Abstract
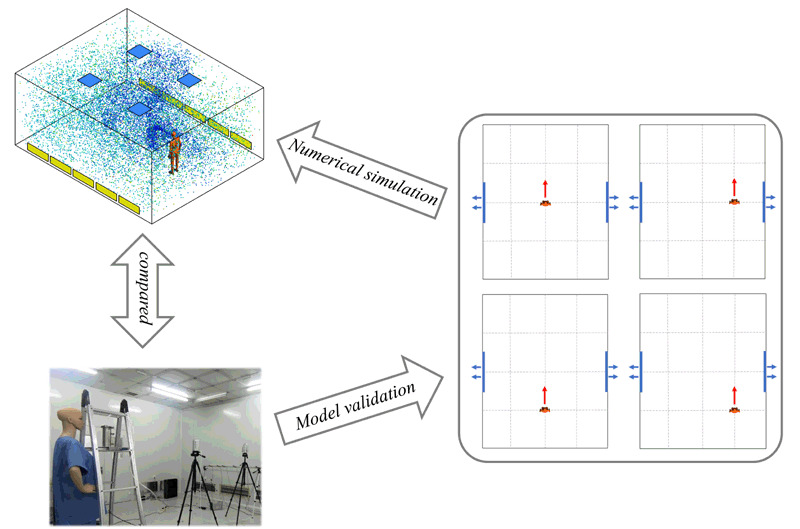
Respiratory viruses can be attached to human exhaled particles and spread from person to person through respiratory activities. The purpose of this study is to obtain the quantitative description formula of human exhaled particles in the ventilated room through amount number of numerical simulation calculations and regression statistical analysis of the simulated data. In this study, a combination of numerical simulation and laboratory experiments was used, and the results were tallied preferably. Bacillus subtilis was released as a release source to investigate the migration and distribution of bioaerosol. The results show that under the condition of high air supply velocity, due to the disturbance of human respiration and airflow, the diffusion velocity of exhaled particles was faster and the diffusion range is larger than that of low air supply velocity within the same time frame. No matter where the location of the manikin was in the room, the exhaled particles would spread to the whole room in at least 900 s. The method used in this study could be used to predict the distribution of human exhaled particles concentration in different indoor spaces, such as public transport and hospitals. These findings could provide valuable reference for the location of indoor air purifiers, which plays a guiding role in the construction of a healthy indoor environment.
Keywords: droplet aerosols, particulate concentrations, bioaerosol release experiment, CFD predictions
Acknowledgements
This work was supported by the National Key R&D Program of China (No. 2019YFC1520700), the National Natural Science Foundation of China (No. 41977368), the National Science and Technology Ministry of China (No. 2017YFC0702800), Opening Funds of State Key Laboratory of Building Safety and Built Environment National Engineering Research Center of Building Technology (No. BSBE2017-08).
References
- Bourouiba L, Dehandschoewercker E, Bush JWM. Violent expiratory events: On coughing and sneezing. Journal of Fluid Mechanics. 2014;745:537–563. doi: 10.1017/jfm.2014.88. [DOI] [Google Scholar]
- Chang TJ, Hu TS. Transport mechanisms of airborne particulate matters in partitioned indoor environment. Building and Environment. 2008;43:886–895. doi: 10.1016/j.buildenv.2007.01.030. [DOI] [Google Scholar]
- Chen C, Zhao B. Some questions on dispersion of human exhaled droplets in ventilation room: answers from numerical investigation. Indoor Air. 2010;20:95–111. doi: 10.1111/j.1600-0668.2009.00626.x. [DOI] [PubMed] [Google Scholar]
- Chen C, Yao M, Luo X, et al. Outdoor-to-indoor transport of ultrafine particles: Measurement and model development of infiltration factor. Environmental Pollution. 2020;267:115402. doi: 10.1016/j.envpol.2020.115402. [DOI] [PubMed] [Google Scholar]
- Chow TT, Yang XY. Performance of ventilation system in a non-standard operating room. Building and Environment. 2003;38:1401–1411. doi: 10.1016/S0360-1323(03)00155-0. [DOI] [Google Scholar]
- Chow TT, Lin Z, Bai W. The integrated effect of medical lamp position and diffuser discharge velocity on ultra-clean ventilation performance in an operating theatre. Indoor and Built Environment. 2006;15:315–331. doi: 10.1177/1420326X06067802. [DOI] [Google Scholar]
- Chow TT, Wang J. Dynamic simulation on impact of surgeon bending movement on bacteria-carrying particles distribution in operating theatre. Building and Environment. 2012;57:68–80. doi: 10.1016/j.buildenv.2012.04.010. [DOI] [Google Scholar]
- Dong S, Liu Y, Zhang N, et al. Theoretical study of thermophoretic impulsive force exerted on a particle in fluid. Journal of Molecular Liquids. 2017;241:99–101. doi: 10.1016/j.molliq.2017.06.007. [DOI] [Google Scholar]
- Elghobashi S. Particle-laden turbulent flows: direct simulation and closure models. Applied Scientific Research. 1991;48:301–314. doi: 10.1007/BF02008202. [DOI] [Google Scholar]
- Ge X-Y, Pu Y, Liao C-H, et al. Evaluation of the exposure risk of SARS-CoV-2 in different hospital environment. Sustainable Cities and Society. 2020;61:102413. doi: 10.1016/j.scs.2020.102413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K, Qian H, Zhao D, et al. Indoor exposure levels of bacteria and fungi in residences, schools, and offices in China: A systematic review. Indoor Air. 2020;30:1147–1165. doi: 10.1111/ina.12734. [DOI] [PubMed] [Google Scholar]
- He Q, Niu J, Gao N, et al. CFD study of exhaled droplet transmission between occupants under different ventilation strategies in a typical office room. Building and Environment. 2011;46:397–408. doi: 10.1016/j.buildenv.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. New York: John Wiley & Sons; 1999. [Google Scholar]
- Jo WK, Seo YJ. Indoor and outdoor bioaerosol levels at recreation facilities, elementary schools, and homes. Chemosphere. 2005;61:1570–1579. doi: 10.1016/j.chemosphere.2005.04.103. [DOI] [PubMed] [Google Scholar]
- Jurelionis A, Gagytė L, Prasauskas T, et al. The impact of the air distribution method in ventilated rooms on the aerosol particle dispersion and removal: The experimental approach. Energy and Buildings. 2015;86:305–313. doi: 10.1016/j.enbuild.2014.10.014. [DOI] [Google Scholar]
- Kalogerakis N, Paschali D, Lekaditis V, et al. Indoor air quality—Bioaerosol measurements in domestic and office premises. Journal of Aerosol Science. 2005;36:751–761. doi: 10.1016/j.jaerosci.2005.02.004. [DOI] [Google Scholar]
- Kang Z, Zhang Y, Fan H, et al. Numerical simulation of coughed droplets in the air-conditioning room. Procedia Engineering. 2015;121:114–121. doi: 10.1016/j.proeng.2015.08.1031. [DOI] [Google Scholar]
- Kim J-G, Kim A-H, Kim J-S. Assessment of bioaerosols in public restrooms. Korean Journal of Environmental Health Sciences. 2014;40:304–312. doi: 10.5668/JEHS.2014.40.4.304. [DOI] [Google Scholar]
- Lednicky JA, Lauzardo M, Fan ZH, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. International Journal of Infectious Diseases. 2020;100:476–482. doi: 10.1016/j.ijid.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KW, Liu BYH. Theoretical study of aerosol filtration by fibrous filters. Aerosol Science and Technology. 1982;1:147–161. doi: 10.1080/02786828208958584. [DOI] [Google Scholar]
- Lee BU, Hong IG, Lee DH, et al. Bacterial bioaerosol concentrations in public restroom environments. Aerosol and Air Quality Research. 2012;12:251–255. doi: 10.4209/aaqr.2011.07.0097. [DOI] [Google Scholar]
- Lindsley WG, Noti JD, Blachere FM, et al. Viable influenza A virus in airborne particles from human coughs. Journal of Occupational and Environmental Hygiene. 2015;12:107–113. doi: 10.1080/15459624.2014.973113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lis DO, Pastuszka JS. Bacterial and fungal aerosol in homes without and with mold problem, in Upper Silesia, Poland. Preliminary results. Journal of Aerosol Science. 1997;28:S665–S666. doi: 10.1016/S0021-8502(97)85332-3. [DOI] [Google Scholar]
- Liu W, Liu D, Gao N. CFD study on gaseous pollutant transmission characteristics under different ventilation strategies in a typical chemical laboratory. Building and Environment. 2017;126:238–251. doi: 10.1016/j.buildenv.2017.09.033. [DOI] [Google Scholar]
- Morawska L, Johnson GR, Ristovski ZD, et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. Journal of Aerosol Science. 2009;40:256–269. doi: 10.1016/j.jaerosci.2008.11.002. [DOI] [Google Scholar]
- Patankar SV, Spalding DB. A finite-difference procedure for solving the equations of the two-dimensional boundary layer. International Journal of Heat and Mass Transfer. 1967;10:1389–1411. doi: 10.1016/0017-9310(67)90028-2. [DOI] [Google Scholar]
- Romano F, Marocco L, Gustén J, et al. Numerical and experimental analysis of airborne particles control in an operating theater. Building and Environment. 2015;89:369–379. doi: 10.1016/j.buildenv.2015.03.003. [DOI] [Google Scholar]
- Sadrizadeh S, Tammelin A, Ekolind P, et al. Influence of staff number and internal constellation on surgical site infection in an operating room. Particuology. 2014;13:42–51. doi: 10.1016/j.partic.2013.10.006. [DOI] [Google Scholar]
- Sassi HP, Reynolds KA, Pepper IL, et al. Evaluation of hospital-grade disinfectants on viral deposition on surfaces after toilet flushing. American Journal of Infection Control. 2018;46:507–511. doi: 10.1016/j.ajic.2017.11.005. [DOI] [PubMed] [Google Scholar]
- Srebric J, Vukovic V, He G, et al. CFD boundary conditions for contaminant dispersion, heat transfer and airflow simulations around human occupants in indoor environments. Building and Environment. 2008;43:294–303. doi: 10.1016/j.buildenv.2006.03.023. [DOI] [Google Scholar]
- Wang C, Holmberg S, Sadrizadeh S. Numerical study of temperature-controlled airflow in comparison with turbulent mixing and laminar airflow for operating room ventilation. Building and Environment. 2018;144:45–56. doi: 10.1016/j.buildenv.2018.08.010. [DOI] [Google Scholar]
- Wang C, Holmberg S, Sadrizadeh S. Impact of door opening on the risk of surgical site infections in an operating room with mixing ventilation. Indoor and Built Environment. 2021;30:166–179. doi: 10.1177/1420326X19888276. [DOI] [Google Scholar]
- Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X, Li Y, Chwang ATY, et al. How far droplets can move in indoor environments—Revisiting the Wells evaporation-falling curve. Indoor Air. 2007;17:211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- Yan Y, Li X, Shang Y, et al. Evaluation of airborne disease infection risks in an airliner cabin using the Lagrangian-based Wells-Riley approach. Building and Environment. 2017;121:79–92. doi: 10.1016/j.buildenv.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao M, Zhang L, Ma J, et al. On airborne transmission and control of SARS-Cov-2. Science of the Total Environment. 2020;731:139178. doi: 10.1016/j.scitotenv.2020.139178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Chen Q. Prediction of particle deposition onto indoor surfaces by CFD with a modified Lagrangian method. Atmospheric Environment. 2009;43:319–328. doi: 10.1016/j.atmosenv.2008.09.041. [DOI] [Google Scholar]
- Zhang Y, Feng G, Kang Z, et al. Numerical simulation of coughed droplets in conference room. Procedia Engineering. 2017;205:302–308. doi: 10.1016/j.proeng.2017.09.981. [DOI] [Google Scholar]
- Zhao B, Yang C, Yang X, et al. Particle dispersion and deposition in ventilated rooms: Testing and evaluation of different Eulerian and Lagrangian models. Building and Environment. 2008;43:388–397. doi: 10.1016/j.buildenv.2007.01.005. [DOI] [Google Scholar]
- Zukowska D, Melikov A, Popiolek Z. Impact of personal factors and furniture arrangement on the thermal plume above a sitting occupant. Building and Environment. 2012;49:104–116. doi: 10.1016/j.buildenv.2011.09.015. [DOI] [Google Scholar]


