Abstract
Background
Governments have implemented a range of measures to tackle COVID-19, primarily focusing on changing citizens’ behaviours in order to lower the transmission of the virus. Few studies have looked at the patterns of compliance with different measures within individuals: whether people comply with all measures or selectively choose some but not others. Such research is important for designing interventions to increase compliance.
Methods
We used cross-sectional data from 20 947 UK adults in the COVID-19 Social Study collected from 17 November to 23 December 2020. Self-report compliance was assessed with six behaviours: mask wearing, hand washing, indoor household mixing, outdoor household mixing, social distancing and compliance with other guidelines. Patterns of compliance behaviour were identified using latent class analysis, and multinomial logistic regression was used to assess demographic, socioeconomic and personality predictors of behaviour patterns.
Results
We selected a four-latent class solution. Most individuals reported similar levels of compliance across the six behaviour measures. High level of compliance was the modal response. Lower self-reported compliance was related to young age, high risk-taking behaviour, low confidence in government and low empathy, among other factors. Looking at individual behaviours, mask wearing had the highest level of compliance while compliance with social distancing was relatively low.
Conclusion
Results suggest that individuals choose to comply with all guidelines, rather than some but not others. Strategies to increase compliance should focus on increasing general motivations to comply alongside specifically encouraging social distancing.
Keywords: COVID-19, public health, health
Introduction
Governments have implemented a series of measures to tackle the spread of COVID-19. Many of these measures have focused on changing citizens’ behaviours, such as advertising personal hygiene reminders (eg, washing hands), mandating the wearing of face masks, recommending social distancing in public spaces and prohibiting household mixing. These interventions are effective at reducing the spread of the virus1 but require voluntary cooperation on behalf of citizens. Compliance with these behaviours is not complete.2 3
Given the importance of these measures for tackling pandemics, a sizeable literature has emerged on the determinants and predictors of compliance, both during the current pandemic4 and from previous epidemics.5 Many of these studies have focused on specific behaviours6 or on compliance with guidelines in general.7 8 However, an understudied area is how compliance behaviours ‘cluster’ within individuals; for instance, whether individuals perform some behaviours and not others. Understanding patterns of compliance is important as it may reveal information on behaviours individuals find particularly difficult.
Studies from the current pandemic9–12 and previous epidemics13 using a range of methodological approaches, including cluster analysis,10 factor analysis9 12 14 and latent class analysis,11 13 have found several distinct patterns in compliance behaviours (though, also see ref 14). For instance, a recent German study identified a small group of individuals intending to comply only with behaviours performed in public, such as social distancing and avoiding mass events.11 However, existing studies are typically based on small samples, use data from an early stage of the COVID-19 pandemic (which is limiting as predictors differ through time8 15) or have looked at compliance intentions, rather than performed behaviours.
Therefore, in this study we explored patterns on self-reported compliance with six COVID-19 preventive behaviours using data from a sample of 20 000 UK adults 8 months after lockdown was first implemented in the UK. We further tested whether behavioural patterns were related to a wide range of demographic, socioeconomic and personality trait characteristics.
Methods
Participants
We used data from the COVID-19 Social Study; a large panel study of the psychological and social experiences of over 70 000 adults (aged 18+) in the UK during the COVID-19 pandemic. The study commenced on 21 March 2020 and involved online weekly (from August 2020, monthly) data collection across the pandemic in the UK. The study is not random and therefore is not representative of the UK population, but it does contain a heterogeneous sample. The sample was recruited using three primary approaches. First, convenience sampling was used, including promoting the study through existing networks and mailing lists (including large databases of adults who had previously consented to be involved in health research across the UK), print and digital media coverage and social media. Second, more targeted recruitment was undertaken focusing on (1) individuals from a low-income background, (2) individuals with no or few educational qualifications, and (3) individuals who were unemployed. Third, the study was promoted via partnerships with third sector organisations to vulnerable groups, including adults with pre-existing mental health conditions, older adults, carers and people experiencing domestic violence or abuse. The study protocol and user guide (which includes full details on recruitment, retention, data cleaning, weighting and sample demographics) are available at https://osfio/aswqc/.
A module on compliance behaviours was included in the survey between 17 November and 23 December 2020. For these analyses, we focused on individuals with complete observed compliance behaviours (n=21 066; 91.6% of individuals interviewed between these dates). We excluded participants with missing data on key demographic data that we used to construct survey weights (n=119), leaving a sample of 20 947. This sample represents 29.5% of those with data collection by 23 December 2020. We used entropy balance weighting to create survey weights to weight the data according to age group, gender, ethnicity, country of residence and educational level using UK population statistics (see study user guide for source data), truncating weights below the 1% percentile and above the 99% percentile to reduce the influence of extreme values.
The period from 17 November to 23 December 2020 overlaps with the second wave of COVID-19 in the UK in which there were several changes to COVID-19-related rules. The main UK government public health messages regarding COVID-19 during this period were Hands, Face, Space and Stay Alert, Control the Virus, Save Lives. Description of changes to COVID-19-related rules is provided in the online supplemental information. Online supplemental figure S1 shows 7-day COVID-19 case loads and confirmed deaths, along with the Oxford Policy Tracker, a numerical summary of policy stringency,16 across the study period.
jech-2021-216876supp001.pdf (564.1KB, pdf)
Measures
Compliance behaviours
We analysed six compliance behaviours: hand washing, face mask wearing, social distancing, household mixing indoors, household mixing outdoors and compliance with other guidelines. Participants were asked for their compliance with these behaviours over the previous 7 days (see online supplemental information for question precise wording). The response categories were: never, rarely, occasionally, frequently and always. Items on household mixing were phrased such that higher scores indicated lower compliance. We reverse coded these for consistency with the other behaviours.
Predictors of compliance behaviour
We assessed a range of demographic, socioeconomic and personality trait characteristics as predictors of compliance behaviour. We selected these predictors using previous results from the COVID-19 Social Study8 and considering the COM-B (capability, opportunity, motivation and behaviour) framework of health behaviour.17 The COM-B model posits that behaviour is determined by (subjective and objective) capability, social and physical opportunity for action and autonomic and reflective motivation.
For capability to comply, we included variables for external locus of control, neighbourhood crowding, annual household income, educational level and diagnosed psychiatric condition. For opportunity to comply, we included variables for country of residence (England/Wales/Northern Ireland (NI) vs Scotland) and lockdown tier (Lockdown, Tier 1, Tier 2, Tier 3, Wales, NI), household income, date of data collection (modelled with natural cubic splines with 2 df to capture non-linearities) and ethnicity. (Note the coding of country of residence and tier variable was to ensure non-collinearity in the two variables.) For motivation to comply, we include variables for long-term physical health conditions (0, 1, 2+), age (18–29, 30–45, 46–59, 60+), gender, keyworker status (employment in UK government identified ‘keyworker’ role (see online supplemental information for specific roles)), self-isolation during first data collection, Big Five personality traits (openness, conscientiousness, extraversion, agreeableness and neuroticism), trait empathy, risk taking, household overcrowding (1+ persons per room), living arrangement (alone, not alone without child, not alone with child), confidence in government and mental health experiences during the first lockdown (same, better or worse vis-à-vis prior to the pandemic). Many of these variables were measured at baseline data collection or in modules contained in the survey prior to measurement of compliance. More details on the measurement of the variables in this analysis are provided in the online supplemental information.
Statistical analysis
We estimated latent class models using robust maximum likelihood estimation with 2000 sets of random starting values, repeated for one to nine latent classes. Compliance variables were treated as ordered categorical variables in these models. We selected the final model considering the Bayesian information criterion (BIC) and entropy values, average latent class probabilities and substantive interpretation of the classes identified. We included survey weights in models and so were not able to use the bootstrapped likelihood ratio test for model selection.
After selecting a final latent class solution, we estimated a multinomial logistic regression model to predict compliance patterns according to demographic, socioeconomic and psychological factors using the three-step approach.18 All covariates were added to the model simultaneously. We used the three-step approach as this ensures that the latent class solution is unaltered by the inclusion of predictors in the model, while allowing for uncertainty in latent class membership to be propagated into the multinomial logistic regression results. Due to data missingness, we used multiple imputation in these models (40 imputed data sets, 10 iterations). Data were imputed using the mice R packages with continuous variables imputed using predictive mean matching and categorical variables imputed using multinomial logistic regression. Latent class probabilities were included as auxiliary variables in the imputation models.
We found that average compliance levels differed across the six compliance behaviours. Consequently, as a further analysis, we also estimated models of the predictors of individual compliance behaviours using ordinal regression. We again used multiple imputed data for these models, with separate imputations run for each compliance measure (40 data sets, 10 iterations). No auxiliary variables were included in these models.
In the regression results, we scaled continuous variables, such that a one-unit change is equivalent to 2 SD change in the variable to allow comparison with categorical variables.19 The code to replicate the analysis is available at https://osfio/aswqc/.
Role of the funding source
The funders had no final role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All researchers listed as authors are independent from the funders and all final decisions about the research were taken by the investigators and were unrestricted.
Results
Descriptive statistics
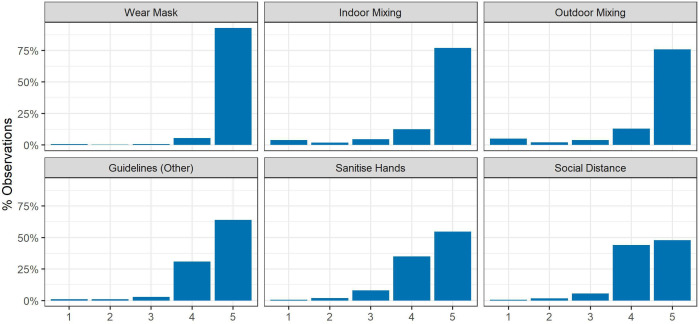
Sample descriptive statistics are shown in online supplemental table S1. The unweighted sample was disproportionately female, of older age, white and highly educated. The distributions of the individual compliance behaviours are displayed in figure 1. For each of the behaviours, the majority of participants reported frequent or complete compliance. Full compliance was greatest for mask wearing and indoor and outdoor social mixing. Lowest compliance levels were observed for hand washing and social distancing. Exploratory factor analysis of the six items identified two factors with eigenvalues greater than 1 (polychoric correlations; promax rotation). Items on mask wearing, other guidelines, hand washing and social distancing loaded onto one factor and the two items on household mixing loaded onto the other (for factor loadings, see online supplemental figure S2). The correlation between the factors was 0.41. Cronbach’s α was 0.61 for the six items.
Figure 1.
Distribution of compliance by behaviour. Response categories: 1. Never, 2. Rarely, 3. Occasionally, 4. Frequently, 5. Always. Items on household mixing were phrased with higher values indicating lower compliance, and so are reverse coded for consistency with the other items.
Patterns of compliance behaviour
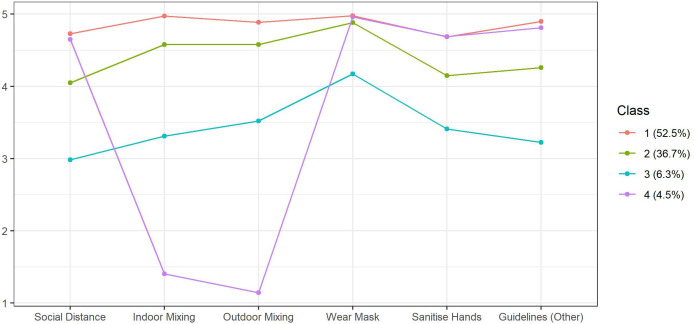
Fit statistics for the latent class analysis models are displayed in table 1. A BIC ‘elbow’ plot is provided in online supplemental figure S3. We selected a four-class solution as this had an entropy value above 0.8 and provided qualitatively different classes to the more restrictive three-class solution, while the less parsimonious five-class solution provided substantively similar results. Mean values for each behaviour according to class for the four-class solution are displayed in figure 2 (online supplemental file 1 alternatively displays this information as predicted probabilities). Sample sizes and latent class probabilities are displayed in table 2. Average class probabilities (the average predicted probability of an individual assigned to their most likely class actually belonging to that class) were over 0.81 in each case.
Table 1.
Latent class analysis fit statistics
| Classes | AIC | BIC | Entropy | Average class probability | |
| Min | Max | ||||
| 1 | 201 155 | 201 346 | 1.000 | 1.00 | |
| 2 | 184 808 | 185 198 | 0.75 | 0.900 | 0.94 |
| 3 | 179 920 | 180 508 | 0.84 | 0.870 | 0.97 |
| 4 | 176 180 | 176 967 | 0.82 | 0.811 | 0.95 |
| 5 | 174 645 | 175 631 | 0.77 | 0.770 | 0.95 |
| 6 | 173 956 | 175 141 | 0.79 | 0.767 | 0.97 |
| 7 | 173 317 | 174 700 | 0.80 | 0.678 | 0.97 |
| 8 | 172 981 | 174 563 | 0.81 | 0.678 | 0.97 |
| 9 | 172 653 | 174 433 | 0.79 | 0.608 | 0.97 |
AIC, Akaike information criterion; BIC, Bayesian information criterion.
Figure 2.
Average compliance levels by latent class.
Table 2.
Average latent class membership probability (column) by most likely latent class (row), and expected sample sizes by latent class
| Class | Average class probability | n (%) | |||
| 1 | 2 | 3 | 4 | ||
| 1 | 0.954 | 0.045 | 0.000 | 0.000 | 11 006.29 (52.54) |
| 2 | 0.161 | 0.824 | 0.014 | 0.001 | 7691.16 (36.72) |
| 3 | 0.006 | 0.169 | 0.811 | 0.014 | 1310.42 (6.26) |
| 4 | 0.032 | 0.014 | 0.013 | 0.941 | 939.13 (4.48) |
The majority of participants were predicted to be full compliers (class 1: 52.5%), reporting high compliance levels with each of the behaviours. A large minority of individuals (class 2: 36.7%) were frequent compliers, exhibiting frequent or complete compliance with each behaviour. Compared with full compliers, these individuals reported similar compliance with mask wearing and somewhat lower compliance with social distancing, hand sanitising and compliance with other guidelines. A small minority were occasional compliers (class 3: 6.3%), reporting occasional or frequent compliance with each behaviour. Again, these individuals reported highest compliance with mask wearing and lower compliance with social distancing and other behaviours. Full, frequent and occasional compliers displayed broadly consistent levels of compliance across behaviours, while the final group, household mixers (class 4: 4.5%), instead reported high compliance with each behaviour, except household mixing, for which they reported non-compliance. Note, however, that the items on household mixing were reverse coded, and so this pattern may be explained by participant inattention.
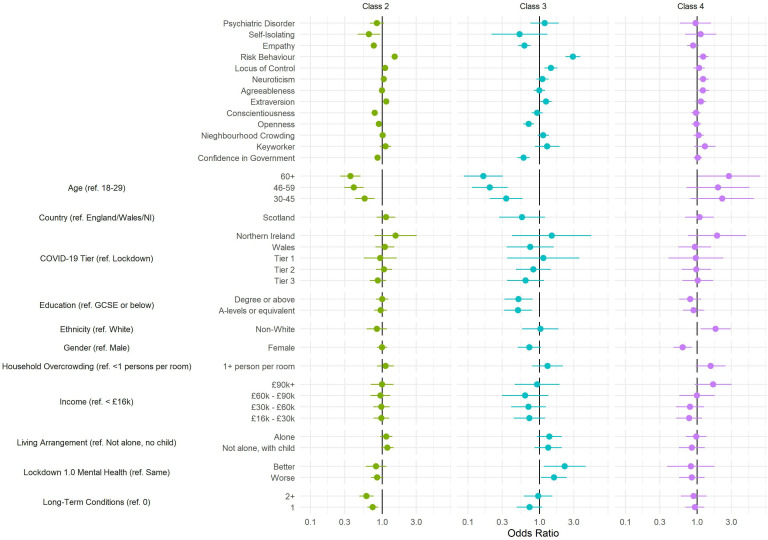
Predictors of compliance patterns
Descriptive statistics by most likely class are displayed in online supplemental table S2. The predictors of the compliance patterns drawn from the three-step multinomial regression model are displayed in figure 3 (see online supplemental file 1 for specific values). Compared with full compliers, there was clear evidence that frequent compliers (left panel) have lower confidence in government, lower empathy, and a greater external locus of control, are younger, more risk taking, have lower trait openness, are less conscientious and are less likely to have been self-isolating at first data collection or have a long-term condition. Of these factors, age (60+ vs 18–29: OR=0.36, 95% CI 0.26 to 0.5) and risk-taking behaviour (OR=1.5, 95% CI 1.37 to 1.64) were particularly strongly related to frequent compliance. Qualitatively similar results were observed comparing occasional compliers with full compliers, with the exception that there was also stronger evidence that individuals whose mental health did not stay the same during the first national lockdown were more likely to be occasional compliers, though both improved and worsened mental health were related to occasional compliance. Association between occasional compliance and age (60+ vs 18–29: OR=0.16, 95% CI 0.09 to 0.31) and risk-taking behaviour (OR=2.9, 95% CI 2.29 to 3.68) was also particularly strong. Few factors were clearly related to household mixing (exceptions were ethnicity, risk behaviour and gender), which again may suggest this category reflects inattentive responses.
Figure 3.
Results of multivariate multinomial regression model of latent class on participant characteristics. Reference class: class 1. Three-step regression procedure and use of multiple imputed data (40 data sets). Model includes mutual adjustment for all presented variables. GCSE, General Certificate of Secondary Education; NI, Northern Ireland.
Predictors of individual compliance behaviours
The results of ordinal regression models predicting individual compliance behaviours are displayed in online supplemental figure S5 (see online supplemental table S4 for specific values). Associations between compliance and individual characteristics were generally consistent across different compliance behaviours. Again, risk behaviour and age were strong predictors of compliance. There were some specificities in the findings, however. For instance, trait extraversion was most strongly related to lower compliance with indoor and outdoor household mixing guidelines (ORs=0.75 (0.69, 0.81) and 0.65 (0.61, 0.7), respectively).
Discussion
Using latent class analysis, we identified four groups of compliance behaviours. While some behaviours, such as face mask wearing, were performed more frequently overall, most individuals reported broadly consistent levels of compliance across the six behaviours. Further, high level of compliance across each behaviour was the modal response. A small minority of individuals reported low compliance levels on household mixing but not other measures, though this may be explained by inattentive responses. Behaviour patterns and compliance with individual behaviours were each related to individual characteristics. Most notably, there was evidence that high compliance was strongly related to older age and to lower risk-taking behaviour, consistent with previous research using the COVID-19 Social Study.8 Both of these represent motivations for compliance, and are consistent with a previous study applying the COM-B model to COVID-19 hygiene practices that identified motivation as the most important predictor of compliance behaviour.20 However, it should be noted that large differences have been observed between longitudinal and cross-sectional associations with individual characteristics and compliance.7
The results suggest that individuals choose to comply with all guidelines, rather than some but not others. This suggests that strategies to increase compliance should focus on increasing motivations to comply in general, for instance, through campaigns advertising the risks of non-compliance for personal, family and public health (of which the UK government’s Stay Home, Protect the NHS, Save Lives campaign is an example). This is supported by the results of several experimental studies that show intentions to practise preventive behaviours are higher following public health messaging that emphasises the risks of COVID-19 for one’s self and others.21–23
Reported compliance was high; a notable finding given that data were collected 8 months after the first lockdown in the UK and fears at the beginning of the pandemic that extended lockdown may induce ‘behavioural fatigue’24 (though, also see ref25–28). Compared with the other behaviours, compliance with social distancing was relatively low. This may reflect the issue that individuals’ capacity to socially distance is constrained by the behaviour of others and the environment (for instance, due to the layout of shops). Given the higher level of compliance with other measures, the results suggest that lower compliance with social distancing is not a matter of low willingness to comply, though it is also possible that non-compliance with social distancing is opportunistic, for instance, when meeting friends. Compliance with mask wearing was particularly high, frequently being carried out even among the low compliance group. This may reflect that mask wearing is legally mandated, typically involves little personal sacrifice, is easily observed by others (there is evidence that shame and guilt motivate compliance29) and that clearer cues to action exist in the environment than for other compliance behaviours.30
We observed some differences with our prior work using data from the COVID-19 Social Study.8 Notably, we did not observe evidence that low compliance was related to higher income or higher education. However, the measure of compliance (single item on compliance with guidelines overall) differed from the present study and may incorporate knowledge of guidelines to a greater extent. Further, the present study used data from the second wave, in which (compared with mid-summer) overall compliance increased.2
This study had a number of strengths. Unlike several previous studies, we used a large sample and focused on reported compliance behaviour, rather than compliance intentions or a general measure of compliance. The measures we included reflected several important behaviours for reducing transmission of COVID-19.1 We also studied compliance further into the pandemic than has been explored to date. We were able to assess a rich set of compliance predictors, though the associations we tested were cross-sectional—previous research shows large differences in between-person and within-person correlations.7 The latent class analysis provided a good solution and revealed important insights into compliance behaviour.
However, this study also had several limitations. As noted, we used cross-sectional data, so results may be biased by unobserved confounding. Our measures of compliance also relied on self-report data. While participants provided anonymous responses, responses may still be subject to social desirability concerns. Further, though the pandemic is a salient event, the opportunities for non-compliance are many. Individuals may not recall compliance accurately. Guidelines also changed over the study period, which may have influenced responses. Last, we used data from a non-representative (although heterogeneous and weighted) sample with substantial attrition rates. High compliers with COVID-19 are likely to be over-represented in the data, though high levels of compliance have been found in other samples.2
Overall, our results suggest that while compliance with some behaviours is higher in general, individuals comply consistently across recommended compliance behaviours. In line with previous studies,8 20 this suggests that motivation is a particularly important determinant of compliance behaviour. Interventions that increase or maintain motivation to comply may be particularly effective at reducing transmission of COVID-19.
What is already known on this subject.
A sizeable literature has looked at the predictors of compliance with individual COVID-19 preventive behaviours, such as social distancing or wearing of face masks. Less is known about how these behaviours cluster within individuals.
What this study adds.
We find evidence that individuals typically display consistent levels of compliance across different preventive behaviours, though average compliance with social distancing was lower than for other behaviours.
The results suggest that efforts to increase compliance should focus on increasing motivation to comply in general.
Acknowledgments
The researchers are grateful for the support of a number of organisations with their recruitment efforts including: the UKRI Mental Health Networks, Find Out Now, UCL BioResource, HealthWise Wales, SEO Works, FieldworkHub and Optimal Workshop.
Footnotes
Correction notice: This article has been corrected since it first published online. On page 4 the sentence '…frequent compliers (left panel) have…a greater internal locus of control.’ has been corrected to ’…frequent compliers (left panel) have…a greater external locus of control’ and on page 2 the sentence 'For capability to comply, we included variables for locus…' has been corrected to 'For capability to comply, we included variables for external locus…' Minor errors have also been corrected in the Supplementary material.
Contributors: LW, AS and DF conceived and designed the study. LW analysed the data and wrote the first draft. All authors provided critical revisions. All authors read and approved the submitted manuscript.
Funding: This COVID-19 Social Study was funded by the Nuffield Foundation (WEL/FR-000022583). The study was also supported by the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by the UK Research and Innovation (ES/S002588/1) and by the Wellcome Trust (221400/Z/20/Z). DF was funded by the Wellcome Trust (205407/Z/16/Z). LW was funded by the Economic and Social Research Council through the UCL, Bloomsbury and East London Doctoral Training Partnership (ES/P000592/1). The study was also supported by HealthWise Wales, the Health and Car Research Wales initiative, which is led by Cardiff University in collaboration with SAIL, Swansea University.
Disclaimer: The views expressed are those of the authors and not necessarily the Nuffield Foundation. The funders had no final role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All researchers listed as authors are independent of the funders and all final decisions about the research were taken by the investigators and were unrestricted.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the UCL Research Ethics Committee (12467/005) and all participants gave informed consent.
References
- 1. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020;395:1973–87. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ipsos MORI . Most Britons continue to say they are following coronavirus rules; almost half believe lockdown measures are not strict enough, 2021. Available: https://www.ipsos.com/ipsos-mori/en-uk/most-britons-continue-say-they-are-following-coronavirus-rules-almost-half-believe-lockdown [Accessed 25 Feb 2021].
- 3. YouGov . Personal measures taken to avoid COVID-19, 2021. Available: https://yougov.co.uk/topics/international/articles-reports/2020/03/17/personal-measures-taken-avoid-covid-19 [Accessed 21 Sep 2020].
- 4. Perra N. Non-pharmaceutical interventions during the COVID-19 pandemic: a review. Phys Rep 2021:S0370157321000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol 2010;15:797–824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bargain O, Aminjonov U. Trust and compliance to public health policies in times of COVID-19. J Public Econ 2020;192:104316. 10.1016/j.jpubeco.2020.104316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wright L, Steptoe A, Fancourt D. Predictors of self-reported adherence to COVID-19 guidelines. A longitudinal observational study of 51,600 UK adults. Lancet Reg Health Eur 2021;4:100061. 10.1016/j.lanepe.2021.100061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wright L, Fancourt D. Do predictors of adherence to pandemic guidelines change over time? A panel study of 22,000 UK adults during the COVID-19 pandemic. Prev Med 2021;153:106713. 10.1016/j.ypmed.2021.106713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brouard S, Vasilopoulos P, Becher M. Sociodemographic and psychological correlates of compliance with the COVID-19 public health measures in France. Can J Polit Sci 2020:1–6. 10.1017/S0008423920000335 [DOI] [Google Scholar]
- 10. Kamenidou IE, Stavrianea A, Liava C. Achieving a Covid-19 free country: citizens preventive measures and communication pathways. Int J Environ Res Public Health 2020;17:4633. 10.3390/ijerph17134633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tomczyk S, Rahn M, Schmidt S. Social distancing and stigma: association between compliance with behavioral recommendations, risk perception, and Stigmatizing attitudes during the COVID-19 outbreak. Front Psychol 2020;11:11. 10.3389/fpsyg.2020.01821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Toussaint LL, Cheadle AD, Fox J, et al. Clean and contain: initial development of a measure of infection prevention behaviors during the COVID-19 pandemic. Ann Behav Med 2020;54:619–25. 10.1093/abm/kaaa064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liao Q, Cowling BJ, Wu P, et al. Population Behavior Patterns in Response to the Risk of Influenza A(H7N9) in Hong Kong, December 2013-February 2014. Int J Behav Med 2015;22:672–82. 10.1007/s12529-015-9465-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Breakwell GM, Fino E, Jaspal R. The COVID-19 preventive behaviors index: development and validation in two samples from the United Kingdom. Eval Health Prof 2021;44:77-86. 10.1177/0163278720983416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. van der Weerd W, Timmermans DR, Beaujean DJ, et al. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health 2011;11:575. 10.1186/1471-2458-11-575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.et alHale T, Angrist N, Cameron-Blake E. Oxford COVID-19 Government Response Tracker. Oxford: : Blavatnik School of Government, 2020. Available: https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker [Accessed 22 Oct 2020].
- 17. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Asparouhov T, Muthén B. Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using M plus. Struct Equ Model Multidiscip J 2014;21:329–41. 10.1080/10705511.2014.915181 [DOI] [Google Scholar]
- 19. Gelman A. Scaling regression inputs by dividing by two standard deviations. Stat Med 2008;27:2865–73. 10.1002/sim.3107 [DOI] [PubMed] [Google Scholar]
- 20. Gibson Miller J, Hartman TK, Levita L, et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br J Health Psychol 2020;25:856–64. 10.1111/bjhp.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Capraro V, Barcelo H. The effect of messaging and gender on intentions to wear a face covering to slow down COVID-19 transmission. J Behav Econ Policy 2020;4:45–55. 10.31234/osf.io/tg7vz [DOI] [Google Scholar]
- 22. Lunn PD, Timmons S, Belton CA, et al. Motivating social distancing during the COVID-19 pandemic: an online experiment. Soc Sci Med 2020;265:113478. 10.1016/j.socscimed.2020.113478 [DOI] [PubMed] [Google Scholar]
- 23. Jordan J, Yoeli E, Rand DG. Don’t get it or don’t spread it: Comparing self-interested versus prosocial motivations for COVID-19 prevention behaviors. PsyArXiv 2020. 10.31234/osf.io/yuq7x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harvey N. Behavioral fatigue: real phenomenon, naïve construct, or policy Contrivance? Front Psychol 2020;11:589892. 10.3389/fpsyg.2020.589892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Petherick A, Goldszmidt R, Andrade EB, et al. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat Hum Behav 2021. 10.1038/s41562-021-01181-x. [Epub ahead of print: 03 Aug 2021]. [DOI] [PubMed] [Google Scholar]
- 26. Wright L, Steptoe A, Fancourt D. Trajectories of compliance with COVID-19 related guidelines: longitudinal analyses of 50,000 UK adults. Public and Global Health 2021. 10.1101/2021.04.13.21255336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shearston JA, Martinez ME, Nunez Y, et al. Social-distancing fatigue: evidence from real-time Crowd-sourced traffic data. medRxiv 2021. s 10.1101/2021.03.04.21252917. [Epub ahead of print: 08 Mar 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Martinez-Garcia M, Rabasa A, Barber X. Yet another lockdown? A large-scale study on people’s unwillingness to be confined during the first 5 months of the COVID-19 pandemic in Spain. Public and Global Health 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nivette A, Ribeaud D, Murray A, et al. Non-Compliance with COVID-19-related public health measures among young adults in Switzerland: insights from a longitudinal cohort study. Soc Sci Med 2021;268:113370. 10.1016/j.socscimed.2020.113370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. West R, Michie S, Rubin GJ, et al. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Hum Behav 2020;4:451–9. 10.1038/s41562-020-0887-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2021-216876supp001.pdf (564.1KB, pdf)
Data Availability Statement
No data are available.