Abstract
Objectives
Task-specific movement training is a proposed intervention for patellofemoral pain aimed to optimise movement during daily tasks. Focused, progressive task practice emphasising optimal limb alignment may yield improvements in performance-based function and hip muscle strength, and transfer learnt movement patterns to untrained tasks. The purpose of this study was to determine if task-specific movement training improves performance-based function (composite score, movement, pain during movement) in an untrained task. Our secondary purpose was to test whether hip muscle strength improved following the movement training intervention.
Methods
This study was a secondary analysis of a prospective, non-randomised, within-group, double-baseline study. Twenty-three females with patellofemoral pain underwent task-specific movement training two times/week for 6 weeks. Outcomes were collected at three time points: enrolment (baseline), 6 weeks (preintervention) and 12 weeks (postintervention). A repeated measures analysis of variance tested whether the change during the intervention phase was greater than the change during the control phase. Y-balance composite score, hip and knee kinematics and pain during the Y-balance test were primary outcome measures; strength of the hip lateral rotator, abductor and extensor muscles was a secondary outcome measure.
Results
The change in composite score for the Y-balance test was not statistically significantly different between the intervention and control phases (p=0.16). The change during the intervention phase exceeded the change during the control phase for hip and knee kinematics and pain during the Y-balance test, with all variables improving (p<0.0001). The change during the intervention phase was greater than the control phase for hip muscle strength, with all variables improving (p<0.04).
Conclusion
Although the Y-balance test composite score did not improve, performance-based function during an untrained task, measured by movement and pain during the test, improved following task-specific movement training. Hip muscle strength improved, despite no focused muscle strengthening.
Level of evidence
Level II.
INTRODUCTION
Patellofemoral pain is a common, often chronic, musculoskeletal pain condition that may develop from a movement pattern termed dynamic knee valgus.1 Described as a medial ‘collapse’ of the lower extremity, dynamic knee valgus commonly occurs during functional, weight-bearing activities. Recommended management approaches for patellofemoral pain include exercise interventions to increase hip strength, which is thought to reduce dynamic knee valgus.2,3 A more direct approach, movement retraining, aims to change movement patterns through reprogramming motor patterns, and address dynamic knee valgus through repeated practice of optimal movement during weight-bearing.
Our recent feasibility study4 investigated a novel, task-specific movement training intervention focused on correcting pain-provoking movement patterns during daily activities. Based on work by Lang and Birkenmeier,5 Marich et al6 and Lanier et al,7 the intervention leveraged principles of motor learning including individualised, high-repetition challenging practice of daily tasks emphasising optimal limb alignment (eg, maintain a level pelvis, keep the knee over the second toe). An important component of the intervention was a home programme to incorporate appropriate limb alignment during all daily activities, which reinforced what was practised during intervention sessions.
While the primary study findings4 indicated the task-specific movement training intervention yielded improvements in average and maximum pain, patient-reported function and three-dimensional kinematics during a trained task (single-limb squat),4 the emphasis on applying new motor patterns across all daily activities, beyond the tasks performed during physical therapy, may encourage generalisability and transfer to untrained tasks. In addition, the progressive nature of the intervention may improve important physical outcome measures of performance-based function during the untrained task and hip muscle strength, typical targets for exercise-based interventions for patellofemoral pain.8–11
Clinically, lower extremity function is typically assessed with both self-report and performance-based measures.12 Performance-based measures provide objective measurement and tracking of functional performance beyond subjective patient-reported outcome measures. The Y-balance test is a frequently used, reliable,13 performance-based outcome measure that assesses dynamic balance during a single-limb squat. The task is goal oriented, in that the typical ‘score’ is a composite of the normalised distance reached by the non-weight-bearing limb in each of three directions, with farther distances (greater % leg length) indicating a better score. While the score itself may be informative,14,15 we assessed two additional components of performance on the Y-balance test that are highly relevant for people with movement-provoked pain problems such as patellofemoral pain: hip and knee movement and pain during the test.
Given the theoretical principles on which our task-specific movement training intervention is based, movement and pain during an untrained task such as the Y-balance test should improve following the intervention. Further, the progressive loading principles of the intervention may yield improvements in hip muscle strength. As hip muscle weakness is a common intervention target for patellofemoral pain, task-specific movement training may yield additional benefit (improved hip muscle strength) for individuals with patellofemoral pain.
This report is a secondary analysis of a prospective, non-randomised, within-group, double-baseline study that investigated the feasibility and preliminary efficacy of a novel, task-specific movement training intervention in women with patellofemoral pain. The primary purpose of this report was to test whether performance-based function (assessed comprehensively via composite score, movement and pain during the test) during an untrained task improved following a task-specific movement training intervention. Our secondary purpose was to test whether hip muscle strength improved following the intervention.
METHODS
Study design
A detailed description of the primary study design, methodology and intervention can be found in Salsich et al’s4 study. Twenty-five female participants (mean age±SD=22.2±3.8 years) were enrolled based on the following criteria: pain originating from the patellofemoral articulation, average daily pain rated at least 3/1016 and pain present during at least two of three provocation tests (resisted quadriceps contraction, single-limb squat, step down). Participants had to have observable dynamic knee valgus during a single-limb squat test, based on previously validated criteria.16,17 We excluded participants if they had a body mass index >30 kg/m2, a history of knee ligament, tendon or cartilage injury, patellar dislocation or instability, history of knee surgery, known pregnancy and any neurological involvement. Two participants were lost to follow-up between the baseline assessment and the 6-week assessment (preintervention). Twenty-three participants completed the intervention and were used for data analysis (table 1).
Table 1.
Participant Characteristics (Adapted from Salsich, et al.)4
| Participants Included in Analysis (n=23) Mean (SD) | Range (min-max) n=23 | |
|---|---|---|
| Age (years) | 21.8 (3.7) | 18–36 |
| BMI (kg/m2) | 22.2 (2.0) | 17.5–26.6 |
| Pain Duration (years) | 4.1 (3.4) | 0.5–10 |
| Pain Level: average past week (NPRS) | 3.7 (1.0) | 2–6 |
| Involved (tested) Side (n) | Left (11) Right (12) | |
| Bilateral Pain (n) | Bilateral (20) Unilateral (3) | |
| Frequency of Activities Limited by Pain † (n) | Running (18) Stairs (14) Squatting (12) Prolonged Sitting (9) | |
| Previous Physical Therapy Treatment for Patellofemoral Pain (n) | 10 |
n= number of participants; SD = Standard Deviation; NPRS = numeric pain rating scale (0 = no pain, 10 = worst imaginable pain)
Habitual Physical Activity (Range for each index: 1–5, where 1=inactive and 5=highly active)
Most frequently reported activities limited by pain, as noted on the Patient-specific Functional Scale
Participants were assessed at baseline, 6 weeks (preintervention), 12 weeks (postintervention) and 16 weeks. See Salsich et al’s4 study for a description of the measures assessed at each time point. For the purposes of this secondary analysis, we analysed performance-based function using the Y-balance test (composite score, two-dimensional (2D) hip and knee joint movement, pain), and hip strength data at baseline, 6 weeks and 12 weeks.
Intervention
A licensed physical therapist with specialist certification in orthopaedics and 24 years of experience administered the task-specific movement training intervention for 45 min two times/week for 6 weeks. This intervention, engrained in principles of motor learning, focused on optimal limb alignment with supervised practice of functional daily tasks. All participants were trained in single-limb squat, double-limb squat, sit to stand/stand to sit and stair ascent/descent. As participants progressed through the intervention, they were given two to three more tasks specific to their sport, work or leisure (eg, running and cutting). Participants were instructed in the following concepts of optimal movement: maintain a level pelvis (no contralateral hip drop), level trunk (no side bending) and keep their knee over their second toe (no valgus).4 External cueing from the physical therapist was removed early in the intervention to allow the patient to develop intrinsic feedback, a well-studied key component to facilitate motor learning.18 Throughout the session, participants performed tasks with challenging, high-repetition practice to encourage motor learning. Tasks were progressed based on the ability to maintain optimal limb alignment without increasing pain. Example progressions include increasing the squat depth, adding weight to the sit to/from stand and changing the stability of the supporting surface. (See Salsich et al’s4 study for a detailed description of the intervention.) Participants were instructed in their home exercise programme to practise three tasks for five repetitions per day for conceptual reinforcement, and to move optimally in all daily activities.
Data collection
2D movement analysis was to assess hip and knee joint movement during the Y-balance (posteromedial direction) (figure 1). 2D measurements are clinically available and can detect changes in movement before and after intervention.19,20 When performing the Y-balance test, the physical therapist instructed participants to push the box as far as possible using any strategy, contingent on maintaining balance. The Y-balance task was done without shoes. Reach distances during the Y-balance task were measured from three trials on the involved limb and averaged for a composite score in all three directions (ie, anterior, posterolateral, posteromedial). Values were expressed as a percentage of the individual’s leg length. Pain during the Y-balance test was assessed using a visual analogue scale, a 100 mm line with 0 indicating no pain, and 100 indicating worst imaginable pain. Participants were asked to rate their pain during the Y-balance test after they completed the test in all directions by placing a hash mark on the line. Visual analogue scores were calculated using the distance in millimetres from the ‘0’ point to where the participant’s mark crossed the line.
Figure 1.
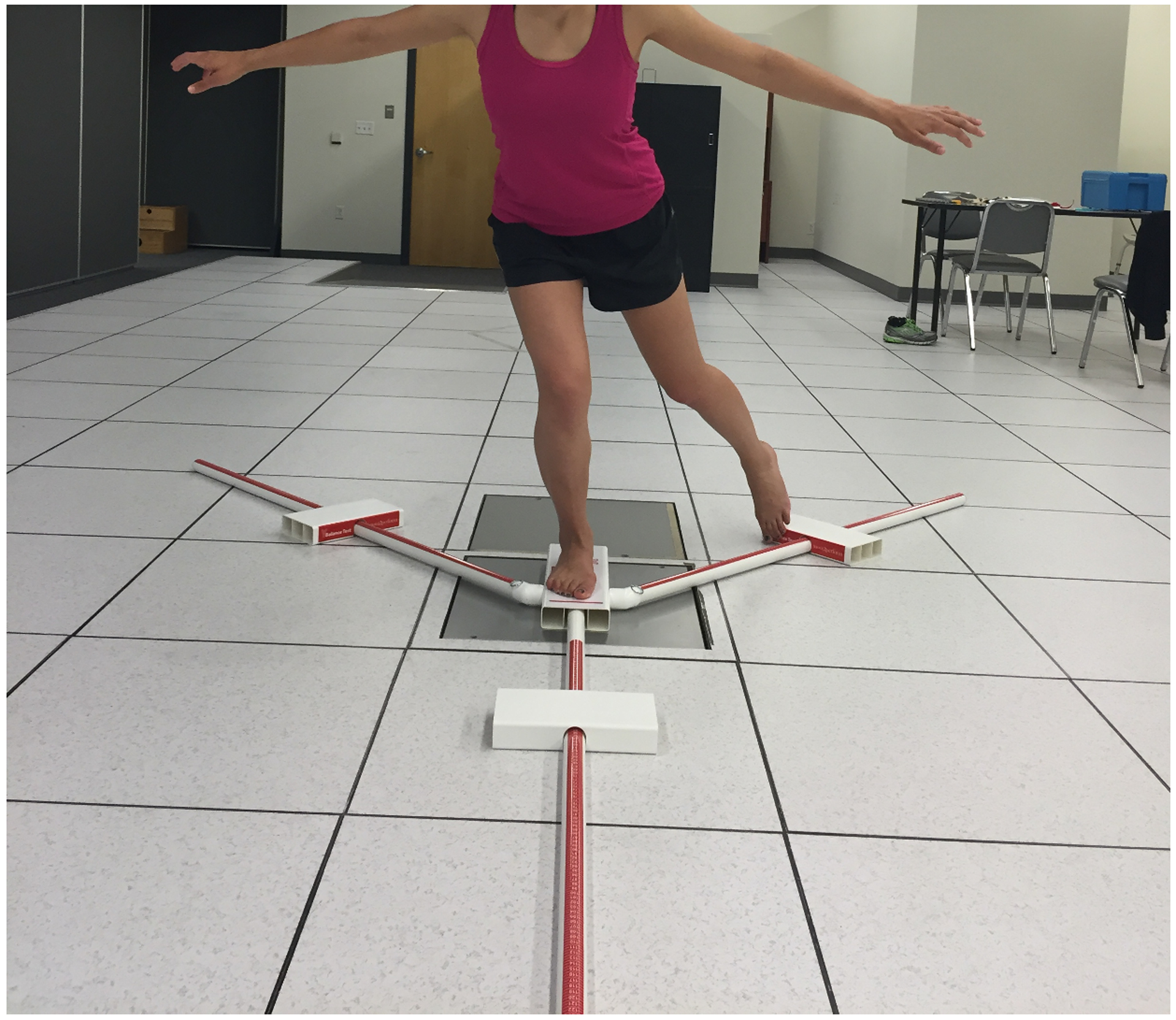
Y-balance test (posteromedial direction).
2D data were captured during the Y-balance task (posteromedial direction) using a Canon VIXIA HF M50 video camera (Cannon USA, Huntington, New York) or a Bonita 720c digital camera (Vicon Motion Systems, Oxford, England). The cameras were positioned at a height of 45 cm, 3 m anterior to the participant. The posteromedial direction was chosen because it allowed full visualisation of the pelvis, thigh and leg. Hip and knee frontal plane projection angles (FPPA) were measured with Dartfish ProSuite 7 (Dartfish, Fribourg, Switzerland) at the peak knee flexion (PKF) angle and averaged across three trials on the involved limb. Hip and knee FPPAs were measured by blinded investigators according to previously published criteria.20 The hip angle is made up of a line drawn between the anterior superior iliac spines and a line drawn from the midpoint of the patella, bisecting the thigh (figure 2). The knee angle was defined using a line drawn from the midpoint of the knee to the midpoint of the ankle (figure 2). The kinematic calculations used to quantify FPPA for the hip and knee were 90-α and 180-β, respectively (figure 2) where increasing numbers represented an increase in dynamic knee valgus.
Figure 2.
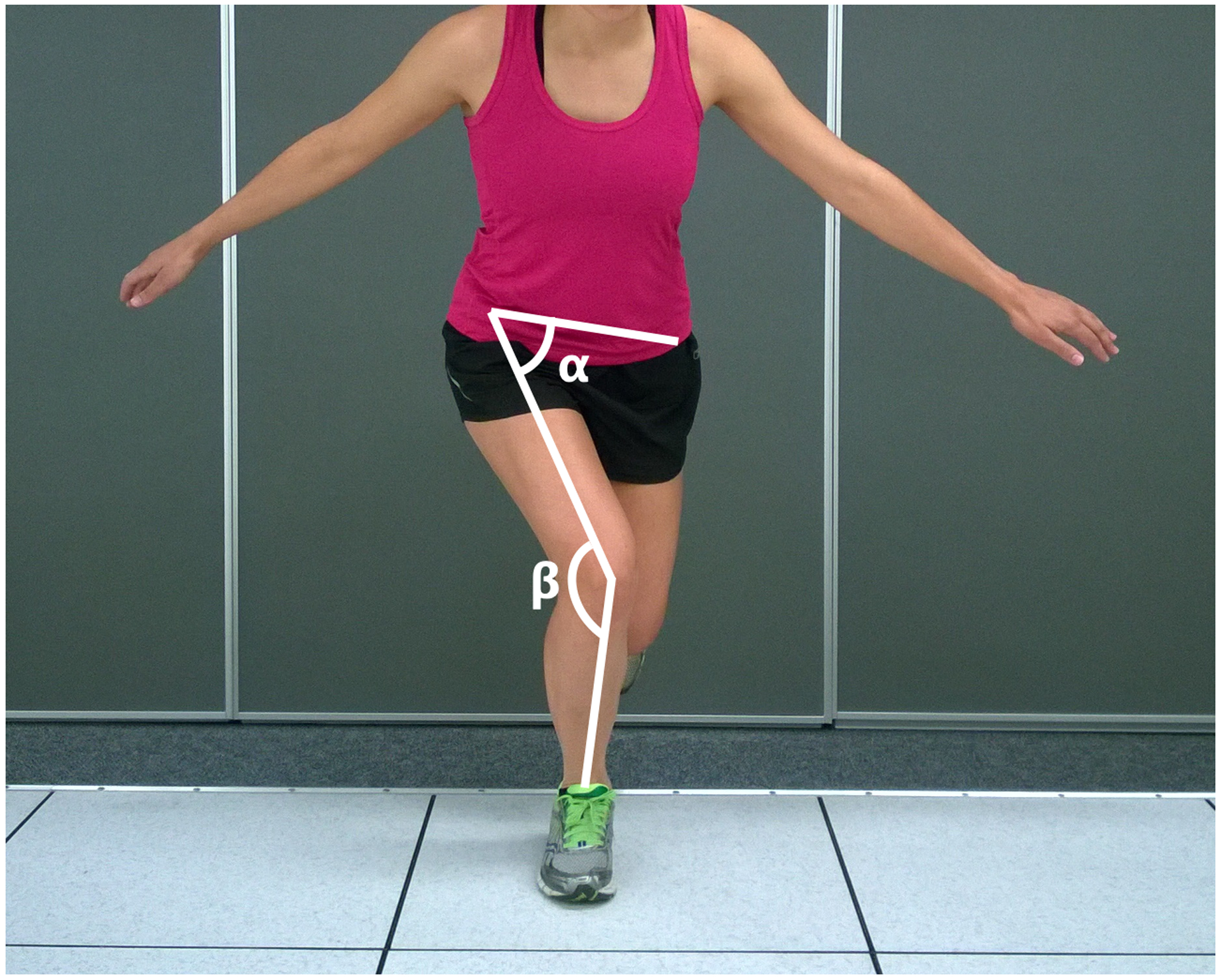
Calculation of hip (α) and knee (β) frontal plane projection angles (FPPAs). Kinematic calculations include 90-α for the hip and 180-β for the knee, with increasing numbers representing increased dynamic knee valgus.
Reliability of the hip and knee FPPA was determined by having two investigators measure on two occasions a set of 10 videos randomly selected from all time points. The inter-rater intraclass correlation coefficient (ICC) was: ICC(3,1): hip=0.98, knee=0.99. The intrarater ICC(2,1) for the lead author was: hip=0.99, knee=0.95.
Isometric strength of the hip lateral rotators, abductors and extensors was quantified with a handheld dynamometer using the manual muscle testing procedures described by Kendall et al.21 The examiner applied a perpendicular force to the limb segment which increased until the subject’s resistance ‘broke’, signified by limb movement out of test position. Breaking force was documented, and the test was repeated three times. The average force value was computed and expressed in newtons.22 Gluteus medius strength was tested with participants in side lying on their uninvolved limb, with the uninvolved hip and knee flexed. The involved limb was placed in hip abduction, extension and lateral rotation with the trunk and pelvis in neutral. The handheld dynamometer was positioned 2 cm proximal to the lateral malleolus and force was applied perpendicular to the limb towards hip adduction and flexion. Gluteus maximus strength was tested with the participant in prone and the involved knee flexed to 90°. The involved hip was extended as far as possible with the pelvis maintained in neutral. The force was applied perpendicular to the limb into hip flexion. Finally, the strength of the hip lateral rotators was tested with participants in a seated position with hips and knees flexed to 90°. The knee joint centre was aligned with the hip joint centre using a small towel under the distal thigh. The participant’s involved limb was positioned into lateral rotation, with the femur stabilised by the examiner. The force was applied perpendicular to the limb into medial rotation, with the dynamometer placed 2 cm proximal to the medial malleolus.
Analysis
This study investigated the following primary variables of interest: Y-balance composite score, hip and knee FPPA at PKF and pain during the Y-balance test. Strength of the hip lateral rotator, abductor and extensor muscles was a secondary variable of interest. Analysis for all variables was a mixed model repeated measures analysis of variance (RM-ANOVA) that included data from all study visits. The reported p value is from a statistical contrast within the RM-ANOVA that tested the a priori null hypothesis that the change during the intervention phase (6–12 weeks) was equal to the change during the control phase (baseline to 6 weeks). The appropriateness of the covariance structure was confirmed with correlations and the Schwarz Bayesian information criteria. If the outcome did not follow the multivariate normal distribution, data were transformed to satisfy normality. Reported values are means±SD unless otherwise specified.
RESULTS
The change in composite score for the Y-balance test (values expressed as % leg length) did not improve following the intervention (p=0.16) (table 2). For the hip and knee FPPAs, the change during the intervention phase was greater than the change during the control phase, with both variables decreasing (improving) after intervention (p<0.0001) (figure 3, table 2). Pain during the Y-balance task improved more in the intervention phase compared with the control phase (p<0.0001) (table 2). Finally, for hip muscle strength, improvements during the intervention phase were greater than during the control phase for hip lateral rotator (p=0.003), abductor (p=0.005) and extensor (p=0.04) muscle strength measures (figure 4, table 2).
Table 2.
Values of primary and secondary outcome measures and change scores at each time point (Change calculations: Pre-intervention-Baseline, Post-intervention-Pre-intervention; values are mean ± SD).
| Baseline | 6 Weeks (Pre-intervention) | 12 Weeks (Post-intervention) | Change: Baseline to 6 Weeks (control phase) | Change: 6 to 12 weeks (intervention phase) | P-value* | |
|---|---|---|---|---|---|---|
| Composite Y-balance score † | 88.30 ± 6.89 | 89.98 ± 6.18 | 91.27 ± 5.79 | 1.67 ± 5.34 | 1.29 ± 4.36 | 0.16 |
| Hip FPPA (°) | 24.25 ± 4.56 | 22.87 ± 6.01 | 18.75 ± 6.15 | −0.9 ± 4.3 | −4.1 ± 7.2 | 0.0006* |
| Knee FPPA (°) | 22.22 ± 8.65 | 18.93 ± 10.78 | 8.54 ± 9.96 | −2.3 ± 5.4 | −10.4 ± 12.9 | <0.0001* |
| Pain during Y-balance (VAS) | 24.39 ± 17.33 | 28.70 ± 21.16 | 6.09 ± 10.08 | 4.30 ± 9.68 | −22.6 ± 20.45 | <0.0001*# |
| Lateral Rotator Strength (N) | 106.6 ± 21.43 | 104.6 ± 18.76 | 111.0 ± 16.40 | −1.9 ± 9.9 | 6.4 ± 10.3 | 0.003* |
| Hip Abductor Strength (N) | 86.90 ± 26.96 | 87.03 ± 22.32 | 96.63 ± 21.67 | 0.1 ± 18.6 | 9.6 ± 16.9 | 0.005* |
| Hip Extensor Strength (N) | 158.7 ± 40.60 | 160.1 ± 39.29 | 173.8 ± 38.53 | 1.4 ± 31.8 | 13.7 ± 30.2 | 0.04* |
SD = Standard Deviation; FPPA=frontal plane projection angle; N=newtons; VAS= visual analog scale
P-value: change during intervention phase compared to change during control phase (statistically significant at 0.05 alpha level)
values reported as % of leg length
Prior to analysis, data were log transformed to follow the multivariate normal distribution.
Figure 3.
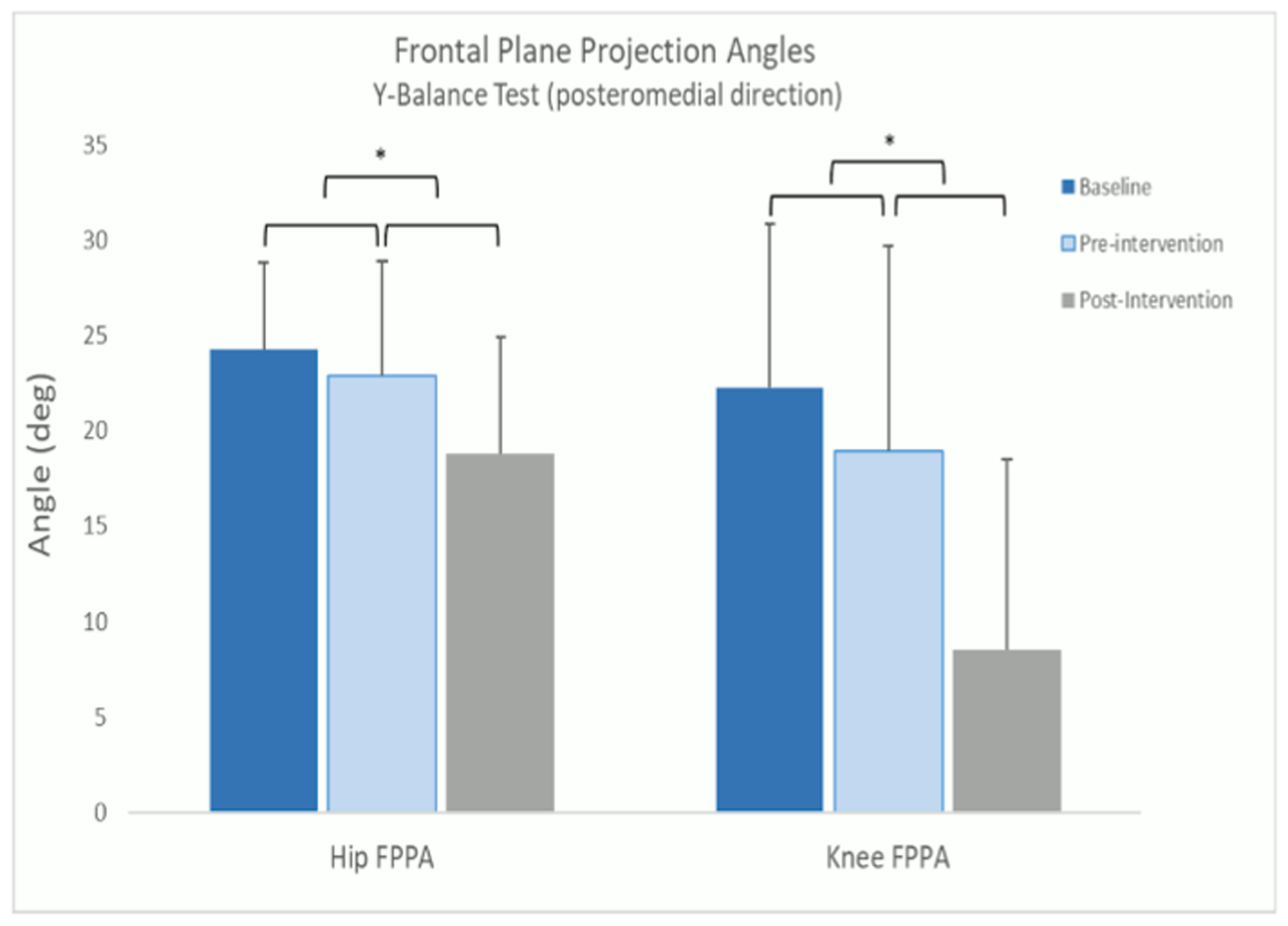
Hip and knee frontal plane projection angles (FPPA) at peak knee flexion during the Y-balance test (posteromedial direction). Error bars represent 1 SD. *Indicates differences in changes during the intervention phase compared with the control phase, p<0.05.
Figure 4.
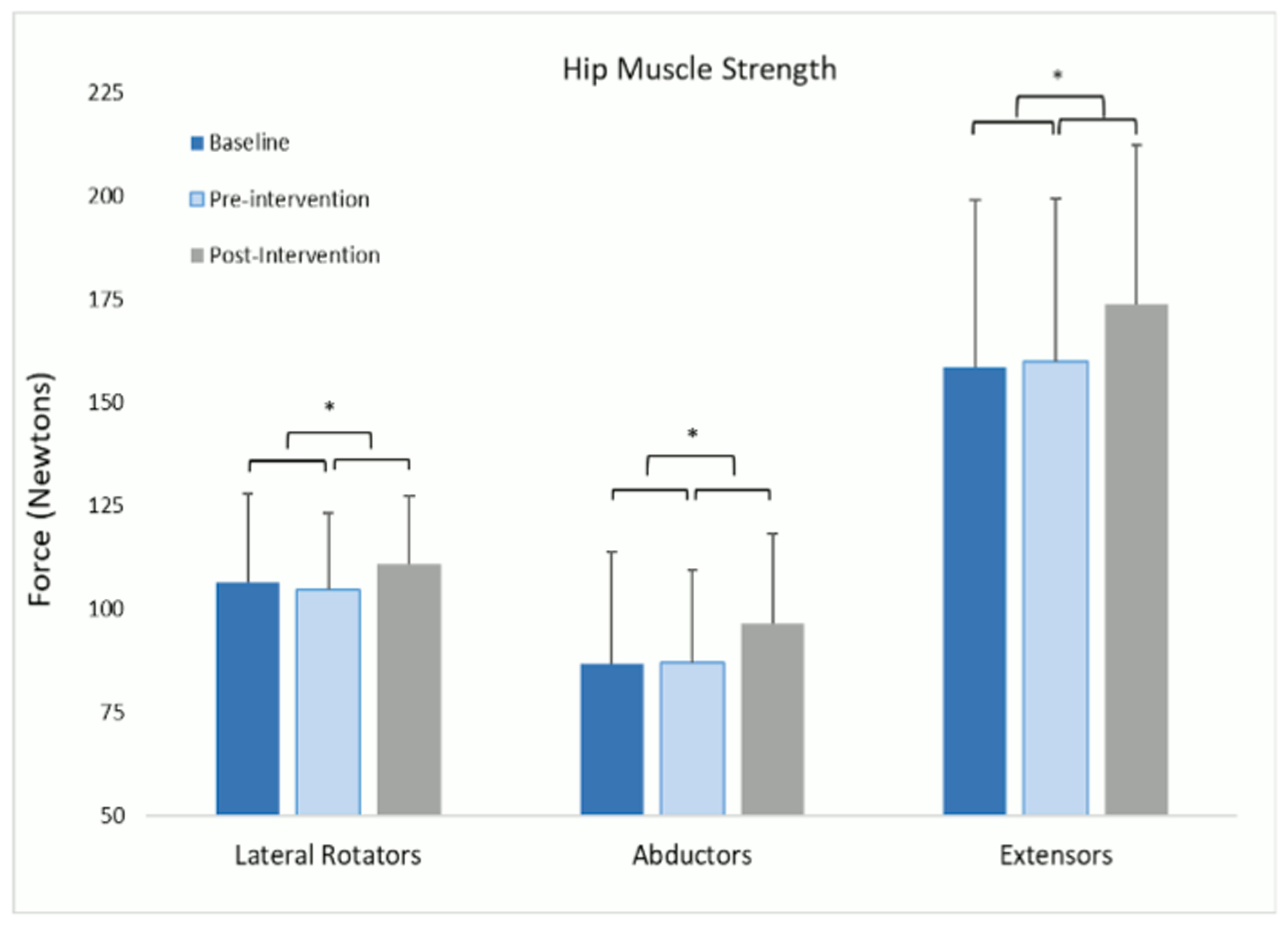
Isometric hip strength of hip lateral rotators, abductors and extensors, expressed in newtons. Error bars represent 1 SD. *Indicates differences in changes during the intervention phase compared with the control phase, p<0.05.
DISCUSSION
The primary purpose of this report was to determine if the task-specific movement training intervention resulted in improved performance-based function on an untrained task assessed via composite score, movement quality and pain during the test. The secondary purpose was to determine if hip muscle strength improved following the intervention. Our data indicate that 2D hip and knee kinematics improved and pain was reduced during the Y-balance test, hip muscle strength improved following the task-specific movement training intervention, but the composite score on the Y-balance test did not.
Scores on the Y-balance did not improve from preintervention to postintervention. This finding could be due to a variety of reasons, for example, a ceiling effect or insufficient sensitivity of the measure, insufficient variability in performance in this population or the effect was not large enough to reach statistical significance. At baseline, our participants functioned similarly to reference values in young, healthy females (20.61±1.1 years old; 93.3±7.3; mean±SD).23 These data suggest that although participants functioned similarly to a reference group of young, healthy females based on composite score, they were able to improve their quality of movement and reduce their pain during the Y-test over the period of the intervention. Our results reflect recent evidence seen in outcomes after anterior cruciate ligament reconstruction. When considering return to sport after anterior cruciate ligament reconstruction, evidence suggests quantifying commonly used limb symmetry indexes may not be sensitive enough to determine outcomes related to quality of movement.24 Our findings suggest primarily assessing the composite scores of the Y-balance test, on its own, may lead to misinterpretation of performance-based function when other clinical deficits may be present.
The improvement (ie, lower FPPA) in hip and knee FPPA during the Y-balance test after intervention suggests our intervention was successful in improving movement patterns. Importantly, we did not use the Y-balance task in the intervention when training participants. Participants were not given instructions on movement during the Y-balance assessment, they were told to achieve the greatest distance they could. Thus, the improvements seen in this task demonstrate a carry-over effect, that is, a transfer of a newly learnt skill to an untrained movement task. Previous literature has shown that training movement changes neural networks related to the development of a new motor pattern.25 The intention of task-specific movement training is the practice of a skill to acquire the motor pattern for successful movement in a new motor skill, shown via skill transfer.25–27 Motor learning requires repetition and task specificity, and sufficient challenge to the system and a transition to use of intrinsic feedback to be successful.5
The ability to transfer a motor skill or control strategy to an unlearnt task has high clinical relevance. Skill transfer to an environment salient to the patient is an important goal of physical therapy. The transfer effect seen in our study is consistent with reported transfer effects from running to single-leg squats28 and stair descent,29 and indicates that participants understand how to maintain optimal alignment during trained tasks and daily activities (our home exercise programme), and were able to do so with accuracy and consolidated the motor skill.
Pain during the Y-balance task decreased from preintervention to postintervention. Primary outcomes from our study4 showed reductions in daily and weekly pain ratings, but did not report changes in pain during movement. Improvements in patient-reported pain during movement are an important clinical outcome, as many individuals who have chronic patellofemoral pain report pain during activities of daily living.2 Because patellofemoral pain may be induced by repeated abnormal loading using altered hip and knee kinematics,30,31 being able to generalise improved movement patterns4 to untrained tasks is important to improve performance-based function and reduce pain in daily life.
Hip muscle strength improved following the intervention despite the lack of a focused strengthening component to the intervention. The strength improvements may indicate that a challenging and progressive task-specific movement training programme may provide enough stimulus to elucidate a strengthening effect of the involved musculature. It is possible that to complete the more difficult activities, a higher demand was placed on the hip muscles resulting in a strengthening effect over the course of the intervention phase. Our data showed muscle strength increases in all muscle groups (ie, lateral rotators, hip abductors, hip extensors) from preintervention to postintervention. While it is not known if these increases are clinically meaningful, they are similar to those reported by Stearns and Powers32 in healthy women following a ‘hip-focused’ training programme. Our study shows that targeting motor control via neuromuscular re-education and progressing the rehabilitation programme may be enough to provide a strengthening stimulus in this patient population.
Hip muscle strengthening alone may not be sufficient at improving movement concurrently. In a recent review of methodology of clinical interventions for patellofemoral pain, Davis et al33 showed strengthening alone does not alter faulty movement patterns, but rather addressing the motor programme itself is needed to make notable improvements in pain. Specifically, Willy and Davis34 reported that healthy females with excessive hip adduction did not change their running mechanics in response to a 6-week strengthening programme. Similarly, Earl and Hoch35 reported no changes in either hip or knee kinematics in women with patellofemoral pain after a strengthening programme. While there is evidence of improved lower extremity kinematics following ‘hip-focused’ interventions,32 if participants were given instructions to maintain a specific joint alignment during the strengthening activities, it is possible the positive effects on kinematics were due to repeated ‘optimal’ movement (ie, movement retraining) versus strengthening. While strengthening interventions alone have not improved movement patterns, our results suggest movement retraining interventions may improve both movement and strength and in turn improve clinically relevant measures of performance-based function.
This study has several limitations to consider when interpreting the results of this secondary analysis. The Y-balance test is similar to a single-limb squat, which was trained during our intervention; however, the test is performed within a different context and with an external goal (distance based rather than movement based). We used 2D measures with FPPAs to assess movement, so we were unable to identify individual joint contributions to changes in kinematics. Pain during movement was measured at the end of the composite Y-balance test and not during each individual direction; however, patients were reminded to consider pain levels during the task.
CONCLUSION
The composite Y-balance scores did not improve following task-specific movement training; however, improvements were noted in other aspects of performance-based function, specifically in 2D hip and knee kinematics and reduced pain during movement. Improvements in kinematics during the Y-balance demonstrated skill transfer to an untrained task. Hip muscle strength improved without a focused strengthening component to the intervention.
What are the new findings.
This study uses clinically available methods to quantify changes in movement and movement-induced pain in response to task-specific movement training.
The composite score of the Y-balance test, a commonly used measure of lower extremity performance-based function, did not improve; however, pain and movement during the Y-balance test and hip muscle strength improved following the intervention.
Task-specific movement training may offer an adequate stimulus for improvements in kinematics, pain during movement and hip muscle strength.
Acknowledgements
The authors would like to acknowledge Angela Reitenbach and Anna DiStaulo for their help with data collection and processing.
Funding
Funding for this project was provided by the NIH/National Center for Advancing Translational Sciences (NCATS) grant UL1 TR000448, NIH/National Center for Medical Rehabilitation Research grant R01 HD047709, Washington University Institute of Clinical and Translational Sciences CTSA 705, the Orthopaedic Section of the American Physical Therapy Association (APTA) and the Saint Louis University Program in Physical Therapy, Doisy College of Health Sciences.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval Informed consent was obtained from all participants and the study was approved by the Saint Louis University Institutional Review Board.
Twitter Elanna K Arhos @elanna_arhos
Data availability statement
Data are available upon reasonable request.
REFERENCES
- 1.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther 2003;33:639–46. [DOI] [PubMed] [Google Scholar]
- 2.Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral pain research retreat, Manchester. Part 1: terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med 2016;50:839–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral pain research retreat, gold Coast, Australia, 2017. Br J Sports Med 2018;52:1170–8. [DOI] [PubMed] [Google Scholar]
- 4.Salsich GB, Yemm B, Steger-May K, et al. A feasibility study of a novel, task-specific movement training intervention for women with patellofemoral pain. Clin Rehabil 2018;32:179–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lang CE, Birkenmeier RL. Upper-extremity task-specific training after stroke or disability: a manual for occupational therapy and physical therapy. 158. Bethesda, MD: AOTA Press, 2013. [Google Scholar]
- 6.Marich AV, Lanier VM, Salsich GB, et al. Immediate effects of a single session of motor skill training on the lumbar movement pattern during a functional activity in people with low back pain: a Repeated-Measures study. Phys Ther 2018;98:605–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanier VM, Lang CE, Van Dillen LR. Motor skill training in musculoskeletal pain: a case report in chronic low back pain. Disabil Rehabil 2019;41:2071–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Şahin M, Ayhan FF, Borman P, et al. The effect of hip and knee exercises on pain, function, and strength in patientswith patellofemoral pain syndrome: a randomized controlled trial. Turk J Med Sci 2016;46:265–77. [DOI] [PubMed] [Google Scholar]
- 9.Rogan S, Haehni M, Luijckx E, et al. Effects of hip abductor muscles exercises on pain and function in patients with Patellofemoral pain: a systematic review and meta-analysis. J Strength Cond Res 2019;33:3174–87. [DOI] [PubMed] [Google Scholar]
- 10.van Linschoten R, van Middelkoop M, Berger MY, et al. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ 2009;339:b4074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crossley K, Bennell K, Green S, et al. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med 2002;30:857–65. [DOI] [PubMed] [Google Scholar]
- 12.Reuben DB, Seeman TE, Keeler E, et al. Refining the categorization of physical functional status: the added value of combining self-reported and performance-based measures. J Gerontol A Biol Sci Med Sci 2004;59:M1056–61. [DOI] [PubMed] [Google Scholar]
- 13.Plisky PJ, Gorman PP, Butler RJ, et al. The reliability of an instrumented device for measuring components of the StAR excursion balance test. N Am J Sports Phys Ther 2009;4:92–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Roe C, Jacobs C, Kline P, et al. Correlations of single-leg performance tests to patient-reported outcomes after primary anterior cruciate ligament reconstruction. Clin J Sport Med 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith CA, Chimera NJ, Warren M. Association of Y balance test reach asymmetry and injury in division I athletes. Med Sci Sports Exerc 2015;47:136–41. [DOI] [PubMed] [Google Scholar]
- 16.Salsich GB, Graci V, Maxam DE. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther 2012;42:1017–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris-Hayes M, Steger-May K, Koh C, et al. Classification of lower extremity movement patterns based on visual assessment: reliability and correlation with 2-dimensional video analysis. J Athl Train 2014;49:304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adkins DL, Boychuk J, Remple MS, et al. Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J Appl Physiol 2006;101:1776–82. [DOI] [PubMed] [Google Scholar]
- 19.Di Staulo AM, Scholtes SA, Salsich GB. A descriptive report of the variability in 3D hip and knee kinematics during a single limb squat in women who have patellofemoral pain and visually classified dynamic knee valgus. Physiother Theory Pract 2019;36:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scholtes SA, Salsich GB. A dynamic valgus index that combines hip and knee angles: assessment of utility in females with Patellofemoral pain. Int J Sports Phys Ther 2017;12:331–40. [PMC free article] [PubMed] [Google Scholar]
- 21.Kendall FP, McCreary EK, Provance PG, et al. Muscles testing and function with posture and pain. Balitmore, MD: Lippincott Williams & Wilkins, 2005. [Google Scholar]
- 22.Long-Rossi F, Salsich GB. Pain and hip lateral rotator muscle strength contribute to functional status in females with patellofemoral pain. Physiother Res Int 2010;15:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alnahdi AH, Alderaa AA, Aldali AZ, et al. Reference values for the Y balance test and the lower extremity functional scale in young healthy adults. J Phys Ther Sci 2015;27:3917–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welling W, Benjaminse A, Seil R, et al. Altered movement during single leg hop test after ACL reconstruction: implications to incorporate 2-D video movement analysis for hop tests. Knee Surg Sports Traumatol Arthrosc 2018;26:3012–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Draganski B, May A. Training-induced structural changes in the adult human brain. Behav Brain Res 2008;192:137–42. [DOI] [PubMed] [Google Scholar]
- 26.Scholz J, Klein MC, Behrens TEJ, et al. Training induces changes in white-matter architecture. Nat Neurosci 2009;12:1370–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karni A, Meyer G, Jezzard P, et al. Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature 1995;377:155–8. [DOI] [PubMed] [Google Scholar]
- 28.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med 2011;45:691–6. [DOI] [PubMed] [Google Scholar]
- 29.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech 2012;27:1045–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Powers CM, Witvrouw E, Davis IS, et al. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral pain research retreat, Manchester, UK: Part 3. Br J Sports Med 2017;51:1713–23. [DOI] [PubMed] [Google Scholar]
- 31.Lankhorst NE, Bierma-Zeinstra SMA, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther 2012;42:81–A12. [DOI] [PubMed] [Google Scholar]
- 32.Stearns KM, Powers CM. Improvements in hip muscle performance result in increased use of the hip extensors and abductors during a landing task. Am J Sports Med 2014;42:602–9. [DOI] [PubMed] [Google Scholar]
- 33.Davis IS, Tenforde AS, Neal BS, et al. Gait retraining as an intervention for Patellofemoral pain. Curr Rev Musculoskelet Med 2020;13:103–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther 2011;41:625–32. [DOI] [PubMed] [Google Scholar]
- 35.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med 2011;39:154–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.


