Abstract
Objective:
Assess cognitive impairment (global cognition and executive functioning) in older incarcerated males overall, and according to education and race.
Design:
Cross-sectional
Participants:
The sample included 239 racially diverse (37.7% White, 41.4% Black, 20.9% Hispanic/Other) incarcerated males age ≥50 (mean age = 56.4±6.1; range 50–79 years).
Measurements:
Global cognitive impairment assessed using the Montreal Cognitive Assessment (MoCA) – standard MoCA scoring (1-point adjustment for ≤12 years education, and score <26 indicating cognitive impairment) versus education- and race-specific cutpoints. Trail Making Test (TMT) assessed executive functioning. The relationship between race and cognitive impairment was evaluated using Chi-Square, One-Way ANOVA, and Tukey’s HSD post-hoc analyses. Chi-Square was also used to evaluate the relationship between race and frequency of missed MoCA items.
Results:
Average MoCA score was 24.12±3.38. Overall, 62.8% and 38.5% of participants met criteria for cognitive impairment using standard scoring and education- and race-specific cutpoints, respectively. This difference was largely attributed to the change in proportion of Blacks who met criteria for cognitive impairment after applying education- and race-specific cutpoints (62.6% versus 19.2%). Fewer White inmates were impaired (51.1% versus 36.7%) after applying demographically-adjusted norms; however, the proportion of Hispanics/Others remained largely unchanged (84% versus 80%). A considerable proportion of participants were mildly impaired on TMT-A (18.2% Whites, 7.1% Blacks) and TMT-B (20.5% Whites, 4.1% Blacks). Race differences were observed in missed MoCA items.
Conclusions:
Cognitive impairment is common in older incarcerated persons, despite applying education- and race-specific norms. Notable race differences highlight need for validated assessments for this diverse population.
Keywords: cognitive impairment, race differences, aging, incarceration
Introduction
The number of older incarcerated persons, defined as age 50 and older, has grown exponentially over the past two decades. In fact, the population of older prisoners is increasing at a rate faster than that of same-aged peers in the general U.S. population.1 Studies increasingly indicate that incarcerated persons experience accelerated aging, characterized by rates of chronic illness, multimorbidity, and mobility impairment that are comparable to considerably older persons.2–5 These high rates are attributed to multiple factors including unhealthy lifestyle prior to (e.g., alcohol and drug abuse) and during (e.g., poor diet) incarceration, limited lifetime access to preventive healthcare, and stressful experiences during incarceration.6,7 Considering the many physical hallmarks of aging that incarcerated persons experience at younger ages than the general population, it is likely that older incarcerated persons also have high rates of cognitive impairment. Yet, estimates of cognitive impairment among older incarcerated persons are lacking.
Improved understanding of the burden of cognitive impairment among older incarcerated persons is important for managing the health and well-being of this growing population. Cognitively impaired older incarcerated persons may be more likely to experience inmate-to-inmate victimization or may receive unjust discipline due to inability to follow staff instructions.7,8 Cognitive impairment may also hinder inmates’ abilities to appropriately engage in legal proceedings (e.g., plea bargains). Thus, estimates are needed to support the necessity of training correctional staff in managing and caring for cognitively impaired prisoners or to determine increased need for prisoner-rights advocates. Further, because the majority of incarcerated persons reenter the community, improved knowledge regarding cognitive impairment during incarceration may impact the discharge planning process.
Recently, Ahalt et al.9 examined prevalence of cognitive impairment among 310 older jailed adults using the Montreal Cognitive Assessment (MoCA). They found that 78% of the sample performed below the MoCA standard cut-score of 26, thus suggesting mild cognitive impairment (MCI), with 25% scoring <20, a cutoff score associated with dementia. Importantly, according to standard practice, Ahalt et al.9 applied a 1-point education adjustment to MoCA scores of those not graduating high school (approximately 30% of the sample). However, no stratification by race was made by Ahalt et al.10–12 Rather than implying biological differences, race stratification may serve as a proxy for social determinants such as education quality, acculturation, and societal discrimination throughout the life course that may differentially affect cognition in older age.10,11 Without these considerations, the proportion of cognitive impairment in black, indigenous, and people of color (BIPOC) samples may be artificially inflated,12 which could further perpetuate structural racism (i.e., thoughts that non-White groups have poorer cognition than their White counterparts). Because BIPOC individuals are over-represented among incarcerated persons in the U.S.,13,14 it is important to consider how these factors may impact estimates of cognitive impairment in older incarcerated persons.
Initial age-related declines in cognition often include abilities involving information processing speed and executive functioning necessary for efficient execution of daily living skills (e.g., planning, goal-setting, problem solving).15 Yet, the MoCA and other cognitive screeners lack detailed assessment of processing speed and executive functioning. Previous studies of mixed-age (i.e., young and middle aged; mean age <35 years) incarcerated samples found a high prevalence of impaired executive functions in areas including problem solving, planning, inhibition, and multi-tasking.16–18 Considering evidence of accelerated aging5 it is likely that incarcerated persons age ≥50 years may experience deficits in these aspects of cognitive function. Yet, to date, no studies specific to older prisoners have evaluated deficits in executive functioning and information processing either overall or according to race.
This study’s objective was to evaluate impairments in global cognition, as well as processing speed and executive functioning, in a racially diverse sample of older incarcerated persons. Expanding upon work by Ahalt et al.,9 we assessed for cognitive impairment not only using education-corrected scores, but also by applying race-based normative scores. We hypothesized that operationalizing cognitive impairment in this way would result in a lower proportion of cognitive impairment in our sample of older incarcerated persons, overall and within racial groups, relative to the proportion determined using standard MoCA cut-scores. In addition, we determined the proportion of processing speed impairment (i.e., amount of time it takes to process information) and an aspect of executive functioning (i.e., ability to shift attention between tasks) using the Trail Making Test (TMT) and hypothesized that rates of impairment would differ by race.
Methods:
Procedure
Data are from the baseline phase of the Aging Inmates Suicidal Ideation and Depression Study (Aging INSIDE), a longitudinal study of individuals “aging in place” in prison. The study was approved by the UConn Health Institutional Review Board and the Research Advisory Committee of the Connecticut Department of Correction (CTDOC). Due to few female participants (n=14), the current study sample included males only.
Recruitment and consent procedures are described elsewhere.19 As shown in Figure 1, between November 2016 and December 2019, CTDOC provided the Aging INSIDE investigators with quarterly lists of inmates who were incarcerated in 1 of the 8 CTDOC prisons, were age ≥50, were sentenced, and were expected to be incarcerated for at least 36 months (N=1,029). Because incarcerated individuals are often released or paroled prior to their maximum end-of-sentence date, this latter criteria was included to account for a potential lag between receipt of the recruitment letter and participant interviews. Letters describing Aging INSIDE were sent to all eligible incarcerated men. Those interested in participating were asked to submit page 2 of the letter which included their name, Inmate Number, housing unit, and date to the designated drop-off location within each facility. This process served as a cognitive screener of sorts; inmates needed a baseline level of cognitive ability to read the recruitment letter and follow directions to submit forms. During this timeframe, 296 (28.8%) eligible inmates submitted letters of interest. Of these, 46 (15.5%) refused to meet with the RAs after up to 3 meeting requests. RAs explained the study purpose to the 250 men who agreed to meet and specified that there were neither incentives for participating or negative consequences for refusing. Inmates described the study purpose and procedures in their own words to ensure adequate understanding. During the meetings, 7 men were deemed to be ineligible (e.g.., had difficulty understanding English) and 4 refused to provide consent. Thus, of the initial 296 men who indicated interest in the study, 244 (82.4%) provided written informed consent, with race data available for 239 of these individuals (see Figure 1). In-person interviews followed consent. Reviews of medical charts and CTDOC data were completed within 2 weeks.
Figure 1.
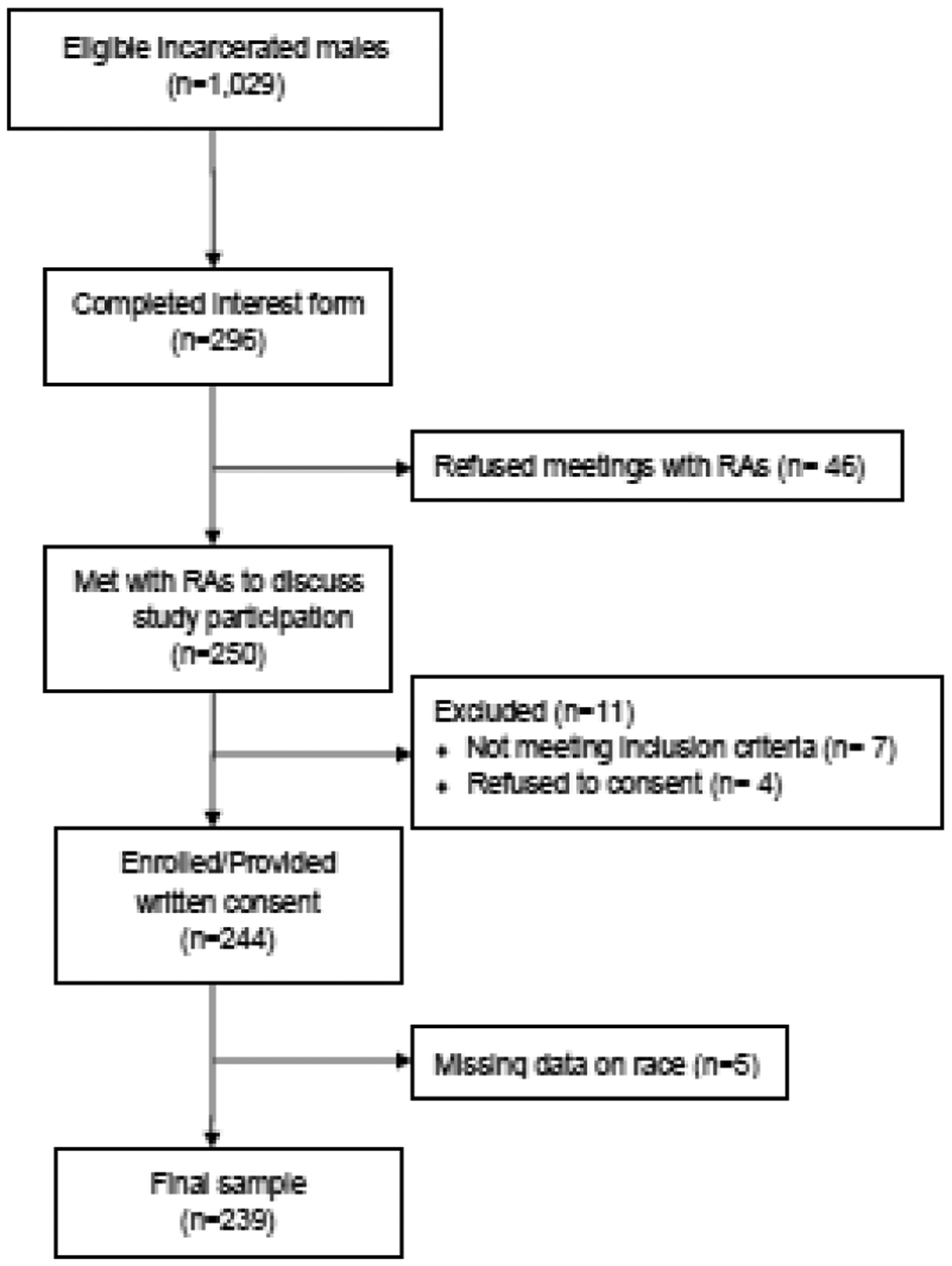
Aging INSIDE recruitment and enrollment.
Measures
Dependent Variable – Cognition
Global cognition
Global cognition was assessed using the Montreal Cognitive Assessment (MoCA), a 30-point screening measure that evaluates aspects of attention, orientation, language, verbal memory, visuospatial abilities, and executive functioning and requires approximately 15 minutes to administer. Although not previously validated for use in prison populations, the MoCA has high sensitivity for detecting MCI and dementia in various racial groups,12 and is frequently used in clinical settings.20,21 Cognitive impairment was defined in two ways. First, using the standard scoring method, participants’ MoCA scores were adjusted upward one point if they had ≤12 years of education. Those performing <26 were considered as cognitively impaired. Second, we applied previously developed cut-points accounting for both education (≤ 12 years, 13–16 years, and >16 years) and race to differentiate between cognitively normal participants and those with MCI.12 For example, among Non-Hispanic Blacks, MoCA cutpoints indicating MCI are ≤19, ≤23, and ≤ 23 for those with ≤12, 13–16, and >16 years of education, respectively.
Executive functioning
Executive functioning was assessed using the Trail Making Test (TMT), a timed two-part test that evaluates processing speed (TMT-A) and set-shifting (TMT-B).22 Each part consists of 25 circles distributed over a sheet of paper. In TMT-A, the individual draws lines connecting numbers in ascending order as quickly as possible. In TMT-B, the circles include both numbers (1–13) and letters (A-L); the individual now alternates between numbers and letters in ascending order (i.e., 1-A-2-B-3-C, etc.) as quickly as possible. Before starting the TMT, participants complete a practice trial of six items to ensure understanding of both tasks. Mild impairment on TMT-A and TMT-B was defined by Halstead-Reitan Neuropsychological Battery norms adjusted for age, education, and race (T-score ≤35).
Demographic Variables:
Age ranged from 50–79. Race was categorized as non-Hispanic White, non-Hispanic Black, and Hispanic/Other. Education was considered as a continuous variable and was also categorized as ≤12, 13–16, and ≥17 years of education, respectively.
Covariates:
Length of time in prison for the current offence was obtained via CTDOC records. Medical record review was used to determine history of either/both HIV or Hepatitis C (coded as a yes/no dichotomous variable) and to determine total number of the following 9 common chronic conditions: hypertension, myocardial infarction, congestive heart failure, transient ischemic attack, cancer, diabetes, hip fracture, arthritis, and chronic lung disease. History of head injury (yes/no) was determined by asking participants if they had ever had a head injury (e.g., concussion). Possible alcohol dependence was assessed using the CAGE measure.23 Lifetime illicit drug use (i.e., drugs/medications not prescribed by a physician) was assessed using Question 1 from the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) version 3.0. (Group 2002) and was coded as a dichotomous variable (yes/no).
Statistical Analyses:
Descriptive statistics were used to report sample demographic characteristics and average MoCA scores and TMT T-scores, overall and according to race. Pearson product-moment correlations evaluated relationships among the MoCA, TMT, and demographic variables (age and education). One-Way ANOVA and Tukey’s HSD post-hoc analyses determined the relationship between race and cognition after controlling for years incarcerated, number of chronic illnesses, HIV or hepatitis C, head injury, alcohol dependence, and illicit substance use. The relationship between race and incorrect items on the MoCA was also analyzed using Chi Square. Due to limited norms for those of Hispanic ethnicity, only non-Hispanic Whites and non-Hispanic Blacks were included in TMT analyses. Analyses were performed using IBM SPSS Version 26.
Results
Demographic Characteristics
Table 1 presents demographic characteristics for the 239 participants. Mean age was 56.4 (SD = 6.07, range 50 – 79) and average years of education was 12.04 (SD = 2.25). Regarding race, 90 (37.7%) identified as non-Hispanic White, 99 (41.4%) as non-Hispanic Black, and 50 (20.9%) as Hispanic/Other. The race distribution is similar to that of males incarcerated in the CT prisons in 2017, when study enrollment began.24 Whites were significantly older (One-Way ANOVA: F2, 236 = 10.22 p<.001) with more years of education (One-Way ANOVA: F2, 236 = 6.99, p<.001) compared with Blacks and Hispanics/Others. Whites were significantly older at first incarceration compared with Blacks and Hispanics/Others (One-Way ANOVA: F2, 236 = 17.75, p<.001), though years in prison for the current offense did not differ by race. Regarding clinical and behavioral factors, race was associated with history of head injury (Chi Square: X2 (2, 239) = 12.13, p = .002) and alcohol dependence (Chi-Square: X2 (2, 239) = 13.298 p = .001).
Table 1.
Demographic characteristics of incarcerated males overall and according to race.
| Participant Characteristics | Participants by Race | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Participants (N = 239) | White (N = 90) | Black (N = 99) | Hispanic/Other1 (N = 50) | F-value3 | Chi-Square4 | df | p-value | Tukey’s post-hoc | |
| Demographics | |||||||||
| Age, mean ± SD (range) | 56.4 ± 6.07 (50–79) | 58.54 ± 7.33 (50–79) | 54.95 ± 4.76 (50–71) | 55.16 ± 4.67 (50–67) | 10.22 | 2,236 | <0.001 | W > B & H/O2 | |
| Education, mean ± SD | 12.04 ± 2.25 | 12.7 ± 2.16 | 11.76 ± 2.04 | 11.40 ± 2.56 | 6.99 | 2,236 | 0.001 | W > B & H/O2 | |
| Education categories, n (%) | 18.95 | 4 | .001 | ||||||
| ≤12 years | 172 (71.9) | 51 (56.7) | 79 (79.8) | 42 (84.0) | |||||
| 13–16 years | 58 (24.3) | 32 (35.6) | 18 (18.2) | 8 (16.0) | |||||
| ≥17 years | 9 (3.8) | 7 (7.8) | 2 (2.0) | -- | |||||
| Incarceration-related factors | |||||||||
| Years in prison for current offense, mean ± SD | 13.22 ± 9.70 | 13.02 ± 9.93 | 14.62 ± 10.13 | 10.78 ± 7.88 | 2.67 | 2,236 | 0.07 | ||
| Age at first incarceration, mean ± SD | 28.36 ± 14.73 | 34.52 ± 17.08 | 22.57 ± 9.86 | 28.72 ± 13.82 | 17.75 | 2,236 | <0.001 | W > H/O > B2 | |
| Clinical and behavioral factors | |||||||||
| Number of chronic conditions, mean ± SD | 2.09 ± 1.13 | 2.16 ± 1.08 | 1.97 ± 1.16 | 2.20 ± 1.17 | .919 | 2,231 | 0.40 | ||
| History of HIV or Hepatitis C, n (%) | 54 (22.6) | 19 (21.1) | 20 (20.2) | 15 (30.0) | 2.23 | 2 | .328 | ||
| History of head injury, n (%) | 97 (40.6) | 30 (33.3) | 53 (53.5) | 14 (28.0) | 12.13 | 2 | .002 | ||
| History of alcohol dependence, n (%) | 104 (43.5) | 53 (58.9) | 33 (33.3) | 18 (36.0) | 13.98 | 2 | .001 | ||
| History of illicit substance use, n (%) | 216 (90.4) | 82 (91.1) | 91 (91.9) | 43 (86.0) | 1.43 | 2 | .490 | ||
Other (N = 16)
W = White; B = Black; H/O = Hispanic/Other
One-Way ANOVA
Chi-Square Test
Cognitive performance: Montreal Cognitive Assessment (MoCA)
Table 2 presents participants’ cognitive performance overall and according to race using the two definitions. Overall, average MoCA score based on standard scoring was 24.12 ± 3.38. Race was associated with MoCA scores (One-Way ANOVA: F2, 234 = 4.43, p = .013). Tukey’s post-hoc analysis indicated that average standard MoCA scores for Whites (M = 24.93, SD = 3.34) and Blacks (M = 24.30, SD = 3.09) were significantly higher than Hispanics/Others’ scores (M = 22.28, SD = 3.38), but scores did not differ between Whites and Blacks. When using standard MoCA scoring and the cutpoint of <26 to indicate cognitive impairment, 168 (62.8%) participants are considered cognitively impaired. In contrast, 38.5% met criteria for cognitive impairment when applying the education- and race-specific cutoff scores. Consequently, 61% of those 168 individuals no longer met criteria when applying the education- and race-specific cutoff scores. Moreover, there were race differences in the proportion of those scoring <26 based on standard MoCA scoring (Chi-Square: X2 (2, 239) = 14.88, p = .001), with a considerably lower proportion of cognitively impaired Whites compared with Blacks and Hispanics/Others. After applying the education- and race-specific cutpoints, Blacks experienced the greatest reduction in those meeting criteria for impairment (from 62.6% to 19.2%). Thus, of the 61 Black participants who met criteria for cognitive impairment based on standard scoring, only 31% (19/61 = 31.1%) were still considered cognitively impaired. In contrast, the majority of Whites (33/46 = 71.7%) and Hispanics/Others (40/42 = 95%) who were cognitively impaired based on the first definition, were still considered cognitively impaired when applying the education- and race-specific cutpoints.
Table 2.
Cognitive Performance for the Study Sample Overall and According to Race.
| Overall (N=239) | White (n=90) | Black (n=99) | Hispanic/Other1 (n=50) | F-value3 | Chi-Square4 | df | p-value | Tukey’s post-hoc | |
|---|---|---|---|---|---|---|---|---|---|
| Montreal Cognitive Assessment (MoCA) | |||||||||
| MoCA score, mean ± SD | 24.12 ± 3.38 | 24.93± 3.34 | 24.30 ± 3.09 | 22.28 ± 3.38 | 4.43 | 2,236 | .013 | W & B > H/O2 | |
| Cognitively impaired based on standard MoCA scoring <26, n (%) | 150 (62.8) | 46 (51.1) | 61 (62.6) | 42 (84.0) | 14.88 | 2 | .001 | ||
| Cognitively impaired based on education- and race-specific cutpoints, n (%) | 92 (38.5) | 33 (36.7) | 19 (19.2) | 40 (80.0) | 52.09 | <0.001 | |||
| Trails Making Test | |||||||||
| TMT-A, mean ± SD | 41.52 ± 19.46 | 39.08 ± 16.41 | 43.13 ± 20.99 | 42.66 ± 21.20 | 1.13 | 2,235 | 0.326 | ||
| TMT-B, mean ± SD | 131.53 ± 86.08 | 104.20 ± 52.09 | 138.23 ± 82.51 | 167.61 ± 121.46 | 9.76 | 2,234 | <0.001 | W > B & H/O2 | |
| TMT-A t-score <=35, n (%) | 34 (16.2) | 16 (18.2) | 7 (7.1) | 4.25 | 1 | .039 | |||
| TMT-B t-score <=35, n (%) | 34 (16.3) | 18 (20.5) | 4 (4.1) | 10.25 | 1 | .001 |
Other (N = 16)
W = White; B = Black; H/O = Hispanic/Other
One-Way ANOVA. The variables that were controlled for include number of chronic conditions and history of head injury, substance use, and either/both HIV or Hepatitis C.
Chi-Square Test
Figure 2 shows the proportion of participants who correctly answered each of the 14 scored MoCA items according to race. As compared with Blacks and Hispanics/Others, a significantly higher proportion of Whites had correct responses on cube drawing (White: 61%; Black: 46.5%; Hispanic/Other: 50%; X2 (2, 239) = 6.17, p = .046), digits backward (White: 88%; Black: 75%; Hispanic/Other: 58%; X2 (2, 239) = 15.88, p <.001), serial sevens (White: 87%; Black: 81%; Hispanic/Other: 66%; X2 (2, 239) = 8.64, p = .013), sentence repetition (White: 50%; Black: 42%; Hispanic/Other: 16%; X2 (2, 239) = 7.63, p = .022), and abstraction (White: 61%; Black: 40%; Hispanic/Other: 22%; X2 (2, 239) = 20.99, p <.001). Although race was associated with Orientation to time, there were only 2 Hispanic/Other participants who incorrectly answered this item out of all participants (White: 100%; Black: 100%; Hispanic/Other: 96%; X2 (2, 239) = 7.62, p = .022). For one item, verbal fluency, the proportion of correct responses was highest for Blacks (White: 66%; Black: 73%; Hispanic/Other: 52%; X2 (2, 239) = 7.60, p = .041).
Figure 2.
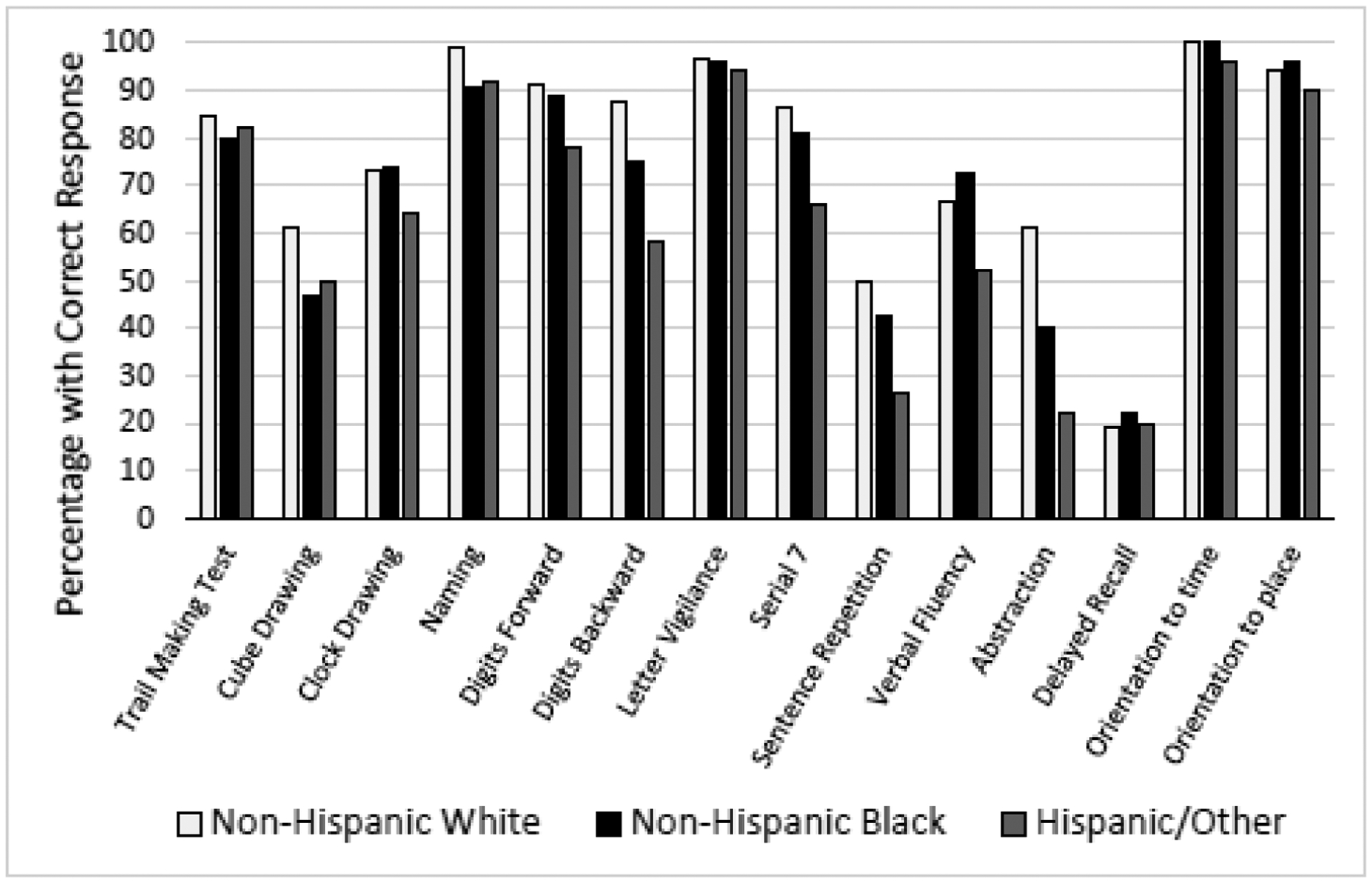
Proportion of participants who correctly answered each of the 14 MoCA items according to race.
Cognitive performance: Trails Making Tests A & B (TMT-A & TMT-B)
Table 2 also presents results from TMT A & B overall and by race. Average completion time for TMT-A was 41.52 (±19.46) seconds and TMT-B was 131.53(±86.08) seconds. Time to complete TMT-B differed significantly by race (One-Way ANOVA: F1, 232 = 8.38, p <.001). Tukey’s post-hoc analysis demonstrated that Whites performed faster than Blacks (p = .015) and Hispanics/Others (p <.001), but there was no difference between time to complete TMT-B between Blacks and Hispanics/Others (p = .108). Using values normed for education and race, approximately 16% of the sample (includes Whites and Blacks only) had a t-score ≤35 on TMT-A and TMT-B, respectively, indicating cognitive impairment. When stratifying by race, there were differences in the proportion of Whites (18%) and Blacks (7.1%) who had a t-score ≤35 on TMT-A (Chi-Square: X2 (2, 191) = 4.25, p = .039), as well as Whites (20.5%) and Blacks (4.1%) who had a t-score ≤35 on TMT-B (Chi-Square: X2 (2, 191) = 10.25, p = .001).
Discussion
With the growth of the older incarcerated population, and evidence pointing towards accelerated aging in this group, the prevalence of cognitive impairment and dementia in this population may increase substantially. Yet, knowledge regarding cognitive function in older incarcerated persons is limited. Moreover, what little is known does not consider how education and race differences may impact estimates of cognitive impairment. In the present study, we assessed cognitive impairment in older incarcerated persons, operationalized as global cognition and executive functioning (i.e., information processing and set shifting), by applying standard education- and race-based normative scores. We found that cognitive impairment is common in older incarcerated persons. We also found that the considerable difference in the proportion of those who meet criteria for cognitive impairment before and after applying education- and race-based norms is driven largely by the difference within older incarcerated Blacks. This finding raises concerns regarding the meaningfulness of using race-based norms to assessing cognitive impairment in a carceral setting. We also found that despite applying education- and race-based scores to indicate cognitive impairment, racial differences persist.
In this racially diverse sample of older, incarcerated persons, nearly 63% met criteria for cognitive impairment based on standard MoCA scoring procedures, where those with ≤12 years of education get a 1-point adjustment. However, after applying education- and race-specific normative scores to indicate cognitive impairment, the proportion reaching the threshold for impairment dropped to approximately 40%. This proportion is still considerably higher than what is reported among older people living in the community.25 Whereas 15% fewer non-Hispanic Whites and 4% fewer Hispanics/Others in our study met the criteria for cognitive impairment after applying these cutpoints, 43% fewer Blacks met the threshold. This is a striking difference. Recently, Ahalt et al.9 reported that 78% of their sample had MoCA scores <26. Furthermore, even when using a lower cutpoint of <25, 70% of their study participants met criteria for cognitive impairment. Given that more than 75% of the participants in the Ahalt et al.9 study were non-White, it is likely that the proportion of those meeting criteria for cognitive impairment in that study would have been considerably smaller had education- and race-based scores been applied. However, together, our findings and those of Ahalt et al. highlight the lack of clarity regarding what constitutes cognitive impairment in a carceral setting and raise concerns regarding potential implications of deriving estimates of cognitive impairment among older incarcerated persons based on norms developed from community-dwelling persons. For example, it is possible that applying race-based norms, and attempting to account for lifelong inequities experienced by BIPOC groups (e.g., growing up in up in disadvantaged neighborhoods with lower-achieving schools and fewer community resources),26,27 could inadvertently result in the underestimation of cognitive impairment. This, in turn, could lead to provision of fewer resources for a vulnerable population. Alternately, it is also possible that failure to account for race as an indicator of systemic differences may overestimate cognitive impairment in older, incarcerated Blacks and propagate negative stereotypes. Thus, these findings encourage researchers to evaluate the sensitivity and specificity of the MoCA for assessing cognitive impairment in older incarcerated persons, and to consider how different cutpoints map with inmates’ abilities to navigate day-to-day living in this unique setting. This information is critical for informing the need for enhanced staff training and prisoner-rights advocates, and for developing appropriate discharge plans for those transitioning back to the community.
Of note, Hispanics/Others had the highest proportion of cognitive impairment, regardless of whether standard <26 MoCA scores or education and race-based MoCA cutpoints were applied. The high proportion of Hispanics/Others meeting criteria for cognitive impairment likely reflects at least in part, that English was not the primary language of at least 9 of the 50 individuals who identified as Hispanic/Other. This finding may also explain why a low proportion of Hispanics/Others correctly answered items related to language (i.e., sentence repetition, verbal fluency, verbal abstraction). In addition, the majority of non-Hispanic Black participants scored incorrectly on cube drawing and abstraction. These items have previously been criticized as being particularly prone to socio-educational and/or cultural bias.28 Further studies are needed to evaluate the validity and clinical usefulness of individual MoCA items in BIPOC incarcerated persons.
We also found 16% of this sample met criteria for cognitive impairment in aspects of executive functioning. Interestingly, this proportion is relatively similar to the proportion expected in community-dwelling samples from various age groups.29–31 In the present study, a considerable proportion of White and Black inmates were at least mildly impaired on a measure of processing speed (18.2% and 7.1%, respectively) and executive-functioning (20.5% and 4.1%, respectively). Regarding the TMT, a disproportionately greater number of White inmates were considered at least mildly impaired on a measure of processing speed (i.e., TMT-A) and executive functioning (i.e., TMT-B) relative to Black inmates, which contradicts findings typically seen in studies on community-dwelling older persons.32 By contrast, when comparing overall scores (i.e., not limited to those who fall below the cutoff of mildly impaired) racial differences were not observed on the TMT-A, and White inmates performed better than Black and Hispanic/Other inmates on the TMT-B. These contradictory results may, in part, speak to the appropriateness of deriving estimates of cognitive impairment among older incarcerated persons based on norms developed from community samples. For example, geographic differences between the White and Black individuals from which the normative data originate may explain the differences in TMT performance. Black individuals were recruited in one Western City (San Diego), whereas White individuals came from rural and urban areas across the U.S. Therefore, the TMT normative data may have greater generalizability to Whites in our sample as compared with Blacks. Furthermore, because the Reitan22 normative data is only categorized for Whites and Blacks, the Hispanic/Other participants were excluded from TMT standard analyses. Given the disproportionately high rates of incarcerated Hispanics in the U.S.,13,14 rates of cognitive impairment in this group merit further exploration.
The characteristics of our sample may also explain the race differences in cognitive impairment even after applying education- and race-based scoring. Consistent with prior reports,33 average age at first incarceration was more than 10 years younger among Blacks in our study compared with Whites (22.57 years vs. 34.52 years). The inverse relationship between age at first incarceration and rate of cognitive impairment in older incarcerated persons may be explained by several factors. Peak performance in executive functioning occurs sometime between ages 20 and 29.34 Considering that Blacks in our study were first incarcerated, on average, on the lower end of this range, it is possible their executive abilities developed differently in the prison environment than they would have in a non-prison setting. For example, given the highly structured and routinized environment of prisons in which choices and decision-making are limited, there may be reduced need for multi-tasking, decision-making, and planning. This may result in lower cognitive performance in older age, particularly in executive functioning. This explanation may also account for why Blacks had a greater number of missed items related to executive skills on the MoCA (i.e., digit backward, verbal abstraction) and lower overall scores on the TMT-B compared with their White counterparts. The high proportion (53%) of Blacks who reported a history of head injury may also contribute to racial differences in cognition. There is growing evidence supporting a higher risk of poor cognitive performance and dementia among those with head injuries.35 Our study is limited such that we do not have data indicating reason for the head injury. Considering growing awareness of race differences in use of force during arrests/interactions with law enforcement36, understanding the context of the head injury is important for informing future prevention efforts. In addition, longitudinal studies with larger samples of older BIPOC incarcerated persons are needed to understand if change in cognition during incarceration is differentially impacted by head injury.
This study has other limitations that should be noted. Less than 30% of those who were sent Aging INSIDE recruitment letters submitted forms indicating potential interest. Reasons for the low initial interest in the study may include general distrust of researchers, unwillingness to take time away from a prison-issued job, inability to read or understand the recruitment letter due to poor literacy/minimal education, or lack of incentive to participate (i.e., no compensation).37 Yet, despite the low initial response, more than 82% of those expressing interest in the study were enrolled. Finally, because our sample consisted of older incarcerated males from one state, the findings may not be widely generalizable.
Overall, this study demonstrates elevated rates of cognitive impairment in older incarcerated males, particularly in non-Hispanic Blacks and Hispanic/Others. While we attempted to account for racial differences and variability in education, we caution readers not to use these findings to influence decision-making around treatment/management for older incarcerated persons. Rather, these findings should encourage investigators to explore and tease out how social and behavioral factors over the lifecourse, especially among BIPOC individuals who are overrepresented among the incarcerated, may contribute to negative outcomes in older age within the carceral setting. In addition, our findings should help to promote discussion regarding the need for instrumentation and normative data that can optimize assessment of cognitive impairment in the growing population of older, incarcerated persons.
HIghlights.
Improved understanding of the burden of cognitive impairment among the growing population of older incarcerated persons is important. We evaluated impairments in global cognition (MoCA), as well as processing speed and set shifting (Trails A & B), in 239 racially diverse, incarcerated males age ≥50 years. Cognitive impairment is common in older incarcerated persons, despite applying education- and race-specific norms. Notable race differences highlight need for validated assessments for this diverse population.
ACKNOWLEDGEMENTS:
The authors thank Deborah Noujaim, MPH, Alexandra DePalma, and Danielle Zaugg, LCSW for assistance with recruitment, data collection, and data entry; Dorothy Wakefield, MS for assistance with data management; and the CT Department of Correction. This work reflects the opinion of the authors and does not reflect the views of the Connecticut Department of Correction.
FUNDING:
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Mental Health [grant number R01-MH106529; PI: LC Barry].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DECLARATION OF CONFLICTING INTERESTS: The authors have no conflicts of interest to declare.
References
- 1.Cipriani G, Danti S, Carlesi C, Di Fiorino M. Old and dangerous: Prison and dementia. Journal of Forensic and Legal Medicine. 2017;51:40–44. doi: 10.1016/j.jflm.2017.07.004 [DOI] [PubMed] [Google Scholar]
- 2.Barnert ES, Perry R, Morris RE. Juvenile Incarceration and Health. Academic Pediatrics. 2016;16(2). doi: 10.1016/j.acap.2015.09.004 [DOI] [PubMed] [Google Scholar]
- 3.Wangmo T, Handtke V, Bretschneider W, Elger BS. Improving the Health of Older Prisoners: Nutrition and Exercise in Correctional Institutions. Journal of Correctional Health Care. 2018;24(4). doi: 10.1177/1078345818793121 [DOI] [PubMed] [Google Scholar]
- 4.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. The Lancet. 2017;389(10077). doi: 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- 5.Greene M, Ahalt C, Stijacic-Cenzer I, Metzger L, Williams B. Older adults in jail: high rates and early onset of geriatric conditions. Health Justice. 2018;6(1):3. doi: 10.1186/s40352-018-0062-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerbs JJ, Jolley JM. A commentary on age segregation for older prisoners: philosophical and pragmatic considerations for correctional systems. Criminal Justice Review. 2009;34(119–139). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams BA, Stern MF, Mellow J, Safer M, Greifinger RB. Aging in correctional custody: setting a policy agenda for older prisoner health care. Am J Public Health. 2012;102(8):1475–1481. doi: 10.2105/AJPH.2012.300704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feczko A Dementia in the incarcerated elderly adult: Innovative solutions to promote quality care. Journal of the American Association of Nurse Practitioners. 2014;26(12):640–648. doi: 10.1002/2327-6924.12189 [DOI] [PubMed] [Google Scholar]
- 9.Ahalt C, Stijacic-Cenzer I, Miller BL, Rosen HJ, Barnes DE, Williams BA. Cognition and Incarceration: Cognitive impairment and its associated outcomes in older jail inmates. Journal of the American Geriatrics Society. Published online2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manly JJ, Byrd DA, Touradji P, Stem Y. Acculturation, reading level, and neuropsychological test performance among african american elders. Cultural Diversity: A Special Issue of Applied Neuropsychology. 2004;11(1):37–46. doi: 10.4324/9780203764497-5 [DOI] [PubMed] [Google Scholar]
- 11.Norman MA, Moore DJ, Taylor M, et al. Demographically corrected norms for African Americans and Caucasians on the Hopkins Verbal Learning Test-Revised, Brief Visuospatial Memory Test-Revised, Stroop Color and Word Test, and Wisconsin Card Sorting Test 64-Card Version. J Clin Exp Neuropsychol. 2011;33(7):793–804. doi: 10.1080/13803395.2011.559157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milani SA, Marsiske M, Cottler LB, Chen X, Striley CW. Optimal cutoffs for the Montreal Cognitive Assessment vary by race and ethnicity. Alzheimer’s and Dementia: Diagnosis, Assessment and Disease Monitoring. 2018;10:773–781. doi: 10.1016/j.dadm.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carson EA. Prisoners in 2019; U.S. Department of Justice, Bureau of Justice Statistics; October 2020, NCJ 255115. 2020; (October).
- 14.Zeng Z Jail Inmates in 2019; U.S. Department of Justice, Bureau of Justice Statistics; March 2021, NCJ 255608.; 2021.
- 15.Young MH, Justice J. Neuropsychological Functioning of Inmates Referred for Psychiatric Treatment. Archives of Clinical Neuropsychology. 1998;13(3). doi: 10.1016/S0887-6177(97)00032-2 [DOI] [PubMed] [Google Scholar]
- 16.Mann RE, Hanson RK, Thornton D. Assessing Risk for Sexual Recidivism: Some Proposals on the Nature of Psychologically Meaningful Risk Factors. Sexual Abuse: A Journal of Research and Treatment. 2010;22(2). doi: 10.1177/1079063210366039 [DOI] [PubMed] [Google Scholar]
- 17.Hancock M, Tapscott JL, Hoaken PNS. Role of executive dysfunction in predicting frequency and severity of violence. Aggressive Behavior. 2010;36(5):338–349. doi: 10.1002/ab.20353 [DOI] [PubMed] [Google Scholar]
- 18.Ross EH, Hoaken PNS. Executive Cognitive Functioning Abilities of Male First Time and Return Canadian Federal Inmates. Canadian Journal of Criminology and Criminal Justice. 2011;53(4). doi: 10.3138/cjccj.53.4.377 [DOI] [Google Scholar]
- 19.Barry LC, Coman E, Wakefield D, Trestman RL, Conwell Y, Steffens DC. Functional disability, depression, and suicidal ideation in older prisoners. Journal of Affective Disorders. 2020;266:366–373. doi: 10.1016/j.jad.2020.01.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi:JGS53221 [pii] 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 21.Smith T, Gildeh N, Holmes C. The Montreal Cognitive Assessment: Validity and Utility in a Memory Clinic Setting. The Canadian Journal of Psychiatry. 2007;52(5):329–332. [DOI] [PubMed] [Google Scholar]
- 22.Reitan RM. Validity of the Trail Making Test as an Indicator of Organic Brain Damage. Perceptual and Motor Skills. 1958;8(3):271–276. [Google Scholar]
- 23.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82(2):231–235. [DOI] [PubMed] [Google Scholar]
- 24.Connecticut Department of Correction; https://portal.ct.gov/-/media/DOC/Pdf/MonthlyStat/Stat201801.pdf, Accessed onMay 2 2021. Average Confined Inmate Population and Legal Status.; 2017.
- 25.Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: A clinical review. JAMA - Journal of the American Medical Association. 2014;312(23):2551–2561. doi: 10.1001/jama.2014.13806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckner JC, Mezzacappa E, Beardslee WR. Characteristics of resilient youths living in poverty: The role of self-regulatory processes. Development and Psychopathology. 2003;15(1):139–162. doi: 10.1017/S0954579403000087 [DOI] [PubMed] [Google Scholar]
- 27.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology. 2016;35(4):407–411. doi: 10.1037/hea0000242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rossetti HC, Lacritz LH, Hynan LS, Cullum CM, van Wright A, Weiner MF. Montreal Cognitive Assessment Performance among Community-Dwelling African Americans. Arch Clin Neuropsychol. 2017;32(2):238–244. doi: 10.1093/arclin/acw095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karr JE, Garcia-Barrera MA, Holdnack JA, Iverson GL. Advanced clinical interpretation of the Delis-Kaplan Executive Function System: multivariate base rates of low scores. Clinical Neuropsychologist. 2018;32(1):42–53. doi: 10.1080/13854046.2017.1334828 [DOI] [PubMed] [Google Scholar]
- 30.Carlson MC, Xue QL, Zhou J, Fried LP. Executive decline and dysfunction precedes declines in memory: The Women’s Health and Aging Study II. Journals of Gerontology - Series A Biological Sciences and Medical Sciences. 2009;64(1):110–117. doi: 10.1093/gerona/gln008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Binder LM, Iverson GL, Brooks BL. To err is human: “abnormal” Neuropsychological scores and variability are common in healthy adults. Archives of Clinical Neuropsychology. 2009;24(1):31–46. doi: 10.1093/arclin/acn001 [DOI] [PubMed] [Google Scholar]
- 32.Werry AE, Daniel M, Bergström B. Group differences in normal neuropsychological test performance for older non-Hispanic White and Black/African American adults. Neuropsychology. 2019;33(8). doi: 10.1037/neu0000579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogel M, Porter LC. Toward a Demographic Understanding of Incarceration Disparities: Race, Ethnicity, and Age Structure. Journal of Quantitative Criminology. 2016;32(4):515–530. doi: 10.1007/s10940-015-9265-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedman NP, Miyake A, Altamirano LJ, et al. Stability and change in executive function abilities from late adolescence to early adulthood: A longitudinal twin study. Developmental Psychology. 2016;52(2):326–340. doi: 10.1037/dev0000075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mendez MF. What is the Relationship of Traumatic Brain Injury to Dementia? Journal of Alzheimer’s Disease. 2017;57:667–681. doi: 10.3233/JAD-161002 [DOI] [PubMed] [Google Scholar]
- 36.Edwards F, Lee H, Esposito M. Risk of being killed by police use of force in the United States by age, race–ethnicity, and sex. Proceedings of the National Academy of Sciences of the United States of America. 2019;116(34):16793–16798. doi: 10.1073/pnas.1821204116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cislo AM, Trestman R. Challenges and solutions for conducting research in correctional settings: the U.S. experience. Int J Law Psychiatry. 2013;36(3–4):304–310. doi: 10.1016/j.ijlp.2013.04.002 [DOI] [PubMed] [Google Scholar]


