Abstract
COVID-19 has resulted in a mental health crisis across the globe. Understanding factors that may have increased individuals' risk of poor mental health outcomes is imperative. Individual differences in attachment styles have been shown to predict poorer mental health outcomes and insecure individuals struggle to cope with stressful situations. Therefore, we extended past research by examining whether higher attachment insecurity (anxiety and avoidance) predicted worse mental health over time during the COVID-19 pandemic. Study 1 examined mood and mood fluctuations daily over a week in the beginning of lockdown and depression and anxiety weekly over a five-week period (n = 200). Study 2 examined depression and anxiety before and during the pandemic (n = 100 couples). As predicted, individuals higher (vs. lower) in attachment anxiety, but not avoidance, reported greater depression and anxiety during the pandemic in both studies. Individuals lower in attachment anxiety experienced an improvement in mental health over time in Study 1 suggesting that more secure individuals may recover more quickly from the initial change in circumstances. Attachment styles did not significantly predict mood or mood fluctuations. Attachment anxiety is likely to be a risk factor for poor mental health outcomes during COVID-19.
Keywords: Mental health outcomes, Depression, Anxiety, Attachment, COVID-19
The world has currently faced one of the worst public health crises in history. The COVID-19 pandemic has caused a wide range of social and economic disruptions across the world. Early in the pandemic, most governments imposed strict social distancing measures including stay-at-home orders, travel bans, cancellation of most public events, and closure of schools and most non-essential workplaces. The pandemic has led to a serious mental health crisis in the worst hit countries (Fiorillo & Gorwood, 2020; Moccia et al., 2020; Vindegaard & Benros, 2020). For example, the number of people suffering with mental distress has increased from 19% to 27% in the UK (Pierce et al., 2020). Containment measures including social distancing and self-isolation have a strong impact on psychological well-being (Brooks et al., 2020). However, not everyone is impacted by the pandemic equally and some individuals may require more support than others (Moccia et al., 2020). Understanding predictors of poor mental health and distress is urgently needed in order to develop intervention strategies (Sani et al., 2020). Across two longitudinal studies, we importantly add to this growing literature by examining whether attachment insecurity predicts poorer mental health outcomes arising from the pandemic over time.
1.1. Mental health outcomes during COVID-19
A number of studies to date have examined the impact of COVID-19 on various mental health outcomes (e.g., depression, anxiety, stress). A recent systematic review of 43 studies found that across different samples comprising of general public, healthcare professionals, and those infected by COVID-19, the rates of post-traumatic stress-disorder, depression, and anxiety had all increased (Vindegaard & Benros, 2020). However, all but one of the studies (Wang et al., 2020) included in the review were cross-sectional and did not address changes in mental health outcomes over time. A small number of studies examining mental health outcomes over time during the pandemic have been conducted. One study found that depression and anxiety had increased nearly 10% in the UK from pre-pandemic levels after a month of lockdown (Pierce et al., 2020). Another study conducted compared the difference in mental health outcomes in China between the period in which many new cases were being reported and the period in which many were recovering (Wang et al., 2020). A minority of the sample participated in both waves. The study found no significant difference in mental health outcomes between these periods. While these studies provide important insights into how people's mental health has been affected by the pandemic, they only collected data over two time-points. Therefore, it is difficult to make inferences about the trajectory of mental health outcomes over time.
One study has addressed this limitation by examining students' mental health outcomes over the Winter 2020 academic term (from January 6, 2020 for 12 weeks; Huckins et al., 2020). The results showed an increase in depression and anxiety following the pandemic. However, the sample was restricted to students from one college, which may not generalize into other populations. College students are likely to experience very different stressors due to the pandemic compared to non-students who are working or have families. Therefore, further research is needed to investigate whether these findings hold in other samples. In the present study, we use data from two different samples: Study 1 included longitudinal data primarily from non-student individuals who were living with their romantic partner (half of them had children) and Study 2 included pre- and in-pandemic data from both members of the couple. Furthermore, while most of the aforementioned studies have found an increase in mental health problems during the pandemic, little is yet known about who may be more vulnerable to mental health problems during this time. Herein we addressed this issue by examining adult attachment insecurity as a possible vulnerability factor.
1.2. Attachment insecurity and mental health outcomes
Attachment theory (Bowlby, 1969) suggests that individuals form interpersonal bonds with primary caregivers early in their lives. The quality of these early attachment bonds become internalized over time and form relatively stable internal working models, or mental representations, of self and others that guide individuals' behavior in relationships. Based on the internal working models, individuals are generally thought of as either being securely or insecurely attached. Individuals who had caregivers who were available and responsive to their needs develop better emotion regulation strategies in adulthood and become securely attached (for a review, see Mikulincer & Shaver, 2016).
In contrast, individuals who did not experience their caregivers as available and responsive develop secondary attachment strategies to either fight or flee (Mikulincer et al., 2003). Individuals higher in attachment anxiety engage their fight response by hyperactivating their attachment system and continuously seeking support and reassurance in relationships (Brennan & Carnelley, 1999; Cassidy, 1994; Shaver et al., 2005). On the other hand, individuals higher in attachment avoidance flee by deactivating their attachment system and attempting to deal with distress and threat alone, thus becoming compulsively self-reliant (Bartholomew & Horowitz, 1991; Cassidy, 1994; Mikulincer et al., 2009). Maintaining the secondary attachment strategies require resources that make more insecure individuals less adept at dealing with stressful situations and more vulnerable to mental health problems such as anxiety and depression. Insecure individuals may also be less able to seek support from their partner (B. C. Feeney & Collins, 2015). This may put them at a risk particularly during the pandemic given their partner may be the only person available to provide support for mental health difficulties.
A wealth of research has examined the effect of attachment insecurity on coping in stressful situations and mental health outcomes. Individuals higher in attachment anxiety have been shown to engage in emotion-focused coping, such as rumination and self-blame, and tend to focus their attention on their own distress rather than focusing on solutions to current problems (Chung, 2014; Garrison et al., 2014; Trillingsgaard et al., 2011). Anxious attachment is also associated with worrying about the causes and consequences of threatening events (Trillingsgaard et al., 2011). There have been hundreds of studies examining the role of attachment anxiety in predicting mental health problems (Dagan et al., 2018; Mikulincer & Shaver, 2016; Stanton & Campbell, 2014). Attachment anxiety has been associated with poorer mental health outcomes compared to secure individuals in nearly all these studies. Therefore, combined with anxious individuals' tendency to focus on their distress, inability to cope with threatening situations, and higher incidence of mental health problems, we would expect that anxious individuals are particularly vulnerable to poor mental health outcomes during the pandemic.
In contrast, individuals higher in attachment avoidance cope with stressful situations by using distancing strategies such as disengagement, stress denial, and diversion of attention (Holmberg et al., 2011). They are likely to use distractions to cope with stressful situations (J. A. Feeney, 1995) and to repress negative emotions (Mikulincer & Orbach, 1995). Interestingly, attachment avoidance has also been associated with emotion-focused coping in some studies in which the stressors have been more severe suggesting that avoidant individuals may only be able to use distancing strategies with smaller stressors but these strategies may fail when faced with severe and enduring stressors (Birnbaum et al., 1997; Shapiro & Levendosky, 1999). In many studies, attachment avoidance has been associated with poorer mental health outcomes (Liu et al., 2009; Marganska et al., 2013). However, this finding is less robust compared to attachment anxiety with some studies finding no significant association between attachment avoidance and poor mental health (Eberhart & Hammen, 2009; Stanton & Campbell, 2014; Surcinelli et al., 2010). Therefore, it is less clear how individuals higher in attachment avoidance would manage during the pandemic. Because the pandemic is an enduring and a potentially severe stressor, it may be that avoidant individuals' distancing strategies will not be sufficient to buffer against potential effects of the pandemic on mental health outcomes.
1.3. Aims
Only one study to date has examined whether individual differences in attachment styles are associated with mental health outcomes during the early outbreak of COVID-19 in Italy (Moccia et al., 2020). The study found that individuals higher (vs. lower) in anxious attachment were at a significantly higher risk of moderate-to-severe psychological distress, whereas individuals higher (vs. lower) in attachment avoidance or security were at a decreased risk of moderate-to-severe psychological distress. While the study provides first evidence of how attachment styles may be associated with mental health outcomes during the pandemic, it was cross-sectional and therefore cannot speak to how different attachment styles may be associated with mental health outcomes over time. Understanding potential change across time is important to understand whether the pandemic may lead to long-term mental health problems.
Therefore, to extend this literature, our novel aim was to examine whether individual differences in attachment styles can explain why some individuals are coping better during the pandemic than others over time. In Study 1, we examined mood and mental health outcomes over a period of 5 weeks in the beginning of lockdown measures including a daily diary for a period of a week. This study adds to the literature by examining whether attachment styles predict changes in mental health outcomes over time and it is also the first daily diary study examining whether mood fluctuated daily during the pandemic. In Study 2 we examined change in mental health outcomes from before the pandemic to the first wave of the pandemic. It is among the first studies examining mental health outcomes in dyads during the pandemic enabling us to assess whether a partner's attachment style predicts change in actor's mental health outcomes in addition to the actor's own attachment style. It is among the first studies to examine whether attachment is associated with a change in mental health outcomes from pre-pandemic levels to during pandemic and which includes pre-pandemic data. Overall, we expected that attachment insecurity, especially attachment anxiety, would predict poorer mental health outcomes during the pandemic.
1.4. Study 1
In Study 1, we followed 200 participants who were currently living with their romantic partner in a country in which social distancing measures had been put in place weekly over 5 weeks measuring their level of anxiety and depression. Furthermore, to understand whether participants experienced daily fluctuations in mood, we also conducted a week-long daily diary between week 1 and week 2. We expected more insecure individuals, especially those higher in attachment anxiety, to struggle more with mood and mental health problems during the pandemic compared to more secure individuals. We also hypothesized that anxious individuals would be more likely to report that their mood fluctuated during the day compared to avoidant and secure individuals.
2. Method
2.1. Participants
A total of 200 participants completed the baseline. The attrition rate was 4% at the end of the daily diary entries and 8.5% at the end of the 5 weeks. All participants completed at least two time-points and were therefore included in the final analyses. Around half the participants were women (n = 105, 52.5%) and half men (n = 93, 46.5%). Participants were 36.5 (SD = 12.3) years old on average and had been in a relationship for 11.1 years (SD = 9.32). They were primarily white (92.0%), heterosexual (91.0%), educated (63% had a university degree, 19% some university education and 14% graduated high school), in full-time employment (60.5%; part-time 11.5%; self-employed 13.0%; other 10%), and from the United Kingdom (59.5%; USA 8.5%, Portugal 6.5%, Poland 4.6%, other 20.9%). Thirty-one percent said they normally worked from home. Around half the participants were married (51.0%), half cohabiting (49.0%), and half of them had children (52.5%). A minority of participants were keyworkers (individuals working in critical roles such as in healthcare during the pandemic; 17.0%), reported their employment had changed (23.5%), or had shown coronavirus symptoms at baseline (10.5%). All participants reported that the country in which they were living had imposed social distancing measures due to the pandemic. None had been diagnosed with coronavirus at baseline.
2.2. Procedure
The data were collected as part of a larger study on relationships during COVID-19. The methods, hypotheses, and analyses were preregistered on the Open Science Framework: https://osf.io/2vw6y/?view_only=e1c7fe8d17d848f69858ab0e34386651. Data, code, and materials can be found here: https://osf.io/3xf86/?view_only=c473bcd9bce346ca9a6fc42c875d9100. The study received ethical approval from the authors' institutional review board. Participants were recruited via Prolific and were eligible to participate if they were aged 18 or above and currently living with their partner in a country in which social distancing measures were in place. We limited the number of participants to 200 because of funding.1 Participants were reimbursed £4.70 after completing the daily diary and a further £2.00 after completing all follow-ups.
All participants completed the baseline survey (reporting on demographic characteristics and attachment) on 31st March 2020, which was shortly after many countries had gone into lockdown. Participants completed daily surveys for 7 days (the first entry was completed directly after the baseline survey) followed by three further weekly follow-ups. This resulted in a total of seven daily diary entries and five weekly surveys. In the daily entries, participants responded to questions about their mood and mood fluctuation (fluctuated or constant) over the past 24 h and in the weekly entries, the participants responded to questions about depression and anxiety. All surveys were conducted via Qualtrics.
3. Measures
3.1. Attachment
Attachment was measured at baseline using the short version of the Experience in Close Relationships questionnaire (ECR-12; Wei et al., 2007); which includes 12 Likert-scale items with two six-item subscales: anxiety (e.g., “I worry that my partner won't care about me as much as I care about them.”; α = 0.83) and avoidance (e.g., “I don't feel comfortable opening up to my partner.”; α = 0.85). Participants rated their agreement with each item on a scale from 0 (Disagree Strongly) to 10 (Agree Strongly).
3.2. Mental health outcome measures
We used a modified version of the 4-item Patient Health Questionnaire (PHQ4; Kroenke et al., 2009) to assess depression and anxiety weekly over the study period. The questionnaire includes two items on depression (“feeling down, depressed, or hopeless” and “little interest or pleasure in doing things”) and two items on anxiety “feeling nervous, anxious, or on edge” and “not being able to stop or control worrying”). The correlation between the variables was r = 0.78 for depression and r = 0.71 for anxiety. We asked how intense the symptoms were on a Likert scale between 0 (not at all intense) and 10 (extremely intense). In the daily diaries, we also asked participants to rate their mood over the past 24 h on a scale from −10 (negative) to +10 (positive) with 0 being neutral and asked whether their mood had been constant (n = 814) or fluctuated (n = 553) throughout the day.
3.3. Data analysis plan
Time was scaled to start at 0 and was included in both daily diary and weekly analyses. Daily diary data and the weekly longitudinal data were both analyzed separately using hierarchical linear modeling (Raudenbush & Bryk, 2002) with two levels. Attachment anxiety and avoidance were only measured once at baseline and did not vary across time-points. All data were analyzed using the lme4 (Bates et al., 2015) package in R. Four models with and without covariates were preregistered to test the hypotheses and therefore we used an alpha level of p < .0125 as a cutoff for significance. We included all demographic variables in the models initially: gender, age, relationship length, children, employment, education level, employment changed, normally work from home, time since social distancing measures began, key worker, and current coronavirus symptoms. Because the covariates were only measured once and therefore did not have a large number of measurement points, we then removed non-significant covariates from the models and rerun the models with only significant covariates. We presented results for models with and without significant covariates. Models with covariates included can be found in Supplemental material.
We included a random intercept in all models but were only able to retain a random slope of time in the model with mood as an outcome variable. In all other analyses, we only retained a random intercept because otherwise the models failed to converge. A model predicting mood fluctuation with any covariates included also failed to converge and therefore we were unable to examine the model with covariates as preregistered. It is likely that the models failed to converge because we only had a smaller number of timepoints and may not have had enough variance in the data. The code and full results for all analyses conducted can be found on the OSF project page.
4. Results
The means, standard deviations, and correlations for the main study variables can be found in Table 1 . Both attachment anxiety and avoidance were significantly correlated with mood and depression but only attachment anxiety was significantly correlated with anxiety. Neither attachment anxiety nor avoidance were significantly correlated with mood fluctuations.
Table 1.
Correlations among key study variables for Study 1.
| Study 1 | ||||
|---|---|---|---|---|
| Variable | M | SD | Attachment anxiety | Attachment avoidance |
| Attachment anxiety | 3.67 | 2.17 | – | 0.16 [0.11, 0.21] |
| Attachment Avoidance | 2.27 | 1.74 | 0.16 [0.11, 0.21] | – |
| Mood | 3.07 | 4.75 | −0.14 [−0.19, −0.08] | −0.13 [−0.18, −0.08] |
| Anxiety | 3.56 | 2.44 | 0.19 [0.13, 0.25] | 0.03 [−0.04, 0.09] |
| Depression | 3.31 | 2.29 | 0.17 [0.10, 0.23] | 0.08 [0.02, 0.15] |
| Fluctuate | Constant | |||
|---|---|---|---|---|
| Mood fluctuation | n = 553 | n = 814 | 0.05 [−0.00, 0.10] | 0.00 [−0.05, 0.05] |
We expected that individuals higher in attachment insecurity, especially those scoring higher in attachment anxiety, would report more mental health problems during the lockdown (see Table 2 for the full results). As expected, individuals higher in attachment anxiety reported significantly higher levels of anxiety (β = 0.19) and depression (β = 0.16) compared to more secure individuals during the five-week period under lockdown. When accounting for significant covariates (gender for anxiety and age and employment for depression), attachment anxiety remained a significant predictor of anxiety but not depression (see Table S1 in supplemental material). Individuals who were younger (β = −0.22) and employed full-time (β = −0.23) had lower depression symptoms than those who were older and not employed full-time. Attachment avoidance did not significantly predict depression or anxiety levels in the sample. Contrary to our prediction, neither attachment anxiety nor avoidance were significantly associated with mood or mood fluctuations during the daily diary period.
Table 2.
Results for the hierarchical linear models for each outcome variable for Study 1.
| Predictors | Daily |
Weekly |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mood |
Mood fluctuation |
PHQ anxiety |
PHQ depression |
||||||||||||
| B | CI | p | β | Odds ratios | CI | p | B | CI | p | β | B | CI | p | β | |
| Intercept | 2.65 | 2.07–3.24 | <0.001 | 0.96 | 0.68–1.34 | 0.798 | 3.76 | 3.46–4.06 | <0.001 | 3.41 | 3.13–3.69 | <0.001 | |||
| Time | 0.16 | 0.04–0.27 | 0.007 | 0.07 | 0.82 | 0.76–0.88 | <0.001 | −0.02 | −0.03 to−0.00 | 0.007 | −0.06 | −0.01 | −0.02–0.00 | 0.177 | −0.03 |
| Anxiety | −0.24 | −0.48 to −0.01 | 0.042 | −0.11 | 1.08 | 0.95–1.23 | 0.222 | 0.22 | 0.10–0.34 | <0.001 | 0.19 | 0.17 | 0.05–0.28 | 0.004 | 0.16 |
| Avoidance | −0.26 | −0.55–0.03 | 0.076 | −0.12 | 0.98 | 0.83–1.15 | 0.818 | −0.02 | −0.17–0.13 | 0.809 | −0.01 | 0.06 | −0.08–0.21 | 0.371 | 0.05 |
| Random effects | ||||
|---|---|---|---|---|
| σ2 | 8.91 | 3.29 | 2.8 | 2.52 |
| τ00 | 13.61 | 3.03 | 2.92 | 2.59 |
| ICC | 0.60 | 0.48 | 0.51 | 0.51 |
| N | 200 | 200 | 200 | 200 |
| Observations | 1352 | 1347 | 949 | 949 |
| Marginal R2/Conditional R2 | 0.029/0.609 | 0.030/0.495 | 0.041/0.530 | 0.031/0.522 |
Note. We report standardized beta coefficients as a measure of effect size for continuous outcomes and odds ratios for binary outcomes. The marginal R2 refers to the explanatory power of the fixed effects model and the conditional R2 refers to the random effects.
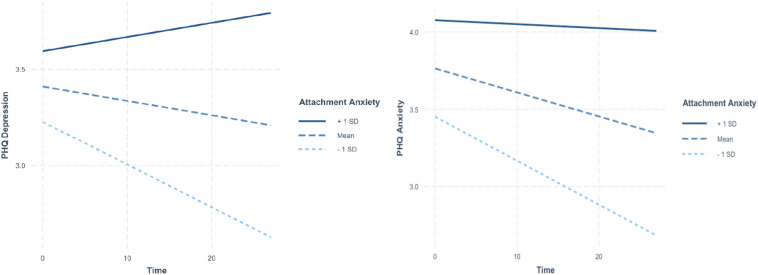
Furthermore, over time participants reported a slight increase in mood (β = 0.07) with people being 1.22 times more likely to report their mood was constant rather than fluctuated. During the course of the 5 weeks, participants also reported less anxiety (β = −0.06) whereas the overall level of depression did not change. We also explored whether the association between attachment and mental health outcomes varied over time by including an interaction of attachment dimensions by time in the models. The results showed that attachment anxiety was a significant moderator between time and depression (β = 0.06 (SE = 0.002), t = 2.72, p = .007; see Fig. 1 ): the simple slopes analyses showed that individuals higher in attachment anxiety did not vary in their level of depression (B = 0.01 (SE = 0.01), t = 0.97)2 whereas individuals lower in attachment anxiety reported a decrease in depression over time (B = −0.02 (SE = 0.01), t = −2.90). The pattern of results was similar, although not significant, for anxiety. Attachment avoidance was not a significant moderator for anxiety or depression.
Fig. 1.
The results of the simple slope analyses depicting the association between Time and Depression (left) and Anxiety (right) at different levels of Attachment anxiety for the longitudinal weekly data note. The main interaction effect for anxiety (SE = 0.002), t = 2.27, p = .020) was not significant at the alpha level of 0.0125 but shows a similar pattern as depression: the simple slopes analyses showed that individuals higher in attachment anxiety did not vary in their anxiety levels (B = 0.002 (SE = 0.01), t = −0.32) whereas individuals lower in anxiety reported a decrease in anxiety over the study period (B = −0.03 (SE = 0.01), t = −3.53).
5. Discussion
Overall, Study 1 provided partial support for the hypotheses: the results showed that individuals higher in attachment anxiety experienced higher levels of depression and anxiety during the first wave of the COVID-19 pandemic compared to individuals lower in attachment anxiety. We also found that individuals higher in attachment anxiety remained higher in anxiety and depression during the study period while those lower in attachment anxiety experienced a reduction in depression and anxiety levels. This may be because anxious individuals' use of hyperactivating strategies require more emotional resources which may not be available during the pandemic. They also seek excessive reassurance in relationships (Brennan & Carnelley, 1999; Cassidy, 1994; Shaver et al., 2005). However, during the pandemic, their partner may not be able to provide reassurance because they themselves may be feeling worried about the pandemic and may not have resources themselves. Recent research has also found that anxiously attached individuals tend to act in punitive ways toward their partners which can create conflict and damage closeness (Overall et al., 2021). This may have undermined the caregiving efforts from partners during the pandemic thus rendering the anxiously attached individuals more vulnerable to distress during the pandemic.
Furthermore, when we included significant covariates in the model, attachment anxiety remained a significant predictor of anxiety. However, age and employment status were better predictors of depression than attachment anxiety. It is understandable that employment would be a stronger predictor of depression during a pandemic when many people are afraid of losing their jobs, there are very few jobs available, and competition is high. Therefore, people in less secure employment situations (e.g., part-time, self-employed) are understandably more at risk of mental health problems. We also cannot rule out the possibility that individuals were in less secure employment situations because of existing mental health problems and thus employment correlated significantly with depression. Furthermore, older individuals are more likely to have children and have more responsibilities and thus be more adversely affected by the pandemic compared to younger people. Employment and age did not significantly correlate with anxiety scores.
Contrary to our hypotheses, attachment avoidance was not associated with mental health outcomes. Previous research has shown that attachment avoidance is inconsistently associated with mental health outcomes (Eberhart & Hammen, 2009; Stanton & Campbell, 2014; Surcinelli et al., 2010) potentially because avoidant individuals may be using distancing strategies (Birnbaum et al., 1997; Shapiro & Levendosky, 1999) that were still working after a month. Furthermore, although the effect was negative, neither attachment anxiety nor attachment avoidance were significantly associated with daily mood or perception in mood fluctuation. Future research should investigate whether this finding is replicated using a different/well-validated mood measure. Many participants (40%) also responded that their mood fluctuated during the day which meant that participants may have rated their average level of mood differently.
Finally, we found that over the five-week period, participants' anxiety reduced but depression did not. This may be because the data collection began in the beginning of the pandemic when uncertainty about the near future was high, but after 5 weeks of similar circumstances people's anxiety levels had stabilized. We would not expect depression to necessarily decrease because most participants were still under the same lockdown rules 5 weeks later and thus remained isolated. Because we did not have pre-pandemic data to examine whether attachment anxiety predicted change in mental health outcomes due to the pandemic, we analyzed data from a second study.
6. Study 2
In order to understand whether attachment insecurity predicted changes in mental health outcomes from before to during the pandemic, we collected data before the pandemic and again during the first wave of the pandemic in Study 2. Furthermore, we collected data from both members of the dyad in order to examine whether partner's attachment styles may be associated with actor's mental health outcomes. Indeed, previous research has shown that attachment anxiety and avoidance can interfere with providing support (Mikulincer & Shaver, 2009). Given that partners may be the only people available for support during the pandemic, it is possible that partner's attachment style may be associated with actor's mental health outcomes. As in Study 1, we expected more insecure individuals, especially those higher in attachment anxiety, to struggle more with mental health problems during the pandemic compared to more secure individuals. We did not make any a priori hypotheses about partner effects given lack of prior literature on the topic. However, if anything, we would expect the partner effects to be similar to actor effects.
7. Method
7.1. Participants
The sample comprised 100 romantic couples (87 heterosexual, 9 lesbian, 1 gay, 3 other non-binary) recruited from a large university in the UK and surrounding community via social media posts, advertisements in local magazines, and at local wedding fairs. Participants were 18–64 years of age (M = 24.15 years, SD = 6.61 years) and were in relationships lasting 3 months to 35.5 years (M = 2.84 years, SD = 4.41 years). Participants identified their race/ethnicity as White (85.5%), Latinx (3%), East Asian (1.5%), South Asian (2.5%), Southeast Asian (2.5%), bi-/multi-racial (3%), and “other” (2%). Approximately 85.5% of the sample were dating casually or exclusively, 1.5% were common-law, 5% were engaged, 1.5% were in a civil partnership, and 6.5% were married. A minority of couples (38%) were cohabiting at Phase 1 (baseline); this increased to 49% at Phase 3 (2.5 months later).
7.2. Procedure
Data were taken from a larger longitudinal study of romantic couples (see https://osf.io/ekv6x/?view_only=25c7b0aad7d04be8b164a2d0aa2e6009) and the preregistration for this study can be found here: https://osf.io/k26q8/?view_only=c35951f412584822ac9679b7be42b58e. The code for the analysis is available here: https://osf.io/3xf86/?view_only=c473bcd9bce346ca9a6fc42c875d9100. The study received ethical approval from the authors' institutional review board. The study had three phases: An initial 2-hour lab session (Phase 1), a 14-day diary period (Phase 2), and a follow-up survey 2 months later (Phase 3). Data for Phases 1 and 2 were collected between mid-January and March 2020, prior to the outbreak of COVID-19 in the UK and the introduction of lockdown and other social restrictions. Phase 3 data were collected between April and May 2020, amid lockdown and physical distancing rule enforcement in the UK. The present analyses use data from Phases 1 and 3 of the parent project. In Phase 1, couples arrived at the lab together and provided informed consent. They then completed several tasks including a battery of questionnaires that contained demographic measures. Phase 3 began 2 months after the end of Phase 2 and involved a 45-minute online follow-up survey which included a measure of depression symptoms. The Phase 3 survey links were individual and set to expire 1 week later. After finishing Phase 3, partners were debriefed and compensated up to GBP-£50.00 each based on how many parts of the study they completed. All surveys were conducted via Qualtrics.
8. Measures
8.1. Attachment
Attachment was measured at Phase 1 using the short version of the Experience in Close Relationships questionnaire (ECR-12; Wei et al., 2007), as in Study 1. Participants rated their agreement with each item on a scale from 1 (strongly disagree) to 7 (strongly agree). The reliability was α = 0.80 for attachment anxiety and α = 0.78 for attachment avoidance.
8.2. Mental health outcome measures
At both Phases 1 and 3, participants completed the PHQ-9 (Kroenke et al., 2001), where they indicated how often they experienced nine depression symptoms (e.g., “Little interest or pleasure in doing things”) using a 4-point scale (0 = not at all, 3 = nearly every day) The reliability was α = 0.86 for Phase 1 and α = 0.88 for Phase 3. Participants also completed the GAD-7 (Spitzer et al., 2006), where they indicated how often they experienced seven anxiety symptoms (e.g., “Feeling nervous, anxious, or on edge”) using a 4-point scale (0 = not at all, 3 = nearly every day). The reliability was α = 0.90 for Phase 1 and α = 0.91 for Phase 3.
8.3. Data analysis plan
The data were analyzed using the Actor-Partner Interdependence Model with hierarchical linear modeling with two levels (individuals nested within dyads; Kenny et al., 2006). All data were analyzed using the lme4 (Bates et al., 2015) package in R. Two models with and without covariates were preregistered to test the hypotheses and therefore we used an alpha level of p < .025 as a cutoff for significance. We included gender, age, and living situation as covariates. The code and full results for all analyses conducted can be found on the OSF project page.
9. Results
The means, standard deviations, and correlations for the main study variables can be found in Table 3 . We hypothesized that individuals higher in attachment insecurity, especially those scoring higher in attachment anxiety, would report more mental health problems during the lockdown (see Table 4 for the full results). As expected, individuals higher in attachment anxiety reported significantly higher levels of anxiety (β = 0.31) and depression (β = 0.29) during the first wave of the pandemic compared to more secure individuals after controlling for pre-pandemic scores for anxiety and depression, respectively. Attachment avoidance or partner's attachment anxiety or avoidance were not significant predictors of actor's anxiety or depression. The results remained the same after including all covariates in the model (see Table S2 in supplemental file).
Table 3.
Means, standard deviations, and correlations with confidence intervals for Study 2.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Attachment Anxiety (A) | 3.88 | 1.30 | |||||||
| 2. Attachment Avoidance (A) | 2.27 | 0.90 | −0.02 [−0.16, 0.12] |
||||||
| 3. P Attachment Anxiety (P) | 3.88 | 1.30 | 0.05 [−0.10, 0.18] |
0.09 [−0.05, 0.23] |
|||||
| 4. P Attachment Avoidance (P) | 2.27 | 0.90 | 0.09 [−0.05, 0.23] |
0.15⁎ [0.01, 0.28] |
−0.02 [−0.16, 0.12] |
||||
| 5. T1 Depression (A) | 6.98 | 5.24 | 0.41⁎⁎ [0.29, 0.52] |
0.06 [−0.08, 0.19] |
0.21⁎⁎ [0.07, 0.34] |
−0.04 [−0.18, 0.10] |
|||
| 6. T1 Anxiety (A) | 6.47 | 5.08 | 0.47⁎⁎ [0.36, 0.57] |
0.03 [−0.11, 0.17] |
0.14⁎ [0.00, 0.27] |
0.07 [−0.07, 0.21] |
0.74⁎⁎ [0.67, 0.80] |
||
| 7. T2 Depression (A) | 6.89 | 5.30 | 0.33⁎⁎ [0.19, 0.46] |
0.12 [−0.03, 0.26] |
0.19⁎ [0.05, 0.33] |
0.02 [−0.13, 0.17] |
0.52⁎⁎ [0.40, 0.62] |
0.49⁎⁎ [0.36, 0.59] |
|
| 8. T2 Anxiety (A) | 6.24 | 5.07 | 0.36⁎⁎ [0.22, 0.48] |
0.08 [−0.07, 0.23] |
0.16⁎ [0.01, 0.30] |
0.00 [−0.15, 0.15] |
0.48⁎⁎ [0.36, 0.59] |
0.57⁎⁎ [0.46, 0.66] |
0.72⁎⁎ [0.64, 0.78] |
Note. M and SD are used to represent mean and standard deviation, respectively. Values in square brackets indicate the 95% confidence interval for each correlation. The confidence interval is a plausible range of population correlations that could have caused the sample correlation.
Indicates p < .05.
Indicates p < .01.
Table 4.
Results for the hierarchical linear models for depression and anxiety for Study 2.
| Predictors | Depression T2 |
Anxiety T2 |
||||||
|---|---|---|---|---|---|---|---|---|
| Estimates | CI | p | β | Estimates | CI | p | β | |
| Intercept | 6.98 | 6.26–7.70 | <0.001 | 6.36 | 5.76–6.96 | <0.001 | ||
| Attachment Anxiety (A) | 1.16 | 0.64–1.68 | <0.001 | 0.29 | 1.21 | 0.72–1.69 | <0.001 | 0.31 |
| Attachment Avoidance (A) | 0.09 | −0.64–0.83 | 0.806 | 0.02 | −0.17 | −0.86–0.52 | 0.633 | −0.03 |
| Attachment Anxiety (P) | 0.41 | −0.10–0.91 | 0.113 | 0.10 | 0.21 | −0.25–0.68 | 0.362 | 0.05 |
| Attachment Avoidance (P) | −0.26 | −0.98–0.46 | 0.481 | −0.04 | 0.44 | −0.23–1.12 | 0.198 | 0.08 |
| T1 control | 0.38 | 0.25–0.51 | <0.001 | 0.38 | 0.45 | 0.33–0.58 | <0.001 | 0.45 |
| Random effects | ||
|---|---|---|
| σ2 | 14.11 | 15.68 |
| τ00 | 4.76 | 0.26 |
| ICC | 0.25 | 0.02 |
| N | 93 | 93 |
| Observations | 172 | 172 |
| Marginal R2/Conditional R2 | 0.328/0.497 | 0.406/0.416 |
Note. A = actor, P = partner. We report standardized beta coefficients as a measure of effect size. The marginal R2 refers to the explanatory power of the fixed effects model and the conditional R2 refers to the random effects. Models are reported after controlling for age, gender, and living status.
10. Discussion
Study 2 provided further support for our hypotheses: the results showed that individuals higher in attachment anxiety experienced higher levels of depression and anxiety compared to individuals lower in attachment anxiety during the pandemic controlling for pre-pandemic levels of anxiety and depression. These results remained significant after accounting for covariates in the model. In line with Study 1, attachment avoidance was not significantly associated with mental health outcomes. Contrary to previous research (Vindegaard & Benros, 2020), the average level of depression and anxiety did not vary from before the pandemic to during the pandemic in the overall sample. This is likely because individuals high in attachment anxiety became more anxious and depressed over the study period compared to individuals low in attachment anxiety who became less anxious and depressed over the study period. In line with many previous studies (e.g., Joel et al., 2020), partner effects of attachment were not significant. This may be because the actors' perception of their partner is more important than their partners' perception of themselves. For example, research has shown that anxious individuals perceive their partners as less supportive regardless of whether their partner reports themselves as being less supportive (Mikulincer & Shaver, 2016). Their partner's attachment style is therefore less important than their own own in predicting anxiously attached individuals' outcomes.
10.1. General discussion
Due to the COVID-19 pandemic, the worst hit countries in the world are facing a mental health crisis among other issues caused by the pandemic (Moccia et al., 2020; Vindegaard & Benros, 2020). Therefore, understanding potential risk factors that are associated with an increased likelihood of poor mental health is urgently needed in order to develop intervention strategies (Sani et al., 2020). The aim of the present research was to answer this call and to extend our current understanding of who may be at a particular risk of mental health problems due to the pandemic. We advanced the literature in several important ways: we used longitudinal data to assess mental health outcomes over the course of the first wave of COVID-19 (Study 1), collected data pre- and during pandemic (Study 2), collected daily diary data to assess the daily impact of the pandemic on mood and mood fluctuations, examined the effect of attachment insecurity on mental health and mood, and examined potential partner effects of attachment insecurity on mental health outcomes. We also assessed attachment styles as moderators for the association between time under lockdown and mental health outcomes to understand potential trajectories over time.
In line with our hypothesis and a previous cross-sectional study (Moccia et al., 2020), the results showed that individuals higher in attachment anxiety were particularly at risk of adverse mental health outcomes. This may be because anxiously attached individuals are preoccupied with their partner's availability because of their fear of being abandoned (Brennan & Carnelley, 1999; Cassidy, 1994; Shaver et al., 2005), thus being unable to focus on taking care of themselves. Furthermore, mounting research has shown that attachment anxiety is one of the most important predictors of poor relationship outcomes during the pandemic (Eder et al., 2021). This is particularly concerning because in the moderator analyses in Study 1, we found that while people lower in attachment anxiety became less anxious and depressed over time, individuals higher in attachment anxiety remained highly anxious and depressed. This is particularly concerning given that this may place more anxiously attached individuals at a risk of poor mental health outcomes longer-term.
However, although the effect was in the expected direction, contrary to our prediction, attachment anxiety was not significantly associated with daily mood or fluctuations in mood in Study 1. This may have been because the daily diary data were collected in the beginning of lockdown and all participants in the study were living with their partners. Individuals higher in attachment anxiety could have been initially experiencing less negative mood because their partner was more available, and they would not have to share their attention or time. However, because anxiously attached individuals doubt their partner's love and availability (Cassidy, 1994; Simpson, 1990), it is possible that over time the initial positive mood created by their partner being at home would wear off. Although not specific to attachment, recent research has found that individuals who were satisfied with the use of online technology experienced a decrease in anxiety, depression, and loneliness (Juvonen et al., 2021). Thus, online technologies may have also contributed to an overall relatively stable mood across the first 5 weeks of the pandemic. However, anxiously attached individuals tend to be less satisfied with the use of online technologies (Young et al., 2020) and thus it is possible that these initial advantages would not have lasted longer-term. Therefore, it is important to examine the long-term impact of the pandemic on daily mood for anxiously attached individuals in future research.
Attachment avoidance did not significantly predict any of the mental health outcomes examined across the two studies. This is contrary to our prediction that avoidant individuals would also be at a higher risk of mental health problems overall, although we did expect that the effect would be stronger for attachment anxiety. The existing literature on attachment avoidance and mental health is complex with many studies showing poorer mental health outcomes (Liu et al., 2009; Marganska et al., 2013) whereas others have not found a significant difference between avoidant and secure individuals (Surcinelli et al., 2010). A previous cross-sectional study conducted during the pandemic actually found that both avoidant and secure attachment were protective factors for poor mental health outcomes during the pandemic (Moccia et al., 2020). It may be that because avoidant individuals tend to use distancing strategies such as distractions, denial, and disengagement (J. A. Feeney, 1995; Holmberg et al., 2011), they are better able to manage potentially distressing thoughts regarding the pandemic. However, it may also be that because avoidant individuals use distancing strategies, they are less likely to acknowledge and report their distress. Some research suggests that the distancing strategies may work initially but may fail when faced with severe and more enduring stressors (Birnbaum et al., 1997; Shapiro & Levendosky, 1999). The pandemic is arguably a severe and enduring stressor, however, we only followed participants during the first wave of the pandemic (until end of April 2020 in Study 1 and May 2020 in Study 2) which may not have been enough time for avoidant individuals' strategies to fail. Future research is needed to understand the potential long-term impacts of the pandemic on individuals higher in avoidance. Future research could also examine well-being outcomes less susceptible to social desirability, like psychophysiological indicators of stress such as raised heart rate or skin conductance level, and ask partners' perceptions of each other's level of anxiety and depression.
11. Strengths and limitations
The study had several strengths: in Study 1 we collected longitudinal data over a five-week period to examine the effect of the pandemic on mental health over time; we collected daily diary data to understand daily mood and fluctuations in mood; and all participants completed the surveys on the same day at the start of most countries' lockdowns capturing the early experiences of people under stay-at-home orders. In Study 2, we compared mental health outcomes from pre-pandemic levels to during the pandemic and collected data from both members of the couple to examine potential partner effects.
However, the findings should be considered with several limitations in mind. First, while we used validated measures for depression, anxiety, and attachment, we created single item measures for mood and mood fluctuation for Study 1. This was therefore only a blunt tool to examine mood in the daily diaries and there may be better ways of measuring mood over time. Many participants reported that their mood fluctuated during the day which may have meant that some participants reported an average whereas others may have given a report of their current mood level when they completed the daily survey. Future research is needed to better understand individuals' mood during lockdown using validated measures. Second, while we provided evidence from two longitudinal studies, these studies only cover the peak of the first wave of the COVID-19 pandemic and cannot address the potential impact of attachment anxiety on long-term mental health outcomes. Therefore, future research is needed to examine these outcomes over a longer period. Third, because the data were collected as part of a larger study, all participants in the sample consisted of individuals who were in a relationship. Individuals who are single and living alone are at an increased risk of social isolation and mental health problems given that they may have spent months without seeing anyone in person (Luchetti et al., 2020). Most of the participants were also white. Preliminary findings have shown that black and minority ethnic groups are at a higher risk of contracting and dying from COVID-19 (Pan et al., 2020; Pareek et al., 2020). Therefore, future research should be conducted in more diverse samples to be able to account for other potential demographic risk factors.
12. Theoretical and practical implications
The present study provides further support for attachment theory's notion that insecurely attached individuals are at a higher risk of emotional difficulties and are less able to cope in stressful situations. The results highlight that highly anxiously attached individuals may be at a particular risk of mental health problems during the pandemic, which may generalize into other enduring stressful situations. This may be because anxious individuals are more likely to engage in emotion-focused coping such as ruminating and focusing on their distress (Chung, 2014; Garrison et al., 2014; Trillingsgaard et al., 2011), making them unable to detach from the situation. Emotion-focused coping may also be particularly problematic during an extended period of stay-at-home orders because partners may grow weary of the anxious individual's expressions of their distress. This may cause more conflict further triggering anxiously attached partners' insecurities. Study 1 also showed that while most participants' mental health improved over the course of the study period, highly anxious individuals' levels of depression and anxiety remained similar throughout the study. This suggests that attachment anxiety may be a risk factor for chronic mental health problems longer term rather than being able to bounce back as restrictions are gradually lifted and some level of normalcy has returned. This notion highlights the potential enduring impact of stressors on anxiously attached individuals as they may lack resources to recover from stressful events.
Practitioners who work with mental health problems may see an influx of clients who are more anxiously attached, and the practitioners may need to tailor treatments to not only address the mental health problem but to also work on increasing the anxious attached individuals' sense of safety and security. Attachment-based or attachment-informed therapies (e.g., Attachment based family therapy [Waraan et al., 2021 and Emotionally-focused therapy [Greenberg & Johnson, 1988) may be particularly helpful during this time as clinicians will need to be aware of the different strategies anxiously and avoidantly attached individuals use to cope with their distress. For example, because avoidant individuals tend to use distancing strategies to cope with distress (Holmberg et al., 2011), they may minimize their level of distress, be reluctant to admit they are struggling, and be less likely to engage with treatment. Anxious individuals, on the other hand, are more likely to engage in therapy but may struggle if the therapist becomes ill or goes on vacation (Yotsidi et al., 2019). Therefore, additional measures may need to be put in place to ensure that anxiously attached clients do not feel abandoned during this highly stressful time.
13. Conclusion
In sum, the present studies added to the emerging literature into how the COVID-19 pandemic is impacting individuals' mental health outcomes over time and examined attachment insecurity as a potential risk factor for poor mental health outcomes. The results showed that individuals higher in attachment anxiety reported higher levels of depression and anxiety during the pandemic controlling for pre-pandemic levels of depression and anxiety in Study 2. Furthermore, while other participants experienced an improvement in depression and anxiety, more anxiously attached individuals' scores remained high in Study 1. These results are especially important when considering interventions to help individuals weather the pandemic.
CRediT authorship contribution statement
Laura M. Vowels: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing. Katherine B. Carnelley: Conceptualization, Methodology, Writing – review & editing. Sarah C.E. Stanton: Conceptualization, Methodology, Investigation, Writing – review & editing.
Footnotes
All data, code, and materials along with the preregistration are available on the Open Science Framework with anonymized links in the manuscript.
Study 1 was supported by the Jubilee Scholarship, University of Southampton, awarded to Laura M. Vowels. Study 2 was supported by a New Investigator Grant awarded to Sarah C. E. Stanton from the Economic and Social Research Council (ESRC) of the United Kingdom.
There are no conflicts of interest to disclose.
The study received ethical approval from the authors' institutional review board and all participants consented to participate in the study.
The power calculation was based on the primary study hypotheses, which included the same number of participants but had up to 4200 observations and had 96.7% power to estimate an average effect size (r = 0.22) in Psychology (Richard et al., 2003).
Note that the simple slopes estimates are unstandardized because R does not provide standardized coefficients for simple slopes. Confidence intervals or p-values are also not available.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.paid.2021.111256.
Appendix A. Supplementary data
Supplementary tables
References
- Bartholomew K., Horowitz L.M. Attachment styles among young adults: A test of a four-category model. Journal of Personality and Social Psychology. 1991;61(2):226–244. doi: 10.1037//0022-3514.61.2.226. [DOI] [PubMed] [Google Scholar]
- Bates D., Maechler M., Bolker B.M., Walker S.C., Mächler M., Bolker B.M., Walker S.C. Fitting linear mixed-effects models using lme4. Journal of Statistical Software. 2015;67(1):1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Birnbaum G.E., Idit O., Mikulincer M., Florian V. When marriage breaks up - Does attachment style contribute to coping and mental health? Journal of Social and Personal Relationships. 1997;14(5):643–654. doi: 10.1177/0265407597145004. [DOI] [Google Scholar]
- Bowlby J. Attachment. 1st ed. Vol 1. Basic Books; 1969. Attachment and loss. [Google Scholar]
- Brennan K.A., Carnelley K.B. Using meaning to mend holes in the nomological net of excessive reassurance-seeking and depression. Psychological Inquiry. 1999;10:282–285. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Www.Thelancet.Com [DOI] [PMC free article] [PubMed]
- Cassidy J. Emotion regulation: Influences of attachment relationships. Monographs of the Society for Research in Child Development. 1994;59:228–283. doi: 10.2307/1166148. [DOI] [PubMed] [Google Scholar]
- Chung M.S. Pathways between attachment and marital satisfaction: The mediating roles of rumination, empathy, and forgiveness. Personality and Individual Differences. 2014;70:246–251. doi: 10.1016/j.paid.2014.06.032. [DOI] [Google Scholar]
- Dagan O., Facompré C.R., Bernard K. Journal of affective disorders. Vol. 236. Elsevier B.V.; 2018. Adult attachment representations and depressive symptoms: A meta-analysis; pp. 274–290. [DOI] [PubMed] [Google Scholar]
- Eberhart N.K., Hammen C.L. Interpersonal predictors of stress generation. Personality and Social Psychology Bulletin. 2009;35(5):544–556. doi: 10.1177/0146167208329857. [DOI] [PubMed] [Google Scholar]
- Eder S.J., Nicholson A.A., Stefanczyk M.M., Pieniak M., Martínez-Molina J., Pešout O.…Steyrl D. Securing your relationship: Quality of intimate relationships during the COVID-19 pandemic can be predicted by attachment style. Frontiers in Psychology. 2021;0:3016. doi: 10.3389/FPSYG.2021.647956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney B.C., Collins N.L. A new look at social support: A theoretical perspective on thriving through relationships. Personality and Social Psychology Review. 2015;19(2):113–147. doi: 10.1177/1088868314544222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney J.A. Adult attachment and emotional control. Personal Relationships. 1995;2(2):143–159. doi: 10.1111/j.1475-6811.1995.tb00082.x. [DOI] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison A.M., Kahn J.H., Miller S.A., Sauer E.M. Emotional avoidance and rumination as mediators of the relation between adult attachment and emotional disclosure. Personality and Individual Differences. 2014;70:239–245. doi: 10.1016/j.paid.2014.07.006. [DOI] [Google Scholar]
- Greenberg L.S., Johnson S.M. Guilford Press; 1988. Emotionally focused therapy for couples. [Google Scholar]
- Holmberg D., Lomore C.D., Takacs T.A., Price L.E., Price E.L. Adult attachment styles and stressor severity as moderators of the coping sequence. Personal Relationships. 2011;18(3):502–517. doi: 10.1111/j.1475-6811.2010.01318.x. [DOI] [Google Scholar]
- Huckins J.F., daSilva A.W., Wang W., Hedlund E., Rogers C., Nepal S.K.…Campbell A.T. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research. 2020;22(e20185):1–13. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joel S., Eastwick P.W., Allison C.J., Arriaga X.B., Baker Z.G., Bar-Kalifa E.…Wolf S. Machine learning uncovers the most robust self-report predictors of relationship quality across 43 longitudinal couples studies. Proceedings of the National Academy of Sciences of the United States of America. 2020;117:19061–19071. doi: 10.1073/pnas.1917036117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juvonen J., Schacter H.L., Lessard L.M. 38(6) 2021. Connecting electronically with friends to cope with isolation during COVID-19 pandemic; pp. 1782–1799. [DOI] [Google Scholar]
- Kenny D.A., Kashy D.A., Cook W.L. Dyadic data analysis. 2006. Over-time analyses: Interval outcomes; pp. 343–370. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Liu Q., Nagata T., Shono M., Kitamura T. The effects of adult attachment and life stress on daily depression: A sample of Japanese university students. Journal of Clinical Psychology. 2009;65(7):639–652. doi: 10.1002/jclp.20572. [DOI] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. The American Psychologist. 2020 doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marganska A., Gallagher M., Miranda R. Adult attachment, emotion dysregulation, and symptoms of depression and generalized anxiety disorder. American Journal of Orthopsychiatry. 2013;83(1):131–141. doi: 10.1111/ajop.12001. [DOI] [PubMed] [Google Scholar]
- Mikulincer M., Orbach I. Attachment styles and repressive defensiveness: The accessibility and architecture of affective memories. Journal of Personality and Social Psychology. 1995;68(5):917–925. doi: 10.1037/0022-3514.68.5.917. [DOI] [PubMed] [Google Scholar]
- Mikulincer M., Shaver P.R. An attachment and behavioral systems perspective on social support. Journal of Social and Personal Relationships. 2009;26(1):7–19. doi: 10.1177/0265407509105518. [DOI] [Google Scholar]
- Mikulincer M., Shaver P.R. 2nd ed. Guildford Press; 2016. Attachment in adulthood: Structure, dynamics, and change. [Google Scholar]
- Mikulincer M., Shaver P.R., Pereg D. Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment-related strategies. Motivation and Emotion. 2003;27(2):77–102. doi: 10.1023/A:1024515519160. [DOI] [Google Scholar]
- Mikulincer M., Shaver P.R., Sapir-Lavid Y., Avihou-Kanza N. What’s inside the minds of securely and insecurely attached people? The secure-base script and its associations with attachment-style dimensions. Journal of Personality and Social Psychology. 2009;97(4):615–633. doi: 10.1037/a0015649. [DOI] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overall N.C., Chang V.T., Pietromonaco P.R., Low R.S.T., Henderson A.M.E. Partners’ attachment insecurity and stress predict poorer relationship functioning during COVID-19 quarantines. Social Psychological and Personality Science. 2021 doi: 10.1177/1948550621992973. [DOI] [Google Scholar]
- Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P.…Pareek M. The impact of ethnicity on clinical outcomes in COVID-19: A systematic review. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pareek M., Bangash M.N., Pareek N., Pan D., Sze S., Minhas J.S.…Khunti K. The Lancet. Vol. 395, Issue 10234. Lancet Publishing Group; 2020. Ethnicity and COVID-19: An urgent public health research priority; pp. 1421–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A.…Abel K.M. The lancet psychiatry. 2020. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population; pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S.W., Bryk A.S. Sage Publications; 2002. Hierarchical linear models: Applications and data analysis methods. [Google Scholar]
- Richard F.D., Bond C.F., Stokes-Zoota J.J. One hundred years of social psychology quantitatively described. Review of General Psychology. 2003;7:331–363. doi: 10.1037/1089-2680.7.4.331. [DOI] [Google Scholar]
- Sani G., Janiri D., Di Nicola M., Janiri L., Ferretti S., Chieffo D. Psychiatry and clinical neurosciences. Vol. 74, Issue 6. Blackwell Publishing; 2020. Mental health during and after the COVID-19 emergency in Italy; p. 372. [DOI] [PubMed] [Google Scholar]
- Shapiro D.L., Levendosky A.A. Adolescent survivors of childhood sexual abuse: The mediating role of attachment style and coping in psychological and interpersonal functioning. Child Abuse and Neglect. 1999;23(11):1175–1191. doi: 10.1016/S0145-2134(99)00085-X. [DOI] [PubMed] [Google Scholar]
- Shaver P.R., Schachner D.A., Mikulincer M. Attachment style, excessive reassurance seeking, relationship processes, and depression. Personality and Social Psychology Bulletin. 2005;31(3):343–359. doi: 10.1177/0146167204271709. [DOI] [PubMed] [Google Scholar]
- Simpson J.A. Influence of attachment styles on romantic relationships. Journal of Personality and Social Psychology. 1990;59(5):971–980. doi: 10.1037//0022-3514.59.5.971. [DOI] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stanton S.C.E., Campbell L. Psychological and physiological predictors of health in romantic relationships: An attachment perspective. Journal of Personality. 2014;82(6):528–538. doi: 10.1111/jopy.12056. [DOI] [PubMed] [Google Scholar]
- Surcinelli P., Rossi N., Montebarocci O., Baldaro B. Adult attachment styles and psychological disease: Examining the mediating role of personality traits. Journal of Psychology: Interdisciplinary and Applied. 2010;144(6):523–534. doi: 10.1080/00223980.2010.508082. [DOI] [PubMed] [Google Scholar]
- Trillingsgaard T., Elklit A., Shevlin M., Maimburg R.D. Adult attachment at the transition to motherhood: Predicting worry, health care utility and relationship functioning. Journal of Reproductive and Infant Psychology. 2011;29(4):354–363. doi: 10.1080/02646838.2011.611937. [DOI] [Google Scholar]
- Vindegaard N., Benros M.E. Brain and Behavior: A Cognitive Neuroscience Perspective, and Immunity. 2020. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waraan L., Rognli E.W., Czajkowski N.O., Mehlum L., Aalberg M. Efficacy of attachment-based family therapy compared to treatment as usual for suicidal ideation in adolescents with MDD. Clinical Child Psychology and Psychiatry. 2021;26(2):464–474. doi: 10.1177/1359104520980776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M., Russell D.W., Mallinckrodt B., Vogel D.L. The experiences in close relationship scale (ECR)-short form: Reliability, validity, and factor structure. Journal of Personality Assessment. 2007;88(2):187–204. doi: 10.1080/00223890701268041. [DOI] [PubMed] [Google Scholar]
- Yotsidi V., Stalikas A., Pezirkianidis C., Pouloudi M. The belationships between client resistance and attachment to therapist in psychotherapy. Journal of Contemporary Psychotherapy. 2019;49(2):99–109. doi: 10.1007/s10879-018-9406-y. [DOI] [Google Scholar]
- Young L., Kolubinski D.C., Frings D. Attachment style moderates the relationship between social media use and user mental health and wellbeing. Heliyon. 2020;6(6) doi: 10.1016/J.HELIYON.2020.E04056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables