Abstract
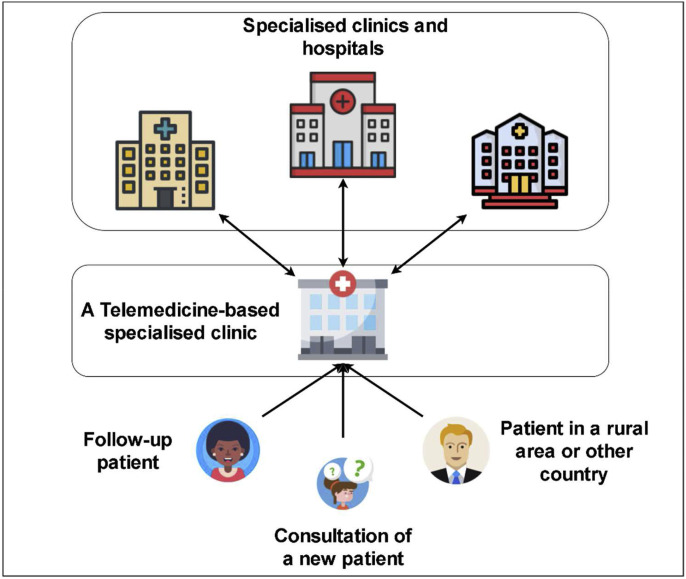
During the coronavirus disease (COVID-19) pandemic, different technologies, including telehealth, are maximised to mitigate the risks and consequences of the disease. Telehealth has been widely utilised because of its usability and safety in providing healthcare services during the COVID-19 pandemic. However, a systematic literature review which provides extensive evidence on the impact of COVID-19 through telehealth and which covers multiple directions in a large-scale research remains lacking. This study aims to review telehealth literature comprehensively since the pandemic started. It also aims to map the research landscape into a coherent taxonomy and characterise this emerging field in terms of motivations, open challenges and recommendations. Articles related to telehealth during the COVID-19 pandemic were systematically searched in the WOS, IEEE, Science Direct, Springer and Scopus databases. The final set included (n = 86) articles discussing telehealth applications with respect to (i) control (n = 25), (ii) technology (n = 14) and (iii) medical procedure (n = 47). Since the beginning of the pandemic, telehealth has been presented in diverse cases. However, it still warrants further attention. Regardless of category, the articles focused on the challenges which hinder the maximisation of telehealth in such times and how to address them. With the rapid increase in the utilization of telehealth in different specialised hospitals and clinics, a potential framework which reflects the authors’ implications of the future application and opportunities of telehealth has been established. This article improves our understanding and reveals the full potential of telehealth during these difficult times and beyond.
Keywords: COVID-19, E-Health, Pandemic, SARS-CoV-2, Telehealth, Telemedicine
1. Introduction
The onset of the COVID-19 pandemic has triggered the rapid shift from traditional care to telehealth [1]. Telehealth technologies have been maximised during public health emergencies, especially in disaster management [2]. On-demand telehealth is a 21st century approach which allows patients to be efficiently screened; the care provided is patient centred and conducive to self-quarantine. This approach protects patients, clinicians and the community from exposure. Moreover, it provides a platform where physicians and patients can interact regardless of time and day using smartphones or webcam-enabled computers. Early clinical signs of COVID-19 include respiratory symptoms, such as fever, cough, presence of sputum, dyspnoea, fatigue, myalgia, and nausea [3]. Automated algorithms are established into the intake process, and local and global epidemiologic information is used to standardise screening and practice patterns across providers; however, these actions require much effort [1]. Several studies were published during the different waves of the COVID-19 pandemic. These studies contributed to the use of telehealth and provided instructions on how to overcome COVID-19. However, no telehealth program can be created overnight. In addition, the telemedical innovations implemented in the USA can only be utilised for the response to COVID-19. In relation to the current pandemic, the authors published duplicate efforts with limited enhancements [4,5]. Thus, this systematic review was performed to investigate the diverse contributions of telehealth during the COVID-19 pandemic. This article provides a comprehensive review of the development of telehealth technologies, applications and approaches which allow the correct assessment of COVID-19 concerns, recommendations and challenges. However, the investigation of correlated improvement towards this multidisciplinary perspective has received minimal attention. Furthermore, a systematic literature review which provides extensive evidence on the impact of COVID-19 through telehealth and which covers multiple directions in a large-scale research remains lacking. This review aims to characterise the utilization of telehealth and its applications during the COVID-19 pandemic in terms of control status, technology used and medical procedure into a coherent taxonomy. Such an assessment is vital for the COVID-19 analysis estimates to determine the value of telehealth in the current pandemic. This article can serve as a reference for policymakers of telehealth technologies. The contributions of this article are summarised as follows:
-
1.
State-of-the-art telehealth and COVID-19 classification taxonomy are provided. Works in different fields are reviewed against such classification.
-
2.
The motivation, challenges and recommended solutions of the integrated fields of study are identified.
-
3.
The identified sets from point 2 are discussed and analysed in consideration of the following concepts: (i) control towards diseases and population; (ii) telehealth technologies towards implementations, strategies and guidelines; and (iii) medical procedures which include the urgent/non-urgent use of telehealth during the COVID-19 pandemic.
In this context, a systematic review can provide clear insights into the impact of telehealth on various fields. This review aims to provide deep insights into the important perspectives in the selected research topic. Moreover, the study aims to present the different contributions of previous research from various points of view.
2. Systematic literature review
This study was conducted in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). A comprehensive understanding of research interest in a specific topic can be achieved while presenting further information for future studies by using the PRISMA protocol [6]. Systematic reviews are an excellent method because of their huge impact on various scientific disciplines and research areas. The systematic review principally contains various processes, including searching techniques, data sources, eligibility criteria, study selection and data extraction [7].
2.1. Information source
Target papers were searched in the following digital databases: (1) ScienceDirect, which contains science and technology papers and articles in highly reliable journals; (2) IEEE Xplore, which provides the abstracts and full texts of papers on computer science, electrical engineering and electronics; (3) Scopus, a large curated abstract and citation database of scientific journals, conference proceedings and books; (4) Web of Science, which contains cross-disciplinary research on social science, science, technologies, humanities and the arts; and (5) Springer, which provides access to millions of scientific documents from journals, books, series, protocols, reference works and proceedings. These databases include sscientific and technical studies on wide and relevant disciplines.
2.2. Search strategy
A two stage-based comprehensive literature search was conducted in the abovementioned databases. The first stage was carried out on the December 8, 2020 after the main highlights of the manuscripts were drafted. The second search was conducted on the July 13, 2021 to ensure that updated and recent articles were included. The advanced search features of the selected databases were used. Two groups of keywords, along with disjunctive and conjunctive Boolean operators (i.e. OR), were employed. In search and filtration, different types of content publications (e.g. published articles, review articles and conferences) which cover the latest and most relevant articles on the designated review topic were considered. The search strategy was generated by the following keywords with respect to each database search strategy:
(‘Telehealth’ OR ‘e-health’ OR ‘Telecare’ OR ‘Telehealth’ OR ‘remote monitoring’ OR ‘mHealth’ OR ‘Medical system’ OR ‘health care service’ OR ‘Telemedicine’) AND (Disease OR Infection OR Virus OR Epidemic OR Outbreak OR Pandemic OR COVID-19 OR COVID-19 OR SARS-COV-2).
2.3. Eligibility criteria
The following criteria were used during the selection of related studies in this review:
-
1.
The article is in an English journal, review or conference paper.
-
2.
The article focuses on the integration of telehealth and its applications to various COVID-19-related contexts.
2.4. Study selection
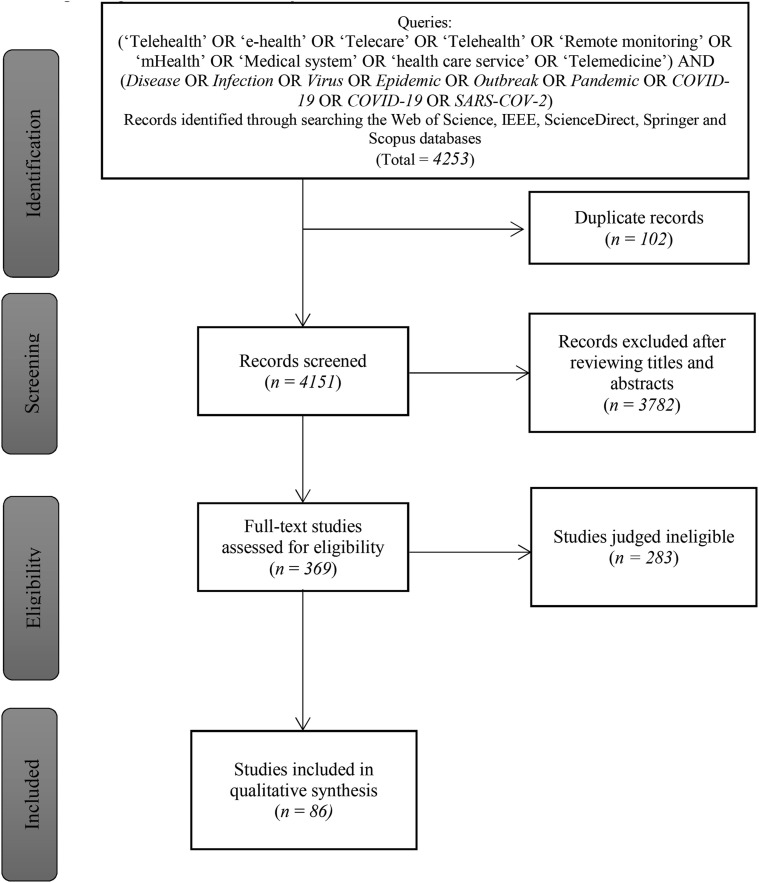
The search process of this study consisted of three sub-processes, namely, collection of articles, scanning of title and abstract and reading of the full text. Each article was assessed by two reviewers to ensure the inclusion criteria and the extracted data. Any disagreement between the two reviewers was resolved by a senior reviewer. The senior reviewer also evaluated the quality of the included articles to ensure their significance to this review. A total of 4253 articles were obtained from the selected databases in the first sub-process. However, 102 articles were duplicates across all the scanned databases. In the second sub-process, all associated articles were identified by scanning titles and abstracts. All articles were then examined by analysing and reading the title and abstract comprehensively to ensure that the eligibility criteria were met. Consequently, 3782 articles were excluded. All eligible articles were subjected to the third sub-process, where the full text was read, and all useful details were obtained to collect the final articles (n = 86), which met the inclusion criteria. During this process, comments and notes (i.e. data extraction) of various articles were collected to provide insights and to determine the final format of this review. Fig. 1 presents the taxonomy of related studies.
Fig. 1.
Taxonomy of related studies.
2.5. Data extraction and classification
The required data were extracted from each article and collected for further analysis. Numerous attributes were grouped and itemised using an Excel spreadsheet. These attributes are presented in Table 1 .
Table 1.
Data extraction and classification contents.
| Item | Description |
|---|---|
| Title | Title of the article |
| Year | Year of article publication |
| Challenges | Concerns and issues raised in the publication |
| Motivations | Identification of benefits or significance in the publication |
| Recommendations | Future directions or advisements of the publication |
| Nature of Application | How telehealth as an application was carried out |
The attributes illustrated in Table 1 were the most relevant attributes for achieving the key points of the systematic review. Each element was selected for a purpose. The title of the article was obtained for future referencing. Challenges were presented to show the readers and future researchers the issues and concerns encountered in previous studies. The motivations served to convey the advantages and significance of previous work. The recommendations were presented to provide the point of view of previous authors in future research and discussions. The nature of application showed how various applications of telehealth have been integrated, and such applications were the main points to be considered when drafting the taxonomy.
2.6. Quality assessment
A quality assessment checklist of 11 criteria was accorded based on the Critical Appraisal Skills Programs checklist and the accumulated list was developed and utilised by Ref. [8] to ensure the quality of the included studies. This method covers the design, data, analysis and conclusion of a research article. This method should cover all the needed parts for a research quality evaluation. Each assessed criterion could be assigned a quality score of 0 for ‘does not meet’, 0.5 for ‘partially meet’ and 1 for ‘fully meet’. The total quality score of each article ranges from 0 to 11. Therefore, a signified high-quality article is with high score. See Table 2 for the quality assessment criteria used.
Table 2.
Quality assessment checklist items.
| Quality Assessment Criteria | |
|---|---|
| Design |
|
| |
| |
| |
| |
| |
| Data acquisition |
|
| Data analysis |
|
| |
| Conclusion |
|
| |
2.7. Quality assessment results
The total score of most assessed studies was 7 or more, indicating the valuable contribution of these studies to this review. Articles with a total score less than 7 were selected because of their value in providing guidelines and framework of telemedicine utilization. However, 24 articles with a total score less than 3 were excluded. Therefore, 86 articles were included for the review. Most articles have not provided definitions of their evaluation metrics, and results were not compared with those of previous research. The results of each assessed study could be found in Appendix 1.
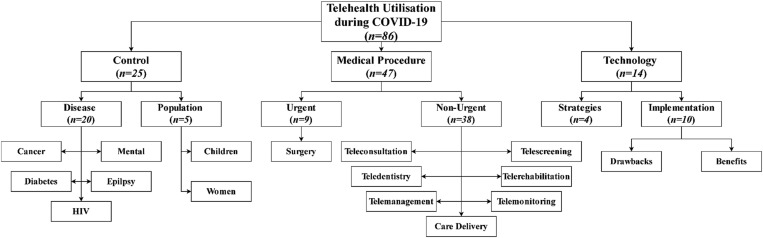
3. Taxonomy
The included articles are shown in Fig. 1. We retrieved 4253 records by searching the abovementioned databases. After the removal of duplicates (n = 112), 4151 works remained. After the review of titles and abstracts, 369 works met the initial selection criteria. After examining the full texts and conducting quality assessment, 86 articles met the inclusion criteria and were included in the final review, which was divided into three major categories. The first category included 25 articles which discussed COVID-19 control through telehealth. The second category contained 14 articles which focused on the technology-related aspects of telehealth and COVID-19. The third category contained 47 articles with a Medical Procedure section. Articles in this category discussed medical procedures which have been integrated into telehealth and used during the COVID-19 pandemic. We observed these patterns, summarised the general categories of articles and refined the classification into literature taxonomy, as shown in Fig. 2 . Several subcategories were identified in the main classes, but overlaps emerged. The subsequent sections describe the observed categories, and simple concomitant statistics are provided in Fig. 2.
Fig. 2.
Taxonomy of related studies.
3.1. Control
This section includes all articles discussing the control of COVID-19 through telehealth and is divided into two parts. The first part includes articles which discussed disease control (n = 20). The second part includes articles which discussed population control (n = 5).
3.1.1. Disease control
While scanning the articles pertaining to disease control, five main diseases were discussed, namely, diabetes, HIV, mental disorder, epilepsy and cancer. Many researchers of previous studies concentrated their studies on these diseases due to their high vulnerability of patients while being infected by COVID-19 more than others. Each disease was controlled and assessed during the COVID-19 pandemic via telehealth. The roles of telehealth and its integration in the control of each disease are discussed in the following sub-sections.
3.1.1.1. Diabetes
Telehealth is presented in the literature on the COVID-19 pandemic in different contexts, and its utilization has been related to the assistance provided to patients with diabetes. Three related works (n = 3) are included. The first work [9] stated that the restricted mobility of patients due to the threat of COVID-19 has complicated face-to-face hospital visits and treatment. The authors studied the feasibility of telehealth in such a scenario. They explored different ways to provide the best care to patients with diabetes. They also searched different scientific databases, such as PubMed and Google Scholar, for existing guidelines. The discussion was based on their search for evidence and general guidelines regarding the role, utility and limitations of telehealth in helping patients with diabetes. Their findings suggest that telehealth is a useful tool for patients with diabetes during the lockdown period despite the limited availability of data, but further research is required. The second study [10] stated that the controlled movement during the COVID-19 pandemic forced endocrinologists and diabetologists to adopt the remote delivery of diabetes care through telehealth. Such an approach might increase access to diabetes healthcare in certain settings. However, it is still jeopardised by the limited availability of diabetes technologies in underprivileged communities. The authors reported their experience with patients; they provided diabetes care effectively and prevented hospital admissions by using telehealth. They concluded that the pandemic opened new ways to manage high-risk patients through telehealth and may result in lasting benefits. In the third study [11], authors analysed the glucose monitoring systems of patients with type 1 diabetes after telemedicine visits. The data of continued and flash glucose monitoring systems were analysed before and after the telemedicine visits. The study concluded that structured telemedicine visits have a positive impact on the glycaemic control of type 1 diabetes and could replace or integrate face-to-face visits effectively.
3.1.1.2. HIV
While telehealth plays a significant role in controlling certain diseases, its use is unexpected for certain diseases such as HIV, especially in the middle of a COVID-19 pandemic lockdown. Two articles (n = 2) discussed the integration of HIV, COVID-19 and telehealth. The first study [12] discussed the care delivery disruption of HIV worldwide during the COVID-19 pandemic. Healthcare systems were expanded through the utilization of telehealth to deliver improved HIV health services and to cover patient needs during the COVID-19 pandemic. These services included HIV treatment and care. The authors claimed that despite the promising early results, providers must consider the implications of telehealth on the patient–provider relationship and the establishment of trust in ongoing care, particularly for the most vulnerable. Therefore, the authors suggested an approach focusing on the values and preferences of patients to improve opportunities in the new HIV care paradigm. The second study [13] discussed that the effective utilization of telehealth systems in HIV care is related to the high satisfaction ratings by patients. The authors also discussed the feasibility and acceptance of telehealth utilization in HIV care services, especially in remote or rural settings and among populations. The authors claimed that telehealth has several benefits, such as reducing the need for transportation in urban areas, i.e. long-distance travel, and addressing the limited transportation access. Moreover, it improved engagement in care and medication adherence, resulting in reduced HIV viral load. The authors reviewed a clinic's transition to telehealth and the implications of providing HIV prevention and care services via telehealth during the COVID-19 pandemic.
3.1.1.3. Mental disorder
Many related studies on mental disease and health have been published during the pandemic. Three studies (n = 3) focused on the utilization of telehealth to address mental disorder. The first work [14] discussed the response of the mental health network to the COVID-19 pandemic and the resource redeployment starting from the early weeks of the pandemic. The authors witnessed the application of psychiatric services to a contingency plan, which included redeployment of human resources, closure of several units and telehealth program implementation for mental health assistance. The second study [15] reported that the COVID-19 pandemic completely changed people's daily lives and psychotherapy clinical operations. Treatment engagement with a population suffering from serious mental illness (SMI) is inherently challenging. This study discussed that the COVID-19 pandemic may pose challenges to treatment engagement because of the rapid change in telehealth and the exacerbation of symptoms, pushing patients to shift to telehealth and stay engaged in treatment. They concluded that using telehealth to address populations with SMI during the pandemic is highly feasibly. The third work [16] stated that the COVID‐19 pandemic forced mental health providers to immediately change their care services, including cognitive processing therapy (CPT) for patients with post-traumatic stress disorder. The authors also discussed the affectivity of CPT when delivered in person or via telehealth and reviewed the restrictions on in‐person mental health therapy delivery throughout the COVID‐19 pandemic. Therefore, the authors presented treatment concerns and guidelines for consistent telehealth implementation during routine treatment assessment.
3.1.1.4. Epilepsy
Epilepsy is another important disease to which telehealth can be applied, and two related studies focused on this topic (n = 2). The first work [17] discussed the strengths and weaknesses of using telehealth for patients with epilepsy. Telehealth utilization during consultations between clinicians and patients with epilepsy has several advantages. For instance, the patients can save the time, consultation fees and travel expenses required to visit their doctors. In addition, patients living in areas with poor medical resources can have access to professional doctors and avoid public exposure, which is highly recommended during the COVID-19 pandemic. The authors also pointed out some limitations, including the difficulties related to physical consultation; examining patients online is challenging, and some epilepsy-related clinical tests, such as blood test, cannot be performed. However, these limitations do not downplay the role of telehealth, particularly during the COVID-19 pandemic. The second study [18] discussed the difficulty of delivering outpatient clinical care for patients with chronic neurological conditions, such as epilepsy, amidst the COVID-19 pandemic. Telehealth has become an option for addressing such difficulties. Furthermore, telehealth can potentially maintain outpatient care at pre-pandemic levels. Therefore, the authors evaluated their experience in a tertiary care epilepsy centre and found that scalable and robust telehealth can help maintain the smooth transition to outpatient care during the COVID-19 pandemic.
3.1.1.5. Cancer
Telehealth plays a major role in controlling serious diseases, such as cancer. Ten studies (n = 10) discussed the use of telehealth to control cancer. Authors in Ref. [19] stated that providing care and continuous support for patients with cancer has been difficult amidst the COVID-19 pandemic. The authors analysed the volume of visits to the Comprehensive Cancer Centre. They compared patient demographics and appointment data in the given time duration before and after the implementation of telehealth. The utilization of telehealth was rapidly scaled in a brief period in response to COVID-19; access to complex oncologic care was maintained while meeting social distancing requirements. Ref. [20] discussed patients with prostate cancer and their treatment. This study explained that the advantages of treatment during routine visits must be weighed against its risks and that resources must be utilised efficiently during the pandemic. Their main work presented several recommendations along with a framework for evaluating management decisions related to the provision of prostate radiation therapy via telehealth. This study showed that resources can be utilised efficiently for patients with prostate cancer in all identified stages. Furthermore, this framework can be utilised to assist in the decision making for other diseases during the global pandemic. Authors in Ref. [21] stated that public healthcare directives have significantly changed the practice of oncologic medicine for patients with cancer and social norms because of the national emergency triggered by COVID‐19. The authors implemented telehealth and a multidisciplinary approach to continue offering standard‐of‐care treatments amidst the pandemic. Considering the lack of feasibility data on telehealth for such patients with cancer, they reported their early experiences at a high‐volume cancer centre at the domestic epicentre of the COVID-19 crisis. Authors in Ref. [22] discussed the same type of cancer. The authors reported that healthcare workers had difficulty managing healthcare services because of the disruption caused by COVID-19 infections. In specific, health care providers experienced difficulty providing services to patients with head and neck cancer and managing the balance between infection risk and disease progression due to long waiting times. Therefore, the authors discussed their service disorder experience and how to address such issues during the COVID-19 pandemic via multi-institution collaboration and telehealth. Authors in Ref. [23] discussed the rapid evolution from the cessation of in-person counselling services to virtual telehealth treatments for tobacco-dependent patients with cancer. They examined the effect of the rapid scaling of tobacco treatment via telehealth on patient engagement, as measured by attendance rates for in-person counselling visits versus remote telehealth counselling visits. They described the challenges encountered by patients, clinicians and healthcare systems in the rapid expansion of individual and group tobacco telehealth services. Authors in Ref. [24] stated that patients with rare types of cancer travel long distances to receive care from experts. During the COVID-19 pandemic, extensive changes in cancer care delivery are required, including rapid telehealth care implementation. Therefore, the authors evaluated the impact of telehealth on patients, clinicians and care delivery during the pandemic and found that telehealth can revolutionise the delivery of cancer care, particularly for patients with rare cancers who often live far away from expert centres. Authors in Ref. [25] mentioned that the COVID-19 pandemic has compromised the peace of mind and mobility of patients and negatively affected the care for non-COVID-19 patients. They mentioned the role of telehealth in providing care services to the population during crises. The authors designed an exploratory survey to assess the changes in hospital-based palliative care practices during the COVID-19 pandemic and the patients’ awareness of cancer care telehealth services. Telehealth can be used to provide palliative care for patients in the community, especially those who lack means to visit healthcare professionals due to a pandemic or a natural disaster. Authors in Ref. [26] stated that many patients with cancer are visiting hospitals for treatment and for frequent status monitoring. Furthermore, immunocompromised patients can be at a higher level of infection risk. Patients with cancer have several risk aspects in common. Unfortunately, no global guidelines exist on how a patient with cancer can ask for assistance during a pandemic. Therefore, the authors reviewed critical issues related to the treatment of patients with cancer during the COVID-19 pandemic. Authors in Ref. [27] discussed different guidelines. The authors stated that the COVID‐19 pandemic caused many hospitals and practices to revoke outpatient clinic visits. Furthermore, most practices were inspired to utilise telehealth as an approach for continuing health care. Hence, the use of telehealth has expanded rapidly during the COVID-19 pandemic, even if patients and physicians lacked proper knowledge on how to utilise the best services. Therefore, the authors provided means for patients and physicians to access hand-outs to prepare them for clinic. Authors in Ref. [28] discussed telemonitoring patients with cancer by evaluating post-charge physical activity, vital signs and patient-reported symptoms of older patients post-discharge after oncological surgery. They demonstrated the complexity of detecting post-discharge complications following oncogeriatric surgery and reported that measurements of several parameters is required. Table 3 discusses the most important highlights regarding the control of each disease along with the references.
Table 3.
Control disease highlights.
| Reference | Highlights |
|---|---|
| Ghosh, Gupta and Misra, 2020 [9] | Discussing the feasibility of telehealth in providing patients with diabetes the best care |
| Peters and Garg, 2020 [10] | Discussing the provision of diabetes care remotely through telehealth during the COVID-19 pandemic |
| Boscari, Ferretto, Uliana, Avogaro and Bruttomesso, 2021 [11] | Evaluating the effects of telemedicine visits on patients with type 1 diabetes. |
| Mgbako, Miller, Santoro, Remien, Shalev, Olender, Gordon and Sobieszczyk, 2020 [12] | Discussing the global disruption of HIV care delivery and the use of telehealth to maintain HIV treatment adherence in COVID-19 |
| Rogers, Coats, Adams, Murphy, Stewart, Arnold, Chan and Nunn, 2020 [13] | Reviewing clinic's transition to telehealth and implications for providing HIV prevention and care services via telehealth during the COVID-19 pandemic |
| Roncero, García-Ullán, Javier, Martín, Andrés, Ojeda, González-Parra, Pérez, Fombellida and Álvarez-Navares, 2020 [14] | Describing the implementation of telehealth programs to assist people with mental health problems in the COVID-19 context |
| Miu, Vo, Palka, Glowacki and Robinson, 2020 [15] | Discussing treatment engagement for people with serious mental illness Discussing populations that rapidly switched to telehealth. |
| Moring, Dondanville, Fina, Hassija, Chard, Monson, LoSavio, Wells, Morland and Kaysen, 2020 [16] | Discussing how to effectively deliver telehealth and in‐person mental health therapy during the pandemic |
| Kuroda, 2020 [17] | Discussing strengths and weaknesses of telehealth with respect to patients with epilepsy during the COVID-19 pandemic |
| Punia, Nasr, Zagorski, Lawrence, Fesler, Nair and Najm, 2020 [18] | Discussing the delivery of outpatient clinical care to patients with epilepsy amidst the COVID-19 pandemic |
| Lonergan, Washington III, Branagan, Gleason, Pruthi, Carroll and Odisho, 2020 [19] | Discussing challenges in providing care and continuous support to patients with cancer in the Comprehensive Cancer Centre and during the COVID-19 pandemic |
| Zaorsky, James, McBride, Dess, Jackson, Mahal, Chen, Choudhury, Henry and Syndikus, 2020 [20] | Discussing the framework for the evaluation of patients with prostate cancer to assess therapy management decisions through telehealth during the COVID-19 pandemic |
| Kang, Wong, Sherman, Rybkin, McBride, Riaz, Tsai, Yu, Chen and Zakeri, 2020 [21] | Implementing telehealth and multidisciplinary approach to the continued provision of standard‐of‐care treatments for patients with cancer during the COVID-19 pandemic |
| Lee, Cho, Lau, Cheng, Wong, Ku, Chan and Yeung, 2020 [22] | Managing the disruption of healthcare cancer services during the COVID-19 pandemic |
| Kotsen, Dilip, Carter-Harris, O'Brien, Whitlock, de Leon-Sanchez and Ostroff, 2020 [23] | Examining the evolution from in-person counselling services to virtual telehealth treatments for tobacco-dependent patients with cancer during the COVID-19 pandemic |
| Smrke, Younger, Wilson, Husson, Farag, Merry, Macklin-Doherty, Cojocaru, Arthur and Benson, 2020 [24] | Delivery of cancer care through telehealth to patients living far from the health centres during the COVID-19 pandemic. |
| Atreya, Kumar, Samal, Bhattacharya, Banerjee, Mallick, Chakraborty, Gupta and Sarkar, 2020 [25] | Exploratory survey to assess the changes in hospital-based practices to raise caregiver's/patient's awareness about the telehealth services provided for cancer care during the COVID-19 pandemic |
| Al‐Shamsi, Alhazzani, Alhuraiji, Coomes, Chemaly, Almuhanna, Wolff, Ibrahim, Chua and Hotte, 2020 [26] | Reviewing potential challenges associated with the management of patients with cancer while suggesting practical approaches during the COVID-19 pandemic |
| Prasad, Brewster, Newman and Rajasekaran, 2020 [27] | Discussing different guidelines for using telehealth to maintain a continuum of care for patients with cancer during the COVID-19 pandemic |
| Jonker, Lahr, Oonk, de Bock and van Leeuwen, 2021 [28] | Discussing the effects of telemonitoring on cancer patients by evaluating post-charge physical activity, vital signs and patient-reported symptoms of older patients post-discharge after oncological surgery |
3.1.2. Population
An important aspect of a disease is its relation to a particular population. Authors were concerned with the role of telehealth in relation to populations during the COVID-19 pandemic. Populations are groups of people with designated specifications (i.e. children or women). Five studies (n = 5) were related to populations. Authors in Ref. [29] discussed that the utilization of telehealth has grown exponentially during the COVID-19 pandemic. The American Academy of Neurology guidelines deemed providing a paediatric practical framework for translating quality care necessary. The authors concluded that telehealth is important to reduce the physical exposure of patients, their families, physicians and the medical staff. Telehealth can effectively address the challenges and downplay the limitations of transportation and health care for the patients and their families. Authors in Ref. [30] reported that precautions were established to mitigate the spread of COVID-19, especially since the concern for the paediatric population has increased. This population is vulnerable to serious mental health consequences. The broad implementation of technology-based remote mental health services for children reportedly proceeded smoothly because of the worldwide stay-at-home directives and sudden changes in health care policy and reimbursement; public health crisis and the challenges encountered were also elucidated. Authors of a children-related study [31] discussed how telehealth was used to help treat paediatric obesity. The authors argued that obesity‐related health complications were apparent during the COVID-19 pandemic. Obesity reduction approaches are required early in life. Therefore, the authors discussed the development of a telehealth paediatric weight management collaborative system to prevent the exacerbation of health issues related to obesity risk factors. They also mentioned other effective interventions which can be delivered remotely to vulnerable children with obesity. Telehealth challenges were discussed, including those related to access of digital technology, privacy, security and social and linguistic differences. Solutions to these issues would support the full realisation of a weight control telehealth strategy for children. Aside from children, women are another important population targeted in the study. Two studies reported that different disease control measures were carried out via telehealth to help women with various medical conditions. Authors in Ref. [32] discussed the rapid integration of telehealth into prenatal care for pregnant women. The implementation goals included consolidating in-person prenatal screening, surveillance and examinations to reduce the number of in-person visits. Furthermore, the implementation goal is to maintain a patient's current antenatal care through telehealth virtual consultations. According to their findings, the incorporation of telehealth into prenatal care was beneficial. However, telehealth virtual visits are not meant to replace in-person prenatal care consultations completely. These visits offer a way to reduce exposure to COVID-19 infections while delivering enhanced in-person medical services. In a review [33], authors searched the Medline and Cochrane databases to identify guidelines and create an expert consensus on the control of outpatient gynaecological problems via telehealth. Their review provided relevant guidelines and summaries. The review included 51 studies on the use of telehealth in gynaecology, and findings of these studies were combined with the society guidelines and expert consensus. In their conclusion, the authors discussed the most suitable and efficient guidelines for treating gynaecological conditions via telehealth during the COVID-19 pandemic. Table 4 lists the most important highlights of each study on population control along with the references.
Table 4.
Control population highlights.
| Reference | Highlights |
|---|---|
| Sattar and Kuperman, 2020 [29] | Discussing the utilization of telehealth to provide paediatric service |
| Gurwitch, Salem, Nelson and Comer, 2020 [30] | Discussing the incorporation of telehealth in paediatric otolaryngology practice during the COVID-19 pandemic. |
| Woo Baidal, Chang, Hulse, Turetsky, Parkinson and Rausch, 2020 [31] | Discussing the growing concerns regarding paediatrics and the implementation of technology-based remote mental health services for children during the COVID-19 pandemic. |
| Aziz, Zork, Aubey, Baptiste, D'alton, Emeruwa, Fuchs, Goffman, Gyamfi-Bannerman and Haythe, 2020 [32] | Discussing how telehealth was used to help alleviate paediatric obesity during the COVID-19 pandemic |
| Grimes, Balk, Dieter, Singh, Wieslander, Jeppson, Aschkenazi, Kim, Truong and Gupta, 2020 [33] | Discussing how telehealth was rapidly integrated into prenatal care for pregnant women during the COVID-19 pandemic |
3.2. Technology
While scanning the literature, 14 articles related to technology, telehealth and COVID-19 were found. These articles were about technology implementation (n = 10) and strategies and guidelines (n = 4).
3.2.1. Implementation
Technology-related aspects varied in their applications. Many technologies were applied to telehealth implementation in relation with COVID-19, as discussed in 10 articles. Authors in Ref. [34] discussed A Guide to Rapid Implementation of Telehealth Services. The authors argued that the strain placed on telehealth capacity by the COVID-19 pandemic caused certain limitations, including restricted insurance contracting, high training costs, low reimbursement, software constraints and insufficient equipment. The authors claimed that telehealth support has minimised some of the required adaptations and limitations, thereby expediting the rapid expansion of telehealth. The authors delivered paediatric service providers with a related guide for telehealth practice expansion through the COVID-19 pandemic. This guide contains five sections, namely, visit implementation, planning, billing/documentation, guiding principles and general telehealth adaptation principles and specific applications. Authors in Ref. [35] discussed telehealth implementation methodologies in relation to the rapid implementation of telehealth in the future. The authors reviewed the current telehealth landscape, including the usage, policies and techniques for ambulatory practice integration. They also reviewed recent trends in telehealth, governmental recommendations for health care delivery during the COVID-19 pandemic and in the future of telehealth. An implementation study [36] stated that ample opportunities to utilise telehealth for distance patient care provision have opened during the pandemic. Numerous health systems transitioned to telehealth to provide outpatient care. Telehealth can be utilised in inpatient care to improve physical distancing for the safety of patients. Authors evaluated the rapid telehealth program utilization to secure inpatients and to improve inpatient telehealth quality initiative. Successful implementation and scaling resulted in a secure telehealth program which provides an instinctive naming convention to providers and capitalises on the widespread use of smartphones and tablets. Another study [37] reported that substantial constraints and obstacles in the provision of in-person health care have arisen because of the threat of COVID-19. The telehealth model can be utilised effectively to improve patient access to subspecialty care. This model includes a multidisciplinary care approach with various therapeutic interventions. The study summarised the learning experiences and essential concerns for telehealth care implementation during the COVID-19 pandemic and beyond. Their most important experiences significantly led to the recognition of various issues related to telehealth implementation, including (1) treatment initiation and patient examination; (2) telehealth visit set-up and structure while maintaining patient privacy; (3) reimbursements and billing considerations; (4) tele-visit limitations and services which do not meet the care needs of patients; and (5) optimisation of the tele-visit. As presented in Ref. [38], a telehealth system was implemented in a healthcare hospital to protect patients from COVID-19 transmission and manage patients infected with COVID-19. The implemented system was assessed by an expert team. The system helped achieve the goals of reaching the stratification of safe risk COVID-19 patients, managing outpatients safely and using the hospital resources appropriately and efficiently during the pandemic. Authors in Ref. [39] presented a survey and implementation of telehealth. The authors examined the perception of mental health clinicians who utilised telehealth services. Despite their limited experience on telehealth in the context of the COVID-19 pandemic, many clinicians adapted to the implementation of telehealth. In Ref. [40], a foetal ultrasound telemedicine service in foetal medicine centres was implemented. This study found that women in obstetric units received foetal medicine consultations in a reliable and feasible option by telemedicine. Furthermore, a telehealth service in radiation oncology was implemented during the COVID-19 pandemic to allow patients access to care [41]. A framework and usage guidelines were developed for incorporating telehealth into on-treatment and follow-up care. Results showed that the implementation of telehealth services generated a positive experience impact and that telehealth services could be broadly used even after the pandemic. Another study [42] implemented a telemedicine service based on phone-call visits to follow-up with patients with benign urological diseases during the COVID-19 pandemic. During the phone call visit, a questionnaire based on 17 items was developed and administered to patients to evaluate their health status and perceptions towards the implemented telemedicine approach to the management of their condition. Results showed that most patients had positive experience towards using telemedicine services for their condition management. Authors in Ref. [43] evaluated the impact of telehealth implementation on underserved populations and no-show rates (e.g. low-income, non-English-speaking and minority patients). A cross-sectional analysis in a medical centre was conducted comparing clinic visits in 2019 with telehealth visits in 2020 in terms of patient demographics. Results indicated that the implementation of telemedicine resulted in changes to patient populations, such as an increased number of non-English-speaking patients, slightly younger patients and white patients with telehealth. The number of Medicaid enrolees in primary care also increased.
3.2.2. Strategies and guidelines
Four studies were related to telehealth with technology strategies during the COVID-19 pandemic. Authors in Ref. [44] stated that systematic protocols are required to guide the use of telehealth interventions in response to COVID-19 outbreaks. Therefore, authors informed health care partners about the collaborative use of telehealth-centred strategies to improve facility outcomes during outbreaks. The facility team is supported remotely by using rapidly deployed technological solutions for the early identification of patients who need their care, monitoring and treating patients, care coordination and the assessment of daily facility needs. They argued that their telehealth-based approach can be incorporated into health care systems to address COVID-19 outbreaks. Another study [45] discussed the strategic role of telehealth technologies in managing the COVID-19 pandemic. Their work provided information published and discussed by scholars and managers from different sources. The authors discussed the implications of telehealth during the outbreak. Therefore, they provided invaluable information related to the impact of telehealth technologies on flattening the COVID-19 infection curve. A telehealth strategy was developed and provided by the authors of this study [46]. The strategy aimed to mitigate the adverse effects of COVID-19 by combining telehealth and medical training. The tele-screening service was operated by supervised medical students, and they were offering potential patients and patients with COVID-19 a free service for supervision purposes. In parallel, medical students were receiving up-to-date information about COVID-19 from professors to assess them with the patients. This strategy reduced the transmission of COVID-19 and allowed medical students to engage in real-life cases and contribute to fight the pandemic. Authors in Ref. [47] aimed to provide guidelines to healthcare workers for performing neurological examination using telemedicine services during the COVID-19 pandemic. A protocol was developed for outpatient visits to provide neurological examination. The findings of the study indicated that the neurosurgical providers gained sufficient information during the telemedicine visits by using the study guidelines to formulate a treatment plan. However, the techniques in the study require validation in the neurosurgical community. Table 5 lists the highlights of the studies on technology implementation and guidelines along with the references.
Table 5.
Highlights of technology section.
| Reference | Highlights |
|---|---|
| Berg, Picoraro, Miller, Srinath, Franciosi, Hayes, Farrell, Cole and LeLeiko, 2020 [34] | Discussing a guide for telehealth service's rapid implementation during the COVID-19 pandemic |
| Saleem, Pasquale, Sidoti and Tsai, 2020 [35] | Discussing telehealth implementation methodologies with the future rapid expansion of telehealth during the COVID-19 pandemic |
| Hron, Parsons, Williams, Harper and Bourgeois, 2020 [36] | Evaluating the usage of a secure and rapidly implemented telehealth program to improve inpatient telehealth quality during the COVID-19 pandemic |
| Strohl, Dwyer, Ma, Rosen, Schneider and Young, 2020 [37] | Providing a summary of learning experiences and essential concerns for telehealth care implementation during the COVID-19 pandemic and beyond |
| Cassar, Borg, Camilleri, Schembri, Anastasi, Buhagiar, Callus and Grech, 2021 [38] | Implementing a telehealth system in a healthcare hospital to protect patients from COVID-19 transmission and managing the infected patients with COVID-19 |
| Gentry, Puspitasari, McKean, Williams, Breitinger, Geske, Clark, Moore, Frye and Hilty, 2021 [39] | Implementing telehealth to examine the perception of mental health clinicians who utilised telehealth services |
| Smith, Marshall, Lie, Bidmead, Beckwith, Van Oudgaarden and Robson, 2021 [40] | Implementing a telemedicine-based foetal ultrasound in foetal medicine centres |
| Goenka, Ma, Teckie, Alfano, Bloom, Hwang and Potters, 2021 [41] | Implementing a telehealth service in radiation oncology during the COVID-19 pandemic to allow patients access to care |
| Checcucci, De Luca, Alessio, Verri, Granato, De Cillis, Amparore, Sica, Piramide and Piana, 2021 [42] | Implementing a telemedicine service in a urology department to follow-up with patients with urological benign diseases during the COVID-19 pandemic |
| Franciosi, Tan, Kassamali, Leonard, Zhou, Krueger, Rashighi and LaChance, 2021 [43] | Evaluating the impact of telehealth implementation on underserved populations and no-show rates |
| Harris, Archbald-Pannone, Kaur, Cattell-Gordon, Rheuban, Ombres, Albero, Steele, Bell and Mutter, 2020 [44] | Discussing and reviewing the systematic protocols for guiding telehealth intervention during the COVID-19 pandemic |
| Leite, Gruber and Hodgkinson, 2020 [45] | Discussing the strategic role of telehealth technologies in managing the COVID-19 pandemic. |
| Cerqueira-Silva, Carreiro, Nunes, Passos, Canedo, Andrade, Ramos, Khouri, Santos and Nascimento, 2021 [46] | Discussing the strategies of telehealth to mitigate the adverse effects of COVID-19 by combining telehealth and medical training |
| Basil, Luther, Burks, Govindarajan, Urakov, Komotar, Wang and Levi, 2021 [47] | Providing guidelines to healthcare workers for performing neurological examination using telemedicine services during the COVID-19 pandemic |
3.3. Medical procedure
While scanning the literature, 47 articles related to medical procedures were found. Such medical procedures include the use of telehealth during COVID-19 for urgent (n = 9) and non-urgent (n = 38) operations. They are discussed in the following sub-sections.
3.3.1. Urgent
For urgent medical procedures, the literature was engulfed around the use of telehealth to aid surgical operations and programs. Different surgical procedures were mentioned and discussed in the following sub-section.
3.3.1.1. Surgery
Telehealth significant integration to minimise the burden on the health sector and government was demonstrated during the COVID-19 pandemic. Considering that surgery is an important procedure, nine works discussed telehealth efforts with respect to performing surgery. Authors in Ref. [48] explored the role of telehealth as an essential instrument of health care service delivery, especially during the pandemic. They argued that its benefits include saving money and time and preventing infections among health care providers. Therefore, the authors evaluated the safety and effectiveness of telehealth visits in providing neurosurgical patients with post-operative care. The findings prove that telehealth is a safe and effective way of delivering post-operative care during the COVID-19 pandemic. Authors in Ref. [49] discussed that due to the pandemic, telehealth was utilised for only post-operative visits in neurosurgery, which led to the rapid expansion of telehealth to address the requirements of the neurosurgical patient population. Based on their analysis, the use of telehealth drastically increased across all divisions of neurosurgery, with a significant increase in online-first encounters, to meet the needs of patients. The lessons learned were discussed in anticipation of the role of telehealth in surgical practices. Authors in Ref. [50] investigated how telehealth can assess the current telehealth utilization capabilities of surgery programs and departments in the United States. This study showed how to determine practice patterns and how these patterns have been immediately impacted by COVID-19. They claimed that the needs of patients were impressively met; furthermore, the authors recognised a significant increase in new telehealth contributions, which are positively correlated with COVID-19 disease burden. Authors in Ref. [51] discussed that the COVID-19 pandemic has forced health care providers to use additional resources and to make extreme changes in terms of physician–patient standard encounter. Significant enhancements have been achieved in technology, which led to different forms of medical practice (i.e. telehealth). The feasible delivery of a viable spine surgery with the use of telehealth would be an advantage. Therefore, various physicians shared their experiences in utilizing telehealth for clinical care delivery. They concluded that the appropriate selection of patients requires a comparison between virtual treatments and in-person visits. Authors in Ref. [52] conducted a teleconference with 13 spine surgeons from across various hospitals to serve as a panel of experts. They discussed topics related to surgeon repurposing, spine telehealth introduction, service continuity, preoperative testing, spinal surgery triaging, new challenges in spine surgeries and post-pandemic preparations. Finally, some guidelines were provided to address issues of spine surgeries during the COVID-19 pandemic and to promote such discussions among other national or regional societies. Authors in Ref. [53] discussed that the COVD-19 pandemic has significantly interrupted neurosurgical care delivery, especially for at-risk neuro-oncologist population. Concurrently, the sudden changes in clinic visits have driven the rapid implementation of telehealth. Therefore, authors discussed a new recommendation care paradigm of neuro-oncologic patients limited by telehealth. They concluded that telehealth, which has become popular during the COVID-19 pandemic, is a powerful and possibly preferential tool for delivering outpatient neuro-oncologic care. Authors in Ref. [54] observed a rapid increase in the number of telehealth visits amidst the COVID‐19 pandemic. However, patient satisfaction with visits to head and neck surgeons remains to be evaluated extensively. Therefore, authors have conducted various surveys that consider patient satisfaction and have identified whether or not telehealth is an appropriate means of care. Results showed that patients were generally highly satisfied with telehealth. Authors in Ref. [55] surveyed neurosurgeons and advanced practice providers to characterise their experience in utilizing telehealth services. They found that telemedicine was heavily utilised for new consultations and post-operative follow-up with patients, despite the limitation of performing neurological examination. Despite the reported limitations, the study indicated that the use of telemedicine will likely continue after the pandemic because its benefits outweigh its limitations. Authors in Ref. [56] evaluated the utilization of telemedicine in paediatric surgery and discussed the experiences of patients and surgeons with telemedicine. They found that the pandemic boosted the utilization of telemedicine in paediatric surgery. Surgeons and patients were open to telemedicine and expressed satisfaction with its service. These findings indicate the applicability of telemedicine in paediatric surgery. Table 6 lists the highlights of urgent medical procedures along with the references.
Table 6.
Highlights of urgent medical procedure section.
| Reference | Highlights |
|---|---|
| Ashry and Alsawy, 2020 [48] | Evaluating the safety and effectiveness of telehealth visits in offering post-operative neurosurgical care for patients during the COVID-19 pandemic |
| Mouchtouris, Lavergne, Montenegro, Gonzalez, Baldassari, Sharan, Jabbour, Harrop, Rosenwasser and Evans, 2020 [49] | Discussing the telehealth utilization and post-operative visits only in neurosurgery to address the needs of the patients during the COVID-19 pandemic |
| Parisien, Shin, Constant, Saltzman, Li, Levine and Trofa, 2020 [50] | Investigating how telehealth can assess the current telehealth utilization capabilities at surgery programs and departments during the COVID-19 pandemic |
| Franco, Montenegro, Gonzalez, Hines, Mahtabfar, Helgeson, Patel and Harrop, 2020 [51] | Discussing improvement in technology and the feasibility of performing a sustainable spine surgery utilizing telehealth during the COVID-19 pandemic |
| Tan, Thadani, Chan, Oh and Liu, 2020 [52] | Discussing and providing guidance related to the introduction of telehealth, triaging of spinal surgeries and guidance during the COVID-19 pandemic |
| Daggubati, Eichberg, Ivan, Hanft, Mansouri, Komotar, D'Amico and Zacharia, 2020 [53] | Discussing neurosurgical service delivery for a population of at-risk neuro-oncology patients and the telehealth care paradigm implementation during the COVID-19 pandemic |
| Layfield, Triantafillou, Prasad, Deng, Shanti, Newman and Rajasekaran, 2020 [54] | Discussing head and neck surgeon visits and patient satisfaction with such visits during the COVID-19 pandemic |
| Ryu, Kerolus and Traynelis, 2021 [55] | Evaluating neurosurgeons and advanced practice providers to characterise their experience in utilizing telehealth services |
| Lakshin, Banek, Keese, Rolle and Schmedding, 2021 [56] | Discussing the utilization of telemedicine in paediatric surgery clinic, and evaluating the experiences of patients and surgeons with telemedicine |
3.3.2. Non-urgent
For non-urgent medical procedures, the literature discussed the following aspects of telehealth utilization during the COVID-19 pandemic: tele-monitoring, management, screening, tele-dentistry, tele-consultation and delivery of care. All these aspects are discussed in the following sub-sections.
3.3.2.1. Tele-monitoring
The term “tele-monitoring” refers to the ability of measuring, storing and forwarding detailed information of patients at any particular moment in time [57]. Four studies used telehealth for monitoring. Authors in Ref. [58] discussed the use of telehealth to monitor COVID-19 patients with mild symptoms who were sent home to recover, considering that some of these patients might deteriorate with disease progression. A telehealth model considering the shortage in the medical workforce was developed to monitor home-quarantined patients with COVID-19 who are at risk of deterioration with disease progression. The telehealth system reduced the delayed hospitalisation risks caused by disease spread and helped patients through self-assessment of their conditions. Patients were able to update the multidisciplinary team via a telehealth cloud-based form. Authors in Ref. [59] described the experiences and lessons learned while designing and implementing a virtual tele-monitoring COVID-19 clinic for patients suspected of having COVID-19. Suspected or confirmed COVID-19 cases were enrolled in telehealth visits every 24 h–72 h based on the severity of the symptoms, and the required care was escalated to in-person care when needed. They concluded that virtual tele-monitoring is an effective surveillance strategy. Virtual tele-monitoring permits close monitoring while maintaining minimum patient and care provider exposure. Authors in Ref. [60] assessed whether or not telehealth with tele-monitoring is a clinically useful and safe tool for monitoring patients with COVID-19. Their results indicate that telehealth with at-home tele-monitoring allows for the clinically useful and safe monitoring of high-risk patients with COVID-19 when used proactively. This approach can help with overall health improvement during the current pandemic. Authors in Ref. [61] analysed the role of tele-monitoring patients with heart failure (HF) during the COVID-19 pandemic and found that this technique expanded the access of patients to cardiac care.
3.3.2.2. Tele-management
Tele-management is the combination of teleconsultation and tele-monitoring services by offering continuous monitoring of outpatients for proper post-treatment management while providing an interaction or consultation between patients and health workers [62]. For tele-management studies, six articles mentioned how telehealth can help manage certain cases. Authors in Ref. [63] aimed to manage emergency patients for dental procedures. Authors provided general knowledge about COVID-19 disease and indications for the management of emergency dental procedures on the basis of recent literature and previous experiences to prevent cross infections in the dental office. Furthermore, they described their experience and highlighted the potential of telehealth for dental practitioners. Authors in Ref. [64] explored the role of telehealth in weight management. The number of in‐person clinical care visits was reduced to comply with the social distancing requirement during the pandemic. Health service providers and patients were urged to adopt clinical care and learn new skills. Furthermore, regulatory organisations and policy makers changed existing policies to meet national emergency requirements. Authors in Ref. [65] discussed the management of orthopaedic cases via telehealth during the COVID-19 pandemic and found that this technique was used to manage and diagnose patients with knee pain. Such encounters are challenging and require high knowledge and action steps to reduce complication risks with expanded telehealth utilization during this pandemic and beyond. Authors in Ref. [66] stated that telehealth is a significant technology for providing sustainable solutions and is an effective communication method during the pandemic. Amid the travel restrictions, lockdown and requirements for physical and social distancing which might affect visits to health care facilities, telehealth can be utilised to provide vital health care services, especially for chronic pain management. Therefore, the authors enumerated the challenges in pain management during the COVID-19 pandemic and discussed telehealth utilization in rescue management vehicles. Authors in Ref. [67] discussed HF management during the COVID-19 outbreak. Authors investigated whether or not the telehealth service established by the Heart Failure University Tertiary Centre 2 during the COVID‐19 outbreak can affect HF. The authors also compared outcomes in terms of period/year, specifically when telehealth was not yet available. They concluded that telehealth allows the follow‐up of HF patients during the COVID‐19 lockdown; it has a positive impact on the outcome. These results indicate that telehealth is a valuable tool which can be used in HF management, as shown for the first time during the COVID‐19 outbreak. Authors in Ref. [68] discussed that people have increasingly become dependent on telehealth platforms to handle outpatient pathology. However, they argued that telehealth approaches have limitations in providing the necessary health care to obtain comprehensive physical examinations. They claimed that several smartphone-based accessories can be used to transmit patient-obtained images. They presented different cases, in which an over-the-counter otoscope was used to change otologic management when social distancing. Furthermore, they improved the efficacy and safety of the examination, which was handled by patients at home with optimised utilization.
3.3.2.3. Tele-screening
Three studies on screening in relation to telehealth efforts during the COVID-19 pandemic were found. The first study [69] discussed some diagnosis issues which hinder health systems from making quarantine decisions, such as shortage of hospital beds and medical supplies, should the number of suspected cases exceed a certain threshold. This study introduced a novel screening strategy which includes consulting experts from centres around the world to provide services in regions with limited access to expertise during the COVID-19 pandemic. The second study [70] recommended telehealth for screening suspected patients to mitigate exposure risks and maximise the protection of the medical staff. This study established a strategy to limit COVID-19 exposure in the emergency department. The patient examination room was equipped with intercom and iPad devices for telecommunication in accordance with a telehealth screening protocol. Then, physicians allowed visual examination of patients via intercom or video conference. The third study [71] reported that many methods are required to screen patients while adhering to physical distancing and other guidelines by Centres for Disease Control and Prevention. Despite the low amount of data on the use of on-demand telehealth to meet the screening needs of patients, this study developed a remote patient screening approach which analysed patient requests. The approach was suitable for preventing patients from visiting health care facilities, which reduced physical contact and the use of personal protective equipment by health care workers.
3.3.2.4. Teledentistry
Two studies on teledentistry were found. The authors discussed how telehealth was used for teledentistry during the COVID-19 pandemic. Authors in Ref. [72] discussed the advantages of using telehealth in dental practice during the COVID-19 pandemic. They listed the various advantages, including the reduction of costs and limitation of human contact, which would decrease the risk of COVID-19 spread. Authors in Ref. [73] discussed the importance of teledentistry during the pandemic. They provided a brief overview of the application of teledentistry and claimed that they offered novel solutions for dentists to resume their practice. They suggested that teledentistry should be incorporated into routine dental practice even after the pandemic.
3.3.2.5. Teleconsultation
The term ‘tele-consultation’ can be defined as an electronic communication between a health professional and a patient or another health professional for delivering health care services [74]. Sixteen articles discussing telehealth as a teleconsultation service during the COVID-19 pandemic were found. Authors in Ref. [75] evaluated the effectiveness of telehealth video consultation services in providing remote health care during the COVID-19 pandemic and assessed patient satisfaction. They claimed that teleconsultation is an effective approach with a high satisfaction rate and plays a major role in supporting vulnerable patients and preventing transmission and infection. Authors in Ref. [76] explored the effectiveness of advanced telecommunication measures in providing all-inclusive and precise teleconsultation services in a resource-limited environment and to vulnerable patients, especially those with behavioural and psychological disorders. They reported that teleconsultation is one of the few feasible options for providing medical advice during the pandemic. Meanwhile, authors in Ref. [77] described and evaluated a risk-stratified prioritisation route for teleconsultation services during the pandemic. The authors asserted that consultations can be managed between a patient and physician in a safety-conscious manner by implementing a novel prioritisation means, which can assist greatly in difficult times, reduce transmission risk and minimise the health care system load, thereby maintaining appropriate health care services for patients. Authors in Ref. [78] described the tele-consultation service experience of a multi-tier hospital network in India during the COVID-19 lockdown. They discussed that teleconsultation tracking and patient information access via electronic medical records allowed the timely initiation of responses. In addition, the current experience provided important insights to manage and monitor patients remotely in the future. Authors in another study [79] discussed the enormous need for telehealth consultation during the COVID-19 pandemic. Authors from the Mayo Clinic argued that tele-consultation services inspired health care institutions to define new ways to follow-up and track individuals who are confirmed or suspected to have COVID-19. They described systems to provide health care to patients virtually, thereby succeeding in meeting the needs of confirmed or suspected cases safely and providing them with systematic health care services during the pandemic. Authors in Ref. [80] discussed potential pitfalls in teleconsultation services during the COVID-19 pandemic and how they can be avoided. They discussed the future of telehealth in health care systems and suggested appropriate settings with enhanced documentations, suitable training and information communication and observation guidelines to avoid remote consultation issues. Authors in Ref. [81] analysed and reported teleconsultation data provided to paediatric patients in the midst of the COVID-19 pandemic to guide future teleconsultation practices on how to assist patients with other health care needs. Such data were beneficial, and patients were encouraged to use the teleconsultation platform and explore currently available multimedia technologies, such as video conferencing and web/mobile-based applications, which can provide a reliable service in patient care. Authors in Ref. [82] attempted to determine the feasibility and patient acceptance of switching to teleconsultation during the COVID-19 pandemic. The collected data on the beliefs about social distancing, perceptions about the clinical examination and the satisfaction score of the first teleconsultation indicated that this approach was feasible and accepted by patients because it rapidly reduced the number of persons travelling to the centre. Without this switch, approximately three-quarters of these patients would not be able to avail of proper medical care. Another feasibility study [83] addressed the feasibility, clinical profile and addressability of using teleconsultation in a tertiary care government medical university during the COVID-19 lockdown. Their results were feasible in a government medical university which provides diagnosis and examination services. Authors in Ref. [84] leveraged the use of technology during the COVID-19 pandemic to support patient teleconsultation. Authors discussed the feasibility of using telehealth to provide outpatient teleconsultation services during the lockdown despite the difficulties. Their results presented how such services can be operated on a massive scale, the ease of operation and the high satisfaction among users and service providers. Authors also concluded that despite the limitations related to the quality and quantity of information sought, telehealth is a viable method for patient–physician communication during the lockdown. Authors in Ref. [85] discussed the importance of teleconsultation services in conducting effective triage and diagnosis and in providing disposition for non-COVID-19 urgent hospital visits, namely, cases requiring emergency treatment. They developed a process which utilises inpatient telehealth video visits and electronic consultations (eConsults) to assess patients with non-procedural needs who were directed to the emergency department or admitted to the hospital. They aimed to describe remote consultation types and the requirements of medical billing and documentation. They also aimed to demonstrate the rapid implementation process. They stated that other consulting specialists can implement similar programs to minimise unwarranted physical exposure without compromising health care. Authors in Ref. [86] assessed the usefulness of emergency tele-ophthalmology with a simple smartphone application or web browser and a webcam as a means of teleconsultation in managing emergency cases in the context of sudden restrained access during the COVID-19 pandemic. They argued that their approach allowed social distancing and prevented the increase of infection rate. Authors in Ref. [87] discussed the deployment of rapid telehealth, particularly real-time video conferencing, for chiropractic services in response to the COVID-19 pandemic. Authors argued that rapidly developing real-time video conferencing tools and other telehealth service forms is important. Thus, they provided information to health care service providers regarding telehealth system set-up to make this advantageous approach available to patients in their communities during the pandemic. Authors in Ref. [88] investigated access to remote consultation and the attitude towards telehealth by using an Internet-based survey. The survey indicated that the patients reacted positively to the continuation of health services during the COVID-19 pandemic by using new strategies. Hence, the application of telehealth is promising. Authors in Ref. [89] evaluated the role of teleconsultation in the follow-up care of children with respiratory illnesses and assessed the satisfaction of caregivers with teleconsultation. The study showed that majority of children with respiratory illnesses can be managed via telemedicine. In addition, most of the caregivers were satisfied using teleconsultation and want to continue using telemedicine even after the COVID-19 pandemic. Authors in Ref. [90] discussed their experience in using teleconsultation for patients with idiopathic inflammatory myopathy. Despite the challenges, the study showed that teleconsultation can be successfully used in patients with IIM.
3.3.2.6. Tele-rehabilitation
Five articles on tele-rehabilitation were found. Authors in Ref. [91] examined the effects of a smartphone-based wearable tele-rehabilitation system for dynamic weight-shifting balance exercises by Parkinson's disease. The study showed a steady-state performance achievement with the exercises. Furthermore, the ability of the participants was improved by the system's repetitive balance exercises to acquire confidence and motor skills in postural control, which could improve daily task performance. Authors in Ref. [92] assessed patients and providers' satisfaction of cancer tele-rehabilitation visits during the COVID-19 pandemic. A cancer rehabilitation program was developed at an academic medical centre. The patients and providers showed a high satisfaction in using video tele-rehabilitation despite the limitations of conducting a thorough physical exam. Authors in Ref. [93] evaluated the satisfaction of patients and physicians with teleconsultation in urology during the COVID-19 pandemic by using the validated telemedicine satisfaction questionnaire. Patients and physicians showed a high level of satisfaction with teleconsultation. Authors in Ref. [94] assessed a home-based pulmonary rehabilitation program using telemedicine in lung transplant candidates with cystic fibrosis. The tele-rehabilitation program was based on a combination of self-selected activity and a fitness application. The study reported that patients with cystic fibrosis adhered the tele-rehabilitation program with no adverse events. The home-based pulmonary rehabilitation program produced the same results as the hospital-based pulmonary program. Authors in Ref. [95] evaluated the utilization of tele-consultation in plastic surgery clinics during the COVID-19 pandemic. A survey was distributed to plastic surgeons to evaluate the effectiveness, modality, safety and utility of virtual consultations. The findings indicated that teleconsultation was time and financially efficient, and allowed patients to continue access to care.
3.3.2.7. Delivery of care
Many studies analysed the use of telehealth to perform medical procedures which do not require immediate intervention. Seven studies discussed different forms of care provision. Authors in Ref. [96] discussed a tool for the remote evaluation of patients during the pandemic. They evaluated the multidisciplinary assessment of patients who used telehealth during the COVID-19 pandemic. Their results emphasised the importance of using such tools in telehealth applications, such as in the triage of patients to increase practice outreach and efficiency. The authors also discussed the role of telehealth in assisting patients when non-emergency medical services were interrupted. Authors in Ref. [97] discussed the delivery of care from a rehabilitation perspective. Telehealth is a possible solution to the disruption in outpatient services caused by the COVID-19 pandemic. Accordingly, authors reported field experiences and first-hand information. The experiences reported were very different in terms of population interventions, professionals, service payment and technologies used. Their findings suggested that regardless of telehealth integration, face-to-face rehabilitation is still the best approach for medical care considering the technology barriers. Furthermore, patients agreed that telehealth can be integrated if required. Authors in Ref. [98] discussed and outlined the ability of facilitating telemedicine in the home care of patients undergoing peritoneal dialysis to avoid COVID-19 transmission. A protocol was developed for care process to follow-up with patients, training new patients, medical management or treatment continuity. As reported, patients were able to continue their treatment in a structured and safe manner through constant communication with their dialysis centres. Authors in Ref. [99] conducted a survey on the care delivery satisfaction of medical providers and patients in utilizing telehealth services. Survey results showed that the respondents expressed a positive experience with receiving care using telehealth services and preferred delivering their care using telehealth instead of face-to-face even post the pandemic. Authors in Ref. [100] investigated the impacts of telemedicine services on the management and delivery of care to patients with transient ischaemic attack (TIA). The study indicated that the virtual TIA clinic was able to deliver ongoing care to their patients despite the challenges, the hospital admission for nonvascular causes were reduced and mimic diagnoses were rapidly reduced during the pandemic. Authors in Ref. [101] evaluated the acceptability, feasibility and integration of telemedicine with in-home monitoring platforms in the interstage period of infants. A program based on tele-activities was developed using home monitoring platforms, video visits and video/photo sharing. The developed framework enhanced the care of infants during the interstage period with overall high acceptability. Authors in Ref. [102] examined the telehealth service provided for veterans with obstructive sleep apnoea. The sleep telemedicine program Telesleep was developed to improve access to care. The study findings reported a high level of satisfaction among patients across different domains. Travel burden decreased, and their convenience level increased due to the high and easy access to care. Table 7 discusses the most important highlights of the studies on non-urgent medical procedures along with the references.
Table 7.
Medical procedure main highlights.
| References | Main Highlights |
|---|---|
| Xu, Huang, Qiu, Liu, Deng, Jiao, Tan, Ai, Xiao and Belliato, 2020 [58] | Using telehealth as a tool to continuously monitor home-quarantined patients with progressive COVID-19 |
| Krenitsky, Spiegelman, Sutton, Syeda and Moroz, 2020 [59] | Designing and implementing virtual tele-monitoring for patients suspected to have COVID-19 |
| Martínez-García, Bal-Alvarado, Guerra, Ares-Rico, Suárez-Gil, Rodríguez-Álvarez, Pérez-López, Casariego-Vales, Rial and Rey, 2020 [60] | Assessing whether or not telehealth with tele-monitoring is clinically useful and safe as a tool for monitoring patients with COVID-19 |
| Wali, Margarido, Shah, Ware, McDonald, O'Sullivan, Posada, Ross and Seto, 2021 [61] | Examining the role of tele-monitoring during the COVID-19 pandemic for patients with heart failure |
| Giudice, Bennardo, Antonelli, Barone and Fortunato, 2020 [63] | Management of emergency dental procedures during the COVID-19 pandemic |
| O'Hara, Johnston and Browne, 2020 [64] | Role of telehealth in weight management during the COVID-19 pandemic |
| Bluman, Fury, Ready, Hornick and Weaver, 2020 [65] | Diagnosis and management of a patient with knee pain during the COVID-19 pandemic |
| Ghai, Malhotra and Bajwa, 2020 [66] | Telehealth as an essential health care service for the management of chronic pain during the COVID-19 pandemic |
| Salzano, D'Assante, Stagnaro, Valente, Crisci, Giardino, Arcopinto, Bossone, Marra and Cittadini, 2020 [67] | Telehealth service for heart failure management during the COVID-19 outbreak |
| Jayawardena, Mankarious, Keamy Jr and Cohen, 2020 [68] | Discussing dependence on telehealth for managing outpatient pathology to comply with social distancing orders |
| Davarpanah, Mahdavi, Sabri, Langroudi, Kahkouee, Haseli, Kazemi, Mehrian, Mahdavi and Falahati, 2020 [69] | Novel screening strategy to provide services in regions with limited access to expertise during the COVID-19 pandemic |
| Chou, Hsieh, Wolfshohl, Green and Bhakta, 2020 [70] | Screening strategy to limit COVID-19 exposure in the emergency department |
| Ratwani, Brennan, Sheahan, Fong, Adams, Gordon, Calabrese, Hwang, Smith and Booker, 2020 [71] | Remotely screening patients and analysing their requests during the COVID-19 pandemic |
| Giudice, Barone, Muraca, Averta, Diodati, Antonelli and Fortunato, 2020 [72] | Describing the advantages of telehealth with respect to dental practices during the COVID-19 pandemic |
| Ghai, 2020 [73] | Providing an overview of teledentistry applications during the COVID-19 pandemic |
| Li, Chan, Huang and Cheng, 2020 [75] | Evaluating the effectiveness of video consultation services during the COVID-19 pandemic and satisfaction of patients |
| Panda, Dawman, Panda and Sharawat, 2020 [76] | Exploring the effectiveness of advanced telecommunications for teleconsultation services in a resource-limited environment during the COVID-19 pandemic |
| Borchert, Baumgarten, Dalela, Jamil, Budzyn, Kovacevic, Yaguchi, Palma-Zamora, Perkins and Bazzi, 2020 [77] | Evaluating a risk-stratified prioritisation pathway for teleconsultation services during the pandemic |
| Das, Rani and Vaddavalli, 2020 [78] | Describing experience in the use of tele-consultation services for a hospital network during the COVID-19 pandemic |
| Crane, Ganesh, Post and Jacobson, 2020 [79] | Utilizing tele-consultation services for tracking and following-up confirmed or suspected COVID-19 infections |
| Iyengar, Jain and Vaishya, 2020 [80] | Discussing remote consultations pitfalls during COVID-19 and how they should be identified and dealt with |
| Deshmukh, Badakere, Sheth, Bhate, Kulkarni and Kekunnaya, 2020 [81] | Analysing and reporting teleconsultation data to guide future teleconsultation practices to assist patients |
| Shenoy, Ahmed, Paul, Skaria, Joby and Alias, 2020 [82] | Investigating the feasibility and acceptance of patients in switching to teleconsultation during the COVID-19 pandemic |
| Pandey, Srivastava, Kumar, Katiyar and Agrawal, 2020 [83] | Understanding the feasibility, clinical profile and addressability of patients using teleconsultation during lockdown |
| Rastogi, Singh and Pandey, 2020 [84] | Using the technology in times of COVID-19 to assist in the teleconsultation of patients during lockdown |
| Gadzinski, Andino, Odisho, Watts, Gore and Ellimoottil, 2020 [85] | Discussing teleconsultation services to rapidly triage, diagnose and provide disposition for non-COVID-19-related urgent and emergency hospital visits |
| Bourdon, Jaillant, Ballino, El Kaim, Debillon, Bodin and N'Kosi, 2020 [86] | Assessing the utility of emergency tele-ophthalmology for the management of emergency cases in a population to which access has been suddenly restrained |
| Green, Pence, Kwan and Rokicki-Parashar, 2020 [87] | Discussing telehealth rapid deployment, especially real-time video conferencing during the COVID-19 pandemic |
| Santonicola, Zingone, Camera, Siniscalchi and Ciacci, 2020 [88] | Investigating the access to remote consultation and the attitude towards the use of telehealth via an Internet-based survey for COVID-19 patients |
| Kumari, Jat and Kabra, 2021 [89] | Evaluating the role of teleconsultation in follow-up care of children with respiratory illnesses and assessing the satisfaction of caregivers with teleconsultation |
| Naveen, Sundaram, Agarwal and Gupta, 2021 [90] | Discussing the experience of using teleconsultation for patients with idiopathic inflammatory myopathy |
| An, Kim, Lai and Lee, 2020 [91] | Examining the effects of a smartphone-based wearable tele-rehabilitation system for dynamic weight-shifting balance exercises by Parkinson's disease |
| Chang, Jay, Kalpakjian, Andrews and Smith, 2021 [92] | Assessing patients and providers' satisfaction of cancer tele-rehabilitation visits during the COVID-19 pandemic |
| Pinar, Anract, Perrot, Tabourin, Chartier-Kastler, Parra, Vaessen, de La Taille and Roupret, 2020 [93] | Evaluating the satisfaction of patients and physicians with teleconsultation in urology during the COVID-19 pandemic by using the validated telemedicine satisfaction questionnaire |
| Layton, Irwin, Mihalik, Fleisch, Keating, Dimango, Shah and Arcasoy, 2021 [94] | Evaluating a home-based pulmonary rehabilitation program using telemedicine approach in lung transplant candidates with cystic fibrosis |
| Sinha, Malik, Nugent, Drake and Cavale, 2021 [95] | Evaluating the utilization of tele-consultation in plastic surgery clinics during the COVID-19 pandemic |
| Capozzo, Zoccolella, Frisullo, Barone, Dell’Abate, Barulli, Musio, Accogli and Logroscino, 2020 [96] | Discussing a care delivery tool for the remote evaluation of patients during the pandemic |
| Negrini, Kiekens, Bernetti, Capecci, Ceravolo, Lavezzi, Zampolini and Boldrini, 2020 [97] | Discussing the delivery of care from a rehabilitation perspective for outpatient damage caused by COVID-19 |
| Polanco, Aquey, Collado, Campos, Guzman, Cuevas‐Budhart, Divino‐Filho and Ramos‐Sanchez, 2021 [98] | Discussing the ability of facilitating telemedicine in the home care of patients undergoing peritoneal dialysis to avoid COVID-19 transmission |
| Volcy, Smith, Mills, Peterson, Kene-Ewulu, McNair, Kelsey and Mbaezue, 2021 [99] | Examining medical providers and patient care delivery satisfaction by utilizing telehealth services |
| D'Anna, Ellis, Bentley, Brown, Halse, Jamil, Jenkins, Malik, Kalladka, Kwan, Venter and Banerjee, 2021 [100] | Investigating the impacts of telemedicine services on the management and care delivery of patients with transient ischaemic attack |
| Foster, Steltzer, Snyder, Alden, Helner, Schinasi, Bohling and Allen, 2021 [101] | Evaluating the acceptability, feasibility and integration of telemedicine with in-home monitoring platforms in the interstage period of infants |
| Nicosia, Kaul, Totten, Silvestrini, Williams, Whooley and Sarmiento, 2021 [102] | Examining a telehealth service for veterans with obstructive sleep apnoea |
4. Discussion
The data extraction and search protocol yielded an extracted literature information pattern. This section aimed to discuss and highlight three major components: (1) challenges and problems observed through previous and existing research and academic studies; (2) motivations related to the benefits and significance of the topic and ideas explained by researchers; and (3) recommendations where authors share their future ideas and aspiration of the future studies.
4.1. Challenges
Different health care challenges emerged during the COVID-19 pandemic. Researchers have provided suggestions for dealing with such challenges, and telehealth technology was adopted or implemented to overcome these obstacles. The major challenges were found in the literature in relation to health care access, health care service, health care system or health care resources. Other major challenges were related to the risk of the novel coronavirus spread and infection to health care professionals or non-infected patients. Telehealth technology is another reported challenge, and it is related to telehealth adoption, ICT infrastructure, telehealth quality, telehealth functionality or telehealth understanding. The main categories of health care challenges in the telehealth domain during the COVID-19 pandemic are shown in Fig. 3 .
Fig. 3.
Telehealth challenges.
4.1.1. Health care challenges
Considering the continuous spread of the novel coronavirus infection in many countries, different governments have applied social distancing and lockdown rules to control disease spread. However, these rules have affected the in-person health care service for many non-infected patients who wish to receive proper medical care [37,46,53]. Given the disruption of medical care delivery, many surgical procedures were postponed [37,42], and many in-clinic patient care services struggled to maintain contact with their patients [87]. Clinical appointments were put on hold, and most routine outpatient visits were cancelled [11,27,61,83,84]. The lack of access to health care facilities during lockdown and social distancing became a large obstacle. Furthermore, the delivery of different medical care services was disrupted [48,84] for patients with HIV [12], neurologic issues [18,55], obstructive sleep apnoea [102] and urological cancer [93]; vulnerable children who are obese [31]; and patients requiring chronic pain treatments [66], mental health care [15,16], and cancer care and treatment [[19], [20], [21],27]. In addition, continuing the services via telehealth was challenging because of the requirement of precise schedule coordination [37]. A shortage of health care resources (i.e. hospital beds, personal protective equipment and medical staff) occurred because of the massive number of patients with COVID-19, the absence of a proper cure [22,27,59,69] and the shortage of COVID-19 laboratory testing kits [69]. Lack of health care professionals was another challenge during the pandemic, e.g. the lack of doctors [42,69]. Health professionals were expected to work longer hours during the pandemic, thereby negatively affecting their health and the provision of health care services [69]. With the improvement of technology in general, the demand for health care systems to meet the evolving requirements increased [23].
4.1.2. Risk of infection
Lack of protection and risk of infection in health care professionals or non-COVID-19 patients were listed as the major challenges in the literature. Health care workers, especially those which work in the frontline, were at high risk of COVID-19 infection because of the long and direct exposure to many potentially infected patients [58,70]. Moreover, in-person screening or evaluation of non-coronavirus patients may increase health care staff exposure to COVID-19 and put patients at risk [70]. Some patients with specific or chronic diseases, such as diabetes [9,11] and cancer [20,21,24,25], are at a higher risk of COVID-19 infection. Mental health patients are at a higher risk of infection than those who do not have mental health disorders [14]. Some procedures in health care practice, such as dental practice, increase the risk of COVID-19 spread [63,72,73]. In addition, the shortage of personal protective equipment was a major challenge which needed to be addressed to stop the spread of the virus [70,85,86]. The long distance between patients and medical centres during the lockdown was another barrier to the proper delivery of health care services. Infection risk of patients using public transportation to reach medical centres increases [24,29]. Overall, safely delivering health care to people who need it without exposing them to COVID-19 was challenging [14]. Patient management was difficult for many cases. Patients who need on-going management are highly affected because of the risk of exposure to the coronavirus during their visits; examples of these cases are patients with diabetes who need glucose management [10], people who require obesity management [64] and patients with tympanic membrane [68]. Managing patients with mild symptoms of COVID-19 was challenging because many of them were sent home to recover; when the disease progressed, some of the mild cases became critical cases, and the delay in treatment possibly led to death [58].
4.1.3. Technology challenges
The challenges related to telehealth vary and are viewed from different perspectives, including acceptance, adoption, functionality, understanding, quality and legislation. As stated in the literature, some patients, especially older patients, did not feel comfortable using telehealth because of the lack of familiarity with technology [97]. The use of telehealth by patients with low technical skills (e.g. uneducated and elderly patients) was challenging [9]. The lack of medico-legal considerations to support telehealth was another challenge in the implementation and adoption of telehealth in different countries [66]. Technological and technical issues were major challenges in implementing and adopting telehealth [30,37,97]. Furthermore, technical issues such as lack of Internet access [17] and slow Internet connection were considered as barriers in using telehealth [49,53,97]. The inability or difficulty to access telehealth technology was another barrier [53,67]. Technological issues, such as lack of additional technological equipment [34,50] and large-scale telehealth solutions, are challenging. Telehealth functionality was challenging [51]. Studies on the functional performance of telehealth as an approach for patients screening are few [71]. Significant gaps in the effectiveness of using telehealth were addressed [51]. The lack of functional assessment of accurate monitoring systems has been considered a challenge [97]. Moreover, some examinations (e.g. blood taking and physical examination) can be performed only by face-to-face interaction and not via telehealth [25,48,50,66,75,76].
4.1.4. Clear guidelines
The lack or unavailability of clear guidelines on appropriate remote health care for different patients was a major challenge [52,66]. For instance, no international guidelines or best practices exist for the management of patients with cancer in any emergency situation during the pandemic [26,27]. In addition, information is lacking on clear guidelines or protocols for different remote practices, such as radiation therapy [20], gynaecologic care [33], post-acute and long-term care [44] and follow-up care of children with respiratory illnesses [89].
4.1.5. Data privacy and security
Data privacy and security issues were major concerns in using telehealth. Different issues were considered major concerns for telehealth, such as data protection and maintaining patient privacy [53]. With the rapid increase in the number of patients’ digital health records daily, the risk of exposure to fraud or data breach has increased. Furthermore, increasing concerns regarding privacy and security issues result from the vulnerability of some telehealth applications. The safety issues of telehealth apps and the use of telecommunication directly affect the data privacy of patients [97].
4.1.6. Other challenges
Other barriers in the use or implementation of telehealth exist. For instance, challenges related to payment exist, whether in relation to the patients or the health services [97]. Some examinations and screenings require the installation of specific equipment (e.g. imaging equipment) in patients' home before telehealth can be performed. However, limited vendors and companies provide such services [65]. Furthermore, loading and visualising patient images during telehealth visits can be challenging [51]. Some patients lack the necessary devices in their homes to access telehealth [97]. Moreover, guiding patients in setting up their device appropriately to allow effective examination can be challenging [10]. The unavailability or the lack of studies on telehealth during the pandemic was evident in the assessment of the effectiveness of laryngology tele-evaluations, the use of telehealth in delivering care for patients with front temporal lobar dementia [96] and in the examination of otolaryngology patients’ satisfaction [54]. Furthermore, limited information is available on the safety of telehealth implementation [60].
4.2. Motivations
Different aspects of motivations were found in the literature, whether related to the telehealth itself, health care improvement or safety improvement. This section highlights the different motivations found during the pandemic. Fig. 4 highlights the main categories of telehealth motivations.
Fig. 4.
Telehealth motivations.
4.2.1. Safety improvement
As mentioned in the literature, improving the safety of individuals, patients or health care professionals was the main motivation in most of the studies; the use of telehealth reduces face-to-face interactions [22,37,46,65,68]. Different studies were motivated to show the minimisation of health care settings during the pandemic [69]. Minimising the visits of outpatients helped mitigate exposure and transmission of the coronavirus [26]. New assistance models which limit the direct contact between patients and doctors need to be developed [72]. Telehealth can assist in containing and controlling this international pandemic. Telehealth's usefulness and ability to provide safe, high-quality and rapid care have become evident worldwide [68,77]. Telehealth minimises the exposure of non-COVID-19 patients and health care professionals to COVID-19 by screening and delivering care to patients without face-to-face contact [9,39,49,50,71,88,96]. The implementation of telehealth can help health care professionals avoid direct interaction with patients suspected of harbouring COVID-19 [60]. Screening potential patients of COVID-19 via telehealth is an effective way to protect patients, health care providers and the community from additional exposure. Telehealth provides an opportunity to protect the communities and improve the delivery of health service during the COVID-19 pandemic and beyond [66]. Vulnerable patients are at a higher risk of COVID-19 infection, and using telehealth is an effective way to minimise their exposure [53]. Providing safe and effective health care services to prevent exposure to COVID-19 is essential for different medical practices, such as dental practice [63], glucose control and management, prenatal care [32], HIV prevention and care [13], cancer care [25] and in the emergency department [70,85].
4.2.2. Save time, cost and resources
Telehealth has become an increasingly valuable resource for patient consultations during the COVID-19 pandemic. In the literature, different researchers were motivated to reduce the overload on hospitals by conserving their time and resources (e.g. personal protective equipment and beds) by concentrating on patients with COVID-19. Eliminating the unnecessary in-person visits would be valuable to preserve medical centre resources [42,53,54]. Furthermore, the waiting time in hospital rooms and clinics can mostly be eliminated using telehealth [51]. In light of the limited availability of COVID-19 testing kits and stringent criteria for testing, the number of patients arriving on-site for care decreased when communication was conducted via telehealth [71]. The shortage of doctors was alleviated with telehealth. With the adoption of telehealth, the efficiency of using medical resources and managing patients increased. Aside from the improvement of clinical efficiency and patient satisfaction, the schedule of surgeons is optimised in telehealth [49]. Utilizing telehealth services allows patients and health providers to save time. Telehealth services lessen the necessity of using personal protection equipment, thereby reducing resource consumption [66]. The aim to minimise the health care costs of patients, especially those who live far from their medical centres, was a motivating factor for the implementation of telehealth [49,54,72]. Supporting severe medicine and disaster response using low-cost mobile health technologies became possible with telehealth.
4.2.3. Improving health access care
The aim to improve health care services and access during the COVID-19 pandemic by using telehealth is a major motivation for many researchers [35,66,75,95,98,102]. Telehealth has the potential to overcome the inability of patients to attend medical appointments in person. Remote monitoring systems have helped health care providers monitor numerous patients who are in different places, whether in different sections inside the hospital [88] or in their homes [51]. During the pandemic, telehealth effectively provided access to care for patients who would remain disconnected without it. Telehealth has been used by different medical centres to maintain and improve access to care, especially for patients who live far from the medical centre; some of these health care services include ophthalmology care [78], rhinology care, dental care [73], HIV treatment [12], diabetes care [9,11], physician care [51], psychiatric care, COVID-19 patient care [79], epilepsy patient care [17,76], urology care [93] and mental health care [16,30]. Furthermore, telehealth can provide patients rapid access to specialists who might not be available in person. Telehealth improves patient management during the pandemic. For instance, telehealth facilitates the continuous glucose monitoring of patients with diabetes [10]. Furthermore, with the help of telehealth, patients who need surgeries were identified in a timely manner. Telehealth provided opportunities to develop physical activity programs for individuals with increased risk of decline. Telehealth could become the preferred communication channel between patients and care givers. Different studies have implied that the use of telehealth can be continued to improve access to health care even after the current pandemic [99]. Telehealth can improve access to care by overcoming geographic and socioeconomic distances [9,24,72]. The adoption of telehealth can enhance patient and health care provider satisfaction [49]. The adoption of telehealth has become a critical way to deliver health care and clinical care. Telehealth can be used to triage COVID-19 patients before hospital admission. It also has the potential to maintain and improve the health care quality of patients [21,75] and enhance clinical efficiency [49]. Health care delivery was effectively transformed when patients and health care providers adopted telehealth. A critical step in outbreak containment was made by remotely monitoring recently discharged patients via telehealth. Delivering comprehensive health care by different health specialists was made possible by the implementation of telehealth during the pandemic. Several health care systems have invested on building their telehealth capacity to become ubiquitous. Telehealth is an emerging technology which has become a sustainable and efficient solution for essential health care service delivery [66]. Telemedicine could improve access to care of underserved populations (e.g. minority, low-income and non-English-speaking patients) by eliminating traditional barriers to care, such as distance from speciality clinics and transportation needs [43].
4.2.4. Providing guidance
Providing practical guidelines for implementing and using telehealth effectively has motivated different researchers during the COVID-19 pandemic [35,66,80]. Different clinicians were motivated to share their best practices in using telehealth to provide guidelines to others who will assist them in continuing to provide care services during the pandemic, such as gynaecology care [33], otolaryngology care [37], ophthalmology care [81], prostate cancer care [20], radiation oncology care [41], children with respiratory illnesses care [89] and physician care [27]. Furthermore, providing guidelines to perform neurological exams remotely was the main motivation of [47]. Another motivation perspective was the provision of guidance to medical students, thereby ensuring that telehealth can be used during and beyond the current pandemic [20].
4.2.5. Evaluation
With the increased implementation of telehealth, many researchers were motivated to evaluate its effectiveness [36,75]. Furthermore, the efficacy of telemonitoring in detecting potentially severe cases was evaluated [60]. A previous study evaluated the effectiveness of telehealth visits on the post-operative care of neurosurgical patients [48]. Another study evaluated and compared the engagement of patients during tobacco treatment via telehealth versus via in-person attendance [23]. A study evaluated the feasibility and patients’ acceptance of the rapid switch to teleconsultation [82]. The principal judgment criteria of proper diagnosis and treatment of eye emergencies using telehealth were evaluated [86]. The changes experienced in the outpatient practice of epilepsy clinics during the COVID-19 pandemic were analysed and evaluated [18].
4.3. Recommendations
In the literature, numerous recommendations were provided from different perspectives. These recommendations were related to prevention or reduction of COVID-19 exposure, further studies, ICT improvement, the expansion of telehealth implementation and the improvement of patient care. Fig. 5 presents the main categories of telehealth recommendations.
Fig. 5.
Telehealth recommendations.
4.3.1. Exposure prevention
In the literature, different recommendations were made to prevent exposure in the current pandemic. For instance, helping patients use telehealth will reduce the number of visits and lessen the risk of exposure [26]. To minimise hospital visits and exposure to many people, surgical consent was obtained prior to surgery using telehealth. Telehealth allows dentists to answer the questions of patients and conduct follow-up visits and remote consultations, thereby minimising the risk of visiting dental offices [63].
4.3.2. Further studies
In the literature, different recommendations were made towards the performance of further studies from different perspectives. For instance, further studies were needed to evaluate the outcomes of patients and health care providers in terms of their use of telehealth. Evaluating the satisfaction of patients and health care providers in using telehealth was also recommended [59]. The efficacy of telehealth in the management of patients with eating disorders and addiction needed further research. Additional studies are needed to determine the impact of COVID-19 on the treatment of patients with mental disorders [14]. Further research is needed to understand the virology and epidemiology of COVID-19 in the cancer community [26]. Further studies were needed to improve telehealth techniques to optimise patient care [37]. Additional research was recommended to determine a multidisciplinary approach combination to deal with SARS-CoV-2 via telehealth. Additional research was recommended to adopt new and useful frameworks for the urology department [77]. The usefulness of telehealth in future pandemics should also be evaluated [60]. Further studies are needed to improve the efficacy and safety of otoscopic examination home devices and to develop optimisation strategies for device utilization [68]. Additional studies explored some of the current challenges of telehealth, such as those related to technical support and data security [25]. Further studies were recommended to evaluate the amount and types of outreach efforts for health providers to achieve the best teletherapy engagement and conversion [15].
4.3.3. Telehealth expansion
In the literature, numerous studies recommended the implementation and expansion of telehealth because of its essential role in the continuation of patient care during the current pandemic and beyond [13,14,39,41]. Telehealth expansion was recommended to improve access to care of underserved populations [43]. Telehealth adoption was recommended to overcome patient flow and to reduce the workload of physicians. A study recommended the large-scale spread and implementation of telehealth with permanent changes in telehealth polices to achieve a meaningful public health impact during the current pandemic and beyond [30]. Recommendations were made for governments to surmount ethical and social data transparency challenges to promote the wide adoption of telehealth by individuals [45].
4.3.4. Quality improvement
The standardisation and validation of neurologic examination scales in telehealth care, such as myelopathy scoring systems, were recommended to ensure quality care. Frequent multidisciplinary communications using telehealth were recommended during the COVID-19 pandemic to ensure that the highest quality of health care can be provided [21]. In laryngology clinics, the telehealth model was recommended to be optimised to provide high-quality care [37].
4.3.5. Technology improvement
Several recommendations were made to improve technology from different aspects, i.e. in relation to ICT improvement or telehealth platforms, tools or methods, including the way by which the current telehealth challenges are addressed. The current telehealth challenges which need to be addressed include privacy and security concerns [31]. Secure photo transfer methods, protocols, platforms or tools must be developed to train patients in the appropriate use of telehealth and to enhance the treatment ability of patients [68]. Another study recommended that patients and providers need to provide systematic responses about teletherapy engagement issues to elucidate such issues [15]. The integration of disease tracking measures, such as contact tracing and self-reporting applications, with telehealth monitoring was recommended to increase patient care while meeting social distancing requirements [59]. Furthermore, increasing the integration of Bluetooth technology could open the opportunity to link external tools with smartphone and telemedicine platforms to improve access to care remotely [55].
4.3.6. Policy improvement
Many health practices were recommended to relax their regulations in the post-COVID-19 era to allow the use telehealth on a routine basis. Large-scale spread and implementation efforts, along with permanent changes in telehealth policies, were recommended to achieve a meaningful health impact during the current COVID-19 pandemic and beyond [30]. The policies of Medicare and Medicaid services for telehealth were recommended to be adjusted for the provision of long-term care by using the system [68]. Risk-based approach has been recommended for policymakers to develop standardised evidence-based assessment processes and legislations for digital health solutions [21].
4.3.7. Other recommendations
A study recommended the promotion of awareness of public health policies [59]. Technical trainings for patients were recommended because many of them lack computer skills. Self-measurement training for obtaining blood pressure and oxygen saturation levels was also recommended for patients. Furthermore, training health care providers in telehealth was recommended for a disease-specific clinic [59]. A study recommended the evaluation of telehealth effects on health care costs. A rapid deployment of telehealth was recommended to reduce the time and cost of travel for patients, thereby helping patients who live in rural areas and who have great health care needs [77].
5. Study implications
Basing from the above, authors of this study have observed different changes in the world towards telehealth and telemedicine and, hence, extracted and drew possible directions of telehealth during and post the COVID-19 era. The utilization of telehealth has started to be normalised with different health clinics and diseases, especially with chronic diseases. Hence, new regulations and rulings should be formulated by governments, health organisations and hospitals to organise the communication between health professionals and patients. Such regulations and rulings include improving patient privacy and security, ensuring service quality, increasing the awareness of telehealth by providing the proper instructions to patients and health professionals and providing proper training on telehealth systems.
Clinics and hospitals in rural areas or in any other country could benefit from telehealth by collaborating with health professionals to facilitate improved health treatment to their patients. As shown in Fig. 6 , authors of the study highlighted a potential framework of telemedicine in the post COVID-19 era. A potential of new opportunities for virtual specialised clinics is opened. These virtual clinics are collaborating and cooperating with specialised centres and hospitals to follow-up with their patients using telemedicine; consult potential patients in local areas, rural areas or in other countries; and transfer them to a suitable clinic/hospital if face-to-face visit is needed. This could improve the business model of specialised clinics and may ease for patients’ access, especially patients with low-income, to high-quality care from all over the world. Furthermore, the business model could be improved by developing external telemedicine-related tools which can be connected to mobile phones or laptops via Bluetooth. These tools could be couriered to patients who are living in another place. Translators or staff who are bilinguals or trilingual should be hired to overcome the language barriers. The following considerations should be taken for this potential framework to succeed:
-
•
Data privacy and security: Improving data privacy and security is important for patients and clinics. Privacy and security are the main factors affecting the decisions of users to adopt and utilise any technology. Authors believe that maintaining high privacy and security systems will increase people's trust and, hence, increase their acceptance to use telehealth services.
-
•
Data integration: Implementing telehealth systems which integrate patient data between virtual specialised clinics and hospitals is essential to understand cases and maintain a high quality of service provided to them.
-
•
Infrastructure: Upgrading the infrastructure of telemedicine in hospitals and clinics is essential to enhance their capability to utilise telemedicine properly.
-
•
Provide training: Training patients and telemedicine providers by providing clear instructions via telephone or videos with multiple languages is important to make them familiar with telemedicine.
Fig. 6.
Potential framework of telehealth services.
6. Conclusion
The recent and rapid incorporation of telehealth applications and efforts during the COVID-19 pandemic, as well as the uncertainty regarding the pandemic, is expected to expand the capability of telehealth. The integration of telehealth to meet COVID-19 needs and the validation of telehealth technologies are the next steps to improve the utility and complete implementation of the system. The COVID-19 pandemic has hastened the advent and utilization of telehealth, leading to a sudden shift towards the use of telehealth technology for the clinical assessment of the virus as a necessary measure. Basing from our experience, we describe the relationship between COVID-19 and telehealth to optimise the quality and efficiency of the utilised technologies, particularly in relation to their role in the control, implementation, strategies, guidelines and medical procedures of common telehealth approaches during the COVID-19 pandemic. We comprehensively analysed some studies to highlight the benefits, challenges and recommendations related to telehealth and COVID-19 classification and found some gaps. These gaps include the lack of rules and regulations towards utilizing telehealth (e.g. medico-legal considerations), lack of telehealth data privacy and security, lack of telehealth systems integration (e.g. data integration), lack of telehealth infrastructure (e.g. large telehealth solutions, tele-examinations equipment), and the lack of clear path of utilizing telehealth after COVID-19. Establishing clear rules and regulations by governments and health organisations can contribute towards avoiding misused telehealth and make patients and providers fully aware of their rights. Improving telehealth infrastructure and systems will contribute to facilitate a higher quality of care to a larger scale of patients. Determining a path for utilizing telehealth after the pandemic can motivate and guide researchers, medical and government personnel to make advanced contributions on the telehealth area. The solutions presented must be considered to address the challenges and issues highlighted in this article. To gain deeper insights into the investigated field, this article provides a broad foundation to industrial trends by exploring the impact of this pandemic on telehealth development. Salient relationships exist between the need for telehealth and its application during the pandemic, as reflected in this article. Different software and tools were developed to support diagnosis and treatment using telemedicine. However, this area is still fresh, and new tools need to be developed for different disease treatments and diagnoses. Proper integration of telehealth as an emerging technology to assist patients, health care providers and policymakers can improve existing applications and promote the development of a medical health care practice of the highest standards.
Declaration of competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors are grateful to the Universiti Pendidikan Sultan Idris, Malaysia for funding this study under Grant No. 2020-0310-106-11.
Appendix.
| Reference | Q1 Aim | Q2 Method | Q3 Research Methods | Q4 Settings & Sample | Q5 Measures Definition | Q6 Measures Relevance | Q7 Data Collection | Q8 Data Analysis | Q9 Comparison | Q10 Findings | Q11 Limitations | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [9] | 1 | 1 | 0.5 | 0 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 6.5 |
| [10] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0 | 8.5 |
| [11] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [12] | 1 | 0.5 | 0 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 4 |
| [13] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 5 |
| [14] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [15] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 10 |
| [16] | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.5 | 3.5 |
| [17] | 1 | 1 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 3.5 |
| [18] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [19] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [20] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [21] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [22] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 0 | 7.5 |
| [23] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [24] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0 | 8.5 |
| [25] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [26] | 1 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0.5 | 0.5 | 3.5 |
| [27] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 6.5 |
| [28] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| [29] | 1 | 1 | 0.5 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 0 | 4.5 |
| [30] | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0.5 | 0 | 1 | 0.5 | 4 |
| [31] | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 5 |
| [32] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0 | 8.5 |
| [33] | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 8.5 |
| [34] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 4 |
| [35] | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 7.5 |
| [36] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0.5 | 9.5 |
| [37] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 9 |
| [38] | 1 | 1 | 1 | 0.5 | 0 | 1 | 0.5 | 1 | 0 | 1 | 0 | 7 |
| [39] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0.5 | 1 | 1 | 9.5 |
| [40] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [41] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0.5 | 8.5 |
| [42] | 1 | 1 | 1 | 1 | 0 | 0.5 | 1 | 1 | 0 | 1 | 1 | 8.5 |
| [43] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [44] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0 | 8.5 |
| [45] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| [46] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [47] | 1 | 1 | 0.5 | 0.5 | 0 | 1 | 0.5 | 1 | 1 | 1 | 1 | 8.5 |
| [48] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [49] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0.5 | 9 |
| [50] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [51] | 1 | 1 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 6 |
| [52] | 1 | 1 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 | 0 | 1 | 1 | 5.5 |
| [53] | 0.5 | 1 | 0.5 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 1 | 0.5 | 4.5 |
| [54] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [55] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [56] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [58] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [59] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0.5 | 8.5 |
| [60] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [61] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [63] | 1 | 1 | 1 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 6.5 |
| [64] | 1 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0 | 1 | 0 | 1 | 0 | 5 |
| [65] | 1 | 1 | 0.5 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 0.5 | 7.5 |
| [66] | 1 | 1 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 0 | 4 |
| [67] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [68] | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 7 |
| [69] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 1 | 8.5 |
| [70] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 1 | 8.5 |
| [71] | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [72] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 9 |
| [73] | 1 | 1 | 0.5 | 0 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 0 | 6 |
| [75] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [76] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [77] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 9 |
| [78] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 8 |
| [79] | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 3.5 |
| [80] | 1 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 0 | 5 |
| [81] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0.5 | 8.5 |
| [82] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [83] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [84] | 1 | 1 | 0.5 | 0.5 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| [85] | 1 | 1 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 1 | 0 | 5 |
| [86] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [87] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 9 |
| [88] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 0 | 8.5 |
| [89] | 1 | 1 | 0.5 | 0.5 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| [90] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| [91] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| [92] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [93] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| [94] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| [95] | 1 | 1 | 0.5 | 0.5 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 7 |
| [96] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [97] | 1 | 1 | 0.5 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 0 | 7.5 |
| [98] | 1 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | 9 |
| [99] | 1 | 1 | 1 | 1 | 0 | 0.5 | 1 | 1 | 0 | 1 | 1 | 8.5 |
| [100] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| [101] | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 0 | 1 | 1 | 9.5 |
| [102] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
References
- 1.Satin A.M., Lieberman I.H. The virtual spine examination: telemedicine in the era of COVID-19 and beyond. Global Spine J. 2020;11:966–974. doi: 10.1177/2192568220947744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joshi A.U., Randolph F.T., Chang A.M., Slovis B.H., Rising K.L., Sabonjian M., Sites F.D., Hollander J.E. Impact of emergency department tele‐intake on left without being seen and throughput metrics. Acad. Emerg. Med. 2020;27:139–147. doi: 10.1111/acem.13890. [DOI] [PubMed] [Google Scholar]
- 3.Albahri A.S., Hamid R.A., Albahri O.S., Zaidan A. Detection-based prioritisation: framework of multi-laboratory characteristics for asymptomatic COVID-19 carriers based on integrated Entropy–TOPSIS methods. Artif. Intell. Med. 2021;111 doi: 10.1016/j.artmed.2020.101983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albahri A.S., Alwan J.K., Taha Z.K., Ismail S.F., Hamid R.A., Zaidan A., Albahri O.S., Zaidan B., Alamoodi A., Alsalem M. IoT-based telemedicine for disease prevention and health promotion: state-of-the-Art. J. Netw. Comput. Appl. 2021;173 [Google Scholar]
- 5.Hirko K.A., Kerver J.M., Ford S., Szafranski C., Beckett J., Kitchen C., Wendling A.L. Telehealth in response to the COVID-19 pandemic: implications for rural health disparities. J. Am. Med. Inf. Assoc. 2020;27:1816–1818. doi: 10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alamoodi A., Zaidan B., Zaidan A., Albahri O., Mohammed K., Malik R., Almahdi E., Chyad M., Tareq Z., Albahri A. Sentiment analysis and its applications in fighting COVID-19 and infectious diseases: a systematic review. Expert Syst. Appl. 2020;167 doi: 10.1016/j.eswa.2020.114155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y., Zhang Z., Dai C., Dong Q., Badrigilan S. Accuracy of deep learning for automated detection of pneumonia using chest X-ray images: a systematic review and meta-analysis. Comput. Biol. Med. 2020;123 doi: 10.1016/j.compbiomed.2020.103898. [DOI] [PubMed] [Google Scholar]
- 8.Binbeshr F., Kiah M.M., Por L.Y., Zaidan A.A. A systematic review of PIN-entry methods resistant to shoulder-surfing attacks. Comput. Secur. 2020;101 [Google Scholar]
- 9.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes, Metab. Syndrome: Clin. Res. Rev. 2020;14:273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peters A.L., Garg S.K. The silver lining to COVID-19: avoiding diabetic ketoacidosis admissions with telehealth. Diabetes Technol. Therapeut. 2020;22:449–453. doi: 10.1089/dia.2020.0187. [DOI] [PubMed] [Google Scholar]
- 11.Boscari F., Ferretto S., Uliana A., Avogaro A., Bruttomesso D. Efficacy of telemedicine for persons with type 1 diabetes during Covid19 lockdown. Nutr. Diabetes. 2021;11:5. doi: 10.1038/s41387-020-00147-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mgbako O., Miller E.H., Santoro A.F., Remien R.H., Shalev N., Olender S., Gordon P., Sobieszczyk M.E. COVID-19, telemedicine, and patient empowerment in HIV care and research. AIDS Behav. 2020;24:1990–1993. doi: 10.1007/s10461-020-02926-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rogers B.G., Coats C.S., Adams E., Murphy M., Stewart C., Arnold T., Chan P.A., Nunn A. Development of telemedicine infrastructure at an LGBTQ+ clinic to support HIV prevention and care in response to COVID-19, Providence, RI. AIDS Behav. 2020;24:2743–2747. doi: 10.1007/s10461-020-02895-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roncero C., García-Ullán L., Javier I., Martín C., Andrés P., Ojeda A., González-Parra D., Pérez J., Fombellida C., Álvarez-Navares A. The response of the mental health network of the Salamanca area to the COVID-19 pandemic: the role of the telemedicine. Psychiatr. Res. 2020;291 doi: 10.1016/j.psychres.2020.113252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miu A.S., Vo H.T., Palka J.M., Glowacki C.R., Robinson R.J. Teletherapy with serious mental illness populations during COVID-19: telehealth conversion and engagement. Counsell. Psychol. Q. 2020;34:1–18. [Google Scholar]
- 16.Moring J.C., Dondanville K.A., Fina B.A., Hassija C., Chard K., Monson C., LoSavio S.T., Wells S.Y., Morland L.A., Kaysen D. Cognitive processing therapy for posttraumatic stress disorder via telehealth: practical considerations during the COVID‐19 pandemic. J. Trauma Stress. 2020;33:371–379. doi: 10.1002/jts.22544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuroda N. Decision making on telemedicine for patients with epilepsy during the coronavirus disease 2019 (COVID-19) crisis. Front. Neurol. 2020;11:722. doi: 10.3389/fneur.2020.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Punia V., Nasr G., Zagorski V., Lawrence G., Fesler J., Nair D., Najm I. Evidence of a rapid shift in outpatient practice during the COVID-19 pandemic using telemedicine. Telemed. e Health. 2020;26:1301–1303. doi: 10.1089/tmj.2020.0150. [DOI] [PubMed] [Google Scholar]
- 19.Lonergan P.E., Washington S.L., III, Branagan L., Gleason N., Pruthi R.S., Carroll P.R., Odisho A.Y. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. J. Med. Internet Res. 2020;22 doi: 10.2196/19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zaorsky N.G., James B.Y., McBride S.M., Dess R.T., Jackson W.C., Mahal B.A., Chen R., Choudhury A., Henry A., Syndikus I. Prostate cancer radiotherapy recommendations in response to COVID-19. Adv. Radiat. Oncol. 2020;5:26–32. doi: 10.1016/j.adro.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang J.J., Wong R.J., Sherman E.J., Rybkin A., McBride S.M., Riaz N., Tsai C.J., Yu Y., Chen L., Zakeri K. The 3 Bs of cancer care amid the COVID‐19 pandemic crisis:“Be safe, be smart, be kind”—a multidisciplinary approach increasing the use of radiation and embracing telemedicine for head and neck cancer. Cancer. 2020;126:4092–4104. doi: 10.1002/cncr.33031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee A.K., Cho R.H., Lau E.H., Cheng H.K., Wong E.W., Ku P.K., Chan J.Y., Yeung Z.W. Mitigation of head and neck cancer service disruption during COVID‐19 in Hong Kong through telehealth and multi‐institutional collaboration. Head Neck. 2020;42:1454–1459. doi: 10.1002/hed.26226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotsen C., Dilip D., Carter-Harris L., O'Brien M., Whitlock C.W., de Leon-Sanchez S., Ostroff J.S. Rapid scaling up of telehealth treatment for tobacco-dependent cancer patients during the COVID-19 outbreak in New York city. Telemed. e Health. 2020;27:1–10. doi: 10.1089/tmj.2020.0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smrke A., Younger E., Wilson R., Husson O., Farag S., Merry E., Macklin-Doherty A., Cojocaru E., Arthur A., Benson C. Telemedicine during the COVID-19 pandemic: impact on care for rare cancers. JCO Global Oncol. 2020;6:1046–1051. doi: 10.1200/GO.20.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atreya S., Kumar G., Samal J., Bhattacharya M., Banerjee S., Mallick P., Chakraborty D., Gupta S., Sarkar S. Patients'/Caregivers' perspectives on telemedicine service for advanced cancer patients during the COVID-19 pandemic: an exploratory survey. Indian J. Palliat. Care. 2020;26:S40. doi: 10.4103/IJPC.IJPC_145_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al‐Shamsi H.O., Alhazzani W., Alhuraiji A., Coomes E.A., Chemaly R.F., Almuhanna M., Wolff R.A., Ibrahim N.K., Chua M.L., Hotte S.J. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID‐19) pandemic: an international collaborative group. Oncol. 2020;25:e936. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prasad A., Brewster R., Newman J.G., Rajasekaran K. Optimizing your telemedicine visit during the COVID‐19 pandemic: practice guidelines for patients with head and neck cancer. Head Neck. 2020;42:1317–1321. doi: 10.1002/hed.26197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jonker L.T., Lahr M.M., Oonk M.H., de Bock G.H., van Leeuwen B.L. Post-discharge telemonitoring of physical activity, vital signs, and patient-reported symptoms in older patients undergoing cancer surgery. Ann. Surg Oncol. 2021;28:1–11. doi: 10.1245/s10434-021-09707-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sattar S., Kuperman R. Telehealth in pediatric epilepsy care: a rapid transition during the COVID-19 pandemic. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gurwitch R.H., Salem H., Nelson M.M., Comer J.S. Leveraging parent–child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychol. Trauma: Theory Res. Pract. Pol. 2020;12:S82. doi: 10.1037/tra0000863. [DOI] [PubMed] [Google Scholar]
- 31.Woo Baidal J.A., Chang J., Hulse E., Turetsky R., Parkinson K., Rausch J.C. Zooming toward a telehealth solution for vulnerable children with obesity during coronavirus disease 2019. Obesity. 2020;28:1184–1186. doi: 10.1002/oby.22860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aziz A., Zork N., Aubey J.J., Baptiste C.D., D'alton M.E., Emeruwa U.N., Fuchs K.M., Goffman D., Gyamfi-Bannerman C., Haythe J.H. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020;37:800. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grimes C.L., Balk E.M., Dieter A.A., Singh R., Wieslander C.K., Jeppson P.C., Aschkenazi S.O., Kim J.H., Truong M.D., Gupta A.S. Guidance for gynecologists utilizing telemedicine during COVID‐19 pandemic based on expert consensus and rapid literature reviews. Int. J. Gynecol. Obstet. 2020;150:288–298. [Google Scholar]
- 34.Berg E.A., Picoraro J.A., Miller S.D., Srinath A., Franciosi J.P., Hayes C.E., Farrell P.R., Cole C.R., LeLeiko N.S. COVID-19—a guide to rapid implementation of telehealth services: a playbook for the pediatric gastroenterologist. J. Pediatr. Gastroenterol. Nutr. 2020;70:734. doi: 10.1097/MPG.0000000000002749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saleem S.M., Pasquale L.R., Sidoti P.A., Tsai J.C. Virtual ophthalmology: telemedicine in a Covid-19 era. Am. J. Ophthalmol. 2020;216:237–242. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hron J.D., Parsons C.R., Williams L.A., Harper M.B., Bourgeois F.C. Rapid implementation of an inpatient telehealth program during the COVID-19 pandemic. Appl. Clin. Inf. 2020;11:452–459. doi: 10.1055/s-0040-1713635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strohl M.P., Dwyer C.D., Ma Y., Rosen C.A., Schneider S.L., Young V.N. Implementation of telemedicine in a laryngology practice during the COVID-19 pandemic: lessons learned, experiences shared. J. Voice. 2020;35:42–49. doi: 10.1016/j.jvoice.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cassar M.R., Borg D., Camilleri L., Schembri A., Anastasi E.A., Buhagiar K., Callus C., Grech M. A novel use of telemedicine during the COVID-19 pandemic. Int. J. Infect. Dis. 2021;103:182–187. doi: 10.1016/j.ijid.2020.11.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gentry M.T., Puspitasari A.J., McKean A.J., Williams M.D., Breitinger S., Geske J.R., Clark M.M., Moore K.M., Frye M.A., Hilty D.M. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed. e Health. 2021;28:8. doi: 10.1089/tmj.2020.0575. [DOI] [PubMed] [Google Scholar]
- 40.Smith V.J., Marshall A., Lie M., Bidmead E., Beckwith B., Van Oudgaarden E., Robson S.C. Implementation of a fetal ultrasound telemedicine service: women's views and family costs. BMC Pregnancy Childbirth. 2021;21:1–8. doi: 10.1186/s12884-020-03532-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goenka A., Ma D., Teckie S., Alfano C., Bloom B., Hwang J., Potters L. Implementation of telehealth in radiation oncology: rapid integration during COVID-19 and its future role in our practice. Adv. Radiat. Oncol. 2021;6:8. doi: 10.1016/j.adro.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Checcucci E., De Luca S., Alessio P., Verri P., Granato S., De Cillis S., Amparore D., Sica M., Piramide F., Piana A. Implementing telemedicine for the management of benign urologic conditions: a single centre experience in Italy. World J. Urol. 2021;39:1–7. doi: 10.1007/s00345-020-03536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Franciosi E.B., Tan A.L.J., Kassamali B., Leonard N., Zhou G.H., Krueger S., Rashighi M., LaChance A. The impact of telehealth implementation on underserved populations and No-show rates by medical specialty during the COVID-19 pandemic. Telemed. e Health. 2021;27:874–880. doi: 10.1089/tmj.2020.0525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harris D.A., Archbald-Pannone L., Kaur J., Cattell-Gordon D., Rheuban K.S., Ombres R.L., Albero K., Steele R., Bell T.D., Mutter J.B. Rapid telehealth-centered response to COVID-19 outbreaks in postacute and long-term care facilities. Telemed. e Health. 2020;27:102–106. doi: 10.1089/tmj.2020.0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leite H., Gruber T., Hodgkinson I.R. Flattening the infection curve–understanding the role of telehealth in managing COVID-19. Leader. Health Serv. 2020;33:221–226. [Google Scholar]
- 46.Cerqueira-Silva T., Carreiro R., Nunes V., Passos L., Canedo B.F., Andrade S., Ramos P.I.P., Khouri R., Santos C.B.S., Nascimento J.D.S. Bridging learning in medicine and citizenship during the COVID-19 pandemic: a telehealth-based case study. JMIR Public Health Surveill. 2021;7 doi: 10.2196/24795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Basil G., Luther E., Burks J.D., Govindarajan V., Urakov T., Komotar R.J., Wang M.Y., Levi A.D. The focused neurosurgical examination during telehealth visits: guidelines during the COVID-19 pandemic and beyond. Cureus. 2021;13:11. doi: 10.7759/cureus.13503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ashry A.H., Alsawy M.F. Doctor-patient distancing: an early experience of telemedicine for postoperative neurosurgical care in the time of COVID-19. Egypt. J. Neurol. Psychiatr. Neurosurg. 2020;56:1–8. doi: 10.1186/s41983-020-00212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mouchtouris N., Lavergne P., Montenegro T.S., Gonzalez G., Baldassari M., Sharan A., Jabbour P., Harrop J., Rosenwasser R., Evans J.J. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parisien R.L., Shin M., Constant M., Saltzman B.M., Li X., Levine W.N., Trofa D.P. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J. Am. Acad. Orthop. Surg. 2020;28:e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franco D., Montenegro T., Gonzalez G.A., Hines K., Mahtabfar A., Helgeson M.D., Patel R., Harrop J. Telemedicine for the spine surgeon in the age of COVID-19: multicenter experiences of feasibility and implementation strategies. Global Spine J. 2020;11:608–613. doi: 10.1177/2192568220932168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tan K.-A., Thadani V.N., Chan D., Oh J.Y.-L., Liu G.K.-P. Addressing coronavirus disease 2019 in spine surgery: a rapid national consensus using the Delphi method via teleconference. Asian Spine J. 2020;14:373–381. doi: 10.31616/asj.2020.0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Daggubati L.C., Eichberg D.G., Ivan M.E., Hanft S., Mansouri A., Komotar R.J., D'Amico R.S., Zacharia B.E. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–e863. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Layfield E., Triantafillou V., Prasad A., Deng J., Shanti R.M., Newman J.G., Rajasekaran K. Telemedicine for head and neck ambulatory visits during COVID‐19: evaluating usability and patient satisfaction. Head Neck. 2020;42:1681–1689. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ryu W.H.A., Kerolus M.G., Traynelis V.C. Clinicians' user experience of telemedicine in neurosurgery during COVID-19. World Neurosurg. 2021;146:E359–E367. doi: 10.1016/j.wneu.2020.10.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lakshin G., Banek S., Keese D., Rolle U., Schmedding A. Telemedicine in the pediatric surgery in Germany during the COVID-19 pandemic. Pediatr. Surg. Int. 2021;37:389–395. doi: 10.1007/s00383-020-04822-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alves D.S., Times V.C., da Silva É.M.A., Melo P.S.A., de Araújo Novaes M. Advances in obstetric telemonitoring: a systematic review. Int. J. Med. Inf. 2020;134 doi: 10.1016/j.ijmedinf.2019.104004. [DOI] [PubMed] [Google Scholar]
- 58.Xu H., Huang S., Qiu C., Liu S., Deng J., Jiao B., Tan X., Ai L., Xiao Y., Belliato M. Monitoring and Management of Home-Quarantined Patients with COVID-19 using a WeChat-based telemedicine system: retrospective cohort study. J. Med. Internet Res. 2020;22 doi: 10.2196/19514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krenitsky N.M., Spiegelman J., Sutton D., Syeda S., Moroz L. Primed for a pandemic: implementation of telehealth outpatient monitoring for women with mild COVID-19. Semin. Perinatol. 2020;44 doi: 10.1016/j.semperi.2020.151285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martínez-García M., Bal-Alvarado M., Guerra F.S., Ares-Rico R., Suárez-Gil R., Rodríguez-Álvarez A., Pérez-López A., Casariego-Vales E., Rial Á.F., Rey R.R. Tracing of COVID-19 patients by telemedicine with telemonitoring. Rev. Clínica Española. 2020;220:472–479. doi: 10.1016/j.rce.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wali S., Margarido M.G., Shah A., Ware P., McDonald M., O'Sullivan M., Posada J.D., Ross H., Seto E. Expanding telemonitoring in a virtual world: a case study of the expansion of a heart failure telemonitoring program during the COVID-19 pandemic. J. Med. Internet Res. 2021;23:12. doi: 10.2196/26165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van Gaalen J.L., Hashimoto S., Sont J.K. Telemanagement in asthma: an innovative and effective approach. Curr. Opin. Allergy Clin. Immunol. 2012;12:235–240. doi: 10.1097/ACI.0b013e3283533700. [DOI] [PubMed] [Google Scholar]
- 63.Giudice A., Bennardo F., Antonelli A., Barone S., Fortunato L. COVID-19 is a new challenge for dental practitioners: advice on patients' management from prevention of cross infections to telemedicine. Open Dent. J. 2020;14:298–304. [Google Scholar]
- 64.O'Hara V.M., Johnston S.V., Browne N.T. The paediatric weight management office visit via telemedicine: pre‐to post‐COVID‐19 pandemic. Pediatr. Obes. 2020;15 doi: 10.1111/ijpo.12694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bluman E.M., Fury M.S., Ready J.E., Hornick J.L., Weaver M.J. Orthopedic telemedicine encounter during the COVID-19 pandemic: a cautionary tale. Trauma Case Rep. 2020;28 doi: 10.1016/j.tcr.2020.100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ghai B., Malhotra N., Bajwa S.J.S. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J. Anaesth. 2020;64:456. doi: 10.4103/ija.IJA_652_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Salzano A., D'Assante R., Stagnaro F.M., Valente V., Crisci G., Giardino F., Arcopinto M., Bossone E., Marra A.M., Cittadini A. Heart failure management during the COVID‐19 outbreak in Italy: a telemedicine experience from a heart failure university tertiary referral centre. Eur. J. Heart Fail. 2020;22:1048–1050. doi: 10.1002/ejhf.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jayawardena A.D., Mankarious L.A., Keamy D.G., Jr., Cohen M.S. Pediatric, family-Centered,“At-home” otologic physical examination in the COVID-19 era. Otolaryngology-Head Neck Surg. (Tokyo) 2020;163:1061–1063. doi: 10.1177/0194599820934776. [DOI] [PubMed] [Google Scholar]
- 69.Davarpanah A.H., Mahdavi A., Sabri A., Langroudi T.F., Kahkouee S., Haseli S., Kazemi M.A., Mehrian P., Mahdavi A., Falahati F. Novel screening and triage strategy in Iran during deadly coronavirus disease 2019 (COVID-19) epidemic: value of humanitarian teleconsultation service. J. Am. Coll. Radiol. 2020;17:734–738. doi: 10.1016/j.jacr.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chou E., Hsieh Y.-L., Wolfshohl J., Green F., Bhakta T. Onsite telemedicine strategy for coronavirus (COVID-19) screening to limit exposure in. Emerg. Med. J. 2020;37:335–337. doi: 10.1136/emermed-2020-209645. [DOI] [PubMed] [Google Scholar]
- 71.Ratwani R.M., Brennan D., Sheahan W., Fong A., Adams K., Gordon A., Calabrese M., Hwang E., Smith M., Booker E. A descriptive analysis of an on-demand telehealth approach for remote COVID-19 patient screening. J. Telemed. Telecare. 2020;27:490–495. doi: 10.1177/1357633X20943339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Giudice A., Barone S., Muraca D., Averta F., Diodati F., Antonelli A., Fortunato L. Can teledentistry improve the monitoring of patients during the covid-19 dissemination? a descriptive pilot study. Int. J. Environ. Res. Publ. Health. 2020;17:3399. doi: 10.3390/ijerph17103399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ghai S. Teledentistry during COVID-19 pandemic, diabetes & metabolic syndrome. Clin. Res. Rev. 2020;14:933–935. doi: 10.1016/j.dsx.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Russo V., Cassini R., Caso V., Donno C., Laezza A., Naddei M., Fiorelli A., Golino P., Nigro G. Nursing teleconsultation for the outpatient management of patients with cardiovascular disease during COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2021;18:2087. doi: 10.3390/ijerph18042087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li H.-L., Chan Y.C., Huang J.-X., Cheng S.W. Pilot study using telemedicine video consultation for vascular patients' care during the COVID-19 period. Ann. Vasc. Surg. 2020;68:76–82. doi: 10.1016/j.avsg.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Panda P.K., Dawman L., Panda P., Sharawat I.K. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Borchert A., Baumgarten L., Dalela D., Jamil M., Budzyn J., Kovacevic N., Yaguchi G., Palma-Zamora I., Perkins S., Bazzi M. Managing urology consultations during COVID-19 pandemic: application of a structured care pathway. Urology. 2020;141:7–11. doi: 10.1016/j.urology.2020.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Das A.V., Rani P.K., Vaddavalli P.K. Tele-consultations and electronic medical records driven remote patient care: responding to the COVID-19 lockdown in India. Indian J. Ophthalmol. 2020;68:1007. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Crane S.J., Ganesh R., Post J.A., Jacobson N.A. Telemedicine consultations and follow-up of patients with COVID-19. Mayo Clin. Proc. 2020;95:S33–S34. doi: 10.1016/j.mayocp.2020.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Iyengar K., Jain V.K., Vaishya R. Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them, Diabetes & Metabolic Syndrome. Clin. Res. Rev. 2020;14:797–799. doi: 10.1016/j.dsx.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Deshmukh A.V., Badakere A., Sheth J., Bhate M., Kulkarni S., Kekunnaya R. Pivoting to teleconsultation for paediatric ophthalmology and strabismus: our experience during COVID-19 times. Indian J. Ophthalmol. 2020;68:1387. doi: 10.4103/ijo.IJO_1675_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shenoy P., Ahmed S., Paul A., Skaria T.G., Joby J., Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic: feasibility and patient response in India. Clin. Rheumatol. 2020;39:2757–2762. doi: 10.1007/s10067-020-05200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pandey N., Srivastava R.M., Kumar G., Katiyar V., Agrawal S. Teleconsultation at a tertiary care government medical university during COVID-19 Lockdown in India–A pilot study. Indian J. Ophthalmol. 2020;68:1381. doi: 10.4103/ijo.IJO_1658_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rastogi S., Singh N., Pandey P. On the brighter side of COVID-19 induced Lockdown: devising the collateral methods to provide Ayurveda consultation during impasse. J. Ayurveda Integr. Med. 2020;12:36–47. doi: 10.1016/j.jaim.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gadzinski A.J., Andino J.J., Odisho A.Y., Watts K.L., Gore J.L., Ellimoottil C. Telemedicine and eConsults for hospitalized patients during COVID-19. Urology. 2020;141:12–14. doi: 10.1016/j.urology.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bourdon H., Jaillant R., Ballino A., El Kaim P., Debillon L., Bodin S., N'Kosi L. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: experience with 500 patients in March and April 2020. J. Fr. Ophtalmol. 2020;43:577–585. doi: 10.1016/j.jfo.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Green B.N., Pence T.V., Kwan L., Rokicki-Parashar J. Rapid deployment of chiropractic telehealth at 2 worksite health centers in response to the COVID-19 pandemic: observations from the field. J. Manipulative Physiol. Therapeut. 2020;43:e401–404. doi: 10.1016/j.jmpt.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Santonicola A., Zingone F., Camera S., Siniscalchi M., Ciacci C. Telemedicine in the COVID-19 era for Liver Transplant Recipients: an Italian lockdown area experience. Clin. Res. Hepatol. Gastroenterol. 2020;45 doi: 10.1016/j.clinre.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kumari J., Jat K.R., Kabra S. Role of telemedicine in follow-up care of children with respiratory illnesses at a tertiary care hospital—an ambispective observational study. Indian J. Pediatr. 2021;88:1–5. doi: 10.1007/s12098-020-03590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Naveen R., Sundaram T., Agarwal V., Gupta L. Teleconsultation experience with the idiopathic inflammatory myopathies: a prospective observational cohort study during the COVID-19 pandemic. Rheumatol. Int. 2021;41:67–76. doi: 10.1007/s00296-020-04737-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.An J., Kim J., Lai E.C., Lee B.-C. 2020. Effects of a Smartphone-Based Wearable Telerehabilitation System for in-Home Dynamic Weight-Shifting Balance Exercises by Individuals with Parkinson's Disease; pp. 5678–5681. 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), IEEE. [DOI] [PubMed] [Google Scholar]
- 92.Chang P.J., Jay G.M., Kalpakjian C., Andrews C., Smith S. Patient and provider-reported satisfaction of cancer rehabilitation telemedicine visits during the COVID-19 pandemic. Pm&R. 2021;13:7. doi: 10.1002/pmrj.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pinar U., Anract J., Perrot O., Tabourin T., Chartier-Kastler E., Parra J., Vaessen C., de La Taille A., Roupret M. Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic. World J. Urol. 2020;39 doi: 10.1007/s00345-020-03432-4. 1991–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Layton A.M., Irwin A.M., Mihalik E.C., Fleisch E., Keating C.L., Dimango E.A., Shah L., Arcasoy S.M. Telerehabilitation using fitness application in patients with severe cystic fibrosis awaiting lung transplant: a pilot study. Int. J. Telemed. Appl. 2021:7. doi: 10.1155/2021/6641853. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sinha V., Malik M., Nugent N., Drake P., Cavale N. The role of virtual consultations in plastic surgery during COVID-19 lockdown. Aesthetic Plast. Surg. 2021;45:777–783. doi: 10.1007/s00266-020-01932-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Capozzo R., Zoccolella S., Frisullo M.E., Barone R., Dell'Abate M.T., Barulli M.R., Musio M., Accogli M., Logroscino G. Telemedicine for delivery of care in frontotemporal lobar degeneration during COVID-19 pandemic: results from Southern Italy. J. Alzheim. Dis. 2020;76:481–489. doi: 10.3233/JAD-200589. [DOI] [PubMed] [Google Scholar]
- 97.Negrini S., Kiekens C., Bernetti A., Capecci M., Ceravolo M.G., Lavezzi S., Zampolini M., Boldrini P. Telemedicine from research to practice during the pandemic." Instant paper from the field" on rehabilitation answers to the Covid-19 emergency. Eur. J. Phys. Rehabil. Med. 2020;56:327–330. doi: 10.23736/S1973-9087.20.06331-5. [DOI] [PubMed] [Google Scholar]
- 98.Polanco E., Aquey M., Collado J., Campos E., Guzman J., Cuevas‐Budhart M.A., Divino‐Filho J.C., Ramos‐Sanchez A. A COVID‐19 pandemic‐specific, structured care process for peritoneal dialysis patients facilitated by telemedicine: therapy continuity, prevention, and complications management. Ther. Apher. Dial. 2021;25:599–612. doi: 10.1111/1744-9987.13635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Volcy J., Smith W., Mills K., Peterson A., Kene-Ewulu I., McNair M., Kelsey R., Mbaezue N. Assessment of patient and provider satisfaction with the change to telehealth from in-person visits at an academic safety net institution during the COVID-19 pandemic. J. Am. Board Fam. Med. 2021;34:S71–S76. doi: 10.3122/jabfm.2021.S1.200393. [DOI] [PubMed] [Google Scholar]
- 100.D'Anna L., Ellis N., Bentley P., Brown Z., Halse O., Jamil S., Jenkins H., Malik A., Kalladka D., Kwan J., Venter M., Banerjee S. Delivering telemedicine consultations for patients with transient ischaemic attack during the COVID-19 pandemic in a comprehensive tertiary stroke centre in the United Kingdom. Eur. J. Neurol. 2021;28:5. doi: 10.1111/ene.14750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Foster C.C., Steltzer M., Snyder A., Alden C., Helner K., Schinasi D.A., Bohling K., Allen K. Integrated multimodality telemedicine to enhance in-home care of infants during the interstage period. Pediatr. Cardiol. 2021;42:349–360. doi: 10.1007/s00246-020-02489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nicosia F.M., Kaul B., Totten A.M., Silvestrini M.C., Williams K., Whooley M.A., Sarmiento K.F. Leveraging Telehealth to improve access to care: a qualitative evaluation of Veterans' experience with the VA TeleSleep program. BMC Health Serv. Res. 2021;21:1–9. doi: 10.1186/s12913-021-06080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]