Abstract
Objectives
To assess the health utilisation status and associated factors among African migrants in China.
Design
A national cross-sectional study was conducted among African migrants in China in 2019.
Setting
Participants were recruited online and offline to participate in a self-report survey. Online participants were recruited through WeChat across China, and offline participants were recruited in Guangzhou.
Participants
We recruited participants who were from an African country; had spent at least 1 month cumulatively in China; were at least 18 years old; were willing to provide informed consent. A total of 1025 participants were recruited online and offline, 19 of them were excluded due to invalid response and 1006 people were finally included in the analysis.
Outcome measures
The primary outcome was health service utilisation and associated factors among African migrants during their stay in China in the past 12 months. The potential factors include the predisposing factors (demographic characteristics and social structure variables), enabling factors (annual income, health insurance in China) and need factors (non-communicable chronic and infectious diseases, depression) which determined by Anderson framework were measured.
Results
Eight hundred and seven online and 218 offline participants completed the survey, including 624 males and 382 females, with an average age of 26.4±8.9 years. Around 28.5% reported health utilization in the past 12 months. Results showed that longer duration in China, migration to China for business (aOR=2.23, 95% CI:1.13-4.40) and study (aOR=5.00, 95% CI:2.74-9.11), living in apartment (aOR=2.59, 95% CI:1.62-4.14) or dormitory (aOR=3.22, 95% CI:2.17-4.80) in China, suffering from chronic diseases, communicable diseases, and greater depressive symptoms (aOR=1.91, 95% CI:1.42-2.56) facilitated health service utilization.
Conclusions
The healthcare service that African migrants received in China is low. The existing public health policies and intervention measures need to be improved to make health utilisation more accessible and feasible for African migrants.
Keywords: health services administration & management, international health services, epidemiology, public health
Strengths and limitations of this study.
The study is one of the few studies that examined the healthcare utilisation rate and associated factors among African migrants in China on a large scale.
Andersen’s behavioural model was applied to determine the influencing factors of healthcare utilisation among Africans in China.
The sampling method may be biased, which might affect the representativeness and generalisability of this study.
The cross-sectional design did not allow the estimation of causal relationships between influencing factors and healthcare utilisation.
Introduction
African migrants in China refer to people who are citizens of African countries or who consider themselves to be from Africa or of African origin and who reside in or visit mainland China, Hong Kong, Macau or Taiwan1. The number of African migrants in China increased rapidly in recent years due to closer economic cooperation and enhanced educational opportunities for Africans in China.2 China has been Africa’s largest trading partner since 2009, surpassing the USA and Europe.3 Approximately 400 000–500 000 African migrants live in China in any 12 calendar months.4 Except for business purposes, China has become a new burgeoning destination for African students in recent years, with about 50 000 African students studying in China.5 According to China’s exit and entry administration law, foreigners who have made outstanding contributions to China’s economic and social development, or meet other requirements can apply for permanent residence qualification.6 Africans migrate to China for different purposes, such as business, study, work or visiting relatives. Most Africans in Beijing are students, diplomats and travellers; most Africans in Shanghai are students, employees of multinational companies and financial practitioners; Africans in Guangzhou, Foshan, Yiwu tend to engage in import and export trade business.7
African migrants often encounter more barriers to health access than local residents in China,8 which makes them more vulnerable to infectious diseases and lower quality of life.9 According to a previous survey, 10.6% of African migrants in China reported health problems, while only 32.7% of them have medical insurance10; the extra medical burden may decrease their willingness to seek medical services in China. Moreover, a higher prevalence of hypertension and diabetes was detected in this group compared with local people, despite being relatively younger on average.11 Thus, health promotion among African migrants in China is an urgent public health priority.
There are unique challenges to improving migrant health in China. China is a traditional non-immigrant country. As such, there are insufficient medical resources tailored to international migrants.12 Many barriers exist and impede their utilisation of health services, such as language, culture and religious differences, in addition to discrimination from residents.13 14 Chinese doctors have few experiences in diagnosing and treating specific diseases affecting Africans, and translation services are mostly unavailable.15 For those who received medical services from hospitals, most rely on emergency care. The private clinics and drugstores are their primary sources of medical care in China.16
Nowadays, African migrants have resided in many Chinese cities, while most existing studies focused on Guangzhou and Yiwu.13 14 16 17 Few studies explored the factors that influence healthcare utilisation on a national scale. Andersen’s behavioural model is the most frequently used tool for identifying factors associated with health service use.18 This study used Andersen’s behavioural model to quantify the health service utilisation and correlates among African migrants in China.
Methods
Study design and participants
This population-based cross-sectional survey was conducted from August to November 2019, using online and offline methods. The online survey was implemented nationwide, and an electronic survey platform (Wenjuanxing, Changsha Ranxing Information Technology, Changsha, China) was used to create the survey link. The survey link was spread via WeChat (the most widely used social media platform in China). We restricted participation to one WeChat account and one mobile phone to avoid duplicate participation. For the offline part, a venue-based survey was implemented in Guangzhou. Guangzhou has the largest African migrant population in China, including over 15 000 registered Africans and thousands of African immigrants without a current visa (without an exact number).7 Most of them are businessmen, and few of them are interested in the online survey according to our fieldwork experiences. International health clinics, restaurants, bars and freight corporations serving African migrants in the Sanyuanli neighbourhood were selected as different recruitment sites.
Inclusion criteria of participants were: originally from an African country, defined by nationality; had spent at least 1 month cumulatively in China; at least 18 years old; willing to provide informed consent.
Data collection
Anonymous questionnaires in English, French and Chinese were available for both online and offline survey participants. The questionnaire was constructed based on the research group’s literature review and fieldwork experiences and modified by experts of African migrant research. Before the formal survey, we have invited three community leaders from active African communities (countries: Nigeria, Ghana and Zimbabwe) in Guangzhou to test the questionnaire and revised it according to their suggestions. The snowball sampling method was used for online survey recruitment. The community leaders sent the survey link to their family members and friends eligible for this survey through WeChat. The online survey was self-administered. Participants completed and submitted questionnaires on their smartphones by clicking the survey link, and they were then encouraged to recruit other eligible individuals. An online consent form was provided to the online participants. The survey would not continue unless the participants chose the option-‘Yes, I have read the information and agree to take the survey.’ Participants would receive US$3.0 for the questionnaire completion. An extra US$1.5 would be given for each effective referral defined by the successful survey completion and submission as incentives.
Participants of the offline survey were organised by a trained research team member who has served African migrants for years in African communities. International health clinics, restaurants, bars and freight corporations were selected to recruit and conduct face-to-face questionnaire surveys. Eligible participants were identified by their appearance; the workers and volunteers in the study sites would help to approach the participants. The investigator would briefly introduce the research purpose and questionnaire contents first, and the participants need to provide written informed consent if he (she) was willing to join. The investigator asked each question and filled the questionnaire according to participants’ answers. About US$3.0 would be provided to participants who finished the questionnaire.
Outcome measures
The primary outcome was health service utilisation rate among African migrants, defined as the participants who received medical services (outpatient or inpatient) in China in the past 12 months.
The analytical framework was based on Andersen’s behavioural model mainly used for the analysis of healthcare utilisation, including three elements, predisposing, enabling and need.18 Predisposing factors, presenting one’s predisposition to use health service, consisted of demographic characteristics, including gender, age, marriage, educational level and purpose of travel; social structure variables, including religious belief, the region of the origin country, duration in China from the last entrance, attitudes of the locals, the living arrangement in China and satisfaction with housing condition. Factors that enable or impede the use of health services were defined as enabling factors, including annual income and health insurance in China. The need factor refers to the need for health service, including lifetime diagnoses of diseases, infectious diseases in the past year and depression status.
We measured depression among African migrants using the Centre for Epidemiologic Studies Depression Scale, which is a self-report measure of depressive symptomatology in the general population. The English,19 French20 and Chinese21 validated versions were available for researchers. The scale includes 20 items answered on a Likert-type scale between 0 and 3. The total score ranges from 0 to 60, with a higher score indicating more severe depression symptoms. Participants who scored 16 or above would be considered depressed.
Statistical analyses
Data from the online investigation were downloaded from the Wenjuanxing platform. Information from the offline questionnaires was collected in a dual input format to Epidata V.3.1 and then exported and merged with data obtained online. The merged data were transferred to a secured server at Dermatology Hospital of Southern Medical University at the end of the research. The server was configured with a redundant hard drive array to ensure reliability. Access to the data will be password protected within the server’s firewall. All the data were analysed by IBM SPSS V.24.0 (IBM). Demographic characteristics were presented according to the distribution of the data. Logistic regression modelling was conducted to examine the associations between predisposing, enabling and needs factors. Potential confounding variables were adjusted in multivariable logistic regression models, including recruitment, age, sex, marital status and annual income. Both crude ORs and adjusted ORs (aORs) with 95% CI were reported, and variables with statistical significance in the logistic regression model were presented. A p value of less than 0.05 was considered statistically significant.
Patient and public involvement
This cross-sectional study among healthy people did not involve patients as subjects. In our follow-up studies to promote health service utilisation, we will inform the surveyed populations of the current results. Our research results will also be published and reported in English journals and international academic conferences.
Results
Sociodemographic characteristics of participants
A total of 1025 participants were recruited in this survey, including 807 online and 218 offline. Three participants declined to provide informed consent, 4 reported cumulative residence in China for less than 1 month and 12 submitted invalid questionnaires. Finally, 1006 people (799 online and 207 offline) were included in the analysis, and 287 (28.5%) participants reported health service utilisation in the past 12 months.
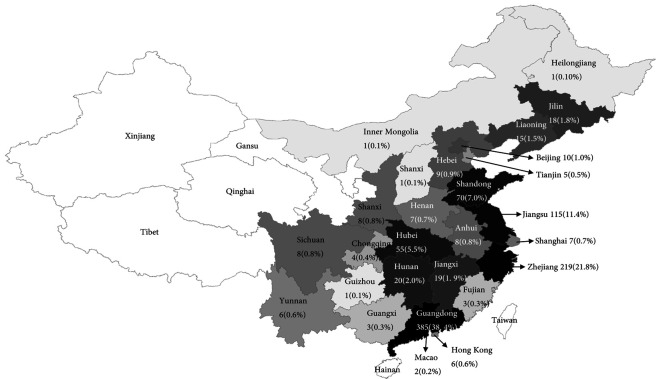
Participants came from 74 cities of 27 provinces and districts in China. They commonly resided in the provinces of Guangdong (385/1006, 38.4%), Zhejiang (219/1006, 21.8%) and Jiangsu (115/1006, 11.4%) (figure 1). The average age of participants was 26.4±8.9 years, and most of them were aged 18–24 years (61.6%), male (62.0%) and never married and not cohabited (77.7%). About 56.7% got a college education, and 36.9% had an annual income of more than US$2000. A total of 745 (74.1%) participants reported themselves as Christian (table 1).
Figure 1.
The geographical distribution of participants.
Table 1.
Demographic characteristics of participants
| Variable | Total (n=1006) |
Health utilisation | P value | |
| Yes (n=287) |
No (n=719) |
|||
| Recruitment | <0.001 | |||
| Online | 799 (79.4) | 191 (66.6) | 608 (84.6) | |
| Offline | 207 (20.6) | 96 (33.4) | 111 (15.4) | |
| Gender | 0.668 | |||
| Male | 624 (62.0) | 181 (63.1) | 443 (61.6) | |
| Female | 382 (38.0) | 106 (36.9) | 276 (38.4) | |
| Age | <0.001 | |||
| 18–24 years | 610 (61.6) | 144 (50.9) | 466 (65.9) | |
| 25–39 years | 285 (28.8) | 87 (30.7) | 198 (28.0) | |
| 40 years | 95 (9.6) | 52 (18.4) | 43 (6.1) | |
| Marriage | <0.001 | |||
| Never married and not cohabitating | 782 (77.7) | 186 (64.8) | 596 (82.9) | |
| Never married but cohabitating | 74 (7.4) | 29 (10.1) | 45 (6.3) | |
| Married | 150 (14.9) | 72 (25.1) | 78 (10.8) | |
| Education level | 0.031 | |||
| <High school | 67 (6.7) | 27 (9.4) | 40 (5.6) | |
| High school | 306 (30.4) | 97 (33.8) | 209 (29.1) | |
| College | 570 (56.7) | 149 (51.9) | 421 (58.6) | |
| >College | 63 (6.3) | 14 (4.9) | 49 (6.8) | |
| Annual income | <0.001 | |||
| Below US$2000 | 635 (63.1) | 144 (50.2) | 491 (68.5) | |
| US$2000–US$5000 | 144 (14.3) | 48 (16.7) | 96 (13.4) | |
| US$5000–US$10 000 | 121 (12.1) | 51 (17.8) | 70 (9.8) | |
| US$10 000 | 104 (10.4)) | 44 (15.3) | 60 (8.4) | |
| Religious belief | 0.033 | |||
| Christianity | 745 (74.1) | 196 (68.5) | 549 (76.4) | |
| Islam | 123 (12.2) | 43 (15.0) | 80 (11.1) | |
| None | 111 (11.0) | 35 (12.2) | 76 (10.6) | |
| Others | 26 (2.7) | 12 (4.2) | 14 (1.9) | |
Migration-related characteristics of participants
About 731 (72.7%) participants have medical insurance while staying in China. Over half (51.7%) of the participants came from Eastern Africa. About 34.1% of the sample stayed in China for over 1 year from their last entrance. The primary purposes of staying in China were study (42.7%) and business (30.6%). Hotels (37.5%) and staff/student dormitories (37.2%) were the most popular living places during their staying in China, and more than half of them felt satisfied (59.7%) about their housing condition. Most participants felt an attitude of friendly (42.0%) and neutral (38.7%) from the local residents (table 2).
Table 2.
Migration-related characteristics of participants
| Variable | Total (n=1006) |
Health utilisation | P value | |
| Yes (n=287) |
No (n=719) |
|||
| Medical insurance in China | <0.001 | |||
| Yes | 731 (72.7) | 178 (62.2) | 553 (77.2) | |
| No | 271 (26.9) | 108 (37.8) | 163 (22.8) | |
| Region of the origin country | <0.001 | |||
| Western Africa | 300 (29.8) | 79 (28.0) | 221 (30.8) | |
| Southern Africa | 53 (5.3) | 8 (2.8) | 45 (6.3) | |
| Northern Africa | 78 (7.8) | 18 (6.4) | 60 (8.4) | |
| Eastern Africa | 520 (52.1) | 150 (53.2) | 370 (51.6) | |
| Central Africa | 48 (4.8) | 27 (9.6) | 21 (2.9) | |
| Duration of stay in China from the last entrance | <0.001 | |||
| Less than 1 week | 162 (16.1) | 15 (5.2) | 147 (20.5) | |
| 2 weeks to 1 month | 187 (18.6) | 51 (17.8) | 136 (19.0) | |
| 2–6 months | 156 (15.5) | 45 (15.7) | 111 (15.5) | |
| 7–12 months | 156 (15.5) | 51 (17.8) | 105 (14.6) | |
| Over 1 year | 342 (34.1) | 124 (43.4) | 218 (30.4) | |
| Purpose of travel | <0.001 | |||
| Tourism | 141 (14.0) | 14 (4.9) | 127 (17.7) | |
| Business | 308 (30.6) | 109 (38.1) | 199 (27.7) | |
| Study | 430 (42.7) | 141 (49.3) | 289 (40.2) | |
| Other | 126 (12.5) | 22 (7.7) | 104 (14.5) | |
| Attitudes of the locals | 0.048 | |||
| Not friendly or very unfriendly | 78 (7.8) | 31 (10.8) | 47 (6.5) | |
| Neutral | 389 (38.7) | 101 (35.2) | 288 (40.1) | |
| Friendly or very friendly | 539 (53.6) | 155 (54.0) | 384 (53.4) | |
| Living arrangement in China | <0.001 | |||
| Hotel | 377 (37.5) | 85 (29.7) | 292 (40.7) | |
| Guest apartment | 54 (5.4) | 14 (4.9) | 40 (5.6) | |
| Rental apartment | 137 (13.7) | 55 (19.2) | 82 (11.4) | |
| Staff/student dormitory | 374 (37.2) | 121 (42.3) | 253 (35.3) | |
| Others | 61 (6.1) | 11 (3.8) | 50 (7.0) | |
| Satisfaction with housing condition | 0.158 | |||
| Very unsatisfied | 36 (3.6) | 14 (4.9) | 22 (3.1) | |
| Unsatisfied | 50 (5.0) | 18 (6.3) | 32 (4.5) | |
| Neither unsatisfied nor satisfied | 212 (21.1) | 49 (17.1) | 163 (22.7) | |
| Satisfied | 601 (59.7) | 173 (60.3) | 428 (59.5) | |
| Very satisfied | 107 (10.6) | 33 (11.5) | 74 (10.3) | |
Physical and psychological health status of participants
Among the participants, there are 47 (4.7%) ever diagnosed with hypertension, 33 (3.3%) with asthma, 30 (3.0%) with cardiovascular diseases, 28 (2.8%) ever infected with past skin diseases patients and another 28 (2.5%) reporting HIV/sexually transmitted infections (STIs). In the past year, 337 (33.5%) participants were infected with influenza, 34 (3.4%) got typhoid fever, 19 (1.9%) got infectious diarrhoea, and 8 (0.8%) reported tuberculosis. A total of 454 (45.4%) participants met the clinical indication for depression (table 3).
Table 3.
Physical and psychological health status of participants
| Variable | Total | Health utilisation | P value | |
| Yes n (%) | No n (%) | |||
| Diseases ever been diagnosed | ||||
| Hypertension | 47 (4.7) | 32 (11.1) | 15 (2.1) | <0.001 |
| Diabetes | 25 (2.5) | 13 (4.5) | 12 (1.7) | 0.008 |
| Asthma | 33 (3.3) | 13 (4.5) | 20 (2.8) | 0.160 |
| Cardiovascular diseases | 30 (3.0) | 19 (6.6) | 11 (1.5) | <0.001 |
| Hyperlipidaemia | 23 (2.3) | 9 (3.1) | 14 (1.9) | 0.255 |
| Skin disease | 28 (2.8) | 14 (4.9) | 14 (1.9) | 0.011 |
| Cerebrovascular disease | 17 (1.7) | 12 (4.2) | 5 (0.7) | <0.001 |
| HIV/STIs | 28 (2.8) | 19 (6.6) | 20 (2.8) | <0.001 |
| Diseases infected in the past year | ||||
| Influenza | 337 (33.5) | 102 (35.7) | 235 (32.8) | 0.382 |
| Tuberculosis | 8 (0.8) | 7 (2.4) | 1 (0.1) | 0.001 |
| Typhoid fever | 34 (3.4) | 15 (5.2) | 19 (2.6) | 0.040 |
| Infectious diarrhoea | 19 (1.9) | 11 (3.8) | 8 (1.1) | 0.004 |
| Depression (CES-D score >16) | <0.001 | |||
| Yes | 454 (45.4) | 156 (54.4) | 298 (41.6) | |
| No | 550 (54.7) | 131 (45.6) | 419 (58.4) | |
CES-D, Centre for Epidemiologic Studies Depression Scale; STIs, sexually transmitted infections.
Associated factors of health service utilisation
After adjusted for recruitment means, age, sex, education, marital status and annual income, participants stay in China for 2 weeks to 1month (Adjusted odds ratio (aOR): 2.00, 95% CI: 1.02 to 3.92), 2 to 6 months (aOR: 3.80, 95% CI: 1.96 to 7.36), 7 to 12 months (aOR: 5.02, 95% CI: 2.61 to 9.65) and over 1 year (aOR: 6.78, 95% CI: 3.73 to 12.33) from last entrance were more likely to utilize medical services in China, comparing with those stay less than one week. Compared with immigrants coming for tourism, significant increased health utilization rates were detected in those who came to China for business (aOR=2.23, 95% CI:1.13-4.40) and study (aOR=5.00, 95% CI:2.74-9.11). Compared with living in a hotel, living in a rental apartment (aOR=2.59, 95% CI:1.62-4.14) and staff/student dormitory (aOR=3.22, 95% CI:2.17-4.80) in China increased the rate of healthcare utilization of Africans.
Participants ever been diagnosed with hypertension (aOR: 4.96, 95% CI: 2.50 to 9.80), HIV/STIs (yes vs. no: aOR: 3.30, 95% CI: 1.47 to 7.38), cardiovascular diseases (yes vs. no: aOR: 2.98, 95% CI:1.32 to 6.76), skin diseases (yes vs. no: aOR: 2.74, 95% CI: 1.23 to 6.13) and cerebrovascular diseases (yes vs. no: aOR: 4.14, 95% CI: 1.34 to 12.84) were associated with higher health utilization rate. Participants diagnosed with tuberculosis (yes vs. no: aOR: 13.00, 95% CI:1.51 to 112.05) and infectious diarrhea (yes vs. no: aOR: 2.63, 95% CI: 1.03 to 6.95) in the past year, and presenting depression symptoms (aOR: 1.91, 95% CI: 1.42 to 2.56) were more likely to use health services in China (table 4).
Table 4.
Association between migration-related factors and health utilisation among participants
| Variable | Health utilisation n (%) | Crude OR (95% CI) | Adjusted OR (95% CI) |
| Religious belief | |||
| Christianity | 196 (26.3) | Ref. | Ref. |
| Islam | 43 (35.0) | 1.51 (1.00 to 2.26)* | 1.48 (0.96 to 2.27) |
| None | 35 (31.5) | 1.29 (0.84 to 1.99) | 1.56 (0.99 to 2.45) |
| Others | 12 (46.2) | 2.40 (1.09 to 5.28)* | 2.86 (1.27 to 6.42)* |
| Duration of stay in China from last entrance | |||
| Less than 1 week | 15 (9.3) | Ref. | Ref. |
| 2 weeks to 1month | 51 (27.3) | 3.68 (1.98 to 6.84)* | 2.00 (1.02 to 3.92)* |
| 2–6 months | 45 (28.8) | 3.98 (2.11 to 7.49)* | 3.80 (1.96 to 7.36)* |
| 7–12 months | 51 (32.7) | 4.76 (2.54 to 8.92)* | 5.02 (2.61 to 9.65)* |
| Over 1 year | 124 (36.3) | 5.57 (3.14 to 9.91)* | 6.78 (3.73 to 12.33)* |
| Purpose of travel | |||
| Tourism | 14 (9.9) | Ref. | Ref. |
| Business | 109 (35.4) | 4.97 (2.73 to 9.05)* | 2.23 (1.13 to 4.40)* |
| Study | 141 (32.8) | 4.43 (2.46 to 7.96)* | 5.00 (2.74 to 9.11)* |
| Other | 22 (17.5) | 1.92 (0.94 to 3.94) | 1.71 (0.82 to 3.60) |
| Living arrangement in China | |||
| Hotel | 85 (22.5) | Ref. | Ref. |
| Guest apartment | 14 (25.9) | 1.20 (0.63 to 2.31) | 1.38 (0.68 to 2.73) |
| Rental apartment | 55 (40.1) | 2.30 (1.52 to 3.50)* | 2.59 (1.62 to 4.14)* |
| Staff/student dormitory | 121 (32.4) | 1.64 (1.19 to 2.27)* | 3.22 (2.17 to 4.80)* |
| Others | 11 (18.0) | 0.76 (0.38 to 1.52) | 1.22 (0.58 to 2.56) |
| Diseases ever been diagnosed | |||
| Hypertension | |||
| No | 255 (26.6) | Ref | Ref |
| Yes | 32 (68.1) | 5.89 (3.14 to 11.06)* | 4.96 (2.50 to 9.8)* |
| HIV/STIs | |||
| No | 271 (27.7) | Ref | Ref |
| Yes | 16 (57.1) | 3.48 (1.03 to 7.83)* | 3.30 (1.47 to 7.38)* |
| Cardiovascular diseases | |||
| No | 268 (27.5) | Ref | Ref |
| Yes | 19 (63.3) | 4.56 (2.14 to 9.72) | 2.98 (1.32 to 6.76)* |
| Skin disease | |||
| No | 273 (27.9) | Ref | Ref |
| Yes | 24 (50.0) | 2.58 (1.22 to 5.49) | 2.74 (1.23 to 6.13)* |
| Cerebrovascular disease | |||
| No | 275 (27.8) | Ref | Ref |
| Yes | 12 (70.6) | 6.23 (2.18 to 17.85) | 4.14 (1.34 to 12.84)* |
| Diseases infected in the past year | |||
| Tuberculosis | |||
| No | 279 (28.0) | Ref | Ref |
| Yes | 7 (87.5) | 17.96 (2.20 to 146.59)* | 13.00 (1.51 to 112.05)* |
| Infectious diarrhoea | |||
| No | 275 (27.9) | Ref | Ref |
| Yes | 11 (57.9) | 3.55 (1.41 to 8.91)* | 2.63 (1.03 to 6.95)* |
| Depression (CES-D score >16) | |||
| No | 131 (23.8) | Ref | Ref |
| Yes | 156 (34.4) | 1.67 (1.27 to 2.01)* | 1.91 (1.42 to 2.56)* |
Multivariable model adjusted for recruitment, age, sex, education, marital status and annual income.
*The bold values mean P<0.05.
CES-D, Centre for Epidemiologic Studies Depression Scale; STIs, sexually transmitted infections.
Discussion
Health services are essential for human health maintenance, especially for migrants who are more vulnerable than residents.22 Although Africans in China met with several health problems, our results showed that only 28.5% of the participants used health services in China in the past year, and this figure is lower than Chinese migrants in China (36.4%).23 Studies have shown that, during the COVID-19 pandemic, providing sufficient health services for the international migrants could help them to avoid being infected and reduce their psychological and emotional distress.22 24 Our study provided evidence to help local governments make targeted COVID-19 control policies among African migrants in China.
The health utilisation behaviour was more significantly explained by predisposing and need factors than enabling factors, which coincides with findings of previous studies.25 26 The low health utilisation rate among African migrants in China may attribute to many factors. First, the Chinese government provides free essential public health services for all the citizens,27 and few African migrants have Chinese nationality, and therefore, cannot receive the related services. Second, perhaps due to the discrimination from residents, African migrants tend to stay in African communities and avoid unnecessary contact with residents and official governors during their stay in China.13 This situation weakens their willingness to use health services in China. Third, few hospitals in China provide exceptional services for international migrants. The lack of language translation service and diagnosis and treatment for specific diseases affecting Africans impede their access to health services.15 Additionally, our study showed that increased stay duration in China would increase the use of health services. However, the majority of participants (65.9%) in our study stayed less than 12 months in China. Future studies are warranted to examine the health services utilisation by including more Africans with different stay duration in China.
Despite the low health service utilisation, we have observed a significant need for health service utilisation among African migrants. Although this group is relatively much younger, while their self-reported prevalence of diabetes, cardiovascular diseases and cerebrovascular diseases in the current study are higher than residents.28 As we noticed, most African communities in China tend to be crowded and with poor sanitation, which facilitates the transmission of communicable diseases, such as influenza and tuberculosis.14 Besides that, a previous study reported that over half of African migrants had sex without condoms during their most recent sexual encounter, and about half of African migrants were unwilling to seek HIV testing after high-risk sexual behaviours,29 and this enlarged the risk of HIV infection and transmission among this group. Depression is another severe health threat for African migrants in China. Almost half (46%) of the participants in our study have significant depressive symptoms, and the rate is much higher than local Chinese residents,30 and African migrants living in America31 and Europe.32 However, many participants with physical and/or psychological health problems did not seek medical care, which leads to a worse disease prognosis.
Therefore, measures are in need to improve health utilisation among African migrants. First of all, China’s Basic Public Health Services Project has more than twenty free or discounted services to promote health utilisation among Chinese citizens. The Chinese government should consider extending these services coverage to documented international migrants. Besides, the active local disease surveillance model for African migrants should be established to obtain sufficient health information unavailable from the current passive surveillance system.33 The enhanced surveillance could help determine the medical needs of African migrants accurately and then implement corresponding interventions. Finally, more international clinics targeting African migrants should be set around the African community clusters to solve culture and custom conflicts, language barriers and distrust, impeding the accessibility of health service utilisation.
Some limitations were presented in this study. First, the research has applied a non-probabilistic sampling method to recruit participants, and students were oversampled (42.7% of the participants), which might lead to an unrepresentative sample. Second, some other potential factors were not included in the current study, such as smoking, drinking, physical exercises and sex behaviours. Third, we did not collect the information on what kinds of specific health services the participants used in China such as outpatient, inpatient and emergency care, which could be improved in further study. Fourth, although the temporary tourists were excluded by asking whether they ‘have spent at least 1 month cumulatively in China’ in this study, few of them might still be included due to their repetitive visiting to China.
Conclusion
The healthcare service that African migrants received in China is low. This situation could increase the disease burden of this group, and impede the communicable disease control works of the Chinese government. The existing public health policy and intervention measures are needed to be improved to make health utilisation more accessible and feasible for African migrants.
Supplementary Material
Acknowledgments
We thank all the study participants who contributed their valuable experience and opinions to this study. We thank the presidents and members of the Ghanaian, Nigerian, and Zimbabwean communities for their generous help during the study recruitment.
Footnotes
Contributors: CW conceptualised this study. MZX was responsible for data curation with input from HC. MZX completed data analysis and wrote the manuscript with inputs from CW. XZ, PZ and BH provided iterative reviews and critical comments.
Funding: This research has been funded by the National Social Science Fund of China (No. 19CSH018); Guangdong Medical Research Foundation (No. A2020427); Joint TDR/WPR Small Grants Scheme for Implementation Research in Infectious Diseases of Poverty (No. 2021/109143).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All the research data are available without restriction.
Ethics statements
Patient consent for publication
Obtained.
Ethics approval
The research has been reviewed and approved by the Ethics Review Committee of Dermatology Hospital of Southern Medical University (GDDHLS-20181203). Participants in this study provided written informed consent prior to their participation.
References
- 1.Bodomo A. Africans in China: a sociocultural study and its implications on Africa-China relations. New York: Cambria Press, 2012. [Google Scholar]
- 2.Mathews GLL, Yang Y. The world in guangzhou: Africans and other foreigners in South China’s global marketplace. Chicago: University of Chicago Press, 2017. [Google Scholar]
- 3.Chinese investors are eyeing on Africa . Secondary Chinese investors are eyeing on Africa, 2013. Available: http://en.gmw.cn/2013-03/20/content_7061674 [Accessed 29 Apr 2021].
- 4.Bodomo APC. Counting beans: some empirical and methodological problems for calibrating the African presence in greater China. J Pan African Studies 2015;7:126–43https://www.semanticscholar.org/paper/Counting-Beans%3A-Some-Empirical-and-Methodological-Bodomo-Pajan%C4%8Di%C4%8D/2712d609a45eca86cd207c8f660d0cbef92cd546?sort=relevance&citationIntent=background [Google Scholar]
- 5.Xingwei W. Foreign students flock to China, secondary foreign students flock to China, 2019. Available: https://www.i21st.cn/story/print_3442.html [Accessed 29 Apr 2021].
- 6.Habicht J. The role of campaigns in law enforcement: the example of Sanfei campaigns in Chinese immigration law, 2020. https://www.nomos-shop.de/shopfiles/leseprobe_978-3-7489-0781-7_leseprobe.pdf [Google Scholar]
- 7.Niu D, Zhang Z. Reasech of African in China: ten years report. Beijing: Social Sciences Academic Press; 2018. [Google Scholar]
- 8.Wang C, Tian Q, Zhao P, et al. Disease knowledge and attitudes during the COVID-19 epidemic among international migrants in China: a national cross-sectional study. Int J Biol Sci 2020;16:2895–905. 10.7150/ijbs.47075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou X, Hall BJ, Xiong M, et al. Post-migration well-being of sub-Saharan Africans in China: a nationwide cross-sectional survey. Qual Life Res 2021;30:1025–35. 10.1007/s11136-020-02663-7 [DOI] [PubMed] [Google Scholar]
- 10.Maimaitijiang R, Qiang-sheng HE, et al. Health status and evaluations on health services in China among African migrants. Chin J Public Health 2019;35:324–7. 10.1186/s12992-019-0449-y [DOI] [Google Scholar]
- 11.Yu-yin L, Zhi-feng J. Prevalence and major risk factors of chronic diseases among residents in Baiyun district of Guangzhou. Chin J of PHM 2012;28:202–3. 10.1038/s41598-019-46857-7 [DOI] [Google Scholar]
- 12.Peng LEI, Zhi-xin F, Jing-ni D. Evaluation of the status quo of medical resource allocation and service utilization in China. Health Economics Research 2019;36:50–5. 10.2196/27345 [DOI] [Google Scholar]
- 13.Lin L, Brown KB, Yu F, et al. Health care experiences and perceived barriers to health care access: a qualitative study among African migrants in Guangzhou, Guangdong Province, China. J Immigr Minor Health 2015;17:1509–17. 10.1007/s10903-014-0114-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLaughlin MM, Lee MC, Hall BJ, et al. Improving health services for African migrants in China: a health diplomacy perspective. Glob Public Health 2014;9:579–89. 10.1080/17441692.2014.908935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall BJ, Chen W, Latkin C, et al. Africans in South China face social and health barriers. Lancet 2014;383:1291–2. 10.1016/S0140-6736(14)60637-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daoyang Z, Li Zheng LZ, et al. Research on NGO participate in medical services in foreign-related communities-a case study of the African community at Xiaobei road, Guangzhou. China Management Informationization 2017;20:184–5https://www.jstor.org/stable/26915626 [Google Scholar]
- 17.Maimaitijiang R, He Q, Wu Y, et al. Assessment of the health status and health service perceptions of international migrants coming to Guangzhou, China, from high-, middle- and low-income countries. Global Health 2019;15:9. 10.1186/s12992-019-0449-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen's model of health services use. Surg Obes Relat Dis 2018;14:404–12. 10.1016/j.soard.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. In: Applied psychological measurement. 1, 1977: 385–401. [Google Scholar]
- 20.Morin AJS, Moullec G, Maïano C, et al. Psychometric properties of the center for epidemiologic studies depression scale (CES-D) in French clinical and nonclinical adults. Revue d'Épidémiologie et de Santé Publique 2011;59:327–40. 10.1016/j.respe.2011.03.061 [DOI] [PubMed] [Google Scholar]
- 21.Zhang Jie WZ, Ge F, Li Juan HB. Development of the Chinese age norms of CES-D in urban area. Chinese Mental Health Journal 2010;24:139–43. 10.3389/fpsyt.2021.559844 [DOI] [Google Scholar]
- 22.Liem A, Wang C, Wariyanti Y, et al. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 2020;7:e20. 10.1016/S2215-0366(20)30076-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yue-ping S, Guang-ying Z. Utilization of public health services and its influencing factors among migrant people with hypertension or diabetes in China. Chin J Public Health 2019;34:63–9. 10.7189/jogh.10.010807 [DOI] [Google Scholar]
- 24.Park H-J, Lee BJ. The role of social work for foreign residents in an epidemic: the MERS crisis in the Republic of Korea. Soc Work Public Health 2016;31:656–64. 10.1080/19371918.2016.1160352 [DOI] [PubMed] [Google Scholar]
- 25.Kim H-K, Lee M. Factors associated with health services utilization between the years 2010 and 2012 in Korea: using Andersen's behavioral model. Osong Public Health Res Perspect 2016;7:18–25. 10.1016/j.phrp.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fleury M-J, Grenier G, Bamvita J-M, et al. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int J Equity Health 2012;11:20. 10.1186/1475-9276-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bing D, Jing L. Utilization status and influencing factors of public health services for chronic disease patients in floating population. Chin J Prev Contr Chron Dis 2020;28:401–5. 10.11847/zgggws1123492 [DOI] [Google Scholar]
- 28.Xiuling S, Ma Wenjun XY, et al. Survey on self-report chronic diseases in Guangdong province,2004. South China Journal of Preventive Medicine 2007;33:50–2. [Google Scholar]
- 29.Cheng S, Han ZG, Liu FH, et al. [Analysis on influencing factors on HIV testing behaviors in some foreigners in Guangzhou]. Zhonghua Liu Xing Bing Xue Za Zhi 2020;41:1092–6. 10.3760/cma.j.cn112338-20200219-00123 [DOI] [PubMed] [Google Scholar]
- 30.Hall BJ, Chang K, Chen W, et al. Exploring the association between depression and shenjing shuairuo in a population representative epidemiological study of Chinese adults in Guangzhou, China. Transcult Psychiatry. In Press2018;55:733–53. 10.1177/1363461518778670 [DOI] [PubMed] [Google Scholar]
- 31.Wheaton FV, Thomas CS, Roman C, et al. Discrimination and depressive symptoms among African American men across the adult lifecourse. J Gerontol B Psychol Sci Soc Sci 2018;73:208–18. 10.1093/geronb/gbx077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mantovani N, Pizzolati M, Gillard S. Engaging communities to improve mental health in African and African Caribbean groups: a qualitative study evaluating the role of community well-being champions. Health Soc Care Community 2017;25:167–76. 10.1111/hsc.12288 [DOI] [PubMed] [Google Scholar]
- 33.Mann M, Mengistu A, Gaeseb J, et al. Active surveillance versus spontaneous reporting for first-line antiretroviral medicines in Namibia: a cost-utility analysis. Drug Saf 2016;39:859–72. 10.1007/s40264-016-0432-y [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All the research data are available without restriction.