Abstract
BACKGROUND
Epidemiologic studies often use self-report as proxy for clinical history. However, whether self-report correctly identifies prevalence in minority populations with health disparities and poor healthcare access is unknown. Furthermore, overlap of clinical vascular events with covert vascular brain injury (VBI), detected by imaging, is largely unexamined.
METHODS
The Strong Heart Study recruited American Indians from 3 regions, with surveillance and adjudication of stroke events from 1989–2013. In 2010–2013, all 817 survivors, aged 65–95 years, underwent brain imaging; neurological history interview; and cognitive testing. VBI was defined as imaged infarct or hemorrhage.
RESULTS
Adjudicated stroke was prevalent in 4% of participants; separately-collected, self-reported stroke in 8%. Imaging-defined VBI was detected in 51%, and not associated with any stroke event in 47%. Compared with adjudication, self-report had 76% sensitivity and 95% specificity. Participants with adjudicated or self-reported stroke had poorest performance on cognitive testing; those with imaging-only (covert) VBI had intermediate performance.
CONCLUSION:
In this community-based cohort, self-report for prior stroke had good performance metrics. A majority with VBI did not have overt, clinically-recognized events, but did have neurological or cognitive symptoms. Data collection methodology for studies in resource-limited setting must balance practical limitations in costs, accuracy, feasibility, and research goals.
Keywords: stroke, MRI, vascular brain injury, American Indians / Native Americans
INTRODUCTION
The functional consequences of vascular brain injury (VBI) are broad, [1, 2] and result from both overt, clinically defined stroke and covert, imaging-defined VBI in those without a history of stroke. [3–7] The incidence and prevalence of stroke in American Indians are substantially greater than that of the general U.S. population. [8–10] However, the degree of overlap between overt and covert VBI in American Indians and the clinical impact of covert VBI in this population are unknown. The Cerebrovascular Disease and its Consequences in American Indians (CDCAI) study, an ancillary neurology examination of the original Strong Heart Study (SHS) cohort, used detailed self-reported questionnaires and cranial magnetic resonance imaging (MRI) to compare the prevalence and manifestations of overt and covert VBI. [11, 12] Three methods were available to define VBI: adjudicated stroke, self-reported stroke, and MRI findings of VBI. The purpose of this analysis is to compare the performance and clinical correlates of these methods among American Indians aged 65 and older.
METHODS
Study Setting
Between 1989 and 1991, 4,549 community-dwelling, adult American Indians aged 35–74 from 13 tribes across three geographic regions of the U.S were recruited into the Strong Heart Study (SHS). [13] In 2010–2013, the CDCAI study recruited 1,033 willing, eligible SHS participants (86% of survivors) to undergo clinical examinations related to VBI and its manifestations, including self-reported neurological history and cranial MRI. [11, 12] One community has since withdrawn from all research and have been removed from analytic datasets, resulting in a sample size of N=817.
Event Surveillance
SHS event adjudications [14, 10] and MRI scan [12] procedures were designed to have comparability with methods used by two other large cohort studies, the Cardiovascular Health Study (CHS) [15, 16] and the Atherosclerosis Risk in Communities Study (ARIC) and Jackson Heart Study (JHS). [17, 18] Surveillance and physician adjudication for overt, clinically defined stroke have been continuously conducted through December 31, 2017, based on methods that have been previously described. [14, 10] In short, surveillance identified possible events through telephone contact, interim clinic visits, and mailed questionnaires. Trained field staff reviewed charts for ICD-9 codes (430–436) and specific terminology related to stroke. These codes and terms were also used to search electronic medical records at the Indian Health Service, other local hospitals, and patient care facilities. A committee of physicians adjudicated events using abstracted medical history, physical examination, emergency room visit, medical consult, medical imaging, discharge summary, surgical operation, and other procedure records for all surveillance-identified events. Adjudicated strokes were delineated as definite (evidence of infarct or hemorrhage on imaging and no other disease process that could cause localizing neurological deficit or coma; or history of rapid onset of localizing neurologic deficit and documentation by unequivocal physician of deficit and/or change in consciousness with >24 hours of duration with no other responsible disease process identified), [14] probable, or possible; this analysis considered only definite strokes.
Cranial MRI Data Collection
For the MRI scan, 1.5T scanners were used to obtain six sequences in contiguous slices, including sagittal and axial T1 and T2, FLAIR, and gradient echo sequences, as described previously, [12]. Two study neuroradiologists blinded to clinical data scored number and location of vascular lesions, including infarcts ≥3 mm in maximum dimension and hemorrhages of any size, with microhemorrhages including those <5mm in maximum dimension. MRI-defined VBI was categorized based on the presence of one or more MRI-imaged cerebral infarct or parenchymal hematoma (hemorrhage), including microhemorrhage. Previous reports have described the collection and distribution of these findings in detail. [19, 12, 20]
Self-reported Neurological Data Collection
At the time of the MRI scan visit, participants were asked, “Has a medical person ever told you that you have had a stroke?” This information was collected independently of the surveillance and adjudication procedures described above and was not used in identification of possible events for chart abstraction. Participants were also asked about symptoms possibly related to stroke, including: double vision, loss of vision, dizziness or loss of balance, paralysis, numbness, and any sudden loss or changes in speech.
Classification of Stroke and Vascular Brain Injury
MRI scans were conducted among survivors from the original baseline SHS cohort. All analyses of prior stroke included only non-fatal, definite adjudicated events that occurred before the time of the MRI scan. Categorization of participants for VBI included: those with overt adjudicated stroke and MRI-defined VBI lesions; those with overt adjudicated stroke but without MRI-defined VBI lesions; those with covert MRI-defined VBI findings, namely presence of VBI without any record of an adjudicated stroke event; and those with neither MRI-defined VBI lesions nor adjudicated stroke. The differentiation in overt adjudicated stroke between those with and without MRI findings may be important to distinguish those with true VBI from those with temporary, or resolved, or subtle pathology or those whose clinical event did not arise from a vascular pathology.
Other Data Collection
Participants also self-reported age in years, binary sex, years of formal education, annual household income, marital status, smoking and alcohol use history. Use of daily medications was recorded by label transcription. Blood pressure was based on two averaged, seated sphygmomanometry measures. Blood samples were collected to measure cerebrovascular risk factors including glucose, cholesterol, and glomerular filtration rate. Participants completed a battery of neuropsychological and functional tests, including: the Modified Mini-Mental State Examination (3MSE), [21] the Weschler Adult Intelligence Scale digit symbol coding subtest (WAIS), [22] the Controlled Word Association F,A,S test (COWA), [23] the California Verbal Learning Test (CVLT) 2nd edition, short form, long delay free recall, [24] a short physical performance battery (SPPB), [25] grip strength test by dynamometer (grip), [26] and Halstead finger tap test (finger tap) for both dominant and non-dominant hand. [27] [27] Cognitive impairment was defined as 1 SD below mean in any of 3MSE, WAIS, COWA, or CVLT.
Statistical Analyses
Overt adjudicated strokes all occurred by definition before the study MRI scan, and only those adjudicated as definite were included in analyses. Participants were divided into three mutually exclusive groups based on evidence for VBI: overt (adjudicated stroke); covert (MRI-defined in those without adjudicated stroke); and no overt or covert VBI. Summary statistics, including mean and standard deviation or count and percent were used to examine differences in characteristics of participants by these three VBI groups. Cross-tabulation was used to examine concurrence between adjudicated and self-reported stroke and between overt adjudicated stroke and covert MRI-defined VBI, with adjudicated stroke being the gold standard. Sensitivity, specificity, correct classification, and receiver operating characteristic (ROC) area under the curve (AUC) values were calculated to evaluate concurrence among categorizations. Cognitive test scores, adjusted for age and years of formal education using linear regression, were also cross-tabulated by VBI categories. Bar graphs with underlaid scatter plots presented distribution of neuropsychological and functional testing scores by feature categorizations, with coloration by age. All analyses were conducted using Stata v 14 (College Station, TX) or R v3.5 (The R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Participants were mostly female and older, with mean age 73 years (Table 1), and age range 64 to 95 (interquartile range 68 to 77). The top quantile of age (n=145) was mean 83 (SD 3.6), range 79–95. Participants had relatively high years of formal education (more than half attended college) but very low income (majority below national poverty threshold for household size of four). The majority were unmarried, ever smokers and drinkers (albeit mostly former), and had hypertension, and high cholesterol; 49% had diabetes. Out of 817 participants, 33 (4.0%) had overt adjudicated stroke; 68 (8.3%) had self-reported stroke; 287 (35%) had MRI findings of vascular brain injury, whether overt or covert; and 263 (32.2%) had covert MRI-defined VBI (i.e. in the absence of record of an overt, adjudicated stroke event). Of the 287 with MRI-defined VBI, 263 (91%) had infarcts, 45 (16%) had hemorrhages, and 35 (12%) had microhemorrhages (defined as hemorrhage < 5mm in maximum dimension).
Table 1:
Selected participant characteristics by groups of vascular brain injury, for American Indian participants of the Strong Heart Study (2010–2013)
| Groups of Vascular Brain Injury* | ||||
|---|---|---|---|---|
| All N=817 | Neither Overt nor Covert VBI N=521 | Covert VBI, MRI-defined N=263 | Overt VBI, Adjudicated stroke N=33 | |
| Field center | ||||
| Northern Plains | 374 (45.8%) | 45.3% | 45.3% | 57.6% |
| Southern Plains | 346 (42.4%) | 42.2% | 42.6% | 42.4% |
| Southwest | 97 (11.9%) | 12.5% | 12.2% | - |
| Age, years | 73.0 (5.6) | 72.0 (5.3) | 74.4 (6.3) | 77.5 (6.8) |
| Male sex | 263 (32.2%) | 32.1% | 32.3% | 33.3% |
| Education: Any college | 445 (54.5%) | 57.6% | 50.0% | 42.4% |
| Income: <$20k | 484 (59.2%) | 55.1% | 66.2% | 69.7% |
| Not married | 507 (62.1%) | 58.2% | 68.8% | 69.7% |
| Ever smoked | 539 (66.0%) | 68.0% | 61.2% | 72.7% |
| Ever drank alcohol | 617 (75.5%) | 78.7% | 70.0% | 69.7% |
| Diabetes | 403 (49.3%) | 49.1% | 49.8% | 48.5% |
| Hypertension | 660 (80.8%) | 78.9% | 83.7% | 87.9% |
| High cholesterol | 423 (51.8%) | 51.4% | 53.2% | 45.5% |
| Chronic kidney disease | 219 (21.8%) | 24.6% | 30.8% | 30.3% |
| Symptoms of stroke | ||||
| Double vision | 66 (8.1%) | 8.6% | 7.2% | 6.1% |
| Loss vision | 45 (5.5%) | 5.6% | 4.6% | 12.1% |
| Dizzy | 279 (34.2%) | 34.8% | 30.4% | 54.6% |
| Paralysis | 48 (5.9%) | 3.1% | 5.7% | 51.5% |
| Numbness | 83 (10.2%) | 8.6% | 8.3% | 48.5% |
| Changes speech | 50 (6.1%) | 3.7% | 6.1% | 45.5% |
Vascular brain injury (VBI), magnetic resonance imaging (MRI)
Numbers given as count and column percentages, except for years of age, which is given as mean (SD).
Adjudicated stroke with or without findings of VBI on the study MRI defines Overt VBI. MRI findings of VBI without adjudicated stroke defines the Covert VBI.
Participants with overt adjudicated stroke were more likely to be older, unmarried, less educated, lower income, smokers, hypertensive, and have kidney disease, compared with those who without overt or covert VBI. They were also less likely to have consumed alcohol or have high cholesterol but did not differ by sex or diabetes.
A history of experiencing symptoms possibly related to stroke was common, with one-third reporting ever having had spells of dizziness, loss of balance, or sensation of spinning and one-tenth reporting sudden numbness or tingling on one or both sides of the body. More than half of participants with overt adjudicated stroke reported these symptoms. Around half of participants with adjudicated stroke also reported sudden paralysis or weakness or changes to speech, which were experienced by very few without VBI. Changes or loss of vision were reported by around one-tenth of participants with adjudicated stroke but were not significantly difference across the three groups.
In comparisons of self-reported with adjudicated stroke as the gold standard (Table 2), sensitivity is 75.8%, specificity is 94.5%, correct classification (CC) is 93.8%, and AUC is 0.85. Adding report of any symptoms of stroke (dizziness, paralysis, numbness, double vision, loss vision, changes to speech) to self-reported stroke improves sensitivity a little (87.9%) but reduces specificity a great deal (58.4%) and reduces overall test performance (CC 59.6%, AUC 0.73). Adding individual symptoms of dizziness, paralysis, numbness, double vision, loss of vision, and changes to speech changed the AUC moderately to 0.74, 0.86, 0.82, 0.83, 0.83, and 0.85 (respectively). The best addition was symptoms of paralysis, with combined sensitivity 78.8%, combined specificity 92.9%, and CC 92.3%. In sensitivity analyses that included participants with adjudicated possible stroke, symptoms were slightly more common (N=40), but most test comparisons were poorer (Supplemental Materials).
Table 2.
Comparison of physician-adjudicated definite stroke, self-reported stroke, and overt and covert MRI-defined vascular brain injury, for 817 American Indian participants of the Strong Heart Study (2010–2013)
| Definite Adjudicated stroke | |||
|---|---|---|---|
| (Yes) N=33 | (No) N=784 | ||
| Self-reported stroke | (Yes) N=68 | 25 | 43 |
| (No) N=749 | 8 | 741 | |
| Sensitivity 75.8%, specificity 94.5%, correct classification 93.8%, AUC 0.85 | |||
| MRI-defined vascular brain injury‡ | (Yes) N=287 | 24 | 263 |
| (No) N=530 | 9 | 521 | |
| Sensitivity 72.7%, specificity 66.5%, correct classification 66.7%, AUC 0.70 | |||
MRI-defined vascular brain injury (N=287) includes cerebral infarcts ≥ 3 mm (N=263) and hemorrhage any size (N=45). These categories are not mutually exclusive, with N=21 having both infarcts and hemorrhages.
When transient ischemic attack (TIA) events are combined with stroke events in both self-report (n=89) and adjudication (n=83), sensitivity increases to 88.0%, specificity to 97.8%, and correct classification to 96.8%, with area under the curve 0.93. Of those with self-reported stroke, 7 did not report prior TIA; of those with adjudicated possible, probable, or definite stroke, 16 did not have a record of prior TIA.
Of the 33 participants with prior overt, definite, adjudicated stroke events, 9 (27%) did not have MRI-defined vascular findings. Of these, all (100%) reported having had symptoms possible related to stroke: 3 had dizziness, 4 had paralysis, 4 had numbness, 0 had double vision, 0 had loss of vision, 2 had changes to speech. Of these 5, 2 also had some degree of cognitive loss.Participants with MRI findings of VBI, whether overt or covert, (N=287) were 4.2 times more common than self-reported stroke (68) and 8.6 times more common than adjudicated stroke (33). Of participants with only covert MRI-defined VBI, 61.2% (161/263) had cognitive loss, and 37.3% (144/263) reported having had symptoms possibly related to stroke, including 30.1% with dizziness, 5.7% with paralysis, 4.6% with double vision, 7.2% with loss of vision, and 6.1% with temporary loss of speech.
Comparing age- and education- adjusted neuropsychological and physical functional testing results for participants across the three VBI groups (Table 3), participants with adjudicated stroke had lowest general cognition (3MSE), slowest processing speed (WAIS), worst verbal fluency (COWA), worst verbal memory (CVLT), worst lower body physical performance and motor control (SPPB and grip strength), and worst fine motor control (finger tap). Participants with covert MRI-defined VBI were intermediate in all cognitive and physical function tests; and participants without VBI performed best in all tests.
Table 3:
Comparing cognitive test scores, by groups of vascular brain injury, for American Indian participants of the Strong Heart Study (2010–2013)
| All N=817 Score (SD; range) | Neither Overt nor Covert VBI N=521 | Covert VBI, MRI-defined N=263 | Overt VBI, Adjudicated stroke N=33 | |
|---|---|---|---|---|
| 3MSE | 88.4 (4.3; 75–100) | 89.0 (4.0; 76–100) | 87.4 (4.4; 76–98) | 85.3 (5.3; 75–98) |
| WAIS | 44.0 (9.2; 16–69) | 45.4 (8.6; 19–69) | 41.9 (9.3; 17–63) | 37.2 (11.2; 16–63) |
| COWA | 24.3 (5.0; 9–40) | 25.0 (4.8; 10–40) | 23.5 (5.0; 11–39) | 21.4 (6.3; 9–36) |
| CVLT LF | 5.5 (0.5; 4–7) | 5.5 (0.4; 4–7) | 5.3 (0.5; 4–6) | 5.0 (0.6; 4–6) |
| SPPB | 7.5 (1.1; 4–10) | 7.5 (1.1; 4–10) | 7.0 (1.2; 4–9) | 6.3 (1.5; 3–9) |
| Grip (kg) | 24.8 (3.1; 15–33) | 25.4 (2.9; 16–33) | 24.1 (3.2; 15–31) | 22.4 (3.8; 15–30) |
| Finger Tap | 35.0 (2.7; 26–42) | 35.4 (2.5; 27–42) | 34.3 (2.8; 26–40) | 32.9 (3.3; 27–40) |
Modified Mini Mental Status Examination (3MSE; general cognition), Weschler Adult Intelligence Scale (WAIS; processing speed), Controlled Oral Word Association (COWA; verbal fluency) and California Verbal Learning Test 2nd edition short form long delay free recall (CVLT LF; verbal memory), Short Physical Performance Battery (SPPB; lower body motor control), grip strength test (Grip; upper body motor control), and Halstead finger tapping test (finger tap; fine motor control), vascular brain injury (VBI)
Similarly, distribution of cognitive test scores (3MSE, WAIS, COWA, CVLT; Figure) and physical function test scores (SPPB, grip strength, and finger tap; Supplemental Figure) were lowest overall for those with the overt adjudicated stroke, intermediate for those with covert MRI-defined VBI, and highest for those with without VBI. The oldest ages (lightest green) were observed throughout the distribution, although tended to be below the median, compared with the youngest ages (darkest purple).
Figure:
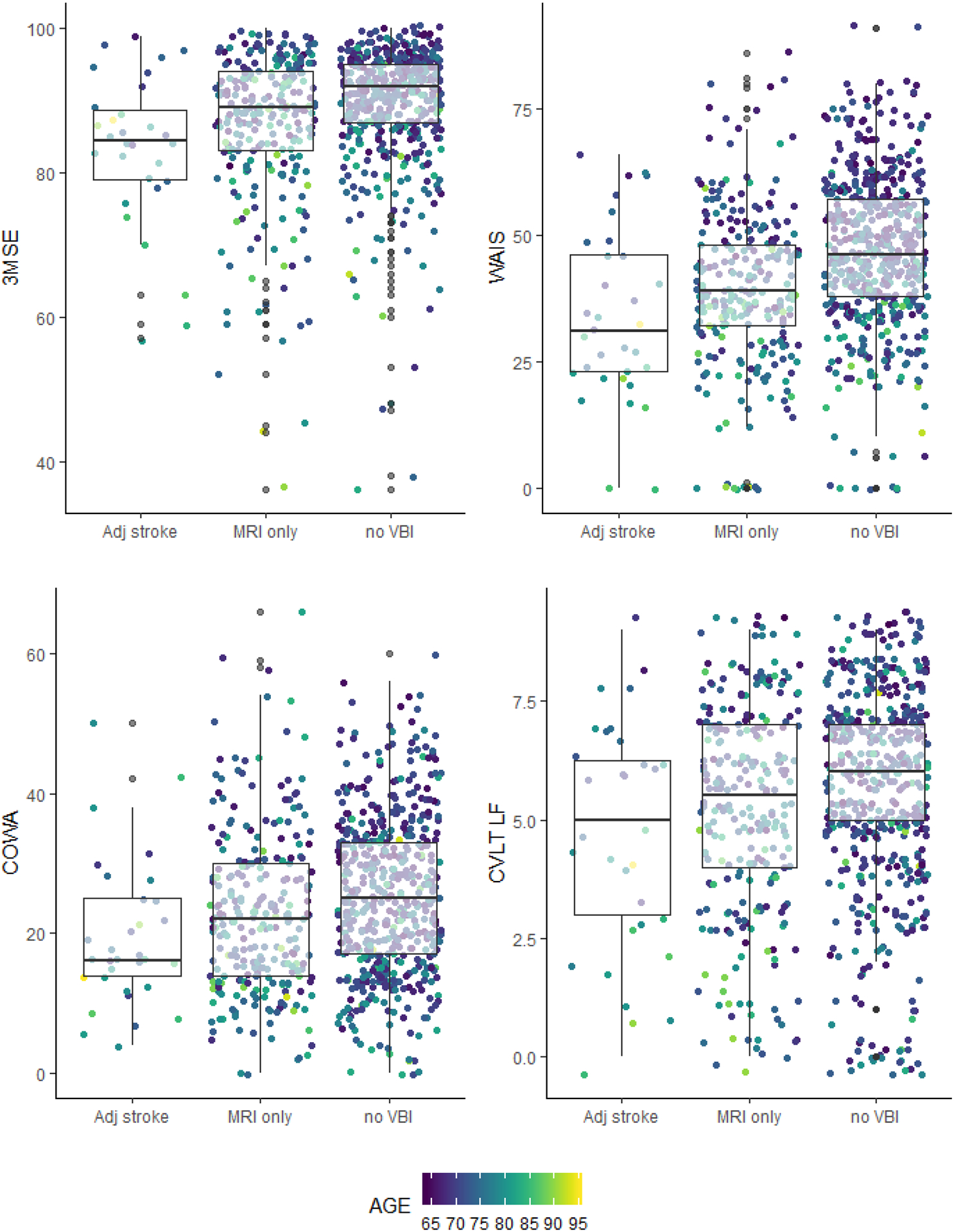
Comparing vascular brain injury and overt clinical, physician adjudicated definite stroke with cognitive test scores and age, for American Indian participants of the Strong Heart Study (2010–2013)
Bar charts and dot plots for cognitive test scores for Modified Mini Mental Status Examination (3MSE; general cognition), Weschler Adult Intelligence Scale (WAIS; processing speed), Controlled Oral Word Association (COWA; verbal fluency) and California Verbal Learning Test 2nd edition short form long delay free recall (CVLT LF; verbal memory) – Y axes – over categories of vascular injury, including those without overt or covert VBI (N=398), those with covert VBI, MRI defined (N=386), and those with overt VBI, adjudicated stroke (N=33) – X axes. Coloration by age, with youngest in dark purple and oldest in light green.
DISCUSSION
This study found moderate sensitivity but high specificity for the self-report method, suggesting that when surveillance and physician adjudication is considered the gold standard, reliance on self-report alone for case ascertainment may result in some missed cases, but few misreported cases. The combination of self-reported events and symptomatology--with temporary paralysis performing best of all symptoms—or addition of TIA improved test characteristics, although whether these features are of interest should be carefully considered in balance with research and clinic objectives.
Evaluation of adjudicated stroke in association with cranial imaging findings suggested a large number of covert vascular findings; these results suggest that if even subtle cerebrovascular changes are of primary research interest, then imaging or detailed case identification methods may be needed. These findings are consistent with previous reports in other populations. [28, 29] Future research should examine whether better screening for subclinical or covert VBI may be warranted by improving vascular, functional, or other health outcomes. Future research may also evaluate predictive capacity of additional post-stroke tests, such as functional disability scores, in both acute and chronic settings, and also to evaluate associations with MRI findings that may not be expected to cause overt clinical events, such as white matter disease.
A small proportion (15%) of participants with prior stroke did not have any evidence of MRI-detected vascular pathology. This result might be unexpected, [30, 31] since adjudicated clinical vascular events should have some underlying brain pathology that would be detectable by MRI. [32, 33] However, similar findings have been reported by the Cardiovascular Health Study, which found up to 41% of incident adjudicated strokes had no evidence of infarct or hemorrhage on the follow-up MRI 5 years later. [34] One potential explanation for such a discrepancy may be that standard methods for reviewing MRI were not adequately sensitive to small, but clinically meaningful vascular events; namely the MRI reading was in error, and a clinical event did occur. However, this explanation is unlikely because duplicate MRI reads included even very small lesions. An alternative explanation might be that the adjudication process to delineate definite stroke may not be adequately specific to vascular events, or may reflect some other pathology with similar neurological symptoms and clinical presentation—namely the medical diagnosis and/or adjudication were in error, and a stroke did not occur, but perhaps some other clinical event did. Or, perhaps, neither was in error, and a stroke did occur, but did not lead to permanent changes in brain tissue that would be identifiable as a VBI event or lesion on a subsequent MRI [35]—challenging the original expectation that a stroke would be recognizable on later imaging.
This analysis included years of formal education as an adjustment feature to address potential confounding, as it is often considered a proxy for achieved education. However, American Indians have been historically subjected to oppressive federal population and educational policies, which may affect these relationships. From the late 19th through much of 20th century, Indigenous US children were forced to attend day or boarding schools—often at great distance from their family homes—and endured abusive disciplinary and other harsh strategies aimed at prohibiting cultural expression and assimilating them into majority US society. [36] At such schools, quality of education was typically low, emphasizing menial labor instead of academic skills. [37] Consequently, quality of achieved education may not be well represented by years of formal education among those who attended such schools; future research should examine these associations using empirical data on educational quality, in order to better assess the confounding relationships on cognition and functional outcomes.
More than 6 million American Indians and Alaska Natives live in the US, with nearly 10% aged 65 years or older; morbidity and mortality statistics suggest that the general health of this subpopulation lags behind that of non-Hispanic Whites. [38, 39] Most American Indians receive federally-guaranteed healthcare from the Indian Health Service, and so documentation of stroke events that occur to members of this population is likely to be comprehensive and complete. However, such coverage has historically been chronically underfunded and often unable to provide specialized treatments or diagnostic tests, such as MRI or comprehensive cognitive assessment, with American Indian adults using health services less often and presenting for care at more advanced stages of disease than their White counterparts. [40, 41] The extreme rurality of many American Indian communities, and its concomitant effects on likelihood for timely care, [42] as well as the limited availability of specialized healthcare and resources such as neurology clinics [43] present additional barriers to neurology care in this underserved population.
A small but meaningful difference was detected by field center in proportion of adjudicated clinical stroke events; no such events were identified among the 97 participants in the Southwest field center, although 3 (12% of 33 such events) would be expected if proportions were consistent by field center and across all events categories. This difference between observed and expected was statistically significant (Chi-squared P-value=0.03). Future research may examine whether any geographic or regional differences can influence events recognition, or whether this observation was due simply to chance.
Strengths of this work include long-term, comprehensive medical and neurological data collection in an understudied population, with extensive, well-documented surveillance, adjudication, and imaging procedures in a large, population-based cohort study. Limitations of our analyses include the possibility of survivor bias: participants were originally recruited in 1989–1991 and followed for adjudicated events prospectively; however, only survivors from the original recruitment were included in CDCAI in 2010–2013. Selective survival could affect findings, if participants were, on average, different from non-participants. Previous comparisons of participation in this follow-up study, based on vascular factors and vascular disease have suggested that is little evidence of selective survival. [44] Additionally, due to neuroradiologists being blinded to clinical data, it can only be circumstantially assumed that a given self-reported or adjudicated stroke is directly related to any specific lesion detected on MRI. However, many participants had covert findings, and an MRI finding in an adjudicated or self-reported stroke case may not be causal or correlated with the identified clinical syndrome. For example, the lesion might be on the opposite side of the brain from the localization of the clinical event.
Overall, research on vascular brain injury in American Indians may benefit from using a combination of imaging, adjudication, or self-reported data, with trade-offs considered on the basis of specific research goals. If the intent is to examine associations with symptomatic events, using self-report or adjudicated data may be warranted. Alternatively, if the association of interest involved some proximal mechanism, using imaging findings alone may comprise the most reasonable approach. Using self-report in place of adjudicated surveillance data may be reasonable if a high degree of case sensitivity is not required. These findings may have implications for studies in other populations, including demonstration of a general need for complementary data collection.
Supplementary Material
Acknowledgements
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Indian Health Service. We thank all Strong Heart Study participants and communities.
Funding Sources
This work and the Strong Heart Study have been funded in whole or in part with federal funds from the National Institutes of Health through research grants K01AG057821, P50AG005136, R01HL109315, R01HL109301, R01HL109284, R01HL109282, and R01HL109319; by cooperative agreements U01HL41642, U01HL41652, U01HL41654, U01HL65520 & U01HL65521; and under contract numbers 75N92019D00027, 75N92019D00028, 75N92019D00029 & 75N92019D00030.
Footnotes
Statement of Ethics
All study and data collection procedures were reviewed by Institutional Review Boards at participating institutions and at regional Indian Health Service organizations, as well as by Research Review Boards for each of the participating tribes and communities. All participants provided written, informed consent.
Conflict of Interest Statement
The authors do not have any conflicts of interest to report.
Data Availability Statement
Data Availability: the data used in this work were collected under research agreements with 13 sovereign Native American / American Indian tribes and communities. Per tribal agreements, these data are owned by the tribes, and as such may not be shared or distributed without their explicit consent.
REFERENCES
- 1.Sachdev PS, Brodaty H, Valenzuela MJ, Lorentz LM, Koschera A. Progression of cognitive impairment in stroke patients. Neurology. 2004November09;63(9):1618–23. [DOI] [PubMed] [Google Scholar]
- 2.Sachdev PS, Lipnicki DM, Crawford JD, Wen W, Brodaty H. Progression of cognitive impairment in stroke/TIA patients over 3 years. J Neurol Neurosurg Psychiatry. 2014December;85(12):1324–30. [DOI] [PubMed] [Google Scholar]
- 3.Mosley TH Jr., Knopman DS, Catellier DJ, Bryan N, Hutchinson RG, Grothues CA, et al. Cerebral MRI findings and cognitive functioning: the Atherosclerosis Risk in Communities study. Neurology. 2005June28;64(12):2056–62. [DOI] [PubMed] [Google Scholar]
- 4.Au R, Massaro JM, Wolf PA, Young ME, Beiser A, Seshadri S, et al. Association of white matter hyperintensity volume with decreased cognitive functioning: the Framingham Heart Study. Arch Neurol. 2006February;63(2):246–50. [DOI] [PubMed] [Google Scholar]
- 5.Rosano C, Brach J, Longstreth WT Jr, Newman AB. Quantitative measures of gait characteristics indicate prevalence of underlying subclinical structural brain abnormalities in high-functioning older adults. Neuroepidemiology. 2006;26(1):52–60. [DOI] [PubMed] [Google Scholar]
- 6.Windham BG, Griswold ME, Shibata D, Penman A, Catellier DJ, Mosley TH Jr. Covert neurological symptoms associated with silent infarcts from midlife to older age: the Atheroscler osis Risk in Communities study. Stroke; a journal of cerebral circulation. 2012May;43(5):1218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meinel TR, Kaesmacher J, Roten L, Fischer U. Covert Brain Infarction: Towards Precision Medicine in Research, Diagnosis, and Therapy for a Silent Pandemic. Stroke; a journal of cerebral circulation. 2020August;51(8):2597–606. [DOI] [PubMed] [Google Scholar]
- 8.Price TR, Manolio TA, Kronmal RA, Kittner SJ, Yue NC, Robbins J, et al. Silent brain infarction on magnetic resonance imaging and neurological abnormalities in community-dwelling older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Stroke; a journal of cerebral circulation. 1997June;28(6):1158–64. [DOI] [PubMed] [Google Scholar]
- 9.Bryan RN, Cai J, Burke G, Hutchinson RG, Liao D, Toole JF, et al. Prevalence and anatomic characteristics of infarct-like lesions on MR images of middle-aged adults: the atherosclerosis risk in communities study. AJNR American journal of neuroradiology. 1999August;20(7):1273–80. [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y, Galloway JM, Welty TK, Wiebers DO, Whisnant JP, Devereux RB, et al. Incidence and risk factors for stroke in American Indians: the Strong Heart Study. Circulation. 2008October7;118(15):1577–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suchy-Dicey AM, Shibata D, Best LG, Verney SP, Longstreth WT Jr., Lee ET, et al. Cranial Magnetic Resonance Imaging in Elderly American Indians: Design, Methods, and Implementation of the Cerebrovascular Disease and Its Consequences in American Indians Study. Neuroepidemiology. 2016September8;47(2):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suchy-Dicey ASD, Madhyastha T, Grabowski T, Longstreth WT, Buchwald D. Findings of Vascular Brain Injury and Structural Loss from Cranial Magnetic Resonance Imaging (MRI) in Elderly American Indians. Neuroepidemiology. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, et al. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. American journal of epidemiology. 1990December;132(6):1141–55. [DOI] [PubMed] [Google Scholar]
- 14.Lee ET, Cowan LD, Welty TK, Sievers M, Howard WJ, Oopik A, et al. All-cause mortality and cardiovascular disease mortality in three American Indian populations, aged 45–74 years, 1984–1988. The Strong Heart Study. American journal of epidemiology. 1998June1;147(11):995–1008. [DOI] [PubMed] [Google Scholar]
- 15.Mittelmark MB, Psaty BM, Rautaharju PM, Fried LP, Borhani NO, Tracy RP, et al. Prevalence of cardiovascular diseases among older adults. The Cardiovascular Health Study. American journal of epidemiology. 1993February1;137(3):311–7. [DOI] [PubMed] [Google Scholar]
- 16.Longstreth WT Jr., Bernick C, Fitzpatrick A, Cushman M, Knepper L, Lima J, et al. Frequency and predictors of stroke death in 5,888 participants in the Cardiovascular Health Study. Neurology. 2001February13;56(3):368–75. [DOI] [PubMed] [Google Scholar]
- 17.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. American journal of epidemiology. 1989April;129(4):687–702. [PubMed] [Google Scholar]
- 18.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke; a journal of cerebral circulation. 1999April;30 (4):736–43. [DOI] [PubMed] [Google Scholar]
- 19.Cholerton B, Omidpanah A, Madhyastha TM, Grabowski TJ, Suchy-Dicey AM, Shibata DK, et al. Total Brain and Hippocampal Volumes and Cognition in Older American Indians: The Strong Heart Study. Alzheimer disease and associated disorders. 2017Apr-Jun;31(2):94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suchy-Dicey A, Shibata D, Cholerton B, Nelson L, Calhoun D, Ali T, et al. Cognitive Correlates of MRI-defined Cerebral Vascular Injury and Atrophy in Elderly American Indians: The Strong Heart Study. Journal of the International Neuropsychological Society: JINS. 2020March;26(3):263–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teng EL, Chang Chui H. The Modified Mini-Mental (3MS) Examination. Journal Clinical Psychiatry. 1987;48(8):314–18. [PubMed] [Google Scholar]
- 22.Wechsler D Wechsler Adult Intelligence Scale (4th ed.). San Antonio, TX: Pearson; 2008. [Google Scholar]
- 23.Benton AL, Hansher K. Multilingual aphasia examination. 2nd ed. Iowa City, IO: AJA Associates; 1976. [Google Scholar]
- 24.Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test (CVLT-II). 2 ed. US: The Psychological Corporation; 2000. [Google Scholar]
- 25.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994March;49(2):M85–M94. [DOI] [PubMed] [Google Scholar]
- 26.Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: Theory and clinical applications. Tucson: Neuropsychology Press; 1993. [Google Scholar]
- 27.Halstead WC. Brain and Intelligence. Chicago: University of Chicago Press; 1947. [Google Scholar]
- 28.Manolio TA, Kronmal RA, Burke GL, Poirier V, O’Leary DH, Gardin JM, et al. Magnetic resonance abnormalities and cardiovascular disease in older adults. The Cardiovascular Health Study. Stroke; a journal of cerebral circulation. 1994February;25(2):318–27. [DOI] [PubMed] [Google Scholar]
- 29.Welty TK, Rhoades DA, Yeh F, Lee ET, Cowan LD, Fabsitz RR, et al. Changes in cardiovascular disease risk factors among American Indians. The Strong Heart Study. Ann Epidemiol. 2002February;12(2):97–106. [DOI] [PubMed] [Google Scholar]
- 30.Kertesz A, Black SE, Nicholson L, Carr T. The sensitivity and specificity of MRI in stroke. Neurology. 1987October;37(10):1580–5. [DOI] [PubMed] [Google Scholar]
- 31.Kleindorfer D, Khoury J, Alwell K, Moomaw CJ, Woo D, Flaherty ML, et al. The impact of Magnetic Resonance Imaging (MRI) on ischemic stroke detection and incidence: minimal impact within a population-based study. BMC Neurol. 2015September25;15:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kucharczyk W, Brant-Zawadzki M. Magnetic resonance imaging of cerebral ischemia and infarction. Magn Reson Annu. 1987:49–69. [PubMed] [Google Scholar]
- 33.Mathews VP, Barker PB, Bryan RN. Magnetic resonance evaluation of stroke. Magn Reson Q. 1992December;8(4):245–63. [PubMed] [Google Scholar]
- 34.Longstreth WT Jr., Dulberg C, Manolio TA, Lewis MR, Beauchamp NJ Jr., O’Leary D, et al. Incidence, manifestations, and predictors of brain infarcts defined by serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2002October;33(10):2376–82. [DOI] [PubMed] [Google Scholar]
- 35.Pinter D, Gattringer T, Enzinger C, Seifert-Held T, Kneihsl M, Fandler S, et al. Longitudinal MRI dynamics of recent small subcortical infarcts and possible predictors. J Cereb Blood Flow Metab. 2019September;39(9):1669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lynch PD C M. The emergence of American Indian leadership in education. Journal of American Indian Education. 1990;29:1–10. [Google Scholar]
- 37.Lomawaima T, McCarty TL. To remain Indian: Lessons in democracy from a century of Native American education. New York, NY: Teachers College Press; 2006 [Google Scholar]
- 38.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the American Indian and Alaska Native adult population: United States, 2004–2008. National Health Statistics Reports: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Interview Statistics; 2010. [PubMed] [Google Scholar]
- 39.Frieden TR, Centers for Disease C, Prevention. Forward: CDC Health Disparities and Inequalities Report - United States, 2011. MMWR Suppl. 2011January14;60(1):1–2. [PubMed] [Google Scholar]
- 40.Kim G, Bryant AN, Goins RT, Worley CB, Chiriboga DA. Disparities in health status and health care access and use among older American Indians and Alaska Natives and non-Hispanic Whites in California. J Aging Health. 2012August;24(5):799–811. [DOI] [PubMed] [Google Scholar]
- 41.Duwe EA, Petterson S, Gibbons C, Bazemore A. Ecology of health care: the need to address low utilization in American Indians/Alaska Natives. Am Fam Physician. 2014February1;89(3):217–8. [PubMed] [Google Scholar]
- 42.Services USDoHH. Defining the Rural Population.
- 43.Kim C. Recruitment and retention in the Navajo Area Indian Health Service. West J Med. 2000October;173(4):240–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suchy-Dicey AM, Muller CJ, Madhyastha TM, Shibata D, Cole SA, Zhao J, et al. Telomere Length and Magnetic Resonance Imaging Findings of Vascular Brain Injury and Central Brain Atrophy: The Strong Heart Study. American journal of epidemiology. 2018June1;187(6):1231–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


