Abstract
In December 2019, with pneumonia-like clinical manifestations, a new severe acute respiratory syndrome coronavirus 2 emerged and quickly escalated into a pandemic. Since the first case detected in early March of last year, 8668 have died with an infection mortality rate of 1.52%, as of March 20, 2021. Bangladesh has been struck by the 2nd wave from mid-march 2021. As data on the second wave are sparse, the present study observed the demographic profile, symptoms, and outcomes of Coronavirus Disease 2019 (COVID-19) patients during this wave.
The study was conducted at Sheikh Russel National Gastroliver Institute on 486 admitted cases during the 2nd wave of COVID-19 in Bangladesh (March 24–April 24, 2021) using a cross-sectional study design and a convenient sampling technique.
Out of 486 cases, 306 (62.9%) were male, and 180 were female, with a mean age of 53.47 ± 13.86. The majority of patients (32.5%) were between the ages of 51 and 60. While fever and cough being the predominant symptoms (>70% cases), the most common co-morbidities were hypertension (41.4) and diabetes mellitus (39.4). Intensive care unit utilization rate was 25%, and a half of the patients had 51% to 70% tomographic lung involvement with an overall mortality rate of 19.3%. Older age, chronic renal disease, percentage of lung involvement, and intensive care unit necessity were important mortality determinants.
The present study gives an insight into the demographic profiles and outcomes of admitted patients with COVID-19 during the second wave at a covid dedicated hospital in Bangladesh.
Keywords: Bangladesh, COVID-19, demography, outcome, the second wave
1. Introduction
In December 2019, with pneumonia-like clinical manifestations, a new severe acute respiratory syndrome coronavirus syndrome emerged and quickly escalated into a pandemic.[1,2] The novel strain has been termed Coronavirus Disease 2019 (COVID-19) by the World Health Organization.[3] On January 30, 2020, the World Health Organization labeled it a Public Health Emergency of International Concern, and on April 11, 2020, it was designated as a pandemic.[4] Fever, cough, dyspnea, myalgia, anosmia, and tiredness are some of the clinical symptoms. Organ malfunction and death may ensue in severe cases. Severity seems to be associated with age, sex, and co-morbidity.[5] About 80% of the COVID-19 illnesses manifest as mild respiratory illness, and these patients who are mobile can typically be treated outside the hospital. Among the others, nearly 15% would require hospitalization (typically for moderate to severe pneumonia), and for the rest, 5% with a critical disease requiring more extensive assistance, usually in the form of intensive care with or without intubation.[6]
Despite enormous attempts to prevent further fast spread, 213 nations and territories have been affected globally, with 182,319,261 confirmed cases and 3,954,324 deaths as of July 2, 2021.[7] In Bangladesh, 568,706 people have tested positive for COVID-19 since the first case was confirmed in early March last year, and 8668 people have died, with an infection mortality rate of 1.52%, till March 20, 20201. Since early December 2020, overall case detection in Bangladesh has been declining, with daily case detection falling below 1000 on January 12, 2021. However, beginning March 16, 2021, there has been a significant increase in case detection, with daily cases exceeding 2000 as of 20 March.[8] As a result, it was predicted that Bangladesh would experience the second wave of covid beginning in mid-March 2021.
Data on the second wave are currently sparse among the Bangladeshi people. This would be one of the pioneer studies observing the demographic profile and outcomes of COVID-19 patients during the second wave. The study would also give an insight into the symptomatology, co-morbidity, and intensive care unit (ICU) utilization during this wave. This would be the baseline data to respond swiftly to combating the pandemic.
2. Methods
This was a cross-sectional observational study conducted at Sheikh Russel National Gastroliver Institute and Hospital, which is a tertiary level covid dedicated hospital in Dhaka. Patients were selected by convenient sampling during the peak of the 2nd wave of the covid in Bangladesh (March 24, 2021 to April 23, 2021). Consecutive patients of 18 years or above who admitted to COVID unit of Sheikh Russel National Gastroliver Institute and Hospital and confirmed as covid case either by positive reverse transcription-polymerase chain reaction (RT-PCR) or positive high-resolution computed tomography (HRCT) chest were included. Patients below 18 years or both RT-PCR and HRCT chest negative or unwilling to give consent were excluded. According to the revised Declaration of Helsinki, appropriate informed written consent was obtained from each patient or legal guardian. The Sheikh Russel National Gastroliver Institute and Hospital's Ethical and Scientific Committee approved the protocol.
Data were collected with a preformed data sheet containing demographics, symptoms, co-morbidity, computed tomography (CT) findings, ICU utilization, and outcome. HRCT of the chest was done if indicated. The same specialized radiologist studied and assessed all CT scan images. The severity score was determined for each patient based on lung involvement by assessing the percentage of each lobar involvement individually and assigning a value from 1 to 5, with score 1 representing 5% involvement, score 2: 5% to 25% involvement, score 3: 26% to 50% involvement, score 4: 51% to 75% involvement, and score 5: >75% involvement. Adding the individual lobar score patient's final score was calculated out of 25; the total lung involvement is then obtained by multiplying the total score by 4. Total lung involvement was classified as follows Minimal: 1% to 25% of total lung involvement, Mild: 26% to 50% total lung involvement, Moderate: 51% to 75% of total lung involvement, and Severe: >75%.[9,10] The outcome was evaluated by whether the patient was discharged or expired.
The Statistical Package for the Social Sciences (SPSS) version 23 (Statistical Package for the Social Sciences) for Windows, Version 23.0 (IBM Corporation, Armonk, New York) was used to perform the statistical analysis. Categorical data were presented as numbers and percentages. Numerical data were presented as mean and standard deviation. An unpaired t test was employed to assess quantitative variables, while the chi-square test was used to assess qualitative ones. Statistical significance was defined as P < .05.
3. Results
A total of 495 patients was admitted to the covid unit of Sheikh Russel National Gastroliver Institute and Hospital during the study period. Nine patients were excluded by exclusion criteria (2 patients had age below 18, and in 7 patients, both RT-PCR for covid and HRCT of chest were negative). Finally, 486 patients were enrolled for the study.
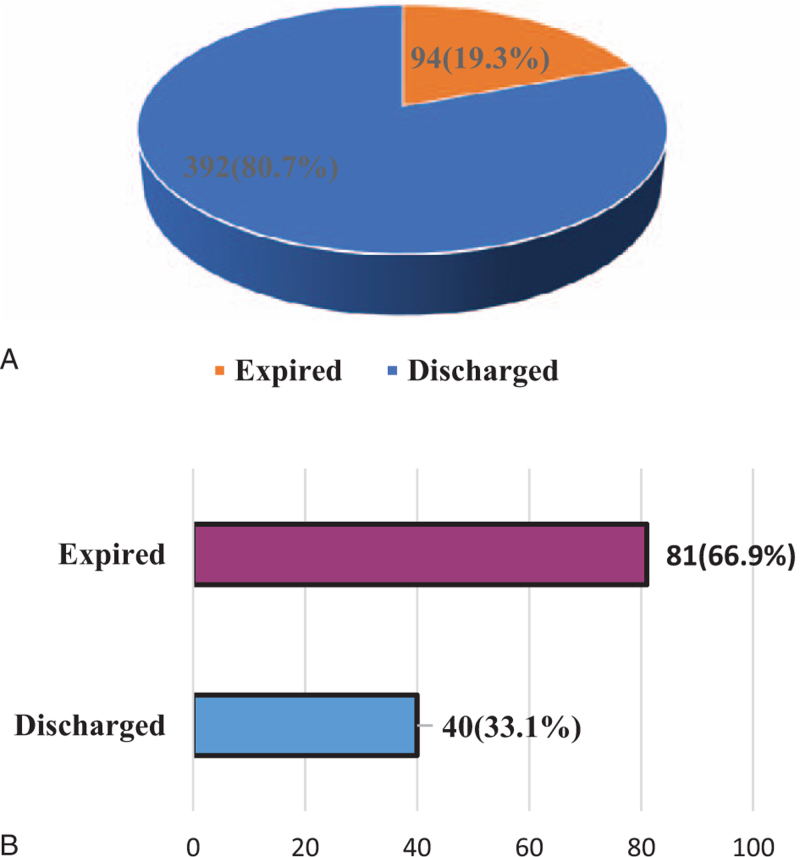
Out of 486, male patients were 306 (62.9%) and 37.1% were female. Most of the patients (50.2%) were in the age 41 to 60 age group. 30.2% were in the >60 age group. Only 1% of the total patients were <20 years. The mean age of the study population was 53.47 ± 13.86. The most common co-morbidity present among the study population was hypertension (HTN) (41.4%). Diabetes mellitus (DM) was present in 39.4% of patients, bronchial asthma in 9.4%, ischemic heart disease in 7.6%, chronic kidney disease (CKD) in 4.1%, and carcinoma was present in 2.5% of the patients. 33.5% had no co-morbidity, and 33.5% had at least 1 co-morbidity. Predominant symptoms among the patients were fever (78.2%) and cough (76.6%). 38.5% of patients had shortness of breath, 18.2% patients had diarrhea, and 14.5% had body ache. Anosmia, lethargy, and chest pain were present in less than 10% of the patients (Table 1). More than 65% of the study population had CT involvement. Among them, 6.2% were severe cases. Around 70% was minimal to mild CT changes. Out of 486 patients, 121 (24.9%) patients required ICU, and 75.1% of patients did not require ICU (Table 2). Overall mortality among the study population was 19.3% (Fig. 1A). Comparison of expired and discharged patients showed that sex and the number of co-morbidities are not significantly associated with mortality. But older age, presence of CKD, and inflammatory bowel disease, percentage of lung involvement, and ICU requirement are the significant factors associated with mortality (Table 3). It was observed that almost the majority (66.9%) of ICU patients had expired (Fig. 1B). Comparison of ICU patients with non-ICU patients showed that there was no significant difference in terms of sex, co-morbidities, and symptoms. But ICU patients were significantly older in age, they had a higher percentage of lung involvement and higher mortality compared to non-ICU patients (Table 4).
Table 1.
Clinicodemographic characteristics of the patients (n = 486).
| Characteristics | Group | Mean ± SD | n |
| Age (in years) | <20 | 5 (1.0) | |
| 21–40 | 53.47 ± 13.86 | 90 (18.5) | |
| 41–60 | 244 (50.2) | ||
| >60 | 147 (30.2) | ||
| Sex | Male | 306 (62.9) | |
| Female | 180 (37.1) | ||
| Number of co-morbidities | None | 163 (35.5) | |
| 1 | 163 (35.5) | ||
| 2 | 118 (24.3) | ||
| 3 or above | 41 (8.4) | ||
| Specific co-morbidity | HTN | 201 (41.4) | |
| DM | 192 (39.4) | ||
| BA | 46 (9.4) | ||
| IHD | 37 (7.6) | ||
| CKD | 20 (4.1) | ||
| Carcinoma | 12 (2.5) | ||
| COPD | 7 (1.4) | ||
| Liver disease | 6 (1.2) | ||
| IBD | 1 (0.2) | ||
| Others | 1 (0.2) | ||
| Predominant symptoms | Fever | 385 (78.2) | |
| Cough | 372 (76.6) | ||
| SOB | 187 (38.5) | ||
| Diarrhea | 89 (18.2) | ||
| Body ache | 70 (14.5) | ||
| Anosmia | 27 (5.5) | ||
| Lethargy | 19 (3.9) | ||
| Chest pain | 10 (2.0) |
Values are presented as frequency, percentage (in the parenthesis).
BA = Bronchial Asthma, CKD = Chronic Kidney Disease, COPD = Chronic Obstructive Pulmonary Disease, DM =Diabetes Mellitus, HTN =Hypertension, IBD =Inflammatory Bowel Disease, IHD = Ischemic Heart Disease, SD =Standard Deviation, SOB =Shortness of Breath.
Table 2.
CT involvement of lung and severity grade with ICU requirement.
| CT involvement of lung | Number of patients n (%) | ||
| Yes | 322 (66.25) | ||
| No | 164 (33.75) |
| Grade of CT involvement | Extent of involvement (%) | Mean ± SD | |
| Minimal | 1–25 | 64 (19.9) | 43.93 ± 19.87 |
| Mild | 26–50 | 161 (50.0) | |
| Moderate | 51–75 | 77 (23.9) | |
| Severe | >75 | 20 (6.2) | |
| ICU required | |||
| Yes | 121 (24.9) | ||
| No | 365 (75.1) | ||
Values are presented as frequency, percentage (in the parenthesis), and mean.
CT =Computed Tomography, ICU = Intensive Care Unit, SD =Standard Deviation.
Figure 1.
Outcome of the COVID-19 admitted patients during the 2nd wave. Overall hospital outcome of the patients (A). Outcome of ICU admitted cases (B). COVID-19 = Coronavirus Disease 2019, ICU = Intensive Care Unit.
Table 3.
Comparison of demography, symptoms, and co-morbidity between discharged and expired patients (n = 486).
| Expired (n = 94) | Discharged (n = 392) | ||||
| Outcome | n | % | n | % | P value |
| Age (mean ± SD) | 62.37 ± 12.74 | 51.34 ± 13.28 | ∗.001s | ||
| Sex | |||||
| Male | 66 | 70.2 | 240 | 61.2 | †.105ns |
| Female | 28 | 29.8 | 152 | 38.8 | |
| Co-morbidity | |||||
| DM | 44 | 36.4 | 148 | 40.5 | †.414ns |
| HTN | 49 | 40.5 | 151 | 41.4 | †.865ns |
| IHD | 11 | 9.1 | 26 | 7.1 | †.479ns |
| CKD | 8 | 6.6 | 12 | 3.3 | †.110ns |
| BA | 6 | 5.0 | 40 | 11.0 | †.051ns |
| COPD | 3 | 2.5 | 4 | 1.1 | †.268ns |
| Carcinoma | 4 | 3.3 | 8 | 2.2 | †.493ns |
| Liver Disease | 3 | 2.5 | 3 | 0.8 | †.152ns |
| IBD | 0 | 0.0 | 1 | 0.3 | †.564ns |
| Others | 1 | 0.8 | 0 | 0.0 | †.082ns |
| Major symptoms | |||||
| Fever | 74 | 78.7 | 311 | 79.3 | †.895ns |
| Cough | 60 | 63.8 | 312 | 79.6 | †.001s |
| Body ache | 4 | 4.3 | 67 | 17.1 | †.001s |
| Anosmia | 1 | 1.1 | 26 | 6.6 | †.034s |
| Diarrhea | 11 | 11.7 | 78 | 19.9 | †.065ns |
| SOB | 36 | 38.3 | 152 | 38.8 | †.931ns |
| Lethargy | 6 | 6.4 | 13 | 3.3 | †.001s |
| Chest pain | 2 | 2.1 | 8 | 2 | †.957ns |
| ICU required | 81 | 86.2 | 40 | 10.2 | †.001s |
s = significant, ns = not significant.
BA = Bronchial Asthma, CKD = Chronic Kidney Disease, COPD = Chronic Obstructive Pulmonary Disease, DM = Diabetes Mellitus, HTN =Hypertension, IBD =Inflammatory Bowel Disease, ICU =Intensive Care Unit, IHD =Ischemic Heart Disease, SD = Standard Deviation, SOB = Shortness of Breath.
P value reached from unpaired t test.
P value reached from chi-square test.
Table 4.
Comparison between ICU and non-ICU patients (n = 486).
| ICU (n = 121) | Non-ICU (n = 365) | ||||
| ICU required | n | % | n | % | P value |
| Age (mean ± SD) | 60.78 ± 13.47 | 51.05 ± 13.14 | ∗.001s | ||
| Sex | |||||
| Male | 83 | 68.6 | 223 | 60.9 | †.138ns |
| Female | 38 | 31.4 | 142 | 39.1 | |
| Co-morbidity | |||||
| DM | 44 | 36.4 | 148 | 40.5 | †.414ns |
| HTN | 49 | 40.5 | 151 | 41.4 | †.865ns |
| IHD | 11 | 9.1 | 26 | 7.1 | †.479ns |
| CKD | 8 | 6.6 | 12 | 3.3 | †.110ns |
| BA | 6 | 5.0 | 40 | 11.0 | †.051ns |
| COPD | 3 | 2.5 | 4 | 1.1 | †.268ns |
| Carcinoma | 4 | 3.3 | 8 | 2.2 | †.493ns |
| Liver Disease | 3 | 2.5 | 3 | 0.8 | †.152ns |
| IBD | 0 | 0.0 | 1 | 0.3 | †.564ns |
| Others | 1 | 0.8 | 0 | 0.0 | †.082ns |
| Major symptoms | |||||
| Fever | 99 | 81.8 | 285 | 77.9 | †.381ns |
| Cough | 83 | 68.6 | 290 | 79.2 | †.014s |
| SOB | 54 | 44.6 | 134 | 36.6 | †.121ns |
| Diarrhea | 15 | 12.4 | 74 | 20.2 | †.052ns |
| Body ache | 6 | 5.0 | 65 | 17.8 | †.001s |
| Lethargy | 6 | 5.0 | 13 | 3.6 | †.492ns |
| Chest pain | 5 | 4.1 | 5 | 1.4 | †.063ns |
| Anosmia | 1 | 0.8 | 26 | 7.1 | †.008ns |
| CT involvement | |||||
| 1–25 | 2 | 1.7 | 62 | 17.0 | |
| 26–50 | 32 | 26.4 | 129 | 35.3 | †.001s |
| 51–75 | 47 | 38.8 | 30 | 8.2 | |
| CT involvement (mean ± SD) | 60.14 ± 16.09 | 37.28 ± 17.3 | ∗.001s | ||
| Outcome | |||||
| Discharged | 40 | 33.1 | 352 | 96.4 | †.001s |
| Expired | 81 | 66.9 | 13 | 3.6 | |
s = significant, ns = not significant.
BA = Bronchial Asthma, CKD =Chronic Kidney Disease, COPD = Chronic Obstructive Pulmonary Disease, CT =Computed Tomography, DM = Diabetes Mellitus, HTN =hypertension, IBD = Inflammatory Bowel Disease, ICU = Intensive Care Unit, IHD = Ischemic Heart Disease, SD = Standard Deviation, SOB = Shortness of Breath.
P value reached from unpaired t test.
P value reached from chi-square test.
4. Discussion
The second wave of COVID-19 has struck the Indian subcontinent, causing widespread devastation. In comparison to the first wave, the second wave is spreading at a phenomenal speed. In recent articles, it has been referred to as a viral tsunami sweeping over India.[11] Being a country of this subcontinent, we are no exception. Beginning in mid-March 2021, Bangladesh has been hit by the second wave. This pioneering study on the second wave in our country would be very useful for establishing baseline data and comparing results.
The present study found most of the patients were in the age group of 41 to 60 (50.2%) with a mean age of 53.47 ± 13.86. Chen et al[12] in their study from Wuhan, found similar mean age and predominant age group. Another study in Spain found that the average age was the same as this one.[13] In this study, male predominance (62.9%) was seen among covid patients. Similar male predominance was also found in several studies done in China and Bangladesh.[12,14,15] It was observed that more than one-third (33.5%) of patients had no co-morbidity, 33.5% had 1 co-morbidity, and in 32.7% of patients, 2 or above co-morbidity was present. A study done by Revathishree et al[16] also found that about 57% of covid patients had 1 or more comorbidity. Among co-morbidities, HTN (413.4%) was the most common co-morbidity found in this study, followed by DM (39.4%), bronchial asthma (9.4%), and ischemic heart disease (7.6%). CKD was present in 4.1%, and carcinoma was present in 2.5% of the patients. Similarly, in other studies conducted in Bangladesh and other countries, DM and HTN were found to be the 2 most common co-morbidities among patients.[17–19] Fever (78.9%) and cough (76.6%) were the most predominant symptoms, with 18% of patients suffering from diarrhea. Studies done previously also found that fever and cough are the most common symptoms in covid patients.[13,15] In a study done by Mowla et al[17] also found that diarrhea may be present in 17% of covid patients. These symptomologies should be compared with the 1st wave in a further study among the Bangladeshi population.
In this study, the mean percentage of total lung involvement in HRCT of the chest of the hospitalized patient was 43.93 ± 19.87, and 50% of patients had lung involvement of 25% to 50%. A previous study in our country reported a mean percentage of lung involvement 33.43 ± 10.45 and found that most patients (29.69%) had lung involvement of <25%.[20] Out of 486 patients enrolled in this study, 121 (25%) patients required ICU. An earlier study done by Oliveira et al[21] and Abate et al[22] reported ICU utilization rates of 30% and 32%, respectively. But former studies from our country reported that ICU requirement was below 10% among admitted covid patients.[15,17] Higher ICU utilization rate in the present research is a notion of more severity of the disease variant. A future comparison study is required to explore higher lung HRCT involvement and increased ICU utilization.
In the present study, out of 486 patients, 392 were discharged (80.7%), while 19.3% expired. Expired patients were higher in age, and they have a significantly higher percentage of CKD. Oliveira et al,[21] in their study, found that older age, CKD, and ICU requirement are the significant factors related to mortality. When ICU and non-ICU patients were compared, there was no significant difference in terms of sex, symptoms, and co-morbidities, but the age of the ICU patients was significantly higher. Again, the percentage of lung involvement and mortality was also significantly higher in ICU patients. Pijls et al,[23] in their study, found that higher age is significantly associated with ICU requirement and Ahlstrand et al[24] reported CT severity score is a significant predictor of ICU admission for COVID-19. Our study is compatible with these studies.
Our work has several limitations; as a cross-sectional study, it was entirely confined to the in-hospital clinical course of the illness, and follow-up details were not available; therefore, no information on relapses was recorded. Furthermore, because the study site was a tertiary care referral center, the characteristics of mild to moderate illness may vary in population-based studies. However, other outcomes of interest primarily focus on the second wave, including recognized risk factors, overall hospital outcome, ICU utilization rate, and outcome, which would provide baseline data for a multicentered study or comparison with previous data or research from other countries.
5. Conclusions
This was one of the pioneer studies done during the 2nd wave of covid in Bangladesh. The study demonstrates clinicodemographic features and outcomes of the COVID-19 pandemic. It concludes that during 2nd wave, older patients were affected more, and the mortality rate was also higher than in previous studies. Cough and fever were the most predominant symptoms, while HTN and DM were the most common co-morbidity. The percentage of lung involvement was higher, and age, presence of CKD, and ICU requirement were the significant factors associated with mortality.
Acknowledgment
The authors express their gratitude to the institute and hospital where the research took place and all the participants and colleagues who made it successful.
Author contributions
Conceptualization: Mohammad Iqbal Hossain, Faruque Ahmed.
Data curation: Sultana Parvin, Mohammad Jane Alam, Subrata Podder, Raj Datta.
Formal analysis: Md Samiul Islam.
Investigation: Mohammad Iqbal Hossain, Mohammad Jane Alam, Subrata Podder, Raj Datta.
Methodology: Sultana Parvin, Mir Jakib Hossain.
Project administration: Faruque Ahmed.
Resources: Mohammad Jane Alam, Subrata Podder, Raj Datta.
Software: Md Samiul Islam.
Supervision: Touhidul Karim Majumder.
Validation: Mir Jakib Hossain.
Writing – original draft: Sultana Parvin.
Writing – review & editing: Touhidul Karim Majumder.
Footnotes
Abbreviations: CKD = Chronic Kidney Disease, COVID-19 = Coronavirus Disease 2019, CT = Computed Tomography, DM = Diabetes Mellitus, HRCT = High-resolution Computed Tomography, HTN = Hypertension, ICU = Intensive Care Unit, RT-PCR = Reverse Transcription-polymerase Chain Reaction.
How to cite this article: Hossain MI, Parvin S, Islam MS, Alam MJ, Podder S, Datta R, Majumdar TK, Hossain MJ, Ahmed F. Demographic profile and outcome of patients admitted to a COVID dedicated hospital in Bangladesh during the second wave. Medicine. 2021;100:37(e27281).
The authors have no funding and conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
References
- [1].Koo JR, Cook AR, Park M, et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis 2020;20:678–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bi Q, Wu Y, Mei S, et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis 2020;20:911–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lippi G, Sanchis-Gomar F, Henry BM. Coronavirus disease 2019 (COVID-19): the portrait of a perfect storm. Ann Transl Med 2020;8:497.doi: 10.21037/atm.2020.03.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020;91:157–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chan JF-W, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020;395:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China. JAMA 2020;323:1239–42. [DOI] [PubMed] [Google Scholar]
- [7].World Health Organization (WHO). Coronavirus disease (COVID-19) pandemic. 2021. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed July 4, 2021. [Google Scholar]
- [8].World Health Organization (WHO). Coronavirus disease (COVID-2019) Bangladesh situation reports. 2021. Available at: https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/. Accessed July 4, 2021. [Google Scholar]
- [9].Al-Mosawe AM, Abdulwahid Hm, Fayadh NAH. Spectrum of CT appearance and CT severity index of COVID-19 pulmonary infection in correlation with age, sex, and PCR test: an Iraqi experience. Egypt J Radiol Nucl Med 2021;52:40.doi: 10.1186/s43055-021-00422-3. [Google Scholar]
- [10].Francone M, Iafrate F, Masci GM, et al. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol 2020;30:6808–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jain VK, Iyengar KP, Vaishya R. Differences between first wave and second wave of COVID-19 in India. Diabetes Metab Syndr 2021;15:1047–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Iftimie S, Lopez-Azcona AF, Vallverdu I, et al. First and second waves of coronavirus disease-19: a comparative study in hospitalized patients in Reus, Spain. PLoS One 2021;16:e0248029.doi: 10.1371/journal.pone.0248029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ali MR, Hasan MA, Rahman MS, et al. Clinical manifestations and socio-demographic status of COVID-19 patients during the second-wave of pandemic: a Bangladeshi experience. J Infect Public Health 2021;S1876-0341(21)00177-5. doi: 10.1016/j.jiph.2021.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hossain HT, Chowdhury T, Majumder MI, et al. Demographic and clinical profile of 190 COVID-19 patients in a tertiary care private hospital of Dhaka, Bangladesh: an observational study. J Med 2020;21:82–8. [Google Scholar]
- [16].Revathishree K, Shyam Sudhakar S, Indu R, Srinivasan K. Covid-19 demographics from a tertiary care center: does it depreciate quality-of-life? Indian J Otolaryngol Head Neck Surg 2020;15:01–8. doi: 10.1007/s12070-020-02144-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mowla SGM, Azad KAK, Kabir A, et al. Clinical profile of 100 confirmed COVID-19 PATIENTS Admitted in Dhaka Medical College Hospital, Dhaka, Bangladesh. J Bangladesh Coll Phys Surg 2020;38:29–36. [Google Scholar]
- [18].Nelson LM, Simard JF, Oluyomi A, et al. US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA Intern Med 2020;180:1020–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Singh AK, Gupta R, Misra A. Comorbidities in COVID-19: outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr 2020;14:283–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Alam SZ, Muid SMAA, Akhter A, Rahman AKMS, Emran MA, Mostakim MTA. HRCT chest evaluation of COVID-19 patients: experience in Combined Military Hospital Dhaka, Bangladesh. J Bangladesh Coll Phys Surg 2020;38:21–8. [Google Scholar]
- [21].Oliveira E, Parikh A, Lopez-Ruiz A, et al. ICU outcomes and survival in patients with severe COVID-19 in the largest health care system in central Florida. PLoS One 2021;16:e0249038.doi: 10.1371/journal.pone.0249038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Abate SM, Ahmed Ali S, Mantfardo B, Basu B. Rate of intensive care unit admission and outcomes among patients with coronavirus: a systematic review and meta-analysis. PLoS One 2020;15:e0235653.doi: 10.1371/journal.pone.0235653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pijls BG, Jolani S, Atherley A, et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open 2021;11:e044640.doi: 10.1136/bmjopen-2020-044640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ahlstrand E, Cajander S, Cajander P, et al. Visual scoring of chest CT at hospital admission predicts hospitalization time and intensive care admission in Covid-19. Infect Dis (Lond) 2021;53:622–32. [DOI] [PMC free article] [PubMed] [Google Scholar]