Abstract
As we enter an era of health care that incorporates telehealth for routine provision of care, we can build a system that consciously and proactively includes vulnerable patients, thereby avoiding further exacerbation of health disparities. A practical way to reach out to Latino patients is to use media they already widely use. Rather than expect patients to adapt to suboptimal systems of telehealth care, we can improve telehealth for Latinos by using platforms already familiar to them and thereby refocus telehealth delivery systems to provide patient-centered care. Such care is responsive to patients’ needs and preferences; for Latinos, this includes using digital devices that they actually own (ie, smartphones). Equity-centered telehealth is accessible for all, regardless of linguistic, literacy, and socioeconomic barriers.
Keywords: health services accessibility, health care disparities, telemedicine, vulnerable populations, limited English proficiency, digital divide
INTRODUCTION
Currently, telehealth systems rely on the patient’s having desktop or laptop access, home broadband, and dexterity in navigating and downloading online platforms and applications. Although the COVID-19 pandemic has ushered in broad, accelerated deployment of telehealth across the United States, these accepted models of telemedicine may have left some of the most vulnerable patients behind.
Historically, health care access has favored generally healthy, well-off, English-speaking, or non-Hispanic white (NHW) patients, and telemedicine has followed suit.1–4 Maintaining current approaches to telehealth implementation risks worsening existing health disparities. As more permanent models are put into place, we should conscientiously consider the needs of increasingly diverse patient populations. Rather than maintain systems that are suboptimal for reaching racial/ethnic minorities, we should meet our patients where they already are on the Web, grounding our approach in equity.
Telehealth can be improved for Latinos by refocusing its delivery systems to provide patient-centered care, which focuses on the patients’ needs, is accessible and equitable, and respects patients’ preferences and socioeconomic conditions.5,6 We should act on this opportunity and correct shortcomings of current systems of care, to create inclusive ones that will not exacerbate health disparities. Below we discuss opportunities to optimize telehealth for Latino populations by providing patient-centered telehealth care to ultimately reduce inequities in telehealth access and uptake .
PATIENT-CENTERED TELEHEALTH
Respecting patients’ socioeconomic conditions: hardware access and use among Latinos
Latinos are less likely than NHWs to have a desktop or laptop computer or home broadband,7 but Latino adults own smartphones at rates similar to NHW adults. Although foreign-born Latinos are somewhat less likely to own smartphones, they nonetheless show high usage, at 69%.7 Moreover, almost a quarter of Latino adults rely on their smartphone for online access at home (ie, they have a smartphone but no home broadband) compared to 10% of NHWs.8 To include Latinos, telemedicine systems should ensure access to virtual visits via smartphones, bridging these substantial racial/ethnic differences in computer ownership and internet access.
Respecting patients’ access patterns and preferences: mobile app use among Latinos
Practicing patient-centered care means meeting patients where they already are on the Internet. Despite increasing general patient portal use overall, racial/ethnic minorities, those whose primary language is not English, and patients with lower incomes, education, and health literacy are significantly less likely to use currently available portal websites.1,4,9–11 Limited email address ownership among Latinos contributes to this disparity. One study in northern California indicated that 80% of NHW and Chinese-American seniors could send and receive email, but less than 60% of Latino seniors could, even with help, and less than half had an email address.12
A practical and equitable way to reach out to Latinos is to integrate care via the media they already use, and also use these channels to guide currently nonparticipating patients into telehealth systems. Although usability and use of mobile health apps is limited among vulnerable populations,13,14 Latinos do show a high use of text messaging.15 Moreover, 85% of US Hispanic adults use YouTube, and about half use WhatsApp.16
Latinos use WhatsApp for various reasons. For Latinos, the advantages of WhatsApp include data cost savings, WhatsApp’s popularity in Latin American countries, an easy-to-use interface,17 optional Spanish-language interface, and the ability to use a consumer’s phone number instead of email for registration and identity verification. WhatsApp enables exchange of information via smartphones and interpersonal communication via voice messages, video messages, and end-to-end encrypted audio and video calls, both locally and internationally. This can all be done over Wi-Fi or via a cellular network, making it more affordable and attractive. To provide privacy and enhance data security, WhatsApp uses Signal encryption protocol, which encrypts and decrypts messages using secret keys available only on users’ devices.18 Only the sender and receiver can access the message, so WhatsApp is one of the most secure messaging applications available when appropriate measures are taken, such as limiting access to the device and employing passwords.18,19
To make telemedicine accessible for Latinos, health systems could send patients links via texts or WhatsApp messages, with direct links to enrollment for patient portals, and also provide direct link access to a video visit. These channels could be used in real time at patient registration or even during a patient encounter—for example, to facilitate transition from a phone visit to a video visit. In the longer term, text or WhatsApp messages could become another method for connecting patients to telehealth. To protect privacy, only expiring links could be used. Protected health information can also be avoided in messages. In the short term, while loosened HIPAA requirements around telehealth remain in place,20,21 health care organizations could also use WhatsApp to provide video encounters for Latinos who do not have access to a particular health system’s platform for virtual visits. WhatsApp messaging via phone or desktop can be integrated into existing health system text messaging workflows. To date, messaging apps including Secure Messaging Apps (SMAs) are poorly interoperable with electronic health record systems, and their integration would be an important step.22 Concurrently, partnerships between researchers, government agencies (eg, Office of Minority Health, Office of the National Coordinator for Health Information Technology), and national telehealth organizations could develop best practices for creating and updating mobile telehealth interfaces, to ensure equitable access and usability nationally. They could create guidelines to standardize the user interface, so it is easy to learn and becomes familiar across apps and institutions.
We could also use WhatsApp and text messages to educate and engage patients. Latinos already use WhatsApp to receive and distribute information, including links to articles and YouTube videos. Health systems should capitalize on this by distributing educational materials the same way. YouTube could be used as a powerful source of patient education. Health systems and institutions could curate a YouTube channel, for example, for patient education videos whose links could be shared via WhatsApp and text messages. Using the ways Latino patients already receive information would make telehealth and patient education more accessible for them. This would give patients access to curated online health information free from bias and misinformation. Reaching patients where they already are on the Web will increase equity in telehealth.
Ensuring access for populations with limited digital literacy
Access to patient portals
The Shared Principles of Primary Care recommended by the American Academy of Family Physicians require that care be readily accessible for everyone, both in person and virtually, regardless of linguistic, literacy, or socioeconomic barriers.5 Yet our current vision of telehealth use requires patients to have not only certain devices, but also the digital literacy to use specific software, although, in fact, they may have neither. Health systems increasingly use online patient portals, purportedly to expand patient access and for virtual visits, despite evidence that not all patient subgroups use such portals similarly. Disparities between NHWs and Latinos in patient portal use persist in the US, despite controlling for individual-level differences.23 Yet this is not from patients’ unwillingness to engage, for vulnerable populations do express interest in portals and desire to receive patient-centered portal education.11,24 Reducing structural (technology, broadband, and digital skill access) and system barriers (software usability, support access, language capabilities) to telehealth use would make our systems more accessible and equitable, and would increase success in engaging all populations. As we rely more heavily on new developments in telehealth, such as electronic monitoring,25 this will be increasingly important.
Access to technological support staff
For telemedicine to be accessible for patients who have not had technological training or experience, patients need access to staff who can provide technical support in real time. Dedicated support staff should be hired to help patients register for patient portals and use video visit platform applications, including practice navigating them. Real-time support would help triage problems in establishing a virtual visit, or even help patients practice connecting to video encounters.3 Ensuring that all clinics and health systems can provide such coordinated care can be addressed at the policy level, through requirements and reimbursement for telehealth support staff.26,27
Access to technological skills: building capacity
Health care organizations also should provide resources so patients can learn to use the software and applications for access to telehealth. Better yet, they could even provide broader training in digital skills via YouTube, for many Americans use YouTube across most demographics.15 Such training might include how to recognize reliable vs unreliable sources of online information. Building digital literacy and skills in vulnerable populations would have a meaningful impact on patients in the long term, enabling them to break down structural barriers to access.
Ensuring access for populations with limited English proficiency
Limited English proficiency (LEP) individuals speak English less than “very well.”28 About 30% of Latinos in the US have LEP.28 Patients with LEP consistently receive lower quality of medical care.29–31 Current systems of care are designed for “mainstream,” English-proficient patients, but are ineffective for LEP populations, which makes them function as structural barriers to LEP patient health care and health outcomes.32
Quality patient-centered telehealth care should be equitably accessible for LEP populations. Meeting the language needs of LEP patients at all points of contact is already required by various statutes.33–36 To meet accessibility standards, telehealth platforms should be available in Spanish and provide multilingual support for delivery of services.27 Interpreters’ services can be incorporated directly into video and phone visit platforms. Translation for functions like messages between patients and providers should be built into electronic health record systems, to avoid introducing potentially dangerous errors which might otherwise be caused by relying on free and nonhealth related websites and apps. Such functions could be improved by patient feedback options (eg, patients click on an embedded link at the end of the message to report whether a translation was clear or confusing).
Ensuring access when virtual care is unavailable
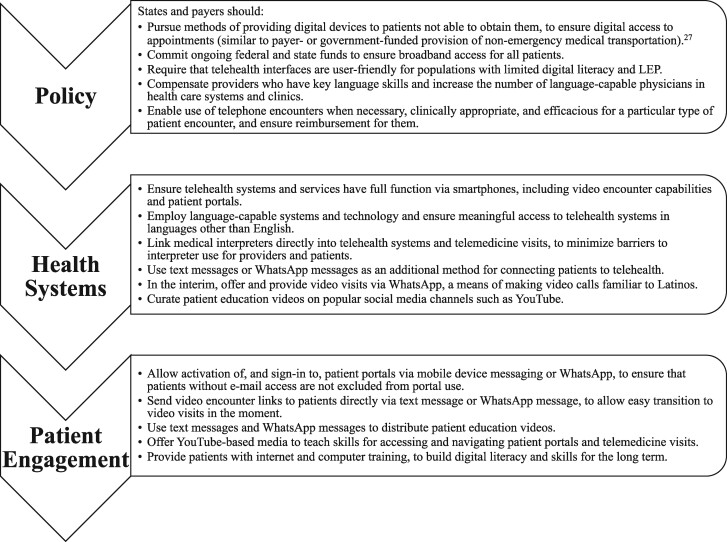
When patients have no access to virtual visits, telephone encounters can be substituted, at least in the short term.37 This stopgap could be supported by payment parity policies, to ensure adequate access to care for all patients.26 Additional state- and payer-level approaches for this are given in Figure 1. While telephone encounters can often be used, in some cases audio-only encounters do not satisfactorily replace in-person or video visits, including in cases in which video visits could be sufficient. When care is provided at a distance, if some patients do not have access to virtual visits but only to audio encounters, how equitable is the health care provided to them, when other populations have access to both? Acknowledging the limitations of telephone encounters should drive health systems to ensure equitable access for all patients to the opportunities and convenience that telemedicine affords. Commitment to preventing further disparities in access and quality of care for Latino populations requires that we ensure providers’ as well as patients’ technological capacity for virtual visits.26
Figure 1.
Opportunities to reduce inequities and provide patient-centered telehealth care.
Limitations and future directions
Our recommendations outline changes to our current models of telehealth, but such changes would have to be encouraged via policy and financial support, as described in Figure 1. Health systems themselves, particularly those in low-resource settings, face challenges to meeting diverse population needs, which underscores the importance of governmental, organizational, and payer support and of aligning policy and funding. Currently, opportunities may exist in COVID-19‒related funding. Future research should include a focus on implementation and dissemination science, to evaluate initiatives and discern hidden or new barriers, and to promote best practices. Solutions for the Latino community are not one-size-fits-all, so we should study telehealth implementation in different Latino populations, by age, nativity, language use, ancestry, etc. Creating a national research agenda on the use of telehealth by other minority and vulnerable populations is vital, focusing on understanding the experience of telehealth from those populations’ perspectives. As Thonon et al state, “it is essential that apps that claim to have a public health objective undergo a rigorous evaluation of their acceptability and efficacy” in including persons of color.38 Our present analysis has been limited by a lack of quantitative data, another area for future research.
CONCLUSION
As health care delivery has shifted rapidly in response to the COVID-19 pandemic, models adopted for providing health care at a distance have left out many who already face too many structural barriers to care. To avoid creating even more barriers for vulnerable populations, we must address the needs of all patients when building innovations for providing health care, so as not to disenfranchise certain communities.
One reason current telehealth care has not been optimally reaching Latinos is that the present system does not account for or address structural barriers that they and other vulnerable communities face. Patient-centered telehealth meets patients where they already are on the Web. Because mobile health app and patient portal use is limited among vulnerable populations, we should incorporate the media they already widely use. To be inclusive of Latinos, telehealth should provide comprehensive access via smartphones, to bridge racial/ethnic differences in computer ownership. Equity-centered telehealth is accessible for all, regardless of linguistic, literacy, and socioeconomic barriers. In the long term, it might even teach patients skills to overcome structural barriers to health care. We will know that we have created a system that includes Latinos when they enroll in and actively use these systems at rates similar to “mainstream” populations.
As we develop how we offer telemedicine in this crucial time of growth, we have an opportunity to provide care that is respectful of, and responsive to, patients’ needs and preferences. We should ensure that the models we adopt for telehealth are truly patient-centered, and, as such, are inclusive of Latinos.
FUNDING
No funding was received for this article.
AUTHOR CONTRIBUTIONS
All those listed as authors have substantially contributed to the underlying research and drafting of the manuscript and are qualified for authorship. All who are qualified to be authors are listed as authors above.
ACKNOWLEDGMENTS
The authors would like to thank Seira Santizo-Greenwood, Chief of Staff of the Center for the Study of Latino Health and Culture (CESLAC), for her instrumental support. The authors are also very grateful to Cynthia L. Chamberlin, CESLAC historian, for her editorial assistance.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY STATEMENT
No new data were generated or analyzed in support of this research.
REFERENCES
- 1.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodman CW, Brett AS.. Accessibility of virtual visits for urgent care among US hospitals: a descriptive analysis [published online ahead of print, May 18, 2020]. J Gen Intern Med 2020; 1–2. doi:10.1007/s11606-020-05888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nouri S, Khoong EC, Lyles CR, Karliner L.. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Deliv 2020. doi: 10.1056/CAT.20.0123. [Google Scholar]
- 4.Walker DM, Hefner JL, Fareed N, Huerta TR, McAlearney AS.. Exploring the digital divide: age and race disparities in use of an inpatient portal. Telemed J E Health 2020; 26 (5): 603–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Primary care collaborative. Shared Principles of Primary Care. https://www.pcpcc.org/about/shared-principles Accessed October 23, 2020.
- 6.What is patient-centered care? NEJM Catal Innov Care Deliv 2017. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559 Accessed October 23, 2020.
- 7.Perrin A, Turner E. Smartphones help blacks, Hispanics bridge some – but not all – digital gaps with whites. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/. Published 2019 Accessed July 27, 2020.
- 8.Horrigan J, Duggan M. Home broadband 2015. Pew Research Center. https://www.pewresearch.org/internet/2015/12/21/1-home-broadband-adoption-modest-decline-from-2013-to-2015/ Accessed May 5, 2021.
- 9.Tieu L, Sarkar U, Schillinger D, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015; 17 (12): e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW.. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26 (10): 1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schickedanz A, Huang D, Lopez A, et al. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J Gen Intern Med 2013; 28 (7): 914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon NP, Hornbrook MC.. Differences in access to and preferences for using patient portals and other ehealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res 2016; 18 (3): e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taha J, Sharit J, Czaja SJ.. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J Appl Gerontol 2014; 33 (4): 416–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarkar U, Gourley GI, Lyles CR, et al. Usability of commercially available mobile applications for diverse patients. J Gen Intern Med 2016; 31 (12): 1417–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duggan M. Cell phone activities 2013. Pew Research Center. https://www.pewresearch.org/internet/2013/09/19/additional-demographic-analysis/ Accessed July 29, 2020.
- 16.Auxier B, Anderson M. Social media use in 2021. 2021. Pew Research Center. https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ Accessed May 5, 2021.
- 17.Koch L. WhatsApp beats out Instagram and Twitter among US Hispanic users. eMarketer. https://www.emarketer.com/content/whatsapp-beats-out-instagram-and-twitter-among-us-hispanic-users Accessed July 28, 2020.
- 18.WhatsApp Security. WhatsApp LLC. https://www.whatsapp.com/security Accessed June 28, 2021.
- 19.Mars M, Morris C, Scott RE.. WhatsApp guidelines – what guidelines? A literature review. J Telemed Telecare 2019; 25 (9): 524–9. [DOI] [PubMed] [Google Scholar]
- 20.Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. US Department of Health and Human Services. Telehealth Discretion During Coronavirus Web site. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Accessed July 28, 2020.
- 21.FAQs on Telehealth and HIPAA during the COVID-19 nationwide, public health emergency. US Department of Health and Human Services. https://www.hhs.gov/sites/default/files/telehealth-faqs-508.pdf Accessed July 28, 2020.
- 22.Masoni M, Guelfi MR.. WhatsApp and other messaging apps in medicine: opportunities and risks. Intern Emerg Med 2020; 15 (2): 171–3. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez M, Sanders-Jackson A, Wright T.. Web-based health information technology: access among Latinos varies by subgroup affiliation. J Med Internet Res 2019; 21 (4): e10389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Casillas A, Perez-Aguilar G, Abhat A, et al. Su salud a la mano (your health at hand): patient perceptions about a bilingual patient portal in the Los Angeles safety net. J Am Med Inform Assoc 2019; 26 (12): 1525–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 2017; 318 (2): 197–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anaya YB, Martinez LE, Bustamante AV, et al. Telehealth & COVID-19 policy considerations to improve access to care. Center for the Study of Latino Health and Culture (CESLAC), UCLA Health, and the Latino Policy & Politics Initiative at UCLA. https://latino.ucla.edu/research/telehealth-covid-19-policy-considerations-to-improve-access-to-care/ Accessed July 28, 2020.
- 27.Kim J-H, Desai E, Cole MB. How the rapid shift to telehealth leaves many community health centers behind during the COVID-19 pandemic. Health Affairs Blog. June 2, 2020. doi:10.1377/hblog20200529.449762.
- 28.2015–2019 American Community Survey 5-year estimates detailed tables: Table B16006 language spoken at home by ability to speak english for the population 5 years and over (Hispanic or Latino). US Census Bureau. https://data.census.gov/cedsci/table?q=LANGUAGE%20SPOKEN%20AT%20HOME%20by%20ability,%20Hispanic%20or%20Latino&g=0100000US&tid=ACSDT5Y2019.B16006&hidePreview=true Accessed May 13, 2021.
- 29.Steinberg EM, Valenzuela-Araujo D, Zickafoose JS, Kieffer E, DeCamp LR.. The “battle” of managing language barriers in health care. Clin Pediatr (Phila) 2016; 55 (14): 1318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A.. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med 2005; 20 (9): 800–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Divi C, Koss RG, Schmaltz SP, Loeb JM.. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care 2007; 19 (2): 60–7. [DOI] [PubMed] [Google Scholar]
- 32.Green AR, Nze C.. Language-based inequity in health care: who is the “poor historian”? AMA J Ethics 2017; 19 (3): 60–7. [DOI] [PubMed] [Google Scholar]
- 33.Guidance to federal financial assistance recipients regarding Title VI prohibition against national origin discrimination affecting limited English proficient persons. US Department of Health and Human Services. http://www.hhs.gov/civil-rights/for-individuals/special-topics/limited-english-proficiency/guidance-federal-financial-assistance-recipients-title-VI/ Accessed August 3 2020.
- 34.The National CLAS Standards. US Department of Health and Human Services, Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=53 Updated October 2, 2018. Accessed August 3, 2020.
- 35.National standards for culturally and linguistically appropriate services in health care: a blueprint for advancing and sustaining CLAS policy and practice. U.S. Department of Health and Human Services, Office of Minority Health; 2013: 1–192. https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedCLASStandardsBlueprint.pdf Accessed August 3, 2020. [Google Scholar]
- 36.The Joint Commission: Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals. Oakbrook Terrace, IL: The Joint Commission; 2010. https://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf Accessed August 3, 2020.
- 37.Bashshur RL, Doarn CR, Frenk JM, Kvedar JC, Shannon GW, Woolliscroft JO.. Beyond the COVID pandemic, telemedicine, and health care. Telemed J E Health 2020; 26 (11): 1310–3. [DOI] [PubMed] [Google Scholar]
- 38.Thonon F, Perrot S, Yergolkar AV, et al. Electronic tools to bridge the language gap in health care for people who have migrated: systematic review. J Med Internet Res 2021; 23 (5): e25131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analyzed in support of this research.