Abstract
In August 2005, Hurricane Katrina caused unprecedented damage, widespread population displacement, and exposed Gulf Coast residents to traumatic events. The hurricane’s adverse impact on survivors’ mental health was apparent shortly after the storm and persisted, but no study has examined the long-term effects now that more than a decade has transpired. Using new data from a panel study of low-income mothers interviewed once before Hurricane Katrina and now three times after, we document changes in mental health, and estimate the sociodemographic and hurricane-related factors associated with long-term trajectories of mental health. We find that post-traumatic stress symptoms (PTSS) declined at each of the three post-Katrina follow-ups, but 12 years after the hurricane, one in six still had symptoms indicative of probable post-traumatic stress disorder. The rate of non-specific psychological distress (PD) remained consistently higher in all three follow-ups, compared to the pre-disaster period. In full covariate-adjusted models, no sociodemographic variables predicted long-run combinations of PTSS and PD. However, 12 years later, exposure to hurricane-related traumatic events and pre-disaster PD significantly predicted co-occurring PTSS and PD. Hurricane-related housing damage predicted PTSS in earlier follow-ups, but no longer predicted PTSS in the long-term. Furthermore, hurricane-related traumatic events significantly differentiated the risk of having persistent PTSS, relative to recovering from PTSS. The results suggest that there is still a nonnegligible group of survivors with continued need for recovery resources and that exposure to traumatic events is a primary predictor of adverse mental health more than a decade post-disaster.
Keywords: Hurricane Katrina, natural disaster, mental health, post-traumatic stress, psychological distress
Introduction
Approximately 10% of the U.S. population will experience one or more natural disasters in their lifetime (Goldstein et al., 2016), with mounting evidence suggesting that such events are increasing in both frequency and intensity (Intergovernmental Panel on Climate Change [IPCC], 2012). Natural disasters are associated with a wide range of adverse mental health consequences, among them post-traumatic stress symptoms (PTSS) and general psychological distress (PD) (for reviews, see Goldmann & Galea, 2014; Norris et al., 2002). In the short-term, these consequences are not distributed equally in the population, as prior research demonstrates that women, persons of color, those with lower socioeconomic status, and those with pre-existing mental health conditions are at increased risk of post-disaster psychiatric adversity (Neria, Nandi, & Galea, 2008; Norris et al., 2002). Less is known, however, about the longer-term mental health impact of natural disasters on vulnerable populations.
In fact, only a handful of studies have tracked survivors a decade or more after the event (for exceptions, see Chen et al., 2016; Goenjian et al., 2018; McFarlane & Van Hoof, 2009; Oishi et al., 2015), and few other studies have pre-disaster data to isolate the effects of the natural disaster from confounding variables (for exceptions, see Frankenberg et al., 2008; Heid, Pruchno, Cartwright, & Wilson-Genderson, 2018; Weems et al., 2007). No published paper to our knowledge has both. In this paper, we fill this gap in the extant literature by studying the effects of Hurricane Katrina on survivors’ mental health over a decade later, exploiting a new wave of data from a cohort panel study of low-income community college students surveyed before Katrina and re-surveyed three times since.
Hurricane Katrina and the Resilience in Survivors of Katrina (RISK) Project
The disproportionate impact of natural disasters on vulnerable populations captured the attention of both the research community and general public in the aftermath of Hurricane Katrina. The hurricane, which made landfall in the U.S. Gulf Coast on August 29, 2005, led to nearly 2,000 deaths, displaced over 650,000 residents, and caused an estimated 125 billion dollars in damages, making it the costliest disaster in the nation’s history (EM-DAT, 2019; Knabb et al., 2005). Hurricane Katrina had a particularly adverse impact on low-income and Black communities, with their neighborhoods sustaining greater damage than those of their high-income and White counterparts (Logan, 2006). Other findings document that low-income and Black residents were more likely to face other disaster-related stressors, such as late evacuation, delayed return migration, and post-disaster job loss (e.g., Elliott & Pais, 2006; Fussell, Sastry, & VanLandingham, 2010).
Epidemiologic studies on mental health after Hurricane Katrina show that the hurricane was associated with elevated mental illness in affected communities, particularly among those with sociodemographic vulnerabilities and who faced high levels of exposure (e.g., Galea et al., 2007; Galea, Tracy, Norris, & Coffey, 2008; Kessler, Galea, Jones, & Parker, 2006; Sastry & VanLandingham 2009). For example, five to seven months post-disaster, Galea and colleagues (2007) found prevalence estimates of 49.1% for probable moderate or serious mental illness, based on assessments of general psychological distress using the Kessler-6 (K6) scale (Kessler et al., 2002; Kessler et al., 2003), and 30.3% for PTSD among pre-disaster residents of the New Orleans metropolitan area. Participants who endured more disaster-related stressors, particularly injuries and physical adversities (e.g., difficulty obtaining adequate food or clothing) were at greater risk for mental illness. Notably, demographic differences in risk – for example, higher prevalence estimates in female, low-education, and low-income participants relative to their counterparts – could not be fully explained by differential exposure to disaster-related stressors.
Several years before Hurricane Katrina, a research team began the Opening Doors study, a randomized control trial of an intervention designed to boost the community college retention rates of low-income single parents between the ages of 18 and 34 years (Richburg-Hayes et al., 2009). One of four sites around the country was New Orleans, and at the time of the hurricane, 1,019 New Orleans-area participants – mostly low-income, Black women – had enrolled in the study and filled out a baseline survey across two community colleges. When the hurricane struck, nearly half of the participants (n = 492, 48.3%) had been involved in the study long enough to have completed a one-year follow-up assessment. Hurricane Katrina led to substantial damages to the community colleges, both of which were closed for the Fall 2005 semester. The New Orleans participants were thus dropped from the larger Opening Doors study, but the project’s Principal Investigators were able to secure funding to follow them as part of a new investigation, which they named Resilience in Survivors of Katrina (RISK) (for more information on the origins and key findings of RISK, see Waters, 2016).
The RISK study has at least three key advantages compared to prior research on disasters and mental health. First, data on the RISK cohort were first collected before Katrina, a unique attribute among disaster studies. Findings from RISK (e.g., Rhodes et al., 2010) and other exceptional studies with pre-disaster data (e.g., Heid, Pruchno, Cartwright, & Wilson-Genderson, 2018; La Greca, Silverman, & Wassterstein, 1998; Weems et al., 2007) demonstrate pre-disaster functioning to be among the strongest predictors of post-disaster mental health, suggesting that studies lacking such data are overestimating the impact of disaster-related exposures and other factors on outcomes. Second, its focus on an at-risk sample of low-income parents, and primarily single Black women, permits exploration of factors that explain variation within this group in post-disaster mental health. Information on such factors could inform ongoing efforts to mitigate disaster-related impacts, as well as actions to prevent psychiatric adversity after future disasters. Third, post-disaster cohort studies typically focus on persons who remained in the disaster-affected location and thus do not capture the experiences of those who are either temporarily or permanently displaced. Prior research indicates that displacement increases risk for post-disaster mental health problems (for a review, see Uscher-Pines, 2009). Findings from RISK have replicated this pattern (Fussell & Lowe, 2014) and suggest that negative mental health consequences could be due in part to disruptions in survivors’ social support networks (Morris & Deterding, 2016). On the other hand, others have shown that displacement can expose some survivors to new opportunities, for example in employment, education, and relationships, perhaps buffering mental health risks (Manove et al., 2019).
The primary analyses of RISK have focused on two key mental health outcomes, general PD and PTSS. Using data from the first post-disaster wave (7–19 months post-disaster), Rhodes and colleagues (2010) showed that higher pre-disaster PD and exposure to more hurricane-related traumatic events predicted both outcomes, and that older age and ethnic minority status were additional predictors of PTSS only. Paxson and colleagues (2012) expanded upon these findings in an analysis published in Social Science & Medicine by drawing on the second wave of post-disaster data, collected 43–54 months post-disaster.
The analysis by Paxson and colleagues (2012) had three key findings. First, although PD and PTSS declined between two post-disaster time points, levels remained elevated, as compared to the pre-disaster assessment. Second, the patterns of factors predicting PD only, PTSS only, and comorbid PD and PTSS were relatively consistent across the two time points. Specifically, a greater number of hurricane-related traumatic events predicted all three outcomes, and home damage and bereavement predicted comorbid PD and PTSD at each wave. Third, the results shed light onto predictors of different symptom patterns over time, showing in particular strong associations between pre-disaster PD, household damage, a greater number of hurricane-related traumatic events, and bereavement and chronic comorbid PD and PTSD.
We extend this work by including data from an additional post-disaster follow-up assessment, conducted approximately 12 years after Hurricane Katrina. In doing so, we address a further key limitation of the extant literature on disaster mental health: the dearth of studies tracking the functioning of survivors over a decade post-disaster. Long-term studies are critical in understanding the consequences of natural disasters and in providing ongoing support to disaster survivors, particularly among those most vulnerable to disaster-related impacts and psychiatric adversity. Without data that span a decade or more post-disaster, we cannot know what proportion of survivors may be in need of ongoing assistance. Further, the factors predicting long-term mental health outcomes may differ from those that predict short-term or intermediate outcomes. Insight into such differences could inform efforts to efficiently allocate limited resources for survivors in the long-term aftermath of Hurricane Katrina and other disasters. Although some notable studies have followed survivors for more than a decade post-disaster (e.g., Goenjian et al., 2018), none to our knowledge share the other strengths of RISK, namely its focus on a vulnerable population, inclusion of displaced participants, and rich pre-disaster data. Further, no published study to our knowledge has tracked survivors of Hurricane Katrina specifically a decade or more after the disaster.
The objectives of the current study are threefold. The first is to identify for vulnerable survivors the pre-disaster and disaster-related predictors of mental health in the long-term. The second is to compare the predictors of long-term mental health outcomes with those of short- and middle-term mental health. The final aim is to pinpoint the factors that render survivors differentially at risk of changes in post-disaster mental health status over time. We address each of these objectives by updating with the newest wave of data the analyses conducted by Paxson, Fussell, Rhodes, and Waters (2012) using the same panel study of Katrina survivors.
Methods
To be eligible for the original Opening Doors study, students at the participating community colleges had to be a parent, between the ages of 18 and 34, and earn less than 200% of the poverty line, yielding a sample of mainly poor, and predominantly Black mothers. In addition to baseline data collected before Katrina in 2003–2004, we rely on three post-hurricane follow-up surveys conducted with the 942 women in the sample (of the original 1,019). The first (PK1) was conducted beginning seven months after Katrina, between March 2006 and March 2007, in which 667 of the original 942 female participants responded (70.8% response rate). A second (PK2) follow-up survey was administered to 702 women between March 2009 and April 2010 (74.5% response rate). A third (PK3) follow-up survey was administered to 715 women between November 2016 and November 2018 (76.0% response rate).
In the end, 882 respondents (94.5%) of the original respondents completed at least one post-hurricane survey, and 468 of respondents (50.2%) completed all three follow-up surveys (original respondents n=933, 942 less 9 due to death). We restrict our analytic sample to the 438 respondents who filled out every post-Katrina survey and had no missing values on our two main outcome variables (PTSS and PD) for any of the waves. Independent-sample t-tests confirm that there were no statistically meaningful differences between our analytic sample and those excluded due to missingness on the outcomes. Thirty respondents were missing on any of the outcomes of interest. Missing data on independent variables were imputed for the regression analyses using chained multiple imputation in STATA 15.1 (Rubin, 1996).
Measures
We measure PTSS using the Impact of Event Scale-Revised (IES-R). The IES-R is a 22-item scale that evaluates distress related to a specific traumatic event (Weiss & Marmar, 1997). We asked respondents to rate the degree to which they were bothered by symptoms of distress about Hurricane Katrina over the past 7 days, using a Likert scale coded from “not at all” (0) to “extremely” (4). We construct an average for each respondent, and we define the cut-off for PTSS at 1.5, because this is the threshold for a high risk of having PTSD (Creamer et al. 2003).
To measure non-specific PD, we rely on the Kessler-6 (K6) scale, a self-report scale developed for the National Health Interview Survey and now commonly used to assess anxiety and mood disorders (Kessler et al., 2002; Kessler et al., 2003). Respondents were asked to report how often in the last 30 days they experienced six types of feelings of distress (e.g. “hopeless”) on a scale from “none of the time” (0) to “all of the time” (4). Responses to the six questions were summed to construct scores ranging from 0 to 24. Following past validation studies (Kessler et al., 2010), we define the threshold of PD as a score greater than 8. K-6 scores of 8–12 indicate probable mild to moderate mental illness (MMI), and scores of 13–24 indicate probable serious mental illness (SMI). In the descriptive analyses, we provide statistics for both MMI and SMI, and in the inferential stage, we focus solely on the single-category of PD (any score greater than 8).
Following the mental health trajectories documented by Norris and colleagues (2002), for each of our outcomes of interest, PTSS and PD, we construct a variable that identifies four patterns of changes in mental health: never, recovered, delayed (or incident for PD), and persistent. PTSS is coded as follows: (1) never had PTSS after Katrina, (2) recovered from PTSS (had PTSS in either the first or second follow-up, and did not have it in the third follow-up), (3) delayed PTSS (did not have PTSS in the first and second follow-up surveys but did in the most recent survey), and (4) persistent PTSS (had PTSS at the first and the third follow-up surveys). The PD trajectory was coded in the same way, but “delayed” is referred to as “incident,” given that the variable is not Katrina-specific.
We also include a set of covariates in our analyses. We use several variables from the pre-hurricane baseline, including monthly earnings (in dollars), a dummy variable for K6 distress, and perceived social support. The social support measure comes from the Social Provisions Scale (Cutrona & Russell, 1987), which asks respondents the degree to which they agree with eight statements, such as “there are people I know who will help me if I really need it.” We coded responses from 1 to 4 with higher values corresponding to greater perceived social support (several items are reverse coded due to wording). The eight items were averaged to construct a total score. We also include several baseline demographic variables: age in years, a dummy variable for marital status, coded 1 for married or cohabitating, and the number of children in each of three age categories: 0 to 5, 6 to 11, and 12 to 17 years old. Race is a dummy variable indicating Black.
We use three indicators of hurricane exposure and loss. The first is a dummy variable for housing damage, coded 1 for respondents whose homes experienced “moderate” or “severe” damage from Hurricane Katrina. The second measure is a summed score from an eight-item trauma scale, based on a survey of Hurricane Katrina survivors conducted shortly after the storm (Brodie et al., 2006). Respondents were asked “yes” or “no” to the following questions about their experiences in the week after Hurricane Katrina: (1) lacked enough fresh water to drink, (2) lacked enough food to eat, (3) felt one’s life was in danger, (4) lacked necessary medicine, (5) lacked necessary medical care, (6) family member lacked necessary medical care, (7) lacked knowledge of safety of children, or (8) lacked knowledge about safety of other family members. Finally, our third measure of hurricane exposure and loss was an indicator of whether a family member or friend died as a result of Hurricane Katrina. The three measures were based on information asked in the first post-Katrina follow-up.
Analyses
To provide estimates that are comparable to those in Paxson and colleagues (2012), we follow their analytic strategy. We begin by analyzing the cross-sectional changes in the proportion of respondents with PTSS without PD, PD without PTSS, and comorbid PD and PTSS in the short-, middle-, and long-term. We then describe the individual-level trajectories of mental health. The inferential stage proceeds in two steps. First, we estimate a series of multinomial logistic regression models for each of the three post-hurricane waves to assess the association between pre-Katrina demographics, health characteristics, and hurricane exposure with PD only, PTSS only, or comorbid PD and PTSS, relative to having neither. Second, we predict within-respondent patterns of PD and PTSS across the three waves, using a categorical variable for each symptom, indicating those with persistent, recovered, delayed onset (or incident), or no experience of symptoms.
Results
Descriptive Statistics
Table 1 presents descriptive statistics for the explanatory variables. The first column shows means and standard deviations of variables for this study’s analytic sample; the second and third columns reflect the sample analyzed by Paxson and colleagues (2012) and the full sample, respectively. The modal respondent is young, low-income, Black, and all are mothers to a child under the age of 18. At the time of Hurricane Katrina, the average respondent was 25 years old, earned $955 per month, and was not married or cohabitating with a partner (75.7%). Before the hurricane, 23.2% of respondents reported PD. The baseline survey was completed between 21 and 2 months before Hurricane Katrina. On average, respondents completed the first follow-up survey 11 months after Hurricane Katrina, the second follow-up 46 months after Katrina, and the final follow-up 148 months or more than 12 years after the storm.
Table 1.
Descriptive statistics for analytic sample
| Analytic sample n=438 | Paxson et al. (2012) n=532 | Full Sample n=923 | |
|---|---|---|---|
| Time from hurricane to first follow-up (SD), months | 10.95 (3.01) | 11.40 (2.92) | |
| Time from hurricane to second follow-up (SD), months | 45.50 (2.61) | 45.39 (2.58) | |
| Time from hurricane to third follow-up (SD), months | 148.29 (7.52) | ||
| Age at time of hurricane (SD), yrs. | 25.17 (4.53) | 26.18 (4.57) | 26.32 (4.54) |
| Race, % | |||
| Black | 81.96 | 83.5 | 83.2 |
| Non-Black | 18.04 | 16.5 | 16.8 |
| Monthly earnings before hurricane (SD), $ | 955.2 (525.1) | 957.0 (497.5) | 971.7 (496.3) |
| Social support before hurricane (SD), 1 to 4 scale | 3.20 (0.46) | 3.22 (0.45) | 3.19 (0.45) |
| PD before hurricane, % | 23.2 | 23.8 | 23.5 |
| Not married or cohabitating before hurricane, % | 75.7 | 75.3 | |
| Children ages 0 to 5 at time of hurricane (SD), # | 1.04 (0.83) | 1.05 (0.83) | |
| Children ages 6 to 11 at time of hurricane (SD), # | 0.56 (0.77) | 0.58 (0.79) | |
| Children ages 12 to 17 at time of hurricane (SD), # | 0.31 (0.63) | 0.30 (0.62) | |
| Home damaged during hurricane, % | 80.8 | 80.8 | |
| Hurricane traumas (SD), 0 to 8 scale | 2.84 (2.20) | 2.93 (2.19) | |
| Relative or friend died because of hurricane, % | 30.7 | 32.1 |
Note: Missing values for demographics in analytic sample: social support (7); earnings (49); baseline psychological distress (8)
Hurricane exposure and associated trauma were widespread in the sample. Four in five respondents (80.8%) experienced moderate or severe damage to their home because of the storm. Respondents experienced 2.84 out of a possible 8 types of hurricane-related trauma on average, with considerable within-sample variation (SD = 2.20). Finally, nearly one in three respondents (30.7%) had a friend or relative die due to Hurricane Katrina.
Table 2 and Figure 1 provide descriptive statistics for mental health outcomes at all three post-Katrina waves. As expected, incidence of PTSS is highest at the first follow-up in 2006–2007, less than a year after the storm, affecting 43.8% of respondents. It has since declined, falling to 32.0% at the second follow-up in 2009–2010 and most recently to 16.7% at the third follow-up in 2016–2018. McNemar’s chi-square test reveal that declines in prevalence within the sample are statistically significant (p < .001).
Table 2.
Psychological distress (PD) and post-traumatic stress symptoms (PTSS) at three follow-ups, including PTSS in combination with probable serious mental illness (n=438)
| Pre-Hurricane | 1st follow-up | 2nd follow-up | 3rd follow-up | Change 2nd to 3rd | Chi-square test, p-value | |
|---|---|---|---|---|---|---|
| PTSS, with or without PD, % | 43.84 | 31.96 | 16.67 | −15.29 | 0.000 | |
| PD, with or without PTSS, % | 23.95 | 35.16 | 30.14 | 28.54 | −1.60 | 0.611 |
| SMI, with or without PTSS, % | 6.05 | 11.64 | 10.73 | 10.73 | 0.00 | 1.000 |
| PTSS and PD Combinations, % | ||||||
| Neither PTSS nor PD | 43.15 | 54.11 | 63.24 | 9.13 | 0.000 | |
| PD alone | 13.01 | 13.93 | 20.09 | 6.16 | ||
| PTSS alone | 21.69 | 15.75 | 8.22 | −7.53 | ||
| PTSS and PD | 22.15 | 16.21 | 8.45 | −7.76 | ||
| PTSS and SMI Combinations, % | ||||||
| Neither PTSS nor SMI | 53.88 | 63.70 | 76.71 | 13.01 | 0.000 | |
| SMI alone | 2.28 | 4.34 | 6.62 | 2.28 | ||
| PTSS alone | 34.47 | 25.57 | 12.56 | −13.01 | ||
| PTSS and SMI | 9.36 | 6.39 | 4.11 | −2.28 |
The final column shows the p-values from chi-square tests for changes from the second to the third follow-up. McNemar’s chi-square test is used for the dichotomous measures of PTSS, PD, and SMI, and McNemar-Bowker chi-square tests for the categorical combination variables.
Figure 1:
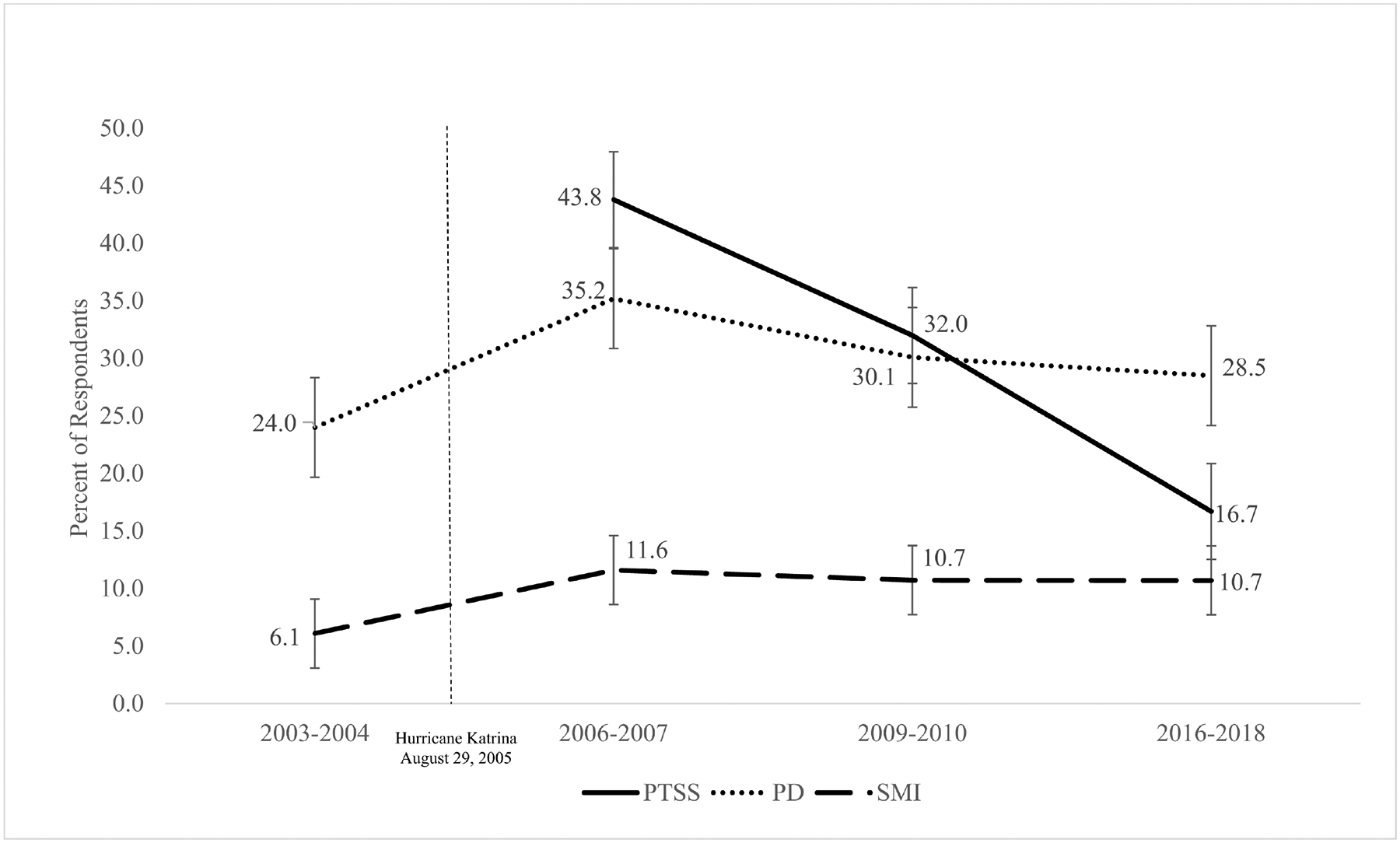
PTSS, PD, and SMI among Resilience in Survivors of Katrina (RISK) sample (n=438) (Means and 95% CI)
Rates of PD also declined with time post-Katrina, albeit to a lesser extent. The proportion of respondents who experienced PD decreased significantly from 35.2% to 28.5% in the 10 years between the first and third follow-ups. Even in 2016–2018, the proportion reporting PD is higher than was observed before the hurricane. In terms of serious mental illness, the prevalence increased from baseline (6.1%) to the first post-Katrina follow-up (11.6%); it remains elevated at the third follow-up (10.7%). McNemar’s chi-square tests, however, reveal no significant change in the proportion of the sample with PD or SMI from the second to third follow-up.
The percent of respondents without either PTSS or PD increased across all three follow-ups, from 43.2% in the first to 54.1% in the second and 63.2% in the most recent wave in 2016–2018. By the third follow-up, about one in five respondents (20.1%) reported PD alone, 8.2% reported PTSS alone, and 8.5% reported PTSS in combination with PD. Finally, only 4.1% of respondents reported PTSS in combination with SMI. Over three in four (76.7%) have neither PTSS nor SMI. Chi-square tests show significant changes in the proportional distributions within each combination variable from the second to the third follow-up.
As a final set of descriptive statistics, we visualize the longitudinal nature of the data and show individual-level trajectories. Figure 2 shows the different trajectory groups for the two mental health outcomes, PTSS (Panel 1) and PD (Panel 2) across the three post-Katrina waves. Across all three waves, 56.2% of the sample reported hurricane-related PTSS at some point while 43.8% did not. At the first follow-up in 2006–2007, 43.8% of the sample reported PTSS. Among those who experienced PTSS in the immediate aftermath, half continued to report PTSS in the second follow-up, and 19.3% reported PTSS at the third follow-up. As expected, the vast majority of respondents without hurricane-related PTSS in the immediate aftermath also did not report PTSS five years or 12 years later. We categorize respondents into four mutually exclusive mental health trajectory groups: persistent (n=60, 14%), recovered (n=173, 39%), delayed onset (n=13, 3%), and never (n=192, 44%).
Figure 2:
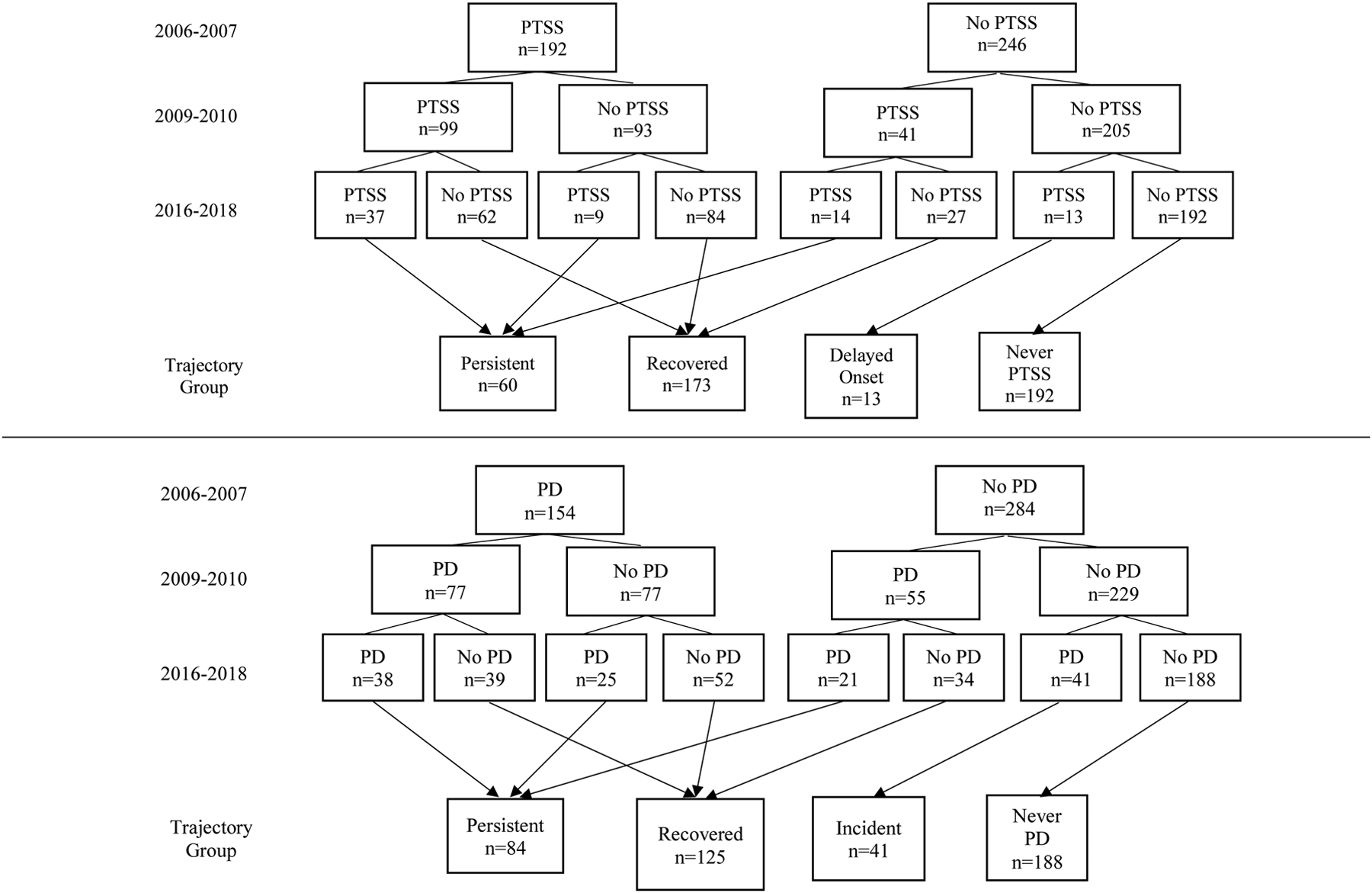
Trajectories of PTSS and PD in Two Panels (n=438)
The second panel of Figure 2 shows the trajectories of the sample for PD. Immediately after the hurricane, 35.1% of respondents reported PD. Similar to the breakdown of PTSS, exactly half of respondents who reported PD in the first post-Katrina survey were still distressed at the second follow-up, and 24.6% were distressed 12 years after the storm. Among those that did not report PD in the immediate aftermath, few reported PD at later follow-ups. Across three follow-up surveys over more than ten years, 57.1% of respondents reported PD at some point, and conversely 42.9% never reported having PD. As with PTSS, we categorize respondents into groups based on trajectories of PD after Katrina: persistent (n=84, 19%), recovered (n=125, 29%), incident (n=41, 9%), and never (n=188, 43%).
Predictors of mental health at three post-Katrina time points
Table 3 presents the relative risk ratios (RRR) from multinomial logistic regression models of PTSS and PD alone and in combination for each of the three waves. The reference category for each model is having neither PTSS nor PD in that wave. At the first follow-up, the risk of having co-occurring PTSS and PD (relative to having neither PD nor PTSS) was 3.62 (p < .05) times greater for Black respondents compared to those of another race, controlling for hurricane-associated trauma and pre-existing PD. Older respondents were also more likely to experience co-occurring PTSS and PD, net of other model covariates. As expected, given prior findings on the exacerbating effect of disasters on pre-existing mental health problems, PD before the hurricane is associated with an increased risk of reporting PD and PTSS, either alone or in combination, immediately after the storm. In fact, risk of having both PD and PTSS is 5.23 (p < .001) times greater for those who reported PD at baseline. All three measures of hurricane exposure and loss also significantly predicted adverse mental health outcomes, raising the likelihood of experiencing a co-occurrence of PTSS and PD. Having a friend or family member die because of Katrina was also associated with an increased risk of experiencing PTSS alone. We did not find evidence that mental health outcomes are associated with cohabitation status, number and age of children, earnings, and social support, each measured before the hurricane, or with the timing of respondents’ interviews.
Table 3.
Relative risk ratios and (95% Confidence Intervals), multinomial logistic models of PTSS alone, PD alone, or co-occurring PTSS and PD (n=438)
| Model 1: First Follow-Up (2006–2007) | Model 2: Second Follow-Up (2009–2010) | |||||
|---|---|---|---|---|---|---|
| PD alone | PTSS alone | PTSS and PD | PD alone | PTSS alone | PTSS and PD | |
| Time to follow-up | 1.01 (0.92, 1.11) | 1.00 (0.92, 1.09) | 0.97 (0.88, 1.06) | 1.02 (0.90, 1.16) | 1.01 (0.91, 1.13) | 0.78** (0.67, 0.91) |
| Age at time of hurricane | 1.02 (0.93, 1.11) | 1.07 (0.99, 1.15) | 1.11* (1.02, 1.21) | 0.98 (0.89, 1.08) | 1.05 (0.97, 1.13) | 1.06 (0.97, 1.16) |
| Baseline partnership status | ||||||
| Married/cohabitating | ||||||
| Not married/cohabitating | 1.25 (0.59, 2.68) | 1.03 (0.54, 1.95) | 1.12 (0.54, 2.33) | 0.83 (0.41, 1.67) | 1.58 (0.73, 3.44) | 0.94 (0.42, 2.12) |
| Race | ||||||
| Non-Black | ||||||
| Black | 0.79 (0.35, 1.76) | 1.66 (0.79, 3.47) | 3.62* (1.25, 10.46) | 1.46 (0.64, 3.31) | 4.05* (1.27, 12.88) | 2.00 (0.74, 5.36) |
| Children ages 0 to 5 | 0.78 (0.50, 1.20) | 1.19 (0.84, 1.68) | 0.95 (0.68, 1.34) | 0.97 (0.65, 1.45) | 1.04 (0.73, 1.46) | 0.83 (0.51, 1.33) |
| Children ages 6 to 11 | 1.21 (0.74, 1.98) | 1.03 (0.73, 1.47) | 0.88 (0.60, 1.29) | 1.08 (0.70, 1.68) | 0.73 (0.46, 1.14) | 1.08 (0.74, 1.57) |
| Children ages 12 to 17 | 0.44* (0.22, 0.90) | 0.93 (0.57, 1.53) | 0.72 (0.42, 1.24) | 0.66 (0.32, 1.36) | 1.24 (0.75, 2.06) | 0.89 (0.46, 1.72) |
| Log monthly earnings before hurricane | 0.87 (0.54, 1.40) | 0.82 (0.56, 1.19) | 0.86 (0.56, 1.33) | 1.22 (0.72, 2.06) | 0.69 (0.47, 1.01) | 0.75 (0.48, 1.18) |
| Social support before hurricane | 0.64 (0.30, 1.36) | 1.33 (0.71, 2.50) | 0.94 (0.47, 1.86) | 0.46* (0.21, 0.98) | 2.11* (1.10, 4.07) | 0.71 (0.31, 1.64) |
| PD before hurricane | 2.95** (1.31, 6.66) | 2.36* (1.13, 4.93) | 5.23*** (2.54, 10.78) | 2.55** (1.32, 4.94) | 2.29* (1.06, 4.91) | 4.12*** (1.91, 8.89) |
| Home damaged during hurricane | 0.97 (0.43, 2.18) | 1.55 (0.75, 3.19) | 2.60* (1.01, 6.72) | 0.73 (0.34, 1.57) | 1.22 (0.54, 2.79) | 8.64** (2.13, 34.97) |
| Hurricane traumas | 1.08 (0.93, 1.26) | 1.09 (0.96, 1.23) | 1.25*** (1.10, 1.42) | 1.12 (0.97, 1.29) | 1.20** (1.05, 1.38) | 1.44*** (1.24, 1.66) |
| Relative/friend died because of hurricane | 1.43 (0.71, 2.90) | 2.17** (1.21, 3.89) | 2.53** (1.41, 4.52) | 1.45 (0.75, 2.81) | 2.10* (1.13, 3.90) | 2.07* (1.09, 3.94) |
| Model 3: Third Follow-Up (2016–2018) | |||
|---|---|---|---|
| PD alone | PTSS alone | PTSS and PD | |
| Time to follow-up | 1.00 (0.97, 1.04) | 1.01 (0.97, 1.06) | 1.03 (0.98, 1.08) |
| Age at time of hurricane | 0.99 (0.92, 1.07) | 1.02 (0.92, 1.13) | 0.99 (0.88, 1.11) |
| Baseline partnership status | |||
| Married/cohabitating | |||
| Not married/cohabitating | 0.71 (0.41, 1.24) | 1.26 (0.43, 3.73) | 0.94 (0.41, 2.17) |
| Race | |||
| Non-Black | |||
| Black | 0.76 (0.41, 1.41) | 2.50 (0.69, 9.11) | 1.42 (0.48, 4.17) |
| Children ages 0 to 5 | 1.27 (0.95, 1.71) | 1.17 (0.70, 1.96) | 0.93 (0.56, 1.55) |
| Children ages 6 to 11 | 0.75 (0.50, 1.13) | 1.15 (0.73, 1.83) | 1.18 (0.79, 1.75) |
| Children ages 12 to 17 | 1.26 (0.81, 1.97) | 1.39 (0.71, 2.71) | 1.28 (0.63, 2.60) |
| Log monthly earnings before hurricane | 0.86 (0.59, 1.23) | 0.67 (0.41, 1.09) | 0.70 (0.46, 1.07) |
| Social support before hurricane | 0.81 (0.44, 1.49) | 0.98 (0.45, 2.14) | 1.15 (0.49, 2.70) |
| PD before hurricane | 1.63 (0.88, 3.04) | 1.50 (0.56, 4.05) | 4.61*** (2.07, 10.26) |
| Home damaged during hurricane | 0.94 (0.48, 1.87) | 0.66 (0.27, 1.63) | 0.86 (0.31, 2.33) |
| Hurricane traumas | 0.95 (0.83, 1.08) | 1.07 (0.90, 1.26) | 1.26* (1.05, 1.51) |
| Relative/friend died because of hurricane | 1.69 (0.99, 2.88) | 1.81 (0.81, 4.02) | 1.63 (0.75, 3.55) |
Notes: Two-tailed t-test.
p<.05,
p<.01,
p<.001.
Huber-White robust standard errors in parentheses. Estimated using multiple imputation.
In the second follow-up, similar patterns emerged. Black respondents again had worse PTSS outcomes compared to respondents from other racial/ethnic groups. Also consistent with the first follow-up, pre-existing PD, hurricane exposure, and hurricane-related trauma are associated with higher risk of PD and/or PTSS. Age, pre-hurricane partnership status, number and age of children, and earnings were unrelated to PTSS and PD in the second follow-up. There is evidence that social support at baseline decreased the likelihood of experiencing PD alone, which was found in previous studies using the same dataset, albeit with different analytic samples (Paxson, Fussell, Rhodes, & Waters, 2012; Chan, Lowe, Weber, & Rhodes, 2015). However, in our model of the second follow-up, we also find that baseline social support increased the likelihood of experiencing PTSS alone, relative to having neither (RRR= 2.11, p=.026). This point estimate of the relative risk ratio is similar to that reported by Paxson and colleagues (2012), although the confidence interval (CI) around their estimate contained 1.
Whereas in the first two follow-ups we found that race was a significant predictor of mental health outcomes, we detected no evidence of persistent racial disparities 12 years after Katrina. Further, no pre-hurricane demographic variables were associated with long-term PTSS, PD, or both in combination, despite evidence of short-run associations with demographic characteristics. PD that pre-dated Hurricane Katrina, however, remains associated with an increased risk of having a combination of PTSS and PD 12 years after the disaster, although it does not predict PD in the absence of PTSS. Finally, the number of traumas experienced due to the hurricane remains a robust predictor of experiencing PTSS and PD in combination, relative to having neither, 12 years after the storm. Each additional trauma increases the relative risk of experiencing combined PTSS and PD by a factor of 1.26 (p < .05), net of all other variables. The magnitude of the increased relative risk associated with each additional hurricane-related trauma has remained relatively consistent (RRR range over time: 1.25 – 1.44) across all three follow-up waves.
Post-Katrina mental health trajectories and their correlates
The analyses above are cross-sectional associations of mental health at different time points after the hurricane. We now move to analyzing predictors of changes in mental health within-individuals, across these time points. Table 4 describes the associations between PTSS trajectories and individual characteristics.
Table 4.
Relative risk ratios and (95% Confidence Intervals), multinomial logistic models of trajectories of PTSS (n=438)
| Model 1: PTSS | ||||||
|---|---|---|---|---|---|---|
| Recovered vs. Never (ref) | Delayed vs. Never (ref) | Persistent vs. Never (ref) | Persistent vs. Delayed (ref) | Delayed vs. Recovered (ref) | Persistent vs. Recovered (ref) | |
| Age at time of hurricane | 1.10** (1.03, 1.17) | 0.98 (0.81, 1.18) | 1.08 (0.98, 1.18) | 1.10 (0.89, 1.34) | 0.89 (0.74, 1.08) | 0.98 (0.90, 1.07) |
| Baseline partnership status | ||||||
| Married/cohabitating | ||||||
| Not married/cohabitating | 1.03 (0.59, 1.78) | 2.01 (0.33, 12.15) | 1.12 (0.48, 2.61) | 0.56 (0.08, 3.92) | 1.95 (0.31, 12.43) | 1.09 (0.49, 2.43) |
| Race | ||||||
| Non-Black | ||||||
| Black | 3.05** (1.56, 5.95) | 6.13 (.98, 38.49) | 2.90* (1.09, 7.69) | 0.47 (0.06, 3.83) | 2.01 (0.30, 13.54) | 0.95 (0.35, 2.59) |
| Children ages 0 to 5 | 1.07 (0.81, 1.42) | 0.61 (0.32, 1.19) | 1.09 (0.68, 1.74) | 1.77 (0.82, 3.84) | 0.57 (0.29, 1.13) | 1.01 (0.65, 1.58) |
| Children ages 6 to 11 | 0.88 (0.63, 1.22) | 0.96 (0.43, 2.13) | 1.16 (0.75, 1.80) | 1.21 (0.53, 2.78) | 1.09 (0.50, 2.41) | 1.33 (0.92, 1.92) |
| Children ages 12 to 17 | 0.90 (0.56, 1.46) | 2.10 (0.68, 6.48) | 1.09 (0.58, 2.06) | 0.52 (0.16, 1.69) | 2.32 (0.75, 7.24) | 1.21 (0.69, 2.12) |
| Log monthly earnings before hurr. | 0.88 (0.62, 1.24) | 0.50* (0.27, 0.90) | 0.70 (0.47, 1.04) | 1.40 (0.72, 2.75) | 0.56 (0.31, 1.04) | 0.79 (0.54, 1.17) |
| Social support before hurricane | 1.19 (0.69, 2.04) | 0.81 (0.24, 2.76) | 1.36 (0.66, 2.84) | 1.68 (0.45, 6.32) | 0.68 (0.20, 2.37) | 1.15 (0.57, 2.34) |
| PD before hurricane | 2.85** (1.51, 5.37) | 4.03* (1.05, 15.45) | 4.63*** (2.01, 10.70) | 1.15 (0.28, 4.77) | 1.41 (0.38, 5.32) | 1.63 (0.78, 3.41) |
| Home damaged during hurricane | 1.86 (0.96, 3.58) | 0.30* (0.09, 0.96) | 1.64 (0.63, 4.27) | 5.55* (1.37, 22.43) | 0.16** (0.05, 0.55) | 0.88 (0.34, 2.31) |
| Hurricane traumas | 1.16** (1.04, 1.30) | 0.88 (0.66, 1.17) | 1.36*** (1.17, 1.58) | 1.55** (1.15, 2.08) | 0.76 (0.57, 1.00) | 1.17* (1.02, 1.35) |
| Relative/friend died because of hurr. | 1.80* (1.09, 2.99) | 0.65 (0.12, 3.57) | 2.58** (1.29, 5.15) | 4.00 (0.69, 23.01) | 0.36 (0.07, 1.97) | 1.43 (0.75, 2.73) |
Notes: Two-tailed t-test.
p<.05,
p<.01,
p<.001.
Huber-White robust standard errors in parentheses. Estimated using multiple imputation.
Age was associated with recovery from, but not the persistent experience of, PTSS, compared to never having experienced PTSS. We also found that Black respondents were more likely to fall into the recovery or persistent PTSS groups rather than into the PTSS-resistant group. However, we did not detect covariate-adjusted associations between race and relative risk of persistent versus recovery from PTSS. Pre-hurricane earnings were protective against delayed onset PTSS compared to never having PTSS. We found no evidence of associations between post-Katrina PTSS trajectory and other pre-disaster characteristics, including partnership status, ages of children, and social support.
In contrast, hurricane-related experiences were associated with within-individual changes in PTSS over time. Having a relative or friend die due to the hurricane predicted experiencing persistent PTSS compared to never experiencing PTSS, and with experiencing but then recovering from PTSS, again compared with never having PTSS. Bereavement did not predict trajectory outcomes among people who experienced PTSS at some point post-Katrina (i.e., those in the persistent, recovery, and delayed groups). We also found that each additional hurricane-related trauma was associated with a 17% increase in the risk of experiencing persistent PTSS rather than experiencing and then recovering from PTSS.
Table 5 describes associations between PD trajectories and individual characteristics. As expected, PD before Katrina heightened the risk of experiencing PD after the hurricane. Specifically, pre-Katrina PD increased the risk of being in the recovery and persistent PD trajectories when each was compared to a reference group that never experienced PD post-Katrina. Pre-hurricane PD did not affect the likelihood of recovering versus persistently experiencing PD. Pre-hurricane measures of age, race, earnings, and social support were not associated with within-individual changes in PD over time. However, marriage or co-habitation was protective against experiencing persistent PD when compared to two of the other outcomes: recovering from and experiencing new onset of PD. Having older children at the time of Katrina was associated with acquiring, or what we call, incident, PD in later waves relative to recovering from PD.
Table 5.
Relative risk ratios and (95% Confidence Intervals), multinomial logistic models of trajectories of PD (n=438)
| Model 1: PD | ||||||
|---|---|---|---|---|---|---|
| Recovered vs. Never (ref) | Incident vs. Never (ref) | Persistent vs. Never (ref) | Persistent vs. Incident (ref) | Incident vs. Recovered (ref) | Persistent vs. Recovered (ref) | |
| Age at time of hurricane | 1.01 (0.95, 1.09) | 0.94 (0.85, 1.05) | 1.02 (0.94, 1.11) | 1.08 (0.96, 1.22) | 0.93 (0.83, 1.04) | 1.00 (0.92, 1.09) |
| Baseline partnership status | ||||||
| Married/cohabitating | ||||||
| Not married/cohabitating | 1.24 (0.67, 2.29) | 1.48 (0.69, 3.22) | 0.60 (0.31, 1.15) | 0.40* (0.17, 0.98) | 1.19 (0.50, 2.83) | 0.48* (0.24, 0.97) |
| Race | ||||||
| Non-Black | ||||||
| Black | 1.32 (0.63, 2.78) | 0.81 (0.36, 1.83) | 0.91 (0.40, 2.07) | 1.12 (0.40, 3.09) | 0.62 (0.24, 1.60) | 0.69 (0.30, 1.58) |
| Children ages 0 to 5 | 0.80 (0.56, 1.15) | 1.24 (0.82, 1.89) | 0.93 (0.66, 1.33) | 0.7 (0.46, 1.21) | 1.55 (0.96, 2.52) | 1.16 (0.80, 1.71) |
| Children ages 6 to 11 | 1.04 (0.73, 1.51) | 0.78 (0.45, 1.37) | 0.90 (0.61, 1.33) | 1.15 (0.62, 2.16) | 0.74 (0.40, 1.37) | 0.85 (0.59, 1.24) |
| Children ages 12 to 17 | 0.71 (0.43, 1.18) | 1.51 (0.86, 2.63) | 0.86 (0.50, 1.47) | 0.57 (0.30, 1.07) | 2.11* (1.15, 3.88) | 1.20 (0.68, 2.11) |
| Log monthly earnings before hurr. | 1.05 (0.70, 1.61) | 0.96 (0.61, 1.52) | 0.84 (0.56, 1.27) | 0.88 (0.53, 1.45) | 0.91 (0.53, 1.54) | 0.80 (0.54, 1.17) |
| Social support before hurricane | 0.57 (0.31, 1.06) | 0.83 (0.37, 1.85) | 0.61 (0.31, 1.23) | 0.74 (0.30, 1.82) | 1.45 (0.61, 3.45) | 1.07 (0.53, 2.16) |
| PD before hurricane | 3.22*** (1.69, 6.15) | 2.02 (0.73, 5.54) | 4.94*** (2.48, 9.81) | 2.45 (0.89, 6.70) | 0.63 (0.23, 1.68) | 1.53 (0.80, 2.92) |
| Home damaged during hurricane | 1.45 (0.70, 3.03) | 0.62 (0.27, 1.39) | 1.52 (0.65, 3.56) | 2.45 (0.89, 6.75) | 0.43 (0.17, 1.09) | 1.04 (0.43, 2.54) |
| Hurricane traumas | 1.17** (1.05, 1.31) | 0.87 (0.70, 1.07) | 1.23** (1.07, 1.41) | 1.42** (1.13, 1.79) | 0.74** (0.60, 0.91) | 1.05 (0.91, 1.20) |
| Relative/friend died because of hurr. | 1.48 (0.87, 2.51) | 1.71 (0.74, 3.92) | 1.93* (1.07, 3.49) | 1.13 (0.46, 2.77) | 1.16 (0.49, 2.71) | 1.31 (0.73, 2.35) |
Notes: Two-tailed t-test.
p<.05,
p<.01,
p<.001.
Huber-White Robust Standard Errors in Parentheses. Estimated using multiple imputation.
Hurricane-related exposure and trauma mattered for PD trajectories. The number of hurricane-related traumas was associated with an increase in the risk of both recovery and persistent, relative to never. It also distinguishes those with an increase in the risk of experiencing persistent versus incident PD, and those with a decrease in the incident relative to recovery transitions. Incident PD was not associated with hurricane traumas. Finally, having a relative or friend die because of Katrina was a particularly important predictor of persistent PD, increasing the risk of experiencing persistent PD, versus never experiencing PD, by 93%. Home damage was not associated with PD trajectories.
Discussion
In the 12 years since Hurricane Katrina, rates of both PTSS and PD in our sample have declined. Before the present study, there was little prior research upon which to build expectations for these changes, such as whether rates of mental health symptoms would decline from five years to more than a decade post-disaster or would level off. Katrina-specific PTSS declined, but even after 12 years, symptoms remained in a sizeable proportion of the sample: exactly one in six (16.7%). We interpret this as a nonnegligible and uniquely vulnerable group who have a potential and need for continued recovery. Our sample proportion with PTSS symptoms is similar to the few other studies tracing long-term PTSS after a traumatic event, which range from 11.6% to about 17.0% (Goenjian et al., 2018). PD also remained high in the sample, persisted in the long-run, and did not return to pre-hurricane levels. In fact, our sample had consistently higher rates of SMI compared to the national estimate of 7.4% for African American adults below 100% of the poverty line in the National Health Interview Survey (National Center for Health Statistics, 2016).
In our covariate-adjusted models, pre-hurricane PD and exposure to traumatic events significantly predicted co-occurring PTSS and PD at each of the three post-hurricane follow-ups, including more than a decade later. Hurricane-related home damage and bereavement, however, no longer significantly predicted co-occurring PTSS and PD in the long-run. This finding is surprising because among the few studies that do trace survivors beyond a decade, several have found that housing damage and human loss are significant predictors of wellbeing, net of other factors (Oishi et al., 2015; Goenjian et al., 2018). Our divergent finding is likely explained by differences in study national contexts and the fact that these other studies do not control for pre-disaster wellbeing.
From a post-disaster aid perspective, it is thus the comparatively less “observable” measures of hurricane experience, namely trauma, that predict mental health problems in the long-term, rather than more easily-identifiable variables, such as housing damage. This poses difficulty for those concerned with providing resources and assistance to meet longer-range mental health needs. Whereas several hurricane-related variables were associated with PTSS without PD at prior post-disaster follow-ups, hurricane-related variables were no longer predictive of PTSS without PD in the long-term, highlighting the need for more studies of symptom comorbidity.
In our analysis of the trajectory of mental health, pre-disaster PD increased the risk of experiencing post-disaster PD, but it was not predictive of transitioning into or out of PD in subsequent time periods. This makes sense given that our measure of PD was not event specific, and respondents likely experienced other stressors in the interim periods. Hurricane traumas were a strong predictor of ever having PTSS relative to never having it, but not a powerful differentiating factor for transitions into or out of PTSS.
Finally, comparing the persistent versus the recovered groups is insightful for assessing the extent to which variables are particularly consequential for long-term change. Although home damage and having a family member or friend pass away are not significantly associated with persistent PTSS, relative to recovery, Katrina trauma increased the risk of having persistent PTSS relative to the risk of having recovered from PTSS. Although it is not possible to say whether this is a direct, long-term impact or an indirect one that impacts long-term PTSS through other pathways, hurricane traumas seem to have a lasting effect on mental health long after the acute experience.
In terms of sociodemographics, we found that with the exception of race, demographic characteristics are statistically unrelated to mental health outcomes long after Hurricane Katrina, although we note that our study sample is demographically homogenous. In the trajectory models, Black respondents were more likely to fall into the recovered or persistent PTSS groups rather than into the PTSS-resistant group, meaning they had an increased risk of PTSS in the immediate aftermath of the hurricane compared to other groups regardless of their recovery trajectory. We also detected that older respondents struggled more with PTSS on average in the short-term, but were also more likely to have the ability to recover. In the second follow-up, social support predicted experiencing PTSS alone relative to having neither mental health problem. One possible interpretation of this result is that due to the dispersion of social networks, those with close pre-Katrina social support were especially distraught following the storm (Morris & Deterding, 2016). Married or cohabitating mothers were at a lower risk of experiencing persistent or incident PD, controlling for other factors, suggesting that although not evident in the short term, marriage and/or cohabitation before the hurricane had a protective effect on later transitions of PD.
Several considerations are necessary to qualify the results above. The first is that our sample is not representative of the pre-Katrina New Orleans population, so it is important to exercise caution in generalizations. This is counterbalanced by the advantage of our large, yet non-representative sample: we have sufficient statistical power to model predictors of mental health within a population that prior research has suggested is particularly vulnerable to adverse outcomes following natural disasters (Fothergill & Peek 2004). Second, we rely on self-reported PTSS and PD, which are screening tools and not substitutes for clinical diagnoses, although previous research demonstrates a probable link between high scores on the IES-R and PTSD, and the K6 and mental illness (Weiss & Marmar, 1997; Kessler et al., 2003).
This study has several clinical and practical implications. Clinically, the high rate of PTSS in the long-term suggests that survivors’ disaster experiences should continue to be addressed as part of treatment. On the other hand, pre-disaster PD was a strong predictor of post-disaster outcomes, suggesting a need for services to address more longstanding mental health problems. As argued elsewhere, post-disaster interventions must be culturally informed to address barriers to care, e.g. stigma, specifically among black survivors (Wang et al., 2007). Practically, the results show that natural disasters exact an enduring toll on a sizable proportion of survivors. Disaster response efforts should reduce exposure to traumatic events by removing barriers to evacuation and should provide both immediate and long-term mental healthcare to those who have been exposed. Comprehensive economic and social estimates of natural disasters, especially under conditions of anthropogenic climate change, must therefore consider the enduring toll on mental health.
Hurricane-related traumas predict persistent post-traumatic stress symptoms (PTSS)
Twelve years after Katrina, PTSS remains in one in six sampled low-income mothers
Hurricane-related traumas predict comorbid psychological distress (PD) and PTSS
Pre-disaster PD increases the likelihood of adverse mental health in the long term
Acknowledgments
For helpful feedback, we thank Meghan Zacher, Subu Subramanian, and the Katrina@10 project teams at New York University and Tulane University. This study was funded by Eunice Kennedy Shriver National Institute of Child Health and Human Development grants P01HD082032, R01HD057599, and R01HD046162, National Science Foundation grant BCS-0555240, MacArthur Foundation grant 04-80775-000-HCD, the Robert Wood Johnson Foundation grant 23029, the Center for Economic Policy Studies at Princeton University, and the Harvard Center for Population and Development Studies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ethan J. Raker, Harvard University.
Sarah R. Lowe, Yale School of Public Health
Mariana C. Arcaya, Massachusetts Institute of Technology
Sydney T. Johnson, Harvard Center for Population and Development Studies
Jean Rhodes, University of Massachusetts, Boston.
Mary C. Waters, Harvard University
References
- Brodie M, Weltzien E, Altman D, Blendon RJ, & Benson JM (2006). Experiences of Hurricane Katrina Evacuees in Houston Shelters: Implications for Future Planning. American Journal of Public Health, 96(8), 1402–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2016. “Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities.” Hyattsville, MD. [PubMed] [Google Scholar]
- Chan CS, Lowe SR, Weber E, & Rhodes JE (2015). The contribution of pre- and postdisaster social support to short- and long-term mental health after Hurricanes Katrina: A longitudinal study of low-income survivors. Social Science & Medicine, 138, 38–43. [DOI] [PubMed] [Google Scholar]
- Chen SL-S, Lee C-S, Yen AM-F, Chen H-H, Chan C-C, Chiu SY-H, … Chang J-C (2016). A 10-year follow-up study on suicidal mortality after 1999 Taiwan earthquake. Journal of Psychiatric Research, 79, 42–49. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, & Failla S (2003). Psychometric properties of the Impact of Event Scale—Revised. Behaviour Research and Therapy, 41(12), 1489–1496. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, & Russell DW (1987). The provisions of social relationships and adaptation to stress. In Jones WH & Perlman D (Eds.), Advances in personal relationships: A research annual (Vol. 1, pp. 37–67). Greenwich, CT: JAI Press. [Google Scholar]
- Elliott JR, & Pais J (2006). Race, class, and Hurricane Katrina: Social differences in human responses to disaster. Social Science Research, 35(2), 295–321. [Google Scholar]
- EM-DAT. (2019). RetrievedJune 10, 2019, fromEM-DAT, The international Disaster Database website: https://www.emdat.be/
- IPCC (2012). Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change. Field CB, Barros V, Stocker TF, Dahe Q, Dokken DJ, Ebi KL, … Midgley PM (Series Ed.). [DOI] [PubMed] [Google Scholar]
- Fothergill A, & Peek LA, (2004). Poverty and disasters in the United States: a review of recent sociological findings. Natural Hazards 32 (1), 89–110. [Google Scholar]
- Frankenberg E, Friedman J, Gillespie T, Ingwersen N, Pynoos R, Rifai IU, … Thomas D (2008). Mental health in Sumatra after the tsunami. American Journal of Public Health, 98(9), 1671–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fussell E, & Lowe SR (2014). The impact of housing displacement on the mental health of low-income parents after Hurricane Katrina. Social Science & Medicine, 113, 137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fussell E, Sastry N, & Vanlandingham M (2010). Race, socioeconomic status, and return migration to New Orleans after Hurricane Katrina. Population and Environment, 31 (1–3), 20–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, … Kessler RC (2007). Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry, 64(12), 1427–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Tracy M, Norris F, & Coffey SF (2008). Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress, 21(4), 357–368. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Khachadourian V, Armenian H, Demirchyan A, & Steinberg AM (2018). Posttraumatic Stress Disorder 23 Years After the 1988 Spitak Earthquake in Armenia. Journal of Traumatic Stress, 31(1), 47–56. [DOI] [PubMed] [Google Scholar]
- Goldmann E, & Galea S (2014). Mental health consequences of disasters. Annual Review of Public Health, 35, 169–183. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, … Grant BF (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heid AR, Christman Z, Pruchno R, Cartwright FP, & Wilson-Genderson M (2016). Vulnerable, But Why? Post-Traumatic Stress Symptoms in Older Adults Exposed to Hurricane Sandy. Disaster Medicine and Public Health Preparedness, 10(3), 362–370. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med, 32 (2002), pp. 959–976 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, … Zaslavsky AM (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Galea S, Jones RT, & Parker HA (2006). Mental illness and suicidality after Hurricane Katrina. Bulletin of the World Health Organization, 84(12), 930–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knabb RD, Rhome JR, & Brown DP (2005). Tropical Cyclone Report, Hurricane Katrina, 23–30 August, 2005 (p. 43). Retrieved from National Hurricane Center website: https://www.nhc.noaa.gov/data/tcr/AL122005_Katrina.pdf
- La Greca AM, Silverman WK, & Wasserstein SB (1998). Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting and Clinical Psychology, 66(6), 883–892. [DOI] [PubMed] [Google Scholar]
- Logan JR (2006). The impact of Katrina: Race and class in storm-damaged neighborhoods. Spatial Structures in the Social Sciences, Brown University; 2006. Working paper. [Google Scholar]
- Manove EE, Lowe SR, Bonumwezi J, Preston J, Waters MC, & Rhodes JE (2019). Posttraumatic growth in low-income Black mothers who survived Hurricane Katrina. American Journal of Orthopsychiatry, 89(2), 144–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, & Van Hooff M (2009). Impact of childhood exposure to a natural disaster on adult mental health: 20-year longitudinal follow-up study. British Journal of Psychiatry, 195(2), 142–148. [DOI] [PubMed] [Google Scholar]
- Morris KA, & Deterding NM (2016). The emotional cost of distance: Geographic social network dispersion and post-traumatic stress among survivors of Hurricane Katrina. Social Science & Medicine, 165, 56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Nandi A, & Galea S (2008). Post-traumatic stress disorder following disasters: a systematic review. Psychological Medicine, 38(4), 467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, & Kaniasty K (2002). 60,000 Disaster Victims Speak: Part I. An empirical review of the empirical literature, 1981—2001. Psychiatry, 65(3), 207–239. [DOI] [PubMed] [Google Scholar]
- Oishi S, Kimura R, Hayashi H, Tatsuki S, Tamura K, Ishii K, & Tucker J (2015). Psychological adaptation to the Great Hanshin-Awaji Earthquake of 1995: 16 years later victims still report lower levels of subjective well-being. Journal of Research in Personality, 55, 84–90. [Google Scholar]
- Paxson C, Fussell E, Rhodes J, & Waters M (2012). Five years later: Recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Social Science & Medicine, 74(2), 150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes J, Chan C, Paxson C, Rouse CE, Waters M, & Fussell E (2010). The impact of Hurricane Katrina on the mental and physical health of low-income parents in New Orleans. The American Journal of Orthopsychiatry, 80(2), 237–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richburg-Hayes L, Brock T, LeBlanc A, Paxson C, Rouse CE, & Barrow L (2009). Rewarding Persistence: Effects of a Performance-Based Scholarship Program for Low-Income Parents. MDRC. https://eric.ed.gov/?id=ED503917 [Google Scholar]
- Rubin DB (1996). Multiple Imputation After 18+ Years. Journal of the American Statistical Association, 91(434), 473–489. [Google Scholar]
- Sastry N, & VanLandingham M (2009). “One Year Later: Mental Illness Prevalence and Disparities Among New Orleans Residents Displaced by Hurricane Katrina.” American Journal of Public Health, 99, 725–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uscher-Pines L (2009). Health effects of relocation following disaster: a systematic review of the literature. Disasters, 33(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Waters MC (2016). Life after Hurricane Katrina: The Resilience in Survivors of Katrina (RISK) Project. Sociological Forum, 31, 750–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Gruber MJ, Power RE, Schoenbaum M, Speier AH, Wells KB, & Kessler RC (2007). Mental Health Service Use Among Hurricane Katrina Survivors in the Eight Months After the Disaster.” Psychiatric Services 58(110): 1403–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster PJ, Holland GJ, Curry JA, & Chang H-R (2005). Changes in Tropical Cyclone Number, Duration, and Intensity in a Warming Environment. Science, 309(5742), 1844–1846. [DOI] [PubMed] [Google Scholar]
- Weems CF, Watts SE, Marsee MA, Taylor LK, Costa NM, Cannon MF, … Pina AA (2007). The psychosocial impact of Hurricane Katrina: contextual differences in psychological symptoms, social support, and discrimination. Behaviour Research and Therapy, 45(10), 2295–2306. [DOI] [PubMed] [Google Scholar]
- Weiss DS, & Marmar CR (1997). The Impact of Event Scale—Revised. In Assessing psychological trauma and PTSD (pp. 399–411). New York, NY, US: Guilford Press. [Google Scholar]


