Abstract
Canalicular adenoma is a unique, rare, benign salivary gland neoplasm whose reported prevalence varies in different studies. According to literature, this neoplasm has a marked predilection to occur in the upper lip of elderly women. Histological features are usually distinctive and diagnostic. This neoplasm has good prognosis after conservative surgical management but the propensity of multifocal nature and recurrence of this lesion mandates regular follow-up. This case report illustrates the case of a canalicular adenoma in the palate in a 71-year-old male patient. Here, we discuss the differential diagnosis with a brief review of literature.
Keywords: dentistry and oral medicine, mouth
Background
Canalicular adenomas (CAs) are rare, benign salivary gland neoplasms which usually present as painless, freely movable submucosal mass, almost exclusively in the oral cavity of elderly people. Clinically, it can bear a resemblance to other salivary gland lesions like mucocele, mucous retention cyst or pleomorphic adenoma and non-salivary gland lesions like epidermoid cyst, nasolabial cysts, lipomas, benign peripheral nerve lesions, benign fibrous lesions, haemangioma or varix. Although this lesion has a predilection for upper lip, it can occasionally be found in other oral sites also.1 There have been many controversies regarding its origin and histologically this neoplasm is composed of cords or columns of cuboidal or columnar cells, usually with a connective tissue capsule and occasional small cystic spaces.1 2 Locally aggressive neoplasms like adenoid cystic carcinoma (ACC) and polymorphous adenocarcinoma (PAC) can display similar histological pattern and the multifocal nature of CA. This commands proper differentiation between these lesions failure of which can result in unwarranted extensive surgery and radiotherapy.3 Though histological features of CA are distinctive and diagnostic, immunohistochemical examination may be essential to differentiate it from other salivary gland neoplasms in ambiguous cases.4 5 This case is important because CAs are relatively rare, benign salivary gland neoplasm whose reported prevalence varies in different studies. In the present case, the lesion is in the palate which is a relatively rare site for the occurrence of CA. As per current literature where definite terminology of CA is given for the lesion in question, the prevalence is in the upper lip. We intend to highlight that CAs need to be included in the differential diagnosis of palatal nodular lesions and in case of ambiguity in diagnosis, immunohistochemical examination must be carried out. Though recurrence is rare multifocal nature of these lesions mandates regular follow-up.
Case presentation
A 71-year-old male patient reported with a painless nodule in the upper left back region of the roof of the mouth for 2 years. On eliciting the history, the patient revealed that the nodule was small when he noticed it initially and gradually progressed to the present size. The nodule was neither painful nor associated with any discharge or bleeding. The patient could not recollect any history of trauma to the area. The patient gave a history of extraction of upper left back tooth 1 month ago which was uneventful. Medical history revealed diabetes and hypertension for which the patient is undergoing treatment. His family history was unremarkable. No abnormalities were detected on extraoral examination. On intraoral examination, a well-defined, solitary, ovoid lesion, approximately 3×2 cm in size in greatest dimension was present at the junction of hard and soft palate, 4 mm from the crest of alveolar ridge on the palatal aspect of maxillary left third molar region. The overlying mucosa was intact. A network of interlacing capillaries was present on the surface (figure 1). The lesion was non-tender, soft to firm in consistency and compressible. No palpable bruit or pulsations felt. Hard tissue examination revealed multiple missing teeth and grade 1 mobility with respect to 27.
Figure 1.

Well-defined, solitary, ovoid lesion, at the junction of hard and soft palate with network of interlacing capillaries on the surface.
Investigations
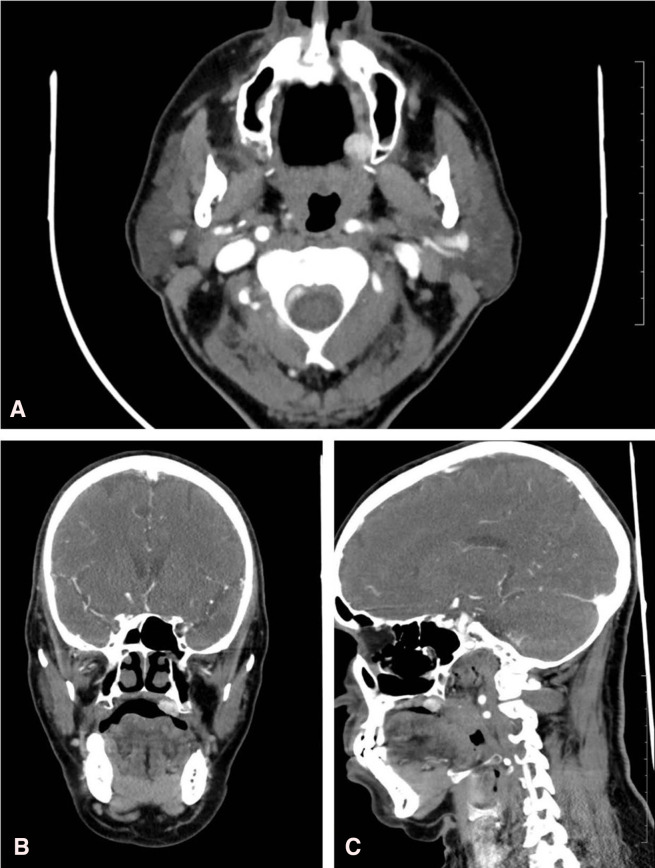
A head and neck CT scan with contrast was ordered. The imaging study revealed an intensely enhancing soft tissue density swelling in the hard palate at the junction of hard and soft palate on the left, probably haemangioma. No bony erosion was present (figure 2A–C). Since the patient was diabetic and hypertensive and under treatment for the same, endocrinologist’s opinion was taken regarding his fitness to undergo operative procedure under general anaesthesia. Preanaesthesia check-up was done. An excisional biopsy of the lesion was planned under general anaesthesia.
Figure 2.
(A) Axial CT image showing intensely enhancing soft-tissue density swelling in the hard palate at the junction of hard and soft palate on the left. (B) Coronal CT image showing intensely enhancing soft-tissue density swelling in the hard palate at the junction of hard and soft palate on the left. (C) Sagittal CT image showing intensely enhancing soft-tissue density swelling in the hard palate at the junction of hard and soft palate on the left.
Differential diagnosis
Based on the history and clinical findings, a clinical differential diagnosis of benign minor salivary gland neoplasm, possibly pleomorphic adenoma or vascular lesion like haemangioma was considered. Other possible differential diagnoses considered were solitary neurofibroma and non-odontogenic soft-tissue infection of the soft palate, possibly a palatal abscess.
Pleomorphic adenoma was considered because it is the most common benign minor salivary gland tumour and it usually presents as a slow growing, painless, firm, submucosal mass on the hard palate.6 The soft to firm consistency of the lesion was not agreeable with that of pleomorphic adenoma. This raised the suspicion that this lesion could be another minor salivary gland neoplasm also.
Haemangioma was included because though they are developmental in origin and often recognised at an early age, a neoplastic form may appear in the advanced age group. Though hard and soft palate involvement is rare, they can appear anywhere in the oral cavity.7 Moreover, in this case, the lesion presented with a network of interlacing capillaries on the surface and was compressible on palpation.
Isolated neurofibromas of the oral cavity presents as sessile or pedunculated, slow growing, painless, submucosal masses. Intraoral isolated neurofibromas are rare but when it occurs, tongue is the most common site involved. It may occur at any intraoral site including palate.8 Although the history and clinical presentation could suggest neurofibroma, this lesion being neurofibroma was less likely due to the presence of interlacing network of capillaries on the surface.
Non-odontogenic soft-tissue infection of the soft palate may present as a swelling but these lesions are classically tender, erythematous and poorly circumscribed. In the present case though the lesion was erythematous, it was non-tender, nodular, well-circumscribed and firm.9 These features along with the long duration of the lesion excluded the possibility of this lesion being a palatal abscess.
Therefore, taking into consideration the patient’s history and presenting features, our provisional diagnosis was that this lesion most probably represented a benign minor salivary gland neoplasm.
Treatment
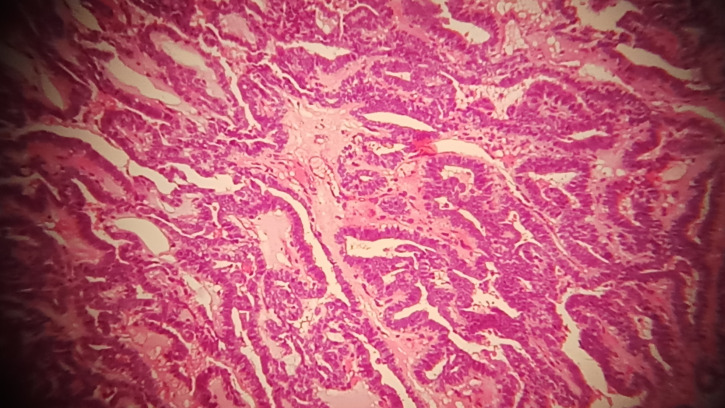
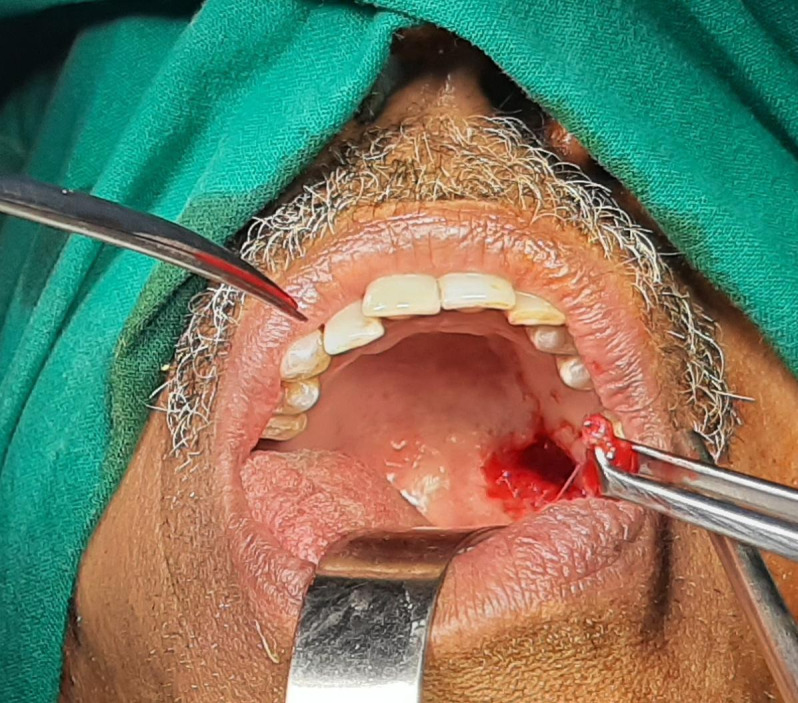
An excision biopsy of the lesion was performed under general anaesthesia. After standard betadine preparation and isolation, an incision was placed around the lesion with an anterior and posterior extension (figure 3). Lesion was undermined throughout, removed and sent for histopathological examination (figure 4). After achieving haemostasis, surgical site was closed with 3–0 Vicryl and packed with Surgicel. Histopathological examination of the excised lesion revealed connective tissue stroma showing a tumour consisting of strands of epithelium consisting of single layer of columnar cells with hyperchromatic nuclei surrounding luminal spaces. The luminal space contained eosinophilic secretory material. In adjacent areas, strands of epithelium giving a typical bilayered pattern was noticed (figure 5).
Figure 3.
Incision around the lesion with anterior and posterior extension.
Figure 4.
Surgical excision of the lesion.
Figure 5.
Photo micrograph showing strands of epithelium surrounding luminal spaces containing eosinophilic material within it. In areas, the adjacent strands of epithelium gives the typical bilayered pattern.
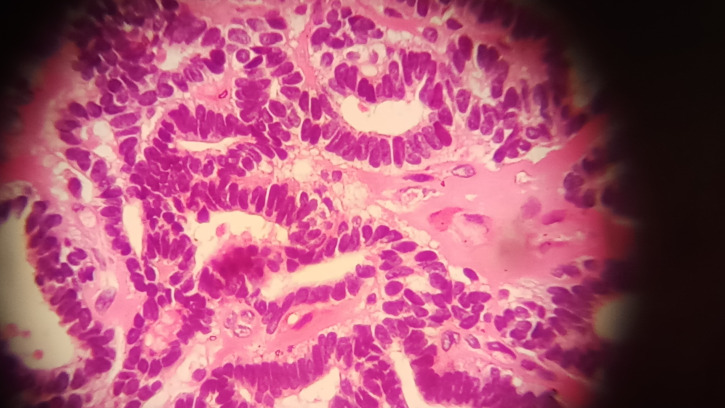
In the periphery numerous epithelial islands and small ductal spaces lined by cuboidal cells with hyperchromatic nuclei were noted. Connective tissue stroma between the tumour tissue was scanty and vascular. Areas of hyalinisation were noticed surrounding the tumour (figure 6). Lobules of normal mucous acini were seen associated with the lesional area. A diagnosis of CA was arrived at based on the histopathological findings. Immunohistochemistry needs to be done only in doubtful cases.
Figure 6.
Photomicrograph shows glandular epithelium consisting of columnar to cuboidal cells with hyperchromatic nuclei, surrounding luminal spaces. The intervening connective tissue stroma is scanty and shows vascular spaces and areas of hyalinisation.
Outcome and follow-up
The patient was recalled after a week for suture removal and postoperative evaluation. The postoperative period was uneventful and healing was found satisfactory (figure 7). The patient was reviewed on the 24th postoperative day and the healing was complete and the patient was kept under follow-up (figure 8).
Figure 7.

First follow-up after 1 week after removal of suture.
Figure 8.

Postoperative photograph on the 24th postoperative day showing complete healing of the lesion.
Discussion
CAs are unique, rare, benign salivary gland neoplasms with a predilection to occur in the elderly female population. There is a wide age range between 40and 90 years with the mean age of 70 years. There is a wide range of reported prevalence of this tumour. As per Thompson et al and Khodaei et al, it represents less than one percent of all salivary gland tumours.10 11 Peraza et al in a systematic review in 2017 reported the prevalence of CA as 1%–3% of all salivary gland tumours.4 According to Buchner et al, CAs constitute 10.3% of benign tumours.12 This disparity may be due to the sample size in different studies and also regional variations. Jones et al reported a prevalence of 4.7% of all salivary gland tumours and 7.3% of all benign tumours.13 This may be the most reliable one as it is a population based study.
The term ‘CA’ was used by Bhaskar and Weinmann to describe this neoplasm as it is now known, after reporting four cases of an intraoral benign salivary gland neoplasms.2 14 The definite differentiating feature suggested is that these kind of tumours do not show any myoepithelial cells separating it from benign mixed tumours.15 Earlier CA together with basal cell adenoma (BCA) was grouped as monomorphic adenoma to differentiate it from pleomorphic adenoma, but WHO classification of salivary gland neoplasms in 1992 considers these lesions as two different entities.16
Most of the minor salivary gland tumours are seen in the palate owing to the increased number of glands in this location unlike CA, which has a marked predilection for upper lip.
Other intraoral sites like buccal mucosa, palate, pharynx and rarely parotid gland can also be involved.1 3 Palatal presentation of this lesion is estimated to be ranging from 3% to 20%.17 Three cases of intramandibular CAs have also been reported.18 Our patient was an elderly male and the lesion was located in the palate. CAs usually present as painless, slow growing, movable, enlarging nodule. The consistency of these lesions ranges from firm to fluctuant. The surface of these tumours can be ulcerated or non-ulcerated. They may also show haemorrhage, inflammation, pigmentation and mucous extravasation.17 Rarely the lesions arising in the palate can present with extensive ulceration, necrosis and bluish and erythematous discolouration. Benign tumours of the palate may compress vascular structures leading to necrosis.19 The clinical features in our patient were consistent with those in literature and made us consider that the lesion is more of a benign nature than malignant. The clinical features that support us to categorise between benign and malignant minor salivary gland tumours are that the malignant lesions show fast growth, pain, ulceration, bleeding, adherence to superficial or deep structures, lymphadenopathy, etc.20 Our patient did not present with any of these features.
Initially, CAs were thought to be of terminal duct origin. There have been many controversies regarding this and an origin from terminal cells of intercalated duct have also been reported.2 10 Histologically, this lesion is made up of cords or columns of cuboidal or columnar cells, usually with a connective tissue capsule. Occasional small cystic spaces are seen.1
Rarely, CAs can present as multifocal lesions clinically and histologically which makes it distinct from other intraoral salivary gland tumours. Multifocal lesions constitute 10% of CAs and can vary from a second tumour mass to over 20 separate tumours and was mentioned as adenomatosis by some authors. According to their growth pattern, the multifocal variants can be categorised as clinical, microscopic and recurrent patterns.3 4 21
BCA is a benign lesion that should be considered in the differential diagnosis of CA. The age of onset, the location of the lesion and the histological features helps differentiate BCA from CA. CA generally occurs in elderly patients. BCA usually arises in major salivary glands when compared with CA.22 BCA has a general propensity to present two different cell types with the development of ductal structures. Ultrastructurally, an excretory duct origin has been indicated for CA although an origin from intercalated duct has also been reported. On the contrary a myoepithelial or intercalated duct lineage is indicted for BCA.2
ACC and PAC are two locally aggressive malignant neoplasms that can display similar histological pattern and multifocal nature to that of CAs. PAC was previously referred to as polymorphous low-grade adenocarcinoma but the recent WHO classification of salivary gland tumours mentions to it as PAC. This mandates proper differentiation between these lesions, failure of which can result in unwarranted extensive surgery and radiotherapy.23 24 Infiltrative nature, perineural invasion, avascularity of the cribriform component, uniformly cuboidal cells with angular nuclei and clear cytoplasm, strong expression of carcinoembryonic antigen and epithelial membrane antigen immunohistochemically, all helps differentiate ACC from CA. PAC can be differentiated from CA by the presence of round to oval neoplastic cells with vesicular nuclei surrounded by mucohyaline connective tissue, perineural and intraneural neurotropism, etc.22 25
Histological features of CA are usually distinctive and diagnostic. Since CAs display distinct immunochemical activity, in uncertain cases, immunohistochemical examination using cytokeratins 13 and 14, vimentin and alpha smooth muscle actin may be essential to differentiate it from other salivary gland neoplasms.4 5
Standard treatment is surgical removal. There are reports of cases of upper lip and buccal mucosa treated by enucleation. Recurrences are rare and is reported to be only 5% in patients treated by surgical excision.4 A case of synchronous bilateral multifocal CA of nasolabial wrinkle of the nose which recurred 1 year after surgical excision was reported by Mansueto et al.5 The recurrent tumours probably signify growth of microscopic foci which persisted subsequent to removal of clinically apparent larger lesions.3 4
Patient’s perspective.
I am relieved of my long-term fear of this lump being a cancer. Even though I did not have much problem during eating, swallowing and speaking earlier, I feel much better now after removing this lump
Learning points.
Though rare, palatal canalicular adenomas (CAs) should be part of differential diagnosis of palatal nodular lesions.
Multifocal CAs can be misdiagnosed as malignant salivary gland neoplasms like adenoid cystic carcinoma (ACC) and polymorphous adenocarcinoma (PAC).
Immunohistochemical analysis is important to differentiate CA from other malignant salivary gland neoplasms like ACC and PAC.
Regular follow-ups of these lesions are mandatory as any residual microscopic foci can lead to recurrence particularly in case of multifocal lesions.
Footnotes
Contributors: Substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work: PKN, BRV, RV and MJ. Drafting the work or revising it critically for important intellectual content: PKN, BRV, RV and MJ. Final approval of the version to be published: PKN, BRV, RV and MJ. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: PKN, BRV, RV and MJ.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Daley TD. The canalicular adenoma: considerations on differential diagnosis and treatment. J Oral Maxillofac Surg 1984;42:728–30. 10.1016/0278-2391(84)90421-X [DOI] [PubMed] [Google Scholar]
- 2.Machado de Sousa SO, Soares de Araújo N, Corrêa L, et al. Immunohistochemical aspects of basal cell adenoma and canalicular adenoma of salivary glands. Oral Oncol 2001;37:365–8. 10.1016/S1368-8375(00)00086-5 [DOI] [PubMed] [Google Scholar]
- 3.Samar ME, Avila RE, Fonseca IB, et al. Multifocal canalicular adenoma of the minor labial salivary glands. Int J Clin Exp Pathol 2014;7:8205–10. [PMC free article] [PubMed] [Google Scholar]
- 4.Peraza AJ, Wright J, Gómez R. Canalicular adenoma: a systematic review. J Craniomaxillofac Surg 2017;45:1754–8. 10.1016/j.jcms.2017.07.020 [DOI] [PubMed] [Google Scholar]
- 5.Mansueto G, Falleti J, De Cecio R, et al. Synchronous bilateral multifocal canalicular adenoma: a case report of an unusual finding. Clin Exp Dermatol 2009;34:e587–9. 10.1111/j.1365-2230.2009.03258.x [DOI] [PubMed] [Google Scholar]
- 6.Patigaroo SA, Patigaroo FA, Ashraf J, et al. Pleomorphic adenoma of hard palate: an experience. J Maxillofac Oral Surg 2014;13:36–41. 10.1007/s12663-012-0448-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh P, Parihar AS, Siddique SN, et al. Capillary haemangioma on the palate: a diagnostic conundrum. BMJ Case Rep 2016;2016:bcr2015210948. 10.1136/bcr-2015-210948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kodiya AM, Ngamdu YB, Sandabe MB, et al. Solitary isolated neurofibroma of the soft palate. J Surg Case Rep 2013;2013:rjs029. 10.1093/jscr/rjs029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D'Silva NJ, Benian R, Flint A, et al. Soft tissue swelling of the upper lip. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:271–3. 10.1016/j.tripleo.2007.08.037 [DOI] [PubMed] [Google Scholar]
- 10.Thompson LDR, Bauer JL, Chiosea S, et al. Canalicular adenoma: a clinicopathologic and immunohistochemical analysis of 67 cases with a review of the literature. Head Neck Pathol 2015;9:181–95. 10.1007/s12105-014-0560-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khodaei M, Amani M, Mirinezhad S, et al. Canalicular adenoma of the hard palate: a rare case report. Dent Res J 2021;18:15. [PMC free article] [PubMed] [Google Scholar]
- 12.Buchner A, Merrell PW, Carpenter WM. Relative frequency of intra-oral minor salivary gland tumors: a study of 380 cases from Northern California and comparison to reports from other parts of the world. J Oral Pathol Med 2007;36:207–14. 10.1111/j.1600-0714.2007.00522.x [DOI] [PubMed] [Google Scholar]
- 13.Jones AV, Craig GT, Speight PM, et al. The range and demographics of salivary gland tumours diagnosed in a UK population. Oral Oncol 2008;44:407–17. 10.1016/j.oraloncology.2007.05.010 [DOI] [PubMed] [Google Scholar]
- 14.Bhaskar SN, Weinmann JP. Tumors of the minor salivary glands; a study of twenty-three cases. Oral Surg Oral Med Oral Pathol 1955;8:1278–97. 10.1016/0030-4220(55)90433-3 [DOI] [PubMed] [Google Scholar]
- 15.Min BH, Miller AS, Leifer C, et al. Basal cell adenoma of the parotid gland. Archives of Otolaryngology - Head and Neck Surgery 1974;99:88–93. 10.1001/archotol.1974.00780030094003 [DOI] [PubMed] [Google Scholar]
- 16.Barnes L, Eveson JW, Reichart P. World Health Organization classification of tumours. Pathology & genetics. Head and neck tumours. Lyon: IARC Press, 2005. [Google Scholar]
- 17.Smullin SE, Fielding AF, Susarla SM, et al. Canalicular adenoma of the palate: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:32–6. 10.1016/j.tripleo.2004.02.065 [DOI] [PubMed] [Google Scholar]
- 18.Dayisoylu EH, Pampu AA, Mungan S, et al. Intra-mandibular canalicular adenoma: report of a rare case. J Pak Med Assoc 2012;62:1239–41. [PubMed] [Google Scholar]
- 19.Allen CM, Damm D, Neville B, et al. Necrosis in benign salivary gland neoplasms. Oral Surg Oral Med Oral Pathol 1994;78:455–61. 10.1016/0030-4220(94)90038-8 [DOI] [PubMed] [Google Scholar]
- 20.Pons Vicente O, Almendros Marqués N, Berini Aytés L, et al. Minor salivary gland tumors: a clinicopathological study of 18 cases. Med Oral Patol Oral Cir Bucal 2008;13:E582–8. [PubMed] [Google Scholar]
- 21.Rousseau A, Mock D, Dover DG, et al. Multiple canalicular adenomasA case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology 1999;87:346–50. 10.1016/S1079-2104(99)70221-0 [DOI] [PubMed] [Google Scholar]
- 22.Siqueira CS, Fernandes KS, Vivas APM, et al. Clinical and histological features of multifocal canalicular adenomas of the upper lip. Braz Dent J 2013;24:542–6. 10.1590/0103-6440201302264 [DOI] [PubMed] [Google Scholar]
- 23.Coca-Pelaz A, Rodrigo JP, Bradley PJ, et al. Adenoid cystic carcinoma of the head and neck–an update. Oral Oncol 2015;51:652–61. 10.1016/j.oraloncology.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 24.Vander Poorten V, Triantafyllou A, Skálová A, et al. Polymorphous adenocarcinoma of the salivary glands: reappraisal and update. Eur Arch Otorhinolaryngol 2018;275:1681–95. 10.1007/s00405-018-4985-5 [DOI] [PubMed] [Google Scholar]
- 25.Suarez P, Hammond HL, Luna MA, et al. Palatal canalicular adenoma: report of 12 cases and review of the literature. Ann Diagn Pathol 1998;2:224–8. 10.1016/S1092-9134(98)80011-7 [DOI] [PubMed] [Google Scholar]