Abstract
Background
Nurses in the frontline of the battle against COVID-19 are highly vulnerable to compassion fatigue (CF), which may affect their mental health, work effectiveness, and patient safety outcomes. However, no studies have investigated nurses' CF in relation to job outcomes and care quality during the pandemic.
Aims
This study aims to examine the mediating role of resilience in the relationship between CF and frontline nurses' job outcomes (job satisfaction and turnover intention) and care quality.
Design
An online, cross-sectional survey containing five self-report scales was used to collect data from 270 frontline nurses in selected hospitals in the Philippines.
Results
Overall, 38.5% of frontline nurses experienced medium to high CF during the second wave of the pandemic. Increased CF was associated with poorer nurse-reported quality of care (β = −0.145, p = 0.019), lower job satisfaction (β = −0.317, p = 0.001), and higher organizational turnover intention (β = 0.301, p = 0.001). Moreover, resilience fully mediated the relationship between CF and quality of care (β = −0.088, p = 0.169), and partially mediated the relationship between CF and job satisfaction (β = −0.259, p = 0.001), and CF fatigue and organizational turnover intention (β = 0.272, p = 0.001).
Conclusion
Frontline nurses are at risk of developing CF during the pandemic. Psychological resilience reduces the negative impact of CF on frontline nurses' job satisfaction, turnover intention, and the quality of care in their assigned unit. Proactive measures to reduce CF should be prioritized by nursing administrators. Resilience-promoting interventions could foster job satisfaction and retention in nurses and, hence, the quality of care delivered in their units.
Keywords: Compassion fatigue, Resilience, Turnover intention, Job satisfaction, Quality of care, Nursing, COVID-19 pandemic
1. Introduction
The coronavirus disease, or COVID-19, originated in China in the later part of 2019 and has created an unprecedented burden for healthcare systems around the world. The pandemic has brought additional stress and psychological burden to healthcare workers, particularly those involved in the direct care and management of coronavirus patients, posing an increased risk for the development of compassion fatigue. Defined as “a state of emotional exhaustion due to the dynamics of a caring relationship with an individual or a group of individuals who have suffered a sudden or severe loss” (Sabo, 2011), compassion fatigue (CF) often occurs as a consequence of persistent exposure to patients' suffering, stressful work conditions, and inadequate utilization of measures to promote self-care (Peters, 2018; Sorenson, Bolick, Wright, & Hamilton, 2017). The global estimate of CF prevalence among nurses during the pre-pandemic period ranged from 22% to 60% (Zhang et al., 2018) and was found to be influenced by myriad factors including personal, work-related, and psycho-social factors (Cavanagh et al., 2020; Ortega-Campos et al., 2020). Age, marital status, education, gender, salary, ethnicity, and overall health condition were identified as personal factors associated with CF. Work-related factors included years of work experience, job rank, job status, work climate, and presence of violence in the workplace; psycho-social factors strongly linked to CF included family support, coping skills, psychological distress, and professional identity (O'Callaghan, Lam, Cant, & Moss, 2020; Xie et al., 2021). Manifestations of CF include decreased energy, reduced ability to empathize, increased hopelessness, and heightened emotional exhaustion (Peters, 2018).
When left unmanaged, CF may have untoward repercussions on nurses' well-being and health, resulting in mental health concerns (e.g., burnout, depression, stress, and anxiety) leading to work impairment (Pérez-García et al., 2021), job dissatisfaction (Kim et al., 2017), and eventual nurse turnover (Wells-English, Giese, & Price, 2019). These conditions could ultimately influence the way nurses provide care, resulting in increased incidence of adverse events, patient errors and missed nursing care, and poorer health service delivery (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c; Peters, 2018). Hence, many healthcare organizations have implemented various efforts to address this issue and to assist healthcare workers (HCWs), including nurses, to effectively deal with the stress that accompanies the pandemic.
Nurses on the frontline against COVID-19 encounter numerous stressors in addition to stressors found in usual circumstances, including increased patient workloads, lack of reliable personal protective equipment (PPEs), additional coronavirus protocols, inadequate preparation related to care of infected patients, and poor working conditions to effectively carry out their duty (Arnetz, Goetz, Arnetz, & Arble, 2020). These conditions, along with heightened fear of being infected or unknowingly infecting their family and friends (Khattak et al., 2021; Labrague and de los Santos, 2021a, Labrague and de los Santos, 2021b), as well as infection control measures (e.g., social distancing, lockdown), could negatively affect nurses' ability to be compassionate and increase their risk of developing CF (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c). Available research has shown that as many as 70% of frontline nurses suffered from moderate to severe CF during the pandemic, with 97% of nurses experiencing at least one symptom of CF (Erkin, Konakçı, & Duran, 2021). A higher rate of CF was mostly observed in nurses assigned to critical care units, emergency care units, and units designated for treating and managing patients with COVID-19 (Ruiz-Fernández et al., 2020), although a significant proportion of nurses from other hospital units were also seen to suffer from CF related to caring for non-COVID-19 patients during the pandemic (Alharbi et al., 2020a).
CF during the pandemic may affect the mental health of frontline nurses, leading to work impairment and reduced capacity to provide quality of care to their patients (Labrague, 2021; Pérez-García et al., 2021). With the continuing battle against COVID-19, along with the increasing number of individuals being infected, the emergence of new coronavirus variants, and seemingly no end in sight for the pandemic, frontline nurses will continue to suffer from CF unless measures are initiated. Considering the costs associated with CF, it is imperative that proactive measures to adequately manage CF be prioritized by hospital and nursing administrators. Harnessing nurses' personal resources, including psychological resilience – defined as a person's ability to rebound from adversities or stress-provoking events – could be an important measure to address CF in this group of nurses.
Resilience has been identified as an essential protective factor against the mental and psychological health effects of traumatic events and adversities including calamities, disaster emergency situations, and outbreaks of infections (Labrague, 2021; Pollock et al., 2020). Pre-pandemic studies consistently associated psychological resilience with sustained health (e.g., mental, psychological, and emotional health) and positive job outcomes (e.g., increased work performance, job engagement, and retention) in nurses despite stressful situations (Cooper et al., 2020; Cooper et al., 2021; Hart et al., 2014). Moreover, during disease outbreaks, including the previous outbreaks of Ebola, SARS, H1NI, and MERS-COV, such personal resources safeguarded nurses' mental and psychological well-being and allowed them to continuously carry out their professional nursing role (Maiorano, Vagni, Giostra, & Pajardi, 2020; Polloch et al., 2020). During the height of the coronavirus crisis, evidence showed that nurses who had adequate levels of resilience better handled the negative impact of the pandemic, resulting in reduced anxiety, post-traumatic stress, emotional exhaustion, and depression (Yörük & Güler, 2021; Zhang et al., 2021). It is therefore not surprising that many healthcare institutions have invested heavily in programs and interventions to harness resilience in healthcare workers serving in the forefront of the pandemic, and hence to improve their overall health and work performance (Adimando, 2018; Dreher, Hughes, Handley, & Tavakoli, 2019).
With regards to CF, a handful of studies showed the efficacy of resilience in reducing fatigue associated with caring for patients (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c; Maiorano et al., 2020). Psychological resilience, along with increased work engagement and positive coping, was attributed to a significant reduction in CF levels among frontline nurses during the early months of the pandemic (Cao & Chen, 2020; Cho & Jung, 2014; Maiorano et al., 2020). Based on this evidence, psychological resilience may also influence the effects of CF on nurses' work outcomes and patient safety outcomes. However, despite these assumptions, the mechanism underlying this relationship remains unexplored. Understanding this mechanism is critically important in the formulation of interventions aimed at supporting the mental health of frontline nurses in order to ensure the delivery of quality, safe, and compassionate care to their patients.
1.1. Theoretical framework
This study was anchored on the Compassion Fatigue Model (CFM; Coetzee & Laschinger, 2018), which conceptualizes lack of resources, inadequate positive feedback, and nurses' reactions to personal distress as drivers of compassion fatigue (Coetzee & Laschinger, 2018). These resources include personal (resilience, coping, self-esteem), organizational (hospital resources, staffing), and energy resources (knowledge, energy, time). According to this model, nurses who are poorly resourced (e.g., lack of resilience, inadequate hospital resources) and lacked empathic focus on the patient are more likely to experience patient's needs as a threat to their resources, resulting in compassion fatigue. Conversely, nurses who are well-resourced and have patient-oriented focus tend not to perceive the patient's needs as a threat, thereby reducing the risk for compassion fatigue (Coetzee & Laschinger, 2018). The current pandemic poses a significant threat to nurses' resources, which could lead to compassion fatigue and subsequently affect their job productivity and the overall delivery of nursing care.
1.2. Hypothesize model
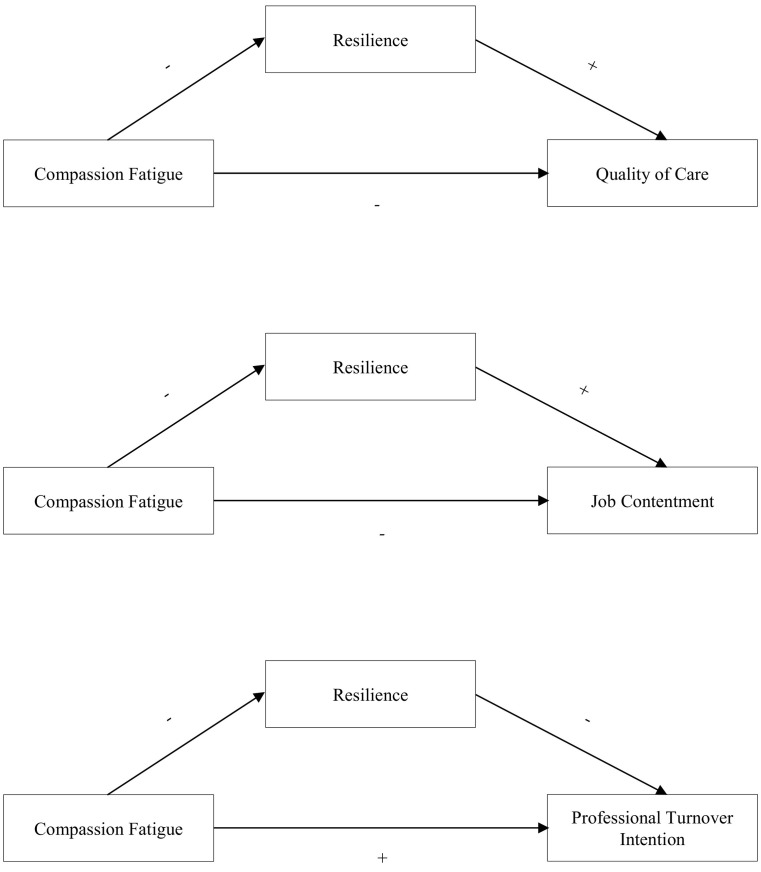
Based on the review of the literature, the following hypotheses were formulated. First, we hypothesized that CF may negatively influence job satisfaction (Hypothesis 1) and quality of care (Hypothesis 2), and positively influence organizational turnover intention (Hypothesis 3). Moreover, we hypothesized that positive coping may mediate the relationship between compassion fatigue CF and job satisfaction (Hypothesis 4), organizational turnover intention (Hypothesis 5), and quality of care (Hypothesis 6). In other words, resilience may reduce the negative effects of CF, resulting in heightened job satisfaction, reduced organizational turnover intention, and increased perceptions of care quality (Fig. 1 ).
Fig. 1.
Hypothesized models.
2. Methods
2.1. Design, samples, and settings
A cross-sectional study using an online survey was conducted in selected hospitals in the Philippines to collect data from nurses who were caring for coronavirus patients. To be eligible for the study, participants were required to be registered and licensed nurses, working in the hospital in the previous six months and directly involved in the care of suspected or infected coronavirus patients. The sample size was calculated using an online calculator (Soper, 2021) for multiple regression. Considering a small effect size, statistical power of 80%, alpha of 0.05, and four initial predictors in the multiple regression, the required sample size was 242. The link to the survey was sent to 300 frontline nurses in the region, of which 270 responded.
2.2. Instrumentation
The 13-item short version of the Compassion Fatigue Scale (CFS) was used to assess CF in frontline nurses in terms of their burnout and secondary trauma. Nurses responded to CFS items using a 10-point Likert scale ranging from 1 (never) to 10 (very frequent). The CFS mean score was calculated by adding all items; a higher mean score reflects a higher degree of CF. The CFS mean scores were divided into three classifications: low CF (1.00–2.33), medium CF (2.34–3.66) and high CF (3.67–5.00) (Barnett & Flores, 2016). The criterion and predictive validity were confirmed in previous studies (Barnett & Flores, 2016). Moreover, previous research reported the internal consistency of the scale within the acceptable level, ranging from 0.85 to 0.91 (Adams, Figley, & Boscarino, 2008).
Frontline nurses' capacity to bounce back from stressful situations brought about by the pandemic was examined using the 4-item Brief Resilient Coping Skills (Smith et al., 2008). Nurses rated items using a five-point Likert scale ranging from 0 (does not describe me at all) to 5 (describes me very well), with a higher composite score representing higher resilience. The criterion validity was established in previous research, while the scales' internal consistency was found to be acceptable (Labrague & de los Santos, 2020).
The Job Satisfaction Scale was used to assess nurses' satisfaction with their present job during the height of the coronavirus crisis (Taunton et al., 2004). Nurses responded to 7-items using a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), with a higher composite score representing a higher level of job satisfaction. The concurrent and criterion validity of this scale were found to be excellent, with acceptable reliability (0.91) (Taunton et al., 2004).
Nurses' intention to leave their current organization was examined by a single-item measure. Using a five-point Likert scale ranging from 0 (strongly disagree) to 5 (strongly agree), nurses responded to the item, “Given the current situation, I am more likely to leave my profession”. Research during the pandemic has established the validity and internal consistency of the scale, with a value of 0.86 (Labrague & de los Santos, 2020).
A single question to measure nurses' judgment and appraisal of the quality of care provided in their assigned unit was used. Nurses appraised the overall nursing care provided in their unit for the previous days using a four-point Likert scale ranging from 0 (poor) to 4 (excellent), with a higher score indicating a higher quality of care delivered. This single-item measure was found to have excellent criterion and predictive validity based on previous research, while the scales' test-retest reliability was found to be within the acceptable range (r = 0.79) (Labrague & de los Santos, 2021b).
The internal consistencies of the multi-item scales were 0.91 for the CFS, 0.85 for the Brief Resilient Coping Skills, and 0.87 for the Job Satisfaction Scale. The test-retest reliabilities of the single-item measures were 0.88 for Organizational Turnover Intention, and 0.86 for Quality of Care.
2.3. Data collection and ethical review
Ethical clearance for the study was provided by the Institutional and Review Taskforce of (omitted for review purposes). Due to the ongoing restrictions regarding in-person collection of research data, a link to the online questionnaire was sent to nurses' official email addresses. The questionnaire was created using Survey Monkey and Google Forms. The link provided a brief description of the study and contained a section to obtain informed consent, whereby nurses indicated whether they agreed or declined to participate in the research. Nurses who agreed to participate in the research were asked to click an ‘I wish to participate’ button, while those who declined to participate were asked to click an ‘I don't wish to participate’ button. To encourage a high response rate, we sent weekly reminders to nurses' email addresses asking them to complete the survey. Nurses were reminded of the survey by sending weekly reminders to their email address or social media accounts. To maintain nurses' confidentiality, no personal identifying information was collected. Data collection took place from 1 November 2020 to 1 December 2020.
2.4. Data analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 23. Prior to conducting analyses, data were inspected for missing values. Three questionnaires with missing values were removed from the data analysis. Descriptive statistics were calculated, including means, standard deviations, frequencies and percentages. To identify relationships and significant differences in key study variables, t-tests, Pearson's r correlations, and ANOVA were used. The mediating effect of resilience was assessed using the 3-step approach described by Baron and Kenny (1986). First, the effects of the independent variable (CF) on the mediator (resilience) were examined. Next, the direct influence of the independent variable (CF) on the outcome variables (nurses' job satisfaction, organizational turnover intention, and quality of care) was calculated. Finally, the direct influence of the mediator (resilience) on the outcome variables (job satisfaction, organizational turnover intention, and quality of care) was examined. The significance of the mediation model was examined using the Sobel Test.
3. Results
The link to the online survey was sent to 300 frontline nurses and 270 completed the survey. The majority of the participants were female (n = 201, 74.5%), not married (n = 153, 56.8%), and held BSN degrees (n = 214, 79.2%). The vast majority held a full-time job role (n = 244, 90.3%), while more than half held staff nurse positions (n = 188, 69.5%). More than half (77.6%) reported the adequacy of the personal protective equipment in their workplace as ‘sufficient’ to ‘very sufficient’, while 52.5% (n = 141) reported the adequacy of the staff as ‘sufficient’ to ‘very sufficient’ (Table 1 ). Pearson's r coefficients identified negative correlations between CF and nurses' age (r = −0.156, p = 0.012) and years of nursing experience (r = −0.170, p = 0.006).
Table 1.
Nurse characteristics (n = 270).
| Variables | Category | n | % | Mean | SD | Test statistic | p value |
|---|---|---|---|---|---|---|---|
| Age | 34.861 | 8.832 | −0.156 | 0.012 | |||
| Years of experience in nursing | 10.671 | 7.532 | −0.170 | 0.006 | |||
| Years of experience in the organization | 6.065 | 5.580 | −0.081 | 0.193 | |||
| Gender | Male | 69 | 25.5 | 2.154 | 0.958 | −0.576 | 0.566 |
| Female | 201 | 74.5 | 2.233 | 0.988 | |||
| Marital status | Married | 117 | 43.2 | 2.079 | 0.992 | −1.923 | 0.056 |
| Unmarried | 153 | 56.8 | 2.315 | 0.960 | |||
| Education | BSN | 214 | 79.2 | 2.179 | 0.958 | −1.029 | 0.307 |
| MSN | 56 | 20.8 | 2.342 | 1.054 | |||
| Job status | Fulltime | 244 | 90.3 | 2.212 | 0.956 | −0.038 | 0.970 |
| Part time | 26 | 9.7 | 2.222 | 1.199 | |||
| Job role | Staff nurse | 188 | 69.5 | 2.215 | 0.932 | 0.047 | 0.963 |
| Nurse manager | 82 | 30.5 | 2.208 | 1.086 | |||
| Facility size | Small | 94 | 34.7 | 2.386 | 1.077 | 2.497 | 0.084 |
| Medium | 77 | 28.6 | 2.052 | 0.845 | |||
| Large | 99 | 36.7 | 2.175 | 0.964 | |||
| Attendance in COVID-19 related trainings | Yes | 144 | 53.3 | 2.193 | 0.985 | −0.352 | 0.725 |
| No | 126 | 46.7 | 2.236 | 0.976 | |||
| Vaccination status | Vaccinated | 211 | 78.0 | 2.161 | 0.923 | ||
| Not vaccinated | 59 | 22.0 | 2.398 | 1.148 | |||
| Personal protective adequacy | 0 | 0.099 | 0.111 | ||||
| Very insufficient | 11 | 4.2 | |||||
| Insufficient | 49 | 18.1 | |||||
| Sufficient | 120 | 44.4 | |||||
| Very sufficient | 90 | 33.2 | |||||
| Staff adequacy | 0 | −0.121 | 0.051 | ||||
| Very insufficient | 29 | 10.8 | |||||
| Insufficient | 99 | 36.7 | |||||
| Sufficient | 109 | 40.5 | |||||
| Very sufficient | 32 | 12.0 |
The composites scores of the scales were as follows: 2.212 (CFS), 1.93 (organizational turnover intention), 3.505 (job satisfaction), and 3.281 (quality of care). Low CF was reported by 61.4% (n = 159) of frontline nurses, while 28.2% (n = 73) and 10.4% (n = 27) reported medium and high compassion fatigue, respectively. Bivariate analysis identified significant correlations between key variables in expected directions. CF negatively and significantly correlated with quality of care (r = −0.145, p = 0.01), job satisfaction (r = −0.317, p = 001), and positively and significantly correlated with organizational turnover intention (r = 0.301, p = 0.001) (Table 2 ).
Table 2.
Correlations between key study variables.
| Variables | Mean | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Quality of care | 3.282 | 0.654 | 1 | |||
| 2. Job satisfaction | 3.506 | 0.954 | 0.367⁎⁎, ⁎ | 1 | ||
| 3. Turnover intention | 1.931 | 1.065 | −0.128⁎ | −0.0106 | 1 | |
| 4. Compassion fatigue | 2.213 | 0.979 | −0.145⁎ | −0.317⁎⁎ | 0.301⁎⁎ | 1 |
p = 0.001.
p = 0.01.
Using multiple regression, the direct and indirect effects of CF on frontline nurses' job satisfaction, organizational turnover intention, and quality of care were tested (Table 3 ). First, CF was negatively associated with quality of care (β = −0.145, p = 0.019) and job satisfaction (β = −0.317, p = 0.001), and positively associated with turnover intention (β = 0.301, p = 0.001). Next, resilience was positively associated with quality of care (β = 0.217, p = 0.001) and job satisfaction (β = 0.272, p = 0.001), and negatively associated with turnover intention (β = −0.178, p = 0.004). Additionally, resilience fully mediated the relationship between CF and quality of care (β = −0.088, p = 0.169). Further, resilience partially mediated the relationship between (a) CF and job satisfaction (β = −0.259, p = 0.001), and (b) CF and organizational turnover intention (β = 0.272, p = 0.001) (Table 3). The final models are shown in Fig. 2 . In other words, resilience reduced the effects of CF on frontline nurses' job satisfaction, organizational turnover intention, and perceived quality of care.
Table 3.
Mediating effects of resilience on the relationship between pandemic fatigue and nurse outcomes.
| Model | B | SE | β | t | p | 95.0% confidence interval |
|
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| Direct effects | |||||||
| Compassion fatigue → quality of care | −0.097 | 0.041 | −0.145 | −2.353 | 0.019 | −0.178 | −0.016 |
| Compassion fatigue → job satisfaction | −0.309 | 0.058 | −0.317 | −5.362 | 0.001 | −0.422 | −0.195 |
| Compassion fatigue → turnover intention | 0.328 | 0.065 | 0.301 | 5.064 | 0.001 | 0.200 | 0.455 |
| Compassion fatigue → resilience | −0.173 | 0.034 | −0.300 | −5.039 | 0.001 | −0.240 | −0.105 |
| Resilience → quality of care | 0.252 | 0.071 | 0.217 | 3.571 | 0.001 | 0.113 | 0.391 |
| Resilience → job satisfaction | 0.459 | 0.101 | 0.272 | 4.524 | 0.001 | 0.259 | 0.659 |
| Resilience → turnover intention | −0.336 | 0.116 | −0.178 | −2.903 | 0.004 | −0.565 | −0.108 |
| Indirect effects | |||||||
| Compassion fatigue → resilience → quality of care | −0.059 | 0.043 | −0.088 | −1.381 | 0.169 | −0.143 | 0.025 |
| Compassion fatigue → resilience → job satisfaction | −0.252 | 0.059 | −0.259 | −4.251 | 0.001 | −0.369 | −0.135 |
| Compassion fatigue → resilience → turnover intention | 0.296 | 0.068 | 0.272 | 4.379 | 0.001 | 0.163 | 0.429 |
Fig. 2.
Final models.
4. Discussion
Findings of this study supported the hypothesized model and provided further evidence of the validity of the Compassion Fatigue Model, which identifies resilience as a personal resource, to reduce the negative effects of compassion fatigue on frontline nurses' job outcomes and care quality.
Prior to the pandemic, the prevalence of CF in nurses ranged from 22% to 60% (Ortega-Campos et al., 2020; Xie et al., 2021), while during the initial surge of the coronavirus crisis, the prevalence reached 70% (Erkin et al., 2021). In the current study, 38.6% of frontline nurses experienced medium to high CF. This rate was lower relative to earlier studies involving physicians and nurses in Spain in which 60.5% of HCWs experienced high levels of compassion fatigue (Ruiz-Fernández et al., 2020). Meanwhile, in a study conducted in Turkey (Erkin et al., 2021), about 70% of nurses reported experiencing high to severe CF. It is worth noting that in the current study, data was collected in selected cities of the country with comparably lower rates of COVID-19 cases, while the studies in Spain and Turkey were conducted in cities with high numbers of cases. This could possibly explain the lower prevalence of CF in our sample. Despite the lower percentage of frontline nurses in the present study experiencing CF in comparison to previous studies (Erkin et al., 2021; Ruiz-Fernández et al., 2020), such a result represents an issue that requires prompt action from nursing administrators. With the number of COVID-19 cases increasing daily, along with the emergence of new coronavirus variants, the number of nurses experiencing CF may continue to grow. Unless herd immunity is achieved or the majority of the population is vaccinated, frontline nurses likely will continue to suffer significant levels of CF as a result of caring for patients and witnessing patient suffering and death due to coronavirus disease. As such, it is imperative that proactive resilience measures be in place to adequately support and safeguard the mental and psychological well-being of nurses.
Additionally, our study found that job satisfaction was moderate to high while organizational turnover intention was low, suggesting that despite CF, nurses were still able to find satisfaction in their jobs, resulting in lower turnover intention. Such a result differs from earlier studies in the local (Labrague & de los Santos, 2020) and international (Irshad, Khattak, Hassan, Majeed, & Bashir, 2020; Zhang et al., 2021) context, in which nurses reported job dissatisfaction and increased levels of organizational and professional turnover intention due to increased fear of the coronavirus disease. Our data collection took place during the months when COVID-19 cases were under control and positive rates were declining due to stringent implementation of infection-control measures (e.g., stay-at-home orders, social distancing), which may explain our finding of a higher job satisfaction level and a lower level of organizational turnover intention. By contrast, previous studies (Irshad et al., 2020; Labrague & de los Santos, 2020; Zhang et al., 2021) were conducted during the earlier surge of the pandemic. At that time, less information was available regarding effective containment and prevention measures, and the best protocols to manage suspected and infected patients were still unknown; hence, nurses were apprehensive and fearful, resulting in higher job dissatisfaction and increased intention to leave their work.
Bivariate analyses found significant negative correlations between CF and nurses' age and years of work experience. As nurses' age and years of work experience increased, their risk of experiencing CF decreased. This result supports findings from a vast number of studies during the pre-pandemic period in which nurses' age and years of nursing experience were strongly linked to CF (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c; Sacco, Ciurzynski, Harvey, & Ingersoll, 2015; Xie et al., 2021). For instance, an integrative review by Alharbi et al. (2019) found that younger nurses experienced a higher level of CF than older nurses, while cross-sectional studies in China, Korea, the US, and Saudi Arabia identified age and work experience as important risk factors for CF (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c; Sacco et al., 2015; Xie et al., 2021). A few possible explanations for these findings are presented here. First, younger nurses have less experience in dealing with different stressors and may have less mature problem-solving and decision-making skills (Saintsing, Gibson, & Pennington, 2011), which are vital when handling patient issues and caring for patients with complex nursing care needs such as COVID-19 patients. Second, younger nurses may lack confidence or self-efficacy, adaptive coping skills, and work experience (García-Martín et al., 2021) to adequately manage the numerous challenges posed by the pandemic. With the ongoing pandemic, it is essential that these groups of nurses are provided adequate support through theory-driven measures to prevent or reduce the consequences of CF.
Multiple regression analyses showed that a higher score on the CFS was associated with decreased job satisfaction, increased organizational turnover intention, and poorer quality of care. This result supported Hypotheses 1, 2, and 3, and suggests that experiencing a higher level of CF during the COVID-19 pandemic may adversely influence frontline nurses' work satisfaction and could provoke them to leave their job. Based on our review of the literature, this study was the first during the pandemic to identify such a pattern of relationships. While we could not locate similar studies during the pandemic, this result is in agreement with reports prior to the pandemic, which established a strong association between CF, work satisfaction, and nurses' intent to leave their jobs (Pérez-García et al., 2021). For example, in China, job engagement and CF explained nurses' decision to leave their current workplace (Cao & Chen, 2020), while in the US, compassion satisfaction and CF were both associated with increased turnover intention among hospital nurses (Wells-English et al., 2019). A similar finding was observed in Korea, in which increased turnover intention was seen in nurses who experienced medium to high levels of CF (Pang, Dan, Jung, Bae, & Kim, 2020). With the ongoing shortage of experienced nurses in the country, along with the increasing number of nurses leaving the country, this result underscores the importance of proactive measures to address CF in frontline nurses to enhance their job satisfaction and improve their retention. Moreover, this study identified that a higher level of CF in nurses could adversely affect the delivery and quality of nursing care provided in their assigned unit. This result supported earlier studies, which linked increased CF with negative patient outcomes, including increased pressure sores, medication administration errors, and patient falls; reduced patient satisfaction; and lower ratings of quality of care (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c).
The key finding of this study was that resilience mediated the relationship between CF and job satisfaction, organizational turnover intention, and nurse-reported quality of care. This result supported Hypotheses 4, 5, and 6. In other words, resilience reduced the negative effect of CF on frontline nurses' job satisfaction and turnover intention, confirming its protective role against various mental and psychological consequences of stress-provoking events including disasters and disease outbreaks (Labrague, 2021). This finding accords with previous studies that identified adequate resilience along with work engagement as a strong precursor of decreased CF among frontline nurses (Cao & Chen, 2020; Cho & Jung, 2014) across different specializations, including those in critical care units, burn wards, and emergency departments (Alharbi et al., 2020a, Alharbi et al., 2020b, Alharbi et al., 2020c; Jo, Na, & Jung, 2020; Tseng, Shih, Shen, Ho, & Wu, 2018). Similarly, in a study involving medical and emergency health personnel in Italy (Maiorano et al., 2020), personal resources including coping, resilience, and hardiness were found to yield protective effects against the impact of the pandemic by reducing CF levels. This result provided additional support to mounting evidence during the pandemic that psychological resilience plays a role in safeguarding nurses' mental health against undesirable consequences of the crisis including stress, anxiety, PTSD, depression, emotional exhaustion, mental fatigue, and sleep disturbance (Labrague & de los Santos, 2020; Yörük & Güler, 2021). In a recent systematic review by Labrague (2021), psychological resilience was found to be imperative in supporting the mental health and psychological well-being of healthcare personnel during the coronavirus outbreak; such well-being is essential to sustain work performance. Moreover, this result of this study further supported an earlier study in the local context (Labrague and de los Santos, 2021a, Labrague and de los Santos, 2021b), in which resilient Filipino nurses were found to have higher levels of job satisfaction and lower organizational turnover intention than nurses with lower levels of resilience. With the increasing number of nurses who are becoming dissatisfied with their job (Irshad et al., 2020) as well as the increasing number of nurses turning away from the bedside (Zhang et al., 2021) during the pandemic due to the increased threats and fear of the virus, harnessing resilience in nurses could be a potential institutional strategy to increase retention of frontline nurses.
Finally, resilience had a full mediating effect on the relationship between CF and nurse-assessed quality of care. This result suggests that fostering resilience in nurses may have a favourable effect on the quality of care provided in their assigned unit. This result was expected since individuals with adequate resilience are able to manage their stress, emotional exhaustion, and depression (Roberts et al., 2021), which are vital for the sustenance of their clinical performance and care provision. Evidence during the pre-pandemic period strongly associated personal resilience with higher patient satisfaction, positive care quality ratings, and lower incidence of patient complications (Rangachari & Woods, 2020). However, despite the importance of resilience in reducing the negative effects of CF, it is worth noting that the obtained mean score in the resilience measure was within the marginal level, highlighting the need for measures to further develop resilience in frontline nurses.
4.1. Limitations of the study
Despite their importance, these study findings should be interpreted with caution given a few limitations. Because the study used a cross-sectional descriptive design, establishing causal relationships may not be possible. Second, respondents were from a single region in the country; hence, results cannot be generalized. Further, the partial mediating effect of resilience on the relationships between CP and job satisfaction and turnover intention suggests that other factors might not have been accounted for. Future research should investigate measures to reduce the risk of and consequences of CF in frontline nurses.
4.2. Implications of the study
CF is a serious health concern during the pandemic that necessitates proactive measures to reduce its negative impact on frontline nurses' job outcomes and patient safety outcomes. As a complex health issue, CF could effectively be addressed by a wide range of interventions including educational programs (Adimando, 2018), self-care skills capacity building (Dreher et al., 2019), mindfulness (Duarte & Pinto-Gouveia, 2016), and compassion skills programmes (Kim et al., 2017). Additionally, brief mindful self-care and resiliency interventions consisting of an educational workshop and a three-week mindfulness practice session were seen to enhance compassion satisfaction and nurses' quality of life, while reducing compassion fatigue (Slatyer, Craigie, Heritage, Davis, & Rees, 2018).
The study findings highlight the importance of implementing resilience-promoting interventions to reduce the impact of CF, foster job satisfaction and retention in nurses, and improve the quality of care delivered in their assigned units. Cognitive framing, mindfulness-based stress therapy, and hardiness training have all been found to foster psychological resilience in nurses (Dong et al., 2020; Huffman et al., 2021). With the current restrictions regarding in-person contact, resilience interventions delivered virtually, including cognitive behavioural therapy, online resilience webinars and workshop, and an interprofessional web-based debriefing intervention (Weiner et al., 2020; Azizoddin, Vella Gray, Dundin, & Szyld, 2020) were shown to harness nurses' resilience and sustain their mental health. Resilience in frontline nurses can be best supported by adequate organizational support and supportive leadership, including the implementation of a resilient work environment, adequate patient-nurse ratio, flexible work schedule, adequate supplies and equipment (e.g., PPEs), up-to-date information regarding the virus, and mental health resources.
5. Conclusion
This study was the first to report the consequences of CF in frontline nurses during the pandemic in terms of job outcome and quality of care, therefore contributing new knowledge to this vital area of research. In accordance with available studies, this study found that the pandemic has contributed to CF among frontline nurses in the Philippines, which has adversely affected their work outcomes as well as the quality of care provided in their respective units. Moreover, psychological resilience was identified as a protective factor against the adverse impact of CF, resulting in higher job satisfaction, increased retention, and a higher perception of quality of nursing care. Implementing interventions to reduce compassion fatigue and harness psychological resilience in nurses should be prioritized by hospital and nursing administrators.
Ethical statement
Ethical approval of this research was granted by the Institutional Research Ethics Committee of Samar State University (irerc ea-001-e).
Funding source
This study was not funded.
CRediT authorship contribution statement
Leodoro Labrague: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Janet Alexis de los Santos: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing.
Declaration of competing interest
All authors declare no conflict of interest.
References
- Adams R.E., Figley C.R., Boscarino J.A. The compassion fatigue scale: Its use with social workers following urban disaster. Research on Social Work Practice. 2008;18(3):238–250. doi: 10.1177/1049731507310190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adimando A. Preventing and alleviating compassion fatigue through self-care: An educational workshop for nurses. Journal of Holistic Nursing. 2018;36(4):304–317. doi: 10.1177/0898010117721581. [DOI] [PubMed] [Google Scholar]
- Alharbi J., Jackson D., Usher K. 2020. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alharbi J., Jackson D., Usher K. Personal characteristics, coping strategies, and resilience impact on compassion fatigue in critical care nurses: A cross-sectional study. Nursing & Health Sciences. 2020;22(1):20–27. doi: 10.1111/nhs.12650. [DOI] [PubMed] [Google Scholar]
- Alharbi J., Jackson D., Usher K. Compassion fatigue in critical care nurses and its impact on nurse-sensitive indicators in Saudi Arabian hospitals. Australian Critical Care. 2020;33(6):553–559. doi: 10.1016/j.aucc.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Arnetz J.E., Goetz C.M., Arnetz B.B., Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: Qualitative analysis of survey responses. International Journal of Environmental Research and Public Health. 2020;17(21):8126. doi: 10.3390/ijerph17218126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azizoddin D.R., Vella Gray K., Dundin A., Szyld D. Bolstering clinician resilience through an interprofessional, web-based nightly debriefing program for emergency departments during the COVID-19 pandemic. Journal of Interprofessional Care. 2020;34(5):711–715. doi: 10.1080/13561820.2020.1813697. [DOI] [PubMed] [Google Scholar]
- Barnett M.D., Flores J. Narcissus, exhausted: Self-compassion mediates the relationship between narcissism and school burnout. Personality and Individual Differences. 2016;97:102–108. [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Cao X., Chen L. The impact of empathy on work engagement in hemodialysis nurses: The mediating role of resilience. Japan Journal of Nursing Science. 2020;17(1) doi: 10.1111/jjns.12284. [DOI] [PubMed] [Google Scholar]
- Cavanagh N., Cockett G., Heinrich C., Doig L., Fiest K., Guichon J.R.…Doig C.J. Compassion fatigue in healthcare providers: A systematic review and meta-analysis. Nursing Ethics. 2020;27(3):639–665. doi: 10.1177/0969733019889400. [DOI] [PubMed] [Google Scholar]
- Cho H.J., Jung M.S. Effect of empathy, resilience, self-care on compassion fatigue in oncology nurses. Journal of Korean Academy of Nursing Administration. 2014;20(4):373–382. [Google Scholar]
- Coetzee S.K., Laschinger H.K. Toward a comprehensive, theoretical model of compassion fatigue: An integrative literature review. Nursing & Health Sciences. 2018;20(1):4–15. doi: 10.1111/nhs.12387. [DOI] [PubMed] [Google Scholar]
- Cooper A.L., Brown J.A., Rees C.S., Leslie G.D. Nurse resilience: A concept analysis. International Journal of Mental Health Nursing. 2020;29(4):553–575. doi: 10.1111/inm.12721. [DOI] [PubMed] [Google Scholar]
- Cooper A.L., Brown J.A., Leslie G.D. Nurse resilience for clinical practice: An integrative review. Journal of Advanced Nursing. 2021;77(6):2623–2640. doi: 10.1111/jan.14763. [DOI] [PubMed] [Google Scholar]
- Dong Z.Q., Ma J., Hao Y.N., Shen X.L., Liu F., Gao Y., Zhang L. The social psychological impact of the COVID-19 pan- demic on medical staff in China: A cross-sectional study. European Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreher M.M., Hughes R.G., Handley P.A., Tavakoli A.S. Improving retention among certified nursing assistants through compassion fatigue awareness and self-care skills education. Journal of Holistic Nursing. 2019;37(3):296–308. doi: 10.1177/0898010119834180. [DOI] [PubMed] [Google Scholar]
- Duarte J., Pinto-Gouveia J. Effectiveness of a mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: A non-randomized study. International Journal of Nursing Studies. 2016;64:98–107. doi: 10.1016/j.ijnurstu.2016.10.002. [DOI] [PubMed] [Google Scholar]
- Erkin Ö., Konakçı G., Duran S. Secondary traumatic stress in nurses working with patients with suspected/confirmed COVID-19 in Turkey. Perspectives in Psychiatric Care. 2021 doi: 10.1111/ppc.12733. [DOI] [PubMed] [Google Scholar]
- García-Martín M., Roman P., Rodriguez-Arrastia M., Diaz-Cortes M.D.M., Soriano-Martin P.J., Ropero-Padilla C. Novice nurse’s transitioning to emergency nurse during COVID-19 pandemic: A qualitative study. Journal of Nursing Management. 2021;29(2):258–267. doi: 10.1111/jonm.13148. [DOI] [PubMed] [Google Scholar]
- Hart P.L., Brannan J.D., De Chesnay M. Resilience in nurses: An integrative review. Journal of Nursing Management. 2014;22(6):720–734. doi: 10.1111/j.1365-2834.2012.01485.x. [DOI] [PubMed] [Google Scholar]
- Huffman E.M., Athanasiadis D.I., Anton N.E., Haskett L.A., Doster D.L., Stefanidis D., Lee N.K. How resilient is your team? Exploring healthcare providers’ well-being during the COVID-19 pandemic. The American Journal of Surgery. 2021;221(2):277–284. doi: 10.1016/j.amjsurg.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irshad M., Khattak S.A., Hassan M.M., Majeed M., Bashir S. How perceived threat of Covid-19 causes turnover intention among Pakistani nurses: A moderation and mediation analysis. International Journal of Mental Health Nursing. 2020 doi: 10.1111/inm.12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo M., Na H., Jung Y.E. Mediation effects of compassion satisfaction and compassion fatigue in the relationships between resilience and anxiety or depression among hospice volunteers. Journal of Hospice & Palliative Nursing. 2020;22(3):246–253. doi: 10.1097/NJH.0000000000000640. [DOI] [PubMed] [Google Scholar]
- Khattak S.R., Saeed I., Rehman S.U., Fayaz M. Impact of fear of COVID-19 pandemic on the mental health of nurses in Pakistan. Journal of Loss and Trauma. 2021;26(5):421–435. [Google Scholar]
- Kim Y.H., Kim S.R., Kim Y.O., Kim J.Y., Kim H.K., Kim H.Y. Influence of type D personality on job stress and job satisfaction in clinical nurses: The mediating effects of compassion fatigue, burnout, and compassion satisfaction. Journal of Advanced Nursing. 2017;73(4):905–916. doi: 10.1111/jan.13177. [DOI] [PubMed] [Google Scholar]
- Labrague L. Psychological resilience, coping behaviors, and social support among healthcare workers during the COVID-19 pandemic: A systematic review of quantitative studies. Journal of Nursing Management. 2021 doi: 10.1111/jonm.13336. Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague L.J., de los Santos J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management. 2020;28(7):1653–1661. doi: 10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague L.J., de los Santos J.A.A. Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nursing. 2021;38(3):382–389. doi: 10.1111/phn.12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague L.J., de los Santos J.A.A. Fear of Covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management. 2021;29(3):395–403. doi: 10.1111/jonm.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiorano T., Vagni M., Giostra V., Pajardi D. COVID-19: Risk factors and protective role of resilience and coping strategies for emergency stress and secondary trauma in medical staff and emergency workers—An online-based inquiry. Sustainability. 2020;12(21):9004. [Google Scholar]
- O’Callaghan E.L., Lam L., Cant R., Moss C. Compassion satisfaction and compassion fatigue in Australian emergency nurses: A descriptive cross-sectional study. International Emergency Nursing. 2020;48:100785. doi: 10.1016/j.ienj.2019.06.008. [DOI] [PubMed] [Google Scholar]
- Ortega-Campos E., Vargas-Román K., Velando-Soriano A., Suleiman-Martos N., Cañadas-de la Fuente G.A., Albendín-García L., Gómez-Urquiza J.L. Compassion fatigue, compassion satisfaction, and burnout in oncology nurses: A systematic review and meta-analysis. Sustainability. 2020;12(1):72. [Google Scholar]
- Pang Y., Dan H., Jung H., Bae N., Kim O. Depressive symptoms, professional quality of life and turnover intention in Korean nurses. International Nursing Review. 2020;67(3):387–394. doi: 10.1111/inr.12600. [DOI] [PubMed] [Google Scholar]
- Pérez-García E., Ortega-Galán Á.M., Ibáñez-Masero O., Ramos-Pichardo J.D., Fernández-Leyva A., Ruiz-Fernández M.D. Qualitative study on the causes and consequences of compassion fatigue from the perspective of nurses. International Journal of Mental Health Nursing. 2021;30(2):469–478. doi: 10.1111/inm.12807. [DOI] [PubMed] [Google Scholar]
- Peters E. Compassion fatigue in nursing: A concept analysis. Nursing Forum. 2018;53(4):466–480. doi: 10.1111/nuf.12274. [DOI] [PubMed] [Google Scholar]
- Pollock A., Campbell P., Cheyne J., Cowie J., Davis B., McCallum J.…Maxwell M. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: A mixed methods systematic review. Cochrane Database of Systematic Reviews. 2020 doi: 10.1002/14651858.CD013779. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangachari P., Woods L.J. Preserving organizational resilience, patient safety, and staff retention during COVID-19 requires a holistic consideration of the psychological safety of healthcare workers. International Journal of Environmental Research and Public Health. 2020;17(12):1–12. doi: 10.3390/ijerph17124267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts N.J., McAloney-Kocaman K., Lippiett K., Ray E., Welch L., Kelly C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respiratory Medicine. 2021;176:106219. doi: 10.1016/j.rmed.2020.106219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Fernández M.D., Ramos-Pichardo J.D., Ibáñez-Masero O., Cabrera-Troya J., Carmona-Rega M.I., Ortega-Galán Á.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Journal of Clinical Nursing. 2020;29(21−22):4321–4330. doi: 10.1111/jocn.15469. [DOI] [PubMed] [Google Scholar]
- Sabo B. Reflecting on the concept of compassion fatigue. Online Journal of Issues in Nursing. 2011;16(1) doi: 10.3912/OJIN.Vol16No01Man01. [DOI] [PubMed] [Google Scholar]
- Sacco T.L., Ciurzynski S.M., Harvey M.E., Ingersoll G.L. Compassion satisfaction and compassion fatigue among critical care nurses. Critical Care Nurse. 2015;35(4):32–42. doi: 10.4037/ccn2015392. [DOI] [PubMed] [Google Scholar]
- Saintsing D., Gibson L.M., Pennington A.W. The novice nurse and clinical decision-making: How to avoid errors. Journal of Nursing Management. 2011;19(3):354–359. doi: 10.1111/j.1365-2834.2011.01248.x. [DOI] [PubMed] [Google Scholar]
- Slatyer S., Craigie M., Heritage B., Davis S., Rees C. Evaluating the effectiveness of a brief mindful self-care and resiliency (MSCR) intervention for nurses: A controlled trial. Mindfulness. 2018;9(2):534–546. [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Soper D. A‐priori sample size calculator for multiple regression. 2021. http://www.danielsoper.com/statcalc/calculator.aspx?id=1 Retrieved from.
- Sorenson C., Bolick B., Wright K., Hamilton R. An evolutionary concept analysis of compassion fatigue. Journal of Nursing Scholarship. 2017;49(5):557–563. doi: 10.1111/jnu.12312. [DOI] [PubMed] [Google Scholar]
- Taunton R.L., Bott M.J., Koehn M.L., Miller P., Rindner E., Pace K.…Dunton N. The NDNQI-adapted index of work satisfaction. Journal of Nursing Measurement. 2004;12(2):101–122. doi: 10.1891/jnum.2004.12.2.101. [DOI] [PubMed] [Google Scholar]
- Tseng H.M., Shih W.M., Shen Y.C., Ho L.H., Wu C.F. Work stress, resilience, and professional quality of life among nurses caring for mass burn casualty patients after Formosa color dust explosion. Journal of Burn Care & Research. 2018;39(5):798–804. doi: 10.1093/jbcr/irx053. [DOI] [PubMed] [Google Scholar]
- Weiner L., Berna F., Nourry N., Severac F., Vidailhet P., Mengin A.C. Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID-19 pandemic: The REduction of STress (REST) study protocol for a randomized controlled trial. Trials. 2020;21(1):1–10. doi: 10.1186/s13063-020-04772-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells-English D., Giese J., Price J. Compassion fatigue and satisfaction: Influence on turnover among oncology nurses at an urban cancer center. Clinical Journal of Oncology Nursing. 2019;23(5):487–493. doi: 10.1188/19.CJON.487-493. [DOI] [PubMed] [Google Scholar]
- Xie W., Wang J., Zhang Y., Zuo M., Kang H., Tang P.…Ma C. The levels, prevalence and related factors of compassion fatigue among oncology nurses: A systematic review and meta-analysis. Journal of Clinical Nursing. 2021;30(5–6):615–632. doi: 10.1111/jocn.15565. [DOI] [PubMed] [Google Scholar]
- Yörük S., Güler D. The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID-19 pandemic: A cross-sectional study in Turkey. Perspectives in Psychiatric Care. 2021;57(1):390–398. doi: 10.1111/ppc.12659. [DOI] [PubMed] [Google Scholar]
- Zhang S.X., Chen J., Jahanshahi A.A., Alvarez-Risco A., Dai H., Li J., Patty-Tito R.M. Succumbing to the COVID-19 pandemic—Healthcare workers not satisfied and intend to leave their jobs. International Journal of Mental Health and Addiction. 2021:1–10. doi: 10.1007/s11469-020-00418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.Y., Han W.L., Qin W., Yin H.X., Zhang C.F., Kong C., Wang Y.L. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. Journal of Nursing Management. 2018;26(7):810–819. doi: 10.1111/jonm.12589. [DOI] [PubMed] [Google Scholar]