Abstract
Personal protective behaviors and their dynamic change are known to play a major role in the community spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal pathogen of the coronavirus disease 2019 (COVID-19) pandemic. In this study, a total of 3229 students in Chinese universities completed an online survey about their knowledge on transmission and personal protective behavior before and after COVID-19 vaccination. Of the respondents, 87.6% had been vaccinated. Most students believed that the large droplet (97.0%) and short-range airborne (89.3%) routes were the two most likely SARS-CoV-2 transmission routes, whereas only 24.1% considered long-range airborne transmission to be possible. Students who would be expected to possess better knowledge about virus transmission (e.g., students of medicine) reported better personal protective behaviors. Female students reported relatively better personal hygiene practices than male students, so did the confident students than their diffident peers. Students washed their hands on average of 5.76 times per day during the pandemic. Students at universities in southern regions washed their hands more frequently but paid less attention to indoor ventilation than did their northern counterparts. Interestingly, students who are fear of being infected had the bad personal hygiene. University students wore 22% less masks in public indoor environments after vaccination. Chinese university students weakened their personal protective behavior after vaccination and it may increase the potential risk of infection in the new waves of variant virus (e.g. delta).
Keywords: COVID-19, University student, Vaccination, Personal protective behavior, Personal hygiene, Mask
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has significantly disrupted economies and human lives. As of the end of June 2021, over 180 million people have been infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal pathogen, and over 4 million have died from the infection (https://covid19.who.int/). Most of these infections might have occurred due to close contact, and the short-range airborne route has been considered as the predominant virus transmission route, although long-range airborne transmission is also possible [1]. Although the surface touch (i.e., fomite) and large droplet routes might also play a role in transmission, this is likely insignificant [2]. Most infections have been transmitted between people in indoor settings, and individual behavior has played a major role in transmission [3,4]. It remained unclear, however, whether people would change their personal infection control behavior after being vaccinated. In 2021, the US CDC announced that masks and distancing no longer need to be observed during indoor gatherings of fully vaccinated people [5]; in contrast, China still encouraged personal precautionary and preventive behavior at the time of our study. Although existing COVID-19 vaccines appear to be effective against new strains of SARS-CoV-2, such as the delta variant [6], their relatively lower effectiveness may also affect human behavior.
We considered university students as the subjects in our study on changes in human behavior. Students have been vulnerable to COVID-19 due to their frequent close contacts [7], ability to transmit infections carried from their homes [8], and potential risk of mental health problems [9]. During the pandemic, many universities were closed to reduce social interaction [10]. Many outbreaks were reported after first few weeks of the fall semester, despite the implementation of various public health measures to reduce the transmission of SARS-CoV-2 [11]. In the US, at least 26,000 new infections were reported at over 750 colleges and universities by August 26, 2020 [12]. In Austin, Texas, 64 of 231 students who had close contact with a case of COVID-19 received positive test results on March 28, 2020 [13]. Some researchers suggested that universities may need to test students every 3 days to prevent major outbreaks [14]. University students also serve as good candidates for a behavioral study, as they are also expected to be relatively more knowledgeable about transmission than the general public.
Although university students are at high risk of exposure, they may be uninclined to be vaccinated because they are not generally clinically vulnerable to COVID-19 [15]. In China, however, a large proportion of students have been vaccinated. China has adopted a best-effort strategy to stop the community spread of SARS-CoV-2, particularly the new variants (e.g., delta). A weakening of personal protective behavior would jeopardize such efforts, as the efficacy of existing vaccines against these new variants may be low [16]. Therefore, it is necessary to understand the anti-COVID-19 protective behavior of university students, especially behavior changes after vaccination.
Some non-pharmaceutical interventions such as indoor ventilation, surgical mask wearing, and hand washing were commonly used in our daily life during the COVID-19 pandemic. Surgical mask was considered reducing the infection risk by around 50% [17], and approaching 80% of infection risk could be reduced if all people wear a mask indoors [18]. People were mandatorily asked for mask wearing when entering all types of public indoor environments in China [19]. Although fomite is not a main transmission route for SARS-CoV-2, action self-efficacy was positively associated with hand washing [20]. Moreover, indoor ventilation plays an important role in COVID-19 spread due to potential transmission route of airborne [21].
In this study, we performed an online survey of both undergraduate and postgraduate students at Chinese universities to understand the levels of COVID-19 transmission knowledge and protective behavior. We also analyzed changes in the students’ protective behavior after vaccination. The results should inform COVID-19 prevention and control efforts at universities.
2. Methods
2.1. Participants and procedures
The online survey was conducted on June 30, 2021. All of the respondents were university students at the time of the survey and completed the survey within that day. Vaccinated students were asked to answer 38 questions, and other respondents were asked to answer 31 questions. A questionnaire was considered invalid if the respondent submitted all responses within 2 min, the answer to the test question “Please select the third option” was wrong, or the respondent was neither an undergraduate nor a postgraduate student. All respondent cannot resubmit the questionnaire if it was invalid at the first time. Of the 3652 collected questionnaires, 423 were invalid. Finally, 3229 valid questionnaires were analyzed.
The survey was conducted using a professional software application (www.wjx.cn) and distributed by a communication group of professors via WeChat, the most widely used messaging and social media app in China. Students were first recruited by their supervisors and then their peers to complete the survey. The survey took approximately 4 min to complete, and the respondents received RMB 10 after a successful valid submission.
2.2. Scope of the survey questions
The survey questions addressed basic personal information, personality characteristics (e.g., confidence level), knowledge about COVID-19, COVID-19 prevention and control in the university setting, and changes in personal protective behavior after vaccination. Solicited personal information included gender, age, undergraduate or postgraduate status, current undergraduate or postgraduate year, major area of study, province where the university was located, and vaccination status. Questions on protection behavior before and after vaccination addressed the hand washing frequency, surface disinfection, air disinfection, mask wearing, attention given to indoor ventilation, personal protective measures taken in different indoor environments, and fear of contracting COVID-19. Questions on non-individual COVID-19 prevention addressed the convenience of hand washing, ventilation in classrooms and student offices, and availability of guidance on COVID-19 prevention and control. Questions on knowledge and personal preferences regarding COVID-19 included vaccine efficacy, possible and dominant SARS-CoV-2 transmission routes, the prevention and control measures perceived as most efficient, intention to be re-vaccinated after vaccination failure, and changes in protective behavior due to outbreaks in other cities. To determine how a confident personality might influence personal protective behaviors, four questions were set based on a study by Weinstein [22]. The personal confidence may not be accurately calculated because we only selected 4 typical questions from 42 questions in original studies. The questions were scored on a 5-point scale, with a score of 5 indicating extremely confident and 1 indicating extremely diffident. We used the average score of these four questions to reflect the personal confidence level of the respondent. The detailed questionnaire is presented in Appendix A.
2.3. Data analysis
The descriptive statistics of university students' protection behavior are presented as means, medians, and frequencies. When processing the data, we first validated the normality of distribution. If the data were consistent with a normal distribution, the independent sample t-test was used to calculate correlations between two factors. Otherwise, the Kruskal–Wallis test was used. Wilcoxon's two-sample t-test was used for correlation analyses of changes in protective behavior due to vaccination. All of the statistical analyses were performed using IBM SPSS 26.0. A two-tailed p-value < 0.05 was considered to indicate statistical significance. In this study, we only analyzed factors significantly correlated with the dependent variables.
3. Results
Of the 3229 respondents, 49.9% (n = 1611) were male, and more than 90% (n = 2914) were between 19 and 27 years of age; 51.4% (n = 1659) were undergraduates and 48.6% (n = 1570) were postgraduates. The majority of students (69.4%, n = 2225) studied engineering, followed by science (14.5%, n = 464), medicine (4.2%, n = 136), and management (3.8%, n = 122). The largest numbers of respondents were from Guangdong (20.9%, n = 675), Liaoning (12.5%, n = 404), Beijing (12.5%, n = 403), Jiangsu (9.6%, n = 310), and Shanghai (7.8%, n = 252) provinces (Fig. S1). Details on the respondents’ personal information are listed in Table S1.
3.1. Vaccination behavior
More male (53.4%) and postgraduate students (50.4%) exhibited a confident personality than did female (40.9%) and undergraduate students (44.1%), respectively (Table S2). Students whose majors were management (27.9% male) and medicine (34.6% male) had the highest and lowest confidence levels, respectively.
Furthermore, 87.6% of the surveyed students were vaccinated at the time of the survey (Table 1 ). Vaccination was significantly associated with gender, education, current undergraduate or postgraduate year, and province (Table 1, Figs. S2 and S3). Male students had a higher vaccination rate (88.9%) than female students (86.3%), and undergraduates had a higher vaccination rate (88.8%) than postgraduates (86.4%). Students whose majors were engineering, science, and medicine had the highest vaccination rates (more than 88%), whereas those in management had the lowest vaccination rate (77.0%). Students at universities in Shanghai, Beijing, and Hubei had the highest vaccination rates (>92%), whereas those in Zhejiang had the lowest rate (78.4%).
Table 1.
Distribution of vaccination behavior by personal attribute.
| Personal attribute | Vaccinated | Not vaccinated | p value |
|---|---|---|---|
| Total, N = 3229 (%) | 2829 (87.6%) | 400 (12.4%) | – |
| Gender, n = 3229 (%) | – | – | 0.028 |
| Male (n = 1611) | 1432 (88.9%) | 179 (11.1%) | – |
| Female (n = 1618) | 1397 (86.3%) | 221 (13.7%) | – |
| Education, n = 3229 (%) | – | – | 0.037 |
| Undergraduate (n = 1659) | 1473 (88.8%) | 186 (11.2%) | – |
| Postgraduate (n = 1570) | 1356 (86.4%) | 214 (13.6%) | – |
| Current year of under-/post-graduatea | – | – | <0.001 |
| Major, n = 2947 (%) | – | – | 0.001 |
| Engineering (n = 2225) | 1975 (88.8%) | 250 (11.2%) | – |
| Science (n = 464) | 415 (89.4%) | 49 (10.6%) | – |
| Medicine (n = 136) | 120 (88.2%) | 16 11.8%) | – |
| Management (n = 122) | 94 (77.0%) | 28 (23.0%) | – |
| Personal confidence | – | – | 0.080 |
| Province distributionb | – | – | <0.001 |
3.2. Personal protective behavior
As shown in Table 2 , students washed their hands, cleaned their desk surfaces, and disinfected the indoor air an average of 5.76, 1.42, and 0.62 times per day, respectively. Almost 20% of the students paid much attention to indoor ventilation, whereas only 0.8% of students paid no attention. Students who reported a higher frequency of hand washing were significantly more likely to report higher frequencies of surface disinfection (p < 0.001) and air disinfection (p < 0.001) and to pay more attention to indoor ventilation (p < 0.001). Male students washed their hands an average of 5.55 times per day during the pandemic, and this value was 6.9% lower than that reported by female students (5.96 times per day). Compared with postgraduates, undergraduates reported significantly higher frequencies of hand washing (p < 0.001) and surface and air disinfection (p = 0.001). Students in engineering, science, and medicine reported a higher frequency of hand washing than did students in management. Compared with diffident students, confident students reported 11.9%, 51.9%, and 108.8% higher frequencies of hand washing (6.00 times per day), surface disinfection (1.58 times per day), and air disinfection (0.71 times per day), respectively.
Table 2.
Distribution of hygiene behavior by personal attribute.
| Personal attribute | Hand washing (time/day) | Surface disinfection (time/day) | Air disinfection (time/day) | Indoor ventilationa |
|---|---|---|---|---|
| Total | 5.76 | 1.42 | 0.62 | 3.86 |
| Gender | p < 0.001 | p = 0.001 | p = 0.179 | p = 0.333 |
| Male | 5.55 | 1.39 | – | – |
| Female | 5.96 | 1.44 | – | – |
| Education | p = 0.048 | p < 0.001 | p = 0.012 | p = 0.191 |
| Undergraduate | 5.97 | 1.56 | 0.70 | – |
| Postgraduate | 5.54 | 1.26 | 0.57 | – |
| Major | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Engineering | 5.77 | 1.45 | 0.62 | 3.87 |
| Science | 5.74 | 1.30 | 0.59 | 3.82 |
| Medicine | 5.73 | 1.29 | 0.46 | 3.81 |
| Management | 5.27 | 1.35 | 0.56 | 3.84 |
| Confidenceb | p = 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Confident | 6.00 | 1.58 | 0.71 | 3.97 |
| Neutral | 5.58 | 1.31 | 0.57 | 3.79 |
| Diffident | 5.36 | 1.04 | 0.34 | 3.64 |
A value of 5 indicates a high level of attention to indoor ventilation, and 1 indicates very little attention.
Confidence is divided into three categories. A score of ≥3.5 is considered confident, ≤ 2.5 is considered diffident, and 2.5–3.5 is considered neutral.
As shown in Table 3 , male students were more likely than female students to report wearing masks in familiar indoor environments, such as homes, dormitories, offices, and libraries, but less likely to wear masks in non-familiar indoor environments, such as shops, gyms, and crowded places (e.g., airports). Undergraduates wore masks more frequently than postgraduates, with higher relative rates of 25.6%, 56.0%, 20.5%, and 10.6% in classrooms, offices, libraries, and gyms, respectively. Students in medicine reported the highest mask wearing rates in almost all indoor environments, whereas students in engineering and science had the lowest rates. Compared with neutral and diffident students, confident students were most likely to wear masks in all indoor environments.
Table 3.
Mask wearing ratesa in different indoor environments.
| Personal Attribute | Home | Dorm | Class | Office | Library | Canteen | Shop | Gym | Crowd-ed places |
|---|---|---|---|---|---|---|---|---|---|
| Total | 2.0% | 3.1% | 27.8% | 17.3% | 38.9% | 30.5% | 81.2% | 33.9% | 94.6% |
| Gender, p value | 0.001 | 0.001 | 0.584 | 0.003 | <0.001 | 0.403 | <0.001 | 0.002 | 0.009 |
| Male | 2.7% | 4.2% | – | 19.2% | 41.9% | – | 78.8% | 31.3% | |
| Female | 1.2% | 2.1% | – | 15.3% | 35.8% | – | 83.7% | 36.5% | |
| Education, p value | 0.678 | 0.217 | <0.001 | <0.001 | <0.001 | 0.072 | 0.490 | 0.038 | 0.358 |
| Undergraduate | – | – | 30.9% | 20.9% | 42.4% | – | – | 35.6% | – |
| Postgraduate | – | – | 24.6% | 13.4% | 35.2% | – | – | 32.2% | – |
| Major, p value | 0.145 | 0.079 | <0.001 | <0.001 | <0.001 | <0.001 | 0.336 | <0.001 | 0.045 |
| Engineering | 2.1% | 3.2% | 29.0% | 17.1% | 38.8% | 31.5% | 80.6% | 33.7% | 94.2% |
| Science | 0.6% | 1.3% | 16.8% | 10.3% | 32.5% | 20.0% | 81.0% | 24.1% | 95.5% |
| Medicine | 2.2% | 3.7% | 35.3% | 29.4% | 38.2% | 36.0% | 86.8% | 39.7% | 99.3% |
| Management | 0.8% | 4.9% | 34.4% | 26.2% | 53.3% | 37.7% | 82.8% | 45.1% | 92.6% |
| Confidence, p value | 0.027 | <0.001 | 0.001 | 0.001 | 0.092 | 0.013 | 0.031 | 0.407 | 0.974 |
| Confident | 2.6% | 4.3% | 30.7% | 19.9% | 40.4% | 33.0% | 81.9% | – | – |
| Neutral | 1.3% | 1.8% | 25.8% | 15.0% | 38.1% | 28.5% | 81.7% | – | – |
| Diffident | 1.8% | 3.2% | 22.1% | 14.6% | 33.9% | 27.1% | 75.4% | – | – |
Mask wearing is defined as practicing this behavior during more than 50% of the time spent indoors.
On average, 91.0%, 26.5%, 2.7%, 0.7%, 1.3%, and 5.6% of the students wore a surgical mask, N95 respirator, face shield, protective clothing, goggles, and gloves, respectively, in crowded indoor environments (e.g., train stations) (Table S3). Compared with male students, female students were more likely to wear surgical masks (89.6% vs. 92.4%) and gloves (3.5% vs. 7.7%). No significant correlation was observed between education level (undergraduate/postgraduate) or major and personal protective measures. Confident students most frequently reported using an N95 respirator (28.3%), face shield (3.5%), and goggles (1.9%) in crowded indoor environments, compared with diffident students.
Table 4 shows that 23.9% and 44.0% of the students reported being afraid and not afraid of being infected, respectively. Female students and undergraduates were slightly more afraid of being infected than were male students and postgraduates. Students in medicine had the lowest level of fear of being infected, whereas those in management had the highest level of fear. Although confident students took more personal protective measures, we found no significant correlation between the level of confidence and fear of being infected. Students who expressed a greater fear of being infected also reported worse personal protective behavior.
Table 4.
Fear of being infected with COVID-19 by personal attribute.
| Personal attribute | Fear of being infecteda | p value |
|---|---|---|
| Total | 3.3 | – |
| Gender | – | <0.001 |
| Male | 3.40 | |
| Female | 3.20 | – |
| Education | – | 0.026 |
| Undergraduate | 3.25 | – |
| Postgraduate | 3.34 | – |
| Major, p value | – | 0.025 |
| Engineering | 3.29 | – |
| Science | 3.40 | – |
| Medicine | 3.46 | – |
| Management | 3.06 | – |
| Confidenceb | – | 0.196 |
A value of 1 indicates a high level of fear of being infected with COVID-19, and 5 indicates no fear during the pandemic.
Confidence is divided into three categories. A score of ≥3.5 is considered confident, ≤ 2.5 is considered diffident, and 2.5–3.5 is considered neutral.
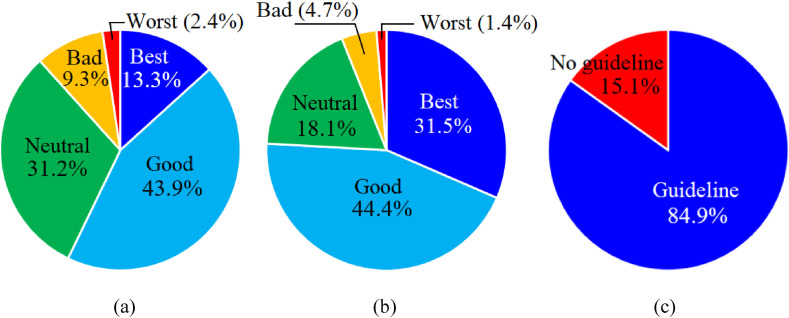
Nearly 76% of the universities provided convenient facilities for hand washing, whereas around 6% had inconvenient facilities (Fig. 1 a). Only 57.2% of the students were satisfied with the indoor ventilation in their universities, and 11.7% were dissatisfied (Fig. 1b). Furthermore, 84.9% of the students knew about the guidelines for COVID-19 prevention at their universities (Fig. 1c).
Fig. 1.
Analysis of COVID-19 prevention and control at Chinese universities. Satisfaction with the (a) convenience of facilities for hand washing, (b) ventilation of indoor spaces, and (c) availability of guidance on COVID-19 prevention.
3.3. Personal knowledge on COVID-19
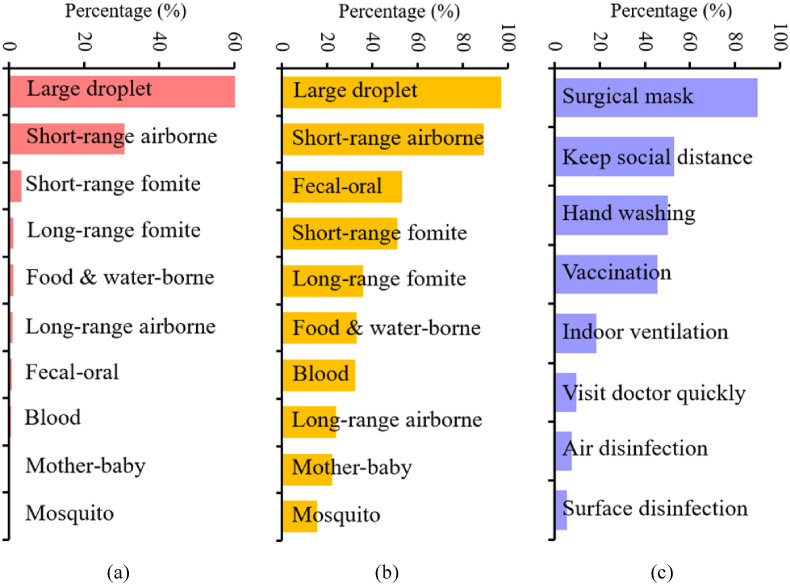
Students believed that large droplet (97.0%), short-range airborne (89.3%), fecal–oral (53.3%), and short-range fomite (e.g., hand shake) (50.9%) were the four main SARS-CoV-2 transmission routes (Fig. 2 a). Only 24.1% of the students believed that long-range airborne transmission of SARS-CoV-2 was possible. As shown in Table S4, female students believed that SARS-CoV-2 could be transmitted via more routes (e.g. fecal–oral, blood, mother–baby, mosquito, and food/water) than did male students. More undergraduates (vs. postgraduates) believed that long-range airborne, blood, mosquito, and food/water transmission routes were possible, whereas more postgraduates (vs. undergraduates) believed that short-range fomite and fecal–oral transmission routes were possible.
Fig. 2.
Students' knowledge about COVID-19. Responses regarding (a) possible transmission routes, (b) most crucial transmission route, and (c) highly efficient personal protective measures for COVID-19 prevention and control (respondents could select no more than 3 options from the 8 listed personal protective measures). Detailed data are presented in Tables S3 and S4.
Most students (60.7%) believed that large droplet transmission was the most important SARS-CoV-2 transmission route, followed by short-range airborne (30.7%) and short-range fomite transmission (3.4%) (Fig. 2b). Only 1.0% of the students believed that the long-range airborne transmission route was most important.
Most students (89.8%) considered wearing surgical masks to be an efficient personal protective measure against COVID-19, followed by maintaining social distancing (53.0%), hand washing (50.1%), and vaccination (45.6%) (Fig. 2c and Table S5). Only 18.5% of students believed indoor ventilation to be the most efficient personal protective measure. Surface disinfection was considered the least important protective measure. More female students (vs. male students) believed surgical mask wearing (92.2% vs. 87.4%) and hand washing (53.8% vs. 46.4%) to be among the most efficient personal measures, whereas more male students believed indoor ventilation to be effective. More postgraduates (vs. undergraduates) believed surgical masks (91.9% vs. 87.8%) and indoor ventilation (19.9% vs. 17.1%) to be very efficient.
As shown in Table 5 , 94.4% of the students believed that the vaccine is effective or highly effective. Confident and vaccinated students were more likely than diffident and non-vaccinated students, respectively, to consider the vaccine highly effective and to express a stronger intention to be re-vaccinated after vaccine failure. Overall, 88.0% of the vaccinated students expressed an intention to be re-vaccinated after vaccine failure. Additionally, 58.8% of the students indicated that outbreaks in other cities would influence their personal protective behavior. Female and vaccinated students were more sensitive to the news of outbreaks in other cities than were male and non-vaccinated students, respectively. Gender and educational factors were not correlated with beliefs about vaccine efficacy or intention to be re-vaccinated after vaccine failure.
Table 5.
Personal beliefs related to COVID-19 by personal attribute.
| Personal attribute | Efficacy of vaccinea |
Injection again after vaccine failure |
Influenced by outbreak in other cities |
||
|---|---|---|---|---|---|
| Vaccinated | Not Vacb | Vaccinated | Vaccinated | Not Vac | |
| Total | 3.53 | 3.30 | 88.0% | 59.3% | 55.5% |
| Gender | p = 0.121 | p = 0.761 | p = 0.278 | p = 0.022 | p = 0.786 |
| Male | – | – | – | 57.2% | – |
| Female | – | – | – | 61.4% | – |
| Major | p < 0.001 | p = 0.116 | p = 0.899 | p = 0.348 | p = 0.041 |
| Engineering | 3.54 | – | – | – | 54.8% |
| Science | 3.41 | – | – | – | 67.3% |
| Medicine | 3.57 | – | – | – | 31.3% |
| Management | 3.61 | – | – | – | 42.9% |
| Confidence3 | p < 0.001 | p = 0.078 | p = 0.026 | p = 0.261 | p = 0.864 |
| Confident | 3.59 | – | 88.0% | – | – |
| Self-abased | 3.38 | – | 82.9% | – | – |
| Education | p = 0.130 | p = 0.535 | p = 0.858 | p = 0.105 | p = 0.292 |
A value of 5 indicates a belief that the vaccine is very highly effective, and a value of 1 indicates a belief that the vaccine is not effective.
Not Vac: Not vaccinated.
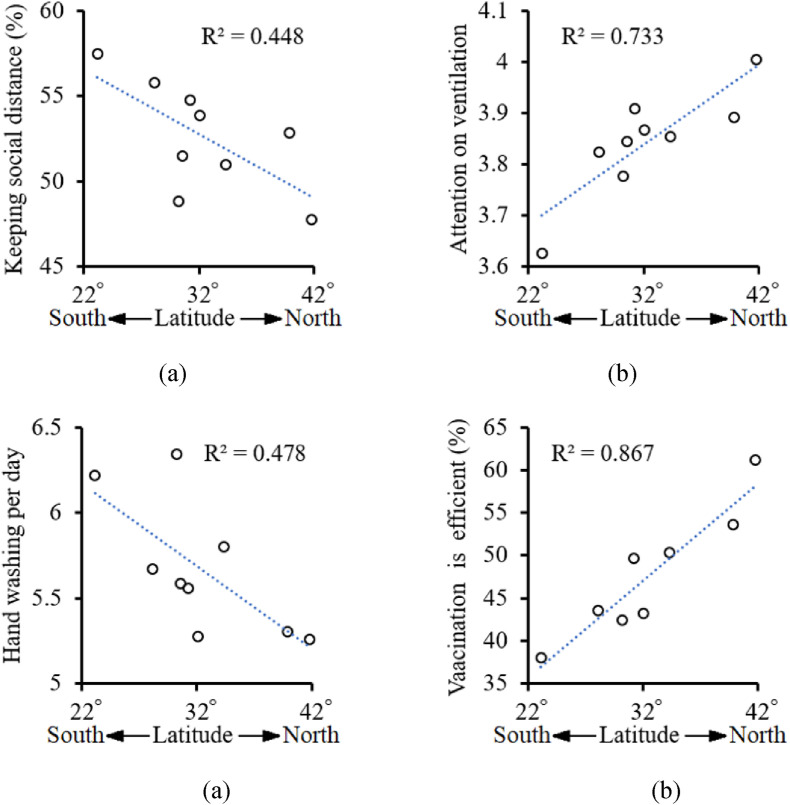
3.4. Effect of location on personal protective behavior
Interestingly, the students’ personal protection behavior was found to partially correlate with their location, especially with respect to latitude (Fig. 3 ). Students at universities in southern regions reported more frequent hand washing but paid less attention to indoor ventilation than their northern counterparts (Fig. 3a and b). Compared with students in northern regions, those in southern regions were also more likely to believe that maintaining social distancing is one of the most efficient COVID-19 prevention measures (Fig. 3c). However, students in northern regions were more likely than their southern counterparts to believe that vaccination is one of the most efficient measures for reducing infection risk (Fig. 3d). A data analysis revealed no significant correlations between location and other personal protective behaviors.
Fig. 3.
Effect of university location on (a) the frequency of hand washing (per day), (b) attention paid to indoor ventilation (high score indicates greater attention), (c) proportion of students who believe that maintaining social distancing is a very efficient preventive measure against COVID-19, and (d) proportion of students who believe that vaccination is a very efficient preventive measure.
3.5. Changes in personal protective behavior against COVID-19 after vaccination
As shown in Table 6 , students were 17.1% less likely to wash their hands but 14.1% and 35.5% more likely to disinfect their desk surfaces and indoor air, respectively, after vaccination. Fewer students wore masks in public areas, including classrooms, offices, libraries, canteens, shops, and crowded indoor environments, after vaccination, with an average rate of decrease in mask wearing of 22.0%. As the recent pandemic situation in China has not been very serious, students were increasingly likely to wear surgical masks rather than N95 respirators after vaccination. Glove wearing decreased by 40.2% after vaccination. Vaccination eased some students’ fears regarding COVID-19. Only 15.8% of the students expressed that they had no fear of being infected before vaccination, but this percentage doubled after vaccination.
Table 6.
Changes in personal protective behavior after vaccination.
| Personal protective behavior, n = 2829 | Before vaccination | After vaccination | p value | |
|---|---|---|---|---|
| Hand washing times per day | 5.67 | 5.36 | <0.001 | |
| Surface disinfection times per day | 1.42 | 1.62 | <0.001 | |
| Air disinfection times per day | 0.62 | 0.84 | <0.001 | |
| Attention to indoor ventilationa | 3.87 | 4.00 | <0.001 | |
| Mask wearing rates | Home | – | – | 0.889 |
| Dormitory | 3.1% | 4.0% | 0.009 | |
| Classroom | 28.0% | 17.6% | <0.001 | |
| Office | 17.3% | 13.6% | <0.001 | |
| Library | 38.4% | 28.1% | <0.001 | |
| Canteen | 30.3% | 21.3% | <0.001 | |
| Shop | 81.3% | 70.8% | <0.001 | |
| Gym | – | – | 0.889 | |
| Crowded indoor environments | 94.5% | 91.1% | <0.001 | |
| Rates of protective measures | Surgical masks | 90.9% | 92.8% | <0.001 |
| N95 respirators | 26.4% | 22.7% | <0.001 | |
| Face shields | – | – | 0.239 | |
| Protective clothing | 0.6% | 1.1% | 0.023 | |
| Goggles | – | – | 0.889 | |
| Gloves | 5.8% | 3.5% | <0.001 | |
| Fear of being infectedb | 3.29 | 3.76 | <0.001 | |
A value of 5 indicates a high level of attention paid to indoor ventilation, and a value of 1 indicates very little attention paid to indoor ventilation.
A value of 1 indicates that the respondent is very afraid of being infected with COVID-19, whereas a value of 5 indicates that the respondent had no fear of infection during the pandemic.
4. Discussion
In 2021, more than 50 million students attend universities and junior colleges in China [23]. As a vulnerable group in COVID-19 pandemic, university students should be given enough attention. Comparing to other cities, China conducted a stricter intervention at universities. Suspending classes and online education were conducted in China for a long time since the winter vacation in 2020 [24]. Students needed to provide negative nucleic acid results within 48 h before returning universities even almost no new cases were reported in China [25]. Diner divider, which could reduce the infection risk sometimes, was also installed in many Chinese universities [26].
University students followed the news and research findings in a timely manner and likely have more knowledge about COVID-19 than the general public. Close-contact transmission routes, including short-range airborne transmission, are considered the most important routes in SARS-CoV-2 transmission [[27], [28], [29]]. In our study, 97.0% and 89.3% of the students respectively believed that large droplet and short-range airborne transmission were possible SARS-CoV-2 transmission routes. Although some studies of indoor outbreaks have shown that long-range airborne transmission is a dominant route, especially in settings with poor ventilation [30,31], only 24.1% of the students believed that this was a possible route of SARS-CoV-2 transmission. The evidence has increasingly demonstrated that fomite transmission plays an insignificant role in the COVID-19 pandemic [32]; however, 50.9% and 36.0% of the students believed that SARS-CoV-2 could be transmitted via the short-range and long-range fomite routes, respectively. No evidence supports the transmission of SARS-CoV-2 via the mother–baby and mosquito routes; however, 22.4% and 15.4% of the students respectively believed that these are possible transmission routes. No gender differences emerged with respect to knowledge about possible transmission routes, consistent with the findings of studies in other countries [33]. Compared with male students, however, female students were more and less likely to believe that the large droplet and short-range airborne routes were the most important SARS-CoV-2 transmission routes.
Knowledge about COVID-19 is a direct determinant of personal protective behavior. As close contact is a dominant factor in SARS-CoV-2 transmission, more than 90% of the students wore surgical masks in crowded indoor environments (e.g., train stations), despite the lack of a serious pandemic situation in China at the time of the survey. Interestingly, 5.6% of the students wore gloves in crowded indoor environments, although one-third of students believed that long-range fomite transmission was possible. Epidemiological findings reported across different parts of the world indicated higher COVID-19-related morbidity and mortality in males than in females [34]. However, our study found that compared with male students, female students were more afraid of being infected but had a lower vaccination rate. Comparatively, female students also reported better personal hygiene habits (e.g., hand washing and surface disinfection) and more frequent mask wearing in unfamiliar indoor environments (e.g., shops and gyms) but less frequent mask wearing in familiar indoor settings (e.g., dormitories and offices). Studies in other countries have also shown that women reported higher levels of precautionary behavior and more negative emotional reactions toward COVID-19 [33,34]. To our knowledge, no other study has revealed differences between undergraduate and postgraduate students in terms of COVID-19 prevention and control behavior. We found that undergraduates were more afraid of being infected than were postgraduates. This may largely explain why only undergraduates were comparatively more likely to be vaccinated and to report better personal hygiene behavior (e.g., hand washing, surface and air disinfection, and mask wearing). In Hubei, although almost no cases were reported after May 2020, local university students had a very high vaccination rate, probably because they had experienced the most serious COVID-19 outbreak in China.
Besides the perceived severity of COVID-19 [35], vaccination efficacy is a key determinant of the vaccination rate in the absence of a mandatory policy. As of April 7, 2021, 5% of world population have received at least one dose of an approved vaccination [36]. Many vaccines (e.g. Pfizer–BioNTech, Moderna, and Sputnik V) were used in different areas globally, and most of them had an efficacy more than 90%, however, there was no reported data on vaccine efficacy on Sinopharm and Sinovac [37], which were commonly used in China. From the local reports of China, Sinopharm had an efficacy of 86% and Sinovac had an efficacy from 50.4% to 83.5% [38,39]. Vaccination can reduce the duration of physical distancing by 36%–78% [40]. In our study, 94.4% of Chinese university students believed that the vaccine is effective or highly effective; furthermore, 86% of the vaccinated students expressed an intent to accept re-vaccination after vaccine failure, which is much higher than the average values of 78.9% in China [41] and 72.2% in America [42]. Vaccination may be not effective for variant virus (e.g. delta), but non-pharmaceutical interventions such as surgical mask wearing and social distancing would be effective no matter what variant virus is. Our study found that university students who participated in our survey believed that surgical mask wearing, maintaining social distancing, and hand washing were more efficient than vaccination in terms of reducing the COVID-19 infection risk, suggesting that students did not believe that the vaccine was effective. The non-pharmaceutical interventions (e.g. mask wearing and social distancing) was still mandatory in many public indoor environments, and it may weaken the intention to be vaccinated again after vaccine failure. Recently, some SARS-CoV-2 variants (e.g., alpha and delta) have emerged and spread rapidly, and these variants have become the main sources of COVID-19 infection in many countries (e.g., India) [43]. If vaccination leads students to reduce their protective behavior, new waves of infection could emerge because the vaccines may be less effective against future variant viruses [16].
The participating students reported that they were less likely to wear masks in familiar indoor environments (e.g., dormitories, offices, and libraries) than in public areas, such as shopping malls and airports. However, people have higher rates of close contacts in familiar indoor environments [44] and maintain shorter interpersonal distances during close contact with acquaintances [45,46]. Studies have shown that the average interpersonal distance between postgraduates during close contact in office settings is 0.8 m, a much shorter distance than that observed in non-familiar indoor environments [46,47]. Furthermore, more than 70% of COVID-19 infections in China were transmitted within families [48,49]. Therefore, universities should strengthen personal protective measures in dormitories, classrooms, and offices to reduce the infection risk during the COVID-19 pandemic. Universities should also strengthen efforts to disseminate COVID-19 prevention and control information, as one-seventh of the students who responded to our survey were unaware of their universities’ guidelines.
Interestingly, we found that a student's major affected their personal protective behavior during the pandemic, possibly due to subject-related differences in the scope of knowledge. In general, students in medicine had the lowest level of fear of being infected and the highest mask wearing rate. In contrast, students in management had the highest level of fear of being infected but the worst personal hygiene habits and lowest mask wearing and vaccination rates. Therefore, we conclude that students who better understand the mechanism of SARS-CoV-2 transmission are less afraid of being infected and maintain better personal protective behavior.
Personality is another key determinant of students’ personal protective behavior during the COVID-19 pandemic. Neuroticism was found to have a negative impact on COVID-19 infection spread [50]. In our study, approximately half of the students were found to be confident, whereas only 8.7% were diffident. Compared with their diffident peers, confident students reported significantly higher frequencies of hand washing and surface and air disinfection, paid more attention to indoor ventilation, and more frequently wore masks in all types of indoor environments. However, we did not find a significant difference in the vaccination rate between confident and diffident students.
Additionally, location was found to be correlated with some aspects of personal protective behavior. Indoor CO2 concentrations are usually higher in Northern China than in Southern China [51], and students at northern universities paid more attention to indoor ventilation; this may have reduced the risk of airborne transmission. In contrast, as a warm, humid climate is associated with a high risk of infectious disease transmission via the fomite route (e.g., norovirus) [52], students at southern universities washed their hands significantly more frequently than did students at northern universities. Because no warm water is offered in most Chinese universities, temperature of tap water may directly determine the frequency on hand washing. The fact that the tap water temperature in southern China is lower than it in northern China, especially in winter, may lead to low frequency on hand washing of students in southern universities. It remains unclear why students at southern universities were less likely than their northern counterparts to consider maintaining social distancing an efficient COVID-19 prevention measure.
The most important finding of the study is less Chinese university students wore masks in public indoor environments after vaccination. The wearing rate was reduced by 22%. The mask wearing rate is reduced in almost all indoor spaces, such as classrooms, officers, libraries, canteens and shops (Table 6). N95 respirator had a higher efficacy (67%–89%) on infection risk reduction than surgical mask (around 50%) [17,53], however, wearing a N95 respirator is much more unconformable. We found that the use rate of N95 respirator was also reduced by 14.0% due to the vaccination. This significant relaxation in personal protection behavior may bring a serious potential risk for following waves of variant virus (e.g. delta). Our survey was performed on June 30, 2021, happened to be just before a new wave of infection of COVID-19 in China, which possibly started from infected airport cleaners after cleaning a Russian flight cabin on July 10, 2021 [54]. Since February 2021, the local transmission of COVID-19 had been mostly well controlled in the country (Fig. S4). Since July 20, 2021, the infection has spread to more than a dozen of provinces, regions and municipalities [55,56]. China had largely managed to keep imported infections from causing major local outbreaks since the country successfully controlled the domestic spread of SARS-CoV-2 during the first phase of the pandemic. Our new survey data revealed that Chinese university students are still on high alert and largely retain their personal protective behavior, similar to elsewhere [57], however, there is also a significant relaxation after vaccination. There is no existing data to show if such observed behavior relaxation after vaccination also exists in other parts of the community, but the common sense tells us that it is very likely so. Such relaxation at community level would possibly provide loopholes for causing the virus transmission as demonstrated in the recent new surge of infection from Nanjing to elsewhere in China [56].
This study has some limitations. Our survey on human behavior could have been affected by response bias because we relied on self-reported data. Most undergraduate and postgraduate (69.4%) students had majors in engineering; therefore, our sample may not be representative of all Chinese university students. Changes in behavior after vaccination may also have been influenced by changes in the pandemic situation, which could have led to error. Although we filtered the submitted questionnaires by several judgements, the quality of the answer may also lead bias of the survey. Some reasonings in the study was based on our understanding, which may be not the real reason.
Students are one of the most important population group in SARS-CoV-2 transmission globally. In the future, changes on personal protective behavior by other population groups such as healthcare workers and retired old people could be studied. Moreover, the pandemic fatigue on personal protective behavior during continuing COVID-19 waves is also critical for SARS-CoV-2 transmission in the future.
5. Conclusions
In China, as of the June 30, 2021, 87.6% of university students had been vaccinated. They believed that the large droplet and short-range airborne routes were the two most likely SARS-CoV-2 transmission routes. University students weakened their personal protective behavior after vaccination. It may bring a high potential risk for following waves of variant virus (e.g. delta). Female and confident students had better personal hygiene habit than male and diffident students.
Practical implications
University student is considered as a vulnerable group in the COVID-19 pandemic due to their frequent close contacts, ability to transmit infections carried from their homes, and potential risk of mental health problems. Based on more than 3200 questionnaires on personal protective behaviors before and after vaccination, we found that Chinese university students weakened their personal protective behavior after vaccination and it may bring a high potential risk for following waves of variant virus (e.g. delta). The results provide a solid support on COVID-19 prevention and control in universities.
Author's contributions
NZ, JX, YL conceived the idea. NZ, XL, TJ, and DM collected the data. NZ, XL, HL, PZ, and BS analyzed the data. NZ and XL prepared the figures. NZ and YL wrote the paper. NZ, PX, JX, and YL made constructive amendments. All authors reviewed the paper.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We are grateful to the professors who disseminated the online questionnaire to their students in several WeChat Groups. This project was partially supported by a GRF grant (no. 17202719) from the Hong Kong Research Grants Council.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.buildenv.2021.108367.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.US CDC Scientific brief: SARS-CoV-2 transmission. 2021. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html Available from: accessed.
- 2.US CDC Science brief: SARS-CoV-2 and surface (fomite) transmission for indoor community environments. 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/surface-transmission.html Available from: accessed. [PubMed]
- 3.Wise T., Zbozinek T.D., Michelini G., et al. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. Roy. Soc. Open Sci. 2020;7:200742. doi: 10.1098/rsos.200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu X., Chew K.A., Xu X., et al. Demographic and social correlates and indicators for behavioural compliance with personal protection among Chinese community-dwellers during COVID-19: a cross-sectional study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-041453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US CDC Interim public health recommendations for fully vaccinated people. 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html Available from: accessed. [DOI] [PubMed]
- 6.Bernal J.L., Andrews N., Gower C., et al. Effectiveness of covid-19 vaccines against the B.1.617.2 (delta) variant. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2108891. [DOI] [PubMed] [Google Scholar]
- 7.Aleta A., Martin-Corral D., Piontti A.P. y, et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020;4:964–971. doi: 10.1038/s41562-020-0931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nixon E., Trickey A., Christensen H., et al. Contacts and behaviours of university students during the COVID-19 pandemic at the start of the 2020/2021 academic year. Sci. Rep. 2021;11:11728. doi: 10.1038/s41598-021-91156-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., et al. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatr. Res. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nurunnabi M., Almusharraf N. Social distancing and reopening universities after the COVID-19 pandemic: policy complexity in G20 countries. J. Public Health Res. 2020;9:1957. doi: 10.4081/jphr.2020.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kostic J., Zikic O., Dordevic V., et al. Perceived stress among university students in south-east Serbia during the COVID-19 outbreak. Ann. Gen. Psychiatr. 2021;20:25. doi: 10.1186/s12991-021-00346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamey G., Walensky R.P. Covid-19: re-opening universities is high risk (the key is to curb community transmission then provide frequent testing) BMJ. 2020;370:m3365. doi: 10.1136/bmj.m3365. [DOI] [PubMed] [Google Scholar]
- 13.Lewis M., Sanchez R., Auerbach S., et al. COVID-19 Outbreak among college students after a spring break trip to Mexico - austin, Texas, March 26-April 5, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:830–835. doi: 10.15585/mmwr.mm6926e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iacobucci G. Covid-19: universities may need to test students every three days to prevent major outbreaks, say researchers. BMJ. 2021;372:n618. doi: 10.1136/bmj.n618. [DOI] [PubMed] [Google Scholar]
- 15.Barello S., Nania T., Dellafiore F., et al. Vaccine hesitancy among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020;35:781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahase E. Delta variant: what is happening with transmission, hospital admissions, and restrictions? BMJ. 2021;373:n1513. doi: 10.1136/bmj.n1513. [DOI] [PubMed] [Google Scholar]
- 17.Sickbert-Bennett E.E., Samet J.M., Clapp P.W., et al. Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Intern. Med. 2020;180:1607–1612. doi: 10.1001/jamainternmed.2020.4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y., Tian H., Zhang L., et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qin J., Xing Y., Ren J., et al. Mandatory mask-wearing and hand hygiene associated with decreased infectious diseases among patients undergoing regular hemodialysis: a historical-control study. Front. Public Health. 2021;9:678738. doi: 10.3389/fpubh.2021.678738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lao C.K., Li X., Zhao N., et al. Using the health action process approach to predict facemask use and hand washing in the early stages of the COVID-19 pandemic in China. Curr. Psychol. 2021 doi: 10.1007/s12144-021-01985-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang J.W., Marr L.C., Li Y., et al. Covid-19 has redefined airborne transmission Improving indoor ventilation and air quality will help us all to stay safe. BMJ. 2021;372:n913. doi: 10.1136/bmj.n913. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein N.D. Unrealistic optimism about future life events. J. Pers. Soc. Psychol. 1980;39:806–820. [Google Scholar]
- 23.NBS (National Bureau of Statistics) Number of students in various academic education at all levels. 2020. https://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0M0201&sj=2020 Available from: accessed.
- 24.Zhang W., Wang Y., Yang L., et al. Suspending classes without stopping learning: China's education emergency management policy in the COVID-19 outbreak. J. Risk Financ. Manag. 2020;13:1–6. [Google Scholar]
- 25.Fan C., Li M., Li X., et al. Who got infected with COVID-19? A study of college students in wuhan (China) Int. J. Environ. Res. Publ. Health. 2021;18:2420. doi: 10.3390/ijerph18052420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu Z., Li R., Wu Y., et al. Numerical study on the effect of diner divider on the airborne transmission of diseases in canteens. Energy Build. 2021;248:111171. [Google Scholar]
- 27.Cheng C.H., Chow C.L., Chow H.K. Trajectories of large respiratory droplets in indoor environment: a simplified approach. Build. Environ. 2020;183:107196. doi: 10.1016/j.buildenv.2020.107196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li Y. Hypothesis: SARS-CoV-2 transmission is predominated by the short-range airborne route and exacerbated by poor ventilation. Indoor Air. 2021;31:921–925. doi: 10.1111/ina.12837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang N., Chan P.T.J., Jia W., et al. Analysis of efficacy of intervention strategies for COVID-19 transmission: a case study of Hong Kong. Environ. Int. 2021;156:106723. doi: 10.1016/j.envint.2021.106723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Qian H., Hang J., et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build. Environ. 2021;196:107788. doi: 10.1016/j.buildenv.2021.107788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang N., Chen X., Jiang W., et al. Evidence for lack of transmission by close contact and surface touch in a restaurant outbreak of COVID-19. J. Infect. 2021;83:207–216. doi: 10.1016/j.jinf.2021.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mondelli M.U., Colaneri M., Seminari E.M., et al. Low risk of SARS-CoV-2 transmission by fomites in real-life conditions. Lancet Infect. Dis. 2021;21:e112. doi: 10.1016/S1473-3099(20)30678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levkovich I., Shinan-Altman S. The impact of gender on emotional reactions, perceived susceptibility and perceived knowledge about COVID-19 among the Israeli public. Int. Health. 2021 doi: 10.1093/inthealth/ihaa101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bwire G.M. Coronavirus: Why men are more vulnerable to Covid-19 than women? SN Compr. Clin. Med. 2020 doi: 10.1007/s42399-020-00341-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang P.W., Ahorsu D.K., Lin C.Y., et al. Motivation to have COVID-19 vaccination explained using an extended protection motivation theory among university students in China: the role of information sources. Vac. 2021;9:380. doi: 10.3390/vaccines9040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mathieu E., Ritchie H., Ortiz-Ospina E., et al. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021;5:947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 37.Doroftei B., Ciobica A., Ilie O.D., et al. Mini-Review discussing the reliability and efficiency of COVID-19 vaccines. Diagnostics. 2021;11:579. doi: 10.3390/diagnostics11040579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin L. Comparison of five vaccines with published efficacy data. 2020. https://baijiahao.baidu.com/s?id=1686575364788125990&wfr=spider&for=pc Available from. accessed.
- 39.Huanqiu Why is there a big difference in phase three of Sinovac vaccine? 2021. https://baijiahao.baidu.com/s?id=1693342268153415934&wfr=spider&for=pc Available from. accessed.
- 40.Huang B., Wang J., Cai J., et al. Integrated vaccination and physical distancing interventions to prevent future COVID-19 waves in Chinese cities. Nat. Hum. Behav. 2021;5:695–705. doi: 10.1038/s41562-021-01063-2. [DOI] [PubMed] [Google Scholar]
- 41.Mo P.K.H., Luo S.T., Wang S.H., et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vac. 2021;9:129. doi: 10.3390/vaccines9020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu T., He Z., Huang J., et al. A comparison of vaccine hesitancy of COVID-19 vaccination in China and the United States. Vac. 2021 doi: 10.3390/vaccines9060649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iacobucci G. Covid-19: single vaccine dose is 33% effective against variant from India, data show. BMJ. 2021;373:n1346. doi: 10.1136/bmj.n1346. [DOI] [PubMed] [Google Scholar]
- 44.Zhang N., Jia W., Lei H., et al. Effects of human behavior changes during the COVID-19 pandemic on influenza spread in Hong Kong. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heshka S., Nelson Y. Interpersonal speaking distance as a function of age, sex, and relationship. Sociometry. 1972;35:491–498. [Google Scholar]
- 46.Zhang N., Chen W., Chan P., et al. Close contact behavior in indoor environment and transmission of respiratory infection. Indoor Air. 2020;30:645–661. doi: 10.1111/ina.12673. [DOI] [PubMed] [Google Scholar]
- 47.Zhang N., Su B., Chan P., et al. Infection spread and high-resolution detection of close contact behaviors. Int. J. Environ. Res. Publ. Health. 2020;17:1445. doi: 10.3390/ijerph17041445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lei H., Xu X., Xiao S., et al. Household transmission of COVID-19-a systematic review and meta-analysis. J. Infect. 2020;81:993–995. doi: 10.1016/j.jinf.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang N., Cheng P., Jia W., et al. Impact of intervention methods on COVID-19 transmission in Shenzhen. Build. Environ. 2020;180:107106. doi: 10.1016/j.buildenv.2020.107106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gori A., Topino E., Palazzeschi L., et al. Which personality traits can mitigate the impact of the pandemic? Assessment of the relationship between personality traits and traumatic events in the COVID-19 pandemic as mediated by defense mechanisms. PloS One. 2021;16 doi: 10.1371/journal.pone.0251984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu J., Dai X., Li X., et al. Indoor air quality and occupants' ventilation habits in China: seasonal measurement and long-term monitoring. Build. Environ. 2018;142:119–129. [Google Scholar]
- 52.Lu J., Fang L., Sun L., et al. Association of GII. P16-GII. 2 Recombinant norovirus strain with increased norovirus outbreaks, Guangdong, China, 2016. Emerg. Infect. Dis. 2017;23:1188–1190. doi: 10.3201/eid2307.170333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ballard D.H., Dang A.J., Kumfer B.M., et al. Protection levels of N95-level respirator substitutes proposed during the COVID-19 pandemic: safety concerns and quantitative evaluation procedures. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-045557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cang W. Nanjing explains how virus was transmitted. China Dail. 30 July 2021 https://www.chinadaily.com.cn/a/202107/30/WS61039ae0a310efa1bd6658be.html Last accessed. [Google Scholar]
- 55.Wong T. China: how Delta threatens a prized zero Covid strategy. 2021. https://www.bbc.com/news/world-asia-china-58095909 6 August 2021. Last accessed.
- 56.Liu R., Woo R. China reports most new COVID-19 cases since January amid Delta surge. Reuters. August 4 2021 https://www.reuters.com/world/china/china-reports-96-new-coronavirus-cases-aug-3-vs-90-day-ago-2021-08-04/ Last accessed. [Google Scholar]
- 57.Reicher S., Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. BMJ. 2021;372:n137. doi: 10.1136/bmj.n137. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.