Abstract
Background
Coxsackie virus group A type 16 (CoxA16) is the main pathogen and usually an alternative to or joins in prevalence with enterovirus 71 (EV71) causing hand, foot and mouth disease (HFMD). The objective of this study was to estimate the seroprevalence of CoxA16 antibody among people of various age groups by a systematic review and meta-analysis.
Methods
The literature of seroprevalence of CoxA16 antibody among people has been systematically searched through databases from the date of their establishment to Jan. 2021. Estimates of seroprevalence of CoxA16 antibody by gender and age groups have been summarized by using fixed- and random- effect models. All analyses have been conducted in STATA version 12.0 software.
Results
A total of 14 publications with 9 in English and 5 in Chinese containing 9562 samples were finally included in the meta-analysis. The seroprevalence of CoxA16 antibody reported in different studies range from 24.85 to 76.92 %. Meta-analysis has revealed that the seroprevalence of CoxA16 antibody was 56.3 % (95 %CI: 47.7 %~64.9 %) in the overall population and 55.1 % (95 %CI: 44.1 %~66.1 %) in the Chinese population. Subgroup analysis by gender has revealed that the seroprevalence of CoxA16 antibody was 56.1 % (95 %CI: 45.2 %~67.1 %) in males and 60.0 % (95 %CI: 50.0 %~69.9 %) in females. Subgroup analysis by age groups has revealed that the seroprevalence of CoxA16 antibody was 49.1 % (95 %CI: 36.2 %~62.0 %) in the 0 ~ 5 age group and 63.9 % (95 %CI: 53.1 %~74.7 %) in the over 5 age group. Begg’s funnel plots have suggested that there were no publication bias in all groups. Sensitive analysis has suggested that the result of the meta-analysis was stable.
Conclusions
The seroprevalence of CoxA16 antibody was closely related to age. Children under 5 years old were the main susceptible groups for CoxA16 and also the key groups for the prevention and control of HFMD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-021-00688-z.
Keywords: Seroprevalence; Coxsackievirus A16; Hand, foot and mouth disease(HFMD); Meta-analysis
Background
HFMD, an infectious disease caused by enterovirus, is common in children under 5 years of age, with the highest morbidity and mortality among children aged from 12 to 23 months [1, 2]. HFMD can cause fever, rashes and ulcers on hands, foot, and mouth. A small number of patients may develop neurological and cardiopulmonary complications such as aseptic meningitis, brainstem encephalitis, acute flaccid paralysis, pulmonary edema, and cerebral hemorrhage, or even death [3]. Viruses causing HFMD belong to the enterovirus family of the small RNA family, among which enterovirus 71 (EV-71) and Coxazivirus A16 (CoxA16) are the most common [4]. CoxA16 can be transmitted by fecal-oral route and close contact, easily causing outbreaks and epidemics in preschool children [5]. Since 1957, when the first HFMD case was reported in Toronto, HFMD has alternated or co-circulated with EV71, causing several pandemics worldwide [4–6]. In the past 20 years, HFMD has been prevalent in the Asia-Pacific region, including Singapore, Malaysia, Japan, South Korea, Thailand, Vietnam and Taiwan of China [7]. On May 2, 2008, HFMD was listed as a notifiable infectious disease in China.
China’s statutory reporting system for infectious diseases features a passive monitoring network, which means under-reporting is inevitable. At the same time, some cases may not be seen in hospitals, so they cannot be captured. The limitations of such a passive monitoring may lead to incomplete reflection of the prevalence of HFMD in China with the existing monitoring data. It has been reported that 50 % ~ 80 % of enterovirus infections are recessive infections with no or mild clinical symptoms, and only a few are manifested as dominant infections [8]. Serological investigation of the antibody levels of EV-A71 and CoxA16 in the population is the most effective way to indirectly reflect the prevalence of HFMD. In the meantime, it can be used to understand the dynamic changes of susceptibilities and immune levels of children at different age, so as to provide reference for the development of vaccination strategies and guide the prevention and control of HFMD.
A previous systematic review and meta-analysis has been conducted to evaluate the seroprevalence of enterovirus 71 antibody among children in China [9]. In this study, we retrospectively retrieved the published epidemiological literature on the seroprevalence of CoxA16 antibody, and the positive rates of CoxA16 antibody in different age groups have been comprehensively analyzed, so as to discuss the susceptibility of the population and the dynamic changes of immune status, and provide reference for the prevention and control of HFMD in the future.
Materials and methods
Search strategy
China National Knowledge Infrastructure (CNKI), WanFang Data, PubMed, EMbase, and the Cochrane Library to collect cross-sectional studies on the seroprevalence of CoxA16 antibody among people of various age groups from the date of their establishment to Jan. 2021 have been searched. The following keywords have been used in the literature search: (“hand foot and mouth disease” OR “HFMD” OR “coxsackievirus A16” OR “CA16” OR “CoxA16”) AND (“seroprevalence” OR “seroprevalent” OR “seronegative” OR “seropositive” OR “seroepidemiology” OR “seroepidemiological” OR “serologic” OR “serological” OR “antibody”). In addition, references of included literature have also been retrieved manually to avoid omission of relevant literature in the above-mentioned databases.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) literature on the seroprevalence of CoxA16 antibody among people published by June 2020; (2) type of study: a cross-sectional study that investigated the status of the seroprevalence of CoxA16 antibody; (3) positive rates of CoxA16 antibody can be calculated either explicitly or indirectly in the literature; (4) for repeated studies, the study with the largest sample size was selected. Exclusion criteria were as follows: (1) literature with obvious erroneous data or incomplete data; (2) types of research including review, conference, and other type of literature; (3) literature takes patients with hand foot and mouth disease as subjects.
Literature screening and data extraction
According to the inclusion criteria and exclusion criteria, two evaluators (PL and YC) have made a preliminary screening by filtering the title and abstract of the literature. After excluding obviously irrelevant literature, full text has been further read to determine the final results for inclusion. Two researchers (PL and YC) have independently screened the literature, extracted and cross-checked the data. In case of differences in the data extraction, the third researcher (AT) assisted in the discussion and decision-making. The missing data have been supplemented by contacting the authors. We have extracted the following information from each eligible article: first author, publication date, survey area, sample size, seroprevalence of CoxA16 antibody, assay method, age range of the studied population, grouping factors.
Quality assessment
The included studies have been evaluated for bias risk in cross-sectional studies according to 11 evaluation criteria recommended by the Agency for Healthcare Research and Quality (AHRQ), and each item has been answered with “Yes (scored 1 point)”, “No (scored 0 point)” or “Unclear (scored 0 point)” respectively [10]. The full score of quality evaluation is 11 points, with scores ranging from 0 to 3 points, from 4 to 7 points, and from 8 to 11 points representing low quality, medium quality and high quality, respectively.
Statistical analysis
The study has been conducted following the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement [11]. The pooled seroprevalence and 95 % confidence interval (CI) was the statistical effect size used to estimate the seroprevalence of CoxA16 antibody among people in different groups. Heterogeneity of the included studies has been determined by Cochran’s Q test and the I2 statistic. If the Cochran’s Q test was with P < 0.1 and I2 ≤ 50 %, indicating that there was no significant difference in the heterogeneity between studies, fixed-effect model was used for meta-analysis [12, 13], otherwise, random-effect model was adopted. Subgroup analysis by gender and age group have also been conducted in the meta-analysis. In addition, the stability of the meta-analysis results has been evaluated in the sensitivity analysis using studies that were excluded one by one. Finally, Begg’s funnel plot and Egger’s linear regression analysis have been used to evaluate publication bias [10]. All statistical analyses have been performed in the STATA 12.0 program (StataCorp LP, College Station, TX, USA). A P-value < 0.05 was considered statistically significant.
Results
Study search results
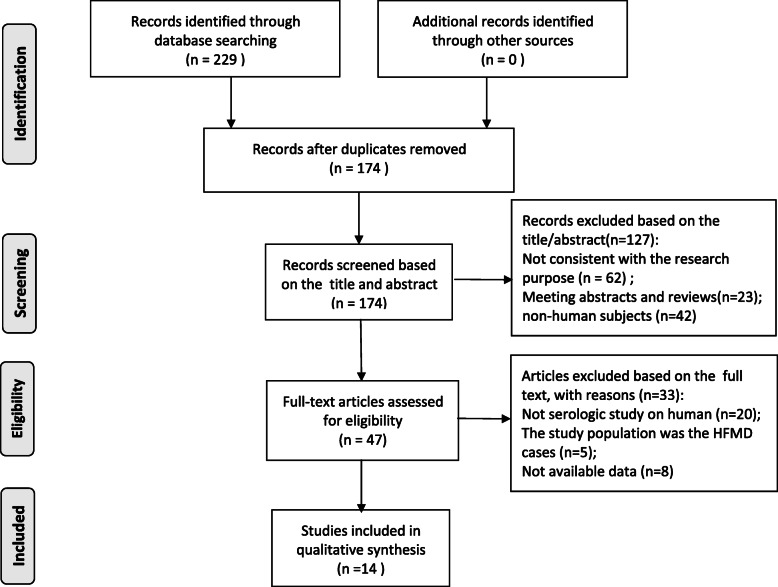
The two authors of this study searched the relevant databases according to the retrieval strategy respectively, and a total of 229 relevant studies have been searched at the initial inspection. The inclusion criteria and exclusion criteria have been used to independently conduct study screening, and the results of data extraction and quality assessment have been compared. After deleting duplicates and screening according to the inclusion and exclusion criteria, a total of 14 studies that met the selection criteria have been included in this meta-analysis [14–27]. A total of 9562 samples have been investigated in 14 studies, among which 5682 had positive neutralizing antibodies against CoxA16, and the seroprevalence of the CoxA16 antibody ranged from 24.85 to 76.92 %. Out of the 14 studies, 5 articles were in Chinese and 9 in English. In addition, 3 medium-quality studies and 11 high-quality studies were included in the studies. The basic information of all studies included in this meta-analysis has been shown in Table 1. The detailed flow chart of article selection for inclusion and exclusion has been presented in Fig. 1.
Table 1.
Basic information of the studies included in the meta-analysis
| First author | Publication year | Country | Location | Sample size | No. positive | Seroprevalence rate (%) | Assay method | Positive threshold | Age range | Group factors | AHRQ scores |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cheng [14] | 2016 | China | Jiangsu | 420 | 125 | 29.76 | NTA | 1:8 | 0–15 yrs | Age, gender | 8 |
| Han [15] | 2014 | China | Shandong | 1000 | 786 | 78.60 | ELISA | OD450 | 0–31 yrs | Age, gender | 8 |
| Mao [16] | 2009 | China | Henan | 337 | 123 | 36.50 | NTA | 1:8 | 7–30 mons | Age | 7 |
| Song [17] | 2020 | China | Tianjin | 171 | 107 | 62.57 | NTA | 1:8 | 0–35 yrs | Age, gender | 7 |
| Ang [18] | 2015 | Singapore | Singapore | 700 | 424 | 60.57 | NTA | 1:8 | 1–17 yrs | Age, gender, ethnic | 9 |
| Zhu [19] | 2012 | China | Jiangsu | 1530 | 1024 | 66.93 | NTA | 1:8 | all ages | Age | 7 |
| Lerdsamran [20] | 2018 | Thailand | Thailand | 696 | 438 | 62.93 | NTA | 1:8 | 6–18 yrs | Age, gender | 8 |
| Rabenau [21] | 2010 | Germany | Germany | 1378 | 989 | 71.77 | NTA | 1:8 | all ages | Age, gender | 8 |
| Wang [22] | 2016 | China | Shandong | 391 | 230 | 58.82 | NTA | 1:8 | all ages | Age, gender | 9 |
| Wang [23] | 2014 | China | Jiangsu | 715 | 400 | 55.94 | NTA | 1:8 | 20–50 yrs | Age, gender | 9 |
| Li [24] | 2013 | China | Guangdong | 900 | 390 | 43.33 | NTA | 1:8 | 1–9 yrs | Age, gender | 9 |
| Zhu [25] | 2010 | China | Mixed | 515 | 128 | 24.85 | NTA | 1:8 | 1–5 yrs | Age | 8 |
| Zhu [26] | 2018 | China | Fujian | 230 | 176 | 76.52 | NTA | 1:8 | all ages | Age, gender | 8 |
| Li [27] | 2017 | China | Tianjin | 420 | 125 | 29.76 | NTA | 1:8 | all ages | Age, gender | 8 |
Fig. 1.
Flow chart of the literature retrieval and selection process
Seroprevalence of CoxA16 antibody
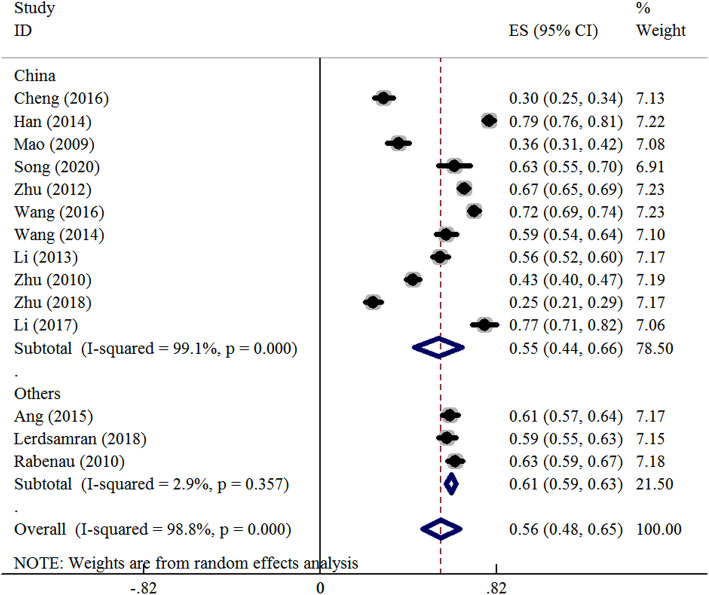
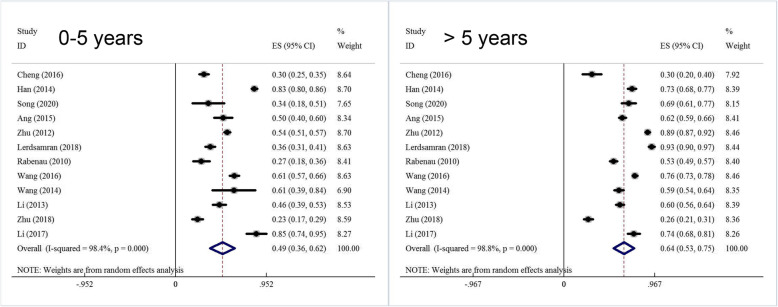
Meta-analysis has been performed on the overall population and stratified based on different genders and age groups. A summary of the meta-analysis has been shown in Table 2. According to the heterogeneity test, significant heterogeneity was found among the studies, and the random-effect model has been used for meta-analysis. The results have showed that the seroprevalence of CoxA16 antibody was 56.3 % (95 %CI: 47.7 %~64.9 %) in the overall population and 55.1 % (95 %CI: 44.1 %~66.1 %) in the Chinese population (Fig. 2). Subgroup analysis by gender has revealed that the seroprevalence of CoxA16 antibody was 56.1 % (95 %CI: 45.2 %~67.1 %) in males and 60.0 % (95 %CI: 50.0 %~69.9 %) in females (Fig. S1 in supplemental materials). Subgroup analysis by age groups has revealed that the seroprevalence of CoxA16 antibody was 17.5 % (12.4 %~24.5 %) in the < 1 age group, 37.5 % (31.2 %~45.5 %) in the 1 ~ 3 age group, 50.8 % (41.6 %~60.0 %) in the 4 ~ 5 age group, 49.1 % (95 %CI: 36.2 %~62.0 %) in the 0 ~ 5 age group and 63.9 % (95 %CI: 53.1 %~74.7 %) in the over 5 age group (Fig. 3).
Table 2.
Meta analysis results of the seroprevalence of CV-A16 (with 95 % confidence interval) in people by ethnicity, gender and age group
| Group | Seroprevalence (%) | 95 %CI (%) | Heterogeneity (P-value) | I2 (%) | Model | Begg’s (P-value) | Egger’s (P-value) |
|---|---|---|---|---|---|---|---|
| Ethnicity | |||||||
| Overall | 56.3 | 47.7 ~ 64.9 | < 0.001 | 99.1 | Random | 0.228 | 0.105 |
| Chinese | 55.1 | 44.1 ~ 66.1 | < 0.001 | 98.8 | Random | 0.335 | 0.156 |
| Others | 61.0 | 58.8 ~ 63.2 | 0.357 | 2.9 | Fixed | 0.224 | 0.135 |
| Gender | |||||||
| Male | 56.1 | 45.2 ~ 67.1 | < 0.001 | 98.0 | Random | 0.436 | 0.213 |
| Female | 60.0 | 50.0 ~ 69.9 | < 0.001 | 97.4 | Random | 0.640 | 0.202 |
| Age | |||||||
| < 1 yrs | 17.5 | 12.4 ~ 24.5 | < 0.001 | 88.6 | Random | 0.336 | 0.215 |
| 1–3 yrs | 37.5 | 31.2 ~ 45.5 | < 0.001 | 92.3 | Random | 0.569 | 0.425 |
| 4−5yrs | 50.8 | 41.6 ~ 60.0 | < 0.001 | 87.6 | Random | 0.758 | 0.628 |
| 0 ~ 5 yrs | 49.1 | 36.2 ~ 62.0 | < 0.001 | 98.4 | Random | 0.837 | 0.266 |
| > 5 yrs | 63.9 | 53.1 ~ 74.7 | < 0.001 | 98.8 | Random | 0.115 | 0.380 |
Fig. 2.
Forest plots for the seroprevalence of CoxA16 antibody among people in the overall population
Fig. 3.
Forest plots for the seroprevalence of CoxA16 antibody among people in different age groups
Sensitivity analysis and publication bias
A sensitivity analysis has been carried out by calculating the pooled seroprevalence of CoxA16 antibody of the remaining studies after excluding one study at a time. The results of the sensitivity analysis have showed that the meta-analysis results were stable. In addition, there was no evidence of publication bias in the current meta-analysis according to the Begg’s funnel plots and Egger’s linear regression test, the results have been shown in Table 2 (Fig. S2 and S3 in supplemental materials).
Discussion
CoxA16 virus is a common enterovirus that causes acute infection in children. It alternates or joins in prevalence with EV71 virus and is the main pathogen of HFMD. CoxA16 infection has become a major public health issue in the western pacific region due to its high transmission rate, especially in recent years [28]. Therefore, it is very important to carry out study on the determination of CoxA16 neutralizing antibody, so as to understand and predict the epidemic trend of HFMD and put forward prevention and control measures.
The present meta-analysis included 14 published studies containing a total of 9562 subjects, among which 5682 had positive neutralizing antibodies against CoxA16. The positive rate of CoxA16 neutralizing antibody in the serum of healthy people was relatively high with 56.3 % (95 %CI: 47.7 %~64.9 %) in the overall population and 55.1 % (95 %CI: 44.1 %~66.1 %) in the Chinese population. The meta-analysis also showed that the positive rate of CoxA16 neutralizing antibody was slightly higher in females than in males. This result was consistent with previous studies conducted in China, Singapore and Germany [17, 18, 21].
The meta-analysis also showed that the positive rate of CoxA16 antibody increased gradually from 1 to 5 years old and remained at a high level after 5 years old. Unfortunately, the positive rate of CoxA16 neutralizing antibodies was not analyzed for infants under 12 months of age. Studies have shown that with the natural attenuation of mother-to-child antibody, the antibody level of newborns decreased gradually from birth to the first year of life. A mother-newborn matching study in Jiangsu, China, found that the average maternal antibody positive rate at birth was 90 %, higher than EV-A71 infection level. However, the antibody level attenuated rapidly in infants of 0 ~ 12 months, which was similar to the change trend of EV-A71. After 1 year of age, antibody levels gradually increased with time due to increased exposure opportunities [19].
A retrospective study of the seroepidemiology of antibodies against EV71 and CoxA16 in prenatal women and their infants conducted by Mao et al. showed that the level of maternal antibody titers decreased dramatically during the first 7 months and remained at a relatively low level thereafter [16]. During the period of 4 ~ 6 years old, children began to study in kindergartens and live together with others, which may lead to increased exposure and infection opportunities of enterovirus and more likely to get and spread HFMD. After that period, children’s antibody level to enterovirus will gradually rise. Rabenau et al. found that the positive rate of CoxA16 neutralizing antibody in German children increased from 27 % in 1–4 years old to 52 % in 5–9 years old [21]. The present meta-analysis showed that CoxA16 antibody levels were significantly higher in children over 5 years of age than in children under 5 years old.
There are some limitations in this meta-analysis. Firstly, there was considerable heterogeneity in this meta-analysis, the causes may relate to the study area, the age range of the study population, the sampling time of objects in the studies and other factors. Due to the insufficient information provided in the original literature, subgroup analysis and meta-regression analysis cannot be carried out further. Secondly, the included literature was mainly from China, and the included regions are not evenly distributed, so the meta-analysis results may not reflect the positive rate of CoxA16 neutralizing antibody in the whole population. Finally, only English and Chinese literatures were included in this meta-analysis, so language bias may exist in this study.
Conclusions
In summary, this meta-analysis showed that the proportion of CoxA16 virus infected population is relatively large, among which the CoxA16 positive rate is the lowest among people under 5 years old. The newborns’ level of CoxA16 neutralizing antibody from mothers is limited, and given there is no efficient vaccine specifically for this so far, the key to control the CoxA16 epidemic lays in prevention and control of children under 5 years old. In the future, public health departments should strengthen the publicity, education and prevention guidance on the prevention and control of HFMD, and urge parents to take personal protection for infants and young children.
Supplementary Information
Additional file 1: Figure S1. Forest plots for the seroprevalence of CoxA16 antibody among people in different genders.
Additional file 2: Figure S2. Sensitive analysis for the seroprevalence of CoxA16 antibody among people in the overall population.
Additional file 3: Figure S3. Begg’s funnel plot for the seroprevalence of CoxA16 antibody among people in the overall population.
Additional file 4: Table 1. The search strategy of seroprevalence of CoxA16 antibody among people.
Acknowledgements
Not applicable.
Abbreviations
- HFMD
Hand foot and mouth disease
- CoxA16
Coxsackie virus group A type 16
- EV-71
Enterovirus 71
- AHRQ
Agency for Healthcare Research and Quality
- PRISMA
Preferred reporting items for systematic reviews and meta-analysis
- 95% CI
95% confidence interval
Authors' contributions
PL and FG participated in the design of the study and performed the statistical analysis, YC and AT performed the data extraction and statistical analysis, and JBY participated in its design and coordination and helped to revise the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by Zhoushan Science and Technology Project (2017C31125, 2018C31118, 2017B02).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Fan Gao, Email: xinran-83-08-18@163.com.
Jian-Bo Yan, Email: yanjianbo02@163.com.
References
- 1.Chang ZR, Zhang J, Sun JL, Zhang WD, Wang ZJ. Epidemiological features of hand, foot and mouth disease in China, 2008–2009. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(7):676–80. [PubMed] [Google Scholar]
- 2.Wang XF, Lu J, Liu XX, Dai T. Epidemiological features of hand, foot and mouth disease outbreaks among Chinese preschool children: a meta-analysis. Iran J Public Health. 2018;47(9):1234–43. [PMC free article] [PubMed] [Google Scholar]
- 3.Cai K, Wang Y, Guo Z, Yu H, Li H, Zhang L, Xu S, Zhang Q. Clinical characteristics and managements of severe hand, foot and mouth disease caused by enterovirus A71 and coxsackievirus A16 in Shanghai, China. BMC Infect Dis. 2019;19(1):285. doi: 10.1186/s12879-019-3878-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji H, Fan H, Lu PX, Zhang XF, Ai J, Shi C, et al. Surveillance for severe hand, foot, and mouth disease from 2009 to 2015 in Jiangsu province: epidemiology,etiology, and disease burden. BMC Infect Dis. 2019;19(1):79. doi: 10.1186/s12879-018-3659-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fan X, Jiang J, Liu Y, Huang X, Wang P, Liu L, Wang J, Chen W, Wu W, Xu B. Detection of human enterovirus 71 and Coxsackievirus A16 in an outbreak of hand, foot, and mouth disease in Henan Province, China in 2009. Virus Genes. 2013;46(1):1–9. doi: 10.1007/s11262-012-0814-x. [DOI] [PubMed] [Google Scholar]
- 6.Noisumdaeng P, Sangsiriwut K, Prasertsopon J, Klinmalai C, Payungporn S, Mungaomklang A. Complete genome analysis demonstrates multiple introductions of enterovirus 71 and coxsackievirus A16recombinant strains into Thailand during the past decade. Emerg Microbes Infect. 2018;7(1):214–20. doi: 10.1038/s41426-018-0215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puenpa J, Wanlapakorn N, Vongpunsawad S, Poovorawan Y. The history of enterovirus A71 outbreaks and molecular epidemiology in the Asia-Pacific Region. J Biomed Sci. 2019;26(1):75. doi: 10.1186/s12929-019-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deng AP, Zhang YH, Sun LM, Zeng HR, Li W, Ke CW, et al. Survey on the recessive infection of pathogen to hand-foot-mouth disease among healthy adults and children in Guangdong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33(2):189–91. [PubMed] [Google Scholar]
- 9.Yang B, Wu P, Wu JT, Lau EH, Leung GM, Yu H, Cowling BJ. Seroprevalence of enterovirus 71 antibody among children in china: a systematic review and meta-analysis. Pediatr Infect Dis J. 2015;34(12):1399–406. doi: 10.1097/INF.0000000000000900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang Y, Wang S, Zhang L, Guo Z, Huang Z, Tu C, Zhu BP. Risk factors of severe hand, foot and mouth disease: a meta-analysis. Scand J Infect Dis. 2014;46(7):515–22. doi: 10.3109/00365548.2014.907929. [DOI] [PubMed] [Google Scholar]
- 11.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and metaanalysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hedges LV, Vevea JL. Fixed-and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504. doi: 10.1037/1082-989X.3.4.486. [DOI] [Google Scholar]
- 14.Cheng C, Pang HY. Seroepidemiologic investigation of enterovirus CA16 among children in Donghai County. Chin J School Doctor. 2016;30(6):454–6. [Google Scholar]
- 15.Han XY, Pan J, Liu LZ, Yang GL, Guan HY, Wang CR. Serological investigation on hand foot and mouth disease in healthy population in Jinan. Chin J Health Lab. 2014;24(6):877–8. [Google Scholar]
- 16.Mao QY, Yang ZW, Yu X, et al. Epidemic tendency of neutralizing antibody against Enterovirus 71 and Coxsackievirus A 16 in Infants in Rural Area of Kaifeng City, Henan Province,China. Chin J Biologicals. 2009;22(9):911–3. [Google Scholar]
- 17.Song D. Serological survey of hand, foot and mouth disease among healthy people in Hebei District, Tianjin City. 2016 ~ 2019 Medical Information. 2020;33(8):147–9. [Google Scholar]
- 18.Ang LW, Tay J, Phoon MC, Hsu JP, Cutter J, James L, Goh KT, Chow VT. Seroepidemiology of Coxsackievirus A6, Coxsackievirus A16, and Enterovirus 71 infections among children and adolescents in Singapore, 2008–2010. PLoS One. 2015;10(5):e0127999. doi: 10.1371/journal.pone.0127999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu FC, Liang ZL, Meng FY, Zeng Y, Mao QY, Chu K, et al. Retrospective study of the incidence of HFMD and seroepidemiology of antibodies against EV71 and CoxA16 in prenatal women and their infants. PLoS One. 2012;7(5):e37206. doi: 10.1371/journal.pone.0037206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lerdsamran H, Prasertsopon J, Mungaomklang A, Klinmalai C, Noisumdaeng P, Sangsiriwut K, Tassaneetrithep B, Guntapong R, et al. Seroprevalence of antibodies to enterovirus 71 and coxsackievirus A16 among people of various age groups in a northeast province of Thailand. Virol J. 2018;15(1):158–62. doi: 10.1186/s12985-018-1074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabenau HF, Richter M, Doerr HW. Hand, foot and mouth disease: seroprevalence of Coxsackie A16 and Enterovirus 71 in Germany. Med Microbiol Immunol. 2010;199(1):45–51. doi: 10.1007/s00430-009-0133-6. [DOI] [PubMed] [Google Scholar]
- 22.Wang JX, Zhu SL, Wang J, Lin Y, Pei YW, Sun DP, Zhang Y, et al. Seroprevalence of Enterovirus A71 and Coxsackievirus A16 in Healthy People in Shandong Province, China. PLoS One. 2016;11(9):e0162373. doi: 10.1371/journal.pone.0162373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang X, Xing M, Zhang C, Yang Y, Chi Y, Tang X, Zhang H, Xiong S, Yu L, Zhou D. Neutralizing antibody responses to enterovirus and adenovirus in healthy adults in China. Emerg Microbes Infect. 2014;3(5):e30. doi: 10.1038/emi.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li W, Yi L, Su J, Lu J, Ke C, Zeng H, Guan D, Ma C, Zhang W, Xiao H, Li H, Lin J, Zhang Y. Seroprevalence of human enterovirus 71 and coxsackievirus A16 in Guangdong, China, in pre- and post-2010 HFMD epidemic period. PLoS One. 2013;8(12):e80515. doi: 10.1371/journal.pone.0080515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu R, Cheng T, Yin Z, Liu D, Xu L, Li Y, Wang W, Liu J, Que Y, Ye X, Tang Q, Zhao Q, Ge S, He S, Xia N. Serological survey of neutralizing antibodies to eight major enteroviruses among healthy population. Emerg Microbes Infect. 2018;7(1):215–21. doi: 10.1038/s41426-017-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu Z, Zhu S, Guo X, Wang J, Wang D, Yan D, Tan X, Tang L, et al. Retrospective seroepidemiology indicated that human enterovirus 71 and coxsackievirus A16 circulated wildly in central and southern China before large-scale outbreaks from 2008. Virol J. 2010;7:300. doi: 10.1186/1743-422X-7-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li P, Chen YM, Wang HL, Wei PN. Survey of neutralizing antibodies against EV71 and Cox A16 in healthy population in Wuqing district, Tianjin. Dis Surveillance. 2017;32(7):573–5. [Google Scholar]
- 28.Mao Q, Wang Y, Yao X, Bian L, Wu X, Xu M, Liang Z. Coxsackievirus A16: epidemiology, diagnosis, and vaccine. Hum Vaccin Immunother. 2014;10(2):360–7. doi: 10.4161/hv.27087. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Forest plots for the seroprevalence of CoxA16 antibody among people in different genders.
Additional file 2: Figure S2. Sensitive analysis for the seroprevalence of CoxA16 antibody among people in the overall population.
Additional file 3: Figure S3. Begg’s funnel plot for the seroprevalence of CoxA16 antibody among people in the overall population.
Additional file 4: Table 1. The search strategy of seroprevalence of CoxA16 antibody among people.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.