The origin of SARS-CoV-2 has received intensive global attention since its spread was first reported to the international community in early January, 2020. Multiple studies1, 2, 3, 4, 5, 6, 7, 8, 9 conducted collaboratively by scientists around the world have found that animal-to-human cross-species spillover is the most likely source of SARS-CoV-2, whereas laboratory leakage is extremely unlikely. However, the research and global health communities have yet to reach a clear conclusion as to the specific time, place, and cross-species transmission route through which SARS-CoV-2 entered the human population.1, 2, 3, 4, 5, 6, 7, 8, 9
Viruses could be made in a laboratory; however, there is no scientific evidence to support the idea that SARS-CoV-2 is artificial, and there are also no data to support the notion that any laboratory had handled SARS-CoV-2 or its proximal ancestor before the COVID-19 pandemic.7, 10, 11 Although the bat coronavirus RaTG13, first reported by Wuhan Institute of Virology (WIV), Chinese Academy of Sciences, shares the highest genome-wide sequence identity (96·2%) with SARS-CoV-2 of all known coronaviruses, it still has more than 1000 nucleotide differences, spread evenly across the genome.2 Wide consensus has been reached by the scientific community11 that such a virus cannot be the direct source of SARS-CoV-2, or even a template for synthesising SARS-CoV-2. The bat coronaviruses isolated or experimented with by WIV scientists, such as strains WIV1 and WIV16, are SARS-like coronaviruses or alpha coronaviruses. Their sequences differ even further from SARS-CoV-2 than RaTG13, and there is no evidence that they could evolve to SARS-CoV-2.12, 13, 14, 15, 16, 17 Furthermore, no one presented with respiratory illness similar to COVID-19 in WIV prior to December, 2019, which was corroborated by institution-wide SARS-CoV-2-specific serological testing.6 These findings suggest that the outbreak did not start from a laboratory incident at WIV.
Since the SARS outbreak in 2003, China has developed rigorous administration and supervision systems to regulate activities in high-level biosafety laboratories, and enacted a series of laws and decrees in this regard.18, 19 These laws, decrees, and regulations have built a strict and complete whole-chain administration, covering aspects including laboratory admission, personnel access, research programme review, experimental operation supervision, facilities and equipment operation, handling of disposals, and health surveillance of laboratory personnel. Each laboratory will be subjected to strict internal audit and unannounced inspections by multiple government authorities every year, making artificial manufacture of a human-made virus or laboratory leakage extremely unlikely. After inspection of the WIV biosafety laboratory, the WHO–China joint expert group also concluded that the introduction of SARS-CoV-2 through a laboratory incident was “extremely unlikely”.6 Therefore, without evidence, a laboratory origin should not be a priority at present for investigating the origin of SARS-CoV-2. Instead, as mentioned in the phase 1 joint report6 of the WHO-convened global study of origins of SARS-CoV-2, internal audit is a better alternative for all high-level biosafety laboratories worldwide to further exclude the “laboratory incident” hypothesis.
Historically, the emergence of infectious diseases in humans has most often been caused by interspecies barrier breakthrough of animal-origin pathogens.20, 21, 22, 23 A natural origin of SARS-CoV-2 is by far the most likely scenario. Pinpointing the precise natural origin of the virus would also help to reject alternative hypotheses. Characterisation of the codon preferences of SARS-CoV-2 and its genome's structure indicate that the circulating virus is highly similar to strains carried by wild animals.24, 25 The virus's evolutionary history in animals and its fast adaptive mutation within the infected human population also suggest that SARS-CoV-2 is more likely to have come from nature than other potential sources.26, 27, 28 A variety of evidence indicates that horseshoe bat species found in Cambodia, Thailand, Japan, and the southwest border areas of China, as well as Malayan pangolins captured in anti-smuggling actions, carry coronaviruses similar to SARS-CoV-2.5, 29, 30, 31, 32, 33 Although the animal viruses that have been identified are not immediate precursors of SARS-CoV-2, their existence suggests that global investigations into the evolutionary characteristics of the animal origin for SARS-CoV-2 are warranted. Such investigations would include testing wild animal hosts of coronaviruses at the nucleic acid and serum levels to positively identify the natural origin of the cross-species spillover. Various studies34, 35, 36, 37, 38, 39, 40, 41 have already reported that several species of mammals (including mink, civets, cats, pangolins, rabbits, ferrets, foxes, deer, etc) are capable of being infected by SARS-CoV-2. It is entirely possible that SARS-CoV-2-related viruses could cross the species barrier between humans and animals repeatedly in many parts of the world. In fact, it is almost certain that such animal-to-human transmissions are happening repeatedly. There are many unsuccessful jumps before a virus takes to humans. Therefore, tracing such sporadic zoonoses and the virus's potential intermediate hosts among an even greater range of animal species in the real world is also of great importance.
Based on research findings to date, SARS-CoV-2 could have a complex origin, making investigation of its origins a hard task. Several studies from multiple countries have found that the virus might have been present in humans before the end of December, 2019, when the first outbreak was detected in Wuhan. For example, an evolutionary dynamics analysis indicated that the virus may have been spreading before the end of December.6, 42 In addition, a number of reports from many parts of the world have revealed the possible existence of COVID-19 cases and environmental positive samples prior to the end of December, 2019. Population-based nucleic acid and serology tests, as well as sewage tests, provide evidence of SARS-CoV-2's presence in Italy during September to December, 2019.43, 44, 45, 46 Similarly, nucleic acid and serology tests provide evidence of the virus's presence in France during December, 2019,47, 48 and nucleic acid tests of sewage provide evidence of its presence in Brazil in November, 2019.49 Furthermore, recent serology test results indicate the possible existence of SARS-CoV-2 infection in a number of states across the USA in December, 2019, much earlier than the first case confirmed in the USA through nucleic acid testing.50, 51 Although some findings have yet to be confirmed by nucleic acid sequencing, some methods used are not standardised, and serological tests might be affected by cross-reactivity of antibodies, this evidence deserves further investigation before it can be formally ruled out.
Additional research has suggested that SARS-CoV-2 may be transmitted via cold chains. Viral nucleic acids were detected and live virus was isolated from frozen foods and their outer packaging in several regions of China, including Beijing and Qingdao, that had COVID-19 outbreaks in 2020. These findings suggest that cold chains may have played an important role in the spread of the virus.52, 53, 54, 55, 56, 57 Studies on the viability and infectivity of the virus at different temperatures on different objects indicate that the virus can remain infectious on foods and other surfaces for a long time at low temperature, and cold-chain workers could become infected by contacting contaminated products, sparking new chains of transmission.58, 59 These results suggest that SARS-CoV-2 could plausibly spread across regions through cold-chain transmission and raise questions as to whether the location in which the virus was first reported was necessarily the site of its origin.
In light of the complexity and unresolved questions surrounding SARS-CoV-2's origin revealed by the WHO-China joint report that focused on Wuhan and China, there is a pressing need for extensive international cooperation in integrating multiple testing techniques to examine early cases and potential positive samples that pre-date the first known outbreak. In addition to combining genome sequencing, data from clinical and epidemiological studies, and results from environmental testing, we recommend that the next phase of investigation into the virus's origin should be carried out synchronously in multiple locations, not just in China. It should include: (1) collection of samples from wild animals, testing and analyses on sarbecoviruses and related serum antibodies, and targeted searching for viruses that have the same origin as SARS-CoV-2 in areas with insufficient samples or that have never been sampled, especially areas with specific species known to carry SARS-CoV-2-related viruses; (2) based on China's experience in investigating upstream and downstream supply chains of wildlife markets, a global retrospective survey of cross-region wildlife markets and upstream and downstream supply chains should be conducted to collect samples, as well as possible preserved early animal and environmental samples, to detect viruses or related serum antibodies; (3) based on the aforementioned possible early case clues, retrospective studies should be carried out worldwide, including the search and re-identification of suspicious cases and deaths, and laboratory re-testing of early patient swabs, tissues, and blood bank samples that may have been retained; (4) through integration of global molecular epidemiological data of high quality viral genome information, phylogenetic analysis and ancestral time analysis should be conducted to construct the evolutionary history of viral lineages, and estimate initial virus quantity and dynamic propagation speed, based on combined epidemiological and geographical information; and (5) to further evaluate the potential role of cold chains in the introduction and transmission of SARS-CoV-2, retrospective sampling and testing should be performed to trace the origin of cold-chain imports, and the viability and infectivity of SARS-CoV-2 at different temperatures should be further analysed.
SARS-CoV-2 is a common enemy of humankind. Like other infectious diseases, it respects no national boundaries. In the face of a pandemic without modern precedent, humankind must work together. This is a humanitarian issue, the gravity and sanctity of which has been respected even during wartime. To cope with the challenge, Chinese scientists and medical workers have always kept an open and cooperative attitude, working vigorously with the international scientific community in all aspects and offering unreserved accurate data even during China's toughest period of fighting against the virus.
Notably, after the initial outbreak of COVID-19, Chinese research institutions, including the Chinese Center for Disease Control and Prevention, Chinese Academy of Medical Sciences, and Chinese Academy of Sciences, conducted parallel detection of case samples, identified SARS-CoV-2 as the causative agent of the pandemic together, and immediately shared the whole genome sequence of the virus with the rest of the world; through these efforts, Chinese researchers contributed critical references for the development of diagnostic reagents, vaccines, and drugs.2, 8, 60, 61, 62, 63 Chinese scientists, along with fellow researchers from other countries, also issued an early warning of a potential pandemic to the international community.64, 65, 66, 67 Moreover, Chinese scientists have conducted a series of research projects to investigate the origin of SARS-CoV-2 since the COVID-19 outbreak, and have made much progress in understanding epidemiology, infection mechanisms, and animal host searching.30, 34, 35, 68, 69
There is yet insufficient evidence to determine whether the natural origin of SARS-CoV-2 was in China or elsewhere. Because Wuhan was the first place where the outbreak of COVID-19 was identified, a WHO-convened study group, together with Chinese experts, has conducted an extensive investigation in Wuhan in the past year; however, no creditable evidence has been found so far to support the idea that initial animal-to-human adaptation occurred in Wuhan. Since whether animal-to-human adaptation took place in or outside Wuhan remains unclear, it is reasonable to propose that the next phase of investigation of SARS-CoV-2's origin should not entirely focus on China; instead a worldwide search at different geographical locations should be carried out to identify where and when the first animal-to-human transmission occurred.
The concept of international health, which focuses on issues outside of one's own country, has evolved into that of global health, which tackles health issues that transcend national boundaries.70 We should view the search for SARS-CoV-2's origin as a collective attempt to better prevent and cope with future potential pandemics. Finding evidence of SARS-CoV-2's origins through scientific inquiry is essential to such efforts. Prior experience with tracing the origin of emerging viruses—eg, HIV—indicates that the task may be very difficult and time consuming, and the location where an epidemic is first reported is not necessarily the place where it originated.71, 72 Moreover, investigations into the origins of SARS-CoV-2 should be carried out by scientists on the basis of science alone, without interference or coercion from political forces. The strongest weapons we can wield to prevent and control future pandemics are unity and cooperation, which not only conform to the common interests of humankind but also serve as the foundation for the community of human health. Chinese scientists are willing, as always, to work with scientists of the world to explore the scientific complexities of the virus's origin objectively in the principles of openness and cooperation. Any hypothesis that lacks scientific evidence may lead to separation within the scientific community and among different population groups. Such speculation is not conducive to the unity and cooperation needed in the global fight against COVID-19 and other pathogens and is contrary to the spirit of science and humanitarianism.
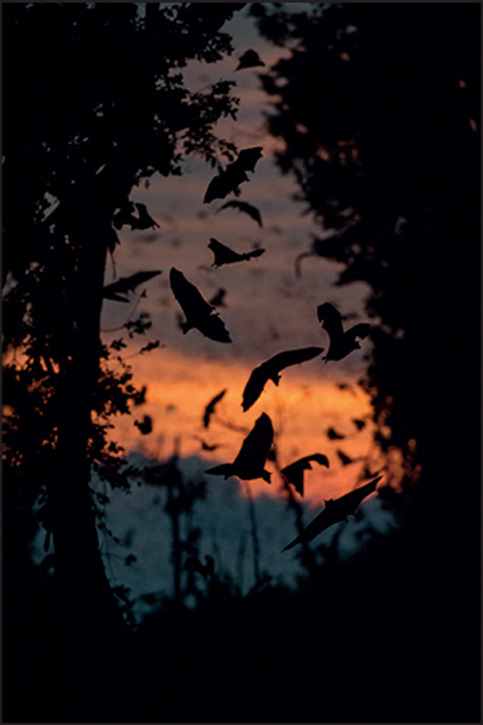
© 2021 Nick Garbutt/Barcroft Media/Getty Images
QJ served as a member of the academic committee of the State Key Laboratory of Virology (SKLV) between 2005 and 2016. SKLV is co-sponsored by Wuhan University and Wuhan Institute of Virology (WIV), Chinese Academy of Sciences (CAS). He now has no connection with SKLV. GW, WT, and WX are part-time researchers of Center for Biosafety Mega-Science, CAS. DG has given several public lectures or talks at WIV, and has published three joint papers with the scientists of WIV. He is a member of the editorial board of the academic journal Virologica Sinica sponsored by WIV, Chinese Society of Microbiology, and Springer. KL is the director of SKLV. He is also an associate editor of Virologica Sinica. He is an employee of Wuhan University and paid solely by Wuhan University. JW was an associate editor of Virologica Sinica between 2017–2019. He is a member of the editorial board of this journal now. ZW, JL, ML, LF, ZQ, LR, WY, and CW declare no competing interests.
References
- 1.Leitner T, Kumar S. Where did SARS-CoV-2 come from? Mol Biol Evol. 2020;37:2463–2464. doi: 10.1093/molbev/msaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beyer RM, Manica A, Mora C. Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS-CoV-1 and SARS-CoV-2. Sci Total Environ. 2021;767 doi: 10.1016/j.scitotenv.2021.145413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Latinne A, Hu B, Olival KJ, et al. Origin and cross-species transmission of bat coronaviruses in China. Nat Commun. 2020;11 doi: 10.1038/s41467-020-17687-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Wacharapluesadee S, Tan CW, Maneeorn P, et al. Evidence for SARS-CoV-2 related coronaviruses circulating in bats and pangolins in southeast Asia. Nat Commun. 2021;12:972. doi: 10.1038/s41467-021-21240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization; Geneva, Switzerland: 2021. WHO-convened global study of origins of SARS-CoV-2: China part; p. 120. [Google Scholar]
- 7.Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ren LL, Wang YM, Wu ZQ, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl) 2020;133:1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calisher CH, Carroll D, Colwell R, et al. Science, not speculation, is essential to determine how SARS-CoV-2 reached humans. Lancet. 2021;398:209–211. doi: 10.1016/S0140-6736(21)01419-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tyshkovskiy A, Panchin AY. There is no evidence of SARS-CoV-2 laboratory origin: Response to Segreto and Deigin (DOI: 10.1002/bies.202000240) Bioessays. 2021;43 doi: 10.1002/bies.202100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holmes EC, Goldstein SA, Rasmussen AL, et al. The origins of SARS-CoV-2: a critical review. Cell. 2021 doi: 10.1016/j.cell.2021.08.017. published online Aug 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ge XY, Li JL, Yang XL, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 2013;503:535–538. doi: 10.1038/nature12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang XL, Hu B, Wang B, et al. Isolation and characterization of a novel bat coronavirus closely related to the direct progenitor of severe acute respiratory syndrome coronavirus. J Virol. 2015;90:3253–3256. doi: 10.1128/JVI.02582-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeng LP, Gao YT, Ge XY, et al. Bat severe acute respiratory syndrome-like coronavirus WIV1 encodes an extra accessory protein, ORFX, involved in modulation of the host immune response. J Virol. 2016;90:6573–6582. doi: 10.1128/JVI.03079-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu B, Zeng LP, Yang XL, et al. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog. 2017;13 doi: 10.1371/journal.ppat.1006698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou P, Fan H, Lan T, et al. Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin. Nature. 2018;556:255–258. doi: 10.1038/s41586-018-0010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo H, Hu B, Si H-R, et al. Identification of a novel lineage bat SARS-related coronaviruses that use bat ACE2 receptor. bioRxiv. 2021 doi: 10.1101/2021.05.21.445091. published online May 21. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.State Council Gazette of the People's Republic of China Regulations on biosafety management of pathogenic microorganism laboratory. 2004. http://www.gov.cn/gongbao/content/2005/content_63265.htm
- 19.Standing Committee of the National People's Congress of the People's Republic of China Biosafety law of the People's Republic of China. 2021. http://www.gov.cn/xinwen/2020-10/18/content_5552108.htm
- 20.Cunningham AA, Daszak P, Wood JLN. One Health, emerging infectious diseases and wildlife: two decades of progress? Philos Trans R Soc Lond B Biol Sci. 2017;372 doi: 10.1098/rstb.2016.0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daszak P, Cunningham AA, Hyatt AD. Emerging infectious diseases of wildlife—threats to biodiversity and human health. Sci. 2000;287:443–449. doi: 10.1126/science.287.5452.443. [DOI] [PubMed] [Google Scholar]
- 22.Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor LH, Latham SM, Woolhouse ME. Risk factors for human disease emergence. Philos Trans R Soc Lond B Biol Sci. 2001;356:983–989. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik YS, Ansari MI, Kattoor JJ, et al. Evolutionary and codon usage preference insights into spike glycoprotein of SARS-CoV-2. Brief Bioinform. 2021;22:1006–1022. doi: 10.1093/bib/bbaa383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matyášek R, Kovařík A. Mutation patterns of human SARS-CoV-2 and bat RaTG13 coronavirus genomes are strongly biased towards C>U transitions, indicating rapid evolution in their hosts. Genes. 2020;11:761. doi: 10.3390/genes11070761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lundstrom K, Seyran M, Pizzol D, et al. Origin of SARS-CoV-2. Viruses. 2020;12 doi: 10.3390/v12111203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He J, Tao H, Yan Y, Huang SY, Xiao Y. Molecular mechanism of evolution and human infection with SARS-CoV-2. Viruses. 2020;12:428. doi: 10.3390/v12040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang T, Wu Q, Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr Biol. 2020;30:1346. doi: 10.1016/j.cub.2020.03.022. 51.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hul V, Delaune D, Karlsson EA, et al. A novel SARS-CoV-2 related coronavirus in bats from Cambodia. bioRxiv. 2021 doi: 10.1101/2021.01.26.428212. published online Jan 26. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou H, Ji J, Chen X, et al. Identification of novel bat coronaviruses sheds light on the evolutionary origins of SARS-CoV-2 and related viruses. Cell. 2021;184:4380. doi: 10.1016/j.cell.2021.06.008. 91.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lam TT, Shum MH, Zhu HC, et al. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature. 2020;583:282–285. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- 32.Xiao K, Zhai J, Feng Y, et al. Isolation of SARS-CoV-2-related coronavirus from Malayan pangolins. Nature. 2020;583:286–289. doi: 10.1038/s41586-020-2313-x. [DOI] [PubMed] [Google Scholar]
- 33.Murakami S, Kitamura T, Suzuki J, et al. Detection and characterization of bat sarbecovirus phylogenetically related to SARS-CoV-2, Japan. Emerg Infect Dis. 2020;26:3025–3029. doi: 10.3201/eid2612.203386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li P, Guo R, Liu Y, et al. The Rhinolophus affinis bat ACE2 and multiple animal orthologs are functional receptors for bat coronavirus RaTG13 and SARS-CoV-2. Sci Bull. 2021;66:1215–1227. doi: 10.1016/j.scib.2021.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu L, Chen Q, Liu K, et al. Broad host range of SARS-CoV-2 and the molecular basis for SARS-CoV-2 binding to cat ACE2. Cell Discov. 2020;6:68. doi: 10.1038/s41421-020-00210-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deng J, Jin Y, Liu Y, et al. Serological survey of SARS-CoV-2 for experimental, domestic, companion and wild animals excludes intermediate hosts of 35 different species of animals. Transbound Emerg Dis. 2020;67:1745–1749. doi: 10.1111/tbed.13577. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 37.Shi J, Wen Z, Zhong G, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016–1020. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alexander MR, Schoeder CT, Brown JA, et al. Which animals are at risk? Predicting species susceptibility to Covid-19. bioRxiv. 2020 doi: 10.1101/2020.07.09.194563. published online July 10. (preprint). [DOI] [Google Scholar]
- 39.Zhao X, Chen D, Szabla R, et al. Broad and differential animal ACE2 receptor usage by SARS-CoV-2. J Virol. 2020;94:e00940–e01020. doi: 10.1128/JVI.00940-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu K, Pan X, Li L, et al. Binding and molecular basis of the bat coronavirus RaTG13 virus to ACE2 in humans and other species. Cell. 2021;184:3438. doi: 10.1016/j.cell.2021.05.031. 51.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chandler JC, Bevins SN, Ellis JW, et al. SARS-CoV-2 exposure in wild white-tailed deer (Odocoileus virginianus) bioRxiv. 2021 doi: 10.1101/2021.07.29.454326. published online July 29. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amendola A, Bianchi S, Gori M, et al. Evidence of SARS-CoV-2 RNA in an oropharyngeal swab specimen, Milan, Italy, early December 2019. Emerg Infect Dis. 2021;27:648–650. doi: 10.3201/eid2702.204632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.La Rosa G, Mancini P, Bonanno Ferraro G, et al. SARS-CoV-2 has been circulating in northern Italy since December 2019: evidence from environmental monitoring. Sci Total Environ. 2021;750 doi: 10.1016/j.scitotenv.2020.141711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gianotti R, Barberis M, Fellegara G, Galvan-Casas C, Gianotti E. COVID-19-related dermatosis in November 2019: could this case be Italy's patient zero? Br J Dermatol. 2021;184:970–971. doi: 10.1111/bjd.19804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Amendola A, Canuti M, Bianchi S, et al. Molecular evidence for SARS-CoV-2 in samples collected from patients with morbilliform eruptions since late summer 2019 in Lombardy, northern Italy. SSRN. 2021 doi: 10.2139/ssrn.3883274. published online Aug 6. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deslandes A, Berti V, Tandjaoui-Lambotte Y, et al. SARS-CoV-2 was already spreading in France in late December 2019. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.106006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carrat F, Figoni J, Henny J, et al. Evidence of early circulation of SARS-CoV-2 in France: findings from the population-based “CONSTANCES” cohort. Eur J Epidemiol. 2021;36:219–222. doi: 10.1007/s10654-020-00716-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fongaro G, Stoco PH, Souza DSM, et al. The presence of SARS-CoV-2 RNA in human sewage in Santa Catarina, Brazil, November 2019. Sci Total Environ. 2021;778 doi: 10.1016/j.scitotenv.2021.146198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Basavaraju SV, Patton ME, Grimm K, et al. Serologic testing of US blood donations to identify severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-reactive antibodies: December 2019–January 2020. Clin Infect Dis. 2021;72:e1004–e1009. doi: 10.1093/cid/ciaa1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Althoff KN, Schlueter DJ, Anton-Culver H, et al. Antibodies to SARS-CoV-2 in All of Us research program participants, January 2 to March 18, 2020. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab519. published online July 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xing Y, Wong GWK, Ni W, Hu X, Xing Q. Rapid response to an outbreak in Qingdao, China. N Engl J Med. 2020;383:e129. doi: 10.1056/NEJMc2032361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu P, Yang M, Zhao X, et al. Cold-chain transportation in the frozen food industry may have caused a recurrence of COVID-19 cases in destination: successful isolation of SARS-CoV-2 virus from the imported frozen cod package surface. Biosaf Health. 2020;2:199–201. doi: 10.1016/j.bsheal.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chi Y, Zheng S, Liu C, Wang Q. Transmission of SARS-CoV-2 on cold-chain food overpacks: a new challenge. J Glob Health. 2021;11 doi: 10.7189/jogh.11.03071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chi Y, Wang Q, Chen G, Zheng S. The long-term presence of SARS-CoV-2 on cold-chain food packaging surfaces indicates a new COVID-19 winter outbreak: a mini review. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.650493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ji W, Li X, Chen S, Ren L. Transmission of SARS-CoV-2 via fomite, especially cold chain, should not be ignored. Proc Natl Acad Sci USA. 2021;118 doi: 10.1073/pnas.2026093118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pang X, Ren L, Wu S, et al. Cold-chain food contamination as the possible origin of COVID-19 resurgence in Beijing. Natl Sci Rev. 2020;7:1861–1864. doi: 10.1093/nsr/nwaa264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chin AWH, Chu JTS, Perera MRA, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kratzel A, Steiner S, Todt D, et al. Temperature-dependent surface stability of SARS-CoV-2. J Infect. 2020;81:452–482. doi: 10.1016/j.jinf.2020.05.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.The State Council Information Office of the People's Republic of China Fighting COVID-19: China in action. 2020. http://www.scio.gov.cn/zfbps/32832/Document/1681809/1681809.htm
- 63.Chen L, Liu W, Zhang Q, et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect. 2020;9:313–319. doi: 10.1080/22221751.2020.1725399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eurosurveillance Editorial Team Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020 doi: 10.2807/1560-7917.ES.2020.25.5.200131e. published online Feb 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.He Z, Ren L, Yang J, et al. Seroprevalence and humoral immune durability of anti-SARS-CoV-2 antibodies in Wuhan, China: a longitudinal, population-level, cross-sectional study. Lancet. 2021;397:1075–1084. doi: 10.1016/S0140-6736(21)00238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan H, Jiao H, Liu Q, et al. ACE2 receptor usage reveals variation in susceptibility to SARS-CoV and SARS-CoV-2 infection among bat species. Nat Ecol Evol. 2021;5:600–608. doi: 10.1038/s41559-021-01407-1. [DOI] [PubMed] [Google Scholar]
- 70.Koplan JP, Bond TC, Merson MH, et al. Towards a common definition of global health. Lancet. 2009;373:1993–1995. doi: 10.1016/S0140-6736(09)60332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lemey P, Pybus OG, Wang B, Saksena NK, Salemi M, Vandamme AM. Tracing the origin and history of the HIV-2 epidemic. Proc Natl Acad Sci USA. 2003;100:6588–6592. doi: 10.1073/pnas.0936469100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sharp PM, Hahn BH. Origins of HIV and the AIDS pandemic. Cold Spring Harb Perspect Med. 2011;1 doi: 10.1101/cshperspect.a006841. [DOI] [PMC free article] [PubMed] [Google Scholar]


