Abstract
Background and Objectives
The first wave of coronavirus disease‐2019 (COVID‐19) dramatically affected the Transfusion Medicine Unit of the Azienda Unità Sanitari Locale ‐ Istituto di Ricovero e Cura a Carattere Scientifico (AUSL‐IRCCS) di Reggio Emilia, which faced a total rearrangement of the procedures for donors and patients. This study aims to assess the major implications of COVID‐19 on our department, focusing on the blood transfusion chain and therapies, in order to support transfusion specialists in seeking efficient ways to face similar future emergencies.
Materials and Methods
This retrospective study compares our Transfusion Medicine Unit data collected between February and May 2020 with the same period in 2017–2019. Data on red blood cells and platelets donations, transfusions and clinical procedures were collected as aggregates from our internal electronic database.
Results
During the lockdown, donor centres were re‐organized to reduce the risk of contagion and avoid unnecessary blood collection. Blood donations were re‐scheduled to meet the decrease in elective surgery; consequently, plateletapheresis was implemented to supply the reduction of buffycoat‐derived platelets. Transfusions significantly decreased together with orthopaedic and vascular surgery, while they were only marginally diminished for both cancer and onco‐haematological patients. Reduced procedures for inpatients and outpatients were matched by remote medicine, addressing the need of a constant healthcare support for patients with chronic diseases.
Conclusions
The described measures were adopted to avoid excessive blood collection and expiration, guarantee the safety of our ward (for both patients and staff) and supply the necessary transfusion therapies. These measures may support the development of appropriate risk management plans and safety procedures for other hospitals and transfusion services that have to face similar events.
Keywords: blood collection, donor recruitment, platelet transfusion, transfusion medicine (in general), transfusion therapy
INTRODUCTION
The first wave of coronavirus disease‐2019 (COVID‐19) significantly impacted Northern Italy, where hospitals faced a rapid and profound re‐organization of the healthcare services supply [1, 2]. The Italian Government declared a lockdown period that, for the Reggio Emilia province, started on 9 March 2020, with a gradual loosening from 3 May 2020 [3]. During this period, all the wards of the AUSL‐IRCCS of Reggio Emilia rearranged their routine procedures to meet the requirements imposed by the COVID‐19 outbreak.
Reggio Emilia hospital is located in Emilia Romagna (Northern Italy) and experienced thousands of COVID‐19 cases, with different grades of severity during the lockdown period [4]. The impact of the pandemic on the healthcare system negatively affected a large number of patients with different pathologies [5, 6, 7, 8, 9]. Emilia Romagna Local Governance listed the healthcare services that could not be postponed during the lockdown, as well as those that could be delayed or developed through remote medicine (i.e., telemedicine, electronic prescriptions, phone consultations), in order to limit the access to hospitals and avoid overcrowding [10].
Despite not being involved in first‐line treatment of COVID‐19 patients, even our Transfusion Medicine Unit faced many changes in its routine clinical practice, due to the close connection with the other hospital departments [11]. To ensure high standards of blood donation and blood safety during the emergency, the Italian National Blood Centre (Centro Nazionale Sangue, CNS), in compliance with the Ministry of Health and the COVID‐19 Technical Scientific Committee (CTS), issued a series of measures that our ward promptly adopted [12, 13].
In the present study, we investigate the effects of the COVID‐19 pandemic and lockdown‐related restrictions on the activity of our Transfusion Medicine Unit, providing a description of the adopted measures and of their effectiveness on blood collection, blood transfusions, transfusion medicine and immune‐haematology clinical practice.
Our aim is to point out, through an evidence‐based analysis, the practices that may help transfusion specialists worldwide to deal with similar emergencies in the future.
MATERIALS AND METHODS
Reggio Emilia is one of the nine provinces located in the Emilia‐Romagna region, accounting for about 532,000 inhabitants. The Emilia‐Romagna region coordinates blood availability and distribution between the provinces via the Regional Blood Centre (Centro Regionale Sangue [CRS]). Reggio Emilia province harbours five hospitals. Nevertheless, there is only a Transfusion Medicine Unit that centralizes the necessity for transfusions, therapies and medical consultations.
Study design
The study was carried out at the Transfusion Medicine Unit of the Azienda USL‐IRCCS di Reggio Emilia. This is a retrospective study comparing data from February to May 2020 with the same period of the previous triennium (2017–2019).
Since one‐way analysis of variance (ANOVA) analysis did not reveal significant difference (p > 0.05) in the mean transfusions among the tested groups (2017–2019), total red blood cells (RBCs) transfusions performed during the 2020 lockdown were compared with the mean transfusions performed during the same period of the previous triennium.
PLTs transfusions' comparison, instead, was performed on 2020 versus 2019. In our OECI Clinical Cancer Centre, between 65% and 90% of PLTs usage is generally destined to haematological and onco‐haematological patients. The number of these patients increased since July 2017, when our hospital established the Cancer and Haematology Centre (CORE). This pavilion became fully functional by the end of 2018 and now centralizes all the onco‐haematological patients of the Reggio Emilia province.
No ethical approval was necessary for collecting the aggregated, anonymous data presented herein.
Transfusion Medicine Unit procedures and organization
Our Transfusion Medicine Unit accounts for 24 collection points (donor centres) covering the whole Reggio Emilia province. The management is equally distributed between the hospital and the volunteer associations (Associazione Volontari Italiani del Sangue, AVIS). Blood processing and distribution are exclusively managed by the Transfusion Medicine Unit.
Our procedures involve therapies and consultations for patients coming from other wards, for inpatients temporarily hospitalized within our ward and for outpatients. Medical offices that compose our Transfusion Medicine Unit are dedicated to patient blood management, bloodlettings/phlebotomies, transfusions, apheresis and sideropaenic anaemia treatment.
Data management and statistical analysis
Data concerning hospitalizations and COVID‐19 patients were collected as aggregates from our hospital discharge database. Data concerning the Transfusion Medicine Unit procedures were collected as aggregates using our internal database interface (Eliot, Engineering Ingegneria Informatica S.p.A., Italy) and downloaded as Excel spreadsheets. Subsequent data analysis was performed on Excel (Microsoft Office 2010, Microsoft Corp., Redmond, WA), Python (3.8) and GraphPad Prism 7.02 (GraphPad Software, San Diego, CA). Data were expressed as number of patients or blood/platelets (PLTs) units and, when possible, as a mean of three different years (2017, 2018 and 2019) with its maximum–minimum range. Statistical significance was assessed using a t‐test when comparing the same time lapse of two different years, while one‐way ANOVA was used to determine statistical significance of the same time lapse in the last 3 years (from 2017 to 2019) either including 2020 or not within the comparison. The significance was set at *p ≤ 0.05, **p ≤ 0.001 and ***p ≤ 0.0001.
RESULTS
Management of the donor centres
During the national lockdown period, Reggio Emilia donor centres were re‐organized to:
Lower the risk of contagion.
Avoid unnecessary blood collection.
To lower the risk of contagion, two small donor centres were temporarily closed and converted into COVID clinics. In the remaining operating centres, some of the personnel were appointed to check the temperature and health status of all donors immediately before their access. Social distancing measures were adopted to avoid overcrowding, and, after each donation, rooms and seats were sanitized. Donations were suspended for students and first donors; when not necessary, eligibility and control exams were halted.
Blood collection
Blood, PLTs and plasma donations are routinely planned with the donors by SMS alert or phone call and scheduled in order to adequately manage the blood bank. During the 2020 lockdown, the schedule was deeply modified to meet the hospital requirements.
According to the Italian Government instructions [3], our hospital re‐scheduled a large majority of surgical procedures. When possible, non‐urgent orthopaedics, cardiovascular and cancer surgeries were postponed or moved to non‐COVID hospitals. This had an impact on the total number of surgical interventions, especially during the most critical lockdown phase (i.e., March and April 2020, data not shown). As a consequence, the Transfusion Medicine Unit faced a decrease in blood components' requests, and blood donation schedules were all re‐considered in order to avoid excessive stored blood units.
Figure 1(a) shows that the number of red blood cells (RBCs) units prepared from whole blood donations between February and May 2020 decreased, particularly between March and April. Consequently, the available buffycoat‐derived PLTs units also diminished. Plateletapheresis was, thus, increased to allow a constant PLTs supply to our blood bank (Figure 1(b)).
FIGURE 1.
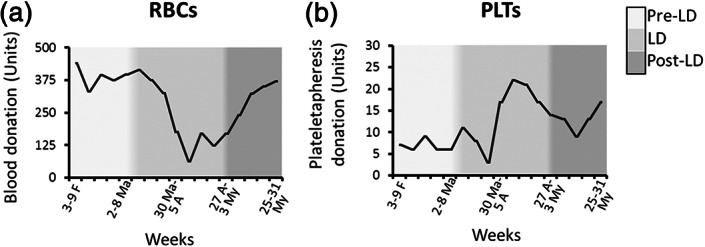
(a) Whole blood–derived RBCs, weekly donations between February and May 2020, and (b) platelets apheresis donations collected in the same period. LD, lockdown; RBCs, red blood cells; PLTs, platelets
Whole blood donations dedicated to group 0 negative (0−) (Supplementary Figure S1) and rare phenotypes reserved for specific cohorts of patients (i.e., thalassaemics and myelodysplastics) were preserved. Rare group donors were scheduled by direct phone call, while all the other appointments were cancelled by SMS.
Since plateletapheresis is a complex and invasive procedure, PLTs donors are generally fewer than blood donors. The collection of a sufficient amount of plateletapheresis‐derived units, therefore, represented a challenge for our recruiting personnel. To overcome this problem, our Transfusion Medicine Unit established a bank of frozen PLTs, which can be stored for up to 2 years. Between August and October 2020, our personnel collected and stored over 50 frozen PLTs units, according to Italian standards [14].
Furthermore, the CRS coordinated blood availability and distribution between the provinces according to the epidemic diffusion. In order to determine how this internal and local re‐organization of blood supply and transfusions affected the coordination with the other transfusion centres of our region, we also analysed the influx/efflux of blood units. Results are reported in Figure S2 of the Supplementary information.
Finally, since plasma can be stored frozen for several months, its collection was not interrupted. The donor centres extended the opening time, while appointments for plasma donations were re‐scheduled to avoid overcrowding and to allow the necessary sanitization (data not shown).
Blood transfusion—RBCs and PLTs
To understand how the pandemic affected the transfusion therapies, we compared the percentages of hospitalized patients transfused between February and May 2020 with those of 2017–2019 (Table 1). Taking into account the number of non‐COVID patients, the 2020 RBCs transfusion rate increased from 18.5% to 22.5%, while only a small number of COVID‐19 patients underwent a transfusion (161 over 1720, 9.4%). These data are in agreement with the hospitalizations that, during the lockdown period, dropped from a 15,771 mean in 2017–2019 to 10,520 in 2020 (that becomes 12,240 if we include COVID‐19 patients, Table SI).
TABLE 1.
Patients transfused and total patients hospitalized by the AUSL‐IRCCS di Reggio Emilia between February and May 2020 (absolute number), compared to the same period of 2017–2019 (mean)
| February–May | Transfused patients | Hospitalized patients | % Transf./Hosp. |
|---|---|---|---|
| 2017–2019 (mean value) | 2920 | 15,771 | 18.5 |
| 2020 COVID negative | 2373 | 10,520 | 22.5 |
| 2020 COVID positive | 161 | 1720 | 9.4 |
Following the suspension of elective and non‐urgent surgical interventions, RBCs transfusions significantly decreased when compared to the previous triennium, both in terms of patients and total units transfused (Figure 2(a)). Starting from this evidence, we further dissected the RBCs transfusions according to the applicant ward. Our data revealed that the most significant decrease of RBCs transfusions was observed for orthopaedic patients and, to a lesser extent, for cardiovascular surgery (Figure 2(b),(c), respectively). Interestingly, the decrease of RBCs usage in the orthopaedic interventions' accounts for about 35% of the total reduction and started around 15 days before the national lockdown. Conversely, there was no significant decrease in RBCs transfusion of cancer patients during the lockdown period and was only a slight decrease of the transfused units in the post‐lockdown period (Figure 2(d)).
FIGURE 2.
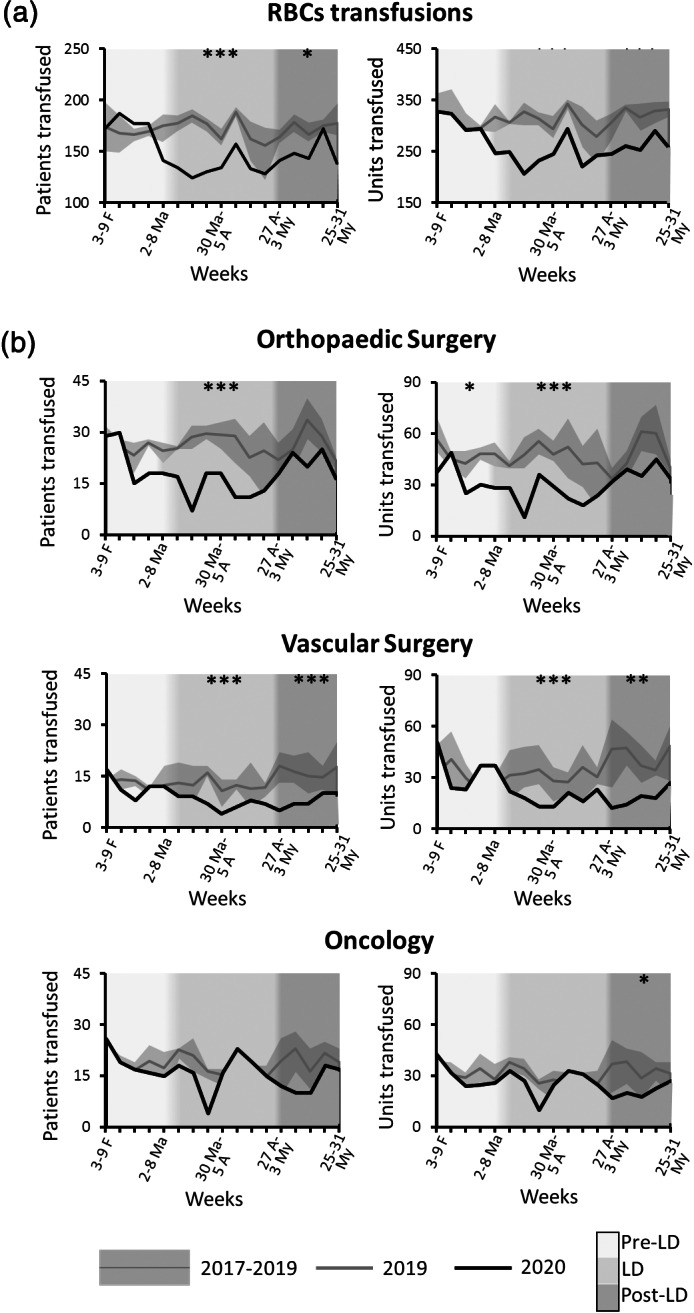
RBCs transfusions in 2020 (black lines), compared with the same period of the previous triennium. (a) Patients transfused with RBCs (left panel) and RBCs units transfused (right panel); (b) patients and units transfused for orthopaedics surgery; (c) patients and units transfused for cardiovascular surgery and (d) patients and units transfused for cancer other than haematological. *p ≤ 0.05, **p ≤ 0.001 and ***p ≤ 0.0001. RBCs, red blood cells
In parallel, we investigated PLTs transfusions, we observed a slight decrease in patients and units transfused during the lockdown (Figure 3(a)), although only these last data are significant (p < 0.01). PLTs transfusions started decreasing 3 weeks after the beginning of lockdown and came back to the 2019 level within 1 month. The largest amount of PLTs units transfused during the second month of lockdown (i.e., April 2020) came from plateletapheresis, as a consequence of the reduction of buffycoat‐derived pools following the decrease of whole blood donations (Figure 3(b)).
FIGURE 3.
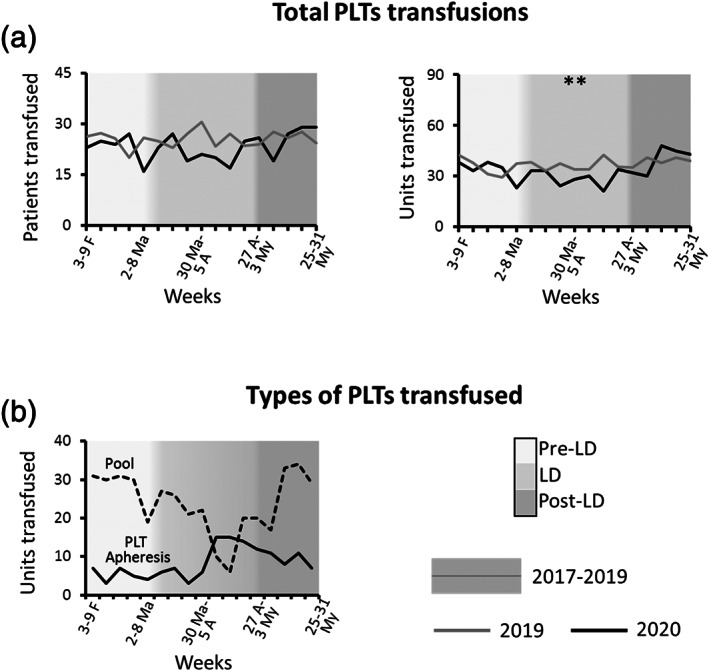
(a) Patients transfused with PLTs (left panel) and PLTs units transfused in 2020, compared to the same period of 2019 and (b) buffycoat‐derived (pool) and apheresis‐derived (PLT apheresis) PLTs units transfused between February and May 2020. *p ≤ 0.05, **p ≤ 0.001 and ***p ≤ 0.0001. LD, lockdown; PLT, platelet
Blood transfusion—RBCs and PLTs in onco‐haematological patients
As mentioned earlier, the establishment of the CORE pavilion implied an increase of hospitalized onco‐haematological patients between 2017 and 2019. Therefore, the effects of the lockdown on transfusion therapies for this sub‐group of patients are described in comparison with 2019 only.
In our hospital, onco‐haematological patients transfused with RBCs account for about 20% of the total, and their caregiving was preserved as much as possible during the first wave of the pandemic. Nevertheless, during the lockdown, we also observed a slight decrease of RBCs transfusions for these patients (Figure 4(a)). Although these data were not highly significant, it is supported by a similar observation on PLTs transfusions (Figure 4(b)).
FIGURE 4.
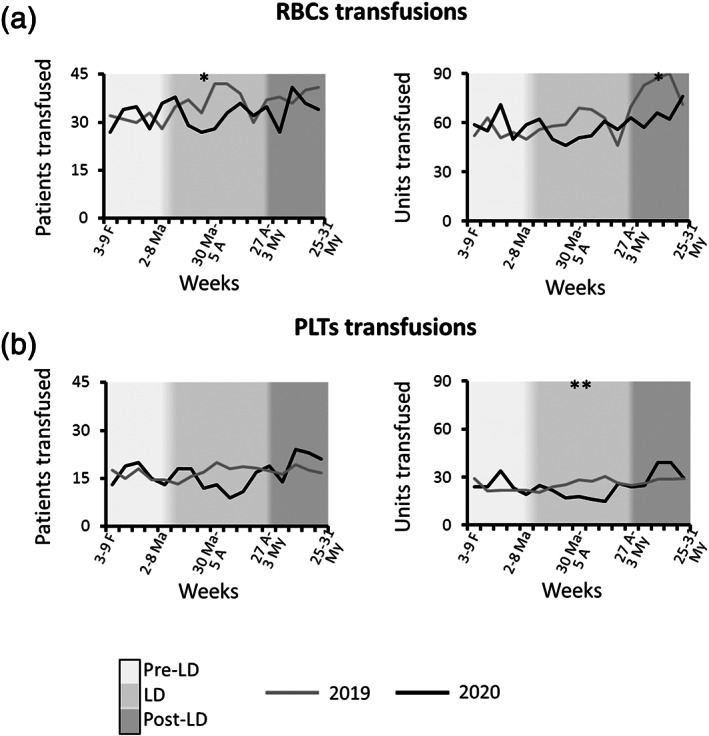
Patients and units transfused for onco‐haematological diseases: (a) RBCs and (b) PLTs. *p ≤ 0.05, **p ≤ 0.001. LD, lockdown; PLTs, platelets; RBCs, red blood cells
Transfusion medicine and immune‐haematology clinical practice
Following the official resolution of the Emilia‐Romagna region [14], our Transfusion Medicine Unit totally re‐organized its services to:
Limit the access of patients to emergencies and unavoidable therapies;
Guarantee transfusions and other therapies to patients coming from other wards;
Extend the opening times of medical offices to ensure an adequate number of procedures and, at the same time, allow the necessary room sanitization after each procedure;
Encourage medical phone consultations to guarantee therapeutic continuity for non‐urgent and chronic patients.
These measures affected all the inpatients' and outpatients' rooms that compose our Transfusion Medicine Unit: patient blood management; bloodlettings/phlebotomy; transfusion; apheresis and sideropaenic anaemia.
Figure 5 resumes the main procedures, procedures and medical consultations performed between February and May 2020, compared with the same period of 2019. The large majority of our procedures decreased during the lockdown. A significant decrease was observed in particular for medical consultations and plasma ‐exchange procedures required for inpatients coming from other hospital wards, as a consequence of the decreased hospitalizations. Despite Reggio Emilia province trying to preserve the healthcare services provided to oncological patients, the number of hospitalized cancer patients decreased, especially during the first weeks of lockdown. Moreover, no autologous or allogeneic stem cell collection for bone marrow transplantation was performed in March 2020 (Figure 5(a)).
FIGURE 5.
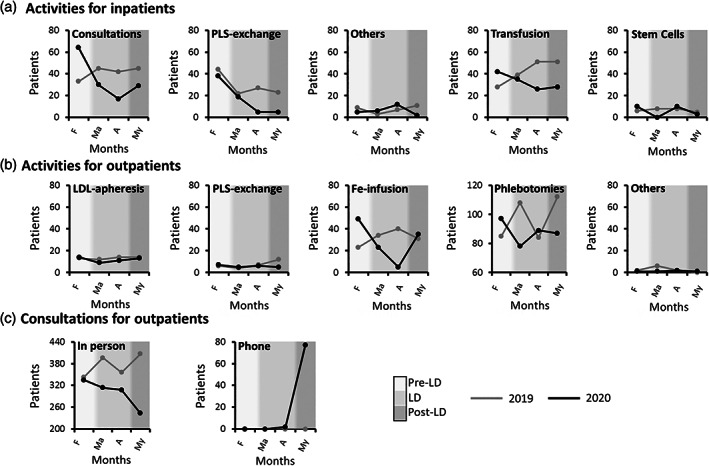
Transfusion medicine and immune‐haematology clinical practice procedures performed for: (a) inpatients coming from other wards; (b) outpatients and (c) medical consultations for outpatients. Black line indicates 2020 procedures, while grey line indicates 2019 procedures. LD, lockdown; LDL, low density lipoprotein; PLS, plasma
Procedures on outpatients decreased as well, particularly iron infusions on anaemic pre‐operative patients (Figure 5(b)). Between April and May, our physicians started implementing medical phone consultations for the outpatients (Figure 5(c)). The Patient Blood Management medical office, which routinely performs medical consultations to pre‐operative patients, temporarily closed due to the lack of elective surgeries imposed by the lockdown.
The treatment of chronically ill patients (thalassaemic, polycythaemic, familial hypercholesterolaemia patients among all) was preserved as much as possible, albeit the patients' appointments were spread over a longer range of time (from 8 am–12 noon to 8 am–6 pm).
All patients were only allowed to stay for the exact time of the hospital procedure. Visitors were not allowed, except when accompanying minors or fragile patients. When possible, on‐site appointments were substituted by remote consultations. Although not shown in this study, medical assistance by phone was implemented during the whole summer in order to be prepared for a second pandemic wave.
DISCUSSION
Between March and May 2020, the Italian Government declared a national lockdown, accompanied by further regional indications on the management of healthcare services that significantly changed the routine and emergency procedures all over the country [3, 10, 15]. The COVID‐19 outbreak also severely affected the procedures of the AUSL‐IRCCS di Reggio Emilia: the number of non‐COVID patients accessing the hospital between February and May 2020 was only 10,520, which is over 33% less than the same period of the previous triennium (15,771).
In accordance with what was previously reported, in our hospital, only a few hospitalized COVID‐19 patients might have received a blood transfusion as a consequence of the pathology (161 over 1720, 9.4%) [16].
However, the temporary suspension of elective surgeries, alongside the need to keep unaltered the clinical routine in some other departments (in particular, oncology and haematology), drastically impacted on our Unit activity. If we consider the non‐COVID patients hospitalized between February and May 2020 (Table 1), the RBCs transfusion rate rose from 18.5% to 22.5%. This evidence suggests that, in a scenario where the hospitalization of non‐serious patients was postponed or even diminished, it was chosen to prioritize the emergencies and the most severe cases that often require blood transfusions.
In terms of organization, the main changes for our Transfusion Medicine Unit involved blood donations, which were significantly reduced and re‐scheduled to meet the decrease need of blood components, as similarly described in other blood centres [17, 18, 19]. To avoid a surplus of RBCs, with the risk of discarding a large amount of expired units, all blood donations were temporarily reduced, except for those of rare groups. Adopting this strategy, our Transfusion Medicine Unit avoided RBCs units expiration for almost the whole lockdown. Moreover, the regional blood supply‐chain system, set up by CRS, buffered the distribution of RBCs units through the Emilia‐Romagna provinces from the least affected to the most affected by the pandemic (Figure S2 panels B and C). Reggio Emilia, for instance, received blood units from the CRS in April, after having faced the peak of COVID‐19 diffusion in the previous month.
After the initial reduction of the routine procedures, the healthcare supply for cancer and onco‐haematological patients was gradually restored following the national and regional indications [10, 15, 20]. Accordingly, a decrease in blood transfusions for the onco‐haematological patients was mainly concentrated in the most critical weeks (between the 20th of March and the 5th of April, Figure 4), while PLTs transfusion (mainly administered to prevent or treat bleeding episodes of onco‐haematological patients) remained constant for the whole lockdown duration.
To compensate for the decrease in buffycoat‐derived PLTs units, we increased the number of PLTs donations (Figure 2(c)). The latter are not easily collected in an adequate quantity to satisfy the request, and we thus adopted a procedure to store frozen PLTs [21]. PLTs cryopreservation is an alternative to the conventional storage temperature (25°C) that allows the product shelf‐life to increase from 5 days to up to 2 years.
Following the decrease of inpatients hospitalized by other wards, our physicians faced a significant decrease of medical consultations (Figure 5(a)) and plasma‐exchange procedures.
In summary, the COVID‐19 pandemic deeply impacted the healthcare systems at all levels, with important implications also for blood donation and transfusion [12, 22]. The mechanisms and procedures adopted to face this serious emergency were necessary to meet the safety requirements for donors, patients and staff. Our experience has, actually, many points in common with other Transfusion Medicine Units in Italy and other parts of the world [11, 12, 23, 24]. Among the strategies developed to meet this health emergency, we believe that, alongside the consolidated practices such as sanitizing procedures, re‐modulation of access and the use of personal protective equipment [25], a provision of frozen blood components that can be stored for several months could be helpful during emergency periods and should be promptly planned. Moreover, remote appointments were revealed as effective, especially for chronically ill patients, and it has been implemented after the lockdown.
Although our data are in agreement with recent literature about transfusion in COVID‐19 patients, [16] we must point out that they come from our internal database, which is not directly connected to clinical records and other hospital databases. Therefore, it is plausible that some data are underestimated, especially those relating to cancer patients (other than onco‐haematological). The latter can be hospitalized by several wards in our hospital, depending on tumour localization, and this implies higher tracing complexity; furthermore, when a physician prescribes a blood component, the diagnosis can sometimes not be well specified, thus generating missing data in our internal database. Nevertheless, our electronic system blocks blood component requirements in case of missing diagnosis, and we are confident that, despite a slight underestimation, the data presented herein are close to reality.
Finally, between February and May 2020, a ‘COVID‐19 diagnosis’ was not present in our database. Therefore, we cannot discriminate between RBCs and PLTs units transfused for COVID‐19 or for medical/surgical reasons. Nevertheless, we traced the requests for transfusions coming from the wards that hosted COVID‐19 patients, and we did not find any significant variation (data not shown).
In conclusion, during the first wave of the pandemic, our Transfusion Medicine Unit both avoided unnecessary blood collection and excessive stored blood units, preserving donor and staff safety. This result was reached by coordinating with the internal (hospital wards and donor centres) and external (i.e, CRS) stakeholders. However, these measures come from an emergency phase, and, despite their effectiveness, they should be implemented with other strategies (such as prioritizing blood use for hospitalized patients during blood shortage events) and integrated in appropriate risk management plans and safety procedures. At the time of writing, the spread of COVID‐19 is still beyond control in many countries worldwide; the knowledge acquired during the emergency should not be dispersed, but exploited, in order to define a more efficient healthcare management.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Appendix S1 Supporting information
ACKNOWLEDGEMENTS
The authors wish to thank all the staff, donors and blood associations volunteers who demonstrated their commitment to patients care during this serious health emergency.
Conceptualization: D.S., L.M., C.M.; Data curation: D.S., G.M., D.S., L.M., Formal analysis: D.S., P.M., P.G.R.; Writinig‐original draft: D.S., L.M., C.M.; Review and editing: L.M., C.M.; E.D.M.; Visualization: L.C., T.A.P.; Resources: R.B.; Supervision: R.B., C.M. All authors have read and agreed to the published version of the manuscript.
Schiroli D, Merolle L, Molinari G, et al. The impact of COVID‐19 outbreak on the Transfusion Medicine Unit of a Northern Italy Hospital and Cancer Centre. Vox Sang. 2022;117:235–242.
Funding information None
REFERENCES
- 1. Prezioso C, Pietropaolo V. COVID‐19: update of the Italian situation. J Neurovirol. 2020;26:834–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Conti S, Ferrara P, Mazzaglia G, et al. Magnitude and time‐course of excess mortality during COVID‐19 outbreak: population‐based empirical evidence from highly impacted provinces in northern Italy. ERJ Open Res. 2020;6:00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gazzetta Ufficiale della Repubblica Italiana Anno 161 Numero 62 – Edizione Straordinaria . Decreto Legge 9 Marzo 2020, n. 14: Disposizioni urgenti per il potenziamento del Servizio sanitario nazionale in relazione all'emergenza COVID‐19. Decreto del Presidente del Consiglio dei Ministri 9 Marzo 2020: 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell'emergenza epidemiologica da COVID‐19, applicabili sull'intero territorio nazionale [in Italian].
- 4. Giorgi Rossi P, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, et al. Characteristics and outcomes of a cohort of COVID‐19 patients in the province of Reggio Emilia. Italy PLoS One. 2020;15:e0238281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in northern Italy. N Engl J Med. 2020;383:88–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health. 2020;4:e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Benazzo F, Rossi SMP, Maniscalco P, Moretti B, Vaienti E, Ruggieri P, et al. The orthopaedic and traumatology scenario during Covid‐19 outbreak in Italy: chronicles of a silent war. Int Orthop. 2020;44:1453–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lambertini M, Toss A, Passaro A, Criscitiello C, Cremolini C, Cardone C, et al. Cancer care during the spread of coronavirus disease 2019 (COVID‐19) in Italy: young oncologists' perspective. ESMO Open. 2020;5:e000759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rosenbaum L. Facing Covid‐19 in Italy – ethics, logistics, and therapeutics on the epidemic's front line. N Engl J Med. 2020;382:1873–5. [DOI] [PubMed] [Google Scholar]
- 10. Direzione Generale Cura della Persona . Salute e Welfare Regione Emilia Romagna. PG/2020/176519 del 28 febbraio 2020; PG/2020/179766 del 29 febbraio 2020; PG/2020/191369 del 4 marzo 2020; PG/2020/0210546 del 10 marzo 2020 [in Italian].
- 11. Stanworth SJ, New HV, Apelseth TO, et al. Effects of the COVID‐19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020;7:e756–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Franchini M, Farrugia A, Velati C, Zanetti A, Romanò L, Grazzini G, et al. The impact of the SARS‐CoV‐2 outbreak on the safety and availability of blood transfusions in Italy. Vox Sang. 2020;115:603–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baron D, Franchini M, Goobie S, et al. Patient blood management during the COVID‐19 pandemic: a narrative review. Anaesthesia. 2020;75:1105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grazzini G, Berti P, Boccagni P & Standard in Medicina Trasfusionale. 3 ed. Milano, Italy: Società Italiana di Medicina Trasfusionale e Immunoematologia; 2017. [in Italian]. [Google Scholar]
- 15. Regione Emilia Romagna Atti Amministrativi Giunta Regionale . Delibera N. 404 del 2/04/2020, seduta n.16 [in Italian].
- 16. Barriteau CM, Bochey P, Lindholm PF, et al. Blood transfusion utilization in hospitalized COVID‐19 patients. Transfusion (Paris). 2020;60:1919–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leung JN, Lee CK. Impact of the COVID‐19 – a regional blood center's perspective. ISBT Sci Ser. 2020;15:362–4. [Google Scholar]
- 18. Wang Y, Han W, Pan L, Wang C, Liu Y, Hu W, et al. Impact of COVID‐19 on blood centres in Zhejiang Province China. Vox Sang. 2020;115:502–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pandey HC, Coshic P, Chippy CS, et al. Blood supply management in times of SARS‐CoV‐2 pandemic – challenges, strategies adopted, and the lessons learned from the experience of a hospital‐based blood Centre. Vox Sang. 2020;116:497–503. [DOI] [PubMed] [Google Scholar]
- 20. Gazzetta Ufficiale Serie Generale n. 45 del 23/02/2020. Decreto del Presidente del Consiglio dei Ministri. Disposizioni attuative del decreto‐legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell'emergenza epidemiologica da COVID‐19 [in Italian].
- 21. Valeri CR, Feingold H, Marchionni LD. A simple method for freezing human platelets using 6% dimethylsulfoxide and storage at‐80 C. Blood. 1974;43:131–6. [PubMed] [Google Scholar]
- 22. Yazer MH, Jackson B, Pagano M, Rahimi‐Levene N, Peer V, Bueno JL, et al. Vox Sanguinis international forum on transfusion services' response to COVID‐19: summary. Vox Sang. 2020;115:536–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Murphy C, Jackson B, Fontaine M. Tools for rapid analysis of blood usage and inventory during the COVID‐19 pandemic. Transfusion. 2020;60:2199–202. [DOI] [PubMed] [Google Scholar]
- 24. Colpo A, Astolfi L, Tison T, de Silvestro G, Marson P. Impact of COVID‐19 pandemic in the activity of a therapeutic apheresis unit in Italy. Transfus Apher Sci. 2020;59:102925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Granero V, Manzini PM, Bordiga AM. A multimodal practical approach in a transfusion medicine Centre to face the COVID‐19 outbreak. Blood Transfus. 2020;18:235–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting information


