Abstract
Background
It is estimated that 20–50% of all radiological examinations are of low value. Many attempts have been made to reduce the use of low-value imaging. However, the comparative effectiveness of interventions to reduce low-value imaging is unclear. Thus, the objective of this systematic review was to provide an overview and evaluate the outcomes of interventions aimed at reducing low-value imaging.
Methods
An electronic database search was completed in Medline – Ovid, Embase-Ovid, Scopus, and Cochrane Library for citations between 2010 and 2020. The search was built from medical subject headings for Diagnostic imaging/Radiology, Health service misuse or medical overuse, and Health planning. Keywords were used for the concept of reduction and avoidance. Reference lists of included articles were also hand-searched for relevant citations. Only articles written in English, German, Danish, Norwegian, Dutch, and Swedish were included. The Mixed Methods Appraisal Tool was used to appraise the quality of the included articles. A narrative synthesis of the final included articles was completed.
Results
The search identified 15,659 records. After abstract and full-text screening, 95 studies of varying quality were included in the final analysis, containing 45 studies found through hand-searching techniques. Both controlled and uncontrolled before-and-after studies, time series, chart reviews, and cohort studies were included. Most interventions were aimed at referring physicians. Clinical practice guidelines (n = 28) and education (n = 28) were most commonly evaluated interventions, either alone or in combination with other components. Multi-component interventions were often more effective than single-component interventions showing a reduction in the use of low-value imaging in 94 and 74% of the studies, respectively. The most addressed types of imaging were musculoskeletal (n = 26), neurological (n = 23) and vascular (n = 16) imaging. Seventy-seven studies reported reduced low-value imaging, while 3 studies reported an increase.
Conclusions
Multi-component interventions that include education were often more effective than single-component interventions. The contextual and cultural factors in the health care systems seem to be vital for successful reduction of low-value imaging. Further research should focus on assessing the impact of the context in interventions reducing low-value imaging and how interventions can be adapted to different contexts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-021-07004-z.
Keywords: Low-value, Diagnostic imaging, Radiology, Reduce, Inappropriate, Intervention
Background
The rapidly expanding use of health services is challenging and health care expenditures are mounting [1]. This has underscored the need for more efficient use of finite healthcare resources. However, according to the Organization for Economic Co-operation and Development (OECD), approximately 10–34% of health service spending is potentially inappropriate, representing ineffective and wasteful use of health care resources [2]. Such services are referred to as low-value care, which is defined “an intervention in which evidence suggest it confers not or very little benefit for patients, or risk of harm exceeds probable benefit or, more broadly, the added costs of the intervention do not provide proportional added benefits” [3].
While diagnostic imaging provides crucial information for the diagnostics of patients [4], inappropriate or low-value imaging are estimated to constitute 20–50% of radiological examinations internationally [2, 5–8]. Several interventions to reduce low-value imaging have been evaluated in the literature, including guidelines such as iRefer, iGuide, as well as national and international initiatives such as the National Institute for Health and Care Excellence (NICE) “Do-not-do list,” and the Choosing Wisely campaign [9–12]. However, the effect of such efforts on low-value diagnostic imaging has been limited due to barriers such as financial incentives, practice behavior, self-referral, lack of feedback, patient expectations, and duplicate imaging examinations [5, 11, 13–17]. Some interventions even seem to increase the use of inappropriate imaging [18, 19].
Several approaches to address the use of inappropriate health services, beyond low-value imaging, have been extensively evaluated. Education or training programs for health care personnel, clinical decision support, feedback, patient education, shared decision making, and economic incentives are but a few examples [5, 20–24]. However, the great quantity and variability of available approaches makes it unclear which measures are most suitable to target low-value imaging and overutilization. While research on interventions to reduce low-value care, in general, recommend implementation of multi-component interventions in complex health care systems [12, 25–28] there is still uncertainty as to why or when an intervention will be effective in diagnostic imaging specifically and/or in which clinical circumstances they are effective. Earlier systematic reviews on interventions in imaging have addressed specific interventions as image sharing or clinical decision support systems or specific imaging examinations or patient complaints [26, 29–32]. However, there is no encompassing systematic review assessing the outcome of various types of interventions to reduce low-value imaging. Thus, the objective of this systematic review was to provide an overview and evaluate the outcomes of interventions aimed at reducing low-value imaging.
Methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (PROSPERO ID: CRD42020208072). The electronic database search was developed in Medline – Ovid (Table 1) and further adapted to Embase-Ovid, Scopus, and Cochrane Library. The terms used were built from medical subject headings (MESH) for Diagnostic imaging/Radiology, Health service misuse/Medical overuse, and Health planning. Keywords were used for the concept of reduction/avoiding. Also, the search was broadened with text word and keyword synonyms. The complete search strategy is available in Additional file 1. Searches were carried out in September and October 2020; last search made on 13th October 2020. Papers written in English, German, Danish, Norwegian, Dutch, and Swedish were eligible and language filters were used to exclude other languages. Keywords were used to exclude studies on animals, mass screening, and unnecessary care besides imaging services. No other limitations were applied.
Table 1.
Search strategy developed in Medline (Ovid)
| # | Medline Ovid |
|---|---|
| 1 | diagnostic imaging/ or cardiac imaging techniques/ or imaging, three-dimensional/ or neuroimaging/ or radiography/ or radionuclide imaging/ or respiratory-gated imaging techniques/ or tomography/ or ultrasonography/ or whole body imaging/ |
| 2 | exp Radiology/ |
| 3 | (MRI or x-ray* or xray* or ultrasound* or mammography or ultrasonography or DEXA or DXA or CT or radiograph* or radiolog* or tomography or imaging).tw. |
| 4 | (CAT adj scan).tw. |
| 5 | (bone adj scan).tw. |
| 6 | (Magnetic adj resonance adj imaging).tw. |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 |
| 8 | exp Health Services Misuse/ or exp. Medical Overuse/ |
| 9 | (Unnecessar* or overuse* or Inappropriate* or wasted or low-value or overdiagn* or overutili* or misuse* or (Low adj value) or unwarrent or redundant).tw. |
| 10 | (Choosing adj wisely).tw. |
| 11 | 8 or 9 or 10 |
| 12 | 7 and 11 |
| 13 | Animal/ not (animal/ and human/) |
| 14 | 12 not 13 |
| 15 | limit 14 to ((danish or dutch or english or german or norwegian or swedish) and last 10 years) |
| 16 | exp Health Planning/ |
| 17 | (reduc* or prevent* or stop* or replac* or abandon* or avoid* or deinvest* or de-invest or deadopt* or de-adopt* or deimplement* or de-implement* or restrict* or lower* or decrease* or (practice adj revers*) or educat* or guidel*).tw. |
| 18 | (academic adj detailing).tw. |
| 19 | 16 or 17 or 18 |
| 20 | 15 and 19 |
| 21 | exp Mass Screening/ |
| 22 | (Unnecessary adj surger*).tw. |
| 23 | (unnecessary adj biops*).tw. |
| 24 | (mammography adj screening).tw. |
| 25 | (lung adj cancer adj screening).tw. |
| 26 | (unnecessary adj invasive adj procedure).tw. |
| 27 | (prenatal adj screening).tw. |
| 28 | (case adj report).tw. |
| 29 | (comment or editorial or letter).pt. |
| 30 | (Radioactive adj Waste).tw. |
| 31 | (machine adj learning).tw. |
| 32 | (deep adj learning).tw. |
| 33 | (radio adj therapy).tw. |
| 34 | (optical adj imaging).tw. |
| 35 | (soil or cell* or fetal or dentist* or denture*).tw. |
| 36 | (cancer adj screening).tw. |
| 37 | 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 |
| 38 | 20 not 37 |
Eligibility criteria
Primary empirical studies assessing interventions to reduce the use of low-value diagnostic imaging examinations were included. Studies designed as randomized controlled trials, non-randomized trials, descriptive studies, mixed-methods studies, and qualitative studies were included. While systematic reviews and meta-analyses were not included, the reference lists of relevant systematic reviews and meta-analyses were hand-searched for additional primary studies for inclusion. Studies published before 2010 were excluded due to the changes in perception on low-value imaging through the preparation and introduction of the Choosing Wisely campaign in 2012. The inclusion and exclusion criteria are provided in Table 2.
Table 2.
Inclusion and exclusion criteria for assessing record eligibility
| Inclusion criteria | Exclusion criteria |
|---|---|
| Empirical study | Published before 2010 or after 2020 |
| Assessing interventions aimed to reduce the use of low-value diagnostic imaging | Dental imaging, optical imaging, thermal imaging, microscopic imaging |
| Outcome of interventions to reduce low-value diagnostic imaging | Patient case reports, letter, comment |
| English, German, Dutch, Danish, Swedish, and Norwegian language | Mass-screening related studies |
Selection of records and methodological quality appraisal
The records were archived using Thomson Reuters EndNote X9.3.3 library and duplicates were removed. All remaining records were transferred to Rayyan QCRI [33] where titles and abstract review (EK and BMH) and full-text review and quality assessment (EK, ERA, LJJS, LvB-V and BMH) were completed by two teams of reviewers. Each study was quality assessed by one reviewer and double checked by EK for consistency. The Mixed Methods Appraisal Tool (MMAT) was used to assess the methodical quality of all included studies as it is considered to be an appropriate tool for appraisal of interventional studies of different methodologies [34]. Any disagreements during abstract or full-text screening were resolved through discussion and consensus. Reference lists of included articles were also hand-searched for relevant articles for inclusion. A grey literature search was also completed (ERA) according to the CADTH Grey Matters checklist [35]. Google Scholar was used for searching for eligible papers that cited the included studies.
Data extraction and synthesis
Data extraction was completed independently by EK, LJJS, LvB-V, BMH and ERA using a standardized summary table consisting of the following categories: author, title and year, country, design, population, clinical setting, outcome measures, low-value practice, intervention, targeted personnel or roles, control or comparator, use of low-value practice before or after intervention, and change in use of low-value practice. Data extraction was discussed in the research team for quality assurance purposes.
The findings from included studies were narratively synthesized. This synthesis was performed due to the variety of study designs among included studies and thus a meta-analysis was not feasible [36]. The narrative synthesis included familiarization, the development of a preliminary synthesis by organizing findings in tables. Then, relationships, patterns, and connections in the data were explored [36]. In addition, a subgroup analysis was done for interventions done in the USA separately.
Results
Search of the literature
As shown in Fig. 1, the electronic database searches resulted in 15,659 records. After the removal of 7468 duplicates, 8191 unique records were screened through title and abstract screening and 8108 records were excluded. An additional 103 records were identified through snowballing techniques and from the grey literature. A total of 186 articles were reviewed in full-text and 91 articles were excluded. Thus, 95 studies were included in the narrative synthesis. An overview of excluded studies with reason for exclusion is provided in Additional file 2.
Fig. 1.
Flow diagram for record selection
Quality of included studies
The 95 included studies [37–131] are summarized in Table 3. All included papers fulfill the screening questions in MMAT. Forty-six papers were given a full score in the MMAT appraisal. These are marked with a * in Table 3 (the full MMAT report is available in Additional file 3), while the others had one criterion unfulfilled, or lacked sufficient information in the report.
Table 3.
Characteristics of the included studies, outcome of the intervention and quality assessment result
| Author (year) | Country | Methods | Population | Clinical setting | Intervention | Low-value practice | Outcome of intervention(s) | Quality assessment |
|---|---|---|---|---|---|---|---|---|
| Arora et al. (2020) [126] | USA | Evaluation of a quality improvement project | 1535 children | Emergency department | Education, decision support, and performance feedback | Head CT | 4.6%-points reduction in use | * |
| Ashykian et al. (2019) [37] | USA | Retrospective review | 1000 reports | Orthopedic and family practice departments | Education | Repeat radiographs for routine follow-up of osteoarthrosis | 50% reduction in use | * |
| Bailey et al. (2013) [38] | USA | Longitudinal data analysis | 800 patients | Emergency department | Health information exchange | Repeated lumbar or thoracic imaging | 64% lower odds of repeat | * |
| Bailey, Wan et al. (2013) [39] | USA | Longitudinal data analysis | 1252 patients | Emergency department | Health information exchange | Diagnostic neuroimaging | 62% lower odds of repeat | * |
| Bairstow et al. (2010) [40] | Australia | Pre/post audit | 1061 patients | Emergency department | Education, request forms | Chest CTA, abdominal XR, imaging with a provisional diagnosis of renal colic and XR despite negative Ottawa Ankle Rule | 13–28% reduction in use | * |
| Baker et al. (2020) [41] | USA | Retrospective registry review | 445 patients | Emergency department | Education and guideline | C-spine CT | > 30% reduction in use | * |
| Ballard et al. (2019) [127] | USA | Nonrandomized clinical trial - secondary analysis | 3859 children | Emergency department | Electronic clinical decision support | Head CT | 2.6% unsignificant reduction in use | * |
| Bhatia et al. (2013) [44] | USA | Prospective, time series analysis | 1711 patients | Academic medical center | Education | Transthoracic echocardiography | 26% reduction in use | |
| Bhatia et al. (2014) [42] | USA | Randomized Control Trial | 88 internal medicine residents and 24 cardiology fellows | Academic medical center | Education | Transthoracic echocardiography | 62% reduction in use | * |
| Bhatia et al. (2017) [43] | Canada/USA | Multicenter, randomized controlled trial | 196 physicians | 8 hospitals | Education and feedback | Transthoracic echocardiogram | 1.3% significant reduction in use | * |
| Blackmore et al. (2011) [45] | USA | retrospective cohort study | 6141 patients | Medical Center | Decision support system | Lumbar MRI, Brain MRI in headache, and sinus CT | 23.2–26.8% significant lower use | |
| Bookman et al. (2017) [46] | USA | Longitudinal, before/after study | 235,858 patient visits | 5 emergency departments | Clinical decision support system | Head/c-spine CT, Chest CTA |
> 6% significant decrease in head and c-spine CT 2% non-significant reduction chest CTA |
* |
| Boutis et al. (2013) [47] | Canada | Interrupted time series with pair matched control design. | 2151 children | 6 emergency departments | Education, reminders, and computerized decision support system | Ankle XR | 22% reduction in use | * |
| Breakell et al. (2018) [48] | UK | Retrospective audit | 101 children | District General Hospital | Education and guideline | Chest XR for Bronchiolitis | 16% reduction in use | |
| Buntine et al. (2018) [49] | Australia | Before and after study | 2931 scans | 3 hospitals | Flowchart | Chest CTA and NM ventilation perfusion | 6 per 1000 scans reduction in use | * |
| Carnevale et al. (2015) [128] | USA | Before-and-after study | 29,395 encounters | Emergency department | Decision support and education | Several | 5–10% reduction in use | * |
| Carpenter et al. (2020) [50] | USA | Retrospective chart review | 1010 children | Hospital | Choosing Wisely | CT/MR or US in cryptorchidism | No significant difference | * |
| Chandra et al. (2019) [51] | Canada | Evaluation of a quality improvement project | 37 physicians | Community teaching hospital | Didactic seminar, Survey | Imaging for low back pain | 4%-points significant increase | * |
| Chang et al. (2018) [52] | USA | Before-and-after study | 202 family physicians and 8 general internists | Clinics | Feedback reports | CT, MRI, and PET | 14.5% reduction in use | * |
| Char et al. (2014) [53] | USA | Retrospective chart review | 510 patients | Emergency department | Increased D-dimer threshold value and clinical probability assessment | Chest CTA | 7%-points Increase in diagnostic yield | |
| Chen et al. (2020) [54] | USA | Before-and-after study | Physicians | Hospital | Alerts | Imaging for lower back pain | 9.6% reduction in total imaging rate and MRI (14.9%), No significant difference in use of CT/XR | * |
| Chien et al. (2017) [55] | USA | Block randomized controlled trial | 1205 clinicians | Multidisciplinary medical group | Financial incentives | CT or MRI for single headache or lower back pain, acute, uncomplicated rhinosinusitis, or DEXA for low risk for osteoporosis | No significant difference | * |
| Depinet et al. (2016) [56] | USA | Interrupted time series trial | 1886 children | Urban tertiary care hospital | Clinical decision support system and pathway | Abdominopelvic CT/US | 2%-points increased use of US and 5%-points reduction in use of CT | * |
| Doyle et al. (2019) [57] | USA | Randomized study | 3524 practitioners | 15 hospitals and 150 clinics | Best practice alerts | Several | 6% reduction in use | |
| Drescher et al. (2011) [58] | USA | Before and after study | 404 cases | Emergency department | Algorithm | Chest CTA | 4.4% increase in use | * |
| Dudzinski et al. (2016) [59] | USA | Before and after study | 65 cardiologists | Ambulatory cardiology practices in hospital | Education and feedback | Transthoracic echocardiography | 6%-points reduction in use | * |
| Dunne et al. (2015) [60] | UK | Before and after study | 5892 examinations | Hospital | Clinical decision support system | Chest CTA | 12.3% reduction in use | * |
| Durand et al. (2013) [61] | USA | Randomized controlled trail | 10 imaging tests | Tertiary teaching hospital | Cost display | Several | No significant difference | * |
| Ehrlichman et al. (2017) [129] | USA | Before-and-after study | 104,454 patients | Emergency department | Feedback | Several | 2.3% reduction | * |
| Fallon et al. (2016) [62] | USA | Prospective, longitudinal study | Children | Level I pediatric trauma center | Development of Trauma Protocol | Abdominal CT for abdominal trauma | 18%-points increase in diagnostic yield | * |
| Ferguson et al. (2017) [63] | USA | Interventional improvement project | 1 Emergency department | Hospital | Education and diagram | Abdominal XR constipation | 38%-points reduction | * |
| Flamm et al. (2013) [64] | Austria | Non-randomized controlled trial with a historical control group | 1363 patients | Hospital | PReOPerative evaluation’ (PROP) | Chest XR | 21.7%-points reduction | |
| French et al. (2013) [65] | Australia | Cluster Randomized trail | 112 general practitioners | Practices | Guideline/ facilitated interactive workshops | Lumbar CT or XR | No significant difference | |
| Gertz et al. (2016) [66] | USA | Before-and-after study | 941 patients | Hospital | Computerized order entry tool | Cardiac stress tests with imaging | No significant difference | |
| Goldberg et al. (2011) [67] | USA | Retrospective cohort chart review | 742 patients | Hospital | Guideline | Head CT | 16% reduction in use | |
| Graves et al. (2018) [68] | USA | Interrupted time series | 76,119 compensation claims | Regional | Policy implementation | Imaging for lower back pain |
5,6%-points significant decrease in use of MRI. 2.46% increase in the use of XR No change in use of CT |
|
| Hardin et al. (2017) [69] | USA | Pre−/post-test design | 339 patients | Hospital | Complex Care Map | CT scans | 62% reduction in use | |
| Hess et al. (2018) [70] | USA | Cluster Randomized Trial | 172 clinicians | Emergency department | Shared decision-making | Head CT (children) | No significant difference | |
| Hong et al. (2017) [71] | USA | Retrospective chart review | 1,547,870 patients | Several | Choosing wisely | Imaging for lower back pain | 4% reduction in use | |
| Hoo et al. (2011) [72] | USA | Retrospective chart review | 457 examinations | Hospital | Mandatory clinical decision rule and selective d-dimer use | Chest CTA | 13%-points Increase in diagnostic yield | * |
| Hui et al. (2014) [73] | USA | Prospective cohort study and retrospective review | 762 patients | Hospital | Education and guideline | Pelvic US | 58% reduction in use | |
| Hurley et al. (2017) [74] | USA | Before-and-after study | 10,554 patients | Hospital | MUSIC imitative Collaborative | Bone scan and CT for prostate cancer | 4.5–7%-points reduction in use | * |
| Ip et al. (2013) [78] | USA | Before-and-after study | 1.8 million patient-months | Hospital | Computerized order entry tool with clinical decision support systems and accountability tools | Multiple | 12% reduction in use | * |
| Ip et al. (2014) [75] | USA | Retrospective cohort study | 21,445 LBP-related primary care visits | Academic quaternary care hospital | Clinical decision support system | Imaging for low back pain | 30.8% reduction in use | * |
| Ip et al. (2015) [77] | USA | Before-and-after study | Emergency department patients | Hospital | Clinical decision support system | Head CT | 13.4% reduction in use | * |
| Ip et al. (2017) [76] | USA | Before-and-after study | 98,894 radiologyorders | Four institutions | Clinical decision support system | Several | 1%-point reduction in use | |
| Jennings et al. (2017) [79] | USA | Evaluation of a quality improvement project | 1346 Children | Community emergency department | Protocol, education, and individual feedback. | CT head of children, minor head injury | 12% reduction in use | |
| Judkins et al. (2013) [80] | Australia | Retrospective chart review | 659 children | Tertiary children’s hospital | NICE guidelines | Ultrasound urinary system, MUCG and dimercaptocsuccinic acid scintigraphy | 50% reduction in the use | |
| Kandiah et al. (2020) [81] | Canada | Evaluation of a quality improvement project | 4480 patients | Hospital | Education and information packages | MRI and CT of joints without red flags |
CT 43% reduction in use MRI 0.6% reduction of use |
* |
| Kanaan et al. (2013) [82] | USA | Retrospective chart review | 200 patients | Tertiary emergency department | Education | Chest CTA | No significant difference | * |
| Keveson et al. (2017) [83] | USA | Evaluation of a quality improvement project | All invasive mechanical ventilator patients | Tertiary hospital | Education and change in routines/referral system | Daily CXR of ventilated patients | 64% reduction in use | * |
| Kobes et al. (2020) [130] | Canada | Retrospective chart review | 28 medical imaging sites | Mobile radiography | Guideline | Chest XR | 3.2% reduction in use | * |
| Lacson et al. (2017) [84] | USA | Retrospective chart review | 63,222 orders | Hospital | Clinical decision support system | Several | No significant difference | |
| Levitt et al. (2015) [120] | USA | Before-and-after study | 415 patients | Hospital | Decision support and education | Stress echocardiography | 12%-points reduction in use | * |
| Lu et al. (2012) [85] | USA | Retrospective chart review | 267 patients | Hospital | Importing images from other institutions into PACS | Repeat imaging | 61%-points reduction in use | |
| Luther et al. (2019) [86] | USA | Retrospective chart review | 273 patients | Hospital | Standardized clinical assessment and management plans | Wrist XR | 60% reduction in use | * |
| Masood et al. (2020) [87] | Canada | Evaluation of a quality improvement project | Parents in the emergency department | Tertiary care center | Education, guideline and checklist, patient handouts, and feedback | Head CT in adults | 7–14% reduction in use | |
| McGrew et al. (2018) [88] | USA | Retrospective chart review | 1934 children | Pediatric Level 2 Trauma Center | Guideline | Head and abdomen/pelvis CT pediatric trauma | 11.5–18.8% reduction in use | |
| Mills et al. (2018) [121] | USA | Before-and-after study | 7987 patients | Emergency department | Decision support | Chest CTA | 2.5% increased diagnostic yield | * |
| Min et al. (2017) [89] | Canada | Retrospective chart review | 4562 patients | Emergency department | Checklist | Imaging in low back pain | 22% reduction in use | |
| Mittal et al. (2014) [91] | USA | Before and after design | 3641 patients | Tertiary care hospital | Clinical practice guidelines | Chest XR | 14.6–20%-points reduction in use | |
| Moriarity et al. (2015) [91] | USA | Retrospective chart review | 33,311 patients | Hospital | Clinical decision support | Inpatient MR, CT, and NM | No significant difference | |
| Mulders et al. (2020) [92] | The Netherlands | Before-and-after comparative prospective cohort study | 1261 patients | Emergency department | Amsterdam Wrist Rules | Wrist XR | 15%-points reduction in use | |
| Mäenpää et al. (2011) [93] | Finland | Retrospective, longitudinal study | 1 regional hospital | Hospital | Regional Health InformationExchange | Several | 16.4% reduction in use | * |
| Nigrovic et al. (2015) [94] | USA | Multifaceted quality improvement initiative | Children < 21 years | Urban tertiary care academic center | Guideline development, feedback, and education | Head CT | 6%-points reduction in use | * |
| O’Connor et al. (2014) [95] | USA | Prospective before and after study | 28,420 CT orders | Tertiaryacademic medical center | Requiring a clinical justification to override a repeat CT alert | Several | Prevented 1 in 13 scans | * |
| Ong et al. (2013) [122] | USA | Before-and-after study | 471 patients | Hospital | Algorithm and guideline | Chest CTA | 26% reduction in use | * |
| Ostby et al. (2020) [96] | USA | Evaluation of a quality improvement project | 235 patients | Emergency department | Specialist consolation before imaging | CT of gynecological cancer patients | 54%-points reduction in use | * |
| Palen et al. (2019) [97] | USA | Stepped-wedge study | 31,426 orders | several | Check boxes | Several | Modest increase in appropriateness | |
| Parikh et al. (2016) [98] | USA | Retrospective cohort study | 220,539 patients | Hospital | Guideline | Chest XR | 6.4% significant reduction in use | * |
| Poeran et al. (2019) [99] | USA | Retrospective interrupted time series | 27,549 orders | Emergency department | Clinical decision support | Low appropriateness imaging | 9%-points reduction in use | * |
| Prevedello et al. (2013) [100] | USA | retrospective cohort study | 2891 patients | Emergency department | Alerts | Chest CTA | 2.2/1000 reduction in use | * |
| Puffenbarger et al. (2019) [123] | USA | Retrospective chart review | 556 visits | Emergency department | Education, guideline, and hand-outs | Head CT | 21.6%-points reduction in use | * |
| Pugel et al. (2018) [101] | USA | Retrospective interrupted time series | 213,532 consultations | Ambulatory care | Education, feedback and guidelines | DEXA and head CT | 23.4% reduction in use | |
| Raja et al. (2012) [103] | USA | Retrospective cohort study | 6838 patients | Quaternary care institution | Clinical decision support system | Chest CTA | 20.1% reduction in use | * |
| Raja et al. (2015) [102] | USA | Prospective randomized controlled trial | 2167 patients | Urban level 1 adult trauma center | Feedback | Chest CTA | 2/1000 reduction in use | * |
| Reiter et al. (2018) [104] | Israel | Prospective cohort study | 544 children | Pediatric Emergency department | Education, guideline cards at computers | Chest XR for Bronchiolitis | 20%-points reduction in use | * |
| Rezaii et al. (2020) [105] | USA | Cohort study | 27 practices, 4601 cases | Academic and private practices | Online educational material and feedback | Chest CTA, advanced imaging of low back pain, follow-up of adnexal cysts | 3% reduction in use | * |
| Rosati et al. (2015) [106] | USA | Retrospective review | 233 children | Level I trauma center | Guideline | C-spine CT | 23% reduction in use | |
| Sclafani et al. (2010) [107] | USA | Retrospective chart review | 1092 patients | Hospital | Education | Head CT, brain MRI and carotid US of syncope patients | No significant difference | |
| Shah et al. (2016) [108] | USA | Chart review | 824 children | Emergency department | Diagnostic algorithm | Abdominal CT appendicitis | 51.2%-points reduction in use | |
| Shelton et al. (2015) [131] | USA | Before-and-after study | 2001 patients | Hospital | Feedback | Several | 38% reduction in use | * |
| Singer et al. (2014) [109] | USA | Before and after trial design | 34,961 children | Academic medical center | Opening a dedicated pediatric ED | Several | 3.2% reduction in use | |
| Sodickson et al. (2011) [110] | USA | Retrospective chart review | 1487 patients | Tertiary care, level I trauma center | Health InformationExchange | Several | 16–18% reduction in use | |
| Sy et al. (2016) [111] | Canada | Evaluation of a quality improvement project | 1492 patients | Intensive care unit | Education, posters, and change in order system | Chest XR | 26% reduction in use | * |
| Tajmir et al. (2017) [124] | USA | Randomized controlled trail | 613 patients | Hospital | Decision support | Ankle XR | Modest change in diagnostic yield | |
| Tyler et al. (2018) [112] | USA | Evaluation of a quality improvement project | 2211 patients | Children’s hospital | Education, feedback, sign pledge, visualizing algorithm, guideline | Chest XR | 12.1%-points reduction in use | |
| Vartanians et al. (2010) [113] | USA | Retrospective study | 118,975 orders | Several | Change in ordering system | Several | 3.5%-points reduction in use | * |
| Walen et al. (2016) [125] | USA | Prospective observational study | 250 patients | Hospital | Wells-score documentation | Chest CTA | 6.6% increase in diagnostic yield | |
| Walker et al. (2020) [114] | Canada | Retrospective chart review | 302 Consultations | Primary care | Electronic communication system | Abdominal, musculoskeletal, neuro, and thoracic imaging | 28% reduction in use | |
| Wang et al. (2018) [115] | USA | Retrospective chart review | 3 clinics | Primary care | On-site and online education and feedback | Lumbar MRI | 3.7 MRIs reduced per month | |
| Wu et al. (2020) [116] | USA | Evaluation of a quality improvement project | 6441 Chest XRs | Medical Intensive care unit | Survey, journal club, discussions, posters, alerts in electronic referral system, education, pocket cards, electronic decision tool | Chest XR | 36.1% reduction in use | |
| Xu et al. (2020) [117] | Canada | Retrospective review | 400 referrals | Tertiary care center | Mandatory check list | Knee MRI | 48% reduction in use | * |
| Zafar et al. (2019) [118] | USA | Randomized cohort study | 54 providers | Tertiary academic health system | Algorithm and alerts | Low back imaging | No significant difference | * |
| Zamora-Flores et al. (2015) [119] | USA | Retrospective chart review | 322 children | Rural community hospital | Guideline | Chest XR | No significant difference |
CT computed tomography, CTA CT angiography, DEXA dual-energy x-ray absorptiometry, MMAT Mixed Methods Appraisal Tool, MRI magnetic resonance imaging, MUCG micturating cystourethrogram, NM nuclear medicine, PET positron emission tomography, US ultrasound, XR X-ray
* Fulfill all MMAT criteria
Italic = Mixed results, Bold = Reduction in use/increase in rate of diagnostic yield, Normal = no significant difference/increase
Characteristics of included studies
A majority of the included studies applied quantitative study designs. Retrospective chart reviews (n = 26) and uncontrolled before-after studies (n = 14) were the most common. Seventy-eight of the studies were conducted in the USA (82%). The setting of the studies included hospital (n = 40), emergency department (n = 24), or outpatient medical center (n = 18). Musculoskeletal (n = 26), neurological (n = 23) and vascular (n = 16) imaging were most commonly evaluated. The most targeted imaging examinations were chest CTA (n = 15) and head CT (n = 12). Further, pulmonary embolism (n = 15), lower back pain (n = 14), and minor head injury (n = 12) were the most commonly explored medical conditions.
Interventions
Guidelines (n = 28) and education (n = 28), either alone or in combination with other measures, were the most common interventions evaluated to reduce low-value imaging. The outcome measures reported in the included studies varied, with the number or rate of imaging examinations (n = 75) most frequently reported primary outcomes. A majority of studies (n = 61) used a single component intervention and most studies (n = 90) targeted referring physicians. An overview of participants exposed to the intervention (referring physicians, imaging staff, patients and/or family members), types of interventions, and combinations of components in multi-component interventions are presented in Fig. 2.
Fig. 2.
Overview of participants, interventions, and combinations in multi-component interventions in the included studies. Figure legend: To the left an overview of single interventions used for each participant group. To the right an illustration for how multi-component interventions were combined. Overlapping circles illustrate different combinations of two of more components
A variety of imaging modalities or patient diagnoses were targeted, and the primary outcomes varied among studies that reported improvements post-intervention. Among studies targeting several imaging modalities or diagnoses, 74–79% of the studies showed a reduction in use of low-value imaging. In contrast, studies targeting one specific modality only showed that targeting X-ray [37, 47, 48, 63, 64, 83, 86, 90, 92, 98, 104, 112, 119, 124, 130], CT [41, 46, 49, 53, 54, 58, 60, 62, 67, 69, 70, 77, 79, 82, 87, 88, 94–96, 101, 102, 106, 108, 121–123, 125–127, 129] or MRI [45, 68, 75, 105, 118] led to a 87, 86, and 83% reduction in low-value imaging, respectively. Few studies included other imaging modalities.
The most commonly targeted patient diagnosis was bronchiolitis [48, 90, 104, 112, 119], pulmonary embolism [49, 58, 60, 82, 100, 102, 121, 122, 125], and head injuries [67, 70, 77, 79, 87, 94, 101, 123, 126, 127]. In studies targeting these complaints, a reduction in use of low-value imaging were reported in 78–80% of the studies, while imaging in lower back pain [38, 45, 51, 53, 54, 65, 68, 71, 75, 89, 115, 118] were reduced in 58% of studies.
Among the 77 studies that reported improvements following the intervention [37–45, 47–49, 52, 53, 56, 57, 59, 60, 62–64, 67, 69, 71–81, 83, 85–90, 92–106, 108–117, 120–123, 125, 128–131], decreases in low-value imaging varied largely from < 1 to 62%. Of the remaining studies, three studies reported mixed results, where only some of the targeted low-value imaging examinations were reduced [46, 54, 68], and 16 studies showed a non-significant change or increase in the use of low-value imaging post-intervention [50, 51, 55, 58, 61, 65, 66, 70, 82, 84, 91, 107, 118, 119, 124, 127].
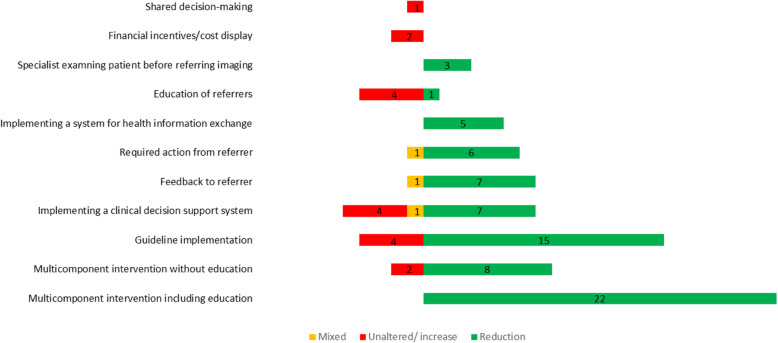
Implementation of multi-component interventions (2 or more components in combination) reportedly reduced the use of low-value imaging among 94% of the included studies [40–44, 47, 48, 51, 53, 56, 59, 63, 72, 78, 79, 81, 83, 86, 87, 94, 101, 104, 105, 111, 115, 116, 118, 120, 122, 123, 126, 128]. Multi-component interventions were found to be more effective when education was one of the components. Following implementation of a single component intervention, 74% of included studies reported decreases in low-value imaging [37–39, 45, 46, 49, 50, 52, 54, 55, 57, 58, 60–62, 64–71, 74–77, 80, 82, 84, 85, 88–93, 95–100, 102, 103, 106–110, 113, 114, 117, 119, 121, 124, 125, 127, 129–131]. Data analyses based on the USA studies demonstrated similar results as 96% of multi-component and 68% of single-component interventions showed reduction in the use of low-value imaging. Thus, county of intervention does not affect the result alone. Implementation of guidelines or clinical decision support systems were the most effective single-component interventions [37–121, 126, 128, 130]. Furthermore, 23% of single-component interventions compared to 6% of multi-component interventions showed no statistically significant difference or an increase in the use of low-value imaging. In Fig. 3, the green bars represent studies with a reduction in the use of low-value imaging, red bars represent no significant change or increase, and orange bars represent mixed results.
Fig. 3.
The number of studies and outcome of different types of interventions to reduce low-value imaging
Single-component interventions such as education, shared-decision-making, and financial measures alone often had no effect on use of low-value imaging [55, 61, 70, 82, 107]. Studies with more than 30% reduction in use of low-value imaging were both single-component (n = 11) and multi-component (n = 8) interventions [37–39, 41, 42, 44, 69, 73, 75, 80, 81, 83, 85, 86, 96, 108, 116, 117, 131]. All these studies targeted refereeing physicians while one also targeted imaging staff. Another targeted referrer, imaging staff, and patients. Of these studies, 16% were from countries other than the USA. Table 4 provides an overview of the type of interventions that resulted in more than a 30% reduction in low-value imaging.
Table 4.
Overview of interventions with more than a 30% reduction in use of low-value imaging examinations
| Components in interventions | Country | Setting | Reduction | Reference |
|---|---|---|---|---|
| Clinical decision support system | USA | Hospital | 31% | [75] |
| Feedback to referrers | USA | Hospital | 38% | [131] |
| Multiple measures for referrers, imaging staff, and patients | Canada | Hospital | 43% | [81] |
| Required action from referrers | Canada | Tertiary care center | 48% | [117] |
| Education | USA | Medical center | 50% | [37] |
| Specialist involved in ordering examinations | USA | Hospital | 54%-points | [96] |
| Education and guideline implementation for referrers and imaging staff | USA | Hospital/Emergency department | 30–58% | [41, 73] |
| Combination of new clinical procedures | USA | Hospital | 60% | [86] |
| Education, feedback, and hand-outs | USA | Academic medical center | 30–62% | [42, 44] |
| Guideline implementation | USA, Australia | Hospital/tertiary hospital | 50–62% | [69, 80, 108] |
| Education, alerts, and new procedure for referrers | USA | Hospital/tertiary hospital | 35–64% | [83, 116] |
| Health information exchange | USA | Hospital | 61–64% lower odds for repeat examination | [38, 39, 85] |
Discussion
A large body of literature evaluating the outcome of interventions aimed at reducing low-value imaging was identified through this systematic review. Broadly, most interventions were found to be effective, with multi-component interventions more frequently reported to be effective compared to single-component interventions. All studies evaluating multi-component interventions with an education component reported reductions in low-value imaging. Multi-component interventions targeting the participants on several points providing education and then feedback and reminders over a longer period seems to be effective as change takes knowledge, motivation, and time [132]. Single-component interventions, particularly guideline implementation, clinical decision support systems, feedback, or actions required from the referrers, showed reduction in use of low-value imaging in several studies but not in all. This might be caused by organizational differences, differences in the clinical setting, or participants motivation [132]. Shared decision-making, new referring procedures, and financial measures demonstrated no effect; however, these interventions were only evaluated in a limited number of studies. Targeting specific examinations for specific conditions (e.g., bronchiolitis), targeting referrers, and only targeting one imaging modality seemed to be more effective than targeting several modalities or examinations referred from a variety of referrer groups (e.g., lower back pain). There was also a variety of outcome measure used among included studies. The number or rate of low-value imaging was the most common. Others included appropriateness and diagnostic yield. This warrants caution when comparing outcomes between different types of interventions.
The present results are in line with previous systematic reviews on interventions to reduce low-value services in general [12, 26, 29–32] and with a previous scoping review on unnecessary imaging, diagnostic tests, and procedures in hospitals [28]. The results indicate great variation in outcomes for many interventions. This is in accordance with research on innovation and interventions suggesting that the formal and informal network in the organization, motivation, flexibility, and fitness to the internal culture and core values in the organization where interventions are implemented, were key factors for a successful and long-lasting change of clinical practice [132–135]. Whether or not an intervention is successful in reducing the use of low-value imaging would thus depend on a variety of factors. Comparing studies conducted in the USA to those from other countries showed no difference in type of interventions used or in the rate of studies demonstrating > 30% reduction in the use of low-value imaging. Thus, the effect of intervention seems to be dependent on local culture and health care organizations rather than the national health system alone. In addition, only a few interventions were directed against patients, which is somewhat surprising as patients are also identified as drivers in the use of low-value imaging [136, 137]. Further research should include the patient perspective and the role of the radiology department in interventions to reduce low-value imaging in addition to a review on cost-effectiveness of interventions to reduce low-value imaging. Further investigation should focus on how interventions can be adapted to the culture and core values of the providers of health services in different contexts.
Our study has several limitations. Publication bias may have been introduced as articles with negative or nonsignificant findings are less likely to be published. Among the included studies, few reported null or low effect. Most studies had an uncontrolled before-after design not considering that there may be a secular downtrend in the use of the low-value imaging examinations due to the attention in campaigns, such as Choosing Wisely. Thus, the outcome may be overestimated. Further, the review may be subject to contextual bias and have limited generalizability, as most of the studies were conducted in the USA. Accordingly, caution is warranted when inferring from and applying the results in different settings. The proportion of single-center studies and observational studies may enhance the overall positive effect of the interventions [26]. Yet another limitation is related to indirect outcome measures, as many publications focus on interventions’ impact on volume and not on value. This is understandable as the change of low-value utilization is a warranted measure, but one should notice that the value of these services is not assessed. Moreover, it may be argued that the spectrum of imaging that is targeted by the interventions is biased by the methods to assess intervention outcomes. Nonetheless, we report a wide variety of interventions targeting many examinations. There are reasons to believe that the interventions are targeted strategically. For example, interventions that are believed to be effective may be targeted towards examinations documented to be of low value.
It may also be argued that retrospective chart reviews are not proper intervention studies, but as they are used systematically to assess change in practice, we have included them in this review. Additionally, the included studies afford providers’ perspective and as indicated, few studies elicited patient preferences or included patient-reported outcome measures. In addition, the snowballing uncovered a few studies published in 2021 not included in our analysis due to the inclusion criteria. The results of these studies are in line with the studies included in the analysis and thus not including these did not reduce the strengths of the analysis in this review [138–142].
Conclusions
This systematic review demonstrates that interventions to reduce low-value imaging can be very effective, but that there is a large variation in types of interventions and their outcomes. We found that multi-component interventions reported reduction in low-value imaging or increased diagnostic yield more frequently compared to single-component interventions. The context in which the intervention is introduced seems to be of vital importance for successful reduction of low-value imaging. Thus, in the future multi-component interventions that are adapted to the local context are more likely to be successful. Further research is needed to assess how interventions to reduce low-value imaging can best be adapted to specific contexts and how to reduce the use of low-value imaging cost-effectively.
Supplementary Information
Additional file 1. Search strategy and hits from database searches.
Additional file 2. Table of excluded studies.
Additional file 3. MMAT registration forms.
Acknowledgements
We would like to thank Senior Research Librarian Karen Marie Øvern at NTNU and academic librarian Jana Myrvold at University of South-Eastern Norway for helping with the development of the search strategy. In addition, we would like to thank Dr. Fiona Clement for her useful suggestions for the search strategy.
Abbreviations
- CT
Computed tomography
- CTA
Computed tomography angiography
- DEXA
Dual-energy X-ray absorptiometry
- MMAT
Mixed Methods Appraisal Tool
- MRI
Magnetic resonance imaging
- MUCG
Micturating cystourethrogram
- NM
Nuclear medicine
- PET
Positron emission tomography
- US
Ultrasound
- XR
X-ray
Authors’ contributions
EK – planning and searching, screening, full-text and quality assessment, analysis, drafting, and revision of manuscript. ERA – planning, full-text and quality assessment, snowballing, analysis, and revision. LJJS – planning, full-text and quality assessment, analysis, and revision. LvB-V – planning, full-text and quality assessment, analysis, and revision. BMH – planning, screening, full-text and quality assessment, analysis, and revision. All authors read and approved the final manuscript
Funding
This project received financial support from The Research council of Norway (Project number 302503).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elin Kjelle, Email: elin.kjelle@ntnu.no.
Eivind Richter Andersen, Email: eivind.r.andersen@ntnu.no.
Lesley J. J. Soril, Email: lsoril@ucalgary.ca
Leti van Bodegom-Vos, Email: L.van_Bodegom-Vos@lumc.nl.
Bjørn Morten Hofmann, Email: bjoern.hofmann@ntnu.no.
References
- 1.Expert Panel on effective ways of investing in Health (EXPH). Defining value in “value-based healthcare. 2019.
- 2.Socha K, Couffinhal A, Forde I, Nader C, Cecchini M, Lee S, et al. Tackling Wasteful Spending on Health.OECD 20172017.
- 3.Scott IA, Duckett SJ. In search of professional consensus in defining and reducing low-value care. Med J Aust. 2015;203(4):179–181. doi: 10.5694/mja14.01664. [DOI] [PubMed] [Google Scholar]
- 4.Brady A, Brink J, Slavotinek J. Radiology and value-based health care. Jama. 2020;324(13):1286–1287. doi: 10.1001/jama.2020.14930. [DOI] [PubMed] [Google Scholar]
- 5.Hendee WR, Becker GJ, Borgstede JP, Bosma J, Casarella WJ, Erickson BA, et al. Addressing overutilization in medical imaging. Radiology. 2010;257(1):240–245. doi: 10.1148/radiol.10100063. [DOI] [PubMed] [Google Scholar]
- 6.Sheng AY, Castro A, Lewiss RE. Awareness, utilization, and education of the ACR appropriateness criteria: a review and future directions. J Am Coll Radiol. 2016;13(2):131–136. doi: 10.1016/j.jacr.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 7.Ingraham B, Miller K, Iaia A, Sneider MB, Naqvi S, Evans K, Gheyi V, Anzilotti K. Reductions in high-end imaging utilization with radiology review and consultation. J Am Coll Radiol. 2016;13(9):1079–1082. doi: 10.1016/j.jacr.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Soltana K, Moore L, Bouderba S, Lauzier F, Clément J, Mercier É, et al. Adherence to clinical practice guideline recommendations on low-value injury care: a multicenter retrospective cohort study. Value Health. 2021. 10.1016/j.jval.2021.06.008. [DOI] [PubMed]
- 9.Choosing Wisely [Internet]. 2021. Available from: https://www.choosingwisely.org/getting-started/lists/.
- 10.Improving health and social care through evidence-based guidance [Internet]. 2021. Available from: https://www.nice.org.uk/.
- 11.Ryan JW, Hollywood A, Stirling A, Glynn M, MacMahon PJ, Bolster F. Evidenced-based radiology? A single-institution review of imaging referral appropriateness including monetary and dose estimates for inappropriate scans. Ir J Med Sci. 2019;188(4):1385–1389. doi: 10.1007/s11845-019-02005-8. [DOI] [PubMed] [Google Scholar]
- 12.Cliff BQ, Avanceña ALV, Hirth RA, Lee SD. The impact of choosing wisely interventions on low-value medical services: a systematic review. Milbank Q. 2021. [DOI] [PMC free article] [PubMed]
- 13.Barth JH, Misra S, Aakre KM, Langlois MR, Watine J, Twomey PJ, Oosterhuis WP. Why are clinical practice guidelines not followed? Clin Chem Lab Med. 2016;54(7):1133–1139. doi: 10.1515/cclm-2015-0871. [DOI] [PubMed] [Google Scholar]
- 14.DeAngelis J, Lou V, Li T, Tran H, Bremjit P, McCann M, Crane P, Jones C. Head CT for minor head injury presenting to the emergency Department in the era of choosing wisely. West J Emerg Med. 2017;18(5):821–829. doi: 10.5811/westjem.2017.6.33685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y, et al. Early trends among seven recommendations from the choosing wisely campaign. JAMA Intern Med. 2015;175(12):1913–1920. doi: 10.1001/jamainternmed.2015.5441. [DOI] [PubMed] [Google Scholar]
- 16.Anderson TS, Leonard S, Zhang AJ, Madden E, Mowery D, Chapman WW, et al. Trends in Low-Value Carotid Imaging in the Veterans Health Administration From 2007 to 2016. JAMA Network Open. 2020;3(9):e2015250-e. [DOI] [PMC free article] [PubMed]
- 17.Berezin L, Thompson C, Rojas-Luengas V, Borgundvaag B, McLeod SL. Lumbosacral spinal imaging for patients presenting to the emergency department with nontraumatic low Back pain. The Journal of Emergency Medicine. 2020;58(2):269–274. doi: 10.1016/j.jemermed.2019.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Pons E, Foks KA, Dippel DWJ, Hunink MGM. Impact of guidelines for the management of minor head injury on the utilization and diagnostic yield of CT over two decades, using natural language processing in a large dataset. Eur Radiol. 2019;29(5):2632–2640. doi: 10.1007/s00330-018-5954-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carpenter CP, Johnston D, Tourville E, Sharadin C, Alzubaidi AN, Giel DW. Inappropriate imaging for management of cryptorchidism: Has the choosing Wisely® recommendation reduced occurrence? J Pediatr Urol. 2020;16(4):462.e1-.e6. [DOI] [PubMed]
- 20.Brink JA. Clinical decision-making tools for exam selection, reporting and dose tracking. Pediatr Radiol. 2014;44(Suppl 3):418–421. doi: 10.1007/s00247-014-3015-z. [DOI] [PubMed] [Google Scholar]
- 21.Armao D, Semelka RC, Elias J., Jr Radiology's ethical responsibility for healthcare reform: tempering the overutilization of medical imaging and trimming down a heavyweight. Journal of magnetic resonance imaging : JMRI. 2012;35(3):512–517. doi: 10.1002/jmri.23530. [DOI] [PubMed] [Google Scholar]
- 22.Allen J, King R, Goergen SK, Melder A, Neeman N, Hadley A, Hutchinson AM. Semistructured interviews regarding patients' perceptions of choosing wisely and shared decision-making: an Australian study. BMJ Open. 2019;9(8):e031831. doi: 10.1136/bmjopen-2019-031831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iyengar R, Winkels JL, Smith CM, Meka AP, Porath JD, Meurer WJ. The effect of financial incentives on patient decisions to undergo low-value head computed tomography scans. Acad Emerg Med. 2019;26(10):1117–1124. doi: 10.1111/acem.13823. [DOI] [PubMed] [Google Scholar]
- 24.Tejedor-Sojo J, Chan KN, Bailey M, Williams A, Killgore M, Gillard L, Campo M, Hua H, Jain S. Improving bronchiolitis Care in Outpatient Settings across a health care system. Pediatr Emerg Care. 2019;35(11):791–798. doi: 10.1097/PEC.0000000000001966. [DOI] [PubMed] [Google Scholar]
- 25.Colla CH. Swimming against the current--what might work to reduce low-value care? N Engl J Med. 2014;371(14):1280–1283. doi: 10.1056/NEJMp1404503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colla CH, Mainor AJ, Hargreaves C, Sequist T, Morden N. Interventions aimed at reducing use of low-value health services: a systematic review. Med Care Res Rev. 2017;74(5):507–550. doi: 10.1177/1077558716656970. [DOI] [PubMed] [Google Scholar]
- 27.Ebdon-Jackson S, Frija G, European Society of R Improving justification of medical exposures using ionising radiation: considerations and approaches from the European Society of Radiology. Insights into Imaging. 2021;12(1):2. doi: 10.1186/s13244-020-00940-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garrubba M, Melder A. Interventions to reduce unnecessary imaging, tests and procedures in hospitals. Centre for Clinical Effectiveness, Monash Health. 2016
- 29.Vest JR, Jung HY, Ostrovsky A, Das LT, McGinty GB. Image Sharing Technologies and Reduction of Imaging Utilization: A Systematic Review and Meta-analysis. J Am Coll Radiol. 2015;12(12 Pt B):1371–9.e3. [DOI] [PMC free article] [PubMed]
- 30.Muhiyaddin R, Abd-Alrazaq AA, Househ M, Alam T, Shah Z. The impact of clinical decision support systems (CDSS) on physicians: a scoping review. Stud Health Technol Inform. 2020;272:470–473. doi: 10.3233/SHTI200597. [DOI] [PubMed] [Google Scholar]
- 31.Suman A, Armijo-Olivo S, Deshpande S, Marietta-Vasquez J, Dennett L, Miciak M, et al. A systematic review of the effectiveness of mass media campaigns for the management of low back pain. Disabil Rehabil. 2020:1–29. 10.1080/09638288.2020.1743777. [DOI] [PubMed]
- 32.Desai S, Liu C, Kirkland SW, Krebs LD, Keto-Lambert D, Rowe BH. Effectiveness of implementing evidence-based interventions to reduce C-spine image ordering in the emergency department: a systematic review. Acad Emerg Med. 2018;25(6):672–683. doi: 10.1111/acem.13364. [DOI] [PubMed] [Google Scholar]
- 33.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic Reviews. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. Journal of Clinical Epidemiology. 2019;111:49–59.e1. [DOI] [PubMed]
- 35.CADTH. Grey Matters: a practical tool for searching health-related grey literature 2019 [Available from: https://www.cadth.ca/resources/finding-evidence/grey-matters.
- 36.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1:b92. [Google Scholar]
- 37.Ashikyan O, Buller DC, Pezeshk P, McCrum C, Chhabra A. Reduction of unnecessary repeat knee radiographs during osteoarthrosis follow-up visits in a large teaching medical center. Skelet Radiol. 2019;48(12):1975–1980. doi: 10.1007/s00256-019-03247-4. [DOI] [PubMed] [Google Scholar]
- 38.Bailey JE, Pope RA, Elliott EC, Wan JY, Waters TM, Frisse ME. Health information exchange reduces repeated diagnostic imaging for back pain. Ann Emerg Med. 2013;62(1):16–24. doi: 10.1016/j.annemergmed.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 39.Bailey JE, Wan JY, Mabry LM, Landy SH, Pope RA, Waters TM, Frisse ME. Does health information exchange reduce unnecessary neuroimaging and improve quality of headache care in the emergency department? J Gen Intern Med. 2013;28(2):176–183. doi: 10.1007/s11606-012-2092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bairstow PJ, Persaud J, Mendelson R, Nguyen L. Reducing inappropriate diagnostic practice through education and decision support. Int J Qual Health Care. 2010;22(3):194–200. doi: 10.1093/intqhc/mzq016. [DOI] [PubMed] [Google Scholar]
- 41.Baker M, Jaeger C, Hafley C, Waymack J. Appropriate CT cervical spine utilisation in the emergency department. BMJ Open Qual. 2020;9(4). [DOI] [PMC free article] [PubMed]
- 42.Bhatia RS, Dudzinski DM, Malhotra R, Milford CE, Yoerger Sanborn DM, Picard MH, Weiner RB. Educational intervention to reduce outpatient inappropriate echocardiograms: a randomized control trial. JACC Cardiovasc Imaging. 2014;7(9):857–866. doi: 10.1016/j.jcmg.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 43.Bhatia RS, Ivers NM, Yin XC, Myers D, Nesbitt GC, Edwards J, Yared K, Wadhera RK, Wu JC, Kithcart AP, Wong BM, Hansen MS, Weinerman AS, Shadowitz S, Elman D, Farkouh ME, Thavendiranathan P, Udell JA, Johri AM, Chow CM, Hall J, Bouck Z, Cohen A, Thorpe KE, Rakowski H, Picard MH, Weiner RB. Improving the appropriate use of transthoracic echocardiography: the Echo WISELY trial. J Am Coll Cardiol. 2017;70(9):1135–1144. doi: 10.1016/j.jacc.2017.06.065. [DOI] [PubMed] [Google Scholar]
- 44.Bhatia RS, Milford CE, Picard MH, Weiner RB. An educational intervention reduces the rate of inappropriate echocardiograms on an inpatient medical service. JACC Cardiovasc Imaging. 2013;6(5):545–555. doi: 10.1016/j.jcmg.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 45.Blackmore CC, Mecklenburg RS, Kaplan GS. Effectiveness of clinical decision support in controlling inappropriate imaging. J Am Coll Radiol. 2011;8(1):19–25. doi: 10.1016/j.jacr.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 46.Bookman K, West D, Ginde A, Wiler J, McIntyre R, Hammes A, et al. Embedded clinical decision support in electronic health record decreases use of high-cost imaging in the emergency department: EmbED study. Acad Emerg Med. 2017;24(7):839–845. doi: 10.1111/acem.13195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boutis K, Grootendorst P, Willan A, Plint AC, Babyn P, Brison RJ, Sayal A, Parker M, Mamen N, Schuh S, Grimshaw J, Johnson D, Narayanan U. Effect of the low risk ankle rule on the frequency of radiography in children with ankle injuries. Cmaj. 2013;185(15):E731–E738. doi: 10.1503/cmaj.122050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Breakell R, Thorndyke B, Clennett J, Harkensee C. Reducing unnecessary chest X-rays, antibiotics and bronchodilators through implementation of the NICE bronchiolitis guideline. Eur J Pediatr. 2018;177(1):47–51. doi: 10.1007/s00431-017-3034-5. [DOI] [PubMed] [Google Scholar]
- 49.Buntine P, Thien F, Stewart J, Woo YP, Koolstra M, Bridgford L, et al. Effect of a clinical flowchart incorporating Wells score, PERC rule and age-adjusted D-dimer on pulmonary embolism diagnosis, scan rates and diagnostic yield. Emerg Med Australas. 2019;31(2):216–224. doi: 10.1111/1742-6723.13125. [DOI] [PubMed] [Google Scholar]
- 50.Carpenter CP, Johnston D, Tourville E, Sharadin C, Alzubaidi AN, Giel DW. Inappropriate imaging for management of cryptorchidism: Has the choosing Wisely(R) recommendation reduced occurrence? J Pediatr Urol. 2020;16(4):462 e1- e6. [DOI] [PubMed]
- 51.Chandra K, Atkinson PR, Chatur H, Fraser J, Adams CL. To choose or not to choose: evaluating the effect of a choosing wisely knowledge translation initiative for imaging in low Back pain by emergency physicians. Cureus. 2019;11(2):e4002. doi: 10.7759/cureus.4002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang E, Buist DSM, Ley M, Johnson E, Fuller S, Pardee R, et al. Primary care physician resource use changes associated with feedback reports. Am J Manag Care. 2018;24(10):455–461. [PubMed] [Google Scholar]
- 53.Char S, Yoon HC. Improving appropriate use of pulmonary computed tomography angiography by increasing the serum D-dimer threshold and assessing clinical probability. Perm J. 2014;18(4):10–15. doi: 10.7812/TPP/14-007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen D, Bhambhvani HP, Hom J, Mahoney M, Wintermark M, Sharp C, Ratliff J, Chen YR. Effect of electronic clinical decision support on imaging for the evaluation of acute low Back pain in the ambulatory care setting. World Neurosurg. 2020;134:e874–e8e7. doi: 10.1016/j.wneu.2019.11.031. [DOI] [PubMed] [Google Scholar]
- 55.Chien AT, Lehmann LS, Hatfield LA, Koplan KE, Petty CR, Sinaiko AD, Rosenthal MB, Sequist TD. A randomized trial of displaying paid Price information on imaging study and procedure ordering rates. J Gen Intern Med. 2017;32(4):434–448. doi: 10.1007/s11606-016-3917-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Depinet H, von Allmen D, Towbin A, Hornung R, Ho M, Alessandrini E. Risk Stratification to Decrease Unnecessary Diagnostic Imaging for Acute Appendicitis. Pediatrics. 2016;138(3). [DOI] [PubMed]
- 57.Doyle J, Abraham S, Feeney L, Reimer S, Finkelstein A. Clinical decision support for high-cost imaging: a randomized clinical trial. PLoS One. 2019;14(3):e0213373. doi: 10.1371/journal.pone.0213373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drescher FS, Chandrika S, Weir ID, Weintraub JT, Berman L, Lee R, van Buskirk PD, Wang Y, Adewunmi A, Fine JM. Effectiveness and acceptability of a computerized decision support system using modified Wells criteria for evaluation of suspected pulmonary embolism. Ann Emerg Med. 2011;57(6):613–621. doi: 10.1016/j.annemergmed.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 59.Dudzinski DM, Bhatia RS, Mi MY, Isselbacher EM, Picard MH, Weiner RB. Effect of educational intervention on the rate of rarely appropriate outpatient echocardiograms ordered by attending academic cardiologists: a randomized clinical trial. JAMA Cardiol. 2016;1(7):805–812. doi: 10.1001/jamacardio.2016.2232. [DOI] [PubMed] [Google Scholar]
- 60.Dunne RM, Ip IK, Abbett S, Gershanik EF, Raja AS, Hunsaker A, Khorasani R. Effect of evidence-based clinical decision support on the use and yield of CT pulmonary angiographic imaging in hospitalized patients. Radiology. 2015;276(1):167–174. doi: 10.1148/radiol.15141208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108–113. doi: 10.1016/j.jacr.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 62.Fallon SC, Delemos D, Akinkuotu A, Christopher D, Naik-Mathuria BJ. The use of an institutional pediatric abdominal trauma protocol improves resource use. J Trauma Acute Care Surg. 2016;80(1):57–63. doi: 10.1097/TA.0000000000000712. [DOI] [PubMed] [Google Scholar]
- 63.Ferguson CC, Gray MP, Diaz M, Boyd KP. Reducing Unnecessary Imaging for Patients With Constipation in the Pediatric Emergency Department. Pediatrics. 2017;140(1). [DOI] [PubMed]
- 64.Flamm M, Fritsch G, Hysek M, Klausner S, Entacher K, Panisch S, Soennichsen AC. Quality improvement in preoperative assessment by implementation of an electronic decision support tool. J Am Med Inform Assoc. 2013;20(e1):e91–e96. doi: 10.1136/amiajnl-2012-001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.French SD, McKenzie JE, O'Connor DA, Grimshaw JM, Mortimer D, Francis JJ, et al. Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PLoS One. 2013;8(6):e65471. doi: 10.1371/journal.pone.0065471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gertz ZM, O'Donnell W, Raina A, Balderston JR, Litwack AJ, Goldberg LR. Implementation of a computerized order entry tool to reduce the inappropriate and unnecessary use of cardiac stress tests with imaging in hospitalized patients. Am J Cardiol. 2016;118(8):1123–1127. doi: 10.1016/j.amjcard.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 67.Goldberg J, McClaine RJ, Cook B, Garcia VF, Brown RL, Crone K, et al. Use of a mild traumatic brain injury guideline to reduce inpatient hospital imaging and charges. J Pediatr Surg. 2011;46(9):1777–1783. doi: 10.1016/j.jpedsurg.2011.02.052. [DOI] [PubMed] [Google Scholar]
- 68.Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin GM. Impact of an advanced imaging utilization review program on downstream health care utilization and costs for low Back pain. Med Care. 2018;56(6):520–528. doi: 10.1097/MLR.0000000000000917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hardin L, Kilian A, Muller L, Callison K, Olgren M. Cross-continuum tool is associated with reduced utilization and cost for frequent high-need users. West J Emerg Med. 2017;18(2):189–200. doi: 10.5811/westjem.2016.11.31916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hess EP, Homme JL, Kharbanda AB, Tzimenatos L, Louie JP, Cohen DM, et al. Effect of the Head Computed Tomography Choice Decision Aid in Parents of Children With Minor Head Trauma: A Cluster Randomized Trial. JAMA Netw Open. 2018;1(5):e182430-e. [DOI] [PMC free article] [PubMed]
- 71.Hong AS, Ross-Degnan D, Zhang F, Wharam JF. Small decline in low-value Back imaging associated with the 'Choosing Wisely' campaign, 2012-14. Health Aff (Millwood) 2017;36(4):671–679. doi: 10.1377/hlthaff.2016.1263. [DOI] [PubMed] [Google Scholar]
- 72.Hoo GW, Wu CC, Vazirani S, Li Z, Barack BM. Does a clinical decision rule using D-dimer level improve the yield of pulmonary CT angiography? AJR Am J Roentgenol. 2011;196(5):1059–1064. doi: 10.2214/AJR.10.4200. [DOI] [PubMed] [Google Scholar]
- 73.Hui JS, Kramer DJ, Blackmore CC, Hashimoto BE, Coy DL. A quality improvement initiative to reduce unnecessary follow-up imaging for adnexal lesions. J Am Coll Radiol. 2014;11(4):373–377. doi: 10.1016/j.jacr.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 74.Hurley P, Dhir A, Gao Y, Drabik B, Lim K, Curry J, Womble PR, Linsell SM, Brachulis A, Sexton DW, Ghani KR, Denton BT, Miller DC, Montie JE, Michigan Urological Surgery Improvement Collaborative A statewide intervention improves appropriate imaging in localized prostate Cancer. J Urol. 2017;197(5):1222–1228. doi: 10.1016/j.juro.2016.11.098. [DOI] [PubMed] [Google Scholar]
- 75.Ip IK, Gershanik EF, Schneider LI, Raja AS, Mar W, Seltzer S, Healey MJ, Khorasani R. Impact of IT-enabled intervention on MRI use for back pain. Am J Med. 2014;127(6):512–518. doi: 10.1016/j.amjmed.2014.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ip IK, Lacson R, Hentel K, Malhotra S, Darer J, Langlotz C, Weiss J, Raja AS, Khorasani R. JOURNAL CLUB: predictors of provider response to clinical decision support: lessons learned from the Medicare imaging demonstration. AJR Am J Roentgenol. 2017;208(2):351–357. doi: 10.2214/AJR.16.16373. [DOI] [PubMed] [Google Scholar]
- 77.Ip IK, Raja AS, Gupta A, Andruchow J, Sodickson A, Khorasani R. Impact of clinical decision support on head computed tomography use in patients with mild traumatic brain injury in the ED. Am J Emerg Med. 2015;33(3):320–325. doi: 10.1016/j.ajem.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 78.Ip IK, Schneider L, Seltzer S, Smith A, Dudley J, Menard A, Khorasani R. Impact of provider-led, technology-enabled radiology management program on imaging. Am J Med. 2013;126(8):687–692. doi: 10.1016/j.amjmed.2012.11.034. [DOI] [PubMed] [Google Scholar]
- 79.Jennings RM, Burtner JJ, Pellicer JF, Nair DK, Bradford MC, Shaffer M, et al. Reducing Head CT Use for Children With Head Injuries in a Community Emergency Department. Pediatrics. 2017;139(4). [DOI] [PubMed]
- 80.Judkins A, Pascoe E, Payne D. Management of urinary tract infection in a tertiary children's hospital before and after publication of the NICE guidelines. Arch Dis Child. 2013;98(7):521–525. doi: 10.1136/archdischild-2012-303032. [DOI] [PubMed] [Google Scholar]
- 81.Kandiah JW, Chan VWY, Luo J, Dong F, Nugent JP, Forster BB. Reducing the volume of low-value outpatient MRI joint Examinations in Patients >/=55 years of age. Can Assoc Radiol J. 2020;71(1):83–91. doi: 10.1177/0846537119885686. [DOI] [PubMed] [Google Scholar]
- 82.Kanaan Y, Knoepp UD, Kelly AM. The influence of education on appropriateness rates for CT pulmonary angiography in emergency department patients. Acad Radiol. 2013;20(9):1107–1114. doi: 10.1016/j.acra.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 83.Keveson B, Clouser RD, Hamlin MP, Stevens P, Msn RN, Stinnett-Donnelly JM, Allen GB. Adding value to daily chest X-rays in the ICU through education, restricted daily orders and indication-based prompting. BMJ Open Qual. 2017;6(2):e000072. doi: 10.1136/bmjoq-2017-000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lacson R, Ip I, Hentel KD, Malhotra S, Balthazar P, Langlotz CP, Raja AS, Khorasani R. Medicare imaging demonstration: assessing attributes of appropriate use criteria and their influence on ordering behavior. AJR Am J Roentgenol. 2017;208(5):1051–1057. doi: 10.2214/AJR.16.17169. [DOI] [PubMed] [Google Scholar]
- 85.Lu MT, Tellis WM, Fidelman N, Qayyum A, Avrin DE. Reducing the rate of repeat imaging: import of outside images to PACS. AJR Am J Roentgenol. 2012;198(3):628–634. doi: 10.2214/AJR.11.6890. [DOI] [PubMed] [Google Scholar]
- 86.Luther G, Miller PE, Mahan ST, Waters PM, Bae DS. Decreasing resource utilization using standardized clinical assessment and management plans (SCAMPs) J Pediatr Orthop. 2019;39(4):169–174. doi: 10.1097/BPO.0000000000000873. [DOI] [PubMed] [Google Scholar]
- 87.Masood S, Woolner V, Yoon JH, Chartier LB. Checklist for Head Injury Management Evaluation Study (CHIMES): a quality improvement initiative to reduce imaging utilisation for head injuries in the emergency department. BMJ Open Qual. 2020;9(1). [DOI] [PMC free article] [PubMed]
- 88.McGrew PR, Chestovich PJ, Fisher JD, Kuhls DA, Fraser DR, Patel PP, et al. Implementation of a CT scan practice guideline for pediatric trauma patients reduces unnecessary scans without impacting outcomes. J Trauma Acute Care Surg. 2018;85(3):451–458. doi: 10.1097/TA.0000000000001974. [DOI] [PubMed] [Google Scholar]
- 89.Min A, Chan VWY, Aristizabal R, Peramaki ER, Agulnik DB, Strydom N, Ramsey D, Forster BB. Clinical decision support decreases volume of imaging for low Back pain in an urban emergency department. J Am Coll Radiol. 2017;14(7):889–899. doi: 10.1016/j.jacr.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 90.Mittal V, Darnell C, Walsh B, Mehta A, Badawy M, Morse R, Pop R, Tidwell J, Sheehan M, McDermott S, Cannon C, Kahn J. Inpatient bronchiolitis guideline implementation and resource utilization. Pediatrics. 2014;133(3):e730–e737. doi: 10.1542/peds.2013-2881. [DOI] [PubMed] [Google Scholar]
- 91.Moriarity AK, Klochko C, O'Brien M, Halabi S. The effect of clinical decision support for advanced inpatient imaging. J Am Coll Radiol. 2015;12(4):358–363. doi: 10.1016/j.jacr.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 92.Mulders MAM, Walenkamp MMJ, Sosef NL, Ouwehand F, van Velde R, Goslings CJ, Schep NWL. The Amsterdam wrist rules to reduce the need for radiography after a suspected distal radius fracture: an implementation study. Eur J Trauma Emerg Surg. 2020;46(3):573–582. doi: 10.1007/s00068-019-01194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mäenpää T, Asikainen P, Gissler M, Siponen K, Maass M, Saranto K, et al. Outcomes assessment of the regional health information exchange: a five-year follow-up study. Methods Inf Med. 2011;50(4):308–318. doi: 10.3414/ME10-01-0048. [DOI] [PubMed] [Google Scholar]
- 94.Nigrovic LE, Stack AM, Mannix RC, Lyons TW, Samnaliev M, Bachur RG, Proctor MR. Quality improvement effort to reduce cranial CTs for children with minor blunt head trauma. Pediatrics. 2015;136(1):e227–e233. doi: 10.1542/peds.2014-3588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O'Connor SD, Sodickson AD, Ip IK, Raja AS, Healey MJ, Schneider LI, Khorasani R. JOURNAL CLUB: requiring clinical justification to override repeat imaging decision support: impact on CT use. Am J Roentgenol. 2014;203(5):W482–WW90. doi: 10.2214/AJR.14.13017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ostby SA, Evans JG, Smith HJ, Boitano TKL, Toboni MD, Heimann MA, Booth JS, Thomas JJ, Michael Straughn J., Jr Reducing emergency department (ED) computed tomography (CT) utilization in women treated for gynecologic cancers. Gynecol Oncol. 2020;156(2):288–292. doi: 10.1016/j.ygyno.2019.11.024. [DOI] [PubMed] [Google Scholar]
- 97.Palen TE, Sharpe RE, Jr, Shetterly SM, Steiner JF. Randomized clinical trial of a clinical decision support tool for improving the appropriateness scores for ordering imaging studies in primary and specialty care ambulatory clinics. AJR Am J Roentgenol. 2019;213(5):1015–1020. doi: 10.2214/AJR.19.21511. [DOI] [PubMed] [Google Scholar]
- 98.Parikh K, Hall M, Blaschke AJ, Grijalva CG, Brogan TV, Neuman MI, et al. Aggregate and hospital-level impact of national guidelines on diagnostic resource utilization for children with pneumonia at children's hospitals. J Hosp Med. 2016;11(5):317–323. doi: 10.1002/jhm.2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Poeran J, Mao LJ, Zubizarreta N, Mazumdar M, Darrow B, Genes N, Kannry J, Francaviglia P, Kennelly PD, Whitehorn J, Kilroy G, Garcia D, Mendelson DS. Effect of clinical decision support on appropriateness of advanced imaging use among physicians-in-training. AJR Am J Roentgenol. 2019;212(4):859–866. doi: 10.2214/AJR.18.19931. [DOI] [PubMed] [Google Scholar]
- 100.Prevedello LM, Raja AS, Ip IK, Sodickson A, Khorasani R. Does clinical decision support reduce unwarranted variation in yield of CT pulmonary angiogram? Am J Med. 2013;126(11):975–981. doi: 10.1016/j.amjmed.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pugel S, Stallworth JL, Pugh LB, Terrell C, Bailey Z, Gramling T, Ward H. Choosing wisely in Georgia: a quality improvement initiative in 25 adult ambulatory medicine offices. Jt Comm J Qual Patient Saf. 2018;44(12):699–707. doi: 10.1016/j.jcjq.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 102.Raja AS, Ip IK, Dunne RM, Schuur JD, Mills AM, Khorasani R. Effects of performance feedback reports on adherence to evidence-based guidelines in use of CT for evaluation of pulmonary embolism in the emergency department: a randomized trial. AJR Am J Roentgenol. 2015;205(5):936–940. doi: 10.2214/AJR.15.14677. [DOI] [PubMed] [Google Scholar]
- 103.Raja AS, Ip IK, Prevedello LM, Sodickson AD, Farkas C, Zane RD, et al. Effect of computerized clinical decision support on the use and yield of CT pulmonary angiography in the emergency department. Radiology. 2012;262(2):468–474. doi: 10.1148/radiol.11110951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Reiter J, Breuer A, Breuer O, Hashavya S, Rekhtman D, Kerem E, Cohen-Cymberknoh M. A quality improvement intervention to reduce emergency department radiography for bronchiolitis. Respir Med. 2018;137:1–5. doi: 10.1016/j.rmed.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 105.Rezaii PG, Fredericks N, Lincoln CM, Hom J, Willis M, Burleson J, Haines GR, Chatfield M, Boothroyd D, Ding VY, Bello JA, McGinty GB, Smith C(D), Yucel EK, Hillman B, Thorwarth WT, Jr, Wintermark M. Assessment of the radiology support, communication and alignment network to reduce medical imaging overutilization: a multipractice cohort study. J Am Coll Radiol. 2020;17(5):597–605. doi: 10.1016/j.jacr.2020.02.011. [DOI] [PubMed] [Google Scholar]
- 106.Rosati SF, Maarouf R, Wolfe L, Parrish D, Poppe M, Manners R, Brown K, Haynes JH. Implementation of pediatric cervical spine clearance guidelines at a combined trauma center: twelve-month impact. J Trauma Acute Care Surg. 2015;78(6):1117–1121. doi: 10.1097/TA.0000000000000643. [DOI] [PubMed] [Google Scholar]
- 107.Sclafani JJ, My J, Zacher LL, Eckart RE. Intensive education on evidence-based evaluation of syncope increases sudden death risk stratification but fails to reduce use of neuroimaging. Arch Intern Med. 2010;170(13):1150–1154. doi: 10.1001/archinternmed.2010.205. [DOI] [PubMed] [Google Scholar]
- 108.Shah SR, Sinclair KA, Theut SB, Johnson KM, Holcomb GW, 3rd, St Peter SD. Computed tomography utilization for the diagnosis of acute appendicitis in children decreases with a diagnostic algorithm. Ann Surg. 2016;264(3):474–481. doi: 10.1097/SLA.0000000000001867. [DOI] [PubMed] [Google Scholar]
- 109.Singer AJ, Garra G, Thode HC., Jr Changes in practice patterns with the opening of a dedicated pediatric emergency department. Pediatr Emerg Care. 2014;30(10):705–709. doi: 10.1097/PEC.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 110.Sodickson A, Opraseuth J, Ledbetter S. Outside imaging in emergency department transfer patients: CD import reduces rates of subsequent imaging utilization. Radiology. 2011;260(2):408–413. doi: 10.1148/radiol.11101956. [DOI] [PubMed] [Google Scholar]
- 111.Sy E, Luong M, Quon M, Kim Y, Sharifi S, Norena M, Wong H, Ayas N, Leipsic J, Dodek P. Implementation of a quality improvement initiative to reduce daily chest radiographs in the intensive care unit. BMJ Qual Saf. 2016;25(5):379–385. doi: 10.1136/bmjqs-2015-004151. [DOI] [PubMed] [Google Scholar]
- 112.Tyler A, Krack P, Bakel LA, O'Hara K, Scudamore D, Topoz I, et al. Interventions to Reduce Over-Utilized Tests and Treatments in Bronchiolitis. Pediatrics. 2018;141(6). [DOI] [PubMed]
- 113.Vartanians VM, Sistrom CL, Weilburg JB, Rosenthal DI, Thrall JH. Increasing the appropriateness of outpatient imaging: effects of a barrier to ordering low-yield examinations. Radiology. 2010;255(3):842–849. doi: 10.1148/radiol.10091228. [DOI] [PubMed] [Google Scholar]
- 114.Walker D, Macdonald DB, Dennie C, Afkham A, Liddy C, Keely E. Electronic consultation between primary care providers and radiologists. AJR Am J Roentgenol. 2020;215(4):929–933. doi: 10.2214/AJR.19.22270. [DOI] [PubMed] [Google Scholar]
- 115.Wang KY, Yen CJ, Chen M, Variyam D, Acosta TU, Reed B, et al. Reducing Inappropriate Lumbar Spine MRI for Low Back Pain: Radiology Support, Communication and Alignment Network. J Am Coll Radiol. 2018;15(1 Pt A):116–22. [DOI] [PubMed]
- 116.Wu Y, Rose MQ, Freeman ML, Richard-Lany NP, Spaulding AC, Booth SC, Kelly DL, Franco PM. Reducing chest radiography utilization in the medical intensive care unit. J Am Assoc Nurse Pract. 2020;32(5):390–399. doi: 10.1097/JXX.0000000000000256. [DOI] [PubMed] [Google Scholar]
- 117.Xu SS, Berkovitz N, Li O, Garvin G. Reduction in inappropriate MRI knee studies after implementation of an appropriateness checklist: Experience at a tertiary care centre. Eur J Radiol. 2020;123:108781. doi: 10.1016/j.ejrad.2019.108781. [DOI] [PubMed] [Google Scholar]
- 118.Zafar HM, Ip IK, Mills AM, Raja AS, Langlotz CP, Khorasani R. Effect of clinical decision support-generated report cards versus real-time alerts on primary care provider guideline adherence for low Back pain outpatient lumbar spine MRI orders. AJR Am J Roentgenol. 2019;212(2):386–394. doi: 10.2214/AJR.18.19780. [DOI] [PubMed] [Google Scholar]
- 119.Zamora-Flores D, Busen NH, Smout R, Velasquez O. Implementing a clinical practice guideline for the treatment of bronchiolitis in a high-risk Hispanic pediatric population. J Pediatr Health Care. 2015;29(2):169–180. doi: 10.1016/j.pedhc.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 120.Levitt K, Edwards J, Chow CM, Bhatia RS. Development of an educational strategy and decision support tool to enhance appropriate use of stress echocardiography at a large Academic Medical Center: a prospective, pre- and Postintervention analysis. J Am Soc Echocardiogr. 2015;28(12):1401–1409. doi: 10.1016/j.echo.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 121.Mills AM, Ip IK, Langlotz CP, Raja AS, Zafar HM, Khorasani R. Clinical decision support increases diagnostic yield of computed tomography for suspected pulmonary embolism. Am J Emerg Med. 2018;36(4):540–544. doi: 10.1016/j.ajem.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ong CW, Malipatil V, Lavercombe M, Teo KG, Coughlin PB, Leach D, et al. Implementation of a clinical prediction tool for pulmonary embolism diagnosis in a tertiary teaching hospital reduces the number of computed tomography pulmonary angiograms performed. Intern Med J. 2013;43(2):169–174. doi: 10.1111/j.1445-5994.2012.02926.x. [DOI] [PubMed] [Google Scholar]
- 123.Puffenbarger MS, Ahmad FA, Argent M, Gu H, Samson C, Quayle KS, Saito JM. Reduction of computed tomography use for pediatric closed head injury evaluation at a nonpediatric community emergency department. Acad Emerg Med. 2019;26(7):784–795. doi: 10.1111/acem.13666. [DOI] [PubMed] [Google Scholar]
- 124.Tajmir S, Raja AS, Ip IK, Andruchow J, Silveira P, Smith S, Khorasani R. Impact of clinical decision support on radiography for acute ankle injuries: a randomized trial. West J Emerg Med. 2017;18(3):487–495. doi: 10.5811/westjem.2017.1.33053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Walen S, de Boer E, Edens MA, van der Worp CA, Boomsma MF, van den Berg JW. Mandatory adherence to diagnostic protocol increases the yield of CTPA for pulmonary embolism. Insights Imaging. 2016;7(5):727–734. doi: 10.1007/s13244-016-0509-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Arora R, White EN, Niedbala D, Ravichandran Y, Sethuraman U, Radovic N, Watson K, Nypaver M. Reducing computed tomography scan utilization for pediatric minor head injury in the emergency department: a quality improvement initiative. Acad Emerg Med. 2020;28(6):655–665. doi: 10.1111/acem.14177. [DOI] [PubMed] [Google Scholar]
- 127.Ballard DW, Kuppermann N, Vinson DR, Tham E, Hoffman JM, Swietlik M, Deakyne Davies SJ, Alessandrini EA, Tzimenatos L, Bajaj L, Mark DG, Offerman SR, Chettipally UK, Paterno MD, Schaeffer MH, Richards R, Casper TC, Goldberg HS, Grundmeier RW, Dayan PS, Pediatric Emergency Care Applied Research Network (PECARN) Clinical Research on Emergency Services and Treatment (CREST) Network. Partners HealthCare Implementation of a clinical decision support system for children with minor blunt head trauma who are at nonnegligible risk for traumatic brain injuries. Ann Emerg Med. 2019;73(5):440–451. doi: 10.1016/j.annemergmed.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 128.Carnevale TJ, Meng D, Wang JJ, Littlewood M. Impact of an emergency medicine decision support and risk education system on computed tomography and magnetic resonance imaging use. J Emerg Med. 2015;48(1):53–57. doi: 10.1016/j.jemermed.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 129.Ehrlichman R, Dezman Z, Klein J, Jeudy J, Lemkin D. Quarterly reporting of computed tomography ordering history reduces the use of imaging in an emergency department. J Emerg Med. 2017;52(5):684–689. doi: 10.1016/j.jemermed.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 130.Kobes KJ, Budau-Bymoen A, Thakur Y, Yong-Hing CJ. Multidisciplinary development of Mobile radiography guidelines reduced the number of inappropriate Mobile exams in patients receiving chest radiographs in British Columbia. Can Assoc Radiol J. 2020;71(1):110–116. doi: 10.1177/0846537119888357. [DOI] [PubMed] [Google Scholar]
- 131.Shelton JB, Ochotorena L, Bennett C, Shekelle P, Kwan L, Skolarus T, Goldzweig C. Reducing PSA-based prostate Cancer screening in men aged 75 years and older with the use of highly specific computerized clinical decision support. J Gen Intern Med. 2015;30(8):1133–1139. doi: 10.1007/s11606-015-3249-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Keyworth C, Hart J, Armitage CJ, Tully MP. What maximizes the effectiveness and implementation of technology-based interventions to support healthcare professional practice? A systematic literature review. BMC Med Inform Decis Mak. 2018;18(1):93. doi: 10.1186/s12911-018-0661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.de Wit K, Curran J, Thoma B, Dowling S, Lang E, Kuljic N, Perry JJ, Morrison L. Review of implementation strategies to change healthcare provider behaviour in the emergency department. Cjem. 2018;20(3):453–460. doi: 10.1017/cem.2017.432. [DOI] [PubMed] [Google Scholar]
- 135.Weiner BJ, Lewis MA, Clauser SB, Stitzenberg KB. In search of synergy: strategies for combining interventions at multiple levels. J Natl Cancer Inst Monogr. 2012;2012(44):34–41. doi: 10.1093/jncimonographs/lgs001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Salerno S, Laghi A, Cantone MC, Sartori P, Pinto A, Frija G. Overdiagnosis and overimaging: an ethical issue for radiological protection. Radiol Med. 2019;124(8):714–720. doi: 10.1007/s11547-019-01029-5. [DOI] [PubMed] [Google Scholar]
- 137.You JJ, Levinson W, Laupacis A. Attitudes of family physicians, specialists and radiologists about the use of computed tomography and magnetic resonance imaging in Ontario. Healthc Policy. 2009;5(1):54–65. doi: 10.12927/hcpol.2009.21002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Halpern DJ, Clark-Randall A, Woodall J, Anderson J, Shah K. Reducing imaging utilization in primary care through implementation of a peer comparison dashboard. J Gen Intern Med. 2021;36(1):108–113. doi: 10.1007/s11606-020-06164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Coombs DM, Machado GC, Richards B, Needs C, Buchbinder R, Harris IA, et al. Effectiveness of a multifaceted intervention to improve emergency department care of low back pain: a stepped-wedge, cluster-randomised trial. BMJ Qual Saf. 2021. [DOI] [PubMed]
- 140.Ehrman RR, Malik AN, Smith RK, Kalarikkal Z, Huang A, King RM, et al. Serial use of existing clinical decisions aids can reduce computed tomography pulmonary angiography for pulmonary embolism. Intern Emerg Med. 2021. [DOI] [PubMed]
- 141.Kharbanda AB, Vazquez-Benitez G, Ballard DW, Vinson DR, Chettipally UK, Dehmer SP, et al. Effect of Clinical Decision Support on Diagnostic Imaging for Pediatric Appendicitis: A Cluster Randomized Trial. JAMA Network Open. 2021;4(2):e2036344-e. [DOI] [PMC free article] [PubMed]
- 142.Singh S, Hearps SJC, Borland ML, Dalziel SR, Neutze J, Donath S, Cheek JA, Kochar A, Gilhotra Y, Phillips N, Williams A, Lyttle MD, Bressan S, Hoch JS, Oakley E, Holmes JF, Kuppermann N, Babl FE. The effect of patient observation on cranial computed tomography rates in children with minor head trauma. Acad Emerg Med. 2021;27(9):832–843. doi: 10.1111/acem.13942. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy and hits from database searches.
Additional file 2. Table of excluded studies.
Additional file 3. MMAT registration forms.
Data Availability Statement
Not applicable.