Abstract
Background
Vaccination has the proven effectiveness in reducing disease burden. As the emergency program is moving towards completion in many countries, there is a new urgency to appropriately assess the societal health benefits in both the near and longer term.
Methods
Using an age-structured mathematical infection model, we evaluate the gains achievable by adopting the ongoing and the possible alternative vaccination strategies to reduce COVID-19 infections in the current pandemic as well as during the future successive waves in Norway. We explicitly consider three allocation strategies, with single focus group on either (i) the older age groups at high risk of dying or (ii) the core-sociable groups at high risk of exposure and onwards transmission, versus strategies focusing on both groups by (iii) switching among the high-risk to the core-sociable.
Findings
Following the Norwegian Institute of Public Health (FHI) schedule, we estimate that allocating vaccines in an age-descending order may reduce around one-third of the infections; while strategy considering age-specific sociability may contribute to an additional ∼10% fewer infections.
Interpretation
A key insight of our study is that prioritizing the high-risk and core-sociable groups may maximize the benefit due to both direct and indirect protections, and thus achieving the larger societal health benefits. Our analyses provides a quantitative tool to planning of future campaigns for Scandinavian and other countries with comparable infection-fatality ratios, demographies and public health infrastructure.
Funding
Research Council of Norway and the Penn State University.
Keywords: Vaccination, Strategies, Effectiveness, Norway
Research in context.
Evidence before this study
We did a literature search in PubMed for studies assessing vaccine allocation strategies of SARS-CoV-2 in English until May 2021, using the following key search terms: “vaccine”, “allocation”, “roll-out”, “Europe”, “Norway” and “strategy”. Preliminary evidence supports that vaccination targeting at the high-risk old people is the key to reducing the burden of mortality. However, projecting vaccine allocation strategies in the near and medium term, in particular in countries with low mortality rate, has not been fully investigated.
Added value of this study
Our study evaluates the gains achievable by adopting the ongoing and the possible alternative vaccination strategies to reduce COVID-19 infections in the current pandemic as well as during the future successive waves in Norway. A key insight of our study is that prioritizing the high-risk and core-sociable groups may maximize the benefit due to both direct and indirect protections, and thus achieving the larger societal health benefits. Such timely finding points to the urgency to keep high-risk and high-contact groups visiting vaccine-providing centers during the campaign to best manage the future circulation.
Implications of all the available evidence
Evidence of this study offers new guidelines and a quantitative tool for considering prioritization of vaccination for Scandinavian and other countries with comparable demographies, public health infrastructure and infection-fatality ratios.
Alt-text: Unlabelled box
1. Introduction
As mass vaccination campaigns commence worldwide, the most pressing question is how to achieve the greatest societal health benefits into the future. Most current policies towards attaining the goal of reducing COVID-19 related mortality by vaccinating the high-risk groups [1]. While evidence have shown a proven effectiveness of these policies in the early stage of vaccine rollout [2], [3], [4], [5], [6], [7], historical evidence from other infectious diseases suggests that direct protective measures may lose primacy in the intermediate and long term [8]. This motivates us to leverage the mathematical tools to tailor vaccine prioritization in the real-world setting.
The Norwegian Institute of Public Health (FHI) has scheduled the country's Covid-19 vaccination program, with the aim of vaccinating all adults over the age of 18 by mid-July 2021 [9]. The program, as broadly adopted across the world, prioritizes at-risk groups, allocating doses in descending order of age. Of note, the relatively low mortality rate and thus the infection-fatality ratio in Norway [10] may implicate alternative vaccination strategies. Here we, using an age-structured mathematical infection model, assess the effectiveness of the current strategy and its effectiveness relative to possible alternative strategies. We assess the effectiveness by focusing on the reduction in the number of infected people in the population, as this is a key metric when considering the number of hospitalizations and thus the health burden locally and for the country as a whole. Vaccine-induced reduction in virus circulation reduces health cost and the ultimate burden of mortality.
2. Methods
2.1. Modelling SARS-CoV-2 dynamics and vaccine allocation strategies
Building on [11], we extend the age-structured multi-compartmental SEIR model (eqs [1]–[5]) to allow for projections of SARS-CoV-2 dynamics with diverse vaccination roll-out strategies. The realistic nature of our age-structured model is represented by observed mixing pattern among age groups and the empirically documented age structure in the population. We include a mobility-term to link the reduction of contacts to reduced mobility. Details of the model and simulations are presented in the supplement. The model captures how transmission happens from symptomatic () and asymptomatic () infections with a force of infection () that depends on age ():
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
The force of infection on susceptibles in age-class at time is , where is the rate of seasonal transmission and is the normalized contact rate between age group and . We consider an all-or-nothing vaccine which provides perfect protection to a fraction, defined by vaccine efficacy, of the vaccinated individuals. To appropriately model the fraction of individuals vaccinated during a campaign, we define the rate of vaccination () as where and is the vaccine coverage and duration of vaccination in age group , respectively; is the vaccine efficacy (taken as 50%–90% in this analysis) [12]. We assume a one-year immunity duration () [13,14], and the same rate of the loss of immunity () for the recovered or vaccinated individuals. We assume an average latent period () and infection period () as 3 and 5 days, respectively [15]. The age-dependent fraction of symptomatic infections is characterized by [15]. Details of model parameters are provided in Table S1.
We initialize the analysis by assessing the effectiveness of the ongoing vaccination program in 23 Norwegian cities covering the range of demography. We assume that all cities follow the recommended prioritization from the FHI conservative vaccination schedule and vaccinate at the same rate. Thus, we translate the number of doses to the group-specific coverage in each city. To quantitatively assess the effectiveness of the current schedule, we consider an alternative strategy based on the sociability of various groups that would allocate vaccines in a descending rank of average age-specific number of daily contacts [16]. Across cities and strategies, we estimate the reduction of infections and mortality by the end of and two months after the campaign (i.e. mid-July and mid-September).
The model allows us to assess the effectiveness of different strategies across various annual vaccination campaigns. We consider programs that generally prioritize the vaccination for the elderly (75+ yr) but subsequently implement three strategies for the rest of the population: strategies with single focus groups on either (i) the older age groups at high risk of dying (hereafter “the age-focused strategy”) or (ii) the core-sociable groups at high risk of exposure and onwards transmission (hereafter “the sociability-focused strategy”), versus strategies focusing on both groups by (iii) switching among the high-risk to the core-sociable (hereafter “the switched strategy”). For each strategy, we evaluate the reduction of infections and mortality over a year for 23 cities and Norway as whole.
2.2. Role of funding source
The funders have no role in study design, data collection, data analysis, interpretation and writing of the report.
3. Results
3.1. Effectiveness of the FHI vaccination schedule
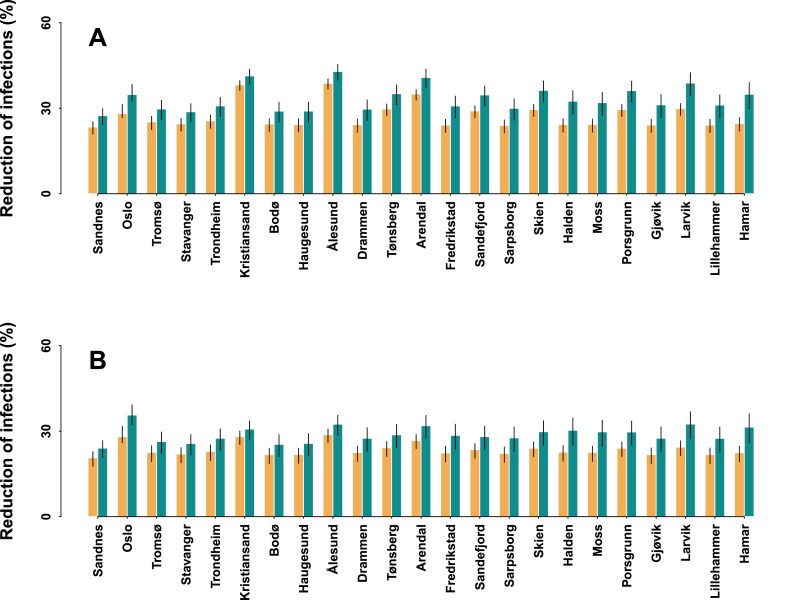
We first examine the effectiveness of the ongoing FHI vaccine roll-out strategy in settings spanning the demographic diversity of Norwegian cities by the end of the current campaign (Fig. 1A, Supplementary Table S2). Across cities and efficacies, the FHI strategy, allocating vaccines in the age-descending order, is predicted to lead to a median of 27% (21%–41%) fewer infections as compared to the absence of vaccination. Of the cities, Kristiansand, Ålesund and Arendal would expect the greatest reduction of infections, achieving gains of over 35%. Assuming the same number of doses as scheduled by the FHI, we demonstrate that allocating the doses by the sociability-descending strategy would be more effective than the scheduled age-descending strategy because of lowered circulation and thus enhanced indirect protection. Across cities we project a median of 35% (25%–47%) less infections by using the alternative strategy, though the incremental gain is predicted to vary among the cities. The variation of the effectiveness among cities may in part be due to the difference in the strength of travel-restrictions and thus the extent to which social contacts are modulated. Over two months after the end of the campaign, we estimate a median of 23% (19%–31%) and 29% (21%–40%) less infections by the FHI and the alternative strategy, respectively (Fig. 1B). Further analysis shows that the sociability-descending strategy may of the equivalent effectiveness with the scheduled age-descending strategy in terms of averting the mortality in the population (Fig. S1).
Fig. 1.
Effectiveness of the ongoing FHI vaccination schedule in 2021. Across cities the effectiveness of the vaccination by the end of (A) mid-July and (B) mid-September are estimated by the reduction of infections as compared with the baseline scenario without the vaccination. The effectiveness of age-descending strategy, designated by the FHI (yellow) is compared with the alternative, sociability-descending strategy (green). Cities are arranged in the descending order of the proportion of the elderly (over 75+ yr). Vaccine efficacy varies in 50%–90%. The median estimates and 95%CI are shown by colored bars and vertical lines, respectively.
3.2. Benefits from the switched vaccination among the high-risk and high-sociable groups
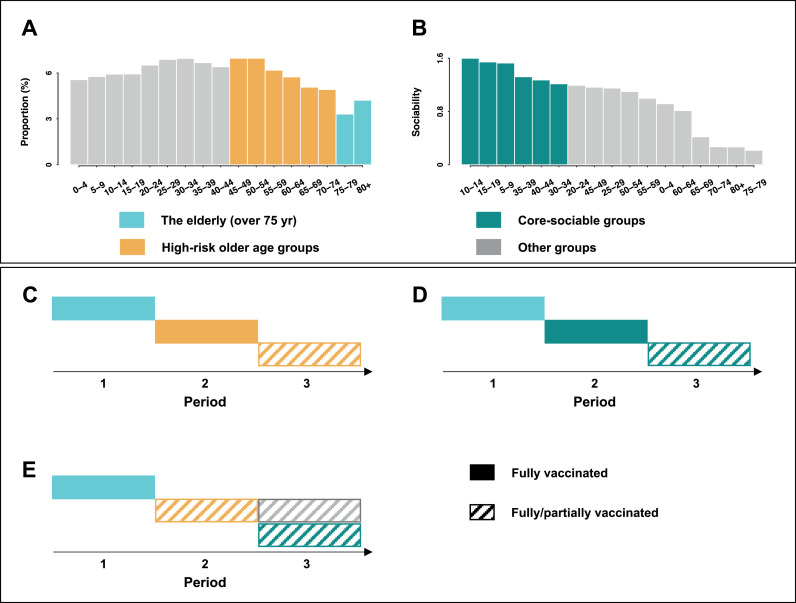
Given the likely transition towards endemicity [11,14], projecting trajectories to intermediate term circulation under different vaccination strategies is key to optimizing management. To highlight this conceptual issue, we lay out a framework considering annual vaccination campaign with prioritization to the elderly (over 75+ yr) and differing strategies to the rest of the population (Fig. 2).
Fig. 2.
Vaccine roll-out strategy in annual campaign. The elderly (over 75 yr), the high-risk older age groups and the core-sociable groups are identified from the (A) demography and the (B) marginal contacts over age groups. Across strategies (C-E) the elderly were fully vaccinate in the first period. Over the next 2 periods, strategies differ in the focused groups of the rest population. (C) ‘the age-focused strategy’ prioritizes and fully vaccinates the high-risk older age groups, and then, depending on the vaccine supply, fully/partially vaccinate the younger age classes. (D) ‘the sociability-focused strategy’ prioritizes and fully vaccinates the core-sociable groups in the second period, moving to all the unvaccinated individuals using the rest of the doses. (E) ‘the switched strategy’ switches the prioritization from the high-risk to the core-sociable ones in the two consecutive periods, together with the unvaccinated individuals in the last period. The coverage is dependent on the total vaccine supply.
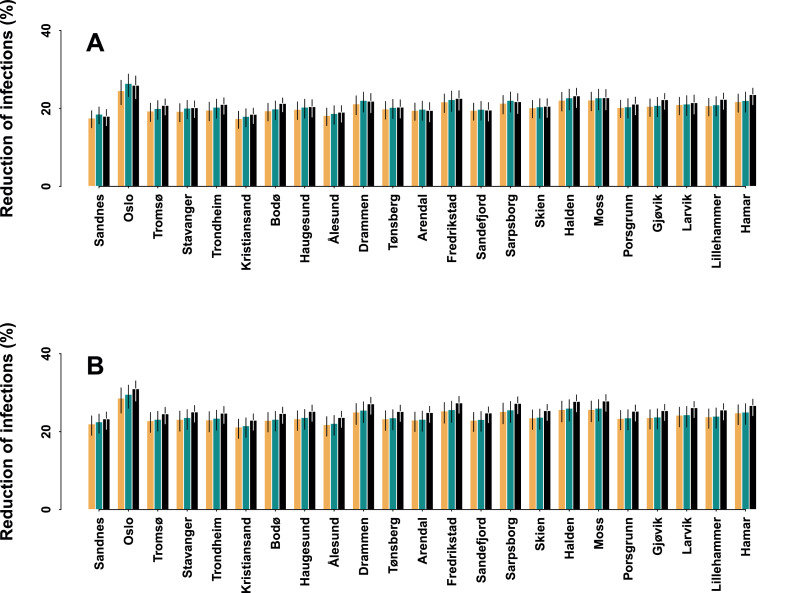
Assuming a one-year immunity duration, a fully re-opened society and an approx. 25% vaccine cover deficit (i.e. the proportion of the under 20 yrs), we first project the reduction of infections over a year for each city under scenarios with differing vaccine efficacies (Fig. 3A, Supplementary Table S3). By distributing the vaccination to core-sociable groups, either through the sociability-focused or switched strategy, our model predictions suggest a slightly larger reduction (∼2%) in the overall infections. This, using Oslo as example, is equivalent to up to 933 less infections than the age-focused strategy, assuming an 80% efficacy. Of note, the effectiveness of vaccination is associated with the vaccine cover deficit. Assuming a low (10%) deficit (Fig. 3B, Supplementary Table S3), we demonstrate a higher effectiveness of the switched strategy across cities, leading to a median of 25% (22%–30%) reduction of infections. If vaccinating with single focused groups, however, we project that the gains would be lowered by around 2%. For example, vaccination focus on single groups would lead to up to 652 fewer infections than the switched strategy in Oslo, assuming an efficacy of 80%. Across cities we document a comparable reduction of mortality by using the switched and age-focused strategies (Fig. S2).
Fig. 3.
Effectiveness of the vaccination strategies in annual campaigns. Assuming (A) approximately 25% (equivalent to the fraction of the under 20 yrs) and (B) 10% vaccine cover deficit, effectiveness of different roll-out strategies is estimated by the reduction of infections over a year as compared with the baseline scenario without the vaccination. The effectiveness of age-focused strategy (yellow) is compared with the sociability-focused (green) and the switched (black) strategies. Cities are arranged in the descending order of the proportion of the elderly (over 75 yr). Vaccine efficacy varies in 50%–90%. The median estimates and 95%CI are shown by colored bars and vertical lines, respectively.
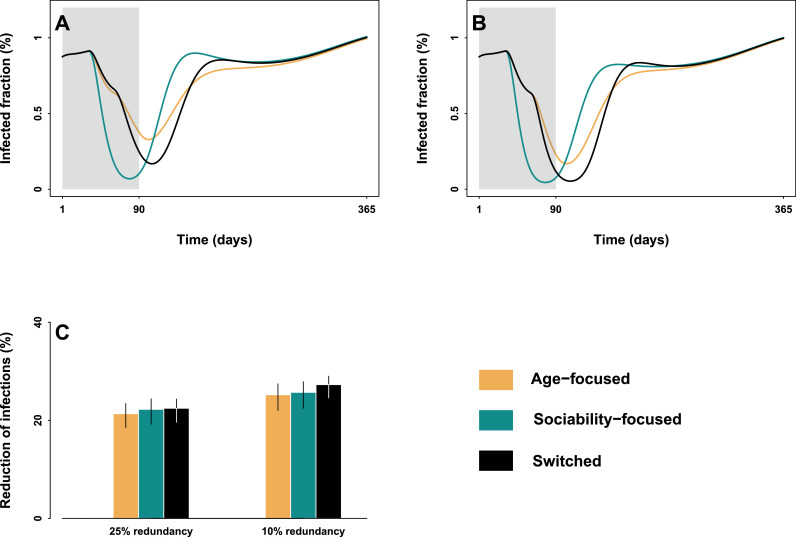
Zooming out the city-level evaluation to Norway as a whole is fundamental to guide policy options. Our scenario analysis shows that the relative effectiveness among strategies is highly dependent on the rate of vaccination and the extent that vaccination can modulate the dynamics of SARS-CoV-2 which in turn related to vaccine cover deficit (Fig. 4A,B). Assuming ∼25% deficit, vaccinating the high-risk older age groups is predicted to have the smallest effect on slowing and reducing the infected fraction. By contrast, the sociability-focused or the switched strategy may have stronger modulation on epidemic dynamics. If lowering the deficit to 10%, vaccination focusing on both the high-risk and core-sociable groups may have the greatest effect on the transmission, leading to the greatest reduction in the burden of infection over a year-long campaign (Fig. 4C).
Fig. 4.
Trajectories and effectiveness of the vaccination strategies in Norway. Assuming a 25% and 10% vaccine cover deficit, (A-B) trajectories of the infected fraction with 80% vaccine efficacy and (C) effectiveness in reducing infections over a year across efficacies by using the age-focused (yellow), the sociability-focused (green) and the switched (black) strategies is projected for Norway as whole.
4. Discussion
Using an age-structured mathematical model, we have assessed the societal health benefits of the ongoing vaccination program and projected public health benefits to various roll-out strategies of future campaigns. Following the FHI vaccination schedule, we estimate that allocating vaccines in an age-descending order may reduce around one-third of the infections. An alternative strategy of allocating vaccines according to age-specific sociability may contribute to an additional ∼10% fewer infections, together with a comparable reduction of mortality. As such vaccination targeting the high contact groups may be more advantageous, in countries such as Norway with relatively low mortality rate [10]. In settings with similar infection-fatality ratios [17,18], our framework provides a quantitative tool for considering prioritization of vaccination for Scandinavian and other countries with comparable demographies and public health infrastructure.
Our projections for future vaccination campaigns highlight that prioritizing the high-risk and core-sociable groups may maximize the benefit due to both direct and indirect protections, and thus achieving the larger societal health benefits. This finding points to the urgency to keep high-risk and high-contact groups visiting vaccine-providing centres during the campaign to best manage the future circulation. To prevent transmission among these key groups, we proposed that prioritizing the older age groups who are at high risk of dying and switching to high transmitters in consecutive stages of the campaign would be an appropriate approach. More importantly, we demonstrate that low vaccine deficit due to high willingness of the public for the vaccination and high vaccine supply is essential. Regardless of the demography, countries with low vaccine deficit should consider a two-pronged plan of targeting the high-risk and core-sociable groups.
Projecting our framework to other countries will need to tailor the social mixing and infection profile in each context. First, we assume a consistent social mixing patterns across cities. Specifying the mixing, together with the demography, will better characterize the heterogeneities in disease dynamics and contextualize the effectiveness of vaccination. Second, infectiousness and proportion of asymptomatic infections may vary over time, and thus are crucial directions to extend our study. Lastly, only the elderly over age 75 is considered in the prioritized groups when applying the framework to highlight the conceptual issue of relative effectiveness among strategies for future vaccination campaigns. Relaxing such assumption is the key to refining and translating our findings from broader range of perspectives such as economics.
Contributors
RL and NCS conceived and designed the analysis. RL performed the analysis. RL, ONB and NCS interpreted the results. RL wrote the manuscript. RL, ONB and NCS critically revised the manuscript and approved the final version.
Data availability statement
Not applicable.
Code availability
Code for the analysis is deposited in https://github.com/ruiyunli90/Corona-vaccine-Norway
Declaration of Competing Interest
The authors have nothing to disclose.
Acknowledgements
This work is funded by the Research Council of Norway Researcher Project for Young Talents 325041 (RL) and COVID-19 Seasonality Project 312740 (NCS), and the Penn State University Seed-Funded COVID-19 Project (ONB).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100200.
Contributor Information
Ruiyun Li, Email: ruiyun.li@ibv.uio.no.
Nils Chr. Stenseth, Email: n.c.stenseth@mn.uio.no.
Appendix. Supplementary materials
References
- 1.National Academies of Sciences, Engineering, and Medicine. Framework for equitable allocation of COVID-19 vaccine. Consensus Study Report. 2020 doi: 10.17226/25917. [DOI] [PubMed] [Google Scholar]
- 2.Biggerstaff M. Modeling strategies for the initial allocation of COVID-19 vaccines. 2020. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-10/COVID-Biggerstaff.pdf
- 3.Slayton RB. Modeling allocation strategies for the initial SARS-CoV-2 vaccine supply. 2020. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-08/COVID-06-Slayton.pdf
- 4.Bubar KM, Reinholt K, Kissler SM, et al. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science. 2020;21 doi: 10.1126/science.abe6959. eabe6959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore S, Hill EM, Dyson L, et al. Modelling optimal vaccination strategy for SARS-CoV-2 in the UK. 2020. https://www.medrxiv.org/content/10.1101/2020.09.22.20194183v2 [DOI] [PMC free article] [PubMed]
- 6.Matrajt L, Eaton J, Leung T, Brown ER. Vaccine optimization for COVID-19: Who to vaccinate first? Sci Adv. 2021;7 doi: 10.1126/sciadv.abf1374. eabf1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bucknera JH, Chowell G, Springborn MR. Dynamic prioritization of COVID-19 vaccines when social distancing is limited for essential workers. Proc Natl Acad Sci USA. 2021;118 doi: 10.1073/pnas.2025786118. e2025786118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lavine JS, King AA, Bjornstad ON. Natural immune boosting in pertussis dynamics and the potential for long-term vaccine failure. Proc Natl Acad Sci USA. 2011;108:7259–7264. doi: 10.1073/pnas.1014394108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The National Institute of Public Health. Vaccination Calendar 30.02.2021 [cited 2021 Apr 13]. https://www.fhi.no/contentassets/71e97765e43c41ee8f059efbd4016ca8/2021.03.30_en-vaksinasjonskalender.pdf
- 10.Our World in Data. Case fatality rate of the ongoing COVID-19 pandemic [cited 2021 Apr 23]. https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&hideControls=true&Interval=Cumulative&Relative+to+Population=false&Align+outbreaks=true&country=ITA∼CHN∼KOR∼OWID_WRL∼ESP∼NOR∼SWE∼DNK&Metric=Case+fatality+rate
- 11.Li R, Metcalf CJE, Stenseth NC, Bjørnstad ON. A general model for the demographic signatures of the transition from pandemic emergence to endemicity. Sci Adv [in press] [DOI] [PMC free article] [PubMed]
- 12.Bjørnstad ON. Springer; New York: 2018. Epidemics: Models and Data using R. [Google Scholar]
- 13.Callow KA, Parry HF, Sergeant M, Tyrrell DA. The time course of the immune response to experimental coronavirus infection of man. Epidemiol Infect. 1990;105:435–446. doi: 10.1017/s0950268800048019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lavine JS, Bjornstad ON, Antia R. Immunological characteristics govern the transition of COVID-19 to Endemicity. Science. 2021;371:741–745. doi: 10.1126/science.abe6522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davies NG, Klepac P, Liu Y, Prem K, Jit M, Eggo RM. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26:1205–1211. doi: 10.1038/s41591-020-0962-9. [DOI] [PubMed] [Google Scholar]
- 16.Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henrik S, Joacim R, Tom B. Evaluating and optimizing COVID-19 vaccination policies: a case study of Sweden. 2021. https://doi.org/10.1101/2021.04.07.21255026
- 18.Pedersen OB, Nissen J, Dinh KM, Schwinn M, Kaspersen KA, Boldsen JK. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection fatality rate among elderly danes: A cross-sectional study on retired blood donors. Clin Infect Dis. 2020:ciaa1627. doi: 10.1093/cid/ciaa1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.