Conflict of interest
None.
Funding sources
The work was supported by Fondazione Cariplo, Fondazione Veronesi, Impact of COVID‐19 infection on patients affected by inflammatory skin diseases on immunosuppressive therapies (COVISKIN); ID 1833073 rif. 2020‐1363.
Dear Editor,
Many healthcare systems have responded to the COVID‐19 pandemic by delaying and/or cancelling elective surgical procedures, particularly during the lockdown. 1 , 2 , 3 There is a concern that this could have affected the early diagnosis of malignant melanoma (MM) that is critical to improve its prognosis. 4 , 5 The objective of this observational study was to investigate whether a reduction in the incidence of new diagnoses of MM has occurred following the COVID‐19 outbreak. All the consecutive histological diagnoses of MM were retrospectively collected in the pathological laboratories of four provinces of the Veneto region in northern Italy, namely Verona, Vicenza, Rovigo and Treviso, between 1 March and 31 October 2020 and the same period of 2019. All cases were stratified into three categories according to Breslow thickness: in situ, <1 and ≥1 mm. The date of MM excision was considered for all the time‐related analyses. The period March–October 2020 was compared with the same period of 2019. Incidence rates (IR) of MM per 100 000 person‐year were computed by considering the overall population of the included provinces in the Veneto region and were presented along with their exact mid‐P 95% confidence intervals (CI). Incidence rates ratios (IRR) comparing IR of 2020 vs. 2019 were produced along with their exact mid‐P 95% CI and P‐values. In addition, IRR comparing the number of observed cases in 2020 and the expected number based on the estimated annual per cent change (APC) of MM from the regional cancer registry was calculated. 6 Univariate logistic regression analysis was used to compare Breslow thickness categories in the same periods of 2020 and 2019. A total of 556 MM cases in the period March–October 2020 vs. 634 MM cases in the same period of 2019 were collected (Table 1). No difference in age, sex and Breslow thickness was observed between the two periods.
Table 1.
Demographics and clinical characteristics of patients by year in the period March‐October 2019 and 2020
| March–October 2019 | March–October 2020 | P † | ||||
|---|---|---|---|---|---|---|
| N = 634 | % | N = 556 | % | |||
| Sex | Female | 283 | 44.6% | 242 | 43.5% | 0.70 |
| Male | 351 | 55.4% | 314 | 56.5% | ||
| Age | Median, IQR | 61.0 | 50.0–72.0 | 62.5 | 51.0–73.0 | 0.69 |
| Breslow | Median, IQR‡ | 0.5 | 0.3–1.1 | 0.5 | 0.3–1.2 | 0.57 |
| In situ | 163 | 25.7% | 133 | 23.9% | 0.62 | |
| <1 mm | 338 | 53.3% | 295 | 53.1% | ||
| 1+ mm | 133 | 21.0% | 128 | 23.0% | ||
IQR, interquartile range.
Continuous variables were presented as medians with interquartile ranges (IQR), while nominal variables as numbers with percentages. Chi‐square test and Mann–Whitney U test were used for nominal and continuous variables, respectively. ‡Excluding in situ melanoma.
The number of MM cases stratified by Breslow thickness category and excision dates in the period March–October 2020 and 2019 with a finer division by 2‐month interval is reported in Fig. 1. The number of missed expected cases, based on an estimated 3.4% annual change of MM incidence from Veneto regional data, is shown as well (Fig. 1).
Figure 1.
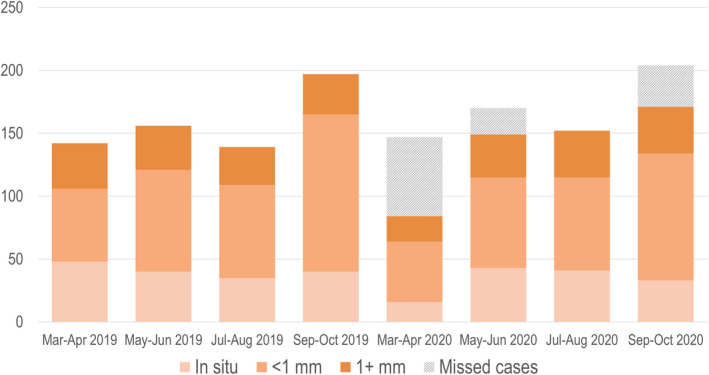
Number of melanoma excisions in the period March–October 2019 and 2020 by Breslow category and biopsy dates. The number of missed expected cases, based on an estimated 3.4% annual change of melanoma incidence from Veneto regional data, is shown as well.
The incidence of MM in the period March–October 2020 vs the same period of 2019 was 28.7 (95% C.I. 26.4–31.2) and 32.8 (95% C.I. 30.2–35.4), respectively; the corresponding IRR was 0.88 (95% C.I. 0.78–0.98, P = 0.02). When considering the number of cases observed vs. those expected based on estimated APC from the regional cancer data for the same period March‐October, a statistically significant difference was confirmed (556 observed vs. 654.7 expected; IRR = 0.85; 95% CI = 0.76–0.95; P = 0.004). The incidence of MM, comparing March–April 2020 vs. the same period of 2019, showed a significant reduction (84 vs. 142 cases per 100 000 person‐years, IRR = 0.59; 95% CI = 0.45–0.77; P < 0.001). This decrease is also confirmed by taking into account the expected number of cases based on estimated annual per cent change from the regional cancer registry (84 vs. 146.7 expected, IRR = 0.57; 95% CI = 0.44–0.75; P < 0.001). The same differences in the reduction of the MM incidence were detected for males and females, while there was a trend in the reduction for increasing age groups, especially those aged ≥65 years. No difference in the distribution of cases according to Breslow thickness categories was documented in the logistic regression analysis. Our data document that a significant reduction in MM new diagnoses has occurred following the COVID‐19 pandemic, similarly to what has been reported for other cancers, 7 , 8 , 9 potentially causing an increase of morbidity, mortality and healthcare costs, which could not be quantified at this stage. 10
Acknowledgements
We thank Dr Luca Finizio, Dr Stefano Chincherini, Dr Paolo Rosina, Dr Gianpaolo Tessari for their contribution. The patients in this manuscript have given written informed consent to publication of their case details.
IRB of the University of Verona reviewed and approved this observational study
References
- 1. O'Reilly‐Shah VN, Van Cleve W, Long DR et al. Impact of COVID‐19 response on global surgical volumes: an ongoing observational study. Bull World Health Organ 2020; 98: 671–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American College of Surgeons . COVID‐19: recommendations for management of elective surgical procedures. URL https://www.facs.org/covid‐19/clinical‐guidance/elective‐surgery (last accessed: 25 April 2021).
- 3. Royal College of Surgeons . COVID‐19: good practice for surgeons and surgical teams. URL https://www.rcseng.ac.uk/standards‐and‐research/standards‐and‐guidance/good‐practice‐guides/coronavirus/covid‐19‐good‐practice‐for‐surgeons‐and‐surgical‐teams/ (last accessed: 25 April 2021).
- 4. Tejera‐Vaquerizo A, Nagore E. Estimated effect of COVID‐19 lockdown on melanoma thickness and prognosis: a rate of growth model. J Eur Acad Dermatol Venereol 2020; 34: e351–e353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arenbergerova M, Lallas A, Nagore E et al. Position statement of the EADV Melanoma Task Force on recommendations for the management of cutaneous melanoma patients during COVID‐19. J Eur Acad Dermatol Venereol 2021; 35: e427–e428. 10.1111/jdv.17252111/jdv.17252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Registro tumori Veneto . La frequenza del tumore: melanoma cutaneo. URL https://gecoopendata.registrotumoriveneto.it/incidenza.php?sede=melanoma_cutaneo&codSede=C43‐C43.9 (last accessed: 25 April 2021).
- 7. Maringe C, Spicer J, Morris M et al. The impact of the COVID‐19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population‐based, modelling study. Lancet Oncol 2020; 21: 1023–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vissio E, Falco EC, Collemi G et al. Impact of COVID‐19 lockdown measures on oncological surgical activity: analysis of the surgical pathology caseload of a tertiary referral hospital in Northwestern Italy. J Surg Oncol 2021; 123: 24–31. [DOI] [PubMed] [Google Scholar]
- 9. Marson JW, Maner BS, Harding TP et al. The magnitude of COVID‐19's effect on the timely management of melanoma and nonmelanoma skin cancers. J Am Acad Dermatol 2021; 84: 1100–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rossi E, Trakatelli M, Giacomelli L et al. The COVID‐19 outbreak in dermatologic surgery: resetting clinical priorities. J Eur Acad Dermatol Venereol 2020; 34: e543–e545. [DOI] [PMC free article] [PubMed] [Google Scholar]


