Abstract
Introduction
The shape of the glucose curve during an oral glucose tolerance test (OGTT) reflects β-cell function in populations without diabetes but has not been as well studied in those with diabetes. A monophasic shape has been associated with higher risk of diabetes, while a biphasic pattern has been associated with lower risk. We sought to determine if phenotypic or metabolic characteristics were associated with glucose response curve shape in adults with type 2 diabetes treated with metformin alone.
Research design and methods
This is a cross-sectional analysis of 3108 metformin-treated adults with type 2 diabetes diagnosed <10 years who underwent 2-hour 75 g OGTT at baseline as part of the Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE). Insulin sensitivity (homeostasis model of insulin sensitivity, HOMA2-S) and β-cell function (early, late, and total incremental insulin and C peptide responses adjusted for HOMA2-S) were calculated. Glucose curve shape was classified as monophasic, biphasic, or continuous rise.
Results
The monophasic profile was the most common (67.8% monophasic, 5.5% biphasic, 26.7% continuous rise). The monophasic subgroup was younger, more likely male and white, and had higher body mass index (BMI), while the continuous rise subgroup was more likely female and African American/black. HOMA2-S and fasting glucose did not differ among the subgroups. The biphasic subgroup had the highest early, late, and total insulin and C peptide responses (all p<0.05 vs monophasic and continuous rise). Compared with the monophasic subgroup, the continuous rise subgroup had similar early insulin (p=0.3) and C peptide (p=0.6) responses but lower late insulin (p<0.001) and total insulin (p=0.008) and C peptide (p<0.001) responses.
Conclusions
Based on the large multiethnic GRADE cohort, sex, race, age, and BMI were found to be important determinants of the shape of the glucose response curve. A pattern of a continuously rising glucose at 2 hours reflected reduced β-cell function and may portend increased glycemic failure rates.
Trial registration number
Keywords: OGTT, glucose, diabetes mellitus, type 2, insulin
Significance of this study.
What is already known about this subject?
The shape of the glucose response curve from an OGTT has been evaluated mostly in persons without diabetes, where it has been shown to be associated with β-cell function and predicts the development of both type 1 and type 2 diabetes.
What are the new findings?
The prevalence of a monophasic glucose response curve shape in adults is more common if male, white or obese.
The prevalence of a continuously rising glucose response curve at 2 hours is more common if female or African American/black.
The continuous rise pattern in adults with type 2 diabetes was associated with lower late insulin and total insulin and C peptide responses to glucose, indicating reduced β-cell function.
How might these results change the focus of research or clinical practice?
The shape of the glucose response curve may provide a biomarker to identify and target those patients with type 2 diabetes who are more likely to have either better (biphasic pattern) or poorer (continuous rise pattern) β-cell function for both research and clinical interventions.
Introduction
Type 2 diabetes is a heterogeneous disorder affecting men and women with varying degrees of obesity from all races and ethnicities. Insulin sensitivity and β-cell function are key determinants in the pathophysiology underlying the development of type 2 diabetes and vary from person to person. Glucose tolerance is typically evaluated by assessing the ability to respond to an oral glucose load. In addition to diagnostic glucose cut-points, the shape of the glucose response curve during an oral glucose tolerance test (OGTT) has been noted to fall into patterns that reflect differences in underlying β-cell function and metabolic risk.1–9 A biphasic or multiphasic glucose profile, characterized by a rise, fall, and subsequent rise in glucose after an oral glucose challenge, has been associated with better β-cell function and lower glucose concentrations compared with a monophasic pattern (simple rise and fall) in adults2–5 and youth7–9 with normal and impaired glucose tolerance. In youth with type 2 diabetes, a third pattern of a glucose that has not yet started to decline within the 2 hours following a glucose load was noted, and this pattern, which we have designated as a continuous rise pattern, was associated with poorer β-cell function and greater risk of progression compared with a monophasic or biphasic pattern.10 Only two studies have evaluated glucose response curve shape in populations that included large numbers of adults with type 2 diabetes (a large Chinese population5 and in European women with history of gestational diabetes6), but both studies only identified monophasic or multiphasic patterns.
The Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) comprises a large, multiethnic, well-characterized population of mostly middle-aged adults with <10 years duration of diagnosed type 2 diabetes. Its participants are broadly representative of the subset of early type 2 diabetes in the USA, the vast majority of whom are treated with metformin on diagnosis. Participants in GRADE underwent a standard 2-hour OGTT at baseline from which glucose response curves were evaluated. The objectives of the current analyses were threefold: first, determine the prevalence of different glucose response curve shapes in adults with type 2 diabetes treated with metformin alone; second, identify demographic and/or anthropometric factors that associate within glucose response curve subgroups by using classification analysis and multiple linear regression models; and third, determine the association between OGTT glucose response curve shape with estimates of insulin sensitivity and β-cell function. We hypothesized that glucose response curve shape would reflect β-cell function measures in type 2 diabetes and that the biphasic curve shape would be associated with better β-cell function consistent with findings in populations without diabetes.
Subjects, materials, and methods
Study design
We report cross-sectional analyses of baseline data of individuals with type 2 diabetes enrolled in the GRADE. GRADE is a multicenter National Institute of Diabetes and Digestive and Kidney Diseases-funded study conducted in 36 centers across the USA.11 The full GRADE protocol has been published11 and is also available on the GRADE website (https://grade.bsc.gwu.edu/ancillary-study-info). GRADE enrollment occurred between 2013 and 2017. All participants provided written informed consent.
Participants
Participants were eligible if they were ≥30 years of age (≥20 years if Native American) at the time of type 2 diabetes diagnosis, had been diagnosed with type 2 diabetes <10 years before study entry, and were treated with metformin alone. Participants eligible after initial screening underwent a run-in period of 6–14 weeks during which the metformin dose was adjusted, aiming for 2000 mg/day, with a minimum of 1000 mg/day. Participants who were unable to tolerate at least 1000 mg/day were ineligible. Participants were enrolled in the study if their hemoglobin A1c (HbA1c) measured at the end of run-in was between 6.8% and 8.5% (51–69 mmol/mol). A complete list of exclusion criteria is provided separately,11 but included suspected type 1 diabetes and treatment with glucose-lowering medication(s) other than metformin within the past 6 months.
A total of 5047 adults were enrolled in GRADE and completed the baseline visit. We present here a cross-sectional analysis on a subgroup of this cohort with complete baseline data available currently (n=3108). Baseline samples for those randomized to glargine (n=1263), one of the four intervention groups, have not yet been assayed for insulin given the need to validate the assay for measurement of glargine insulin and its metabolites and thus were excluded. Also excluded were 676 participants with incomplete glucose, insulin, or C peptide values.
Study procedures
After at least an 8-hour overnight fast, eligible participants underwent a baseline visit. Information about their medical history and current medication use was obtained along with assessment of body size (waist circumference, weight, and height), blood pressure, demographic characteristics (age, sex, race, and ethnicity), and laboratory measurements. A standardized 75 g OGTT was performed. Metformin was held on the morning of the OGTT. Blood samples were drawn at baseline and then at 30, 60, 90 and 120 min after the start of glucose ingestion. Plasma was separated by centrifugation, aliquoted into cryovials, and frozen prior to shipment on dry ice to the central laboratory (University of Minnesota, Minneapolis, Minnesota) where samples were assayed for glucose, insulin, and C peptide.
Assays
HbA1c was measured in EDTA whole blood on the Tosoh high performance liquid chromatography (HPLC) Glycohemoglobin Analyzer (Tosoh Medics, San Francisco, California). This method is calibrated against the National Glycohemoglobin Standardization Program standards. EDTA plasma samples were used to measure glucose with a hexokinase method on the Roche cobas c501 Chemistry Analyzer (Roche Diagnostics, Indianapolis, Indiana) and insulin and C peptide using a sandwich immunoassay (Roche Diagnostics) on the Roche cobas e601 immunoassay analyzer.
Calculations
Insulin sensitivity
The homeostasis model of insulin sensitivity (HOMA2-S) was calculated using the HOMA2 Calculator V.2.2.3 (Diabetes Trials Unit, University of Oxford, Oxford, UK).12 13
Insulin and C peptide responses to glucose
The insulinogenic index, a measure of the early insulin response, was calculated as the change in insulin divided by the change in glucose from 0 to 30 minutes. A similar C peptide index for the early response was calculated as the change in C peptide divided by the change in glucose from 0 to 30 minutes. For each OGTT, the mean incremental area under the curve (incAUC) for glucose, insulin, and C peptide was calculated as the area under the curve using the trapezoidal rule, divided by 120 minus the fasting value. The ratios of the total incAUC insulin and C peptide responses were divided by the incAUC glucose (incAUCins/incAUCglu and incAUC-CP/incAUCglu) to reflect insulin and C peptide responses to glucose over the OGTT. The late insulin response was calculated as 100×(InsulinAUC60–120/60−I0)/GlucoseAUC60–120/60−G0). An estimate of relative fasting insulin clearance was calculated as fasting C peptide divided by fasting insulin.
Glucose response curve classification
Participants were classified into subgroups according to the shape of the glucose response curve over the 120 minutes of the test. For this analysis, we required complete baseline data for glucose, insulin, and C peptide at the 0, 30, 60, 90, and 120 minute time-points (n=3108). A monophasic shape was defined as a simple increase to a peak with a subsequent decrease in glucose. A biphasic shape was defined as a rise in glucose followed by a decrease and a subsequent increase. A continuous rise shape was defined as a profile that increased monotonically with no inflection downward during the 120 min time period. A change in glucose of less than 0.25 mmol/L (4.5 mg/dL) between consecutive time-points was ignored, as done by others.3
Statistical analysis
Participant characteristics were summarized using mean and SD for quantitative variables and counts and column percentages for qualitative variables. Comparisons between pairs of glucose pattern subtypes use the χ² test of independence for qualitative variables and the Student’s t-test with unequal variances for quantitative variables. The overall comparison tests the null hypothesis of equality for all three subtypes and uses the χ² test of independence for qualitative variables and analysis of variance type III F test for quantitative variables. Adjusted p values comparing the proportions of glucose response curve shapes in men and women and between races were obtained from a type III test in a multinomial regression model with race, sex, age, body mass index (BMI), duration of diabetes, estimated glomerular filtration rate (eGFR), and metformin dose as potential determinants.
Extreme outliers were present for the following variables: insulin, HOMA2-S, insulinogenic and C peptide indices, late insulin response, and ratios of incremental insulin and C peptide AUC to incremental glucose AUC. To reduce the influence of outliers on analyses, these variables were winsorized, that is, values above or below specified cut-offs were replaced by the cut-offs. For each variable, the winsorization upper (lower) cut-off was set to the median plus (minus) 8.9 times the distance from the median to the upper (lower) quartiles. For a normally distributed variable, this results in cut-offs 6 SD above and below the mean. The number of winsorized values ranged from 5 (0.2% of values) for insulin at 30 minutes to 26 (0.8%) for the late insulin response.
Differences in metabolic responses between pairs of glucose pattern subtypes were compared using the least square means adjusting for sex, age, race, BMI, diabetes duration, eGFR, and metformin dose. Insulin and C peptide responses were further adjusted for HOMA2-S to assess β-cell function (these are denoted by an asterisk). Adjusted p values were calculated using the Tukey Honest Significant Difference (HSD) approach. The overall p value is based on a type III F test adjusting for the same covariates.
The characteristics of participants with various glucose patterns were summarized by fitting a classification tree model14 with glucose pattern as the response. To examine the effects of both sex and race on the distribution of the glucose patterns, a limited classification tree model was run including only these two covariates (figure 1A). A single classification tree model was also performed including the following covariates: race, sex, BMI as a categorical variable (0–24.9, 25–29.9, 30–34.9, 35–39.9, ≥40), waist to hip ratio, and duration of diabetes (figure 1B). Those with race classified as other, unknown, or Pacific Islander were not included in the classification analysis as the numbers were too small for Pacific Islanders and the groups classified as unknown and other were too varied, including multiracial, that it was hard to draw conclusions (n=2859). An additional four participants were lacking BMI values and thus were excluded from the model that included BMI (n=2855). Classification trees for figure 1 are presented in online supplemental figure 1. In each case, minimal cost-complexity pruning with 20-fold cross-validation was used to obtain the final classification.
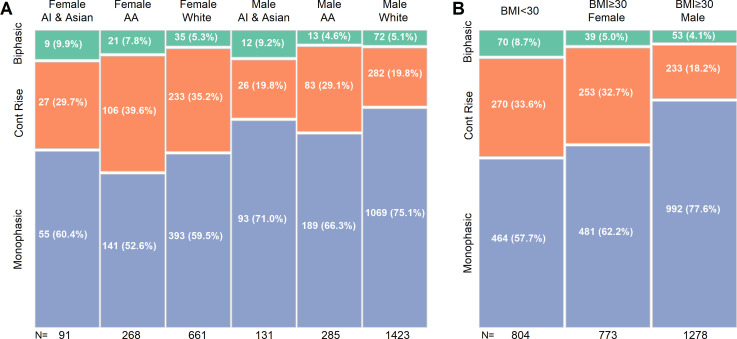
Figure 1.
Classification analysis of OGTT glucose response curve shapes by sex and race (A) and sex, race, BMI, waist to hip ratio, and duration of diabetes (B). In B, only sex and BMI remained as significant independent classifiers. The percentages within each column are shown on the plot. AA, African American; AI, American Indian; BMI, body mass index; OGTT, oral glucose tolerance test.
bmjdrc-2021-002264supp001.pdf (357.6KB, pdf)
All analyses were performed using R V.3.6.015 and p<0.05 was considered statistically significant.
Results
Participant characteristics
Overall, individuals in the cohort were mostly male, middle-aged, obese, and had diabetes for an average of 4 years (table 1). The cohort was racially diverse, with one-third being non-white. Over 90% of participants were taking the maximum dose of metformin (2000 mg/day). Most participants had a monophasic glucose response curve shape (67.8%), while 26.7% demonstrated a continuous rise pattern and only 5.5% a biphasic shape.
Table 1.
Baseline characteristics by glucose response curve shape
| All | Monophasic | Biphasic | Continuous rise | Overall p value | M vs B | M vs C | B vs C | |
| P value | P value | P value | ||||||
| n | 3108 | 2107 | 172 | 829 | ||||
| Female (%) | 1124 (36.2) | 645 (30.6) | 71 (41.3) | 408 (49.2) | <0.001 | 0.005 | <0.001 | 0.070 |
| Age (years) | 56.6 (10.0) | 56.0 (9.9) | 57.0 (10.9) | 58.1 (9.9) | <0.001 | 0.216 | <0.001 | 0.249 |
| Age (years) (%) | <0.001 | 0.048 | <0.001 | 0.242 | ||||
| 22–50 | 835 (26.9) | 602 (28.6) | 49 (28.5) | 184 (22.2) | ||||
| >50–60 | 1095 (35.2) | 757 (35.9) | 49 (28.5) | 289 (34.9) | ||||
| >60–70 | 970 (31.2) | 637 (30.2) | 58 (33.7) | 275 (33.2) | ||||
| >70–85 | 207 (6.7) | 110 (5.2) | 16 (9.3) | 81 (9.8) | ||||
| Race (%) | <0.001 | 0.080 | <0.001 | 0.139 | ||||
| American Indian/Alaska Native | 103 (3.3) | 73 (3.5) | 8 (4.7) | 22 (2.7) | ||||
| Asian | 119 (3.8) | 75 (3.6) | 13 (7.6) | 31 (3.7) | ||||
| Hawaiian/Pacific Islander | 20 (0.6) | 17 (0.8) | 1 (0.6) | 2 (0.2) | ||||
| African American/black | 553 (17.8) | 330 (15.7) | 34 (19.8) | 189 (22.8) | ||||
| White | 2084 (67.1) | 1466 (69.6) | 107 (62.2) | 515 (62.1) | ||||
| Other/multiple | 189 (6.1) | 121 (5.7) | 8 (4.7) | 60 (7.2) | ||||
| Unknown/not reported | 40 (1.3) | 29 (1.4) | 1 (0.6) | 10 (1.2) | ||||
| Hispanic (%) | 611 (19.8) | 391 (18.7) | 34 (19.9) | 186 (22.7) | 0.053 | 0.780 | 0.018 | 0.484 |
| Anthropometrics | ||||||||
| Weight (kg) | 99.6 (22.1) | 103.2 (22.4) | 93.6 (21.8) | 91.4 (19.0) | <0.001 | <0.001 | <0.001 | 0.216 |
| BMI (kg/m2) | 34.2 (6.7) | 34.9 (6.8) | 32.5 (6.4) | 32.5 (6.0) | <0.001 | <0.001 | <0.001 | 0.904 |
| Waist circumference (cm) | 112.2 (15.7) | 114.4 (15.6) | 108.8 (18.1) | 107.3 (14.3) | <0.001 | <0.001 | <0.001 | 0.306 |
| Duration of diabetes (years) | 4.0 (2.8) | 3.9 (2.7) | 4.3 (2.8) | 4.3 (2.8) | 0.006 | 0.108 | 0.004 | 0.907 |
| Metformin dose (mg/day) (%) | 0.001 | 0.040 | <0.001 | 0.478 | ||||
| 1000 | 107 (3.4) | 60 (2.8) | 6 (3.5) | 41 (4.9) | ||||
| 1500 | 125 (4.0) | 70 (3.3) | 12 (7.0) | 43 (5.2) | ||||
| 2000 | 2876 (92.5) | 1977 (93.8) | 154 (89.5) | 745 (89.9) | ||||
| eGFR (mL/min/1.73 m2) | 95.4 (16.9) | 95.7 (16.6) | 95.8 (7.6) | 94.8 (17.4) | 0.414 | 0.913 | 0.204 | 0.478 |
Mean (SD).
B, biphasic shape; BMI, body mass index; C, continuous rise shape; eGFR, estimated glomerular filtration rate; M, monophasic shape.
There were several notable differences in baseline characteristics between the three subgroups. Those with a monophasic glucose response curve shape were more likely to be male, younger, and white, have a shorter duration of diabetes, higher BMI and waist circumference, and taking a higher dose of metformin compared with the other two subgroups. Participants with a continuous rise shape were more likely to be female and African American/black. Differences in prevalence by sex remained significant after adjusting for race, age, BMI, duration of diabetes, eGFR, and metformin dose (p<0.001). Differences in prevalence by race also remained significant after adjusting for sex, age, BMI, duration of diabetes, eGFR, and metformin dose (p=0.019). There were no statistically significant differences between the subgroups by duration of diabetes or renal function.
Prevalence of the glucose response curve shape by classification analysis
Classification analysis revealed subsets by sex, race, and BMI (figure 1). When sex and race were combined in the model, six separate subsets emerged, confirming differential distributions by both race and sex (figure 1A). Asian and American Indian men and women had the highest prevalence of the biphasic shape, while African American/black men had the lowest.
To evaluate if obesity changed the classification analysis, BMI (0–24.9, 25–29.9, 30–34.9, 35–39.9, ≥40) was added to a model including race, sex, waist to hip ratio, and duration of diabetes (figure 1B). Sex and BMI ≥30 identified three distinct subsets, while race, waist to hip ratio, and duration of diabetes dropped out. BMI <30 had a greater proportion of biphasic curve shape, while obese men had the largest fraction of the monophasic curve shape.
Metabolic differences by glucose response curve shape
Figure 2 illustrates the mean and 95% CI for glucose, insulin, and C peptide concentrations over time derived from the OGTT for each subgroup. The metabolic data are presented in table 2. The biphasic subgroup had the lowest peak glucose and mean incAUCglu. The 2-hour glucose and HbA1c were highest in the continuous rise subgroup, but peak glucose and mean incAUCglu were the highest in the monophasic subgroup. Fasting glucose did not differ.
Figure 2.
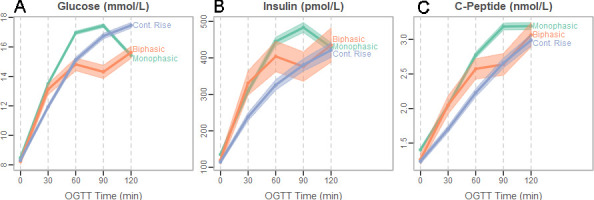
OGTT glucose response curve shape for the whole cohort classified as monophasic, biphasic, or continuous rise. Mean glucose (A), insulin (B), and C peptide (C) are depicted at each OGTT time-point separately for participants within each of the subgroups. Pointwise 95% CIs are drawn around the means at each time-point. OGTT, oral glucose tolerance test.
Table 2.
Comparison of metabolic parameters by glucose response curve shape
| All | Monophasic | Biphasic | Continuous rise | Overall p value | M vs B | M vs C | B vs C | |
| P value | P value | P value | ||||||
| n | 3108 | 2107 | 172 | 829 | ||||
| HbA1c (%) | 7.50 (0.48) | 7.49 (0.48) | 7.49 (0.48) | 7.52 (0.49) | 0.032 | 0.900 | 0.022 | 0.613 |
| HbA1c (% mmol/mol) | 58.4 (5.3) | 58.4 (5.2) | 58.4 (5.2) | 58.7 (5.4) | 0.032 | 0.900 | 0.022 | 0.613 |
| Fasting glucose (mmol/L) | 8.42 (1.71) | 8.48 (1.73) | 8.24 (1.50) | 8.31 (.70) | 0.734 | 0.703 | 0.984 | 0.778 |
| 2-hour glucose (mmol/L) | 15.98 (3.06) | 15.42 (2.98) | 15.63 (2.71) | 17.46 (2.85) | <0.001 | 0.965 | <0.001 | <0.001 |
| Peak glucose (mmol/L) | 17.69 (2.87) | 17.87 (2.88) | 16.40 (2.42) | 17.48 (2.85) | <0.001 | <0.001 | <0.001 | <0.001 |
| Proportions with peak glucose at OGTT time-point, n (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| 30 min | 21 (0.7) | 9 (0.4) | 12 (7.0) | 0 (0.0) | ||||
| 60 min | 793 (25.5) | 721 (34.2) | 61 (35.5) | 11 (1.3) | ||||
| 90 min | 1536 (49.4) | 1377 (65.4) | 19 (11.0) | 140 (16.9) | ||||
| 120 min | 758 (24.4) | 0 (0.0) | 80 (46.5) | 678 (81.8) | ||||
| Mean time to peak glucose (min) | 89.3 (21.7) | 79.5 (14.6) | 89.1 (31.5) | 114.1 (12.9) | <0.001 | <0.001 | <0.001 | <0.001 |
| Mean incAUCglu (mmol/L) | 6.3 (1.6) | 6.5 (1.5) | 5.3 (1.6) | 5.9 (1.5) | <0.001 | <0.001 | <0.001 | <0.001 |
| HOMA2-S model (%) | 56.5 (40.6) | 53.2 (38.) | 60.9 (41.5) | 63.9 (45.6) | 0.077 | 0.979 | 0.058 | 0.588 |
| Fasting insulin (pmol/L) | 128.9 (89.0) | 135.3 (91.7) | 119.6 (81.4) | 114.5 (81.4) | 0.742 | 0.976 | 0.755 | 0.841 |
| Insulinogenic index (nmol/mol)* | 36.5 (30.2) | 36.4 (29.0) | 44.1 (37.0) | 35.3 (31.5) | <0.001 | <0.001 | 0.327 | <0.001 |
| Late insulin response (pmol/mol)* | 40.4 (34.8) | 42.4 (36.7) | 46.3 (39.8) | 34.0 (27.2) | <0.001 | 0.033 | <0.001 | <0.001 |
| incAUCins/incAUCglu (nmol/mol)* | 39.1 (31.5) | 40.5 (32.6) | 45.9 (36.5) | 34.0 (23.6) | <0.001 | 0.001 | 0.008 | <0.001 |
| Fasting C peptide (nmol/L) | 1.35 (0.56) | 1.40 (0.57) | 1.26 (0.49) | 1.23 (0.53) | 0.060 | 0.656 | 0.049 | 0.927 |
| C peptide index (nmol/mmol)* | 0.135 (0.096) | 0.134 (0.089) | 0.155 (0.119) | 0.133 (0.106) | 0.003 | 0.002 | 0.646 | 0.014 |
| incAUC-CP/incAUCglu (µmol/mol)* | 0.19 (0.11) | 0.19 (0.11) | 0.22 (0.13) | 0.17 (0.09) | <0.001 | 0.002 | <0.001 | <0.001 |
| C peptide/insulin (µmol/pmol) | 12.5 (4.6) | 12.3 (4.4) | 12.7 (4.4) | 13.0 (5.1) | 0.070 | 0.442 | 0.075 | 0.999 |
Mean (SD).
All comparisons were adjusted for sex, age, race, BMI, diabetes duration, eGFR, and metformin dose.
*Insulin and C peptide responses were further adjusted for HOMA2-S.
B, biphasic shape; BMI, body mass index; C, continuous rise shape; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c; HOMA2-S, homeostasis model of insulin sensitivity; incAUC-CP, incremental area under curve C peptide; incAUCglu, incremental area under curve glucose; incAUCins, incremental area under curve insulin; M, monophasic shape; OGTT, oral glucose tolerance test.
Participants with the biphasic response pattern had the highest early, late, and total insulin and C peptide responses to glucose load adjusted for insulin sensitivity. Participants with the monophasic and continuous rise response patterns had similar early insulin and C peptide responses, but those with continuous rise had lower late insulin and total insulin and C peptide responses (table 2 and illustrated in figure 2B, C). Those with the continuous rise pattern also appeared to have a relatively delayed glucose rise that was matched by a concomitant delay in the rise in insulin and C peptide concentrations (figure 2). This delay in glucose rise in the continuous rise subgroup was observed in both men and women (figure 3).
Figure 3.
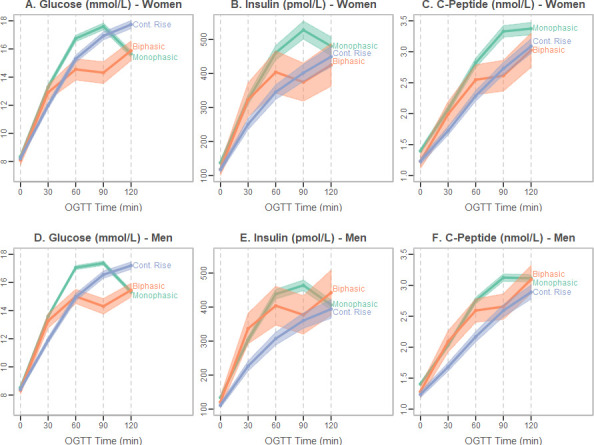
OGTT glucose response curve shapes stratified by sex: monophasic, biphasic, or continuous rise. Mean glucose (A women, D men), insulin (B women, E men), and C peptide (C women, F men) are depicted at each OGTT time-point separately for participants within each of the subgroups. Pointwise 95% CIs are drawn around the means at each time-point. OGTT, oral glucose tolerance test.
HOMA2-S did not differ by glucose curve shape (table 2). Note that all insulin and C peptide responses to glucose were adjusted for insulin sensitivity (HOMA2-S) given the well-known inverse relationship between responses and sensitivity, thereby providing an estimate of β-cell function (table 2, adjustment for HOMA2-S denoted by asterisk).
Conclusions
This study presents novel data on several aspects related to the shape of the glucose response curve during an OGTT. First, it is the first large study of its kind in people with type 2 diabetes, all on metformin only, that includes both men and women over a broad range of ethnicities and BMI. Second, the analysis highlights novel associations in the prevalence of glucose response curve patterns by sex, race, age, and BMI. Third, it investigates a new continuous rise glucose pattern, which has only previously been evaluated in youth in the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study,10 and more recently in youth and adults with impaired glucose tolerance or newly diagnosed type 2 diabetes in the Restoring Insulin Secretion (RISE) study.16 Fourth, the study highlights the differences in β-cell function linked with each glucose response curve pattern, with a biphasic shape, although uncommon, demonstrating better β-cell function and the continuous rise subgroup showing reduced measures of late β-cell function relative to those with a monophasic shape.
Differences by sex in the prevalence of the monophasic and continuous rise subgroups were present that were independent of race and BMI using both a least squares and classification approach. Previous studies found that the biphasic or multiphasic pattern was more common in women (3-hour OGTT analysis in a large Chinese adult population with and without diabetes5 and a European population without diabetes3) or did not differ by sex.2 4 However, none of these studies included an analysis of a continuously rising glucose pattern. In GRADE, we found that more women exhibited a continuous rise shape, which has lower β-cell function, findings that are opposite to that in populations without diabetes, where the biphasic or multiphasic shape, associated with better β-cell function, was more common in women. The reason for a sex difference in the prevalence of the monophasic and continuous rise glucose curve shapes among GRADE participants is not clear but warrants further investigation.
Race also impacted the prevalence of the glucose curve subgroups but was in part due to differences in BMI. When BMI category was added to the classification analysis, race dropped out, but race remained independently associated with glucose response curve shape when adjusting for BMI in the least squares analysis. The most significant finding was a higher prevalence of the continuous rise shape in African American/black. Racial differences in curve shape distribution have not been reported for adults with type 2 diabetes and there were no differences in glucose response curve shape by race in youth with type 2 diabetes in the TODAY study.10 If the continuous rise pattern in adults follows the more aggressive course observed in youth in the TODAY study,10 the greater prevalence of this pattern in African American/black could portend a higher risk of progression to glycemic failure. African American/black individuals are disproportionally affected by type 2 diabetes, with a prevalence in the USA of 16.4% compared with 11.9% in non-Hispanic white.17 They also are at higher risk of developing type 2 diabetes, with the Coronary Artery Risk Development in Young Adults study finding a more than twofold higher risk of developing type 2 diabetes, although the disparity was no longer significant after adjusting for known modifiable risk factors, with biological factors having the greatest impact.18
Differences in both age and diabetes duration were also noted in the prevalence of the monophasic and continuous rise subgroups, with the monophasic subgroup being older and having a longer duration of diabetes. This is perhaps not surprising. A systematic review of the literature indicates that β-cell function declines with aging, consistent with the increase in incidence of type 2 diabetes in the aging population.19
The continuous rise curve shape has not yet been described in a large cohort of adults with type 2 diabetes. The two large studies that evaluated glucose response curve shape in adults with type 2 diabetes5 6 based classification on a 3-hour OGTT rather than the standard 2-hour test. Delays or deficiencies in insulin secretion and response that result in a continuous rise shape on a 2-hour test need a longer sampling time frame to capture the eventual fall in glucose. In essence, the classification of monophasic versus continuous rise glucose curve shapes reflects differences in timing. Thus, classification by curve shape alone during a 3-hour test is likely to miss important differences in timing between monophasic and continuous rise subgroups identified on a 2-hour test.
In GRADE, the early insulin and C peptide responses to glucose did not differ between the continuous rise and monophasic subgroups, but the continuous rise subgroup was characterized by lower late insulin and total insulin and C peptide responses, suggesting greater loss of insulin secretory ability. Peak glucose also differed between these two subgroups, being higher in the monophasic subgroup. Glucose acts not only to stimulate insulin secretion directly but can prime the β-cell to enhance subsequent insulin secretion.20 21 The higher responses in the monophasic subgroup may reflect an effect of higher peak glucose concentrations to potentiate late-phase insulin secretion or β-cells that are more responsive to the effects of potentiation. Consistent with our results, the TODAY study in youth with type 2 diabetes10 and the RISE study comparing youth and adults with impaired glucose tolerance (n=249 adults) or newly diagnosed type 2 diabetes (n=104 adults)16 both found that the continuous rise pattern was associated with the lowest β-cell function.
The continuous rise subgroup appears to have unique characteristics. The profiles for insulin and C peptide depicted in figure 1 suggest a ‘sluggish’ glucose response in those with a continuously rising glucose response curve. The rise in the glucose concentration, which acts as the stimulus for insulin secretion, also appears to be somewhat delayed, and the insulin and C peptide curves mimic the glucose response curve. While not tested in GRADE, one possible explanation for this delay could be that gastric emptying or glucose absorption is delayed. This hypothesis would need to be tested with studies designed to directly measure rates of glucose absorption.
The continuous rise glucose curve shape may identify a subgroup of individuals at higher risk of progression or who may respond differentially to specific treatment approaches. In youth with type 2 diabetes in the TODAY study, a pattern of a continuously rising glucose was associated with a higher HbA1c and lower late insulin and total insulin and C peptide responses, and presaged increased glycemic failure rates and accelerated deterioration of β-cell function.10 In RISE, progression from impaired glucose tolerance to diabetes or change in glycemic outcomes at 12 months did not differ by baseline glucose response curve categorization but may have been limited by the short follow-up time.16 Interestingly, progression from a biphasic to a monophasic and then ultimately to a continuous rise pattern along with corresponding decreasing β-cell function was also recently reported to occur during progression to type 1 diabetes in the TrialNet Pathway to Prevention study.22 Once GRADE is completed, we will be able to test a similar hypothesis in adults to determine if the continuous rise pattern identifies those at highest risk of progression and whether the biphasic pattern identifies those with more stable disease.
The biphasic glucose response pattern was uncommon, being present in only 5.5% of participants. These data are consistent with findings from a large population study in China in which only 3% of those with a diagnosis of type 2 diabetes had a multiphasic pattern based on a 3-hour OGTT.5 In populations without diabetes, biphasic or multiphasic curve shapes correlate with lower glucose values, higher insulin sensitivity and β-cell function,2–4 7 9 and lower risk of progression to diabetes23 and are present in a higher percentage of the population (20%–30% in adults). In GRADE, HbA1c and fasting glucose values were similar with the monophasic and continuous rise subgroups, but estimates of β-cell function were higher. The presence of the biphasic pattern within a small proportion of the diabetes population suggests that this may identify a subgroup that may differ in terms of pathophysiology and/or indicate a lower risk of progression.
The strengths of this study include the large multiethnic cohort of men and women with relatively early type 2 diabetes (<10 years) and use of OGTT to assess β-cell function. As all participants were treated with metformin alone for their diabetes, there was no confounding by use of other glucose-lowering medications. The study is generalizable to a large portion of the US population that has type 2 diabetes treated with metformin alone. Limitations include the cross-sectional analysis and the lack of more precise measures of insulin sensitivity and β-cell function.
In conclusion, this is the first large multiethnic cohort of adults with early type 2 diabetes to identify differences in OGTT glucose curve shape distribution by sex, race, and BMI and metabolic differences between the two most common curve shapes, monophasic and continuous rise. The continuous rise curve shape exhibited more advanced β-cell dysfunction and higher HbA1c compared with the monophasic subgroup and may serve as a biomarker for more advanced disease. Further mechanistic studies are needed to evaluate the metabolic processes underlying these differences. In the future, once GRADE is completed, analysis of GRADE outcome data will allow us to determine if these patterns predict differential progression and/or response to the four glucose-lowering therapies being studied.
bmjdrc-2021-002264supp002.pdf (164.2KB, pdf)
Acknowledgments
Educational materials have been provided by the National Diabetes Education Program. Material support in the form of donated medications and supplies has been provided by Becton, Dickinson and Company, Bristol-Myers Squibb, Merck, Novo Nordisk, Roche Diagnostics, and Sanofi.
Footnotes
Presented at: The abstract for this manuscript was presented at the American Diabetes Association’s 78th Scientific Sessions in Orlando, Florida, June 22–28, 2018.
Collaborators: The GRADE Research Group: JP Crandall, MD McKee, S Behringer-Massera, J Brown-Friday, E Xhori, K Ballentine-Cargill, S Duran, H Estrella, S Gonzalez de la torre, J Lukin, LS Phillips, E Burgess, D Olson, M Rhee, P Wilson, TS Raines, J Boers, J Costello, C Gullett, M Maher-Albertelli, R Mungara, L Savoye, CA White, L Holloway, F Morehead, S Person, M Sibymon, S Tanukonda, C Adams, A Ross, A Balasubramanyam, R Gaba, E Gonzalez, G Montes, C Wright, P Hollander, E Roe, A Jackson, A Smiley, P Burt, L Estrada, K Chionh, F Ismail-Beigi, C Falck-Ytter, L Sayyed Kassem, A Sood, M Tiktin, T Kulow, C Newman, KA Stancil, B Cramer, J Iacoboni, MV Kononets, C Sanders, L Tucker, A Werner, A Maxwell, G McPhee, C Patel, L Colosimo, A Krol, R Goland, J Pring, L Alfano, P Kringas, C Hausheer, J Tejada, K Gumpel, A Kirpitch, H Schneier, JB Green, H AbouAssi, R Chatterjee, MN Feinglos, J English Jones, SA Khan, JB Kimpel, RP Zimmer, M Furst, BM Satterwhite, K Evans Kreider, CR Thacker, CN Mariash, KJ Mather, A Lteif, M Mullen, T Hamilton, N Patel, G Riera, M Jackson, V Pirics, D Aguillar, D Howard, S Hurt, R Bergenstal, A Carlson, T Martens, M Johnson, R Hill, J Hyatt, C Jensen, M Madden, D Martin, H Willis, W Konerza, S Yang, K Kleeberger, R Passi, S Fortmann, M Herson, K Mularski, H Glauber, J Prihoda, B Ash, C Carlson, PA Ramey, E Schield, B Torgrimson-Ojerio, K Arnold, B Kauffman, E Panos, S Sahnow, K Bays, K Berame, J Cook, D Ghioni, J Gluth, K Schell, J Criscola, C Friason, S Jones, S Nazarov, J Barzilay, N Rassouli, R Puttnam, B Ojoawo, K Stokes, R Nelson, M Curtis, B Hollis, C Sanders-Jones, R Nelson, Z El-Haqq, A Kolli, T Tran, D Wexler, M Larkin, J Meigs, B Chambers, A Dushkin, G Rocchio, M Yepes, B Steiner, H Dulin, M Cayford, K Chu, A DeManbey, M Hillard, K Martin, N Thangthaeng, L Gurry, R Kochis, E Raymond, V Ripley, C Stevens, J Park, V Aroda, A Ghazi, Ann Ressing, A Loveland, M Hamm, M Hurtado, A Kuhn, F Mofor, R Garg, HJ Florez, WM Valencia, J Marks, S Casula, L Oropesa-Gonzalez, L Hue, AK Riccio Veliz, R Nieto-Martinez, M Gutt, A Ahmann, D Aby-Daniel, F Joarder, V Morimoto, C Sprague, D Yamashita, N Cady, N Rivera-Eschright, P Kirchhoff, B Morales Gomez, J Adducci, A Goncharova, SH Hox, H Petrovitch, M Matwichyna, V Jenkins, NO Bermudez, L Broadwater, RR Ishii, DS Hsia, WT Cefalu, FL Greenway, C Waguespack, E King, N Haynes, A Thomassie, B Bourgeois, C Hazlett, S Mudaliar, R Henry, S Boeder, J Pettus, E Diaz, D Garcia-Acosta, S Maggs, C DeLue, E Castro, S Hernandez, J Krakoff, JM Curtis, T Killean, M Khalid, E Joshevama, E Diaz, D Martin, K Tsingine, T Karshner, J Albu, FX Pi-Sunyer, S Frances, C Maggio, E Ellis, J Bastawrose, X Gong, MA Banerji, P August, M Lee, D Lorber, NM Brown, DH Josephson, LL Thomas, M Tsovian, A Cherian, MH Jacobson, MM Mishko, MS Kirkman, JB Buse, J Dostou, L Young, K Bergamo, A Goley, J Kerr, JF Largay, S Guarda, J Cuffee, D Culmer, R Fraser, H Almeida, S Coffer, E Debnam, L Kiker, S Morton, K Josey, G Fuller, WT Garvey, A Cherrington, D Golson, MC Robertson, O Griffith, A Agne, S McCullars, RM Cohen, J Craig, MC Rogge, K Burton, K Kersey, C Wilson, S Lipp, MB Vonder Meulen, N Rasouli, C Baker, E Schroeder, C Underkofler, R Lorch, S Douglass, S Steiner, W Sivitz, E Cline, L Knosp, J McConnell, T Lowe, WH Herman, R Pop-Busui, MH Tan, C Martin, A Waltje, A Katona, L Goodhall, R Eggleston, S Kuo, K Whitley, S Bule, N Kessler, E LaSalle, ER Seaquist, A Bantle, T Harindhanavudhi, A Kumar, B Redmon, J Bantle, M Coe, M Mech, A Taddese, L Lesne, S Smith, C Desouza, L Kuechenmeister, V Shivaswamy, AL Morales, MG Rodriguez, K Seipel, A Alfred, J Eggert, G Lord, W Taylor, R Tillson, DS Schade, A Adolphe, M Burge, E Duran-Valdez, J Martinez, S Kunkel, F Ali Jamaleddin Ahmad, D Hernandez McGinnis, B Pucchetti, E Scripsick, A Zamorano, RA DeFronzo, E Cersosimo, M Abdul-Ghani, C Triplitt, M Mullen, RI Garza, H Verastiqui, K Wright, C Puckett, P Raskin, C Rhee, S Abraham, LF Jordan, S Sao, L Morton, O Smith, L Osornio Walker, L Schnurr-Breen, R Ayala, RB Kraymer, D Sturgess, KM Utzschneider, SE Kahn, L Alarcon-Casas Wright, EJ Boyko, EC Tsai, DL Trence, BN Fattaleh, BK Montgomery, KM Atkinson, A Kozedub, T Concepcion, C Moak, N Prikhodko, S Rhothisen, TA Elasy, S Martin, L Shackelford, R Goidel, N Hinkle, C Lovell, J Myers, J Lipps Hogan, JB McGill, M Salam, T Schweiger, S Kissel, C Recklein, MJ Clifton, W Tamborlane, A Camp, B Gulanski, SE Inzucchi, K Pham, M Alguard, P Gatcomb, K Lessard, M Perez, L Iannone, E Magenheimer, A Montoza, W Cefalu, HB Burch, A Bremer, B Linder, J Fradkin, DM Nathan, JM Lachin, JB Buse, SE Kahn, H Krause-Steinrauf, M Larkin, M Tiktin, D Wexler, HB Burch, B Linder, A Bremer, JM Lachin, H Krause-Steinrauf, N Younes, M Backman, I Bebu, CJ Buys, A Fagan Murphy, Y Gao, MR Gramzinski, SD Hall, E Legowski, C Suratt, A Arey, J Bethepu, C Lund, P Mangat Dhaliwal, P McGee, E Mesimer, L Ngo, M Steffes, J Seegmiller, A Saenger, V Arends, D Gabrielson, T Conner, S Warren, J Day, A Scrymgeour, Y Pokharel, EZ Soliman, ZM Zhang, C Campbell, L Keasler, S Hensley, J Hu, Y Li, W Herman, C Martin, A Waltje, S Kuo, R Mihalcea, DJ Min, V Perez-Rosas, L Prosser, K Resnicow, W Ye, H Shao, P Zhang, J Luchsinger, D Sanchez, S Assuras, E Groessl, F Sakha, N Hillery, I Abdouch, P Brantley, FE Broyles, G Canaris, P Copeland, JJ Craine, WL Fein, MS Lee, R Meiners, V Meiners, H O’Neal, JE Park, E Sledge Jr, J Steppel-Resnick, A Turchin.
Contributors: KMU, SEK, and NR contributed to conception and design of research for the manuscript. JIB, EVG, KJM, and MAB contributed to acquisition of data for the manuscript. JML and NY contributed to statistical analysis for the manuscript. JIB, RMC, EVG, SEK, JML, KJM, KMU, FI-B, DJW, NY, NR, and KMU contributed to interpretation of data for the manuscript. JML contributed to acquisition of funding for this manuscript. EVG, JML, KJM, PR, MAB, and KMU contributed to supervision and management of research for the manuscript. JIB, KMU, NR, MAB, and NY contributed to drafting of the manuscript. RMC, EVG, SEK, JML, KJM, PR, KMU, FI-B, NR, and DJW contributed to critical review of the manuscript. NY is the guarantor of this work and as such had full access to all the data in the study and takes responsibility for the integrity and accuracy of the data.
Funding: GRADE is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health under Award Number U01-DK-098246. The planning of GRADE was supported by a U34 planning grant from the NIDDK (U34-DK-088043). The American Diabetes Association supported the initial planning meeting for the U34 proposal. The National Heart, Lung, and Blood Institute and the Centers for Disease Control and Prevention also provided funding support. The Department of Veterans Affairs provided resources and facilities. Additional support was provided by grant numbers P30 DK017047, P30 DK020541-44, P30 DK020572, P30 DK072476, P30 DK079626, P30 DK092926, U54 GM104940, UL1 TR000439, UL1 TR000445, UL1 TR001108, UL1 TR001409, UL1 TR001449, UL1 TR002243, UL1 TR002345, UL1 TR002378, UL1 TR002489, UL1 TR002529, UL1 TR002535, UL1 TR002537, UL1 TR001425, and UL1 TR002548.
Disclaimer: The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Competing interests: KMU reports support from Medtronic and personal fees from Novo Nordisk, outside the submitted work. NR reports grants and other support from Novo Nordisk, outside the submitted work. RMC reports grants from the National Institutes of Health during the conduct of the study, and other support from Bristol Myers Squibb and Pfizer, outside the submitted work. DJW reports grants from NIDDK which funded the trial during the conduct of the study and other support from Novo Nordisk, outside the submitted work. SEK reports grants from NIH during the conduct of the study, personal fees from Boehringer Ingelheim, personal fees from Eli Lilly and Company, and personal fees from Intarcia, Janssen, Merck, Neurimmune, Novo Nordisk, and Pfizer, outside the submitted work. KJM reports grants from the National Institutes of Health during the conduct of the study, and at the time of publication KJM is an employee of Eli Lilly and Company. Data collection, analysis, and preparation of the manuscript occurred prior to this employment and were independent of Eli Lilly and Company. NY, JIB, MAB, EVG, FI-B, JML, and PR have nothing to disclose. KMU and SEK are supported by funding from the US Department of Veterans Affairs.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
the GRADE Research Group:
JP Crandall, MD McKee, S Behringer-Massera, J Brown-Friday, E Xhori, K Ballentine-Cargill, S Duran, H Estrella, S Gonzalez de la torre, J Lukin, LS Phillips, E Burgess, D Olson, M Rhee, P Wilson, TS Raines, J Boers, J Costello, C Gullett, M Maher-Albertelli, R Mungara, L Savoye, CA White, L Holloway, F Morehead, S Person, M Sibymon, S Tanukonda, C Adams, A Ross, A Balasubramanyam, R Gaba, E Gonzalez, G Montes, C Wright, P Hollander, E Roe, A Jackson, A Smiley, P Burt, L Estrada, K Chionh, F Ismail-Beigi, C Falck-Ytter, L Sayyed Kassem, A Sood, M Tiktin, T Kulow, C Newman, KA Stancil, B Cramer, J Iacoboni, MV Kononets, C Sanders, L Tucker, A Werner, G McPhee AMaxwell, C Patel, L Colosimo, A Krol, R Goland, J Pring, L Alfano, P Kringas, C Hausheer, J Tejada, K Gumpel, A Kirpitch, H Schneier, JB Green, H AbouAssi, R Chatterjee, MN Feinglos, J English Jones, SA Khan, RP Zimmer, M Furst, BM Satterwhite, K Evans Kreider, CR Thacker, CN Mariash, KJ Mather, A Lteif, M Mullen, T Hamilton, N Patel, G Riera, M Jackson, V Pirics, D Aguillar, D Howard, S Hurt, R Bergenstal, A Carlson, T Martens, M Johnson, R Hill, J Hyatt, C Jensen, M Madden, D Martin, H Willis, W Konerza, S Yang, K Kleeberger, R Passi, S Fortmann, M Herson, K Mularski, H Glauber, J Prihoda, B Ash, C Carlson, PA Ramey, E Schield, B Torgrimson-Ojerio, K Arnold, B Kauffman, E Panos, S Sahnow, K Bays, K Berame, J Cook, D Ghioni, J Gluth, K Schell, J Criscola, C Friason, S Jones, S Nazarov, J Barzilay, N Rassouli, R Puttnam, B Ojoawo, K Stokes, R Nelson, M Curtis, B Hollis, C Sanders-Jones, R Nelson, Z El-Haqq, A Kolli, T Tran, D Wexler, M Larkin, J Meigs, B Chambers, A Dushkin, G Rocchio, M Yepes, B Steiner, H Dulin, M Cayford, K Chu, A DeManbey, M Hillard, K Martin, N Thangthaeng, L Gurry, R Kochis, E Raymond, V Ripley, C Stevens, J Park, V Aroda, A Ghazi, Ann Ressing, A Loveland, M Hamm, M Hurtado, A Kuhn, F Mofor, R Garg, HJ Florez, WM Valencia, J Marks, S Casula, L Oropesa-Gonzalez, L Hue, AK Riccio Veliz, R Nieto-Martinez, M Gutt, A Ahmann, D Aby-Daniel, F Joarder, V Morimoto, C Sprague, D Yamashita, N Cady, N Rivera-Eschright, P Kirchhoff, B Morales Gomez, J Adducci, A Goncharova, SH Hox, H Petrovitch, M Matwichyna, V Jenkins, NO Bermudez, L Broadwater, RR Ishii, DS Hsia, WT Cefalu, FL Greenway, C Waguespack, E King, N Haynes, A Thomassie, B Bourgeois, C Hazlett, S Mudaliar, R Henry, S Boeder, J Pettus, E Diaz, D Garcia-Acosta, S Maggs, C DeLue, E Castro, S Hernandez, J Krakoff, JM Curtis, T Killean, M Khalid, E Joshevama, E Diaz, D Martin, K Tsingine, T Karshner, J Albu, FX Pi-Sunyer, S Frances, C Maggio, E Ellis, J Bastawrose, X Gong, MA Banerji, M Lee, D Lorber, NM Brown, DH Josephson, LL Thomas, M Tsovian, A Cherian, MH Jacobson, MM Mishko, MS Kirkman, JB Buse, J Dostou, L Young, K Bergamo, A Goley, J Kerr, JF Largay, S Guarda, J Cuffee, D Culmer, R Fraser, H Almeida, S Coffer, E Debnam, L Kiker, S Morton, K Josey, G Fuller, WT Garvey, A Cherrington, D Golson, MC Robertson, A Agne, S McCullars, RM Cohen, J Craig, MC Rogge, K Kersey, C Wilson, S Lipp, MB Vonder Meulen, N Rasouli, C Baker, E Schroeder, C Underkofler, R Lorch, S Douglass, S Steiner, W Sivitz, E Cline, L Knosp, J McConnell, T Lowe, WH Herman, R Pop-Busui, MH Tan, C Martin, A Waltje, A Katona, L Goodhall, R Eggleston, S Kuo, K Whitley, S Bule, N Kessler, E LaSalle, ER Seaquist, A Bantle, T Harindhanavudhi, A Kumar, B Redmon, J Bantle, M Coe, M Mech, A Taddese, L Lesne, S Smith, C Desouza, L Kuechenmeister, V Shivaswamy, AL Morales, K Seipel, A Alfred, J Eggert, G Lord, W Taylor, R Tillson, DS Schade, A Adolphe, M Burge, E Duran-Valdez, J Martinez, S Kunkel, P August, MG Rodriguez, JB Kimpel, JB Kimpel, and O Griffith
Data availability statement
The Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) is being conducted with funding from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). This manuscript is based on the baseline (pretreatment) data from the 5047 participants enrolled into the study. These baseline data will be archived with the NIDDK data repository and will be available for sharing with other investigators upon publication. In accordance with the NIH Public Access Policy, we continue to provide all manuscripts to PubMed Central including this manuscript. GRADE has provided the protocols to the public through its public website (https://grade.bsc.gwu.edu/ancillary-study-info). GRADE abides by the NIDDK data sharing policy and implementation guidance as required by the NIH/NIDDK (https://repository.niddk.nih.gov/studies/grade).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Study protocols were approved by the institutional review board of each clinical center and participating center, and all participants provided written consent. GRADE is a multicenter RCT approved by over 30 institutional review boards, so it is not possible to cite all this information including approval numbers in the main text. The following is the primary review board submission information from the most recent annual renewal: The George Washington University, Office of Human Research - Institutional Review Board (IRB number: 071245; last approved: July 8, 2020, expires: August 23, 2021.
References
- 1.Manco M, Nolfe G, Pataky Z, et al. Shape of the OGTT glucose curve and risk of impaired glucose metabolism in the EGIR-RISC cohort. Metabolism 2017;70:42–50. 10.1016/j.metabol.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 2.Kanauchi M, Kimura K, Kanauchi K, et al. Beta-cell function and insulin sensitivity contribute to the shape of plasma glucose curve during an oral glucose tolerance test in non-diabetic individuals. Int J Clin Pract 2005;59:427–32. 10.1111/j.1368-5031.2005.00422.x [DOI] [PubMed] [Google Scholar]
- 3.Tschritter O, Fritsche A, Shirkavand F, et al. Assessing the shape of the glucose curve during an oral glucose tolerance test. Diabetes Care 2003;26:1026–33. 10.2337/diacare.26.4.1026 [DOI] [PubMed] [Google Scholar]
- 4.de Andrade Mesquita L, Pavan Antoniolli L, Cittolin-Santos GF, et al. Distinct metabolic profile according to the shape of the oral glucose tolerance test curve is related to whole glucose excursion: a cross-sectional study. BMC Endocr Disord 2018;18:56. 10.1186/s12902-018-0286-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng X, Yang N, Li Y, et al. The shape of the glucose response curve during an oral glucose tolerance test heralds β-cell function in a large Chinese population. BMC Endocr Disord 2019;19:119. 10.1186/s12902-019-0446-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tura A, Morbiducci U, Sbrignadello S, et al. Shape of glucose, insulin, C-peptide curves during a 3-H oral glucose tolerance test: any relationship with the degree of glucose tolerance? Am J Physiol Regul Integr Comp Physiol 2011;300:R941–8. 10.1152/ajpregu.00650.2010 [DOI] [PubMed] [Google Scholar]
- 7.Nolfe G, Spreghini MR, Sforza RW, et al. Beyond the morphology of the glucose curve following an oral glucose tolerance test in obese youth. Eur J Endocrinol 2012;166:107–14. 10.1530/EJE-11-0827 [DOI] [PubMed] [Google Scholar]
- 8.Kim JY, Michaliszyn SF, Nasr A, et al. The shape of the glucose response curve during an oral glucose tolerance test heralds biomarkers of type 2 diabetes risk in obese youth. Diabetes Care 2016;39:1431–9. 10.2337/dc16-0352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bervoets L, Mewis A, Massa G. The shape of the plasma glucose curve during an oral glucose tolerance test as an indicator of beta cell function and insulin sensitivity in end-pubertal obese girls. Horm Metab Res 2015;47:445–51. 10.1055/s-0034-1395551 [DOI] [PubMed] [Google Scholar]
- 10.Arslanian S, El Ghormli L, Young Kim J, et al. The shape of the glucose response curve during an oral glucose tolerance test: forerunner of heightened glycemic failure rates and accelerated decline in β-cell function in today. Diabetes Care 2019;42:164–72. 10.2337/dc18-1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care 2013;36:2254–61. 10.2337/dc13-0356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- 13.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care 2004;27:1487–95. 10.2337/diacare.27.6.1487 [DOI] [PubMed] [Google Scholar]
- 14.Breiman L, Friedman J, Olshen RA. Classification and regression trees: Wadsworth, 1984. [Google Scholar]
- 15.R Core Team . R: a language and environment for statistical computing: R Foundation of statistical computing; 2019, 2021. Available: https://www.R-project.org/ [Accessed 7 May 2021].
- 16.Arslanian SA, El Ghormli L, Kim JY, et al. OGTT glucose response curves, insulin sensitivity, and β-cell function in rise: comparison between youth and adults at randomization and in response to interventions to preserve β-cell function. Diabetes Care 2021;44:817–25. 10.2337/dc20-2134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC . National diabetes statistics report 2020 estimates of diabetes and its burden in the United States 2020 2021.
- 18.Bancks MP, Kershaw K, Carson AP, et al. Association of modifiable risk factors in young adulthood with racial disparity in incident type 2 diabetes during middle adulthood. JAMA 2017;318:2457–65. 10.1001/jama.2017.19546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguayo-Mazzucato C. Functional changes in beta cells during ageing and senescence. Diabetologia 2020;63:2022–9. 10.1007/s00125-020-05185-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grill V, Adamson U, Cerasi E. Immediate and time-dependent effects of glucose on insulin release from rat pancreatic tissue. Evidence for different mechanisms of action. J Clin Invest 1978;61:1034–43. 10.1172/JCI109002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cerasi E. Potentiation of insulin release by glucose in man I. Quantitative analysis of the enhancement of glucose-induced insulin secretion by pretreatment with glucose in normal subjects. Acta Endocrinol 1975;79:483–501. [PubMed] [Google Scholar]
- 22.Ismail HM, Cleves MA, Xu P, et al. The pathological evolution of glucose response curves during the progression to type 1 diabetes in the TrialNet pathway to prevention study. Diabetes Care 2020;43:2668–74. 10.2337/dc20-0701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdul-Ghani MA, Lyssenko V, Tuomi T, et al. The shape of plasma glucose concentration curve during OGTT predicts future risk of type 2 diabetes. Diabetes Metab Res Rev 2010;26:280–6. 10.1002/dmrr.1084 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2021-002264supp001.pdf (357.6KB, pdf)
bmjdrc-2021-002264supp002.pdf (164.2KB, pdf)
Data Availability Statement
The Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) is being conducted with funding from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). This manuscript is based on the baseline (pretreatment) data from the 5047 participants enrolled into the study. These baseline data will be archived with the NIDDK data repository and will be available for sharing with other investigators upon publication. In accordance with the NIH Public Access Policy, we continue to provide all manuscripts to PubMed Central including this manuscript. GRADE has provided the protocols to the public through its public website (https://grade.bsc.gwu.edu/ancillary-study-info). GRADE abides by the NIDDK data sharing policy and implementation guidance as required by the NIH/NIDDK (https://repository.niddk.nih.gov/studies/grade).