Abstract
Background:
Flooding following heavy rains precipitated by hurricanes has been shown to impact the health of people. Earth observations can be used to identify inundation extents for subsequent analysis of health risks associated with flooding at a fine spatio-temporal scale.
Objective:
To evaluate emergency department (ED) visits before, during, and following flooding caused by Hurricane Harvey in 2017 in Texas.
Methods:
A controlled before and after design was employed using 2016–2018 ED visits from flooded and non-flooded census tracts. ED visits between landfall of the hurricane and receding of flood waters were considered within the flood period and post-flood periods extending up to four months were also evaluated. Modified Poisson regression models were used to estimate adjusted rate ratios for total and cause specific ED visits.
Results:
Flooding was associated with increased ED visits for carbon monoxide poisoning, insect bite, dehydration, hypothermia, intestinal infectious diseases, and pregnancy complications. During the month following the flood period, the risk for pregnancy complications and insect bite was still elevated in the flooded tracts.
Significance:
Earth observations coupled with ED visits increase our understanding of the short-term health risks during and following flooding, which can be used to inform preparedness measures to mitigate adverse health outcomes and identify localities with increased health risks during and following flooding events.
Keywords: Exposure Modeling, Epidemiology, Geospatial Analyses, Population Based Studies, Health Studies
Introduction
Floods are the most common natural disaster and accounted for 43% of all-weather related disasters in the world between 1995 and 2015 (1). Between 1995 and 2015, flooding has affected 2.3 billion people causing 157,000 deaths (1). In the United States, flooding caused by heavy rains is a common disaster, and as per the Congressional Budget Office (CBO), the expected annual economic loss due to flood damage is 25 billion dollars (2). Between 2000 and 2017, the portion of land area that experienced extreme one-day precipitation increased by 108% in the United States (3). Mean global surface temperature is expected to increase by 2°C by around 2055, which is predicted to increase tropical cyclone intensities by 5% (4). Also, anthropogenic warming might increase the rainfall rates of tropical cyclones by 10–15% under a 2°C global warming scenario (4). Hence, with more intense storms and increases in rainfall, we are likely to encounter more flooding events in the future.
Flooding affects human health both directly and indirectly. Direct consequences of floods include drowning, injuries, chemical contamination, and hypothermia, which result when people try to escape the danger and during cleanup activities in the recovery period (5,6). Indirectly, the displacement of populations and lack of clean drinking water due to flooding increase the risks of waterborne diseases such as hepatitis A, shigellosis, cholera, cryptosporidiosis, leptospirosis, nonspecific diarrhea, poliomyelitis, rotavirus, typhoid, and paratyphoid (5–7). Water insecurity following flooding also can lead to increase in dehydration among children and older adults (8,9). Disruptions in the supply of electricity, the presence of debris, flooding of buildings and stagnation of water both during and following floods can lead to increases in vector-borne and rodent-borne disease transmission, carbon monoxide (CO) poisoning, hypothermia, mold allergies and respiratory illness (5,6). The lack of access to health services also leads to worsening of chronic health conditions such as diabetes (7). Flooding has also been associated with long-term health impacts such as disability and mental health issues such as PTSD, depression, and anxiety (5,6).
Texas has faced major flooding events following heavy rainfall precipitated by hurricanes and tropical storms. Hurricane Harvey is one such hurricane that brought historic rainfall and caused catastrophic flooding in 2017 (10). Hurricane Harvey made landfall as a Category 4 hurricane on San José Island, Texas on August 26, 2017 (10). It caused 125 billion U.S. dollars in damage, which made it the second most costly hurricane in United States history (10). Historic rainfall of 100 cm was recorded in some counties of Texas(10) which caused significant flooding that displaced over 30,000 people, damaged over 200,000 homes (11) and resulted in 70 deaths (12). About 300,000 buildings were flooded (10), and over 1,057 square miles of land were inundated in southeastern Texas between the day of landfall and September 4, 2017 (13) . After the landfall of the hurricane, 336,000 customers lost electricity (10), and even after three weeks, a minimum of 3,900 homes were still without electricity, and 19 water systems and 31 waste water systems remained offline (14).
While previous studies have evaluated health outcomes following hurricanes, including Hurricane Harvey (15–18), the association between residential flooding and ED visits has been less studied. To address this gap, this study leverages remote sensing products to understand differences in ED visits of residents in census tracts that experienced flooding versus those that did not experience flooding. We have delineated emergency department (ED) visits from census tracts that experienced flooding compared to those that did not experience flooding during and following Hurricane Harvey using inundation extents generated from satellite observations(13) and flooding duration from United States Geological Survey (USGS) stream gauge measures. ED visits during the flood period and short-term (up to four months) post-flood period are compared to control periods. As remote sensing products are available within days following flooding and ED visits are synchronized to near-real time availability (19), such analysis can help in understanding health risks in flooded communities and would further aid in deployment of medical resources and services during future flooding events to mitigate adverse health outcomes.
Materials and Methods
Study area
The study area comprises 118 counties in Texas covering a total area of 333,964 km2 (Figure 1), which were selected based on the availability of the inundation data from the Dartmouth Flood Observatory, as described below. Sixteen metropolitan statistical areas (MSA) including Dallas, Houston, San Antonio, Austin, and Corpus Christi fall within the study area. There are 2,882 census tracts with a total population of 15.5 million. The mean annual temperature in the study area ranges between 17°C and 24°C, and the mean annual rainfall ranges between 39 and 130 mm. As the study area is closer to the North Atlantic basin, hurricanes or tropical storms are commonly experienced between June and October, predominantly during August and September (20). Starting the day of landfall of Hurricane Harvey through the five consecutive days, some parts of the study area experienced precipitation of over 35 cm. Sixteen USGS stream gauges measured stages higher than the National Weather Service (NWS) flood stage, indicating flooding in the stream, for eight consecutive days following hurricane landfall (Figure 2).
Figure 1:
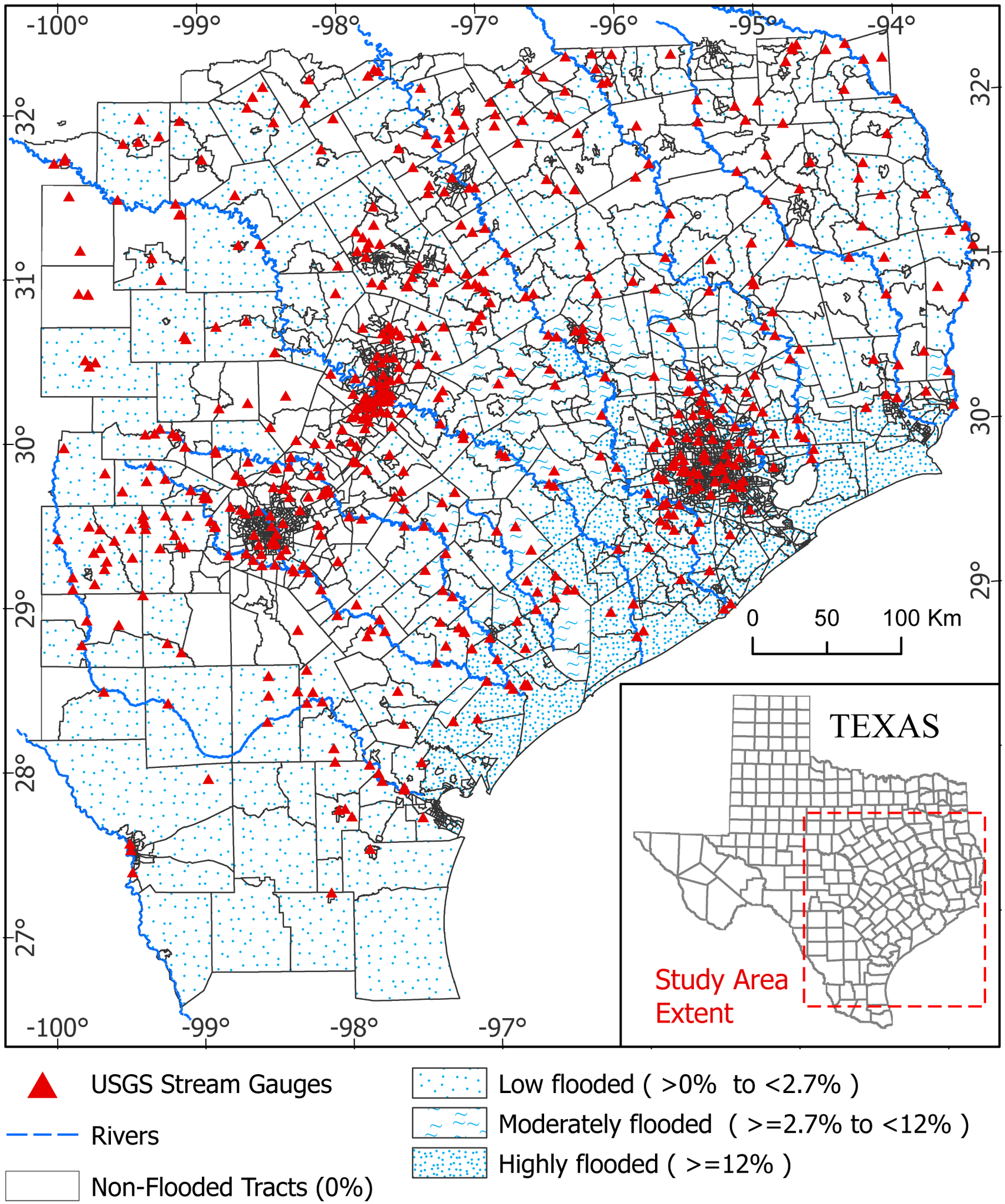
Study area map. Census tracts were classified into four classes based on the percentage of land area inundated which was calculated from the inundation map published by Dartmouth Flood Observatory(13): 0% non-flooded, > 0% to < 2.7% low flooded, >=2.7% to <12% moderately flooded, >=12% highly flooded. The red triangles on map indicate the USGS stream gauges in the study region (United States Geological Survey(USGS), 2020) which were used to determine the number of days flood persisted in the study region.
Figure 2:

Number of ED visits per million people for flooded and non-flooded tracts. The black dashed lines show the number of USGS stream gauges that recorded flooding between August 20, 2017 to September 20, 2017 in the study region. Data Source (32). The solid lines represent the sum of ED visits from the flooded(blue) or non-flooded(orange) census tracts divided by the corresponding sum of population from those tracts multiplied by 1million. The dashed lines are the average of the number of ED visits per million over each period: flood, post-flood 1 and post-flood 2 periods. The dotted lines represent the average number of ED visits per million over the control period(baseline). The average number of ED visits per million in the flooded tracts were lesser than that of non-flooded tracts compared to their corresponding baselines during the flood period.
Data Used
Outcome Data
Total and cause-specific emergency department (ED) visits were used as the outcome variable. Inpatient (IP) and outpatient (OP) ED visit data between July to December of 2016, April to December of 2017, and July to December of 2018 were obtained from the Texas Department of Health and Human Services. Variables that were included in the acquired ED visit data are patient’s sex, age, race, ethnicity, zip code, census tract geocoded from patient’s street address, accuracy of geocoding, status by the end of care, primary International Classification of Diseases (ICD)-10 diagnostic code, and secondary ICD-10 diagnostic codes. ED visits were filtered based on the census tracts in the study area defined above, which resulted in a total of 9,139,648 records. The geocoding code in the filtered records indicated that the geocoding done to assign census tract ID for these records were accurate up to address level for 99% of the records and to census block group level for the remaining records. After removing records in the washout period (i.e., ED visits one week before the landfall of Hurricane Harvey, 1% of total records), there were 9,050,051 records. An additional 0.03% of the records were removed due to missingness in fields or unrealistic age values (values:132,167, and 168), resulting in 9,047,462 records for analysis. The age range of the patients in the final dataset ranged from 0 to 118, and additional demographic information is provided in supplementary Table 1. This study was approved by the Virginia Polytechnic Institute and State University’s Institutional Review Board (IRB Protocol # 18-914) and the Texas Department of State Health Services Institutional Review Board (IRB Protocol # 19-024).
In addition to total ED visits, we focused on 11 cause-specific ED visit types, as well as mortality during service, for further analysis, informed by previous literature: CO poisoning, drowning, dehydration, heat-related illness, hypothermia, insect bite, asthma, chest pain, intestinal infectious diseases, acute respiratory infections (ARI), pregnancy complications (5–8,21–31). A detailed presentation of the previous literature is presented in the discussion section. Mortality events among the ED visits were filtered using the patient’s status as of the end date of service while the rest of the cause-specific ED visits were filtered using the principal and secondary ICD-10 diagnostic codes (Table 1).
Table 1:
Health outcomes related to flooding and their corresponding inclusion and exclusion criteria ICD-10 codes for filtering the Emergency Department (ED) visits.
| Outcome | Inclusion ICD-10 Codes | Exclusion ICD-10 Codes |
|---|---|---|
| Acute Respiratory Infections (ARI) | J0, J1, J2 | |
| Asthma | J45 | |
| Insect Bite | T633, T634, W57 | |
| Chest pain/Palpitations | R002, R079, R0789 | |
| CO Poisoning | T58 | |
| Dehydration | E860, E861, E869 | |
| Drowning | T751, W67, W69, W73, W74 | W65 |
| Heat-related illness | T67, X30 | W92 |
| Hypothermia | T68, X31, T33, T34 | T885, R680 |
| Intestinal infectious diseases | A0 | |
| Pregnancy Complications | O03, O20, O60, O47, O23, O1, O24, O99 |
Exposure Data
Inundation data from the Dartmouth Flood Observatory (13) was used to define the extent of flooding in each census tract by mapping the surface waters after hurricane landfall and then subtracting those areas occupied by permanent water bodies using temporal observations from NASA MODIS, ESA Sentinel 1, ASI Cosmo SkyMed, and Radarsat 2 data. The total area inundated in Texas as of September 4, 2017 was 1,173,010 ha. Using this inundation raster, the tracts were classified into flooded and non-flooded tracts (Figure 1). There were 1,300 flooded tracts and 1,582 non-flooded tracts. The flooded tracts were further classified into three evenly spaced categories (i.e., tertile breaks) based on the proportion of land area flooded within each census tract: low flooded (>0% to <2.7%), moderately flooded (>=2.7% to <12%) and highly flooded (>=12%). These categories of flooding assigned to the census tracts were linked to the ED visits using the patient’s residing census tract information included in each ED visit record.
To find the number of days during which flooding prevailed in the region, we used a similar method to Milojevic et al. (2012)(30), who defined the flood period based on the days when the water level rose above a “normal” level. We collected flood stage data as measured by 597 USGS stream gauges in the study area (Figure 1) (32). The corresponding NWS flood stage for these gauges was used to determine if the stream gauge was flooded. It was observed that, on the day of landfall, three gauges indicated flooding, and this number increased to a maximum of 56 gauges on August 29th. By September 14th all the gauges were below the flood stage. Therefore, the flood period was defined as August 26th to September 13th (Figure 2). To capture potential differences in ED visits during the recovery phase, such as injuries during cleanup activities (5,6) and CO poisoning, a one-month post-flood period was considered following the end of the flood period (September 14th to October 13th). A second post-flood period was also considered as October 14th to December 30th to capture the delayed impacts of flooding. ED visits one week before the landfall of Hurricane Harvey were removed from analysis (i.e., washout period), and the rest of the ED visits covering the days from July 1st to December 31st of 2016, April 1st to August 2017 18th, and July 1st to December 31st of 2018 were assigned to the control period (i.e., baseline).
Study Design and Statistical Analysis
This study follows a controlled before and after design (33) where a control group that was not exposed to floods is considered while examining differences between ED visits in the control versus flooding periods. This enables defining differences in ED visit rates between the flooded and non-flooded tracts during and following the flood period with respect to the baseline average rates in both the flooded and non-flooded tracts (Figure 2). The addition of a control group also helps to control for history bias due to other interventions that occurred at the same time (33). A modified Poisson regression that incorporates sandwich error estimation (34) was implemented using a generalized estimating equation, adding a random effect term for census tract of residence (35). The model’s equation is as follows:
Where πi indicates the probability of patient i for experiencing the cause-specific ED visit (e.g., dehydration), and predictor variables are represented on the right side of the equation (34), with the daily total ED visit counts from each census tract as the offset, such that outcome represents the rate of a cause-specific ED visit, with the total ED visit within the census tract as the denominator. For predictor variables, “flooded” is dichotomous indicating whether the patient’s tract was flooded (0) or not, or multicategory indicating the flood category described above: no flood (reference), low flooded, moderately flooded, or highly flooded. “Period” represents one of the four periods: control period, flood period, post-flood 1 and post-flood 2 (Figure 2). “Sex” in the equation represents the patient sex, 0 for male and 1 for female; “age” is a continuous variable representing the age of the patient, and “race” represents white (reference), African American, or Other, which includes Asian or Pacific Islander, American Indian, Eskimo, and Aleut. “OP” is a dichotomous variable indicating if the visit was inpatient (0) or outpatient (1). Seasonality and weekly trends were modeled by adding year, month, and day of week as categorical predictor variables. The exponent of the estimates for β2 in the equation provides the rate ratio for cause-specific ED visits among the non-flooded census tracts during each exposure period (i.e., flood, post-flood 1, and post-flood 2) compared to the baseline or control period, controlling for individual-level covariates, and yearly, seasonal and weekly time trends. The interaction term (β3) gives the rate ratio for flooded census tracts during each exposure period in comparison to baseline, accounting for changes that occurred in non-flooded tracts between the control and exposure period. This can also be interpreted as the difference between the change in mean rate of ED visits during the flood (or post-flood) periods within the flooded tracts, while accounting for baseline differences in ED visits in flooded and non-flooded tracts.
Results
Among the 9,047,462 ED visits from the 118 counties in the study area, 45% were from census tracts that were flooded following Hurricane Harvey. There were 3,259,155 ED visits during the control period from flooded tracts and 102,698 visits during the flood period, compared to 3,901,224 visits during the control period and 141,724 during the flood period from the unflooded tracts, with additional breakdown of ED visit counts by predictor variables included in Supplementary Tables 2 and 3.
Overall ED visits were decreased slightly in non-flooded tracts during the flood period compared to the baseline period (RR =0.98;CI: 0.97–0.99) (Supplementary Figure 1, Supplementary Table 4). ED visits were more decreased among flooded tracts (Figure 2), amounting to an additional 10% (95% CI: 9–11%) decrease in flooded census tracts, after accounting for the decrease in non-flooded tracts (Figure 3). During the initial month following flooding (i.e., first post-flood period), this additional decrease in flooded census tracts reduced to 3% (2%–4%), and by two months following the flooding period, there were no differences between the flooded and non-flooded census tracts (post-flood 2 RR=1.01 CI: 0.99–1.02).
Figure 3:
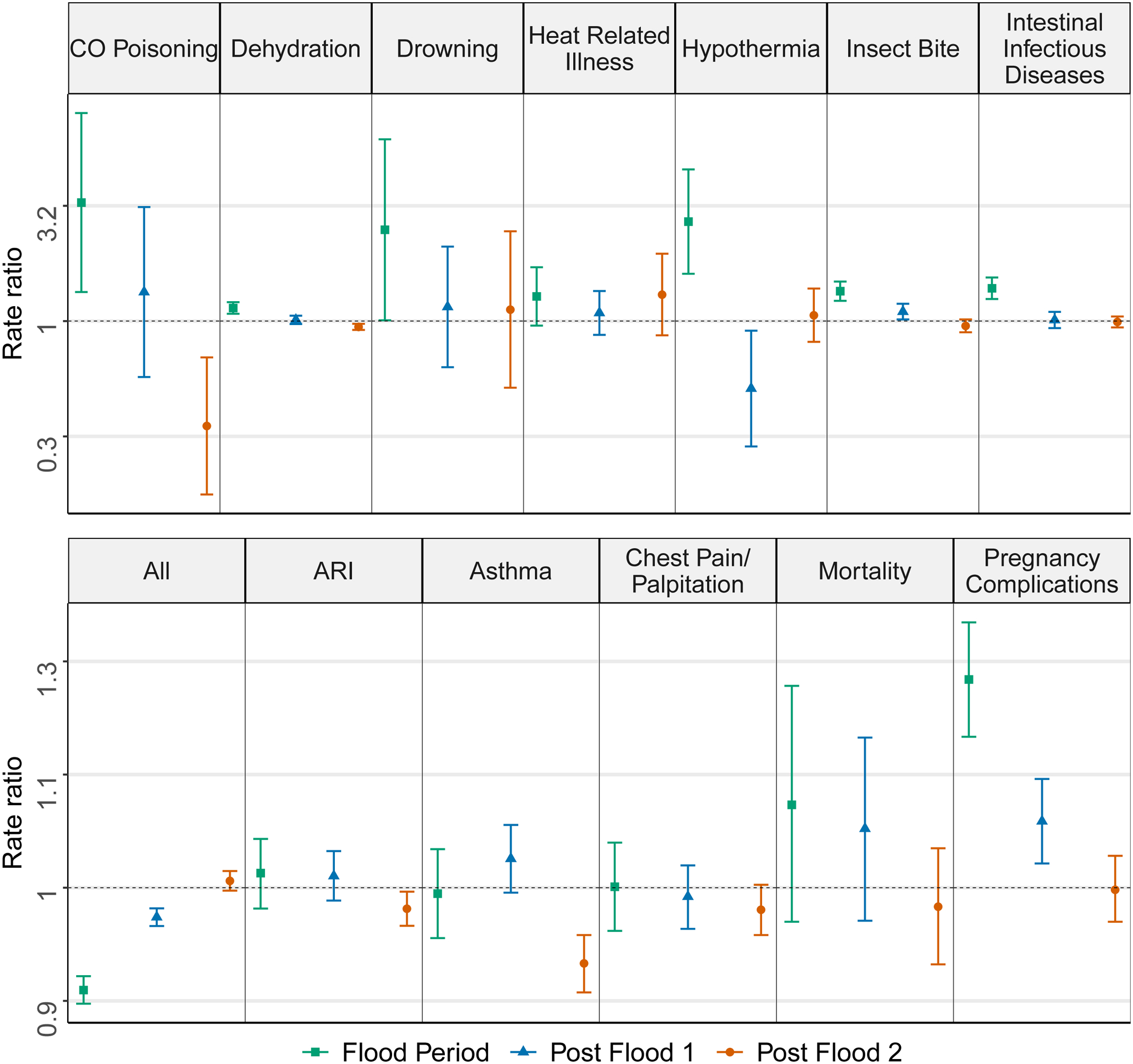
Rate ratio for ED visits related to each outcome for flood period (2017-09-26 to 2017-9-13), post-flood1 (2017-09-14 to 2017-10-13) and post-flood2(2017-10-14 to 2017-12-30). The rate ratios were calculated for flood (square), post-flood1(triangle) and post-flood 2(circle) periods by analyzing the average ED visits from the flooded census tracts with respect to the average ED visits from non-flooded census tracts in each period after controlling for the baseline. The ED visits for each outcome were filtered using ICD codes provided in Table 1. The 95% confidence intervals are shown. The average rate of ED visits related to CO poisoning, dehydration, drowning, hypothermia, insect bite and intestinal infectious diseases were higher in flooded census tracts compared to non-flooded census tracts.
Though total ED visits decreased in the flooded tracts in comparison to the non-flooded tracts during the flood and post-flood 1 periods, some cause-specific ED visits increased (Figure 3). The rate ratio for pregnancy complications and insect bite were 1.24 (1.17–1.31) and 1.35 (1.22–1.48), respectively, during the flood period, both of which gradually reduced to 1.07 (1.02–1.12) and 1.10 (1.02–1.19) during the first post-flood period (Figure 3). During the flood period, flooded tracts experienced a 226% (34% – 698%) increase in ED visits for CO poisoning and 149% (1% – 514%) increase in visits related to drowning compared to non-flooded tracts. The average rate of ED visits for hypothermia was 2.69 (1.6–4.54) times greater in flooded tracts compared to the non-flooded tracts during the flood period. Also, ED visits related to dehydration and intestinal infectious diseases showed a 14% (7%–21%) and 39% (25%–54%) increase in the flooded tracts compared to the non-flooded tracts during this period. To understand if increased dehydration is linked to increased intestinal infectious diseases related ED visits, an additional analysis estimating the rate ratio for ED visits that identified dehydration and intestinal infectious disease was performed. There was a non-significant increase for ED visits coded for both (RR= 1.28; conf: 0.99 – 1.65). During the first post-flood period, ED visits for hypothermia decreased by 49% (9%–71%), and ED visits for asthma decreased by 7% (5%–10%) during the second post-flood period. No significant difference was observed in the average rate of ED visits over any of the three periods between flooded and non-flooded tracts for acute respiratory infections, chest pain/palpitations, heat-related illness, and deaths among ED visits (Figure 3/Supplementary Table 5).
In order to analyze the association between the proportion of land area flooded and the changes in ED visits, a secondary analysis was done using the flooded census tract categories of low, moderate, and high, and their mean ED visits over each study period were compared to the corresponding periods of the non-flooded census tracts. The rate ratio of the ED visits shows a gradual increase from low to medium to highly flooded tracts for insect bite during the flood period (Figure 4). The rate ratio for pregnancy complications was higher in the moderately flooded tracts compared to the low flooded tracts during the flood period.
Figure 4:

Rate ratio for ED visits related to each outcome during the flood period in the low, moderate and highly flooded census tracts compared to the non-flooded census tracts. The rate ratios were calculated for the flood period by analyzing the average ED visits from low flooded (square) , moderately flooded (triangle) and highly flooded(circle) census tracts with respect to the average ED visits from non-flooded census tracts after controlling for the baseline. The 95% confidence intervals are shown. The rate ratio for ED visits related to insect bite and drowning are subsequently higher in each level of flooding compared to the previous level.
Though no difference was observed between the average rate of deaths among ED visits from the flooded tracts as a whole and the non-flooded tracts, after subcategorizing the flooded tracts, deaths among ED visits in the moderately flooded tracts showed a 17% (0.2%–38%) increase compared to the non-flooded tracts during the flood period (Figure 4). Similarly, ED visits for asthma and heat-related illness also showed an increase of 8% (2%–13%) and 45% (9%–93%) respectively in the highly flooded tracts during the first post-flood period, which was not reflected in the analysis comparing flooded versus non-flooded tracts (Figure 5). During the second post-flood period none of the cause specific ED visits were increased among the low, moderate or highly flooded tracts compared to the non-flooded tracts (Supplementary Figure 2). Supplementary Tables 6,7, and 8 present the estimated rate ratios of this analysis in tabular form.
Figure 5:

Rate ratio for ED visits related to each outcome during the post-flood1 in low, moderate and highly flooded census tracts compared to the non-flooded census tracts. The rate ratios were calculated for the post-flood1 period by analyzing the average ED visits from low flooded (square), moderately flooded (triangle) and highly flooded(circle) census tracts with respect to the average ED visits from non-flooded census tracts after controlling for the baseline. The 95% confidence intervals are shown. The average rate of ED visits related to asthma was higher in highly flooded census tracts which was not reflected in dichotomous comparison of flooded versus non-flooded (Figure3).
Influence of Area-level Sociodemographic Factors and Post-Flood Period Definition
While models used for estimating the rate ratio of the cause-specific ED visits were adjusted for individual level factors available on the ED visit records, census tract-level factors could also explain some variation in ED visits during and following floods. The Centers for Disease Control and Prevention (CDC) Social Vulnerability Index (SVI) is a percentile rank assigned to census tracts formed using 15 census level social factors that have been described to influence community’s resilience from disaster impacts (36). So, for the sensitivity analysis, the four theme specific indices (socioeconomic status, household composition, race/ethnicity/language, and housing/transportation) of the CDC SVI (36) where added as additional covariates, and SVI adjusted rate ratios along with the magnitude of difference with respect to the SVI unadjusted model were estimated (Supplementary Table 9). The magnitude of difference was calculated as the percentage of change between the SVI adjusted and SVI unadjusted rate ratios and was less than 1.7% for all the rate ratios estimated (total as well as the 11-cause specific ED visits).
It is apparent from the rate graph of overall ED visits (Figure 2) that after the landfall of Hurricane Harvey, the parallel trend of ED visits from flooded and non-flooded tracts were interrupted, with a return to normal visually by October 9th . In order to estimate the rate ratio between flooded and non-flooded tracts between this period where the flood waters retracted and when the ED visits in flooded tracts returned to normal, the first post-flood period definition was altered to cover the time period from September 14th to October 8th, and the analysis was repeated. The rate ratio obtained for the modified post-flood period (Supplementary Table 10) was similar to the previous results except that slight changes were reflected in the rate ratios of insect bite and pregnancy complications during post-flood 1; additionally, the ED visits for asthma reflected a 5% (2%–9%) increase in the flooded tracts during post-flood 1.
Discussion
Our study is one among the very few studies (28,37) that uses satellite data to determine the exposure of populations to flooding and the only study that has used the USGS real time stream gauge data to determine the period of exposure for estimating the health risks associated with flood exposure. Our results suggest that after the landfall of Hurricane Harvey, there was a decrease in ED visits in flooded tracts compared to non-flooded tracts. An overall decrease in ED visits following Hurricane Harvey as well as Hurricane Sandy has been noted in previous studies (38–40). This decrease might be due to evacuation of residents, transport difficulty to health care facilities due to submerged or blocked roads, or closures or reduced capacity of health care facilities due to infrastructure damage or reduced workforce. A study that analyzed the impact of flooding on 66 hospitals in Harris county after the landfall of Hurricane Harvey reported 24% of the hospitals experienced damage due to flooding (41). With respect to acute direct impacts, relative rates of ED visits for drowning and hypothermia increased in flooded tracts compared to non-flooded tracts during the flood period compared to control periods in the present study which was consistent with previous literature on the direct health impacts of flooding (5,42,43). During and following Hurricane Sandy, hypothermia accounted for 4.3% of reported fatalities (42), and increases in hypothermia cases were also reported after Hurricane Floyd (26). During the flood period, the average rate of deaths among ED visits was increased in the moderately flooded tracts compared to the non-flooded tracts. This was contradictory to the results of the study that analyzed the effects of flooding on mortality in England (37), which showed no significant change in deaths within the flooded postcodes up to 44 weeks following the floods. We note that the present analysis only accounts for deaths that occur at a reporting facility after intake through the ED; therefore, we cannot draw conclusions on how total deaths were different during the flooding. Most cases of CO poisoning following natural disasters are acute effects attributed to power outages during which people depend on portable gasoline-powered generators for running appliances (45,46), and neglecting safe operating procedures leads to exposure to CO emitted by these generators. We observed a five-fold increase in ED visits for CO poisoning in highly flooded tracts compared to non-flooded tracts during the flood period following Hurricane Harvey, which is consistent with previous studies that reported increases in CO poisoning following an ice storm (21,22), hurricane (43–45), or flooding (46). In the case of Hurricane Harvey, almost 336,000 customers lost power on the day of landfall (10), which can potentially explain the increase in ED visits related to CO exposure.
Several studies have documented the association between flooding and diarrheal diseases (8,26,47–50). The present analysis suggests a 39% increase in ED visits for intestinal infectious diseases in flooded tracts, and the rate ratio was higher in moderately flooded tracts than in the low flooded tracts. A similar study that used remote sensing data to quantify seasonal flooding in Cambodia and understand the association between flooding and diarrhea showed that the incidence rate ratio for diarrhea increased with increasing flood water area at a lag of one and three months (28). An increase in risk of gastroenteritis has also been shown to be positively associated with depth of flood waters (27). Positive associations between flooding and increase in diarrhea or gastroenteritis or nonspecific intestinal infections was reported following Hurricane Floyd in eastern North Carolina (26,51) and Hurricane Allison in Houston (49). Reasons for increases in intestinal infectious diseases following flooding may include lack of access to clean drinking water and exposure to contaminated flood water. Studies have shown increased fecal indicators, such as Escherichia coli (E. coli) in stagnated floodwaters (52,53). A study conducted in Bolivia after historic floods in 2014 showed that water insecurity was associated with nine times higher odds of diarrhea in adults (8). The same study also showed that the odds of dehydration was higher among children with high water insecurity when compared to the children with low water insecurity. Dehydration following hurricanes might be due to lack of food, water, and access to refrigeration and air conditioning (54,55). In this study, we observed a 14% increase in ED visits for dehydration during the flood period in the flooded tracts compared to non-flooded tracts. Similar results were found post Hurricane Sandy, with a 66% increase in inpatient hospitalizations for dehydration two weeks following the landfall compared to the previous four years (9). Two weeks after Hurricane Katrina’s landfall, displaced people in shelters reported dehydration (55,56).
Exposure to hurricanes has been shown to be associated with pregnancy complications such as spontaneous abortion, premature labor and preterm birth, and increased odds of fetal death (31,57–61). We observed similar results in the present analysis, with ED visits for pregnancy complications increased during the flood and post-flood 1 periods from census tracts that were exposed to flooding. Possible explanations highlighted in various studies regarding pregnancy complications are injuries caused by the impact of the disaster, and mental stress experienced by pregnant individuals due to property damage and long-lasting power outages (31,58,62). The other cause-specific ED visits that share this indirect pathway of mental stress is chest pain/ palpitations and increased incidence of heart palpitations and chest pain following hurricanes or typhoons has been reported previously (29,56). However, we did not find an association between ED visits for chest pain or heart palpitations and flooding in the present study. One potential reason for the dissimilar results might be the difference in exposure metric between the current study and the above studies where the above studies used damage to livelihood and loss of property following the tropical cyclone as the exposure metric.
ED visits for bites from venomous or non-venomous spiders and other arthropods increased during and following the flooding in the flooded tracts compared to the non-flooded tracts. Increased insect bite cases have also been observed following Hurricane Floyd, Hurricane Hugo, Hurricane Marilyn, Hurricane Opal, and Hurricane Katrina (26,63–66). This result is consistent with previous studies showing increased presence and bites from fire ants, wasps, bees, centipedes and Black flies (67). The disruption of insect habitats by flood waters and downed trees, and increased potential exposure time due to clean-up activities could explain this increase (63,66).
Previous studies provide conflicting evidence on whether asthma exacerbation events or acute respiratory illnesses increase during flooding (27,68,69). In the present study, we found a marginal increase in asthma-related ED visits during the first post-flood period only in the highly flooded tracts (RR=1.08). During the second post-flood period, ED visits for asthma were decreased in the flooded tracts (RR=0.93, CI:0.90–0.95). Another study, which analyzed the rate ratio for asthma in 16 typhoon-affected cities located in Korea between 2003 to 2009, showed a similar decrease in outpatient visits (RR = 0.79; 95% confidence, 0.77–0.83) at a six day lag after typhoon and heavy rain affected 7 cities in 2006, however they reported increased outpatient visits for asthma immediately (lag=0) after the impact of the typhoon and heavy rains in one of the 16 cites during 2007 (69). Reacher et al. (2004) (27) showed a threefold increase in worsening of asthma among adults in flooded areas, however, the study cautioned about interpreting the association as they found a trend of declining risk for increasing depth of flooding. The conflicting results across these studies suggests additional research is needed to understand the association between asthma exacerbation events and flooding. Some potential pathways for asthma exacerbation are change in pollen density and indoor mold infestations (70). An Institute of Medicine (IOM) report on health impacts of indoor dampness affirms suggestive evidence for association between dampness and upper respiratory tract symptoms and asthma symptoms in sensitized persons, and suggestive evidence for development of asthma (71). Exposure to molds and dampness among people living in buildings inundated by floods, and increased risk of acute respiratory infections (ARIs) among such residents was documented post Hurricane Katrina and Rita in New Orleans (72). Other studies are inconsistent, with some showing an increase in ARI and respiratory symptoms among populations within flooded areas after one, three (28) and six months (30) following flooding and others showing no significant increase in respiratory illness during (30) and following storms or flooding (73,74). We did not find an increase in ED visits for ARI in the present study, possibly due to the shorter post-flood period analyzed compared to these previous studies.
Overall, the inundation data that was prepared using remote sensing techniques was helpful in understanding the impacts of flooding caused by Hurricane Harvey. As inundation data are readily available within a few days to weeks following flooding (28), they can be used to analyze health outcomes immediately after flooding to identify communities that may have higher risks for certain flood associated health outcomes. One of the limitations of using earth observation products is that the flood maps are created using a mosaic of satellite images collected on different days over different regions. Hence, the flood extent might be underestimated at places where the data were captured days after the flooding event. Flood mapping products that provide daily inundation extent can be used to overcome the underestimation of inundation, but high temporal resolution satellite observed flooding products currently available are at coarser spatial resolution (75).
Isolating the effects of flooding from other effects of hurricanes is difficult. We have attempted to isolate the effects of flooding by accounting for effects in nearby unflooded tracts within our study design, and through our analysis of differences across low, moderate and highly flooded tracts. For example, in Harris County, which was the most affected county, 27% of the census tracts were non-flooded and were surrounded by flooded tracts. These non-flooded tracts received high rainfall and likely similar wind effects of the surrounding census tracts that became flooded; however, on the scale of this study covering 2,882 census tracts, most non-flooded tracts likely wouldn’t have been as impacted by the hurricane, hence our analysis of health impacts across different levels of flooding are important in further teasing out the effects of flooding. A study that defined exposure to tropical cyclones by wind speeds ≥34 knots found increased hospitalizations for respiratory diseases and no significant variation in intestinal infections (76), while the association between flooding and ED visits presented in our study only detected increased ED visits related to intestinal infectious diseases.
Several studies have shown longer term health impacts associated with flooding such as malnutrition among children and PTSD (77,78) as well as delayed increases in acute respiratory infections (30), while this study only addresses ED visit differences up to 4 months post Hurricane Harvey landfall, defining control periods in years before and after to control for overall secular trends. Also, as this analysis is limited to ED visit data, more subtle health outcomes which did not require urgent medical attention, such as diarrhea or dehydration, are likely underrepresented. Additional health conditions were not considered in this study and would likely be underrepresented in ED data include anxiety, depression, and PTSD. Data collected through surveys of residents from flooded and non-flooded census tracts might be helpful to assess more subtle health outcomes. The small number of ED visits related to drowning, CO poisoning, dehydration, and hypothermia add uncertainty to our results for these cause-specific ED visits. As our aim was to characterize the risk of several flood related health outcomes using remotely sensed data as a means for determining flood exposure, an in-depth stratified analysis to determine effect modification by age, sex, race and ethnicity was not completed in the present analysis, but would be important to further characterize potentially vulnerable populations for adverse health outcomes following flooding events.
Using satellite observations as a proxy for determining the exposure to floods that followed the landfall of Hurricane Harvey, this study found an increased risk for drowning, CO poisoning, pregnancy complications, insect bite, intestinal infectious disease, hypothermia, and dehydration among the population in census tracts that were exposed to flooding. Even after the retraction of floods, risks of insect bite and pregnancy complications were elevated in the flooded tracts.
Supplementary Material
Acknowledgements
The authors appreciate Dr. Thomas Pingel, Department of Geography, Virginia Polytechnic Institute and State University for his support in providing computational resources for running our models. Authors are also grateful to Suwei Wang, Department of Population Health Sciences, Virginia Polytechnic Institute and State University for her guidance in implementing the models used in the study.
This study was funded by the National Aeronautics and Space Administration (NASA) Applied Sciences Program Grant #80NSSC18K1594.
Funding
This study was supported by the National Aeronautics and Space Administration (NASA) Applied Sciences Program Grant #80NSSC18K1594.
Footnotes
Conflict of Interest
The authors declare that there is no conflict of interest.
References:
- 1.Centre for Research on the Epidemiology of Disasters (CRED); United Nations Office for Disaster Risk Reduction (UNISDR). The human cost of weather-related disasters 1995–2015 | Environmental Migration Portal [Internet].2015. [cited 2020 Sep 9]. Available from: https://environmentalmigration.iom.int/human-cost-weather-related-disasters-1995-2015
- 2.Congressional Budget Office. Expected Costs of Damage From Hurricane Winds and Storm-Related Flooding [Internet].2019April [cited 2020 Sep 9]. Available from: https://www.cbo.gov/publication/55019
- 3.NOAA. U.S. Climate Extremes Index [Internet]. Vol. 2010, Climate Services and Monitoring Division. 2020. [cited 2020 Sep 27]. Available from: http://www.ncdc.noaa.gov/extremes/cei/ [Google Scholar]
- 4.Knutson T, Camargo SJ, Chan JCL, Emanuel K, Ho CH, Kossin J, et al. Tropical cyclones and climate change assessment part II: Projected response to anthropogenic warming. Bull Am Meteorol Soc [Internet].2020March1 [cited 2020 Sep 9];101(3):E303–22. Available from: 10.1175/BAMS-D-18-0194.1 [DOI] [Google Scholar]
- 5.Du W, Fitzgerald GJ, Clark M, Hou XY. Health impacts of floods. Vol. 25, Prehospital and Disaster Medicine. Cambridge University Press; 2010. p. 265–72. [DOI] [PubMed] [Google Scholar]
- 6.Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F. Global health impacts of floods: Epidemiologic evidence. Epidemiol Rev [Internet].2005July1 [cited 2020 Sep 6];27(1):36–46. Available from: http://www.em-dat. [DOI] [PubMed] [Google Scholar]
- 7.Saulnier DD, Brolin Ribacke K, Von Schreeb J. No Calm after the Storm: A Systematic Review of Human Health Following Flood and Storm Disasters. Vol. 32, Prehospital and Disaster Medicine. Cambridge University Press; 2017. p. 568–79. [DOI] [PubMed] [Google Scholar]
- 8.Rosinger AY. Household water insecurity after a historic flood: Diarrhea and dehydration in the Bolivian Amazon. Soc Sci Med. 2018Jan 1;197:192–202. [DOI] [PubMed] [Google Scholar]
- 9.Swerdel JN, Rhoads GG, Cosgrove NM, Kostis JB. Rates of Hospitalization for Dehydration Following Hurricane Sandy in New Jersey. Disaster Med Public Health Prep [Internet].2016April1 [cited 2020 Sep 7];10(2):188–92. Available from: https://pubmed.ncbi.nlm.nih.gov/26654113/ [DOI] [PubMed] [Google Scholar]
- 10.Blake E, Zelinsky D. National Hurricane center tropical cyclone report: Hurricane Harvey. Natl Hurric Center, Natl Oceanogr Atmos Assoc. 2018; [Google Scholar]
- 11.Office for Coastal Management, National Oceanic and Atmospheric Administration. Fast Facts Texas [Internet].2018. [cited 2020 Sep 9]. Available from: https://coast.noaa.gov/states/texas.html
- 12.Godfroy M, Jonkman SN. Fatalities due to hurricane Harvey (2017) [Internet].4TU Federation. 2017. [cited 2020 Sep 10]. Available from: https://data.4tu.nl/articles/Fatalities_due_to_hurricane_Harvey_2017_/12708032 [Google Scholar]
- 13.Brakenridge GR, Kettner AJ. DFO Flood Event 4510 [Internet].Dartmouth Flood Observatory, University of Colorado, Boulder, Colorado, USA,. 2017. [cited 2020 Sep 11]. Available from: http://floodobservatory.colorado.edu/Events/2017USA4510/2017USA4510.html [Google Scholar]
- 14.Amadeo K Hurricane Harvey Facts, Damage and Costs What Made Harvey So Devastating [Internet].2019. [cited 2020 Sep 11]. Available from: https://www.thebalance.com/hurricane-harvey-facts-damage-costs-4150087
- 15.Flores AB, Collins TW, Grineski SE, Chakraborty J. Disparities in Health Effects and Access to Health Care Among Houston Area Residents After Hurricane Harvey. Public Health Rep [Internet].2020July1 [cited 2021 Feb 19];135(4):511–23. Available from: http://journals.sagepub.com/doi/10.1177/0033354920930133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oluyomi AO, Panthagani K, Sotelo J, Gu X, Armstrong G, Luo DN, et al. Houston hurricane Harvey health (Houston-3H) study: assessment of allergic symptoms and stress after hurricane Harvey flooding. Environ Heal [Internet].2021December19 [cited 2021 Feb 19];20(1):9. Available from: https://ehjournal.biomedcentral.com/articles/10.1186/s12940-021-00694-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow NA, Toda M, Pennington AF, Anassi E, Atmar RL, Cox-Ganser JM, et al. Hurricane-Associated Mold Exposures Among Patients at Risk for Invasive Mold Infections After Hurricane Harvey — Houston, Texas, 2017. MMWR Morb Mortal Wkly Rep [Internet].2019May31 [cited 2021 Apr 26];68(21):469–73. Available from: http://www.cdc.gov/mmwr/volumes/68/wr/mm6821a1.htm?s_cid=mm6821a1_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwartz RM, Tuminello S, Kerath SM, Rios J, Lieberman-Cribbin W, Taioli E. Preliminary assessment of hurricane harvey exposures and mental health impact. Int J Environ Res Public Health [Internet].2018May13 [cited 2021 Feb 19];15(5):974. Available from: www.mdpi.com/journal/ijerph [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gould DW, Walker D, Yoon PW. The Evolution of BioSense: Lessons Learned and Future Directions. Public Health Rep [Internet].2017July1 [cited 2021 Apr 26];132(1):7S–11S. Available from: http://journals.sagepub.com/doi/10.1177/0033354917706954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roth D Texas Hurricane History [Internet].2010. [cited 2020 Sep 11]. Available from: https://www.weather.gov/media/lch/events/txhurricanehistory.pdf
- 21.Lutterloh EC, Iqbal S, Clower JH, Spiller HA, Riggs MA, Sugg TJ, et al. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 2011May1;126(SUPPL. 1):108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daley WR, Smith A, Paz-Argandona E, Malilay J, McGeehin M. An outbreak of carbon monoxide poisoning after a major ice storm in Maine. J Emerg Med. 2000January1;18(1):87–93. [DOI] [PubMed] [Google Scholar]
- 23.Daley WR, Shireley L, Gilmore R. A flood-related outbreak of carbon monoxide poisoning - Grand Forks, North Dakota. J Emerg Med. 2001;21(3):249–53. [DOI] [PubMed] [Google Scholar]
- 24.Dellinger AM, Kachur PS, Sternberg E, Russell J. Risk of Heat-Related Injury to Disaster Relief Workers in a Slow-Onset Flood Disaster. J Occup Environ Med [Internet].1996;38(7). Available from: https://journals.lww.com/joem/Fulltext/1996/07000/Risk_of_Heat_Related_Injury_to_Disaster_Relief.11.aspx [DOI] [PubMed] [Google Scholar]
- 25.Jonkman SN, Maaskant B, Boyd E, Levitan ML. Loss of life caused by the flooding of New Orleans after hurricane Katrina: Analysis of the relationship between flood characteristics and mortality. Risk Anal. 2009May1;29(5):676–98. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC and others). Morbidity and Mortality Associated With Hurricane Floyd --- North Carolina, September--October 1999. MMWR Morb Mortal Wkly Rep [Internet].2000. [cited 2020 Aug 9];49(17):369–72. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4917a3.htm [PubMed] [Google Scholar]
- 27.Reacher M, McKenzie K, Lane C, Nichols T, Kedge I, Iversen A, et al. Health impacts of flooding in Lewes: A comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Commun Dis Public Health. 2004April1;7:39–46. [PubMed] [Google Scholar]
- 28.Saulnier D, Hanson C, Ir P, Mölsted Alvesson H, von Schreeb J. The Effect of Seasonal Floods on Health: Analysis of Six Years of National Health Data and Flood Maps. Int J Environ Res Public Health [Internet].2018April3 [cited 2020 Jun 4];15(4):665. Available from: http://www.mdpi.com/1660-4601/15/4/665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chae E-H, Kim Tong Won, Rhee S-J, Henderson TD. The Impact of Flooding on the Mental Health of Affected People in South Korea. Community Ment Health J [Internet].2005December [cited 2020 Jun 10];41(6):633–45. Available from: http://link.springer.com/10.1007/s10597-005-8845-6 [DOI] [PubMed] [Google Scholar]
- 30.Milojevic A, Armstrong B, Hashizume M, McAllister K, Faruque A, Yunus M, et al. Health effects of flooding in rural Bangladesh. Epidemiology. 2012January;23(1):107–15. [DOI] [PubMed] [Google Scholar]
- 31.Xiao J, Huang M, Zhang W, Rosenblum A, Ma W, Meng X, et al. The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Sci Total Environ. 2019August15;678:755–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.United States Geological Survey(USGS). WaterWatch [Internet]. United States Geological Survey(USGS). 2020. [cited 2020 Nov 9]. Available from: https://waterwatch.usgs.gov/webservices/floodstage?format=csv [Google Scholar]
- 33.Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol [Internet].2018. [cited 2020 Apr 3];47(6):2082–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29982445 [DOI] [PubMed] [Google Scholar]
- 34.Zou G A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am J Epidemiol [Internet].2004April1 [cited 2020 Oct 6];159(7):702–6. Available from: https://academic.oup.com/aje/article/159/7/702/71883 [DOI] [PubMed] [Google Scholar]
- 35.Yelland LN, Salter AB, Ryan P. Performance of the modified poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol [Internet].2011October15 [cited 2020 Oct 6];174(8):984–92. Available from: https://academic.oup.com/aje/article/174/8/984/155441 [DOI] [PubMed] [Google Scholar]
- 36.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A Social Vulnerability Index for Disaster Management. J Homel Secur Emerg Manag [Internet].2011January5 [cited 2019 Nov 6];8(1). Available from: https://www.degruyter.com/document/doi/10.2202/1547-7355.1792/html [Google Scholar]
- 37.Guidry VT, Margolis LH. Unequal respiratory health risk: Using GIS to explore hurricane-related flooding of schools in Eastern North Carolina. Environ Res. 2005July1;98(3):383–9. [DOI] [PubMed] [Google Scholar]
- 38.Weinberger KR, Kulick ER, Boehme AK, Sun S, Dominici F, Wellenius GA. Association Between Hurricane Sandy and Emergency Department Visits In New York City By Age and Cause. Am J Epidemiol [Internet].2021April28 [cited 2021 May 20]; Available from: https://academic.oup.com/aje/advance-article/doi/10.1093/aje/kwab127/6257048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee DC, Smith SW, Carr BG, Doran KM, Portelli I, Grudzen CR, et al. Geographic Distribution of Disaster-Specific Emergency Department Use after Hurricane Sandy in New York City. Disaster Med Public Health Prep [Internet].2016June1 [cited 2021 May 20];10(3):351–61. Available from: https://pubmed.ncbi.nlm.nih.gov/26857616/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chambers KA, Husain I, Chathampally Y, Vierling A, Cardenas-Turanzas M, Cardenas F, et al. Impact of hurricane harvey on healthcare utilization and emergency department operations. West J Emerg Med [Internet].2020. [cited 2021 May 21];21(3):586–94. Available from: /pmc/articles/PMC7234707/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hines E, Reid CE. Hurricane Harvey hospital flood impacts: Accuracy of federal emergency management agency flood hazard areas in Harris County, Texas. Am J Public Health [Internet].2020March11 [cited 2021 May 20];110(4):574–9. Available from: http://ajph.aphapublications.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Diakakis M, Deligiannakis G, Katsetsiadou K, Lekkas E. Hurricane Sandy mortality in the Caribbean and continental North America. Disaster Prev Manag. 2015February2;24(1):132–48. [Google Scholar]
- 43.Chen J-H, Lauper U, Pantea C, Lin S, Chang H-G. Carbon Monoxide Poisoning during Hurricane Sandy in Affected New York State Counties. Online J Public Health Inform. 2015February2;7(1). [Google Scholar]
- 44.Noji E Carbon Monoxide Poisoning from Hurricane-Associated Use of Portable Generators --- Florida, 2004. MMWR Morb Mortal Wkly Rep. 2005July22;54:697. [PubMed] [Google Scholar]
- 45.Van Sickle D, Chertow DS, Schulte JM, Ferdinands JM, Patel PS, Johnson DR, et al. Carbon Monoxide Poisoning in Florida During the 2004 Hurricane Season. Am J Prev Med. 2007April1;32(4):340–6. [DOI] [PubMed] [Google Scholar]
- 46.Daley WR, Shireley L, Gilmore R. A flood-related outbreak of carbon monoxide poisoning - Grand Forks, North Dakota. J Emerg Med. 2001October1;21(3):249–53. [DOI] [PubMed] [Google Scholar]
- 47.DAUDENS-VAYSSE E, Barrau M, Aubert L, Portecop P, Fontanille E, Forgeot C, et al. Short-term health impact assessment after Irma in French islands. Online J Public Health Inform. 2019May30;11(1). [Google Scholar]
- 48.Pradhan EK, West KP, Katz J, LeClerq SC, Khatry SK, Shrestha SR. Risk of flood-related mortality in Nepal. Disasters [Internet].2007March1 [cited 2020 Sep 6];31(1):57–70. Available from: http://doi.wiley.com/10.1111/j.1467-7717.2007.00340.x [DOI] [PubMed] [Google Scholar]
- 49.Waring S, -Kendrick MdesVignes, Arafat R, Reynolds KM, Souza GD, Bishop SA, et al. Tropical Storm Allison Rapid Needs Assessment --- Houston, Texas, June 2001. MMWR Morb Mortal Wkly Rep 2002May3;51(17)365–9. 2002 May 3;MMWR Morb:365–9. [PubMed] [Google Scholar]
- 50.Zhang N, Song D, Zhang J, Liao W, Miao K, Zhong S, et al. The impact of the 2016 flood event in Anhui Province, China on infectious diarrhea disease: An interrupted time-series study. Environ Int [Internet].2019June1 [cited 2020 Apr 7];127:801–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0160412019300406 [DOI] [PubMed] [Google Scholar]
- 51.Setzer C, Domino ME. Medicaid outpatient utilization for waterborne pathogenic illness following Hurricane Floyd. Public Health Rep [Internet].2004. [cited 2020 Sep 7];119(5):472–8. Available from: /pmc/articles/PMC1497662/?report=abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Soller JA, Schoen ME, Bartrand T, Ravenscroft JE, Ashbolt NJ. Estimated human health risks from exposure to recreational waters impacted by human and non-human sources of faecal contamination. Water Res [Internet].2010. [cited 2020 Sep 7];44(16):4674–91. Available from: https://pubmed.ncbi.nlm.nih.gov/20656314/ [DOI] [PubMed] [Google Scholar]
- 53.Yu P, Zaleski A, Li Q, He Y, Mapili K, Pruden A, et al. Elevated Levels of Pathogenic Indicator Bacteria and Antibiotic Resistance Genes after Hurricane Harvey’s Flooding in Houston. Environ Sci Technol Lett [Internet].2018August14 [cited 2019 Nov 5];5(8):481–6. Available from: https://pubs.acs.org/doi/10.1021/acs.estlett.8b00329 [Google Scholar]
- 54.Morris S, Miner M, Rodriguez T, Stancil R, Wiltz-Beckham D, Chorba T. Tuberculosis control activities after hurricane Harvey — Texas, 2017[Internet]. Vol. 66, Morbidity and Mortality Weekly Report. Department of Health and Human Services; 2017. [cited 2020 Jul 16]. p. 1362–3. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5730212/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wilson JF. Health and the environment after hurricane Katrina[Internet]. Vol. 144, Annals of Internal Medicine. American College of Physicians; 2006. [cited 2020 Sep 7]. p. 153–6. Available from: www.kerrn.org [DOI] [PubMed] [Google Scholar]
- 56.Greenough PG, Lappi MD, Hsu EB, Fink S, Hsieh Y-H, Vu A, et al. Burden of Disease and Health Status Among Hurricane Katrina–Displaced Persons in Shelters: A Population-Based Cluster Sample. Ann Emerg Med [Internet].2008April1 [cited 2020 Sep 7];51(4):426–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0196064407004490 [DOI] [PubMed] [Google Scholar]
- 57.Zahran S, Snodgrass JG, Peek L, Weiler S. Maternal Hurricane Exposure and Fetal Distress Risk. Risk Anal. 2010October;30(10):1590–601. [DOI] [PubMed] [Google Scholar]
- 58.Zahran S, Peek L, Snodgrass JG, Weiler S, Hempel L, Zahran S, et al. Abnormal labor outcomes as a function of maternal exposure to a catastrophic hurricane event during pregnancy. lumhs.edu.pk [Internet].2013. [cited 2020 Sep 6];66:61–76. Available from: http://lumhs.edu.pk/jlumhs/Vol11No02/pdfs/v11n2oa06.pdf [Google Scholar]
- 59.Harville EW, Giarratano G, Savage J, Barcelona de Mendoza V, Zotkiewicz TM. Birth Outcomes in a Disaster Recovery Environment: New Orleans Women After Katrina. Matern Child Health J. 2015November1;19(11):2512–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harville EW, Xiong X, Buekens P. Hurricane Katrina and Perinatal Health. Birth [Internet].2009December1 [cited 2020 Sep 6];36(4):325–31. Available from: http://doi.wiley.com/10.1111/j.1523-536X.2009.00360.x [DOI] [PubMed] [Google Scholar]
- 61.Grabich SC, Robinson WR, Engel SM, Konrad Charles E, David, et al. Hurricane Charley Exposure and Hazard of Preterm Delivery, Florida 2004. Matern Child Health J [Internet].2069. [cited 2020 Sep 6];20:2474–82. Available from: http://www.nhc.noaa.gov/dcmi.shtml [DOI] [PubMed] [Google Scholar]
- 62.Mallett LH, Etzel RA. Flooding: what is the impact on pregnancy and child health? Disasters. 2018July1;42(3):432–58. [DOI] [PubMed] [Google Scholar]
- 63.Brewer RD, Morris PD, Cole TB. Hurricane-Related Emergency Department Visits in an Inland Area: An Analysis of the Public Health Impact of Hurricane Hugo in North Carolina. Ann Emerg Med. 1994April1;23(4):731–6. [DOI] [PubMed] [Google Scholar]
- 64.Bourque LB, Siegel JM, Kano M, Wood MM. Weathering the Storm: The Impact of Hurricanes on Physical and Mental Health. Ann Am Acad Pol Soc Sci [Internet].2006March8 [cited 2020 Sep 6];604(1):129–51. Available from: http://journals.sagepub.com/doi/10.1177/0002716205284920 [Google Scholar]
- 65.Centers for Disease Control and Prevention. Surveillance for injuries and illnesses and rapid health-needs assessment following Hurricanes Marilyn and Opal, September-October 1995. MMWR Morb Mortal Wkly Rep. 1996;45(4):81–5. [PubMed] [Google Scholar]
- 66.Faul M, Weller NF, Jones JA. Injuries after hurricane Katrina among Gulf Coast evacuees sheltered in Houston, Texas. J Emerg Nurs. 2011;37(5):460–8. [DOI] [PubMed] [Google Scholar]
- 67.Dayrit JF, Bintanjoyo L, Andersen LK, Davis MDP. Impact of climate change on dermatological conditions related to flooding: update from the International Society of Dermatology Climate Change Committee [Internet]. Vol. 57, International Journal of Dermatology. Blackwell Publishing Ltd; 2018. [cited 2021 May 10]. p. 901–10. Available from: [DOI] [PubMed] [Google Scholar]
- 68.Hendrickson LA, Vogt RL, Goebert D, Pon E. Morbidity on Kauai before and after Hurricane Iniki. Prev Med (Baltim) [Internet].1997September1 [cited 2020 Sep 8];26(5):711–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091743597901961 [DOI] [PubMed] [Google Scholar]
- 69.Park KJ, Moon JY, Ha JS, Kim SD, Pyun BY, Min TK, et al. Impacts of Heavy Rain and Typhoon on Allergic Disease. Osong Public Heal Res Perspect [Internet].2013June1 [cited 2020 Sep 8];4(3):140–5. Available from: http://linkinghub.elsevier.com/retrieve/pii/S2210909913000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.D’Amato G, Chong-Neto HJ, Monge Ortega OP, Vitale C, Ansotegui I, Rosario N, et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens [Internet]. Vol. 75, Allergy: European Journal of Allergy and Clinical Immunology. Blackwell Publishing Ltd; 2020. [cited 2021 May 11]. p. 2219–28. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/all.14476 [DOI] [PubMed] [Google Scholar]
- 71.Institute of Medicine (IOM). Damp Indoor Spaces and Health [Internet]. Washington, D.C.: The National Academies Press; 2004. [cited 2021 May 12]. 29–89 p. Available from: http://jare.org.gy/wp-content/uploads/2015/12/Rose-S-An-evaluation-of-the-prevalence-of-respiratory-FNS.pdf [Google Scholar]
- 72.Cummings KJ, Cox-Ganser J, Riggs MA, Edwards N, Hobbs GR, Kreiss K. Health effects of exposure to water-damaged New Orleans homes six months after Hurricanes Katrina and Rita. Am J Public Health [Internet].2008May1 [cited 2020 Sep 8];98(5):869–75. Available from: http://ajph.aphapublications.org/doi/10.2105/AJPH.2007.118398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Quinn B, Baker R, Pratt J. Hurricane Andrew and a Pediatric Emergency Department. Ann Emerg Med. 1994April1;23(4):737–41. [DOI] [PubMed] [Google Scholar]
- 74.Alhinai MY. Tropical cyclone Gonu: Number of patients and pattern of illnesses in the primary health centers in A’Seeb area, Muscat, Sultanate of Oman. Oman Med J [Internet].2011. [cited 2020 Sep 8];26(4):223–8. Available from: /pmc/articles/PMC3191707/?report=abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.John Galantowicz, Jeff Picton, Root Ben. Mapping Daily and Maximum Flood Extents at 90-m Resolution During Hurricanes Harvey and Irma Using Passive Microwave Remote Sensing. In: Atmospheric and Environmental Research (AER) [Internet].American Geophysical Union, Fall Meeting; 2017, abstract #NH23E-2833; 2017. [cited 2021 May 3]. Available from: https://ui.adsabs.harvard.edu/abs/2017AGUFMNH23E2833G/abstract [Google Scholar]
- 76.Parks RM, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, Kioumourtzoglou MA. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat Commun [Internet].2021December1 [cited 2021 Jun 3];12(1):1–12. Available from: 10.1038/s41467-021-21777-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rodriguez-Llanes JM, Ranjan-Dash S, Degomme O, Mukhopadhyay A, Guha-Sapir D. Child malnutrition and recurrent flooding in rural eastern India: A community-based survey. BMJ Open [Internet].2011January1 [cited 2021 May 18];1(2):e000109. Available from: http://bmjopen.bmj.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dai W, Wang J, Kaminga AC, Chen L, Tan H, Lai Z, et al. Predictors of recovery from post-traumatic stress disorder after the dongting lake flood in China: A 13–14 year follow-up study. BMC Psychiatry [Internet].2016November8 [cited 2021 May 18];16(1):1–9. Available from: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-016-1097-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


