. Anderson had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis as the guarantor. Dr. Anderson attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Study concept and design: Anderson, Stevens. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Anderson. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Anderson, Dechin, O'Donoghue. Obtained funding: Stevens. Administrative, technical, or material support: Stevens. Study supervision: Stevens.
SPONSOR'S ROLE
Google.org had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval, of the manuscript; and decision to submit the manuscript for publication.
ACKNOWLEDGMENTS
The data, technology, and services used in the generation of these research findings were provided by the COVID‐19 Research Database partners, who are acknowledged at https://covid19researchdatabase.org/. Drs. O'Donoghue and Stevens and Ms. Dechen are funded by an unrestricted philanthropic gift from Google.org.
Anderson TS, O'Donoghue AL, Dechen T, Herzig SJ, Stevens JP. Trends in telehealth and in‐person transitional care management visits during the COVID‐19 pandemic. J Am Geriatr Soc. 2021;69(10):2745–2751. 10.1111/jgs.17329
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of Beth Israel Deaconess Medical Center or Harvard Medical School.
REFERENCES
- 1. Coleman EA, Boult C, American Geriatrics Society Health Care Systems Committee . Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556‐557. [DOI] [PubMed] [Google Scholar]
- 2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418‐1428. [DOI] [PubMed] [Google Scholar]
- 3. Bindman AB, Blum JD, Kronick R. Medicare's transitional care payment—a step toward the medical home. N Engl J Med. 2013;368(8):692‐694. [DOI] [PubMed] [Google Scholar]
- 4. Bindman AB, Cox DF. Changes in health care costs and mortality associated with transitional care management services after a discharge among medicare beneficiaries. JAMA Intern Med. 2018;178(9):1165‐1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agarwal SD, Barnett ML, Souza J, Landon BE. Adoption of medicare's transitional care management and chronic care management codes in primary care. JAMA. 2018;320(24):2596‐2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marcotte LM, Reddy A, Zhou L, Miller SC, Hudelson C, Liao JM. Trends in utilization of transitional care management in the United States. JAMA Netw Open. 2020;3(1):e1919571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Medicare & Medicaid Services. Expansion of Medicare Telehealth Services for CY; 2014. https://www.cms.gov/Regulations‐and‐Guidance/Guidance/Transmittals/Downloads/R2848CP.pdf. Accessed March 2, 2021.
- 8. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID‐19 pandemic in the US. JAMA Intern Med. 2020;16:388‐391. 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. COVID‐19 research database consortium. Data. https://covid19researchdatabase.org/. Accessed March 16, 2021.
- 10. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID‐19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID‐19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Krumholz HM. Post‐hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171‐2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States during the COVID‐19 pandemic. JAMA Intern Med. 2020;180(10):1389‐1391. [DOI] [PMC free article] [PubMed] [Google Scholar]


