Abstract
Objective.
The rapid emergence of the Covid-19 pandemic in the United States has dramatically altered daily life and taken a toll on Americans’ physical, mental, social, and financial well-being. Based on previous widespread disasters, future high prevalence of short- and long-term adverse mental health consequences are anticipated. Studies of Covid-19 outside the U.S. indicated moderately high levels of distress, but we have little information regarding Americans’ distress nor the factors associated with relative distress or adjustment during this unprecedented time. This study represents the first national view of Americans’ distress during the massive disruption of Covid-19 and identifies levels of stress exposure, protective psychosocial resources, and coping strategies.
Method.
Data were collected April 7–9, 2020 from an online platform, employing best practices for ensuring high-quality data; 1015 completed respondents are included [(53.9% women; average age = 38.9 years; mostly White (82.4%) and Non-Hispanic (91.5%)]. Respondents’ locations ranged across the U.S., from 18.5% in the Northeast to 37.8% in the South.
Results.
Fairly high levels of stress exposure and peritraumatic and general distress (depression, anxiety, and stress) were reported. Emotion regulation skills along with active and distraction coping emerged as the strongest predictors of lower distress levels.
Conclusions.
These results identify potential targets for online mental health interventions—focusing on engaging in adaptive emotion regulation and coping (e.g., through telehealth mental health first aid)—during the pandemic to offset the likely rise in distress over the months ahead.
Keywords: Covid-19 pandemic, stressors, peritraumatic distress, social support, emotion regulation skills, coping
The rapid emergence of the Covid-19 pandemic in the United States substantially altered daily routines and brought tremendous uncertainty and disruption. Americans were abruptly forced to navigate school and business closures, employment insecurity, and drastic changes in social behavior. Based on early reporting of Covid-19—and on the experiences of SARS, terrorist attacks, and other widespread crises—adverse mental health consequences such as anxiety, depression, and post-traumatic stress symptoms (PTSS) are expected to be substantial and persistent (Galea et al., 2020).
Early Covid-19 studies from China suggest moderate impacts on mental health early in the pandemic (late 2019 and early 2020) (Qiu et al., 2020; Zhang et al., 2020). For example, although less than one-third of a national sample in China reported elevated depression, anxiety, or stress, 53.8% reported severe PTSS (Wang et al., 2020). Americans reported higher general distress in April 2020 compared to April 2018, suggesting the pandemic was taking a toll (McGinty et al., 2020). We aimed to document levels of distress in the US and identify the factors associated with distress early in the pandemic. To identify these factors, we applied the transactional stress/coping model (Lazarus & Folkman, 1984). According to this model, individuals’ psychosocial resources and coping responses influence the impact of stress exposure on distress (Aldwin, 2007).
This paper presents survey results of Americans in early April 2020 assessing both general distress (i.e., depression, anxiety, and stress) and distress specific to Covid-19 (peritraumatic distress; PTD). PTD is particularly relevant in the current pandemic: PTD concerns cognitive and affective responses during exposure to severe stressors (e.g., horror, helplessness, fear for safety, grief) (Brunet et al., 2001) and is closely associated with subsequent longer-term adverse mental health sequelae, especially PTSS, in community-wide disasters (e.g., Bell et al., 2017). However, PTD has only been assessed retrospectively—usually long afterward—rather than during a long-lasting and open-ended crisis such as the current pandemic.
Previous research following natural (e.g., floods), technological (e.g., nuclear meltdown), and terrorist-initiated (e.g., 9/11) community-wide disasters has identified potentially helpful demographic factors (male gender, older age, greater financial resources), psychosocial resources (e.g., emotion regulation skills, social support, mindfulness), and coping strategies (the specific ways that individuals manage stressors, such as actively trying to resolve some aspects of the situation) (Bell et al., 2017; Bonanno et al., 2007). However, whether these helpful resources and coping apply in the context of Covid-19, an ongoing, evolving, and society-wide disruption with proscriptions on many usual social behaviors (CDC, 2020) remains unknown.
Emotion regulation skills have been shown to be protective for individuals exposed to community disasters (Ehring & Quack, 2010), and social support has long been recognized as mitigating the impact of stress on mental health following community-wide disasters (e.g., Pietrzak et al., 2014). In one study of Hurricane Katrina survivors, social support moderated effects of exposure on depression and PTSS two years later (McGuire et al., 2018). Curiously, although mindfulness is a recent focus of stress research (e.g., Johnson et al., 2014), relatively little work has linked mindfulness to post-disaster adjustment, and of that work, results are mixed. Some studies have found beneficial relations between mindfulness and PTSS (e.g., Nitzan-Assayag et al., 2015) while others have not (e.g., An et al., 2018).
Regarding coping, some strategies generally regarded as helpful, such as active coping and seeking social support (Aldwin, 2007), have been associated with lower PTSS following a community-wide crisis (e.g., Baral & Bhagawati, 2019; Park et al., 2012) while other generally maladaptive strategies, such as substance abuse coping, have been related to higher levels of distress including PTSS specifically following community-wide crises (e.g., Park et al., 2012). In the context of disaster, however, many different coping strategies may be associated with less distress, given the myriad high and low controllability stressors that disaster encompasses (Park & Blake, 2020). For example, religious coping and positive reappraisal are not always shown to be helpful, but following disasters, are often related to less distress (see Park & Blake, 2020, for a review). Similarly, distraction—often shown to be unhelpful (Aldwin, 2007)—may help individuals to cope with aversive aspects of disaster that they can do nothing to solve. The complex role of coping was demonstrated in a study of Nepalese after a major earthquake, in which both active coping and distraction related to lower PTSS ten months afterward (Baral et al., 2019).
We aimed to document levels of distress in our national sample of Americans early in the pandemic and to test whether psychosocial resources and coping strategies shown to be beneficial in previous disasters would uniquely demonstrate similar favorable relations with distress in the context of Covid-19. Because we expected individuals with greater stress exposure and certain demographic characteristics (e.g., non-male gender, younger age, financial insecurity) to exhibit stronger stress responses to the COVID-19 pandemic (see Park et al., 2020), these static risk factors were included as covariates to illuminate the unique associations of psychosocial resources (emotion regulation mindfulness, social support) and coping--all important modifiable factors, on mental health. We hypothesized that the psychosocial resources and coping shown to be helpful in previous studies reviewed above would be helpful here, but we also speculated that a broader range of coping might be favorably related with lower distress given the ongoing nature of the pandemic and diverse stressors it entailed. Identifying helpful psychosocial resources and coping strategies may assist in understanding processes of adaptive adjustment and provide actionable insights for immediate interventions as well as inform future preventive and resilience-enhancing efforts.
Method
Participants
Participants were recruited from the Amazon Mechanical Turk (MTurk) online worker pool. Eligible participants were adults aged 18 or older, residing in the U.S., and able to read English. Of the 1086 unique responses to the baseline study, the final baseline sample included 1015 participants after removing duplicates and responses completed too quickly (see analysis section below for details). MTurk workers are more diverse than typical student or online forum samples and fairly representative of larger populations, including the U.S. (Sheehan & Pittman, 2016). Evaluations have found the data obtained on MTurk to be high quality, replicable, and valid across comparisons with frequently used academic platforms and student and professional samples (Kees et al., 2017; Sheehan, 2018). Although some research suggests that MTurk respondents report higher levels of depression than the general population (e.g., Ophir et al., 2019), other studies indicate mental health of MTurk workers approximates that of the general U.S. population (e.g., Elhai et al., 2016; Kim & Hodgins, 2017; Mortensen & Hughes, 2017).
Data Collection
The University of Connecticut IRB (X20–0057) approved all study materials. Participants signed up for the study on the MTurk homepage and provided informed consent prior. The project was advertised as an anonymous, longitudinal study of the impact of Covid-19 on daily life, providing $2 in Amazon.com credit for each timepoint completed. Data presented here were collected from April 7–9, 2020, approximately 3 weeks after widespread shelter-in-place recommendations were first issued in the U.S.
Measures
Demographics
Participants reported on their location by state, financial security, whether they were a primary caregiver for a dependent, partner status, gender, sexual orientation, race, ethnicity, and age. For descriptive purposes, states were categorized into four distinct regions based on divisions used in the U.S. Census (West, Midwest, Northeast, and South; US Census, 2020).
Covid-19 Stressors
Based on previous work during SARS and the early months of the Covid-19 pandemic (Brooks et al., 2020; Main et al., 2011; Qiu et al., 2020), we created a novel measure of Covid-19 stressors. This measure assesses individuals’ exposure (“Yes” vs “No”) to 23 stressors in the past week (see Figure 1 for items). A total score of stressor exposure was tallied by summing together the total number of “Yes” responses (possible range 0–23).
Figure 1.
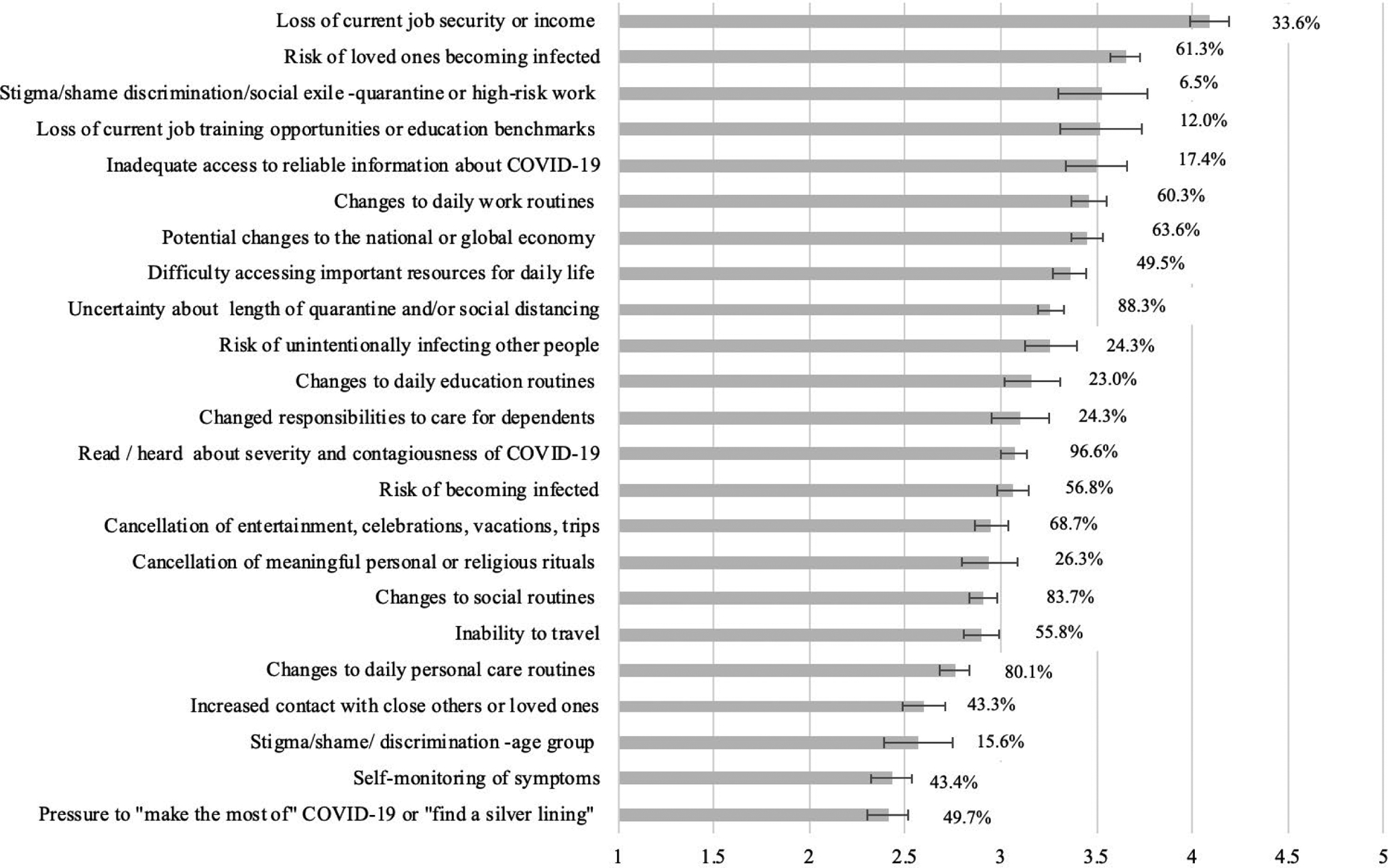
Stress Exposure and Appraised stressfulness of COVID-19 stressors
Notes. Percentages listed next to the shaded bars represent the proportion of the total sample (N = 1015) who endorsed experiencing each item. Stress appraisal items (rated 1 (“not at all stressful”) to 5 (“extremely stressful”)) were only completed for items endorsed. Error bars represent 95% confidence intervals for stress appraisals. A comparison of demographic differences in % experienced and average stress appraisals is available in Park et al., 2020.
Mindfulness.
Mindfulness was assessed using the 10-item Cognitive Affective Mindfulness Scale-Revised (CAMS-R; Feldman et al., 2007). The CAMS-R demonstrates strong psychometric properties in samples not regularly engaged in mindfulness training (Feldman et al., 2007; Finkelstein-Fox et al., 2018). Items on the CAMS-R address present moment awareness and acceptance, non-specific to stressful experience. Items are rated on a scale of 1 (“rarely/not at all”) to 4 (“almost always”). Cronbach’s alpha in the present sample was .88.
Emotion Regulation Skills.
To assess emotion regulation skills, we used the (inverse score of the) 18-item Difficulties in Emotion Regulation Scale (DERS-18; Kaufman et al., 2016; Victor & Klonsky, 2016). The DERS covers domains of emotional awareness, clarity, acceptance, goal pursuit, impulse control, and access to strategies. An inverse of the sum score of the DERS was used to assess general adaptive emotional regulation ability, with total possible scores ranging from – 90 to −18. Cronbach’s alpha was .92 in the present sample.
Social Support.
Participants completed the brief 4-item appraisal subscale of the Interpersonal Support Evaluation List-12 (ISEL-12; Cohen et al., 1985) as a measure of the perceived availability of supportive others. The ISEL-12 has demonstrated strong psychometric properties in a wide range of samples. The appraisal subscale was selected here as the most appropriate type of social support to assess given social distancing and other constraints. Items are rated from 0 (“definitely false”) to 3 (“definitely true”) and summed to create a total subscale score for the 4 appraisal items (range = 0–12). Cronbach’s alpha in the present sample was .88.
Covid-19-Specific Coping.
Selected subscales from the Brief COPE (Carver, 1997) assessed the use of active coping (2 items, r = .62, p < .001), self-distraction (2 items, r = .32, p <.001), behavioral disengagement (2 items, r = .59, p <.001), humor (2 items, r =.79, p <.001), substance use (4 items, alpha = .96), emotional support-seeking (2 items, r =.72, p <.001), instrumental support-seeking (2 items, r =.71, p <.001), and religious coping (2 items, r =.83, p <.001). For each item, participants were prompted to indicate how much they had coped with “Covid-19 related stressors” over the past week on a 4-point Likert scale ranging from 1 (“I haven’t been doing this at all”) to 4 (“I’ve been doing this a lot”). To address stress mobilization effects often seen in cross-sectional studies of stress and coping (i.e., coping is positively related to distress; Aldwin, 2007), we calculated 1) average of items in each coping subscale and 2) total of all averaged coping subscales converted these average scores into a ratio score (e.g., active coping/total coping expenditure; Vitaliano et al., 1987). Coping scores should thus be interpreted as relative amounts of each coping strategy compared to one’s total coping expenditure.
General Distress.
Past-week general distress was assessed using the 21-item version of the Depression, Anxiety, and Stress Scales (DASS-21; Lovibond & Lovibond, 1995). Items on the DASS-21 are rated on a Likert scale ranging from 0 (“Did not apply to me at all“) to 3 (“Applied to me very much or most of the time“). Scores are summed and multiplied by 2 to create separate seven-item subscales (subscale scores range from 0–42). The DASS-21 demonstrated good psychometric properties in a Chinese sample exposed to Covid-19 (Wang et al., 2020) as well as for participants recruited via MTurk (e.g., Arditte et al., 2016). Cronbach’s alphas were .92 for depression, .89 for anxiety, and .90 for stress in the present sample. Although the DASS-21 is a self-report measure and not appropriate for clinical diagnoses, depression scores from 10–12 indicate mild, 13–20 indicate moderate, 21–27 indicate severe, and 28 indicate extreme severity. Anxiety scores from 7–9 indicate mild, 10–14 indicate moderate, 15–19 indicate severe, and 20–42 indicate extreme severity. Stress scores from 11–18 indicate mild, 19–26 indicate moderate, 27–34 indicate severe, and 35–42 indicate extreme severity.
Covid-19-Specific Distress.
The Peritraumatic Distress Inventory (PDI; Brunet et al., 2001) is a 13-item self-report measure of distress during a trauma (in this case, Covid-19). Items were scored from 0 (“not at all”) to 3 (“extremely true”); we inadvertently excluded the response option “slightly true.” The PDI has shown strong internal consistency and test-retest reliability and validity in previous research (Brunet et al., 2001). An average of all 13 items was tallied. Cronbach’s alpha was .90 in the present sample. To facilitate comparison with the original published measure, scores were also calculated based on response options presented to participants (i.e., 0, 2, 3, and 4), excluding the “slightly true” (1) option. Original raw scores were used as outcomes for bivariate correlation and regression analyses while the re-calculated sum score was used for mean comparisons only (as noted below).
Analysis Plan
Primary analyses to test study hypotheses include basic descriptive (mean and standard deviation), bivariate correlation, and multiple linear regression. The final multiple regression models were tested separately for each of the four distress outcomes (PDS, depression, anxiety, stress), entering Covid-19 stressor exposure, coping ratios, and psychosocial resources simultaneously as covariates. A priori power analysis for the longitudinal parent study of demographic differences in stress-related adjustment throughout the Covid-19 pandemic suggested that a sample size of N = 1050 would provide 80% power to detect small (d = .20) differences between categorical groups imbalanced at a 3:1 ratio and approximately 90% power to detect small (d = .20) group differences between groups equally balanced at a 1:1 ratio (two-tailed alpha = 0.05). Data cleaning and analyses were conducted in SPSS (version 26).
Duplicate responses were deleted based on participants’ self-reported MTurk IDs, retaining the first completed response (N = 12). Responses submitted in <10 minutes (i.e., less than half of the expected time based on pilot testing) were excluded from analyses (N = 59). The final dataset consisted of 1015 unique participants. Missingness for all items was <1%. Male gender was the comparison group for all gender comparisons; thus, coefficients for female and other gender refer to the size mean difference for female vs. male and other gender vs. male participants, holding all other predictors constant. Because coping ratio scores were calculated for each coping scale in relation to the others, behavioral disengagement coping was selected as the reference group for the other strategies assessed and omitted from simultaneous multiple regression analyses to prevent perfect multicollinearity.
Results
Our sample was fairly evenly split between male (n = 453, 44.6%) and female (n = 547, 53.9%) gender, with an additional 15 (1.5%) participants endorsing non-binary, transgender, self-described, or prefer not to say (collectively coded as “other”), with an average age of 38.9 years (SD = 13.50, range = 18–88). The sample was primarily White (n = 836, 82.4%) and non-Latinx (n = 929, 91.5%) and included African-Americans (n = 122, 12.0%), Asian/Asian-Americans (n = 121, 11.9%), Native Hawaiian/Other Pacific Islanders (n = 50; 4.9%), and American Indian/Alaskan Natives (n = 70; 6.9%). About half of participants (n = 513; 50.5%) endorsed having at least “mostly” enough money to meet their needs. Locations were reported across the U.S. (n = 188, 18.5% in the Northeast; n = 199, 19.6% in the Midwest; n = 244, 30.0% in the West; and n = 383, 37.7% in the South). Of the full sample of 1015, just 61 participants (6.0%) indicated that they had “felt unwell/sick or had a fever in the last 7 days or tested positive for COVID-19.”
Covid-19 Stress Exposure and Appraisal
As shown in Figure 1, participants’ stressful appraisal ratings were highest for loss of job security or income, followed by risk of loved ones becoming infected, stigma, or shame regarding quarantine or high-risk work, loss of job or education benchmarks, lack of access to reliable information about Covid-19, changes to daily work routines, and potential changes to the national economy; many stressors were appraised above the scale midpoint. Of these stressors, many were very commonly reported (e.g., reading/hearing about Covid-19, uncertainty about quarantine/social distancing) while others were quite infrequent (e.g., stigma).
Characterizing COVID-19 Distress in the Present Sample
Means for our psychological distress measures suggested a substantial portion of the sample was experiencing heightened distress (see Table 1). The item mean for the rescaled PDI of 1.13 (SD = 0.80), assessing PTD, was higher than that reported in survivors of earthquakes in Christchurch, New Zealand, assessed retrospectively two years later (1.02; Bell et al., 2017) but lower than that reported in survivors of earthquakes in Haiti assessed retrospectively two and a half years later (1.5; Cénat & Derivois, 2014).
Table 1.
Descriptives and Bivariate Correlations
| M(SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Emotion Regulation Skills | −36.84 (13.13) | 1 | |||||||||||||||
| 2. Mindfulness | 29.03 (5.81) | .63*** | 1 | ||||||||||||||
| 3. Social Support | 8.86 (3.30) | .45*** | .35*** | 1 | |||||||||||||
| 4. Total Stressor Exposure | 10.82 (3.81) | −.19*** | −.03 | .00 | 1 | ||||||||||||
| 5. Active coping | 0.16 (0.04) | .25*** | .29*** | .09** | .00 | 1 | |||||||||||
| 6. Substance coping | 0.09 (0.04) | −.26*** | −.19*** | −.19*** | .02 | −.30*** | 1 | ||||||||||
| 7. Distraction coping | 0.17 (0.05) | .03 | −.05 | −.07* | −.03 | .05 | −.10** | 1 | |||||||||
| 8. Behav Diseng coping | 0.09 (0.04) | −.37*** | −.31*** | −.35*** | .06 | −.31*** | .22*** | −.09** | 1 | ||||||||
| 9. Humor coping | 0.12 (0.05) | −.06 | −.07* | −.09** | −.08** | −.22*** | .07* | −.19*** | −.01 | 1 | |||||||
| 10. Instrumental support coping | 0.12 (0.04) | −.03 | −.01 | .15*** | .12*** | −.11** | −.25*** | −.21*** | −.17*** | −.24*** | 1 | ||||||
| 11. Emotional support coping | 0.14 (0.04) | .21*** | .18*** | .43*** | .06 | −.11*** | −.26*** | −.20*** | −.33*** | −.26*** | .36*** | 1 | |||||
| 12. Religious coping | 0.11 (0.05) | .11*** | .08* | .01 | −.03 | −.08* | −.26*** | −.29*** | −.13*** | −.26*** | −.14*** | −.10** | 1 | ||||
| 13. PDI2 | 0.93 (0.73) | −.52** | .24*** | −.19*** | .47*** | −.12*** | .12*** | −.07* | .20*** | −.18*** | .16*** | .03 | −.02 | 1 | |||
| 14. Depression | 9.59 (10.46) | −.71*** | −.47*** | −.50*** | .23*** | −.26*** | .28*** | .02 | .41*** | .03 | −.02 | −.20*** | −.15*** | .60*** | 1 | ||
| 15. Anxiety | 5.76 (8.19) | −.60*** | −.30*** | .29*** | .27*** | −.18*** | .21*** | .15*** | .27*** | −.03 | .07* | −.10** | .00 | .67*** | .67 *** | 1 | |
| 16. Stress | 10.51 (9.65) | −.67** | −.43*** | .31*** | .35*** | −.21*** | 26*** | −.05 | .28*** | .01 | .04 | −.10** | .12*** | .65*** | .77 *** | .74*** | 1 |
Notes.
p < .001,
p < .01,
p < .05.
All coping subscales represent a ratio of the specific type of coping vs. total amount of coping (e.g., average active coping / total of all coping averages).
“Emotion Regulation Skills” taken as the inverse of the DERS total score.
Peritraumatic Distress was on a 0–3 scale, as originally administered.
Means of the DASS-21 subscales demonstrated heightened distress. For depression, 60.2% of the sample scored in the normal range, 7.9% in the mild, 15.1% in the moderate, and 16.7% in the severe/extremely severe. For anxiety, 72.0%, 5.0%, 7.8%, and 16.7%, respectively. For stress, 71.6%, 8.9%, 10.3%, and 10.1%, respectively. These figures were somewhat higher than the Covid-19 study in China (Wang, 2020), which found 4.3% of the sample in the severe/extremely severe range for depression, 8.4% for anxiety, and 2.6% for stress. Means for depression and anxiety were somewhat elevated compared to a nationally representative sample of Americans (Sinclair et al., 2012) and other recent MTurk studies (e.g., Elhai et al., 2016; Kim & Hodgins, 2017; Mortensen & Hughes, 2017), but lower than that from another study of MTurk workers (Arditte et al., 2016).
Bivariate Associations between Stressors, Resources, Coping and Distress
Bivariate correlation analyses demonstrated moderate positive associations between stressor exposure and distress (rs = .47 for PTD, .23 for depression, .27 for anxiety, and .35 for stress, all ps < .001) and all four distress measures were positively correlated (rs from .60 to .77, all ps < .001). Bivariate correlations between continuous variables are reported in in Table 1.
Transactional Regression Models of Stressors, Resources, and Coping Predicting Distress
Full results of multivariate linear regression models testing the strength of unique associations between stress exposure, psychosocial resources and Covid-19-specific coping strategies on four indicators of distress are provided in Table 2. Significant positive predictors of PTD included female gender (female vs. male β = 0.10, p < .001), stress exposure (β = 0.33, p < .001), and mindfulness (β = 0.12, p < ,001), whereas greater financial resources (β = −0.07, p = .01), emotion regulation skills (β = −0.48, p < .001), and use of distraction (β = −0.12, p < .003), humor (β = −0.22, p < .001), and active (β = −0.08, p = .03) coping had unique negative associations with PTD (Adj R2 =0.47, F(15, 999) = 60.34, p < .001). Stress exposure was the sole significant positive predictor of depression (β = 0.11, p < .001), while greater emotion regulation skills (β = −0.51, p < .001), social support (β = −0.22, p < .001), and coping involving active (β = −0.21, p < .001), substance use (β = −0.07, p = .048), distraction (β = −0.13, p < .001), humor (β = −0.18, p < .001), religious coping (β = −0.24, p < .001), and seeking instrumental (i.e., asking for tangible help or assistance from others) (β = −0.12, p < .001) and emotional (i.e., discussing one’s feelings with others) (β = −0.10, p = .003) support were each uniquely negatively associated with depression (Adj R2 = .60, F(15, 999) = 100.36, p < .001). Stress exposure (β = 0.14, p < .001) and mindfulness (β = 0.12, p < .001) were the only significant positive predictors of anxiety symptoms, whereas older age (β = −0.08, p = .01), emotion regulation skills (β = −0.55, p < .001), social support (β = −0.07, p = .03), and use of active (β = −0.08, p = .04), distraction (β = −0.18, p < .001), and humor (β = −0.12, p = .004) coping were uniquely negatively associated with anxiety (Adj R2 = .42, F(15, 999) = 49.82, p < .001). Finally, significant positive predictors of stress symptoms included female gender (β = 0.08, p = .001) and stress exposure (β = 0.21, p < .001), whereas emotion regulation skills (β = −0.53, p < .001), distraction (β = −0.08, p = .03), and religious (β = −0.09, p = .03) coping were significant unique negative correlates of stress (Adj R2 = .52, F(15, 999) = 73.25, p < .001).
Table 2.
Multivariate Linear Regression Predicting Distress
| Peritraumatic Distress1 | ||||
|---|---|---|---|---|
| Estimate | 95% CI | β | p | |
| Intercept | 0.05 | [−0.69, 0.78] | - | .90 |
| Age | −0.01 | [−0.00, 0.00] | −.02 | .35 |
| Financial Needs Met | −0.03 | [−0.05, −0.01] | −.07 | .01 |
| Male v Female | 0.11 | [0.06, 0.16] | .10 | <.001 |
| Male v Other | 0.02 | [−0.18, 0.23] | .01 | .82 |
| Emotion Regulation Skills1 | −0.02 | [−0.02, −0.02] | −.48 | <.001 |
| Mindfulness | 0.01 | [0.01, 0.02] | .12 | <.001 |
| Social Support | −0.00 | [−0.01, 0.01] | −.03 | .36 |
| Total Stressor Exposure | 0.05 | [0.04, 0.05] | .33 | <.001 |
| Active Coping Ratio | −0.99 | [−1.86, −0.10] | −.08 | .03 |
| Substance Coping Ratio | −0.51 | [−1.56, 0.55] | −.04 | .35 |
| Distraction Coping Ratio | −1.35 | [−2.25, −0.44] | −.12 | .003 |
| Humor Coping Ratio | −2.40 | [−3.28, −1.51] | −.22 | <.001 |
| Instrumental Support Coping Ratio | 0.16 | [−0.90, 1.22] | .01 | .77 |
| Emotional Support Coping Ratio | −0.11 | [−1.06, 0.85] | −.01 | .83 |
| Religious Coping Ratio | −0.80 | [−1.68, 0.07] | −.08 | .07 |
| F(15, 999) = 60.34, p <. 001, Adj R2 = .47 | ||||
| Depression | ||||
| Estimate | 95% CI | β | p | |
| Intercept | 30.41 | [18.14, 42.69] | - | <.001 |
| Age | −0.00 | [−0.04, 0.03] | −.00 | .94 |
| Financial Needs Met | −0.84 | [−1.20, −0.49] | −.10 | <.001 |
| Male v Female | 0.67 | [−0.20, 1.55] | .03 | .13 |
| Male v Other | −0.94 | [−4.39, 2.52] | −.01 | .60 |
| Emotion Regulation Skills | −0.40 | [−0.45, −0.36] | −.51 | <.001 |
| Mindfulness | 0.04 | [−0.06, 0.13] | .02 | .43 |
| Social Support | −0.68 | [−0.84, 0.53] | −.22 | <.001 |
| Total Stressor Exposure | 0.30 | [0.19, 0.42] | .11 | <.001 |
| Active Coping Ratio | −48.32 | [−63.06, −33.57] | −.21 | <.001 |
| Substance Coping Ratio | −17.85 | [−35.57, −0.14] | −.07 | .048 |
| Distraction Coping Ratio | −29.39 | [44.47, −14.31] | −.13 | <.001 |
| Humor Coping Ratio | −38.48 | [53.29, −23.67] | −.18 | <.001 |
| Instrumental Support Coping Ratio | −34.56 | [52.29, 16.84] | −.12 | <.001 |
| Emotional Support Coping Ratio | −24.33 | [−40.33, −8.33] | −.10 | .003 |
| Religious Coping Ratio | −46.13 | [−60.76, −31.50] | −.24 | <.001 |
| F(15, 999) = 100.36, p <. 001, Adj R2 = .60 | ||||
| Anxiety | ||||
| Estimate | 95% CI | β | p | |
| Intercept | −0.20 | [−11.71, 13.31] | - | .97 |
| Age | −0.04 | [−0.08, −0.01] | −.07 | .01 |
| Financial Needs Met | −0.15 | [−0.48, 0.19] | −.02 | .38 |
| Male v Female | 0.74 | [−0.08, 1.56] | .05 | .08 |
| Male v Other | 0.09 | [−3.15, 3.35] | .00 | .96 |
| Emotion Regulation Skills | −0.35 | [−0.39, −0.30] | −.55 | <.001 |
| Mindfulness | 0.17 | [0.08, 0.26] | .12 | <.001 |
| Social Support | −0.16 | [−0.31, −0.02] | −.07 | .03 |
| Total Stressor Exposure | 0.29 | [0.18, 0.40] | .14 | <.001 |
| Active Coping Ratio | −14.41 | [−28.23, −0.59] | −.08 | .04 |
| Substance Coping Ratio | 2.95 | [−13.65, 19.56] | .02 | .73 |
| Distraction Coping Ratio | −29.83 | [−43.97, −15.69] | −.17 | <.001 |
| Humor Coping Ratio | −20.42 | [−34.30, −6.54] | −.12 | .004 |
| Instrumental Support Coping Ratio | −3.84 | [−20.46, 12.77] | −.02 | .65 |
| Emotional Support Coping Ratio | −8.27 | [−23.27, 6.73] | −.04 | .28 |
| Religious Coping Ratio | −3.46 | [−17.18, 10.26] | −.02 | .62 |
| F(15, 999) = 49.82, p <. 001, Adj R2 = .42 | ||||
| Stress | ||||
| Estimate | 95% CI | β | p | |
| Intercept | 1.83 | [−10.54, 14.19] | - | .77 |
| Age | −0.02 | [−0.06, 0.01] | −.03 | .20 |
| Financial Needs Met | −0.26 | [−0.62, 0.10] | −.03 | .15 |
| Male v Female | 1.51 | [0.62, 2.39] | .08 | .001 |
| Male v Other | 2.94 | [−0.54, 6.42] | .04 | .10 |
| Emotion Regulation Skills | −0.39 | [−0.44, −0.35] | −.53 | <.001 |
| Mindfulness | −0.05 | [−0.14, 0.05] | −.03 | .32 |
| Social Support | −0.14 | [−0.29, 0.02] | −.05 | .08 |
| Total Stressor Exposure | 0.54 | [0.43, 0.66] | .21 | <.001 |
| Active Coping Ratio | −11.99 | [−26.84, 2.86] | −.06 | .12 |
| Substance Coping Ratio | 11.89 | [−5.96, 29.74] | .05 | .19 |
| Distraction Coping Ratio | −16.67 | [−31.86, −1.48] | −.08 | .03 |
| Humor Coping Ratio | −13.99 | [−28.91, 0.92] | −.07 | .07 |
| Instrumental Support Coping Ratio | −8.75 | [−26.61, 9.10] | −.03 | .34 |
| Emotional Support Coping Ratio | 0.61 | [−15.51, 16.74] | .00 | .94 |
| Religious Coping Ratio | −16.05 | [−30.79, −1.31] | −.09 | .03 |
| F(15, 999) = 73.25, p <. 001, Adj R2 = .52 | ||||
Notes. Key covariates were identified as age, financial resources, and gender, based on robust evidence of group differences in stress, coping, and mental health. Models were also tested including race, ethnicity, marital status, and sexual orientation as simultaneous covariates, based on significant patterns of bivariate association (reported in Park et al., 2020]). These covariates did not significantly impact model fit or coefficient interpretation and were removed from the final model.
“Emotion Regulation Skills” taken as the inverse of the DERS total score.
Peritraumatic Distress was on a 0–3 scale, as originally administered.
Discussion
Overall, Americans exhibited elevations in general distress similar to those seen in China in the midst of the Covid-19 outbreak. Yet our sample appeared more distressed than participants in these studies as well as some recent studies of the MTurk worker pool (e.g., Kim & Hodgkins, 2017). Noted elevations may be due to cultural differences regarding social distancing and other prevention practices, or to the fact that earlier studies (e.g., Wang et al., 2020) were conducted prior to the full-scale pandemic. In addition, PDI scores suggest levels comparable to those of previous studies of high magnitude trauma, with a substantial minority experiencing very high levels. Thus, our results suggest a great deal of psychological suffering, which may bode poorly for long-term mental health (Galea et al., 2020), similar to what has been observed in previous community disasters (e.g., Fergusson et al., 2014).
The transactional stress and coping framework allowed us to home in on factors that may lead to better adjustment in the midst of living in a pandemic. Similar to previous studies (e.g., Bell et al., 2017), older age and male gender were protective demographics, suggesting that younger adults and women may be more vulnerable. When all other variables were held constant, individuals with limited financial resources were still at greater risk for peritraumatic distress and depression, but not anxiety and psychological stress. We focused particularly on individuals’ stress exposure, resources and coping, given that specific stress management interventions can be effectively delivered online (e.g., Heber et al., 2016). Even when self-regulation and coping resources were accounted for, higher levels of stress exposure remained uniquely associated with PTD, depression, anxiety, and stress; thus, some level of emotional reaction to COVID-19 may be inevitable in instances of very high stress exposure, even when individuals are otherwise well-equipped to manage adjustment. Psychosocial resources were also associated with less distress. In particular, in multivariate analyses, emotion regulation skills were strongly associated with less distress in all domains. Emotion regulation consistently relates to better adjustment in both acute and chronic stressful situations (Sloan et al., 2017), so its salutary relations, in the context of the high-stress pandemic, is encouraging albeit not surprising.
Curiously, although perceived social support and mindfulness related to less distress at the bivariate level, these effects weakened when considered in multivariate models including other psychosocial resources and coping as predictors. Participants’ perceived social support was uniquely associated with lower depression and anxiety, but not PTD or stress levels, perhaps due to perceived social support’s strong overlap with emotion regulation resources. Also unexpectedly, in multivariate analyses, mindfulness actually related to greater PTD and anxiety. These findings may reflect the shared variance between emotion regulation skills and mindfulness; even in bivariate associations, emotion regulation related much more strongly to distress than did mindfulness (cf. Finkelstein-Fox et al., 2018). Mindfulness has been posited to influence well-being through emotion regulation (e.g., Roemer et al., 2015); it may be that once the shared variance with adaptive emotion regulation is accounted for, remaining elements of mindfulness, such as pure awareness, are associated with increased attention to distress. Although some recent research from Covid-19 participants in China found mindfulness minimally effectiveness in alleviating distress (Sweeny et al., unpublished), salutary effects of mindfulness may emerge over time, particularly for individuals with limited self-regulatory resources (e.g., Finkelstein-Fox et al., 2018).
Although the present results are important in portraying Americans’ early responses to the pandemic, limitations must be noted. First, we studied MTurk workers, who are not fully nationally representative (Walters et al., 2018). Results are cross-sectional in nature, and neither causal nor even temporal ordering can be inferred. Clearly, multiple assessments over a longer timeframe are needed (Bonanno et al., 2007), particularly given the rapidly changing nature of the pandemic and its implications for Americans’ lives. Although we captured many constructs, many others were left out, and we used some abbreviated measures with suboptimal psychometric properties (e.g., Brief COPE; Carver, 1997). We also inadvertently excluded the response option “slightly true” for the PTD measure.
Intervention implications
These findings suggest that interventions promoting emotion regulation and coping skills may help individuals endure lengthy periods of social isolation despite little control over many of the stressors at hand (Sloan et al., 2017). We found a wide range of coping strategies were associated with less distress. In particular, use of active coping, seeking social support, distraction, humor, religious coping and even substance use, relative to total coping expenditure (including behavioral disengagement) were associated with at least one indicator of resilient mental health. Contrary to the general coping literature, beneficial effects of emotion-focused strategies such as humor and distraction were observed and even outweighed the effects of active coping for managing COVID-19-related distress. This unusually wide array of coping related to less distress may due to individuals’ needs to employ a variety of strategies to deal with different demands required by different pandemic-related stressors. Many of these stressors are low in controllability (e.g., uncertainty, lack of social contact) and many strategies that may normally be employed (e.g., seeking company, working out at the gym) are unavailable. Collectively, these coping activities may reflect managing one’s stressful situation to the extent possible and accepting those aspects beyond control while also protecting immediate mental well-being (Finkelstein & Park, 2019). This approach, employing a wide range of coping strategies simultaneously, may provide a sense of agency and alleviate feelings of helplessness in the context of an ongoing and multifaceted stressful pandemic (Aldwin, 2007).
These findings have important implications for both likely long-term mental health and potential immediate online and technology-assisted interventions. Women, younger adults, and individuals with financial strain, reporting more distress during the pandemic, may particularly benefit from remote mental health intervention. Adaptive emotion regulation and active coping, along with gradual re-exposure to feared stimuli such as crowded public spaces and use of healthy distraction from ongoing worries, may serve as potent targets for remotely-delivered cognitive behavioral therapies to offset the likely rise in PTSS as the pandemic unfolds in the months ahead (e.g., Litz et al., 2007; Yuen et al., 2015). Given the likelihood of on-going recommendations for quarantine and restrictions on in-person socialization, mental health professionals may also proactively develop and disseminate telehealth mental health first aid and provide suggested structure and content for broadly disseminated online resources. For example, practices that counter rumination and anxiety by actively redirecting attention and reframing negative interpretations could be taught (e.g., Berking et al., 2008; Sweeny et al., 2012). Interventions that teach discernment of controllability of stressors and implementation of appropriate strategies have been developed largely in behavioral medicine and delivered online (e.g., Cox et al., 2018); such programs could be adapted to the pandemic to help individuals implement more active coping for stressors amenable to direct change and reappraisal or distraction for those less amenable. Many mobile interventions for anxiety and stress management are already available (e.g., Christensen et al., 2014). For example, the National Center for PTSD is now disseminating a free Covid-specific stress management app, Covid Coach (NCPTSD, 2020).
Concurrently, policymakers can assess the equitable access to high-bandwidth technology needed to support computer-mediated resources for this mode of care delivery, taking particular care to articulate tailored outreach for vulnerable segments of their communities. Extreme social inequality, characteristics of many US Covid-19 “hotspots” (Maroko et al., 2020), creates considerable challenges in addressing access to care (see Cockerham et al., 2017, for a comprehensive review), and in the long run, this inequality will need to be addressed to minimize the longterm harmful sequelae from this pandemic (Auerbach & Miller, 2020).
Clinical Impact Statement:
These findings on stress exposure and distress of Americans early in the pandemic highlight psychosocial resources and coping strategies potentially useful to interventionists seeking to mitigate the immediate adverse mental health effects of the pandemic and to potentially dampen long-term sequelae. This information may also be useful to policymakers preparing for the demands of increased mental health services in the months and years ahead.
Funded by NIAAA:
1R34AA027455
References
- Aldwin CM (2007). Stress, coping, and development (2nd ed.). New York: Guilford Press. [Google Scholar]
- An Y, Yuan G, Zhang N, Xu W, Liu Z, & Zhou F (2018). Longitudinal cross-lagged relationships between mindfulness, posttraumatic stress symptoms, and posttraumatic growth in adolescents following the Yancheng tornado in China. Psychiatry Research, 266, 334–340. doi: 10.1016/j.psychres.2018.03.034 [DOI] [PubMed] [Google Scholar]
- Arditte KA, Çek D, Shaw AM, & Timpano KR (2016). The importance of assessing clinical phenomena in Mechanical Turk Research. Psychological Assessment, 28, 684–691. doi: 10.1037/pas0000217 [DOI] [PubMed] [Google Scholar]
- Auerbach J, & Miller BF (2020). COVID-19 Exposes the Cracks in Our Already Fragile Mental Health System. American Journal of Public Health, 110, e1–e2. doi: 10.2105/AJPH.2020.305699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral IA, & Bhagawati KC (2019). Post traumatic stress disorder and coping strategies among adult survivors of earthquake, Nepal. BMC Psychiatry, 19(1), 118. doi: 10.1186/s12888-019-2090-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CJ, Boden JM, Horwood LJ, & Mulder RT (2017). The role of peri-traumatic stress and disruption distress in predicting symptoms of major depression following exposure to a natural disaster. Australian & New Zealand Journal of Psychiatry, 51, 711–718. doi: 10.1177/0004867417691852 [DOI] [PubMed] [Google Scholar]
- Berking M, Wupperman P, Reichardt A, Pejic T, Dippel A, & Znoj H (2008). Emotion regulation skills as a treatment target in psychotherapy. Behaviour Research and Therapy, 46, 1230–1237. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, & Vlahov D (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75, 671–682. doi: 10.1037/0022-006X.75.5.671 [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet A, Weiss DS, Metzler TJ, Best SR, Neylan TC, Rogers C, … & Marmar CR (2001). The Peritraumatic Distress Inventory: A proposed measure of PTSD criterion A2. American Journal of Psychiatry, 158, 1480–1485. doi: 10.1176/appi.ajp.158.9.1480 [DOI] [PubMed] [Google Scholar]
- Carver C (1997). You want to measure coping but your protocol’ too long: Consider the brief cope. International Journal of Behavioral Medicine, 4, 92–100. doi: 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Cénat JM, & Derivois D (2014). Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adult survivors of earthquake in Haiti after 30 months. Journal of Affective Disorders, 159, 111–117. doi: 10.1016/j.jad.2014.02.025 [DOI] [PubMed] [Google Scholar]
- CDC. (2020). Coronavirus (COVID-19): Daily life and coping. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/index.html
- Christensen H, Batterham P, & Calear A (2014). Online interventions for anxiety disorders. Current Opinion in Psychiatry, 27(1), 7–13. [DOI] [PubMed] [Google Scholar]
- Cohen S & Hoberman HM (1983). Positive life events and social supports as buffers of life change stress. Journal of Applied Social Psychology, 13, 99–125. doi: 10.1111/j.1559-1816.1983.tb02325.x [DOI] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, & Hoberman HM (1985). Measuring the functional components of social support. In Sarason IG & Sarason BR (Eds.), Social support: Theory, research, and applications (pp. 73–94). Seattle, WA: Martinus Nijhoff. [Google Scholar]
- Cox CE, Hough CL, Carson SS, White DB, Kahn JM, Olsen MK, … & Porter LS (2018). Effects of a telephone-and web-based coping skills training program compared with an education program for survivors of critical illness and their family members. a randomized clinical trial. American Journal of Respiratory and Critical Care Medicine, 197(1), 66–78. [DOI] [PubMed] [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41, 587–598. doi: 10.1016/j.beth.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Elhai JD, Levine JC, Dvorak RD, & Hall BJ (2016). Fear of missing out, need for touch, anxiety and depression are related to problematic smartphone use. Computers in Human Behavior, 63, 509–516. doi: 10.1016/j.chb.2016.05.079 [DOI] [Google Scholar]
- Feldman G, Hayes A, Kumar S, Greeson J, & Laurenceau J-P (2007). Mindfulness and emotion regulation. Journal of Psychopathology and Behavioral Assessment, 29, 177–190. doi: 10.1007/s10862-006-9035-8 [DOI] [Google Scholar]
- Finkelstein-Fox L, & Park CL (2019). Control-coping goodness-of-fit and chronic illness: A systematic review of the literature. Health Psychology Review, 13, 137–162. doi: 10.1080/17437199.2018.1560229 [DOI] [PubMed] [Google Scholar]
- Finkelstein-Fox L, Park CL, & Riley KE (2018). Mindfulness and emotion regulation: Promoting well-being during the transition to college. Anxiety, Stress, & Coping, 31, 639–653. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM, & Mulder RT (2014). Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry, 71, 1025–1031. [DOI] [PubMed] [Google Scholar]
- Galea S, & Coffey SF (2018). Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: Effects for displaced and nondisplaced residents. Journal of Traumatic Stress, 31, 223–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Merchant R,M, & Lurie N (2020). The mental health consequences of Covid-19 and physical distancing the need for prevention and early intervention. JAMA Internal Medicine. DOI: 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- Heber E, Lehr D, Ebert DD, Berking M, & Riper H (2016). Web-based and mobile stress management intervention for employees: a randomized controlled trial. Journal of Medical Internet Research, 18(1), e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DC, Thom NJ, Stanley EA, Haase L, Simmons AN, Shih PAB, … & Paulus MP (2014). Modifying resilience mechanisms in at-risk individuals: A controlled study of mindfulness training in Marines preparing for deployment. American Journal of Psychiatry, 171, 44–853. doi: 10.1176/appi.ajp.2014.13040502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman E, Xia M, Fosco G, Yaptangco M, Skidmore C, & Crowell S (2016). The difficulties in emotion regulation scale short form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment, 38, 443–455. doi: 10.1007/s10862-015-9529-3 [DOI] [Google Scholar]
- Kees J, Berry C, Burton S, & Sheehan K (2017). An analysis of data quality: Professional panels, student subject pools, and Amazon’s Mechanical Turk. Journal of Advertising: Themed Issue - Methodology in Advertising Research, 46, 141–155. doi: 10.1080/00913367.2016.1269304 [DOI] [Google Scholar]
- Kim HS, & Hodgins DC (2017). Reliability and validity of data obtained from alcohol, cannabis, and gambling populations on Amazon’s Mechanical Turk. Psychology of Addictive Behaviors, 31, 85–94. doi: 10.1037/adb0000219 [DOI] [PubMed] [Google Scholar]
- Kung WW, Liu X, Goldmann E, Huang D, Wang X, Kim K, … & Yang LH (2018). Posttraumatic stress disorder in the short and medium term following the World Trade Center attack among Asian Americans. Journal of Community Psychology, 46, 1075–1091. doi: 10.1002/jcop.22092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, coping and appraisal. New York, NY: Guilford. [Google Scholar]
- Litz BT, Engel CC, Bryant RA, & Papa A (2007). A randomized, controlled proof-of-concept trial of an internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry, 164, 1676–1683. Doi: 10.1176/appi.ajp.2007.06122057 [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33, 335–343. [DOI] [PubMed] [Google Scholar]
- Main A, Zhou Q, Ma Y, Luecken LJ, & Liu X (2011). Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology, 58, 410–423. doi: 10.1037/a0023632 [DOI] [PubMed] [Google Scholar]
- Maroko AR, Nash D, & Pavilonis B (2020). Covid-19 and Inequity: A comparative spatial analysis of New York City and Chicago hot spots. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty EE, Presskreischer R, Han H, & Barry CL (2020). Psychological distress and loneliness reported by us adults in 2018 and April 2020. JAMA, 324(1), 93–94. doi: 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire AP, Gauthier JM, Anderson LM, Hollingsworth DW, Tracy M, Galea S, & Coffey SF (2018). Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms. Journal of Traumatic Stress, 31, 223–233. doi: 10.1002/jts.22270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen K, & Hughes TL (2018). Comparing Amazon’s Mechanical Turk platform to conventional data collection methods in the health and medical research literature. Journal of General Internal Medicine, 33, 533–538. doi: 10.1007/s11606-017-4246-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for PTSD (2020). Covid Coach App. https://www.ptsd.va.gov/appvid/mobile/COVID_coach_app.asp,
- Nitzan-Assayag Y, Aderka IM, & Bernstein A (2015). Dispositional mindfulness in trauma recovery: Prospective relations and mediating mechanisms. Journal of Anxiety Disorders, 36, 25–32. 10.1016/j.janxdis.2015.07.008 [DOI] [PubMed] [Google Scholar]
- Ophir Y, Sisso I, Asterhan C, Tikochinski R, & Reichart R (2020). The Turker blues. Clinical Psychological Science, 8, 65–83. doi: 10.1177/2167702619865973 [DOI] [Google Scholar]
- Park CL & Blake EB (2020). Resilience and recovery following disasters: The meaning making model (pp. 9–25). In Schulenberg SE (Ed.), Disaster mental health and positive psychology. New York, NY: Springer. [Google Scholar]
- Park CL, Riley KE, & Snyder LB (2012). Meaning making coping, making sense, and post-traumatic growth following the 9/11 terrorist attacks. The Journal of Positive Psychology, 7, 198–207. doi: 10.1080/17439760.2012.671347 [DOI] [Google Scholar]
- Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, … & Harrison D (2014). Trajectories of PTSD risk and resilience in World Trade Center responders: An 8-year prospective cohort study. Psychological Medicine, 44, 205–219. [DOI] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, & Xu Y (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic. General Psychiatry, 33, 1–3. doi: 10.1136/gpsych-2020100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, & Becker J (2020). Americans’ Covid-19 stress, coping, and adherence to CDC Guidelines. Journal of General Internal Medicine, 35, 2296–2303. doi: 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Williston SK, & Rollins LG (2015). Mindfulness and emotion regulation. Current Opinion in Psychology, 3, 52–57. [Google Scholar]
- Sheehan KB, & Pittman M (2016). Amazon’s Mechanical Turk for academics: The HIT handbook for social science research. Irvine, CA: Melvin & Leigh. [Google Scholar]
- Sheehan KB (2018). Crowdsourcing research: Data collection with Amazon’s Mechanical Turk. Communication Monographs, 85, 140–156. doi: 10.1080/03637751.2017.1342043 [DOI] [Google Scholar]
- Sinclair SJ, Siefert CJ, Slavin-Mulford JM, Stein MB, Renna M, & Blais MA (2012). Psychometric evaluation and normative data for the Depression, Anxiety, and Stress Scales-21 (DASS-21) in a nonclinical sample of US adults. Evaluation & the Health Professions, 35, 259–279. doi: 10.1177/0163278711424282 [DOI] [PubMed] [Google Scholar]
- Sloan E, Hall K, Moulding R, Bryce S, Mildred H, & Staiger PK (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders. Clinical Psychology Review, 57, 141–163. [DOI] [PubMed] [Google Scholar]
- Sweeny K (2012). Waiting well: Tips for navigating painful uncertainty. Social and Personality Psychology Compass, 6, 258–269. doi: 10.1111/j.1751-9004.2011.00423.x [DOI] [Google Scholar]
- Sweeny K, Rankin K, Cheng X, Hou L, Long F, Meng Y, … Zhang W Flow in the time of COVID-18: Findings from China [submitted manuscript). psyarxiv.com/e3kcw/ [DOI] [PMC free article] [PubMed]
- US Census Bureau. (n.d.). Census regions and divisions of United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
- Victor SE, & Klonsky ED (2016). Validation of a brief version of the Difficulties in Emotion Regulation Scale (DERS-18) in five samples. Journal of Psychopathology and Behavioral Assessment, 38, 582–589. 10.1007/s10862-016-9547-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Maiuro RD, Russo J, & Becker J (1987). Raw versus relative scores in the assessment of coping strategies. Journal of Behavioral Medicine, 10, 1–18. doi: 10.1007/BF00845124 [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, & Ho RC (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1–25 doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters K, Christakis DA, & Wright DR (2018). Are Mechanical Turk worker samples representative of health status and health behaviors in the US?. PloS one, 13(6). doi: 10.1371/journal.pone.0198835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen EK, Gros DF, Price M, Zeigler S, Tuerk PW, Foa EB, & Acierno R (2015). Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: Preliminary results. Journal of Clinical Psychology, 71, 500–512. doi: 10.1002/jclp.22168. [DOI] [PubMed] [Google Scholar]
- Zhang Y, & Ma ZF (2020). Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. International Journal of Environmental Research and Public Health, 17, 1–12 doi: 10.3390/ijerph17072381 [DOI] [PMC free article] [PubMed] [Google Scholar]


