Abstract
Objective
This study aims to investigate factors influencing COVID-19 vaccination intention in the United States.
Methods
A cross-sectional survey was conducted with 800 respondents recruited from an online panel managed by a survey company. Path analysis was employed to examine the relationships between the study variables.
Results
First, perceived susceptibility to COVID-19 vaccine side effects was negatively associated with vaccination intention whereas perceived severity did not show any significant impact. Second, vaccine-related knowledge was not directly related to vaccination intention, but it had an indirect and positive effect on vaccination intention via decreasing perceived susceptibility. Third, doctor-patient communication strengthened the negative effect of vaccine knowledge on perceived susceptibility and severity.
Conclusion
The results of this study offer insights on how to increase people’s vaccination intention and reduce their psychological concerns when making COVID-19 vaccine-related decisions.
Practice implications
Government agencies should actively promote the effectiveness and importance of vaccination, while addressing concerns about vaccine safety in the public; Health initiatives also need to enhance the level of knowledge about COVID-19 vaccines through various media channels; Doctors can start the conversations about COVID-19 vaccination with their patients at the point of care and/or via online communication platforms.
Keywords: COVID-19, Vaccination intention, Risk perception, Knowledge, Doctor-patient communication
1. Introduction
Although government agencies across the globe have enacted precautionary measures such as use of masks and social distancing to flatten the COVID-19 infection curve, the long-term control of the COVID-19 pandemic will depend on the development and public acceptance of a safe and effective vaccine for achieving population immunity [1]. To date, several COVID-19 vaccines such as Moderna and Pfizer-BioNtech have been authorized for use in many countries in adult individuals. However, a sizeable portion of population is still unsure about getting vaccinated. For instance, a national survey revealed that in the UK and Ireland more than 30% of the respondents have a relatively low level of intention to take COVID-19 vaccines [2]. Likewise, around one quarter of the US citizens also reported that they do not intend to get vaccinated against COVID-19 [3]. Lin and colleagues found that the intention for COVID-19 vaccination significantly varies across countries, and many people prefer to wait until others have become vaccinated [4]. Increasing the public’s intention to get vaccinated is a potentially essential step to ensure the success of COVID-19 vaccination program. Therefore, the objective of this study is to investigate factors influencing COVID-19 vaccination intention in the context of the United States.
To date, many studies have explored various demographic factors (e.g., gender, age, health status) in relation to COVID-19 vaccination intention [2], [5], [6]. Although useful, such results are limited in explaining why a portion of people do not intend to uptake COVID-19 vaccines. A more informative approach would be to identify drivers and barriers to COVID-19 vaccination intention because it can provide information regarding targets for interventions [2]. For example, several studies from vaccine-related literature have examined the direct effect of vaccine-related knowledge in promoting vaccination intention, suggesting that the better understanding of the vaccine, the more likely people might choose to be vaccinated [7], [8], [9]. Health knowledge constitutes a background factor that promotes health prevention activities. People with more knowledge about health risks, signs and symptoms, and benefits of preventive actions tend to have a healthier lifestyle [10]. A higher level of health knowledge is also associated with less difficulty in navigating health care system, greater access to health care and more effective utilization of health resources for disease prevention [11]. Despite the crucial role of knowledge, many of the mediators and moderators between vaccine knowledge and vaccination intention have been poorly understood. To fill this research gap, the current study aims to explore the mediating role of individuals’ risk perception, a psychological factor that links knowledge to vaccination intention, and to investigate the moderating effect of doctor-patient communication, a contextual factor that strengthens the relationship between vaccine knowledge and vaccination intention. Understanding these drivers and mechanisms of people’s vaccination intention would help both public health scholars and practitioners implement evidence-based interventions to increase COVID-19 vaccination uptake and limit the spread of the coronavirus. The following section reviews the key concepts examined in this study.
1.1. Perceived risk of COVID-19 vaccine side effects
Perceived risk of vaccine side effects could be the most common barrier to vaccination [12]. The concept of risk perception is defined as beliefs about potential harm or the possibility of loss, which consists of two subdimensions: susceptibility and severity [13]. Perceived susceptibility is the probability that a person will be affected by the risk (e.g., side effects of a vaccine) whereas perceived severity is the extent of harm the risk would cause [13]. According to the secondary risk theory, people would evaluate the potential risk of some risk-reducing behaviors (e.g., getting vaccinated against COVID-19). If they deem the advocated behavior as risky, their intention to protect themselves from the primary risk (e.g., COVID-19) might decrease [14]. Previous studies have demonstrated the negative impact of vaccine risk perception on vaccination intention. For example, a national survey in the United States showed that perceived risk of vaccine adverse effects is negatively related to the intention to get vaccinated against a hypothetical avian flu among American adults [8]. In the context of COVID-19, concerns over vaccine safety and side effects were considered one of the most primary barriers to vaccination [12], [15]. Furthermore, recent studies have indicated that perceptions of susceptibility and severity may function differentially in risk communication contexts although they are the two subdimensions of perceived risk [16], [17], [18]. For example, although an illness is not highly serious, people may still take health-related actions if they perceive the possibility of getting this illness is high [19]. Therefore, in the current study, we examine the negative effects of vaccine-related susceptibility and severity on COVID-19 vaccination intention separately.
1.2. COVID-19 vaccine knowledge
To cope with the escalating susceptibility and severity of vaccine side effects, imparting relevant knowledge about the vaccine matters [20]. The knowledge-attitude-behavior theory presumes that individuals’ health knowledge and information serves as an important foundation for intention to perform a health-related behavior [21]. More specifically, people who have sufficient knowledge about a particular vaccine can better understand its potential benefits and importance, which would further shape positive beliefs about the vaccine and strengthen trust in vaccination. As such, they would not perceive vaccination as a risky behavior [22]. On the contrary, those with a lower level of knowledge are more likely to connect vaccines with adverse events and believe in misinformation about the safety of vaccines, which might increase perceived risk of vaccine side effects [23], [24], [25]. Moreover, as one facet of individuals’ health literacy, knowledge about specific health issues can be viewed as a prerequisite for health decision-making, including vaccine uptake [26], [27]. Some prior research has demonstrated a positive and direct association between vaccine knowledge and vaccination intention. For instance, Schulz and Hartung [9] found that the effect of general knowledge about vaccines on vaccination behavior is positive and consistent across six different vaccines, such as tetanus, pertussis, measles and influenza. Another survey study in China also suggested that more knowledge about vaccines is associated with a stronger intention to get vaccinated [28]. Therefore, it is important to explore the role of vaccine-related knowledge in reducing vaccine risk perception and triggering vaccination intention in the context of the COVID-19 pandemic.
1.3. Doctor-patient communication
Besides the roles of knowledge and risk perception, which are both at the intrapersonal level that is internal to the individual, we also explore the contextual influence of doctor-patient communication at the interpersonal level. There is an increasing recognition that doctor-patient communication plays a crucial role in maximizing the benefits of health promotion and treatment [29]. Quality doctor-patient communication focuses on doctors’ communication that respects and responds to patients’ preferences, needs and values, and ensures that patient values guide medical decision making [30]. To combat negative attitudes toward COVID-19 vaccination, doctors can play a key role. In this study, we argue that a good quality of doctor-patient communication would strengthen the relationship between health knowledge and risk perception, reasoned as follows. First, exchanging health information is a key function of doctor-patient communication. Attending to patients’ information needs may help enhance their understanding of a health-related issue and assist them to assess the severity and susceptibility to the issue, thereby engaging in quality health decision-making [31], [32]. Second, managing uncertainty via doctor-patient communication is also critical to health knowledge acquisition and decision-making. Uncertainty is particularly salient in the context of COVID-19 vaccination, because it is still relatively new and involves unpredictable side effects. An effective communication with doctors can provide both cognitive strategies and reassurance to manage negative emotions in order to handle health uncertainties [33]. Hence, given the utility of exchanging information and reducing uncertainties, it can be assumed that when people have good doctor-patient communication, they might become more knowledgeable about health issues (e.g., COVID-19 vaccine), and less concerned with vaccine safety and side effects.
1.4. Research hypotheses
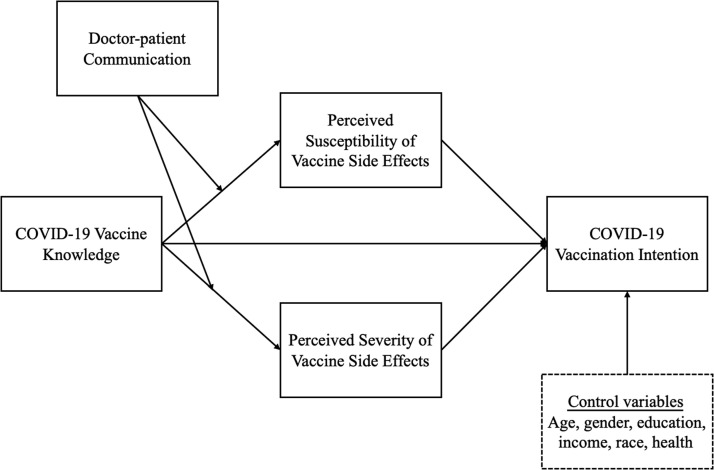
Taken together, this study proposes a research model to examine factors associated with COVID-19 vaccination intention (see Fig. 1). First, we hypothesize that perceived susceptibility and severity of vaccine side effects are negatively associated with vaccination intention. Second, we posit that COVID-19 vaccine knowledge is negatively associated with vaccine susceptibility and severity. Third, we explore the direct relationship between COVID-19 vaccine knowledge and vaccination intention. Finally, we investigate the moderating role of doctor-patient communication in influencing the relationship between COVID-19 vaccine knowledge and perceived susceptibility and severity of vaccine side effects.
Fig. 1.
Research model examining factors associated with COVID-19 vaccination intention.
2. Method
2.1. Sample
To test our proposed research model, we conducted a cross-sectional survey in the United States. The sample was recruited from an online panel managed by the survey company, Qualtrics. The company sent out an invitation email to 3106 panel members, and 800 respondents completed the survey, with the response rate of 25.8%, which is considered satisfactory for opt-in online panel surveys [34]. Quota sampling was used to ensure that the sample distribution (i.e., age, gender, ethnicity) was similar to the national profile of the country. Data collection was completed between 5 and 23 February 2021, an early stage of vaccination programs in the United States. The survey was conducted in English and took approximately 15 min to complete. This study was approved by the Institutional Review Board of the hosting university before data collection. Respondents’ informed consent was also obtained.
2.2. Measures
2.2.1. Perceived susceptibility
To assess perceived susceptibility to COVID-19 vaccine side effects, three items adapted from Farooq et al. [35] were used, including “I am vulnerable to contracting the side effects of COVID-19 vaccine in given circumstances”, “I think I am likely to get the side effects of COVID-19 vaccine”, and “I am at risk of catching the side effects of COVID-19 vaccine”. A 5-point Likert scale was used, ranging from “Strongly disagree” to “Strongly agree”. The average of the three items was created (M = 3.01, SD = 1.10, α = 0.86).
2.2.2. Perceived severity
Perceived severity of COVID-19 vaccine side effects was assessed using three items (1 = “Strongly disagree”, 5 = “Strongly agree”): “The negative impact of COVID-19 vaccine is very high”, “The negative impact of COVID-19 vaccine can be life-threatening”, and “The negative impact of COVID-19 vaccine is a serious threat for someone like me” [35]. The average of the three items was created (M = 3.14, SD = 1.19, α = 0.86).
2.2.3. Vaccination intention
On a five-point scale (1 = “Strongly disagree”, 5 = “Strongly agree”), we used four items derived from Wong et al. [36] to measure COVID-19 vaccination intention: “If a vaccine against COVID-19 infection is available in the market, I would take it”, “I intend to get vaccinated against COVID-19″, “I will get vaccinated against COVID-19 even if I must pay for the vaccine”, and “I am willing to put my name on the list to get vaccinated against COVID-19″. The four items were averaged to create a composite scale (M = 3.44, SD = 1.29, α = 0.94).
2.2.4. Doctor-patient communication
To assess quality of doctor-patient communication, drawn from the Health Information National Trends Survey [37], six items were used to ask participants to rate how often their doctors did the following in the past (1 = “Never”, 5 = “Always”): “Give you the chance to ask all the health-related questions you had”, “Give the attention you needed to your feelings and emotions”, “Involve you in decisions about your health care as much as you wanted”, “Make sure you understood the things you needed to do to take care of your health”, and “Help you deal with feelings of uncertainty about your health or health care”. The six items were averaged to create a composite measure (M = 3.59, SD = 0.95, α = 0.92).
2.2.5. Vaccine knowledge
Since the development of COVID-19 vaccines is still in progress, COVID-19 vaccine knowledge was assessed with a self-developed scale, following prior research’s approach to measuring knowledge about novel and emerging health-related issues [38]. It had eight items that were formulated based on the information presented by the official website of the World Health Organization, which regularly updates answers to questions that are frequently asked about COVID-19 vaccines [39]. The response categories for the knowledge items were “True” or “False”. Items answered correctly were assigned 1 point while incorrect answers were assigned 0 point. The eight items were as follows: “COVID-19 vaccines must be proven safe and effective in phase III clinical trials (True)”, “currently, there is some evidence that flu vaccines will protect against COVID-19 (False)”, “unlike most other vaccines, COVID-19 vaccines will be 100% effective (False)”, “all the COVID-19 vaccines are designed to teach the body’s immune system to safely recognize and block the virus that causes COVID-19 (True)”, “COVID-19 vaccines will provide long-term protection (False)”, “once COVID-19 vaccines are demonstrated to be safe and efficacious, they must be approved by World Health Organization (False)”, “most COVID-19 vaccines being tested or reviewed now are using two dose regimens (True)”, and “people who are immunocompromised, babies, and pregnant women can get COVID-19 vaccine (False)”. All the responses to these eight items were summed up to create one index, with a higher score representing a higher level of knowledge (M = 5.06, SD = 1.58, range: 0 – 8).
2.3. Data analysis
Path analysis was conducted to test the research model as it can simultaneously examine the patterns of relationships between variables and allow for mediation and moderation analyses. Six demographic factors including age, gender, education, income, race, and general health status were entered as control variables predicting vaccination intention. R software with the package “lavaan” was used to perform the analysis [40]. In addition, we used the package “psych” to conduct the mediation analysis as well as moderation analysis [41]. We estimated confidence intervals (CIs) with 1000 non-parametric bootstrap simulations.
3. Results
3.1. Sample characteristics
Table 1 summarizes the demographic information of the sample. Among the 800 respondents, 48.9% were male and 51.1% were female. The respondents had a mean age of 45.3 years (SD = 16.5, median = 41, range: 18 – 87). The median education level was “post high school or some college” and the median annual income was “$35,000 - $49,999″ in the sample. Overall, the sample distribution was similar to the U.S. population, based on census data from the CIA World Fact Book.1
Table 1.
Demographic characteristics of the U.S. respondents (N = 800).
| Demographic variable | n | % | |
|---|---|---|---|
| Gender | Male Female | 391409 | 48.951.1 |
| Age | 18–2425–3435–4445–5455 + | 6219419997248 | 7.824.224.912.131.0 |
| Education | High school or belowPost high school or some collegeCollege or above | 217 215368 | 27.126.946.0 |
| Annual income | $0–$49,999$50,000–$99,999$100,000 + | 421199180 | 52.622.524.9 |
| Ethnicity | WhiteNon–white | 576224 | 72.028.0 |
3.2. Results of path analysis
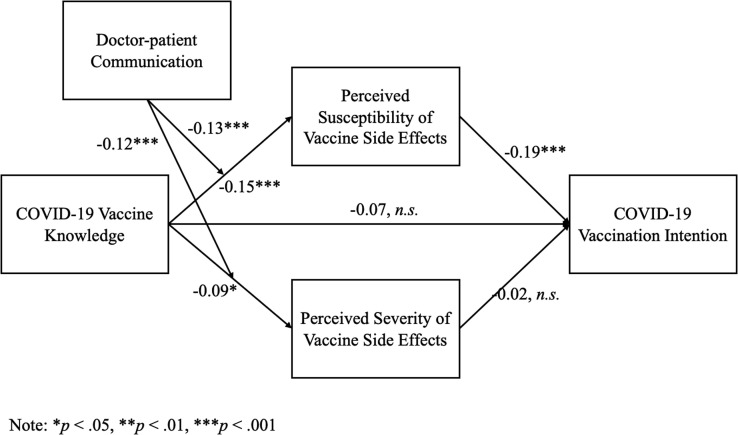
First, the path model had good model fit: χ2 (13) = 29.89, p = .005; CFI = 0.97; TLI = 0.95; RMSEA = 0.04. The model accounted for 17.4% of the variance in COVID-19 vaccination intention. Next, the path analysis showed that perceived susceptibility to vaccine side effects was negatively related to vaccination intention (β = −0.19, p < .001). However, perceived severity was not significantly related to vaccination intention (β = −0.02, p = .67). Further, vaccine knowledge was not directly associated with vaccination intention (β = −0.07, p = .06). On the other hand, vaccine knowledge was negatively associated with perceived susceptibility (β = −0.15, p < .001) as well as perceived severity (β = −0.09, p = .01).
The mediation analysis showed that the indirect effect of vaccine knowledge on vaccination intention via perceived susceptibility was positive (95% CI [0.03, 0.12]), whereas the indirect effect via perceived severity was insignificant (95% CI [−0.01, 0.08]). Finally, doctor-patient communication negatively moderated the negative effect of vaccine knowledge on perceived susceptibility (β = −0.13, p < .001) and vaccine severity (β = −0.12, p < .001). That means, the better quality of doctor-patient communication, the stronger negative relationship between vaccine knowledge and perceived susceptibility and severity.
Among the control variables, age (β = 0.19, p < .001), education (β = 0.11, p = .004), income (β = 0.12, p = .003), and general health status (β = 0.11, p = .001) were positively associated with vaccination intention. In addition, compared to gender (male), gender (female) was negatively related to vaccination intention (β = −0.12, p = .001). Race was not a significant predictor of vaccination intention. Fig. 2.
Fig. 2.
Factors associated with COVID-19 vaccination intention in the United States.
4. Discussion and conclusion
4.1. Discussion of major findings
This study proposed a research model to examine the impact of COVID-19 vaccine knowledge and risk perception of COVID-19 vaccine side effects on vaccination intention in the United States. First, we found that perceived susceptibility to COVID-19 vaccine side effects decreases vaccination intention whereas perceived severity does not exert any impact. This finding is in line with the existing studies, suggesting that vaccine-related risk perception is the major barrier to vaccination behavior [8], [12], [20]. For example, a recent survey conducted in Finland showed that people who perceive vaccines as a risk would refuse vaccination although they are worried about the COVID-19 situation [7]. More importantly, our study shows that when deciding whether to take vaccination, the American adults have more concern about the probability of contracting side effects of COVID-19 vaccines than the severity of these side effects. One possible explanation could be that the side effects are reported to be mild symptoms such as pain and mild fever after injection, which are acceptable for those supporting vaccination [42].
Second, we observed that knowledge about COVID-19 vaccines is not directly related to vaccination intention. This finding is inconsistent with several existing studies demonstrating a positive relationship between vaccine knowledge and vaccination intention [5], [27], [28]. Some theories might provide hints to explain the insignificant effect of knowledge. For instance, according to the diffusion of innovation theory [43], although imparting knowledge is an essential step in driving new practice adoption, it also involves sequential stages that lead to behavioral change. This argument is also in line with the key principle of the stages of change model [44]. On the other hand, we found that knowledge indirectly increases vaccination intention via reducing perceived susceptibility. This mediating effect implies that people who have more COVID-19 vaccine knowledge would not treat the vaccine as a threat, thereby showing more willingness to uptake vaccines. In contrast, those with a lower level of knowledge would view themselves as susceptible to some undesirable vaccine-related side effects and thus prefer not to get vaccinated against COVID-19.
Third, there is a negative interaction effect between doctor-patient communication and vaccine knowledge on perceived risk of COVID-19 vaccine side effects. This result highlights the importance of medical communication in influencing self-protective values and behaviors. Quality doctor-patient communication features that doctors provide useful health information, build partnership with patients, and offer reassurance and encouragement [45]. Under such circumstance, patients would have a better understanding of health issues at hand, and lower worry or concern about negative consequences of health risks, therefore, leading to disease prevention. The significant moderation effect of doctor-patient communication also reflects the core tenet of the ecological model of health care that advocates for the focus of patients’ social context, such as interpersonal communication at the point of care, in promoting population health [46]. Thus, to encourage vaccination during the COVID-19 pandemic, a productive interaction between doctors and patients could be a motivating factor.
4.2. Limitations and future directions
This study is not without limitations. First, it used a cross-sectional design to test our proposed model, which cannot establish causal claims between the variables. Experimental or longitudinal designs should be adopted in future studies to further test the causal assumptions of this model. Second, participants in this study were recruited from an online panel managed by the survey company. Although quota sampling strategy was used, only people who had access to the Internet were able to participate in the study, making the results difficult to be generalizable to the U.S. population. Third, we used a self-developed scale to assess COVID-19 vaccine knowledge. Although this scale was developed based on the information from the WHO, it might not capture all available knowledge about COVID-19 vaccines. Future studies should propose more comprehensive scales regarding COVID-19 vaccine knowledge when the development of COVID-19 vaccines progresses. Fourth, in this study, we only examined the mediating role of risk perception of COVID-19 vaccine side effects, whereas other factors could be in play as well. For example, perceived effectiveness of COVID-19 vaccine is another important consideration for many individuals. Prior research has well documented that a person’s belief as to whether the vaccine can actually help avoid the disease is a motivating factor of vaccination uptake [47]. Future research should continue to investigate other underlying mechanisms leading to vaccination intention.
4.3. Practice implications
Despite these limitations, this study has three major practical contributions. First, our findings provide important evidence regarding the impact of perceived susceptibility to COVID-19 vaccine side effects on vaccination intention in a sample of American adults. While the development of COVID-19 vaccines represents a significant ongoing scientific and political effort around the world, this study suggests that another battle that health professionals might face is to reduce perceived risk associated with vaccine side effects in the public [2]. To this end, government agencies need to actively promote the effectiveness and importance of vaccination for combating the pandemic [1]. This does not mean that the side effects of COVID-19 vaccines (e.g., tiredness, muscle pain) should be concealed because some people indeed experience them after injection. Instead, government agencies should design appropriate communication campaigns that balance the safety, effectiveness, and side effects of vaccines. In this manner, the public will have a more comprehensive understanding and objective assessment of vaccines.
Second, our study offers support for the indirect and positive role of vaccine knowledge in influencing COVID-19 vaccination intention. Health professionals need to enhance the level of knowledge about COVID-19 vaccines in the public through updating latest news about vaccine development via various channels such as newspapers, television, and social media. In addition, due to the prevalence of health misinformation on social media platforms [1], it is important to educate the public about how to discern accurate vaccine knowledge from misinformation. For instance, health authorities can present lay people information regarding counterarguments to misinformation and misinformation dissemination strategies used by those anti-vaccine groups in order to promote skepticism toward misinformation about vaccines in the public [48].
Finally, doctor-patient communication plays a crucial role in facilitating vaccination intention. We suggest that one way to promote decision-making about vaccination can start from the doctor’s office. Quality doctor-patient communication places patients at the center of care and fosters trusting healing relationships. Particular strategies to build trust and facilitate patient involvement in the relationship can include partnership building and encouragement, joint agenda setting, active listening, taking measures to ensure patient understanding, and nonverbal behaviors conveying empathy and warmth. Due to the great trust in doctors, patients’ worry about the safety and effectiveness of vaccines may be lower. Not surprisingly, doctors’ recommendation for vaccination becomes a strong driving force of vaccination uptake. Thus, doctors can try to start the conversations about COVID-19 vaccination with their patients. If time in medical encounters is limited, such conversations can also be done via e-mail and social media.
4.4. Conclusion
Understanding factors associated with COVID-19 vaccination intention is a key step in ensuring the success of COVID-19 vaccination program. In this study, we found that perceived susceptibility to vaccine side effects is a negative predictor of COVID-19 vaccination intention, and vaccine-related knowledge has an indirect and positive effect on vaccination intention via decreasing perceived susceptibility. Further, doctor-patient communication strengthens the negative effect of vaccine knowledge on perceived susceptibility and severity. Future vaccine promotion initiatives should take the roles of vaccine knowledge and doctor-patient communication into account when addressing the negative consequence of perceived susceptibility to COVID-19 vaccine side effects.
CRediT authorship contribution statement
Han Zheng: Conceptualization, Writing – original draft, Data analysis. Shaohai Jiang: Writing – original draft, Writing – review & editing. Qiaofei Wu: Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Funding: This work was supported by the Singapore Academic Research Fund Tier 1 (project number: FY2019-FRC4-002).
Footnotes
References
- 1.Chou W.-Y.S., Budenz A. Considering Emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35:1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 2.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:1–15. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thunstrom L., Ashworth M., Finnoff D., Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. SSRN Electron J. 2020 doi: 10.1007/s10393-021-01524-0. https://ssrn.com/abstract=3593098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin C., Tu P., Beitsch L.M. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2021;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46:270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S., et al. Fearing the disease or the vaccine: The case of COVID-19. Pers Individ Dif. 2021;172 doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nancy Chen N.-T. Predicting vaccination intention and benefit and risk perceptions: the incorporation of affect, trust, and television influence in a dual-mode model. Risk Anal. 2015;35:1268–1280. doi: 10.1111/risa.12348. [DOI] [PubMed] [Google Scholar]
- 9.Schulz P.J., Hartung U. Unsusceptible to social communication? The fixture of the factors predicting decisions on different vaccinations. Health Commun. 2020:1–9. doi: 10.1080/10410236.2020.1771119. [DOI] [PubMed] [Google Scholar]
- 10.Aweke Y.H., Ayanto S.Y., Ersado T.L. Vol. 12. Community-based cross-sectional study; Southern Ethiopia: 2017. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone. (PLoS One). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akhu-Zaheya L.M., Jagbir M.T., Othman A., Ahram M. Media use for seeking health/cancer-related information: findings from knowledge, attitudes and practices towards cancer prevention and care survey in Jordan. Int J Nurs Pr. 2014;20:608–615. doi: 10.1111/ijn.12196. [DOI] [PubMed] [Google Scholar]
- 12.Nguyen K.H., Srivastav A., Razzaghi H., Williams W., Lindley M.C., Jorgensen C., et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination — United States, September and December 2020. Am J Transpl. 2021;21:1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darker C. In: Risk perception BT - encyclopedia of behavioral medicine. Gellman M.D., Turner J.R., editors. Springer New York; New York, NY: 2013. pp. 1689–1691. [DOI] [Google Scholar]
- 14.Cummings C.L., Rosenthal S., Kong W.Y. Secondary risk theory: validation of a novel model of protection motivation. Risk Anal. 2021;41:204–220. doi: 10.1111/risa.13573. [DOI] [PubMed] [Google Scholar]
- 15.Chu H., Liu S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ Couns. 2021;104:1878–1886. doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.So J., Kuang K., Cho H. Information seeking upon exposure to risk messages: predictors, outcomes, and mediating roles of health information seeking. Communic Res. 2019;46:663–687. [Google Scholar]
- 17.Li J., Zheng H. Online informationseeking and disease prevention intent during COVID-19 outbreak. J Mass Commun Q. 2020 doi: 10.1177/1077699020961518. [DOI] [Google Scholar]
- 18.Lu J., Luo M., Yee A.Z.H., Sheldenkar A., Lau J., Lwin M.O. Do superstitious beliefs affect influenza vaccine uptake through shaping health beliefs? Vaccine. 2019;37:1046–1052. doi: 10.1016/j.vaccine.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 19.Thompson J.K., Ata R., Roehrig M., Chait S. In: Tanning: natural and artificial. Cash TBT-E of BI H.A., editor. Academic Press; Oxford: 2012. pp. 775–782. [DOI] [Google Scholar]
- 20.Betsch C., Wicker S. E-health use, vaccination knowledge and perception of own risk: drivers of vaccination uptake in medical students. Vaccine. 2012;30:1143–1148. doi: 10.1016/j.vaccine.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 21.Kallgren C.A., Wood W. Access to attitude-relevant information in memory as a determinant of attitude-behavior consistency. J Exp Soc Psychol. 1986;22:328–338. [Google Scholar]
- 22.MacDonald N.E., Smith J., Appleton M. Risk perception, risk management and safety assessment: what can governments do to increase public confidence in their vaccine system? Biologicals. 2012;40:384–388. doi: 10.1016/j.biologicals.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Reyna V.F. Risk perception and communication in vaccination decisions: a fuzzy-trace theory approach. Vaccine. 2012;30:3790–3797. doi: 10.1016/j.vaccine.2011.11.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rozbroj T., Lyons A., Lucke J. Psychosocial and demographic characteristics relating to vaccine attitudes in Australia. Patient Educ Couns. 2019;102:172–179. doi: 10.1016/j.pec.2018.08.027. [DOI] [PubMed] [Google Scholar]
- 25.Moran M.B., Frank L.B., Chatterjee J.S., Murphy S.T., Baezconde-Garbanati L. Information scanning and vaccine safety concerns among African American, Mexican American, and non-Hispanic White women. Patient Educ Couns. 2016;99:147–153. doi: 10.1016/j.pec.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L., Zhang Y., Young R., Wu X., Zhu G. Effects of vaccine-related conspiracy theories on chinese young adults’ perceptions of the HPV vaccine: an experimental study. Health Commun. 2021;36:1343–1353. doi: 10.1080/10410236.2020.1751384. [DOI] [PubMed] [Google Scholar]
- 27.Loke A.Y., Kwan M.L., Wong Y.-T., Wong A.K.Y. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8:349–362. doi: 10.1177/2150131917742299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu Z., Yang J.Z. In the wake of scandals: how media use and social trust influence risk perception and vaccination intention among Chinese parents. Health Commun. 2021;36:1188–1199. doi: 10.1080/10410236.2020.1748834. [DOI] [PubMed] [Google Scholar]
- 29.Epstein R., Street R. Patient-centered communication in cancer care: promoting healing and reducing suffering. Natl Cancer Inst. 2007 [Google Scholar]
- 30.Institute of Medicine (US) Committee on Quality of Health Care in America. Quality of Health Care in America. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. 2001.
- 31.Mauksch L.B., Dugdale D.C., Dodson S., Epstein R. Relationship, communication, and efficiency in the medical encounter: creating a clinical model from a literature review. Arch Intern Med. 2008;168:1387–1395. doi: 10.1001/archinte.168.13.1387. [DOI] [PubMed] [Google Scholar]
- 32.Borah P., Hwang J. Trust in doctors, positive attitudes, and vaccination behavior: the role of doctor–patient communication in H1N1 vaccination. Health Commun. 2021:1–9. doi: 10.1080/10410236.2021.1895426. [DOI] [PubMed] [Google Scholar]
- 33.Hasan I., Rashid T. Clinical communication, cancer patients & considerations to minimize the challenges. J Cancer Ther. 2016;07:107–113. [Google Scholar]
- 34.Sauermann H., Roach M. Increasing web survey response rates in innovation research: an experimental study of static and dynamic contact design features. Res Policy. 2013;42:273–286. [Google Scholar]
- 35.Farooq A., Laato S., Islam A.K.M.N. Impact of online information on self-isolation intention during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. 2020;22:19128. doi: 10.2196/19128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16:2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Cancer Institute . Health Information National Trend Survey. Natl Cancer Inst 2019. https://hints.cancer.gov/about-hints/learn-more-about-hints.aspx.
- 38.Ho S.S., Peh X., Soh V.W.L. The cognitive mediation model: Factors influencing public knowledge of the H1N1 pandemic and intention to take precautionary behaviors. J Health Commun. 2013;18:773–794. doi: 10.1080/10810730.2012.743624. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization . Coronavirus disease (COVID-19): Vaccines. World Heal Organ 2020. https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey=%7Badgroupsurvey%7D&gclid=Cj0KCQjwsqmEBhDiARIsANV8H3a7gAT5b2a7T2YUHJDmQ3pMFwDcQPdZxJ1kV4KB5y36ydERAwvhhHIaAuWKEALw_wcB.
- 40.Rosseel Y. Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA) J Stat Softw. 2012;48:1–36. [Google Scholar]
- 41.Revelle W. Using the psych package to generate and test structural models. Recuper Http//Bioconductor Stat Tu-Dortmund de/Cran/Web/Packages/Psych/Vignettes/Psych_for_sem Pdf 2017.
- 42.Sah R. , Shrestha S. , Mehta R. , Sah SK , Raaban AR , Dharma K. , et al. AZD1222 (Covishield) vaccination for COVID-19: experiences, challenges and solutions in Nepal. Travel Med Infect Dis 2021. [DOI] [PMC free article] [PubMed]
- 43.Rogers E.M. Free Press; New York, NY: 2003. Diffusion of innovations. [Google Scholar]
- 44.Glanz K. Public Health Service, National. US Department of Health and Human Services,; 1997. Theory at a glance: a guide for health promotion practice. [Google Scholar]
- 45.Jiang S. How does patient-centered communication improve emotional health? An exploratory study in China. Asian J Commun. 2018;28:298–314. [Google Scholar]
- 46.Street R.L., Jr. Handbook of Health Communication. Lawrence Erlbaum Associates Publishers,; Mahwah, NJ, US: 2003. Communication in medical encounters: an ecological perspective; pp. 63–89. [Google Scholar]
- 47.Krieger J.L., Sarge M.A. A serial mediation model of message framing on intentions to receive the human papillomavirus (HPV) vaccine: revisiting the role of threat and efficacy perceptions. Health Commun. 2013;28:5–19. doi: 10.1080/10410236.2012.734914. [DOI] [PubMed] [Google Scholar]
- 48.Cook J., Lewandowsky S., Ecker U.K.H. Neutralizing misinformation through inoculation: exposing misleading argumentation techniques reduces their influence. PLoS One. 2017;12 doi: 10.1371/journal.pone.0175799. [DOI] [PMC free article] [PubMed] [Google Scholar]