Abstract
Context
Weakness of the gluteus medius and gluteus maximus is associated with a variety of musculoskeletal disorders. However, activation of synergistic muscles that are not targeted should be considered when prescribing side-lying hip-abduction (SHA) exercises. Log-rolling positions may affect hip-abductor activity during SHA.
Objective
To determine the effects of log-rolling positions on gluteus medius, gluteus maximus, and tensor fasciae latae activity during SHA in participants with gluteus medius weakness.
Design
Controlled laboratory study.
Setting
University research laboratory.
Patients or Other Participants
Twenty-one participants with gluteus medius weakness.
Intervention(s)
Three types of SHA were performed: frontal-plane SHA in neutral position (SHA-neutral), frontal-plane SHA in anterior log-rolling position (SHA-anterior rolling), and frontal-plane SHA in posterior log-rolling position (SHA-posterior rolling).
Main Outcome Measure(s)
Surface electromyography was used to measure hip-abductor activity. One-way repeated-measures analysis of variance was calculated to assess the statistical significance of the muscle activity.
Results
The SHA-anterior rolling showed greater gluteus medius and gluteus maximus activation than the SHA-neutral (P = .003 and P < .001, respectively) and SHA-posterior rolling (P < .001 and P < .001, respectively). The SHA-neutral demonstrated greater gluteus medius and gluteus maximus activation than the SHA-posterior rolling (P < .001 and P = .001, respectively). The SHA-anterior rolling produced less tensor fasciae latae activation than the SHA-neutral (P < .001) and SHA-posterior rolling (P < .001). The SHA-neutral showed less tensor fasciae latae activation than the SHA-posterior rolling (P < .001).
Conclusions
The SHA-anterior rolling may be an effective exercise for increasing activation of the gluteus medius and gluteus maximus while decreasing activation of the tensor fasciae latae in participants with gluteus medius weakness.
Keywords: exercise, muscles, recovery of function, surface electromyography
Key Points
Weakness of the gluteus medius or gluteus maximus muscles is associated with a variety of musculoskeletal disorders.
Among exercises that increase gluteus medius or gluteus maximus activity, side-lying hip-abduction (SHA) exercises are frequently used in rehabilitation to improve neuromuscular control or strength.
Activation of synergistic muscles that are not targeted should be considered when prescribing SHA exercises.
The SHA in anterior log-rolling position produced more gluteus medius and gluteus maximus activation and less tensor fasciae latae activation in participants with gluteus medius weakness.
The gluteus medius and gluteus maximus muscles are crucial for performing functional activities such as walking and running.1,2 During gait, the gluteus medius, especially the posterior fibers, help stabilize the pelvis and control femoral adduction and internal rotation; the upper fibers of the gluteus maximus act as a hip external rotator and abductor.3–7 Weakness of these muscles has been associated with a variety of musculoskeletal disorders, including such gait disorders as Trendelenburg gait, greater trochanteric pain syndrome, patellofemoral pain syndrome, anterior cruciate ligament sprains, and chronic ankle instability.8–10
Previous researchers11–13 have examined the effectiveness of such exercises as the hip clam, single-limb squat, side bridge, and side-lying hip abduction (SHA) to increase gluteus medius or gluteus maximus activity. Among these exercises, SHA exercises are frequently used in rehabilitation to improve neuromuscular control or strength.14 However, activation of synergistic muscles that are not targeted should be considered when prescribing SHA exercises. The tensor fasciae latae is one such synergistic muscle.15 Pain in the lower back, hip, and knee may be associated with a dominant tensor fasciae latae that compensates for a weak gluteus medius.14 Patients with a degenerative hip joint condition also show atrophy of the gluteus medius and gluteus maximus relative to the tensor fasciae latae.16–18 In particular, hip flexion relative to the frontal plane can be caused by a dominant tensor fasciae latae during SHA.14
For this reason, earlier authors studied the effects of interventions for decreasing tensor fasciae latae activity during SHA. External hip rotation resulted in greater tensor fasciae latae activation than gluteus medius and gluteus maximus activation, whereas internal rotation resulted in less tensor fasciae latae activation than gluteus medius and gluteus maximus activation during SHA.15,19 Yet these SHA positions may not be prescribed to patients who have greater trochanteric pain syndrome or a limited range of hip rotation. Thus, it may be valuable to assess how SHA in various log-rolling positions affects the activity of the hip-abductor muscles rather than hip rotation during SHA in participants with gluteus medius weakness.
We aimed to determine the effects of log-rolling positions in the transverse plane (frontal-plane SHA in neutral position [SHA-neutral], frontal-plane SHA in anterior log-rolling position [SHA-anterior rolling], and frontal-plane SHA in posterior log-rolling position [SHA-posterior rolling]) on the gluteus medius, gluteus maximus, and tensor fasciae latae activity during SHA in participants with gluteus medius weakness. We hypothesized that the gluteus medius and gluteus maximus would show more activation during SHA-anterior rolling than during SHA-neutral or SHA-posterior rolling and that the tensor fasciae latae would show less activation during SHA-anterior rolling than during SHA-neutral or SHA-posterior rolling.
METHODS
Participants
The sample size was calculated using G Power Software (version 3.1; Heinrich-Heine-Universität). The required sample size of 6 participants was calculated from data obtained from a pilot study of 5 participants that measured the same variables in the same conditions to achieve a power of 0.80, effect size (ES) of 1.20 (calculated with partial η2 of 0.59 from the pilot study), and α level of .05. The current study consisted of 21 participants (Table 1). The inclusion criteria were as follows: gluteus medius weakness (grade 3 or lower as determined by manual muscle testing), no past or current lower extremity injury (eg, sprains or fractures), and the ability to maintain SHA for 5 seconds while in the log-rolling positions.14 The participants with bilateral gluteus medius weakness performed all exercises on their weaker leg, as our primary goal was to investigate the effects of these exercises on weak gluteus medius muscles. The weaker leg was defined as the leg with the lower strength measurement as determined using a handheld dynamometer (mobile MT-100, SAKAI Medical Co, Ltd). The exclusion criteria were past or present musculoskeletal, cardiopulmonary, or neurologic disease; inflammatory arthritis; back pain; or lower extremity dysfunction. In addition, patients with shortness of the iliotibial band as identified via the modified Ober test (positive if the test leg does not drop toward the table beyond 10°)20 were also excluded. Fatty tissue acts as a low-pass filter for electrical signals, so participants who were obese or overweight (body mass index >25, calculated as kg/m2) were excluded.21,22 The study protocol was approved by the Yonsei University Wonju Institutional Review Board (No. 1041849-201812-BM-125-02). Before the study, participants read and signed a written consent form.
Table 1.
Participant Characteristics (N = 21)
| Characteristic |
No. |
| Men/women | 13/8 |
| Mean ± SD |
|
| Age, y | 22.1 ± 1.9 |
| Height, m | 1.7 ± 0.1 |
| Mass, kg | 66.7 ± 12.2 |
| Body mass index, kg/m2 | 23.2 ± 3.0 |
Instrumentation
A Tele-Myo DTS EMG instrument with a wireless telemetry system (Noraxon, Inc) was used for data collection. The sampling rate was 1500 Hz. A digital band-pass filter, between 20 and 450 Hz, filtered the raw signals, and the root mean square values were calculated with a moving window of 50 milliseconds. We used MyoResearch Master (edition 1.06 XP; Noraxon, Inc) to analyze the electromyographic (EMG) data.
A MyoMotion (Noraxon, Inc) 3-dimensional (3D) motion-analysis system was used to calculate hip-abduction range of motion and pelvic rotation by log rolling and monitoring compensatory movement (hip flexion or extension in the sagittal plane, hip rotation in the transverse plane, pelvic tilt in the sagittal plane, and pelvic obliquity in the frontal plane) during SHA exercise. A small inertial measurement unit sensor placed on a body segment tracked the 3D angular orientation. Two inertial measurement unit sensors were attached to the pelvis (between the posterior-superior iliac spines) and the anterior region of the thigh. The sampling frequency was 200 Hz, and MyoResearch 3 software was used to analyze the 3D motion data.
Procedures
Before the experiment, participants warmed up by jogging for 5 minutes at submaximal speed to reduce discomfort or pain while performing the exercises.23 They were then familiarized with the exercises until they demonstrated an ability to precisely perform them.
Each SHA condition was conducted 3 times at a comfortable speed, with a 3-minute rest between exercises.24 To avoid the influence of fatigue and effects of learning, the sequence of exercises was randomized with random numbers generated in Excel (Microsoft Corp). The EMG data were collected for 5 seconds during the isometric phase, which represents an operational measure of the force output, and were calculated from the average of the middle 3 seconds of each exercise to reduce any starting or ending effects on the skin-electrode connecting element.25–28 The mean values were used for statistical analysis.28
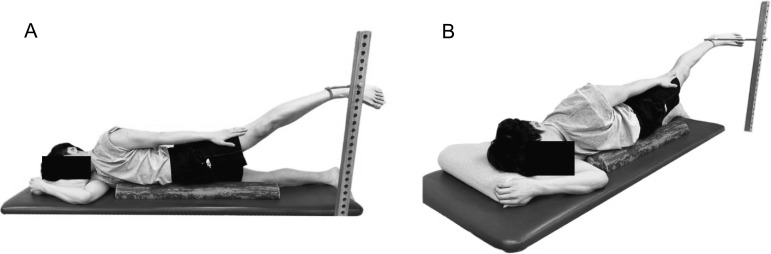
Frontal-Plane SHA-Neutral
The participants were positioned on their side on a mat with the upper trunk and pelvis aligned in a straight line. The bottom leg was in full extension. A wooden target bar was placed at 50% of the frontal hip-abduction's maximal range of motion, accommodating each person's range of motion. Thus, the participant abducted the test leg to 50% of the maximal range of motion with knee extension until the lateral aspect of the distal tibia (above the lateral malleolus) touched the target bar. He or she maintained the position for 5 seconds and then slowly returned to the starting position. The MyoMotion 3D motion-analysis system monitored the compensatory movement (Figure 1A and B). If the trunk, pelvis, or hip joint lost its neutral position during SHA-neutral, the data were discarded.
Figure 1.
Frontal hip-abduction exercise in neutral position while side lying. A, Frontal view. B, Oblique view.
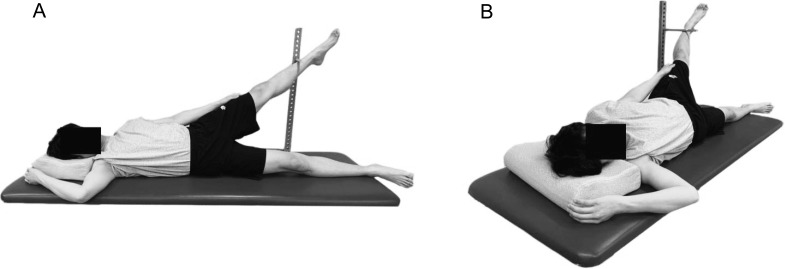
Frontal-Plane SHA-Anterior Rolling
The SHA-anterior rolling was performed in the same way as SHA-neutral except for anterior log rolling. The participants were positioned on their side on a mat with the upper trunk and pelvis aligned in a straight line and the bottom leg fully extended. Then, the individual reclined on a half-foam roller by rolling the body anteriorly until the pelvis was rotated 45° in the transverse plane (Figure 2A and B). If the trunk, pelvis, or hip joint lost its neutral alignment in the reclined position during the front SHA-anterior rolling, the data were discarded.
Figure 2.
Frontal hip-abduction exercise in anterior-rolling position while side lying. A, Frontal view. B, Oblique view.
Frontal-Plane SHA-Posterior Rolling
The SHA-posterior rolling was performed in the same way as SHA-neutral, except for posterior log rolling. The participants were positioned on their side on a mat, with the upper trunk and pelvis aligned in a straight line and the bottom leg fully extended. Then, the participant reclined on a half-foam roller by rolling the body posteriorly until the pelvis was rotated 45° in the transverse plane (Figure 3A and B). If the trunk, pelvis, or hip joint lost its neutral alignment in the reclined position during front SHA-posterior rolling, the data were discarded.
Figure 3.
Frontal hip-abduction exercise in posterior-rolling position while side lying. A, Frontal view. B, Oblique view.
Electromyographic Data Collection
We prepared the electrode sites by shaving any hair from the immediate vicinity of the muscle belly and cleaning the skin with isopropyl alcohol, applied with a sterile gauze pad to reduce EMG signal impedance and allow proper electrode fixation.29 For the hip-abductor muscles, electrodes were placed over the midsection of the muscle bellies25,30 as described by Criswell.31 For the gluteus medius, electrodes were placed proximally at one-third of the distance between the iliac crest and greater trochanter. For the gluteus maximus, electrodes were placed at half the distance between the second sacral spinous process and the greater trochanter. For the tensor fasciae latae, electrodes were placed approximately 2 cm below the anterior-superior iliac spine. Proper placement of the electrodes was confirmed by observing the participants as they completed 5 SHA repetitions.31 The electrode contacts were checked before all contractions.
The maximal voluntary isometric contraction (MVIC) in the standard manual muscle test position was used to normalize the gluteus medius, gluteus maximus, and tensor fasciae latae.20 The MVIC was performed for 5 seconds, with a 10-second rest between contractions and a 3-minute rest between muscles.14 To obtain the MVIC for the gluteus medius, we positioned the participants on their side with the test leg up and the bottom hip and knee flexed for stabilization. The individual then abducted the test leg to approximately 50% of hip abduction with slight extension and external rotation of the hip joint. An examiner applied a downward force at the ankle with 1 hand while stabilizing the hip with the other hand. For the gluteus maximus MVIC, the participants were positioned prone with the test leg flexed at 90° at the knee joint. The examiner applied a downward force at the posterior thigh while the participant extended the hip under resistance. To obtain the tensor fasciae latae MVIC, the participants were positioned in the supine position with the test leg flexed and maximal internal rotation of the hip joint with the knee extended. The examiner applied force at the ankle in the direction of hip extension. The examiner measured the MVIC for the gluteus medius, gluteus maximus, and tensor fasciae latae twice; the mean value from the 2 trials was used for data analysis. The collected EMG amplitudes for the gluteus medius, gluteus maximus, and tensor fasciae latae during each exercise were expressed as a percentage of the mean MVIC (% MVIC).
Statistical Analysis
To perform all statistical analyses, we used SPSS Statistics for Windows (version 24.0; IBM Corp). Kolmogorov-Smirnov Z tests were conducted to assess the normality of the distribution. A 1-way repeated-measures analysis of variance was calculated to assess the statistical significance of the gluteus medius, gluteus maximus, and tensor fasciae latae muscle activity during the SHA exercises with various log-rolling conditions (SHA-neutral, SHA-anterior rolling, and SHA-posterior rolling). Statistical significance was set at .05. If a difference was found, we performed a Bonferroni adjustment (α = 0.05/3 = 0.017). The ES was calculated to identify meaningful changes between interventions.32
RESULTS
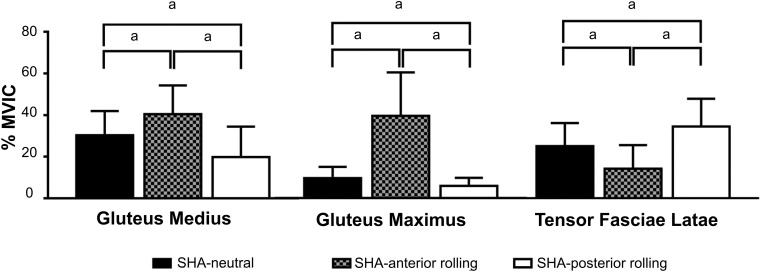
Differences were observed among the 3 log-rolling conditions during SHA for gluteus medius activity (F = 15.005, P < .001), gluteus maximus activity (F = 31.592, P < .001), and tensor fasciae latae activity (F = 33.196, P < .001). The SHA-anterior rolling showed greater gluteus medius and gluteus maximus activation than the SHA-neutral (P = .003, ES = 0.750; P < .001, ES = 1.400, respectively) and SHA-posterior rolling (P < .001, ES = 1.180; P < .001, ES = 1.489, respectively). The SHA-neutral displayed greater gluteus medius and gluteus maximus activation than the SHA-posterior rolling (P < .001, ES = 0.738; P = .001, ES = .738, respectively). The SHA-anterior rolling demonstrated less tensor fasciae latae activation than the SHA-neutral (P < .001, ES = 0.878) and SHA-posterior rolling (P < .001, ES = 1.267). The SHA-neutral produced less tensor fasciae latae activation than the SHA-posterior rolling (P < .001, ES = 0.723; Table 2, Figure 4).
Table 2.
Gluteus Medius, Gluteus Maximus, and Tensor Fasciae Latae Muscle Activity in Various Log-Rolling Positions During Side-Lying Hip Abduction
| Muscle |
Side-Lying Hip-Abduction Condition |
% Maximal Voluntary Isometric Contraction, Mean ± SD (95% CI) |
| Gluteus medius | Neutral | 30.2 ± 11.7 (24.9, 35.6) |
| Anterior rolling | 40.5 ± 13.8 (34.2, 46.8) | |
| Posterior rolling | 19.8 ± 14.6 (13.2, 26.5) | |
| Gluteus maximus | Neutral | 9.6 ± 5.4 (7.2, 12.1) |
| Anterior rolling | 39.6 ± 21.0 (30.1, 49.1) | |
| Posterior rolling | 5.9 ± 3.9 (4.1, 7.7) | |
| Tensor fasciae latae | Neutral | 25.0 ± 11.1 (20.0, 30.1) |
| Anterior rolling | 14.1 ± 11.4 (9.0, 19.3) | |
| Posterior rolling | 34.5 ± 13.3 (28.3, 40.6) |
Figure 4.
Comparison of muscle activity in the gluteus medius, the gluteus maximus and the tensor fasciae latae among different log-rolling conditions during side-lying hip-abduction (SHA) exercises. Abbreviations: SHA-anterior rolling, frontal-plane SHA in anterior-rolling position; SHA-neutral, frontal-plane SHA in neutral position; SHA-posterior rolling, frontal-plane SHA in posterior-rolling position. a Indicates difference using Bonferroni adjustment (P < .017).
DISCUSSION
We aimed to compare gluteus medius, gluteus maximus, and tensor fasciae latae activation during 3 SHA exercises (SHA-neutral, SHA-anterior rolling, and SHA-posterior rolling) in participants with gluteus medius weakness. Activation of the gluteus medius and gluteus maximus was higher during SHA-anterior rolling than during SHA-neutral or SHA-posterior rolling, and activation of the tensor fasciae latae was lower during SHA-posterior rolling than during SHA-neutral or SHA-anterior rolling.
Gluteus medius activity was greater during SHA-anterior rolling than during SHA-neutral (by 10.3%) and SHA-posterior rolling (by 20.7%). This finding was consistent with that reported in previous studies. Earl33 described greater gluteus medius activity in hip abduction with internal rotation than in hip abduction with external rotation during single-legged stance. Further, Lee et al14 observed greater gluteus medius activity during SHA with internal hip rotation than during SHA with neutral and external hip rotation. Our results may be explained by the gluteus medius being at the highest location in the transverse plane of the upper thigh when the participants were in the anterior log-rolling position because the gluteus medius attaches to the external ilium and the greater trochanter. Thus, the gluteus medius was activated to sustain the isometric hip-abduction position and counter gravity.14
Gluteus maximus activity was greater during SHA-anterior rolling than during SHA-neutral (by 30.0%) and SHA-posterior rolling (by 33.7%). This outcome was consistent with that of Willcox and Burden,34 who reported that activation of the gluteus maximus during the clam exercise was greater with a neutral pelvis than with a posteriorly reclined pelvis.34 This finding may be explained by the antigravity mechanism. During SHA-anterior rolling, as participants sustained the frontal hip-abduction position without hip flexion or extension, the gluteus maximus was activated to counteract gravity pulling the leg downward. Thus, SHA-anterior rolling was effective in increasing activation of the gluteus medius and gluteus maximus.
Tensor fasciae latae activity was lower during SHA-anterior rolling than during SHA-neutral (by 10.9%) and SHA-posterior rolling (by 20.3%). This finding was consistent with that reported in previous studies. McBeth et al15 described greater tensor fasciae latae activity than gluteus maximus activity during hip abduction with external rotation. Lee et al14 observed less tensor fasciae latae activity during SHA with a neutral hip than with hip external rotation. When participants rolled the body posteriorly, the tensor fasciae latae was in a favorable position to contract because it was at the highest position in the transverse plane and was activated to counteract gravity, pulling the leg downward. However, when participants rolled anteriorly, the gluteus maximus was in a favorable position to contract. Therefore, the tensor fasciae latae might not have been activated because it was not shortening against gravity.
To the best of our knowledge, we are the first to investigate the effects of log rolling on gluteus medius, gluteus maximus, and tensor fasciae latae activity during SHA in participants with gluteus medius weakness. The gluteus medius and gluteus maximus activity during SHA-anterior rolling was 40.5% and 39.6% MVIC, respectively. Previous authors25,35 have suggested that 40% to 60% of MVIC is the neuromuscular activation threshold that can effectively stimulate muscle strength gains. Our results indicate that gluteus medius and gluteus maximus activation during SHA-anterior rolling nearly reached this threshold. Therefore, SHA-anterior rolling, rather than traditional SHA-neutral or SHA-posterior rolling, may be recommended as an early, low-level exercise for strengthening the gluteus medius and gluteus maximus to prevent musculoskeletal conditions such as gait disorders, patellofemoral pain syndrome, anterior cruciate ligament sprains, and chronic ankle instability in participants with gluteus medius weakness.
This study had several limitations. First, the cross-sectional design prevented assessment of the long-term effects. Second, all participants were 18 to 30 years old. Thus, these results should not be generalized. Third, although all safety measures were taken, cross-talk between the gluteus medius and tensor fasciae latae was possible. Further work is required to determine the long-term effects of SHA-anterior rolling on the gluteus medius, gluteus maximus, and tensor fasciae latae in participants of all ages with gluteus medius weakness.
CONCLUSIONS
We examined the effects of various log-rolling exercises on gluteus medius, gluteus maximus, and tensor fasciae latae activity during SHA exercises in participants with gluteus medius weakness. In the SHA-anterior rolling condition, activity of the gluteus medius and gluteus maximus was greatest, whereas that of the tensor fasciae latae was the lowest. Thus, SHA-anterior rolling could be an effective exercise for increasing gluteus medius and gluteus maximus activation while decreasing tensor fasciae latae activation in participants with gluteus medius weakness.
REFERENCES
- 1.Hamstra-Wright KL, Huxel Bliven K. Effective exercises for targeting the gluteus medius. J Sport Rehabil. 2012;21(3):296–300. doi: 10.1123/jsr.21.3.296. [DOI] [PubMed] [Google Scholar]
- 2.Lieberman DE, Raichlen DA, Pontzer H, Bramble DM, Cutright-Smith E. The human gluteus maximus and its role in running. J Exp Biol. 2006;209(pt 11):2143–2155. doi: 10.1242/jeb.02255. [DOI] [PubMed] [Google Scholar]
- 3.Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39(8):1227–1232. doi: 10.1249/mss.0b013e3180601109. [DOI] [PubMed] [Google Scholar]
- 4.Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10(3):169–175. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Calais-Germain B, Anderson S. Anatomy of Movement. Eastland Press; 1993. [Google Scholar]
- 6.Lyons K, Perry J, Gronley JK, Barnes L, Antonelli D. Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. An EMG study. Phys Ther. 1983;63(10):1597–1605. doi: 10.1093/ptj/63.10.1597. [DOI] [PubMed] [Google Scholar]
- 7.Neumann DA. Kinesiology of the Musculoskeletal System Foundations for Rehabilitation 3rd ed. St Louis, MO: Elsevier;; 2017. [Google Scholar]
- 8.Youdas JW, Adams KE, Bertucci JE, Brooks KJ, Nelson MM, Hollman JH. Muscle activation levels of the gluteus maximus and medius during standing hip-joint strengthening exercises using elastic-tubing resistance. J Sport Rehabil. 2014;23(1):1–11. doi: 10.1123/jsr.2012-0082. [DOI] [PubMed] [Google Scholar]
- 9.Monteiro RL, Facchini JH, de Freitas DG, Callegari B, Joao SM. Hip rotations' influence of electromyographic activity of gluteus medius muscle during pelvic-drop exercise. J Sport Rehabil. 2017;27(1):65–71. doi: 10.1123/jsr.2015-0097. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 11.Distefano LJ, Blackburn JT, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39(7):532–540. doi: 10.2519/jospt.2009.2796. [DOI] [PubMed] [Google Scholar]
- 12.Ekstrom RA, Donatelli RA, Carp KC. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007;37(12):754–762. doi: 10.2519/jospt.2007.2471. [DOI] [PubMed] [Google Scholar]
- 13.Reiman MP, Bolgla LA, Loudon JK. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiother Theory Pract. 2012;28(4):257–268. doi: 10.3109/09593985.2011.604981. [DOI] [PubMed] [Google Scholar]
- 14.Lee JH, Cynn HS, Choi SA, Yoon TL, Jeong HJ. Effects of different hip rotations on gluteus medius and tensor fasciae latae muscle activity during isometric side-lying hip abduction. J Sport Rehabil. 2013;22(4):301–307. doi: 10.1123/jsr.22.4.301. [DOI] [PubMed] [Google Scholar]
- 15.McBeth JM, Earl-Boehm JE, Cobb SC, Huddleston WE. Hip muscle activity during 3 side-lying hip-strengthening exercises in distance runners. J Athl Train. 2012;47(1):15–23. doi: 10.4085/1062-6050-47.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grimaldi A, Richardson C, Stanton W, Durbridge G, Donnelly W, Hides J. The association between degenerative hip joint pathology and size of the gluteus medius, gluteus minimus and piriformis muscles. Man Ther. 2009;14(6):605–610. doi: 10.1016/j.math.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Grimaldi A, Richardson C, Durbridge G, Donnelly W, Darnell R, Hides J. The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia lata muscles. Man Ther. 2019;14(6):611–617. doi: 10.1016/j.math.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Marshall AR, Noronha MD, Zacharias A, Kapakoulakis T, Green R. Structure and function of the abductors in patients with hip osteoarthritis: systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2016;29(2):191–204. doi: 10.3233/BMR-150614. [DOI] [PubMed] [Google Scholar]
- 19.Lee JH, Cynn HS, Kwon OY, et al. Different hip rotations influence hip abductor muscles activity during isometric side-lying hip abduction in subjects with gluteus medius weakness. J Electromyogr Kinesiol. 2014;24(2):318–324. doi: 10.1016/j.jelekin.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Kendall FP, McCreary EP, Provance PG, Rodgers MM, Romani WA. Muscles Testing and Function With Posture and Pain. Lippincott Williams & Wilkins; 2005. 5th ed. [Google Scholar]
- 21.Wong YM. Skin thickness and VMO:VL ratio. J Orthop Sports Phys Ther. 1999;29(11):686. doi: 10.2519/jospt.1999.29.11.686. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 23.Hunter AM, St Clair Gibson A, Lambert MI, Nobbs L, Noakes TD. Effects of supramaximal exercise on the electromyographic signal. Br J Sports Med. 2003;37(4):296–299. doi: 10.1136/bjsm.37.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sykes K, Wong YM. Electrical activity of vastus medialis oblique muscle in straight leg raise exercise with different angles of hip rotation. Physiotherapy. 2003;89(7):423–430. doi: 10.1016/S0031-9406(05)60076-4. [DOI] [Google Scholar]
- 25.Ayotte NW, Stetts DM, Keenan G, Greenway EH. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther. 2007;37(2):48–55. doi: 10.2519/jospt.2007.2354. [DOI] [PubMed] [Google Scholar]
- 26.Soderberg GL, Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther. 2000;80(5):485–498. [PubMed] [Google Scholar]
- 27.Disselhorst-Klug C, Schmitz-Rode T, Rau G. Surface electromyography and muscle force: limits in sEMG-force relationship and new approaches for applications. Clin Biomech (Bristol Avon) 2009;24(3):225–235. doi: 10.1016/j.clinbiomech.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 28.De Luca CJ. The use of surface electromyography in biomechanics. J Appl Biomech. 1997;13(2):135–163. doi: 10.1123/jab.13.2.135. [DOI] [Google Scholar]
- 29.Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361–374. doi: 10.1016/s1050-6411(00)00027-4. [DOI] [PubMed] [Google Scholar]
- 30.Bolgla LA, Uhl TL. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. J Orthop Sports Phys Ther. 2005;35(8):487–494. doi: 10.2519/jospt.2005.35.8.487. [DOI] [PubMed] [Google Scholar]
- 31.Criswell E. Cram's Introduction to Surface Electromyography. Jones and Bartlett; 2011. 2nd ed. [Google Scholar]
- 32.Portney LG, Watkins MP. Foundations of Clinical Research Applications to Practice. Pearson/Prentice Hall; 2015. 3rd rev ed. [Google Scholar]
- 33.Earl JE. Gluteus medius activity during 3 variations of isometric single-leg stance. J Sport Rehabil. 2005;14(1):1–11. doi: 10.1123/jsr.14.1.1. [DOI] [Google Scholar]
- 34.Willcox EL, Burden AM. The influence of varying hip angle and pelvis position on muscle recruitment patterns of the hip abductor muscles during the clam exercise. J Orthop Sports Phys Ther. 2013;43(5):325–331. doi: 10.2519/jospt.2013.4004. [DOI] [PubMed] [Google Scholar]
- 35.Andersen LL, Magnusson SP, Nielsen M, Haleem J, Poulsen K, Aagaard P. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther. 2006;86(5):683–697. [PubMed] [Google Scholar]