Abstract
Objective:
Military veterans with posttraumatic stress disorder (PTSD) exhibit heightened rates of deliberate self-harm; yet, few studies have explored underlying mechanisms. Addressing this critical gap in the literature, the present study examined the roles of negative and positive emotion dysregulation in the relation between PTSD severity and deliberate self-harm.
Method:
Data were collected from 465 trauma-exposed military veterans in the community (Mage= 38.00, 71.4% male, 69.5% white) who responded to an online survey.
Results:
Findings indicated that PTSD severity was indirectly related to deliberate self-harm through overall positive (but not negative) emotion dysregulation. Secondary analyses indicated an underlying role of the negative emotion dysregulation domains of difficulties controlling impulsive behaviors when experiencing negative emotions and lack of emotional clarity and the positive emotion dysregulation domains of nonacceptance of positive emotions, difficulties engaging in goal-directed behavior when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions in the association between PTSD severity and deliberate self-harm.
Conclusions:
This study offers preliminary evidence for specific domains of negative and positive emotion dysregulation as possible pathways linking PTSD severity and deliberate self-harm. Findings highlight new avenues for research and treatment focused on the effects of emotion dysregulation on deliberate self-harm among trauma-exposed military veterans.
Keywords: posttraumatic stress disorder, PTSD, deliberate self-harm, negative emotion dysregulation, positive emotion dysregulation
1. Introduction
Deliberate self-harm is the intentional, direct destruction of one’s own body tissue without suicidal intent and for reasons not socially sanctioned (Gratz, 2001). Deliberate self-harm is a substantial health concern associated with higher rates of psychiatric disorders (Haw, Hawton, Houston, & Townsend, 2001). While previous work in this area has focused on deliberate self-harm in the context of borderline personality disorder (e.g., Favazza, 1998), a growing body of research links deliberate self-harm with posttraumatic stress disorder (PTSD; Gratz, & Tull, 2012; Forbes, et al., 2019; Ford & Gómez, 2015). For example, deliberate self-harm is common among United States military veterans with PTSD, with more than half of PTSD treatment-seeking veterans reporting deliberate self-harm (Calhoun et al., 2017; Kimbrel et al., 2016). Thus, there is a need for further research examining the relationship between PTSD symptoms and deliberate self-harm, particularly among veterans.
Emerging research provides strong evidence for the effect of PTSD symptoms on engagement in deliberate self-harm (for a review, see Smith, Kouros, & Meuret, 2014); however, little is known about the underlying mechanisms. One key factor worth exploring in this regard is emotion dysregulation. Gratz and Roemer (2004) broadly define emotion dysregulation as a multidimensional construct involving deficits in the awareness, understanding, and acceptance of emotions; impulse control problems and difficulties pursuing goal-directed behavior when experiencing emotions; and lack of access to effective strategies to modulate emotions. It is well-established in the literature that individuals with greater PTSD symptom severity exhibit elevated emotion dysregulation (e.g., Tull, Barrett, McMillan, & Roemer, 2007; Weiss, Tull, Anestis, & Gratz, 2013), including among veterans (Sippel, Roy, Southwick, & Fichtenholtz, 2016). Moreover, emotion dysregulation has been found to underlie the relationship between PTSD symptoms and various risky or impulsive behaviors, inclusive of deliberate self-harm (Weiss, Tull, Viana, Anestis, & Gratz, 2012). Trauma-exposed individuals with heightened emotion dysregulation may be less equipped to cope with the distress associated with PTSD symptomology and related distress and might then turn to deliberate self-harm as a method of coping (Smith, Kouros, & Meuret, 2014). Therefore, deliberate self-harm may function to down-regulate or avoid negative trauma-related emotions in the short-term. Indeed, prior studies have established emotion dysregulation as a robust risk factor for deliberate self-harm among diverse clinical and non-clinical samples (for a review, see You et al., 2018). In particular, veterans with PTSD have been found to use more maladaptive strategies (e.g., suppression) to regulate emotions compared to veterans without PTSD (Sippel et al., 2016); this could put these military veterans with PTSD at risk of turning to deliberate-self harm as a means to cope with trauma-related emotions. Taken together, research suggests that emotion dysregulation may be an important factor explicating deliberate self-harm among veterans with PTSD.
Importantly, extant research has been limited by an overwhelming focus on negative emotion dysregulation in the context of both PTSD and deliberate self-harm. Yet, recent studies have found that individuals with heightened PTSD symptoms experience exacerbated emotion dysregulation extending to positive emotions (Weiss, Contractor, Forkus, Goncharenko, & Raudales, in press; Weiss, Contractor, Raudales, Greene, & Short, in press; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018; Weiss, Nelson, Contractor, & Sullivan, in press). Moreover, positive emotion dysregulation has been shown to be linked to a wide range of risky or impulsive behaviors (e.g., substance misuse, risky sexual behavior; Weiss, Forkus, Contractor, Darosh, Goncharenko, & Dixon-Gordon, 2019; Weiss, Forkus, Contractor, & Schick, 2018), including in the context of PTSD (Weiss, Forkus, Raudales, Schick, & Contractor, in press; Weiss, Schick, Contractor, & Dixon-Gordon, 2019). In line with negative affect interference (Frewen, Dean, & Lanius, 2012), among individuals with PTSD, positive emotions may be negatively evaluated due to the heightened levels of physiological arousal (Litz, Orsillo, Kaloupek, & Weathers, 2000) or maladaptive cognitions (Norman, Wilkins, Myers, & Allard, 2014) they elicit that overlap with trauma symptomology (American Psychiatric Association, 2013). This, in turn, may lead individuals to use deliberate self-harm as a means to dampen or avoid positive emotions. Non-acceptance of positive emotions also may elicit secondary negative emotions (e.g., guilt, shame) that increase the likelihood of deliberate self-harm (Muehlenkamp & Kerr, 2010). Alternatively, positive emotion dysregulation may cause individuals to be more susceptible to behavioral dyscontrol in the context of elevated positive emotional experiences, such as by elevated distractibility (Dreisbach & Goschke, 2004) or impaired decision-making (Slovic, Finucane, Peters, & MacGregor, 2004). Indeed, a tendency to engage in rash action in the context of intense positive emotions has been found to be associated with deliberate self-harm and to underlie the relation of PTSD symptom severity to various risky or impulsive behaviors, inclusive of deliberate self-harm (Weiss, Tull, Sullivan, Dixon-Gordon, & Gratz, 2015). Thus, additional research is needed to investigate the role of positive emotion dysregulation in the association between PTSD symptoms and deliberate self-harm.
Despite research highlighting the role of emotion dysregulation in PTSD and deliberate self-harm, separately, no studies to our knowledge have tested the role of emotion dysregulation underlying the link between PTSD and deliberate self-harm. Previous work is also limited by the exclusion of examinations of positive emotion dysregulation. To address this gap in the literature, the current study examined the underlying roles of negative and positive emotion dysregulation in the association between PTSD and deliberate self-harm among trauma-exposed military veterans. Examination of these variables among military veterans may be important considering the high rates of PTSD and deliberate self-harm in this population (Calhoun et al., 2017). We hypothesized that PTSD severity will be indirectly related to engagement in deliberate self-harm through both negative and positive emotion dysregulation.
2. Methods
2.1. Procedure/Participants
Participants were recruited from Amazon’s Mechanical Turk (MTurk), an internet-based crowdsourcing platform that generates reliable data (Buhrmester, Kwang, & Gosling, 2011; Shapiro, Chandler, & Mueller, 2013), and represents the general population in terms of demographics (Mischra & Carleton, 2017) and prevalence of mental health problems (Shapiro et al., 2013), including PTSD (van Stolk-Cooke et al., 2018). To optimize data quality, validity checks in the survey assessed for attentive responding and comprehension (n = 4; e.g., “I have never brushed my teeth;” Aust, Diedenhofen, Ullrich, & Musch, 2013; Meade & Craig, 2012; Thomas & Clifford, 2017), and military-specific knowledge (n = 2; e.g., “What is the acronym for the locations where final physicals are taken prior to shipping off for basic training?;” Lynn & Morgan, 2016). Participants who failed any of the six validity checks were excluded.
Inclusionary criteria for the present study were living in North America, at least 18 years of age, having working knowledge of the English language, and being a veteran of the United States military. Eligible participants provided informed consent, completed the survey on Qualtrics (data collection platform), and were compensated $2.50 for study participation. All procedures were approved by the university Institutional Review Board.
2.2. Exclusions and Missing Data
Of the obtained 2,644 responses, 997 participants were excluded for not meeting at least one inclusionary criterion (remainder n = 1,647). We then excluded 899 participants who failed any of four validity checks (remainder n = 748), 134 participants who failed to pass any of the military-specific validity questions (remainder n = 614), and 79 participants who attempted to answer the questionnaire more than once (remainder n = 535). For the current study, an additional 70 participants were excluded for not endorsing a trauma on the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013). The final sample included 465 participants. Participants ranged in age from 18 to 76 (M = 38.00, SD = 11.45), and were mostly male (71.4%) and white (69.5%). Additional demographics are provided in Table 1.
Table 1.
Descriptive Characteristics of the Sample
| Full Sample (n = 465) | |
|---|---|
|
| |
| Variables | Mean (SD) |
| Age | 38.00 (11.45) |
|
| |
| n (%) | |
|
| |
| Gender | |
| Female | 131 (28.2%) |
| Male | 332 (71.4%) |
| Other | 1 (0.2%) |
| Race (could endorse more than one category) | |
| White | 323 (69.5%) |
| African American/Black | 108 (23.2%) |
| Asian | 26 (5.6%) |
| American Indian/Alaska Native | 19 (4.1%) |
| Native Hawaiian/Other Pacific Islander | 5 (1.1%) |
| Not Listed | 4 (0.9%) |
| Ethnicity | |
| Hispanic or Latino/a | 112 (24.1%) |
| Not Hispanic or Latino/a | 344 (74.0%) |
| Employment Status | |
| Employed Part-time | 40 (8.6%) |
| Employed Full-time | 394 (84.7%) |
| Not in Labor Force (student, homemaker) | 14 (3.0%) |
| Unemployed | 12 (2.6%) |
| Family Annual Income | |
| < $15,000 | 224 (47.3) |
| $15,000 - $24,999 | 18 (3.7) |
| $25,000 - $34,999 | 23 (4.9%) |
| $35,000 - $49,999 | 51 (6.1%) |
| $50,000 - $64,999 | 67 (14.3%) |
| $65,000 - $79,999 | 27 (5.6%) |
| $80,000 or higher | 55 (11.4%) |
| Branch of Service | |
| Army | 301 (64.7%) |
| Navy | 44 (9.5%) |
| Air Force | 85 (18.3%) |
| Marines | 29 (6.2%) |
| Coast Guard | 6 (1.3%) |
| Number of deployments | |
| None | 98 (21.1 %) |
| One | 127 (27.3%) |
| Two | 105 (22.6%) |
| Three or more | 135 (29.0%) |
| Involved in Combat Operations | |
| Yes | 231 (49.7%) |
| No | 100 (21.7%) |
2.3. Measures
Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013).
The LEC-5 is a 17-item self-report measure of lifetime trauma. Participants indicate their exposure to each event on a 6-point scale: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. Trauma exposure – consistent with the DSM-5 Criterion A – was based on the endorsement of any of the first four response options (American Psychiatric Association [APA], 2013). Further, participants indicate which traumatic event was the most distressing. The LEC has demonstrated strong convergent validity with measures assessing traumatic exposure and psychopathology known to relate to traumatic exposure (Gray, Litz, Hsu, & Lombardo, 2004). Table 2 details the prevalence rates of index traumatic events.
Table 2.
List of Index Traumas from the Life Events Checklist for the DSM-5
| Potentially Traumatic Events | n (%) |
|---|---|
| Sudden accidental death | 67 (14.4%) |
| Assault with a weapon (e.g., being shot, stabbed, threatened with a knife, gun, bomb) | 49 (10.5%) |
| Transportation accident (e.g., car accident, boat accident, train wreck, plane crash) | 47 (10.1%) |
| Life-threatening illness or injury | 46 (9.9%) |
| Physical assault (e.g., being attacked, hit, slapped, kicked, beaten up) | 38 (8.2%) |
| Natural disaster (e.g., flood, hurricane, tornado, earthquake) | 32 (6.9%) |
| Captivity (e.g., being kidnapped, abducted, held hostage, prisoner of war) | 30 (6.5%) |
| Other unwanted or uncomfortable sexual experience | 29 (6.3%) |
| Serious injury, harm, or death you caused to someone else | 21 (4.5%) |
| Exposure to toxic substance (e.g., dangerous chemicals, radiation) | 18 (3.9%) |
| Serious accident at work, home, or during recreational activity | 17 (3.7%) |
| Sexual assault (e.g., rape, attempted rape, made to perform any type of sexual act through force or threat of harm) | 13 (2.8%) |
| Any other very stressful event or experience | 11 (2.4%) |
| Fire or explosion | 8 (1.7%) |
| Combat or exposure to a war-zone (i.e., in the military or as a civilian) | 3 (0.6%) |
| Severe human suffering | 2 (0.4%) |
| Sudden violent death (e.g., homicide, suicide) | 1 (0.2%) |
PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013).
The PCL-5 is a 20-item self-report measure of symptoms corresponding to the DSM-5 criteria for PTSD (APA, 2013). Participants complete the PCL-5 in response to the most distressing traumatic event endorsed on the LEC-5. Participants indicate how often they have been bothered by each of the symptoms over the past month using a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). A total score was calculated by summing all the items, with higher scores indicating greater PTSD symptom severity. The PCL-5 has excellent psychometric properties (Blevins et al., 2015; Bovin et al., 2016; Wortmann et al., 2016). The PCL-5 demonstrated excellent reliability in the current sample (α = .98).
Difficulties in Emotion Regulation Scale – 16 (DERS-16; Gratz & Roemer, 2004).
The DERS-16 is a 16-item self-report measure of difficulties regulating negative emotions across five domains: nonacceptance of negative emotions, difficulties engaging in goal-directed behavior when distressed, difficulties controlling impulsive behaviors when distressed, limited access to effective emotion regulation strategies for negative emotions, and lack of emotional clarity. Participants rate the extent to which items apply to them using a 5-point Likert-type scale ranging from 1 (almost never) to 5 (almost always). A total score was calculated by summing all the items, with higher scores indicating greater negative emotion dysregulation. The DERS-16 has sound psychometric properties, demonstrating good test-retest reliability, convergent validity, and discriminant validity (Bjureberg et al., 2016). In the present study, reliability for the DERS was good to excellent for the total score (α = .97) and nonacceptance (α = .86), goals (α = .88), impulsivity (α = .91), strategies (α = .91), and clarity (α = .88) subscales.
Difficulties in Emotion Regulation Scale – Positive (DERS-P; Weiss, Gratz, et al., 2015).
The DERS-P is a 13-item self-report measure of difficulties regulating positive emotions across three domains: nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions. Participants rate each item using a 5-point Likert-type scale ranging from 1 (almost never) to 5 (almost always). A total score was computed by summing all items, with higher scores indicating greater positive emotion dysregulation. The DERS-P demonstrates excellent psychometric properties (Weiss, Gratz, et al., 2015), including in the current study for the total score (α = .98) and nonacceptance (α = .95), goals (α = .91), impulsivity (α = .95) subscales.
Deliberate Self-Harm Inventory (DSHI; Gratz, 2001).
The DSHI is a 17-item self-report measure of various aspects of deliberate self-harm, including frequency, onset, and last episode. Participants indicate whether or not they have intentionally engaged in specific behaviors (e.g., “Have you ever intentionally [i.e., on purpose] cut your wrist, arms, or other area[s] of your body without intending to kill yourself?). Items indicating presence of behaviors are summed, with higher scores indicating greater deliberate self-harm. The DSHI has previously shown adequate test-retest reliability and construct, discriminant, and convergent validity among diverse samples (Fliege et al., 2006; Gratz, 2001). Reliability for the DSHI in the present study was good (α = .86).
2.4. Data Analytic Plan
Data were first assessed for violations to assumptions of normality. Next, intercorrelations were examined among primary study variables. To address the questions of whether overall negative and positive emotion dysregulation, separately, explain the relation between PTSD and deliberate self-harm, we conducted indirect effect analyses (Preacher & Hayes, 2004) with the PROCESS SPSS macro (Model 4; Hayes, 2012). Furthermore, as supplemental analyses, we conducted indirect effect analyses to examine specific negative and positive emotion dysregulation subscales. Lastly, to confirm the direction of the indirect effect, we tested the models when switching the intermediate and outcome variables. The PROCESS procedures use ordinary least squares regression and bootstrapping methodology, which confers more statistical power than do standard approaches to statistical inference and does not rely on distributional assumptions. Bootstrapping was done with 5,000 random samples generated from the observed covariance matrix to estimate bias-corrected 95% confidence intervals (CIs) and significance values (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Preacher & Hayes, 2004). The effect is significant if the 95% confidence interval does not contain zero (Preacher & Hayes, 2004). Indirect effects are reported as standardized.
3. Results
3.1. Preliminary Analyses
Almost half of participants (n = 195; 41.94%) reported a history of deliberate self-harm, with scores on the DSHI among these participants ranging from 1 to 17 (M = 5.79, SD = 4.08). Scores on the DSHI were found to be positively skewed (skewness = 1.62); therefore, a logarithmic transformation was computed and utilized for all subsequent analyses. Other variables were within the acceptable ranges for skewness (range = 0.14 to 0.86) and kurtosis (range = −1.28 to −0.72). Descriptive information and intercorrelations among variables are presented in Table 3. Significant positive associations were identified among PTSD, negative emotion dysregulation, positive emotion dysregulation, and deliberate self-harm.
Table 3.
Descriptive statistics and zero-order correlations for variables of interest
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PCL-5 | 29.62 | 23.32 | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ |
| 2. DERS-16 | 40.80 | 16.61 | .68** | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ |
| 3. DERS-16 Clarity | 5.87 | 2.36 | .62** | .85** | __ | __ | __ | __ | __ | __ | __ | __ | __ | __ |
| 4. DERS-16 Goals | 9.46 | 3.31 | .56** | .84** | .64** | __ | __ | __ | __ | __ | __ | __ | __ | __ |
| 5. DERS-16 Impulse | 8.58 | 3.75 | .59** | .88** | .74** | .67** | __ | __ | __ | __ | __ | __ | __ | __ |
| 6. DERS-16 Strategy | 15.32 | 5.21 | .66** | .95** | .78** | .75** | .79** | __ | __ | __ | __ | __ | __ | __ |
| 7. DERS-16 Accept | 9.16 | 3.49 | .57** | .87** | .70** | .65** | .68** | .79** | __ | __ | __ | __ | __ | __ |
| 8. DERS-P | 26.04 | 14.62 | .58** | .70** | .71** | .46** | .69** | .66** | .58** | __ | __ | __ | __ | __ |
| 9. DERS-P Accept | 10.13 | 5.25 | .57** | .67** | .67** | .42** | .66** | .64** | .55** | .95** | __ | __ | __ | __ |
| 10. DERS-P Goals | 10.10 | 4.87 | .53** | .67** | .70** | .45** | .64** | .62** | .56** | .93** | .82** | __ | __ | __ |
| 11. DERS-P Impulse | 12.49 | 6.68 | .55** | .66** | .66** | .45** | .65** | .62** | .54** | .96** | .88** | .85** | __ | __ |
| 12. DSHI | 2.46 | 3.91 | .58** | .44** | .44** | .33** | .42** | .42** | .35** | .51** | .49** | .46** | .50* | __ |
Note. PCL-5 = PTSD Checklist for DSM-5; DERS-16 = Difficulties in Emotion Regulation Scale – 16, subscales for nonacceptance of negative emotions, difficulties engaging in goal-directed behavior when distressed, difficulties controlling impulsive behaviors when distressed, limited access to effective emotion regulation strategies for negative emotions, and lack of emotional clarity; DERS-P = Difficulties in Emotion Regulation Scale – Positive, subscales for nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, difficulties controlling impulsive behaviors when experiencing positive emotions; DSHI = Deliberate Self-Harm Inventory. Non-transformed DSHI scores are presented for descriptive data only.
p < .001.
3.2. Primary Analyses
We examined two models explicating the roles of negative and positive emotion dysregulation, separately, in the relation between PTSD and deliberate self-harm. Models for total negative and positive emotion dysregulation are shown in Figures 1 and 2, respectively. In the first model examining negative emotion dysregulation, the association between PTSD and negative emotion dysregulation was found to be significant (B = 0.48, SE = 0.02, t = 19.65, p < .001). However, the association between negative emotion dysregulation and deliberate self-harm was not significant (B = 0.002, SE = 0.001, t = 1.83, p = .07). Furthermore, the indirect effect of PTSD on deliberate self-harm through negative emotion dysregulation was not significant (β = 0.06, SE = 0.04, 95% CI [−0.01, 0.15]). The direct effect linking PTSD and deliberate self-harm when accounting for negative emotion dysregulation was significant (B = 0.01, SE = 0.001, t = 9.96, p < .001). When examining the negative emotion dysregulation subscales, however, significant indirect effects were found for difficulties controlling impulsive behaviors when distressed (β = 0.07, SE = 0.03, 95% CI [0.01, 0.14]) and lack of emotional clarity (β = 0.09, SE = 0.03, 95% CI [0.02, 0.16]), but not for nonacceptance of negative emotions (β = 0.02, SE = 0.03, 95% CI [−0.03, 0.08]), difficulties engaging in goal-directed behavior when distressed (β = 0.004, SE = 0.03, 95% CI [−0.05, 0.05]), or limited access to effective emotion regulation strategies for negative emotions (β = 0.05, SE = 0.03, 95% CI [−0.02, 0.12]).
Figure 1.
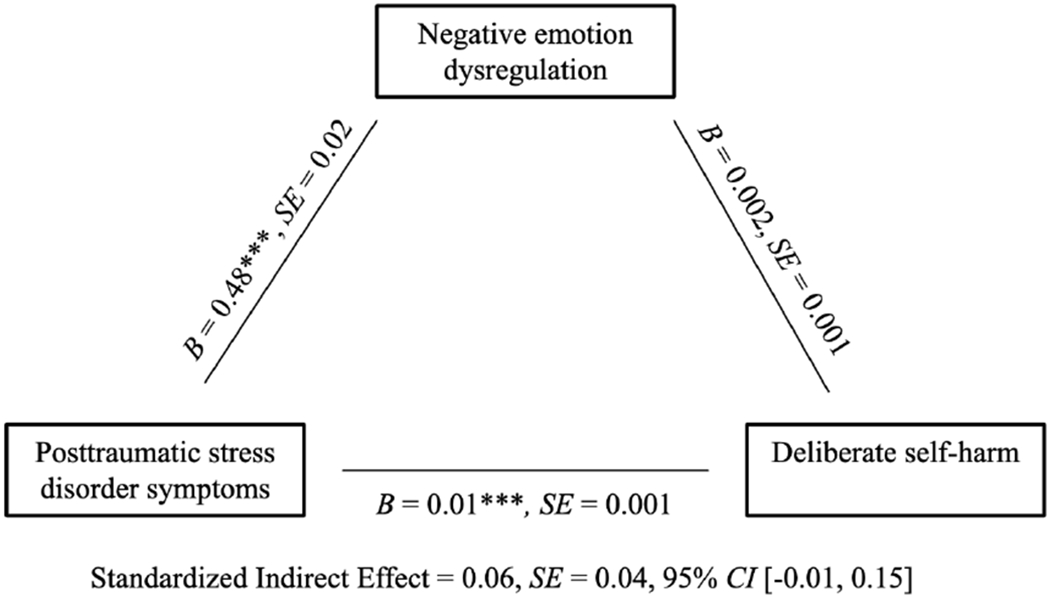
The underlying effects of negative emotion dysregulation in the association between posttraumatic stress disorder symptoms and deliberate self-harm. *** p < .001
Figure 2.
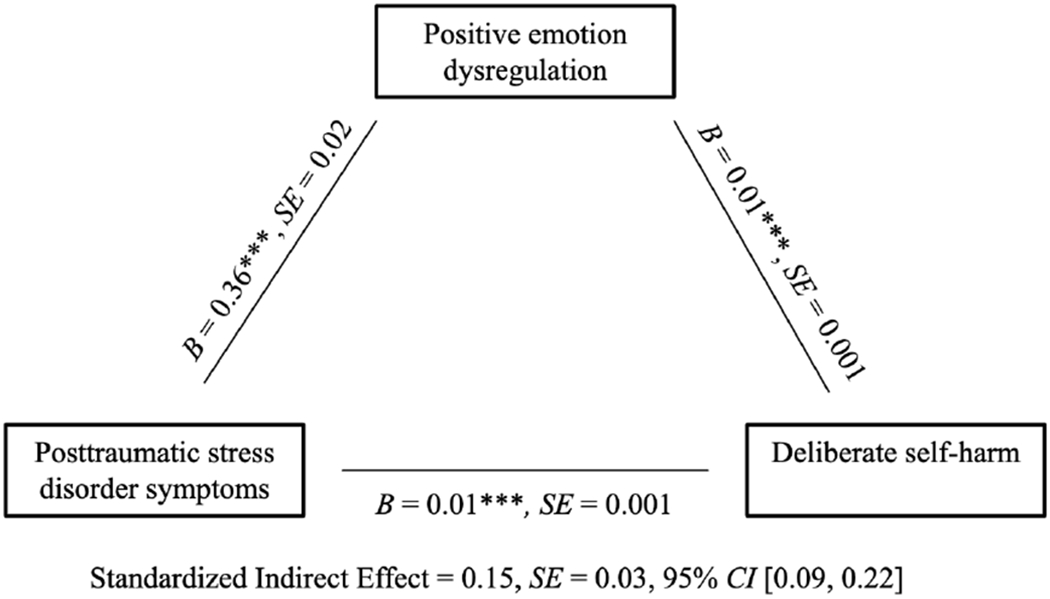
The underlying effects of positive emotion dysregulation in the association between posttraumatic stress disorder symptoms and deliberate self-harm. *** p < .001
Of note, these results do not differ when including age and gender as covariates. Specifically, the indirect effect of PTSD on deliberate self-harm through negative emotion dysregulation remained non-significant (β = 0.05, SE = 0.04, 95% CI [−0.04, 0.13]). Significant indirect effects were maintained for difficulties controlling impulsive behaviors when distressed (β = 0.07, SE = 0.04, 95% CI [0.003, 0.14]) and lack of emotional clarity (β = 0.08, SE = 0.04, 95% CI [0.002, 0.15]), but not for nonacceptance of negative emotions (β = 0.01, SE = 0.03, 95% CI [−0.05, 0.07]), difficulties engaging in goal-directed behavior when distressed (β = −0.01, SE = 0.03, 95% CI [−0.07, 0.04]), or limited access to effective emotion regulation strategies for negative emotions (β = 0.03, SE = 0.04, 95% CI [−0.04, 0.10]).
In alternate models that switched the intermediate and outcome variables, deliberate self-harm did not significantly account for the relationship between PTSD and negative emotion dysregulation (β = 0.03, SE = 0.03, 95% CI [−0.02, 0.08]). Moreover, deliberate self-harm significantly underlied the relationship between PTSD and difficulties controlling impulsive behaviors when distressed (β = 0.06, SE = 0.03, 95% CI [0.003, 0.12]) and lack of emotional clarity (β = 0.06, SE = 0.03, 95% CI [0.002, 0.12]), but not for nonacceptance of negative emotions (β = 0.01, SE = 0.03, 95% CI [−0.04, 0.07]), difficulties engaging in goal-directed behavior when distressed (β = −0.01, SE = 0.03, 95% CI [−0.06, 0.04]), or limited access to effective emotion regulation strategies for negative emotions (β = 0.02, SE = 0.02, 95% CI [−0.03, 0.07]).
Next, in the model examining positive emotion dysregulation, significant associations were identified between PTSD and positive emotion dysregulation (B = 0.36, SE = 0.02, t = 14.95, p < .001) and positive emotion dysregulation and deliberate self-harm (B = 0.01, SE = 0.001, t = 5.99, p < .001). Additionally, there was a significant indirect effect of PTSD on deliberate self-harm through positive emotion dysregulation (β= 0.15, SE = 0.03, 95% CI [0.09, 0.22]). Yet, the direct effect linking PTSD symptoms and deliberate self-harm when accounting for positive emotion dysregulation remained significant (B = 0.01, SE = 0.001, t = 9.47, p < .001). Furthermore, when separately probing the emotion dysregulation subscales, significant indirect effects held across three domains: nonacceptance of positive emotions (β = 0.13, SE = 0.03, 95% CI [0.07, 0.20]), difficulties engaging in goal-directed behaviors when experiencing positive emotions (β = 0.11, SE = 0.03, 95% CI [0.06, 0.17]), and difficulties controlling impulsive behaviors when experiencing positive emotions (β = 0.15, SE = 0.03, 95% CI [0.09, 0.21]).
Of note, these results do not differ when including age and gender as covariates. Specifically, there was a significant indirect effect of PTSD on deliberate self-harm through positive emotion dysregulation (β= 0.18, SE = 0.03, 95% CI [0.11, 0.25]). Significant indirect effects were found for nonacceptance of positive emotions (β = 0.15, SE = 0.03, 95% CI [0.09, 0.22]), difficulties engaging in goal-directed behaviors when experiencing positive emotions (β = 0.13, SE = 0.03, 95% CI [0.08, 0.19]), and difficulties controlling impulsive behaviors when experiencing positive emotions (β = 0.17, SE = 0.03, 95% CI [0.11, 0.24]).
In alternate models that switched the intermediate and outcome variables, deliberate self-harm significantly accounted for the relationship between PTSD and positive emotion dysregulation (β = 0.16, SE = 0.03, 95% CI [0.10, 0.22]). Furthermore, deliberate self-harm significantly underlied the relationship between PTSD and nonacceptance of positive emotions (β = 0.14, SE = 0.03, 95% CI [0.08, 0.20]), difficulties engaging in goal-directed behaviors when experiencing positive emotions (β = 0.14, SE = 0.03, 95% CI [0.08, 0.21]), and difficulties controlling impulsive behaviors when experiencing positive emotions (β = 0.17, SE = 0.03, 95% CI [0.11, 0.23]).
4. Discussion
The present study uniquely brings together two burgeoning lines of research examining the relations between emotion dysregulation and both PTSD (Tull et al., 2007; Weiss et al., 2013) and deliberate self-harm (You et al., 2018) among a sample of trauma-exposed military veterans. Results indicate that two specific aspects of negative emotion dysregulation, difficulties controlling impulsive behaviors when distressed and lack of emotional clarity, may help to explain the link between PTSD severity and engagement in deliberate self-harm. Furthermore, extending extant work that primarily focuses on negative emotion dysregulation, the current study also implicates the potential underlying role of positive emotion dysregulation in the association between PTSD symptoms and deliberate self-harm. Effects held across all domains of positive emotion dysregulation: nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions. Findings add to a growing body of research highlighting a need to target emotion dysregulation among veterans.
Partially consistent with our hypothesis, we found that PTSD severity was indirectly related to deliberate self-harm through only two of the five domains of negative emotion dysregulation, and no significant indirect effect was detected for overall negative emotion dysregulation, even when accounting for age and gender. Results of the current study suggest that impulse control problems and lack of emotional clarity, specifically, may be driving the association between PTSD severity and deliberate self-harm. These findings align with past studies highlighting these domains of negative emotion dysregulation as important factors underlying the etiology (Glenn & Klonsky, 2010; Gratz & Roemer, 2008; Turner, Chapman, & Layden, 2012) and treatment (Gratz & Gunderson, 2006; Slee, Spinhoven, Garnefski, & Arensman, 2008) of deliberate self-harm, and suggest their relevance in the context of PTSD in particular. Given evidence that individuals with greater difficulties controlling impulsive behaviors when distressed may be more likely to engage in deliberate self-harm to escape from intense negative emotions (Anestis, Kleiman, Lavender, Tull, & Gratz, 2014), it is not surprising that deliberate self-harm may function to reduce the heightened distress accompanying PTSD. Further, increased confusion regarding one’s negative emotions brought on by PTSD symptoms (Monson, Price, Rodriguez, Ripley, & Warner, 2004) might lead individuals to resort to behaviors such as deliberate self-harm as a means of coping. Future longitudinal research is needed to better understand the functional associations among PTSD symptoms, negative emotion dysregulation, and deliberate self-harm in this population.
It warrants mention that other aspects of negative emotion dysregulation have been found to strongly relate to deliberate self-harm in other samples (e.g., among substance users; Gratz, & Tull, 2010). It is possible that we did not detect a significant indirect effect for overall negative emotion dysregulation and other negative emotion dysregulation domains due to the overlap of general negative affect associated with both negative emotion dysregulation and PTSD (Bradley et al., 2011). Further work should investigate the differential associations among aspects of negative emotion dysregulation and deliberate self-harm as it relates to PTSD and while accounting for overall negative affect. Alternatively, difficulties with impulse control and emotional clarity in the context of negative emotions could be salient factors underlying deliberate self-harm among those experiencing elevated symptoms of PTSD in particular. Thus, future investigations that test the role of negative emotion dysregulation to deliberate self-harm among populations with diverse clinical presentations (e.g., mood and anxiety disorders) are warranted.
The present study adds to the literature on deliberate self-harm by providing preliminary evidence that positive emotion dysregulation may account, in part, for the relation between PTSD and deliberate self-harm. These results are consistent with prior work demonstrating that positive emotion dysregulation is linked to other risky or impulsive behaviors (e.g., substance use) in the context of PTSD (Weiss, Forkus, Raudales, Schick, & Contractor, in press; Weiss, Schick, Contractor, & Dixon-Gordon, 2019). Notably, we found that all domains of positive emotion dysregulation (i.e., nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions) played significant roles within the association between PTSD severity and deliberate self-harm, even when controlling for age and gender. Therefore, positive emotion dysregulation more broadly may be an important construct underlying risk for deliberate self-harm as it relates to PTSD symptomology. Individuals with elevated symptoms of PTSD might utilize deliberate self-harm to down-regulate positive emotions that are experienced as aversive (Weiss, Forkus, Raudales, Schick, & Contractor, in press), or may be more susceptible to engage in deliberate self-harm due to proximal factors including greater distractibility (Dreisbach & Goschke, 2004) and diminished decision-making (Slovic et al., 2004) that increase behavioral dyscontrol in the context of positive emotions. Given the dearth of research in this area, further work is needed to better understand how positive emotion dysregulation in the context of PTSD symptoms could confer risk for deliberate self-harm.
To assess for specificity in the direction of underlying effects, we tested alternative models, whereby the intermediate and outcome variables were switched. Specifically, for negative emotion dysregulation, significant indirect effects were detected for difficulties controlling impulsive behaviors when distressed and lack of emotional clarity, but not for nonacceptance of negative emotions, difficulties engaging in goal-directed behavior when distressed, or limited access to effective emotion regulation strategies for negative emotions. Also, significant indirect effects were found for nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions. These findings shed light on two potential pathways: (1) PTSD symptoms may contribute to emotion dysregulation, thereby increasing the likelihood of engaging in deliberate self-harm, or, (2) PTSD symptoms may motivate individuals to engage in deliberate self-harm, thereby heightening emotion dysregulation. Of note, bidirectional relations among these variables may be likely. While deliberate self-harm may be used to provide immediate relief from trauma-related symptoms in the short term, over time, it is likely to have paradoxical effects, interfering with emotional processing (Foa & Kozak, 1986) and subsequently increasing emotion dysregulation (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). Alternatively, deliberate self-harm may lead to negative secondary emotions (e.g., shame) that exacerbate emotion dysregulation (Bachtelle & Pepper, 2015). Future work would benefit from the application of micro-longitudinal methods to better understand the temporal associations among PTSD symptoms, negative and positive emotion dysregulation, and deliberate self-harm.
The present findings suggest the potential utility of assessing for and targeting emotion dysregulation within treatments for deliberate self-harm among trauma-exposed individuals. Indeed, interventions that focus on emotion dysregulation have exhibited promising effects for both PTSD (e.g., Skills Training in Affective and Interpersonal Regulation; Cloitre, Koenen, Cohen, & Han, 2002) and deliberate self-harm (e.g., Emotion Regulation Group Therapy; Gratz, Tull, & Levy, 2014). Considering support here that emotion dysregulation extending to positive emotions may also play a role in the PTSD-deliberate self-harm relation, it might be particularly helpful for clinicians to teach skills that foster adaptive responses to or tolerance of positive emotions. Future studies are warranted to test whether outcomes for deliberate self-harm can be improved by incorporating elements that target negative and/or positive emotion dysregulation in the context of PTSD symptomology, particularly among veterans.
Interpretations of our findings should be considered in tandem with some limitations. While findings offer insight on the intercorrelations among PTSD symptoms, emotion dysregulation, and deliberate self-harm, the cross-sectional data precludes conclusions regarding the precise nature and direction of these associations; subsequent longitudinal investigations are necessary. This study also relied on self-report measures, which are founded on the willingness and/or ability to accurately report on one’s own emotional experiences. Thus, future studies would benefit from incorporating behavioral or psychophysiological assessments of emotion dysregulation. Given evidence that distinct facets of impulsivity represent unique risks for self-harm (for a review, see Lockwood, Daley, Townsend, & Sayal, 2017), future work should investigate the impulse control domain of emotion dysregulation in the lab. While the present findings suggest that difficulties controlling impulsive behaviors in the context of both negative and positive emotions are important for understanding deliberate self-harm, we were unable to differentiate between planned versus unplanned (e.g., impulsive) episodes of self-harm. Furthermore, although use of a community sample of United States military veterans, who are characterized by elevated rates of PTSD and deliberate self-harm (Calhoun et al., 2017), is a notable strength of our study, the generalizability of results to other trauma-exposed (e.g., sexual trauma) and military (e.g., treatment-seeking) remains unclear. Additional research should test whether findings can be replicated among more diverse populations.
Despite these limitations, the current study represents a critical step in the literature by identifying a need to consider negative and positive emotion dysregulation in the pathway linking PTSD severity and deliberate self-harm. These findings signify new avenues for future research on the mechanisms through which negative and positive emotion dysregulation might confer vulnerability to deliberate self-harm among trauma-exposed individuals.
Clinical Impact Statement:
Military veterans with posttraumatic stress disorder (PTSD) frequently engage in deliberate self-harm. The current study explored whether the relation between PTSD and deliberate self-harm would be explained by negative and positive emotion dysregulation. We found that heightened PTSD severity was related to engagement in deliberate self-harm through overall positive emotion dysregulation, but not overall negative emotion dysregulation. Further analyses indicated underlying roles across domains for positive emotion dysregulation, and for two specific aspects of negative emotion dysregulation. This study identifies a potential need to consider the effects of emotion dysregulation on understanding and treating deliberate self-harm among military veterans.
Acknowledgments
Work on this paper by the second author (NHW) was supported by National Institute on Drug Abuse grant K23DA039327.
References
- American Psychiatric Association; (2013). The Diagnostic and Statistical Manual of Mental Disorders: DSM 5: bookpointUS. [Google Scholar]
- Anestis MD, Kleiman EM, Lavender JM, Tull MT, & Gratz KL (2014). The pursuit of death versus escape from negative affect: An examination of the nature of the relationship between emotion dysregulation and both suicidal behavior and non-suicidal self-injury. Comprehensive Psychiatry, 55(8), 1820–1830. [DOI] [PubMed] [Google Scholar]
- Aust F, Diedenhofen B, Ullrich S, & Musch J (2013). Seriousness checks are useful to improve data validity in online research. Behavior Research Methods, 45(2), 527–535. [DOI] [PubMed] [Google Scholar]
- Bachtelle SE, & Pepper CM (2015). The physical results of nonsuicidal self-injury: The meaning behind the scars. The Journal of Nervous and Mental Disease, 203(12), 927–933. [DOI] [PubMed] [Google Scholar]
- Bekh Bradley D, DeFife JA, Guamaccia C, Phifer MJ, Fani MN, Ressler KJ, & Westen D (2011). Emotion dysregulation and negative affect: association with psychiatric symptoms. The Journal of Clinical Psychiatry, 72(5), 685–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjureberg J, Ljótsson B, Tull MT, Hedman E, Sahlin E, Lundh L-G, … Gumpert CH, 2016. Development and validation of a brief version of the difficulties in emotion regulation scale: the DERS-16. Journal of Psychopathology and Behavioral Assessment, 38(2), 284–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6(1), 3–5. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Van Voorhees EE, Elbogen EB, Dedert EA, Clancy CP, Hair LP, … & Kimbrel NA (2017). Nonsuicidal self-injury and interpersonal violence in US veterans seeking help for posttraumatic stress disorder. Psychiatry Research, 247(1), 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, & Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. [DOI] [PubMed] [Google Scholar]
- Dreisbach G, & Goschke T (2004). How positive affect modulates cognitive control: reduced perseveration at the cost of increased distractibility. Journal of Experimental Psychology: Learning, Memory, and Cognition, 30(2), 343. [DOI] [PubMed] [Google Scholar]
- Fliege H, Kocalevent R, Walter OB, Beck S, Gratz KL, Gutierrez PM, et al. (2006). Three assessment tools for deliberate self-harm and suicide behavior: evaluation and psychopathological correlates. Journal of Psychosomatic Research, 61(1), 113–121. [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: exposure to corrective information. Psychological Bulletin, 99(1), 20. [PubMed] [Google Scholar]
- Forbes CN, Tull MT, Richmond JR, Chapman AL, Dixon-Gordon KL, & Gratz KL (2019). Motives for Nonsuicidal Self-Injury in Individuals with Lifetime Depressive Disorders and Posttraumatic Stress Disorder. Journal of Psychopathology and Behavioral Assessment, 1–10. [Google Scholar]
- Ford JD, & Gómez JM (2015). The relationship of psychological trauma and dissociative and posttraumatic stress disorders to nonsuicidal self-injury and suicidality: A review. Journal of Trauma & Dissociation, 16(3), 232–271. [DOI] [PubMed] [Google Scholar]
- Frewen PA, Dean JA, & Lanius RA (2012). Assessment of anhedonia in psychological trauma: Development of the Hedonic Deficit and Interference Scale. European Journal of Psychotraumatology, 3(1), 8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL (2001). Measurement of deliberate self-harm: Preliminary data on the deliberate self-harm inventory. Journal of Psychopathology and Behavioral Assessment, 23(4), 253–263. [Google Scholar]
- Gratz KL, & Tull MT (2010). The relationship between emotion dysregulation and deliberate self-harm among inpatients with substance use disorders. Cognitive Therapy and Research, 34(6), 544–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Tull MT (2012). Exploring the relationship between posttraumatic stress disorder and deliberate self-harm: The moderating roles of borderline and avoidant personality disorders. Psychiatry Research, 199(1), 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, & Levy R (2014). Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine, 44(10), 2099–2112. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Gratz KL, & Roemer L (2008). The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy, 37(1), 14–25. [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Gunderson JG (2006). Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy, 37(1), 25–35. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric Properties of the Life Events Checklist. Assessment, 11(4), 330–341. [DOI] [PubMed] [Google Scholar]
- Glenn CR, & Klonsky ED (2010). A multimethod analysis of impulsivity in nonsuicidal self-injury. Personality Disorders: Theory, Research, and Treatment, 1(1), 67. [DOI] [PubMed] [Google Scholar]
- Haw C, Hawton K, Houston K, & Townsend E (2001). Psychiatric and personality disorders in deliberate self-harm patients. The British Journal of Psychiatry, 178(1), 48–54. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. In: University of Kansas, KS. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, & Morissette SB (2016). Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research, 243(1), 232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May AM, & Glenn CR (2013). The relationship between non-suicidal self-injury and attempted suicide: Converging evidence from four samples. Journal of Abnormal Psychology, 122(1), 231–237. [DOI] [PubMed] [Google Scholar]
- Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, & Couper M (2004). Psychological research online: Report of Board of Scientific Affairs' Advisory Group on the Conduct of Research on the Internet. American Psychologist, 59(2), 105–117. [DOI] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology, 109(1), 26–39. [DOI] [PubMed] [Google Scholar]
- Lockwood J, Daley D, Townsend E, & Sayal K (2017). Impulsivity and self-harm in adolescence: a systematic review. European Child & Adolescent Psychiatry, 26(4), 387–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn BM-D, & Morgan JK (2016). Using Amazon’s Mechanical Turk (MTurk) to recruit military veterans: Issues and suggestions. The Military Psychologist, 31(3), 8–14. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott MJ, Tull MT, Gratz KL, Daughters SB, & Lejuez CW (2009). The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. Journal of Anxiety Disorders, 23(5), 591–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. [DOI] [PubMed] [Google Scholar]
- Mischra S, & Carleton N (2017). Use of online crowdsourcing platforms for gambling research. International Gambling Studies, 17(1), 125–143. [Google Scholar]
- Monson CM, Price JL, Rodriguez BF, Ripley MP, & Warner RA (2004). Emotional deficits in military-related PTSD: An investigation of content and process disturbances. Journal of Traumatic Stress, 17(3), 275–279. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, & Kerr PL (2010). Untangling a complex web: How non-suicidal self-injury and suicide attempts differ. The Prevention Researcher, 17(1), 8–11.20835367 [Google Scholar]
- Norman SB, Wilkins KC, Myers US, & Allard CB (2014). Trauma informed guilt reduction therapy with combat veterans. Cognitive and Behavioral Practice, 21(1), 78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. [DOI] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1(2), 213–220. [Google Scholar]
- Sippel LM, Roy AM, Southwick SM, & Fichtenholtz HM (2016). An examination of the roles of trauma exposure and posttraumatic stress disorder on emotion regulation strategies of Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn veterans. Cognitive Behaviour Therapy, 45(5), 339–350. [DOI] [PubMed] [Google Scholar]
- Slee N, Spinhoven P, Gamefski N, & Arensman E (2008). Emotion regulation as mediator of treatment outcome in therapy for deliberate self-harm. Clinical Psychology & Psychotherapy, 15(4), 205–216. [DOI] [PubMed] [Google Scholar]
- Slovic P, Finucane ML, Peters E, & MacGregor DG (2004). Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk, and rationality. Risk Analysis: An International Journal, 24(2), 311–322. [DOI] [PubMed] [Google Scholar]
- Smith NB, Kouros CD, & Meuret AE (2014). The role of trauma symptoms in nonsuicidal self-injury. Trauma, Violence, & Abuse, 15(1), 41–56. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, & Roemer L (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38(3), 303–313. [DOI] [PubMed] [Google Scholar]
- Thomas KA, & Clifford S (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Computers and Human Behavior, 77(3), 184–197. [Google Scholar]
- Turner BJ, Chapman AL, & Layden BK (2012). Intrapersonal and interpersonal functions of non suicidal self-injury: Associations with emotional and social functioning. Suicide and Life-Threatening Behavior, 42(1), 36–55. [DOI] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M (2018). Crowdsourcing trauma: Psychopathology in a trauma-exposed sample recruited via Mechanical Turk. Journal of Traumatic Stress, 31(4), 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weiss NH, Contractor AA, Forkus SR, Goncharenko S, & Raudales AM (in press) Positive emotion dysregulation among community individuals: The role of traumatic exposure and posttraumatic stress disorder. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Contractor AA, Raudales AM, Greene T, & Short NA (in press). Extending our understanding of the association between posttraumatic stress disorder and positive emotion dysregulation: A network analysis approach. Journal of Anxiety Disorders. doi: 10.1016/j.janxdis.2020.102198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Darosh A, Contractor AA, Schick MR, & Dixon-Gordon KL (2019). Confirmatory validation of the factor structure and psychometric properties of the Difficulties in Emotion Regulation Scale – Positive. Journal of Clinical Psychology, 75(7), 1267–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender JM (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-Positive. Behavior Modification, 39(3), 431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Schick MR, Contractor AA, & Dixon-Gordon KL (2019). Posttraumatic stress disorder and substance use: Identifying the underlying role of difficulties regulating positive emotions. Addictive Behaviors, 96, 119–126. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, & Tull MT (2015). Explicating the role of emotion dysregulation in risky behaviors: A review and synthesis of the literature with directions for future research and clinical practice. Current Opinion in Psychology, 3, 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128(1-2), 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, & Gratz KL (2015). Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence, 155, 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, & Hembree EA (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. [DOI] [PubMed] [Google Scholar]
- You J, Ren Y, Zhang X, Wu Z, Xu S, & Lin MP (2018). Emotional dysregulation and nonsuicidal self-injury: A meta-analytic review. Neuropsychiatry, 8(2), 733–748. [Google Scholar]
- Zullig KJ (2016). The association between deliberate self-harm and college student subjective quality of life. American Journal of Health Behavior, 40(2), 231–239. [DOI] [PubMed] [Google Scholar]


