Abstract
Objectives
The aim of this study was to identify the predictive factors for suboptimal result in side branch (SB) in chronic total occlusion (CTO) bifurcation lesions and clinical outcomes of patients with suboptimal result in SB.
Background
There is little evidence on the optimal strategy for bifurcation lesions in CTO.
Methods
We retrospectively reviewed 314 consecutive bifurcation lesions in CTO with SB ≥ 2.5 mm in 3 hospitals from March 2010 to June 2018. Patients were divided into the two groups based on the suboptimal SB treatment (SST) and optimal SB treatment (OST) groups. The baseline characteristics, procedural and clinical outcomes were compared between the two groups. This study also evaluated the predictors of suboptimal result in SB.
Results
Suboptimal result in SB occurred in 47 cases. Presence of stenosis in SB, bifurcations located within the occluded segment and sub-intimal tracking at SB ostium was an independent predictor of suboptimal result in SB. The cumulative incidence of target lesion revascularization (TLR) in all lesions was not significantly different between the two groups, however, TLR in right coronary artery (RCA) was significantly higher in the SST group. In the Cox regression analysis, suboptimal result in SB in RCA and sub-intimal tracking were independent predictors of TLR for MB. In patients with bifurcations located within the occluded segment, usage of two-stent technique was significantly lower in the SST group.
Conclusions
Meticulous procedures are required for SB preservation to improve not only SB prognosis but also MB, especially in RCA.
Keywords: Bifurcation, Coronary chronic total occlusion, Side branch
Abbreviations: CTO, chronic total occlusion; IVUS, intravascular ultrasound; MB, main branch; PCI, percutaneous coronary intervention; SB, side branch; TIMI, Thrombolysis In Myocardial Infarction; TLR, target lesion revascularization
1. Introduction
Percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) is a well-accepted revascularization procedure and the hybrid algorithm for CTO-PCI has been associated with increased success rate [1], [2], [3], [4], [5], [6]. However, CTO-PCI still has a low success rate compared to non-CTO lesions. CTO lesions usually extend from side branch (SB) to SB histopathologically [7]. It means that many CTO lesions include bifurcation lesions, indicating the demand of strategical management of bifurcation lesion when treating the CTO. This presence of bifurcation lesions in CTO may increase the difficulty of its treatment. Basically, provisional stenting strategy is recommended for the treatment of bifurcation lesion. Randomized trials have demonstrated the advantages of provisional stenting compared with two-stent technique for non-CTO bifurcation lesions [8], [9], [10], [11]. Besides SB occlusion after provisional stenting for non-CTO bifurcation lesions was one of the serious complications, the independent predictors of SB occlusion were SB ostial disease, proximal main vessel stenosis, SB lesion length, and acute coronary syndrome [12], [13]. Nonetheless, the reports concerning the strategy for the treatment of bifurcation involved in CTO lesions are still limited. In addition, it is currently uncertain what the predictive factors are of suboptimal result in SB in CTO bifurcation lesions. The aim of this study was to identify the predictive factors for suboptimal result in SB in CTO bifurcation lesions and clinical outcomes of patients with suboptimal result in SB.
2. Methods
2.1. Patient population and study design
From January 2010 to March 2018, consecutive patients who underwent CTO-PCI were extracted from the database at three centers (Toyohashi Heart Center, Nagoya Heart Center, Gifu Heart Center). Data was collected retrospectively from 1649 consecutively treated CTO lesions. Initially, this study excluded failed cases (n = 141), cases with missing data from follow up after PCI (n = 301), and no bifurcation lesions (n = 893). Finally, we retrospectively analyzed data from 314 CTO lesions which had SB ≥ 2.5 mm in diameter, located either at the proximal or distal end of the CTO or within the occluded segment. The flow chart of the study is Fig. 1. The protocol was approved by the ethics committees of each participating center. Patients were divided into the two groups based on the suboptimal SB treatment (SST) (n = 47) and the optimal SB treatment(OST) groups (n = 267). SST was defined that the final Thrombolysis In Myocardial Infarction (TIMI) flow of SB less than grade 3. Coronary angiogram was analyzed by 2 independent observers who categorized the patients into SST group or OST group. The treatment strategy was selected by the operators’ discretion. All procedures were performed under intravascular ultrasound (IVUS) guidance. Heparin was administered to maintain an activated clotting time >300 sec during the procedure. All the stents deployed were drug-eluting stents (DES). All patients were pre-treated with dual antiplatelet therapy and were prescribed lifelong aspirin (100 mg/daily). The duration of dual antiplatelet therapy (DAPT) was determined by the operator, but DAPT was continued at least 6 months after CTO-PCI.
Fig. 1.
Inclusion flow diagram of study population.
2.2. Definitions
CTO was defined as a coronary obstruction with TIMI flow grade 0 with an estimated duration of more than 3 months [14]. We assessed bifurcation lesions according to the Medina classification [15]. SB was defined as a vessel with a diameter ≥ 2.5 mm by visual angiographic estimation in the 15-segment American Heart Association classification. Bifurcation lesions were divided into 3 types regarding the SB location: (a) proximal, which was defined that SB presence was within 3 mm proximally from the beginning of CTO, (b) occluded segment in which bifurcation lesions were within the occluded segment and (c) distal, which was also defined that SB presence was within 3 mm distally from the end of CTO. The SB location was evaluated according to collateral vessels flowing into the SB detected by coronary arteriography or coronary computed tomography angiography. Carina shift or plaque shift was defined as aggravation of SB ostial stenosis after main branch (MB) stent implantation angiographically. We checked IVUS recordings in all cases to evaluate the wire tracking patterns at SB ostium. The IVUS catheter was advanced into the target lesion after wiring or ballooning and an automatic or manual pullback was performed. Wire tracking patterns at SB ostium were categorized as intimal or sub-intimal tracking based on the IVUS findings. IVUS images were analyzed by 2 independent observers. Technical bifurcation success was defined as a recovery of a final TIMI flow grade 3 for both branches. Clinical follow-up was performed with coronary computed-tomography angiography or coronary angiography at approximately 1 year after CTO-PCI. Clinical outcomes were evaluated by cardiac death, myocardial infarction (MI), and clinically driven target lesion revascularization (TLR). Clinically driven TLR was defined as any repeat PCI with ischemic symptoms.
2.3. Statistical analysis
All statistical analyses were performed using IBM SPSS statistics 22 (SPSS, Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± standard deviation (SD) or median and interquartile range (IQR), depending on variable distribution. Categorical data is expressed as percentages of the total. Comparisons between the two groups were made using chi-squared tests for categorical covariates, and one-way analysis of variance and the Mann–Whitney U test for continuous covariates, depending on the variable’s distribution. The Kaplan–Meier method was used to estimate the cumulative incidence of differences between the two groups and each was assessed using the log-rank test. A univariate logistic regression analysis was performed to obtain the odds ratio (OR) for prediction of suboptimal result in SB for appropriate clinical variables. A Cox regression analysis was also performed to calculate the hazard ratio (HR) for TLR. Thereafter, a multivariate analysis was performed using the variables with p-values < 0.05 in the univariate analysis to examine their independent association with suboptimal result in SB and TLR. Kaplan-Meier methods were used to estimate the cumulative incidence of TLR in the two groups. Differences in survival in each group were compared with the log-rank test. All statistical tests were 2-sided, and p-values < 0.05 were considered statistically significant.
3. Results
3.1. Baseline and procedural patient characteristics
Baseline characteristics are presented in Table 1. Of the 314 lesions included in this study, 15.0% (n = 47) was in the SST group and 85.0% (n = 267) was in the OST group. There was no significant difference in baseline clinical characteristics between the two groups. In angiographic characteristics, although there was no difference in the distribution of target vessel and Medina classification, the SB location was significantly different between the two groups. In approximately half of the SST group, SB originated from the occluded segment and presence of a stenosis in SB was also more frequently observed in the SST group (78.7% vs 44.6%; p < 0.001). Procedural patient characteristics are described in Table 2. Recanalization techniques were similar between the two groups. Sub-intimal tracking at SB ostium was also observed more frequently in the SST group than the OST group (68.1% vs. 21.3%; p < 0.001). There was no significant difference in stenting technique between the two groups. Suboptimal result in SB was significantly higher in bifurcation lesions with SB dissection (31.9% vs. 8.6%; p < 0.001) or carina shift / plaque shift (14.9% vs. 5.6%; p < 0.05).
Table 1.
Baseline patient characteristics.
| Overall | Suboptimal side branch treatment | Optimal side branch treatment | ||
|---|---|---|---|---|
| Patients, n | n = 314 | n = 47 | n = 267 | p value |
| Baseline clinical characteristics | ||||
| Age, years | 69.2 ± 9.5 | 68.9 ± 9.2 | 69.5 ± 10.2 | 0.89 |
| Male, n | 267 (85.0%) | 38 (80.9%) | 229 (85.8%) | 0.33 |
| BMI, kg/m2 | 24.6 ± 12.4 | 23.9 ± 13.0 | 24.9 ± 13.2 | 0.85 |
| Diabetes mellitus, n | 45 (14.3%) | 6 (12.8%) | 39 (14.6%) | 0.21 |
| Hypertension, n | 122 (38.9%) | 19 (40.4%) | 103 (38.6%) | 0.22 |
| Dyslipidemia, n | 116 (36.9%) | 15 (31.9%) | 101 (37.8%) | 0.78 |
| CKD, n | 122 (38.9%) | 16 (34.0%) | 106 (39.7%) | 0.11 |
| Hemodialysis, n | 28 (8.9%) | 5 (10.6%) | 23 (8.6%) | 0.13 |
| Current smoker, n | 22 (7.0%) | 5 (10.6%) | 17 (6.3%) | 0.20 |
| Previous PCI, n | 31 (9.9%) | 4 (8.5%) | 27 (10.1%) | 0.38 |
| Previous CABG, n | 19 (6.1%) | 4 (8.5%) | 15 (5.6%) | 0.41 |
| Previous MI, n | 85 (27.1%) | 13 (27.7%) | 72 (27.0%) | 0.45 |
| Occlusion location | ||||
| Left anterior descending | 146 (46.5%) | 25 (53.2%) | 121 (45.3%) | 0.25 |
| Left circumflex | 82 (26.1%) | 9 (19.1%) | 73 (27.3%) | |
| Right coronary artery | 86 (27.3%) | 13 (27.7%) | 73 (27.3%) | |
| Medina classification | ||||
| 1, 1, 1 | 110 (35.0%) | 26 (55.3%) | 84 (31.5%) | <0.05 |
| 1, 0, 1 | 19 (6.1%) | 5 (10.6%) | 14 (5.2%) | |
| 0, 1, 1 | 27 (8.6%) | 6 (12.8%) | 21 (7.9%) | |
| 1, 1, 0 | 38 (12.1%) | 4 (8.5%) | 34 (12.7%) | |
| 1, 0, 0 | 91 (29.0%) | 4 (8.5%) | 87 (32.6%) | |
| 0, 1, 0 | 29 (9.2%) | 2 (4.3%) | 27 (10.1%) | |
| Presence of stenosis in the side branch | 156 (49.7%) | 37 (78.7%) | 119 (44.6%) | <0.001 |
| Side branch location | ||||
| Proximal | 144 (45.9%) | 14 (29.8%) | 130 (48.9%) | <0.05 |
| Occluded segment | 82 (26.1%) | 22 (46.8%) | 60 (22.5%) | |
| Distal | 88 (28.0%) | 11 (23.4%) | 77 (28.9%) |
Values are numbers (%), mean ± SD. BMI, body mass index; CABG, coronary artery bypass graft; CKD, chronic kidney disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Table 2.
Procedural patient characteristics and clinical outcome.
| Overall | Suboptimal side branch treatment | Optimal side branch treatment | ||
|---|---|---|---|---|
| Patients, n | n = 314 | n = 47 | n = 267 | p value |
| CTO strategy | ||||
| Antegrade technique | ||||
| AWE, n | 204 (64.9%) | 12 (25.5%) | 192 (71.9%) | 0.11 |
| ADR, n | 4 (1.3%) | 1 (2.1%) | 3 (1.1%) | |
| Retrograde technique | ||||
| RWE, n | 21 (6.9%) | 3 (6.3%) | 18 (6.7%) | <0.05 |
| RDR, n | 85 (27.1%) | 31 (66.0%) | 54 (20.2%) | |
| Wire tracking patterns at side branch ostium | ||||
| Intimal tracking, n | 225 (71.7%) | 15 (31.9%) | 210 (78.7%) | <0.001 |
| Sub-intimal tracking, n | 89 (28.3%) | 32 (68.1%) | 57 (21.3%) | |
| Stenting method | ||||
| 1. One-stent technique, n | 286 (91.1%) | 44 (93.6%) | 242 (90.6%) | 0.45 |
| Kissing balloon technique, n | 165 (52.5%) | 24 (51.1%) | 141 (52.8%) | 0.88 |
| 2. Two-stent technique, n | 28 (8.9%) | 3 (6.4%) | 25 (9.4%) | 0.39 |
| Main vessel | ||||
| Stent length, mm | 24.6 ± 6.9 | 23.4 ± 6.7 | 24.3 ± 6.9 | 0.64 |
| Stent diameter, mm | 3.1 ± 0.3 | 3.4 ± 0.4 | 3.2 ± 0.3 | 0.31 |
| Side branch dissection n | 38 (12.1%) | 15 (31.9%) | 23 (8.6%) | <0.001 |
| Carina shift / plaque shift, n | 22 (7.0%) | 7 (14.9%) | 15 (5.6%) | <0.05 |
| Hemodynamic support with IABP, n | 18 (5.7%) | 3 (6.4%) | 15 (5.6%) | 0.81 |
| Clinical outcome on follow-up | ||||
| Cardiac death within 1 year, n | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – |
| Myocardial infarction within 1 year, n | 1 (0.3%) | 0 (0.0%) | 1 (0.4%) | 0.47 |
| TLR for main branch within 1 year, n | 30 (9.6%) | 6 (12.8%) | 24 (9.0%) | 0.65 |
| Left anterior descending | 11(7.6%) | 2/25 (8.0%) | 9/121 (7.4%) | 0.64 |
| Left circumflex | 9 (11.0%) | 1/9 (11.1%) | 8/73 (11.0%) | 0.76 |
| Right coronary artery | 10 (11.6%) | 3/13 (23.1%) | 7/73 (9.6%) | 0.04 |
| TLR for side branch within 1 year, n | 12 (3.8%) | 7 (14.9%) | 5 (1.9%) | <0.001 |
| Left anterior descending | 7 (4.8%) | 4/25 (16.0%) | 3/121 (2.5%) | <0.001 |
| Left circumflex | 2 (2.4%) | 1/9 (11.1%) | 1/73 (1.4%) | <0.001 |
| Right coronary artery | 3 (3.5%) | 2/13 (15.4%) | 1/73 (1.4%) | <0.001 |
Values are numbers (%), mean ± SD. ADR, antegrade dissection reentry; AWE, antegrade wire escalation; CTO, chronic total occlusion; IABP: Intra‑aortic balloon pump; MB, main branch; RDR, retrograde dissection reentry; RWE, retrograde wire escalation; SB, side branch; TLR, target lesion revascularization.
3.2. Predictive factors of suboptimal result in side branch
The logistic regression analysis of the association between suboptimal result in SB and clinical findings is presented in Table 3. In the univariate analysis, hemodialysis, presence of stenosis in the SB, retrograde technique, and sub-intimal tracking at SB ostium were associated with a high incidence of suboptimal result in SB. The multivariate regression analysis indicated that the presence of a stenosis in SB (OR: 1.44, 95% CI; 1.09–1.90: p = 0.011), bifurcations located within the occluded segment (OR: 1.49, 95% CI; 1.06–2.09: p = 0.022) and sub-intimal tracking at SB ostium (OR: 2.27, 95% CI; 1.39–3.58: p < 0.001) were independent predictors of suboptimal result in SB. We also performed a sub-analysis of 82 bifurcation lesions located within the occluded segment in this study (Supplemental Table 1). This lesion type was found in approximately 25% of our subjects. Two-stent technique significantly reduced suboptimal result in SB compared to one-stent technique in this group (18.2% vs. 35.0%; p < 0.05).
Table 3.
Univariate and Multivariate regression analysis for the association between suboptimal result in side branch and clinical findings.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Explanatory variables | OR | 95% CI | p value | OR | 95% CI | p value |
| Adjusting factors | ||||||
| Hemodialysis | 2.07 | 1.17–3.63 | 0.012 | 1.26 | 0.67–2.39 | 0.48 |
| Presence of stenosis in the side branch | 2.88 | 2.28–3.63 | <0.001 | 1.44 | 1.09–1.90 | 0.011 |
| Bifurcations located within the occluded segment | 1.66 | 1.24–2.23 | 0.001 | 1.49 | 1.06–2.09 | 0.022 |
| Retrograde technique | 1.51 | 1.06–2.14 | 0.02 | 1.19 | 0.85–1.68 | 0.31 |
| Sub-intimal tracking at SB ostium | 2.73 | 1.63–4.45 | <0.001 | 2.27 | 1.39–3.58 | <0.001 |
OR, odds ratio; other abbreviations as in Table 1.
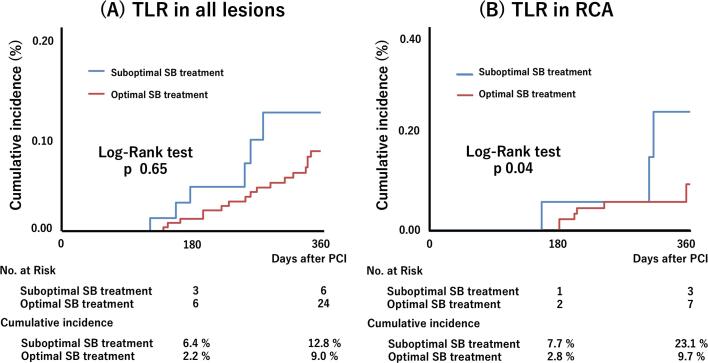
3.3. Results at follow-up
Patients were clinically evaluated with a median follow-up duration of 444 days (interquartile range: 222–494 days). The follow-up findings are presented in Table 2. There were no significant differences in cardiac death, myocardial infarction, TLR between the two groups. Kaplan–Meier analysis of cumulative 1-year incidence of TLR is presented in Fig. 2. Although it didn’t show significantly different between the two groups (Fig. 2A, 12.8% vs. 9.0%; p 0.65) in all lesions, the probability of cumulative 1-year incidence of TLR in right coronary artery (RCA) was significantly higher in the SST group (Fig. 2B, 23.1% vs. 9.7%; p 0.04). There was no difference in incidence of TLR in other vessels except for RCA (Table 2). Moreover, suboptimal result in SB in RCA and sub-intimal tracking at SB ostium were independent predictors of TLR for MB in the Cox regression analysis for the association between TLR for MB and clinical findings (Table 4).
Fig. 2.
Kaplan–Meier curve showing cumulative incidence of (A) target lesion revascularization in all lesions and (B) target lesion revascularization in right coronary artery in the suboptimal side branch treatment and optimal side branch treatment groups.
Table 4.
Cox regression analysis for the predictors of target lesion revascularization for main branch.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Explanatory variables | HR | 95% CI | p value | HR | 95% CI | p value |
| Adjusting factors | ||||||
| CKD | 1.37 | 0.31–6.11 | 0.68 | |||
| Suboptimal result in side branch | ||||||
| in the left anterior descending | 1.02 | 0.74–1.40 | 0.92 | |||
| in the left circumflex | 1.08 | 0.93–1.26 | 0.32 | |||
| in the right coronary artery | 1.15 | 1.01–1.30 | 0.03 | 1.12 | 1.00–1.25 | 0.04 |
| Presence of stenosis in the side branch | 1.62 | 1.02–2.59 | 0.04 | 1.12 | 0.79–1.58 | 0.54 |
| Bifurcations located within the occluded segment | 1.13 | 0.47–2.88 | 0.79 | |||
| Retrograde technique | 1.12 | 0.58–2.19 | 0.73 | |||
| Sub-intimal tracking at SB ostium | 1.41 | 1.05–1.89 | 0.02 | 1.32 | 1.01–1.72 | 0.04 |
| Two-stent technique | 0.25 | 0.03–2.20 | 0.21 | |||
| Carina shift / plaque shift | 1.26 | 0.92–1.74 | 0.15 | |||
4. Discussion
In this study, we demonstrated the importance of preserving the SB in CTO-PCI to avoid adverse events. Although there are many papers that analyze the outcome of CTO lesions or bifurcation lesions respectively, there are only a few publications that are reporting comprehensively about the treatment of bifurcation lesions in CTO. To the best of our knowledge, this is the first report of a detailed evaluation about the relationship between the management of bifurcation lesions in CTO and clinical outcome.
Histopathologically, CTO lesions usually extend from SB to SB [7]. So, we not only need CTO procedure but also the appropriate management of bifurcation lesions in the treatment of CTO’s, because many CTO lesions include bifurcation lesions.
Currently, the best strategy in non-CTO bifurcation lesions have been widely reported, the provisional approach is regarded as the standard technique for this lesion type [8], [9], [10], [11]. However, the provisional approach may lead to SB occlusion after stenting in the MB, which is the main reason for shifting to a two-stent procedure. The relationship between SB occlusion and adverse clinical outcomes has been reported previously [13]. The hybrid algorithm has been associated with increased success rates in CTO treatment [16], [17]. In this algorithm, dissection re-entry techniques (antegrade or retrograde), which use the sub-intimal space to cross the lesion, are among the common strategies. However, there is a clinical concern that the induced dissection due to sub-intimal tracking may affect suboptimal result in SB. It was recently reported that sub-intimal tracking was higher in the retrograde approach (24.2% vs. 12.3%; p 0.10) and that sub-intimal tracking frequently caused periprocedural myocardial infarction [18], [19]. Although the follow up evaluation of the SB was uncertain in these studies, the SB condition after the CTO procedure may relate to some adverse events.
In the present study, we focused on the relationship between SB fate and clinical outcome of the CTO treatment. We performed IVUS in 314 lesions and evaluated intimal or sub-intimal tracking at SB ostium. Sub-intimal tracking was observed in 28.3 % of all lesions, which was a strong predictor of suboptimal result in SB. Although there were no significant differences between the two groups when considering TLR in all lesion in this study, TLR in RCA was significantly higher in the SST group. In addition, suboptimal result in SB in RCA and sub-intimal tracking at SB ostium negatively affect TLR for MB of RCA. Unlike the left coronary artery, RCA has significant and sizable bifurcation branches such as the posterior descending branch and the atrioventricular node branch distally. Due to these anatomical differences, distal blood flow restriction may occur when suboptimal result in SB occurred in RCA, resulting in TLR for MB. Also, it was reported that sub-intimal tracking and re‐entry procedure cause high rates of MB restenosis [20]. SB occlusions as result of sub-intimal tracking may cause limited distal blood outflow and predisposing a higher TLR risk. Therefore, we should make every effort to perform CTO recanalization by intimal tracking as much as possible, especially for bifurcation lesions with sizable SB to avoid the reported adverse events.
Furthermore, we found that bifurcation lesions located within the occluded segment were frequently observed in the SST group. As a result of sub-analysis for 82 bifurcation lesions located within the occluded segment in this study, it was found that two-stent technique significantly reduced suboptimal result in SB compared to one-stent technique in this group (18.2% vs. 35.0%; p < 0.05). Another study has reported that 8% of patients with CTO bifurcation lesions were treated with a two-stent technique [21], the frequency of the two-stent technique for CTO bifurcation lesions in our study was similar. Recent reports prove that there were no differences in procedural or mid-term clinical outcomes between the one-stent and two-stent technique for the treatment of CTO bifurcation lesions [22]. It was reported that the mini-crush technique for CTO bifurcation lesions located within the occluded segment, has a higher major adverse cardiac and cerebrovascular events-free survival at 1 year than T-provisional stenting [23]. Although the two-stent technique was better to preserve SB patency in bifurcation within the occluded segment in our study, optimal stent strategy for CTO bifurcation lesions is still controversial. We may need to choose different stent techniques depending on SB position in CTO or wire position at SB ostium. To date the impact of suboptimal result in SB on MB is uncertain, and therefore further investigation is highly desired.
5. Limitations
Several limitations should be addressed in this study. 1) This study is a retrospective and non-randomized design. 2) The angiographic follow-up rate was relatively low. 3) The number of patients enrolled was limited. 4) Multiple IVUS systems were used, and patients with manual pullback were included, therefore, the length of sub-intimal tracking could not be measured. 5) The strategy and technical success of bifurcation lesions involved in CTO treatment is dependent on the operator’s experience. 6) Strategies for SB preservation have not been sufficiently informed from coronary angiogram, because we retrospectively analyzed data from CTO lesions.
6. Conclusions
The presented study demonstrated that sub-intimal tracking at the SB ostium as a cause of suboptimal result in SB is the significant predictors of TLR in the treatment of CTO bifurcation. In particular, since suboptimal result in SB in RCA may lead to TLR for MB, it is clinically important to keep the wire intraplaque to preserve SB for achieving technical bifurcation success. We need to pay special attention and apply sophisticated wire manipulation for the treatment of CTO bifurcation lesions, especially in RCA.
7. Permissions information
The authors do hereby declare that all illustrations and figures in the manuscript are entirely original and do not require reprint permission.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The authors thank Akira Murata, MD, Yoshiaki Kawase, MD, Munenori Okubo, MD, Yoriyasu Suzuki, MD, Tatsuya Ito, MD, Hitoshi Matsuo, MD, Takahiko Suzuki, MD, for patient recruitment.
Sources of Funding
None.
Disclosures
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2021.100873.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Surmely J.F., Tsuchikane E., Katoh O., Nishida Y., Nakayama M., Nakamura S., Oida A., Hattori E., Suzuki T. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J. Invasive Cardiol. 2006;18:334–338. [PubMed] [Google Scholar]
- 2.Surmely J.-F., Katoh O., Tsuchikane E., Nasu K., Suzuki T. Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc. Interv. 2007;69(6):826–832. doi: 10.1002/ccd.20816. [DOI] [PubMed] [Google Scholar]
- 3.Tsuchikane E., Katoh O., Kimura M., Nasu K., Kinoshita Y., Suzuki T. The first clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. J. Am. Coll. Cardiol. Intv. 2010;3(2):165–171. doi: 10.1016/j.jcin.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Christopoulos G., Menon R.V., Karmpaliotis D., Alaswad K., Lombardi W., Grantham A., Patel V.G., Rangan B.V., Kotsia A.P., Lembo N., Kandzari D., Carlson H., Garcia S., Banerjee S., Thompson C.A., Brilakis E.S. The efficacy and safety of the “hybrid” approach to coronary chronic total occlusions: insights from a contemporary multicenter US registry and comparison with prior studies. J. Invasive Cardiol. 2014;26(9):427–432. [PMC free article] [PubMed] [Google Scholar]
- 5.Galassi A.R., Sianos G., Werner G.S., Escaned J., Tomasello S.D., Boukhris M., Castaing M., Büttner J.H., Bufe A., Kalnins A., Spratt J.C., Garbo R., Hildick-Smith D., Elhadad S., Gagnor A., Lauer B., Bryniarski L., Christiansen E.H., Thuesen L., Meyer-Geßner M., Goktekin O., Carlino M., Louvard Y., Lefèvre T., Lismanis A., Gelev V.L., Serra A., Marzà F., Di Mario C., Reifart N., Euro CTO Club Retrograde recanalization of chronic total occlusions in Europe: procedural, in-hospital, and long-term outcomes from the multicenter ERCTO registry. J. Am. Coll. Cardiol. 2015;65(22):2388–2400. doi: 10.1016/j.jacc.2015.03.566. [DOI] [PubMed] [Google Scholar]
- 6.Wilson W.M., Walsh S.J., Yan A.T., Hanratty C.G., Bagnall A.J., Egred M., Smith E., Oldroyd K.G., McEntegart M., Irving J., Strange J., Douglas H., Spratt J.C. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102(18):1486–1493. doi: 10.1136/heartjnl-2015-308891. [DOI] [PubMed] [Google Scholar]
- 7.Srivatsa S.S., Edwards W.D., Boos C.M., Grill D.E., Sangiorgi G.M., Garratt K.N., Schwartz R.S., Holmes D.R., Jr. Histologic correlates of angiographic chronic total coronary artery occlusions: influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J. Am. Coll. Cardiol. 1997;29(5):955–963. doi: 10.1016/s0735-1097(97)00035-1. [DOI] [PubMed] [Google Scholar]
- 8.Gao X.-F., Zhang Y.-J., Tian N.-L., Wu W., Li M.-H., Bourantas C.V., Jiang X.-M., Wang Z.-M., Li B., Mao W.-X., Zhang J.-J., Chen S.-L. Stenting strategy for coronary artery bifurcation with drug-eluting stents: a meta-analysis of nine randomised trials and systematic review. EuroIntervention. 2014;10(5):561–569. doi: 10.4244/EIJY14M06_06. [DOI] [PubMed] [Google Scholar]
- 9.Zhang F., Dong L., Ge J. Simple versus complex stenting strategy for coronary artery bifurcation lesions in the drug-eluting stent era: a meta-analysis of randomised trials. Heart. 2009;95(20):1676–1681. doi: 10.1136/hrt.2009.168641. [DOI] [PubMed] [Google Scholar]
- 10.Hildick-Smith D., Behan M.W., Lassen J.F., Chieffo A., Lefèvre T., Stankovic G., Burzotta F., Pan M., Ferenc M., Bennett L., Hovasse T., Spence M.S., Oldroyd K., Brunel P., Carrie D., Baumbach A., Maeng M., Skipper N., Louvard Y. The EBC TWO Study (European Bifurcation Coronary TWO): a randomized comparison of provisional T-stenting versus a systematic 2 stent culotte strategy in large caliber true bifurcations. Circ Cardiovasc Interv. 2016;9(9) doi: 10.1161/CIRCINTERVENTIONS.115.003643. [DOI] [PubMed] [Google Scholar]
- 11.Milasinovic D., Wijns W., Ntsekhe M., Hellig F., Mohamed A., Stankovic G. Step-by-step manual for planning and performing bifurcation PCI: a resource-tailored approach. EuroIntervention. 2018;13(15):e1804–e1811. doi: 10.4244/EIJ-D-17-00580. [DOI] [PubMed] [Google Scholar]
- 12.Aliabadi D., Tilli F.V., Bowers T.R., Benzuly K.H., Safian R.D., Goldstein J.A., Grines C.L., O'Neill W.W. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am. J. Cardiol. 1997;80(8):994–997. doi: 10.1016/s0002-9149(97)00591-2. [DOI] [PubMed] [Google Scholar]
- 13.Hahn J.-Y., Chun W.J., Kim J.-H., Song Y.B., Oh J.H., Koo B.-K., Rha S.W., Yu C.W., Park J.-S., Jeong J.-O., Choi S.-H., Choi J.-H., Jeong M.-H., Yoon J.H., Jang Y., Tahk S.-J., Kim H.-S., Gwon H.-C. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II registry (COronary BIfurcation Stenting) J. Am. Coll. Cardiol. 2013;62(18):1654–1659. doi: 10.1016/j.jacc.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 14.Sianos G., Werner G.S., Galassi A.R., Papafaklis M.I., Escaned J., Hildick-Smith D., Christiansen E.H., Gershlick A., Carlino M., Karlas A., Konstantinidis N.V., Tomasello S.D., Di Mario C., Reifart N., EuroCTO Club Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;2012(8):139–145. doi: 10.4244/EIJV8I1A21. [DOI] [PubMed] [Google Scholar]
- 15.Medina A., Suárez de Lezo J., Pan M. A new classification of coronary bifurcation lesions. Rev. Esp. Cardiol. 2006;59(183) [PubMed] [Google Scholar]
- 16.Maeremans J., Walsh S., Knaapen P., Spratt J.C., Avran A., Hanratty C.G., Faurie B., Agostoni P., Bressollette E., Kayaert P., Bagnall A.J., Egred M., Smith D., Chase A., McEntegart M.B., Smith W.H., Harcombe A., Kelly P., Irving J., Smith E.J., Strange J.W., Dens J. The hybrid algorithm for treating chronic total occlusions in Europe: the RECHARGE registry. J. Am. Coll. Cardiol. 2016;68(18):1958–1970. doi: 10.1016/j.jacc.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 17.Harding Scott A., Wu Eugene B., Lo Sidney, Lim Soo Teik, Ge Lei, Chen Ji-Yan, Quan Jie, Lee Seung-Whan, Kao Hsien-Li, Tsuchikane Etsuo. A new algorithm for crossing chronic total occlusions from the Asia Pacific Chronic Total Occlusion Club. JACC Cardiovasc. Interv. 2017;10(21):2135–2143. doi: 10.1016/j.jcin.2017.06.071. [DOI] [PubMed] [Google Scholar]
- 18.Muramatsu Toshiya, Tsuchikane Etsuo, Oikawa Yuji, Otsuji Satoru, Fujita Tsutomu, Ochiai Masahiko, Kawasaki Tomohiro, Abe Mitsunori, Sakurada Masami, Kishi Koichi. Incidence and impact on midterm outcome of controlled subintimal tracking in patients with successful recanalisation of chronic total occlusions: J-PROCTOR registry. EuroIntervention. 2014;10(6):681–688. doi: 10.4244/EIJV10I6A119. [DOI] [PubMed] [Google Scholar]
- 19.Song Lei, Maehara Akiko, Finn Matthew T., Kalra Sanjog, Moses Jeffrey W., Parikh Manish A., Kirtane Ajay J., Collins Michael B., Nazif Tamim M., Fall Khady N., Hatem Raja, Liao Ming, Kim Tiffany, Green Philip, Ali Ziad A., Batres Candido, Leon Martin B., Mintz Gary S., Karmpaliotis Dimitri. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions and association with procedural outcomes. JACC Cardiovasc Interv. 2017;10(10):1011–1021. doi: 10.1016/j.jcin.2017.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carlino M., Godino C., Latib A., Moses J.W., Colombo A. Subintimal tracking and re-entry technique with contrast guidance: a safer approach. Catheter Cardiovasc. Interv. 2008;72(6):790–796. doi: 10.1002/ccd.21699. [DOI] [PubMed] [Google Scholar]
- 21.Ojeda S., Pan M., Gutiérrez A., Romero M., Chavarría J., de Lezo J.S., Mazuelos F., Pardo L., Hidalgo F., Carrasco F., Segura J., Durán E., Ferreiro C., Sánchez J.J., Rodríguez S., Oneto J., de Lezo J.S. Bifurcation lesions involved in the recanalization process of coronary chronic total occlusions: incidence, treatment and clinical implications. Int. J. Cardiol. 2017;1(230):432–438. doi: 10.1016/j.ijcard.2016.12.088. [DOI] [PubMed] [Google Scholar]
- 22.Baeza Garzón F., Pan Álvarez-Ossorio M., Romero Moreno M.Á., Martín Palanco V., Herrera Arroyo C., Suárez de Lezo Cruz Conde J. One versus 2-stent strategy for the treatment of bifurcation lesions in the context of a coronary chronic total occlusion. A multicenter registry. Rev. Esp. Cardiol. (Engl. Ed.) 2018;71(6):432–439. doi: 10.1016/j.rec.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 23.Baystrukov V.I., Kretov E.I., Boukhris M., Osiev A.G., Grazhdankin I.O., Biryukov A.V., Najjar H., Verin V.V., Zubarev D.D., Naryshkin I.A., Bogachev-Prokophiev A.V., Mashayekhi K., Galassi A.R., Prokhorikhin A.A. A randomized trial of bifurcation stenting technique in chronic total occlusions percutaneous coronary intervention. Coron. Artery Dis. 2018;29(1):30–38. doi: 10.1097/MCA.0000000000000551. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.