Abstract
Background:
Year 2020 started with global health crisis known as COVID-19. In lack of established tools and management protocols, COVID-19 had become breeding ground for fear and confusion, leading to stigma toward affected individuals.
Method:
A cross-sectional study was conducted to estimate prevalence of stigma in discharged COVID-19 patients from a COVID hospital in India. Participants were approached telephonically using a semistructured questionnaire to record their experiences. Questions were asked regarding stigma at six major domains of daily life. Among total 1,673 discharged participants, 600 were conveniently selected and out of them 311 responded on telephonic interviews.
Result:
We found that 182 (58.52%) participants (95% CI: 53.04–64.00) have self-perceived stigma, 163 (52.41%) participants (95% CI: 46.86–57.96) experienced quarantine-related stigma, 222 (71.38%) participants (95% CI: 66.36–76.40) experienced neighborhood stigma, 214 (68.81%) participants (95% CI: 63.66–73.95) experienced stigma while going out in marketplaces, 180 (57.88%) participants (95% CI: 52.39–63.37) experienced stigma at their work place, and 207 (66.56%) participants (95% CI: 61.31–71.80) reported stigma experienced by their family members. With a total of 84.5% (95% CI: 80.06–88.39) participants experiencing stigma at some domain and about 42.8% of participants facing stigma at all six domains. The commonest noted cause of stigma was fear of getting infected, reported by 184 (59.2%) participants.
Conclusion:
This study shows high prevalence of stigma in COVID-19 patients suffering in their common domains of daily lives.
Keywords: COVID-19, discrimination, India, psychosocial, stigma
Key Messages:
COVID-19 patients suffer stigma in their day to day lives. Stigma varies depending upon the sociodemographic profile of patient. Stigma brings upon stress and affects quality of life.
Stigma is an ancient Greek term denoting a mark made to brand a person a traitor, criminal, or slave.1 Throughout history, epidemics have been associated with stigma and social discrimination toward the infected individuals. During historical outbreaks of tuberculosis,2 and more recently Influenza, Ebola, Zika, and SARS,3,4 infected individuals have suffered stereotyping, discrimination, separation, and loss of status.5 Such discrimination negatively impacts illness outcomes.6 Stigma is experienced by not only the patient but also the caregivers and family members, increasing psychosocial burden and subsequently increases morbidity.7
COVID-19 is a highly contagious disease that has already affected tens of millions of people worldwide, with devastating health and societal impact, including stigmatization of its victims. The experiences of stigma in COVID-19 patients vary widely among people and communities, based on social, cultural, economic, and political contexts.8 The fear and confusion associated with the COVID-19 pandemic has fostered stigma toward the infected individuals and caregivers and has been described as occurring in communities in Italy, Spain, and the United Kingdom during recent out breaks.9
Stigma can be divided into two sections: internal stigma, that is, self-perceived stigma, and external stigma. External stigma can be subdivided into (a) stigma due to affiliated entity, that is, family, friends, and associated acquaintances; and (b) stigma due to public entity, that is, stigma experienced at various domains of public life such as marketplace and work.10 Even before COVID-19, caring for patients and families in India has been challenged by both cultural traditions such as caste and modern challenges such as unemployment or poverty that may be perceived as stigmatizing.
Recently, Indian media have reported various scattered incidents of social discrimination among COVID-19 patients. During routine telephonic follow-up conversations conducted with discharged COVID-19 patients, we at National Cancer Institute, Jhajjar, AIIMS, New Delhi, noted a striking finding of patients reporting stigma in their day-to-day lives. There has been no study available to provide insight into the prevalence, burden, or impact of stigma among Indian COVID-19 patients. Hence, we designed a study to estimate the prevalence of stigma in COVID-19 patients and explore its associations with various sociodemographic determinants.
Materials and Methods
Study design. A cross-sectional, observational study was designed at a tertiary care center catering exclusively to COVID-19 patients, to assess the prevalence of stigma and its demographic associations among discharged COVID-19 patients.
Participants. As part of routine care, all individuals discharged from the hospital were contacted telephonically after two weeks of discharge. They were informed about the survey, and those willing to participate were enrolled in our study. Sociodemographic profile of participants is depicted in Table 1.
Table 1.
The Demographic Profile of all Participants (N = 311)
| Baseline Demographic Details | Number of Participants |
| Sex | |
| Male | 246 |
| Female | 62 |
| Others* | 3 |
| Age (years) | |
| ≤15 | 4 |
| 16–30 | 129 |
| 31–45 | 107 |
| 46–60 | 53 |
| >60 | 18 |
| Education | |
| Illiterateα | 4 |
| Up to 5th class | 13 |
| 5th–10th class | 51 |
| 11th–12th class | 82 |
| Graduate | 144 |
| Postgraduate | 17 |
| Occupation | |
| Unemployedβ | 37 |
| Student | 23 |
| Self-employed | 91 |
| Private employee | 83 |
| Government employee | 49 |
| Defense/police/security | 28 |
| Family income (INRδ per month) | |
| Up to 5,000 | 14 |
| 5,000–10,000 | 31 |
| 10,000–20,000 | 83 |
| 20,000–30,000 | 92 |
| 30,000–50,000 | 64 |
| >50,000 | 27 |
| Religion | |
| Hindu | 240 |
| Muslim | 65 |
| Others | 6 |
| Residence/society | |
| Slums: daily wagers/labors/vendors | 92 |
| Private colonies | 130 |
| Government colonies | 57 |
| Camps (police/army/paramilitary) | 32 |
Note. *All three patients were transgender. α: illiterate refers to participants having no formal schooling; β: unemployed comprises homemakers, students, and retired persons; γ: self-employed consists of nonstructured employment such as manual labors, daily wagers, vendors, drivers, and shopkeepers; δ: Indian rupee.
Questionnaire. Since COVID-19 is a novel disease and an existing questionnaire appropriate for use in India was not available to measure stigma, we designed a semistructured questionnaire. After getting clearance from our Institute Ethics Committee (IEC-402/08.5.2020), we initially conducted telephonic interviews with 25 participants, asking various questions about stigma. Their responses were sent to five experts having experience in these areas. After analyzing these responses and incorporating comments sent by the experts, the draft questionnaire was modified, and the final questionnaire was formulated to measure various important domains of stigma. The final questionnaire consisted of six key domains of daily life where we had identified stigma in our preliminary interviews with the patients. These domains are self-perceived stigma, neighborhood stigma, quarantine-related stigma, stigma experienced at the market, stigma experienced at work, and stigma experienced by patients’ family members. Each domain included items that assessed the presence (“yes”) or absence (“no”) of multiple specific causes of stigma. If the respondent reported ≥1 items within a domain, they were considered as having experienced stigma for that domain (Table 2). Respondents were asked additional team-derived questions to assess perceived causes of stigma, level of perceived stress on a Likert scale of 1–5 (1–5, “no stress” to “very severe stress”), and overall quality of life (QoL) on a Likert scale of 1–5 (1–5, “very poor” to “very good”). After administering the survey, we used an open-ended question (“Do you wish to share any other experience not included in the questionnaire?”) to ask respondents to share any additional relevant experiences, and these responses were recorded in patient’s own language.
Table 2.
Responses Recorded During Data Collection at Various Domains
| Stigma at Various Domains | Options | Number of Participants Who Responded1 | Stigma2 (Yes/No) | |
| Yes | No | |||
| Self-perceived stigma | I feel dirty and ashamed because of the infection; therefore, I don’t tell anybody about it | 125 | 182 | 129 |
| I feel guilty that people got infected by me | 115 | |||
| I feel worthless, and my life has become meaningless because of the disease | 123 | |||
| I feel it all is my own fault that I became positive | 71 | |||
| I don’t feel dirty, ashamed, guilty, and worthless because of my disease | 129 | |||
| Quarantine-related stigma | I felt discriminated by police, govt. officials, or any other nonmedical staff involved in my care | 122 | 163 | 148 |
| I felt discriminated against by ambulance service operators | 105 | |||
| I felt discriminated against by reception staff at the hospital/quarantine center | 107 | |||
| I felt discriminated against by housekeeping staff during my stay at the hospital/quarantine | 119 | |||
| I felt discriminated against by doctors who were visiting me | 50 | |||
| I was not discriminated against by administrative/nonmedical/health care staff at all | 148 | |||
| Neighborhood stigma | My neighbors resist stay in locality for me/my family | 139 | 222 | 89 |
| My neighbors blame me/my family if someone else in the locality gets infected | 123 | |||
| I feel my neighbors/relatives/friends will not invite my family and me to their social events | 139 | |||
| They don’t show their hesitation, but I feel that they are keeping distance from me/my family | 190 | |||
| They blame my ways of living, including religious rituals, for my disease and making derogatory comments on me/my family | 77 | |||
| I feel no change | 89 | |||
| Stigma experienced by patients’ family members | They feel hesitant to tell their friends about my disease | 207 | 207 | 104 |
| They feel no hesitation in telling their friends about my disease | 104 | |||
| Stigma experienced at the market | People shut their doors when they see me walking outside my house | 139 | 214 | 97 |
| People make unusual physical distance from me (which is beyond advisable limits of social distancing) | 179 | |||
| Shopkeepers and vendors ask me not to come closer to their shops | 145 | |||
| I am not able to purchase my supplies because vendors are not willing to sell products to me | 124 | |||
| I feel no change | 97 | |||
| Stigma experienced at work | I feel less respect at my workplace, and my ideas are not given as much values as before | 142 | 180 | 131 |
| I feel discriminated against as my colleagues feel hesitant to include me in their groups | 137 | |||
| I feel that my promotion and perks will get affected because of my disease | 107 | |||
| I feel the firm wants me to self-resign from the job | 110 | |||
| I lost my job because I got fired by the firm | 77 | |||
| I am feeling no change in behavior towards me at my workplace | 131 | |||
Note. 1Total number of participants who opted for a response. (Questions were designed in multiple-choice pattern, so one participant can opt one or more than one option.) 2All affirmative responses to a question were cumulatively considered as “yes” to stigma. Option depicting no discrimination was considered as “no” to stigma.
Sample size. On March 15, 2020, our hospital was declared COVID-19 hospital and experts of various departments were deployed in the treating team. We started recruiting patients on the same date. Since there was no previous study available, we discussed the matter with our experts (faculties in the Dept. of Psychiatry). Based on their clinical experience with other infectious diseases, they suggested that the prevalence would vary from 50% to 70%. Assuming that 50% of patients experienced stigma for any domain and a 15% relative margin of error (margin of error = 1.96 × standard error of proportion, i.e., 7.5%), with the goal of a 99% confidence level, we required a sample of 295 patients. Based on a conservative response rate of 50%, we decided to approach 600 patients, to be assured of adequate number of participants.
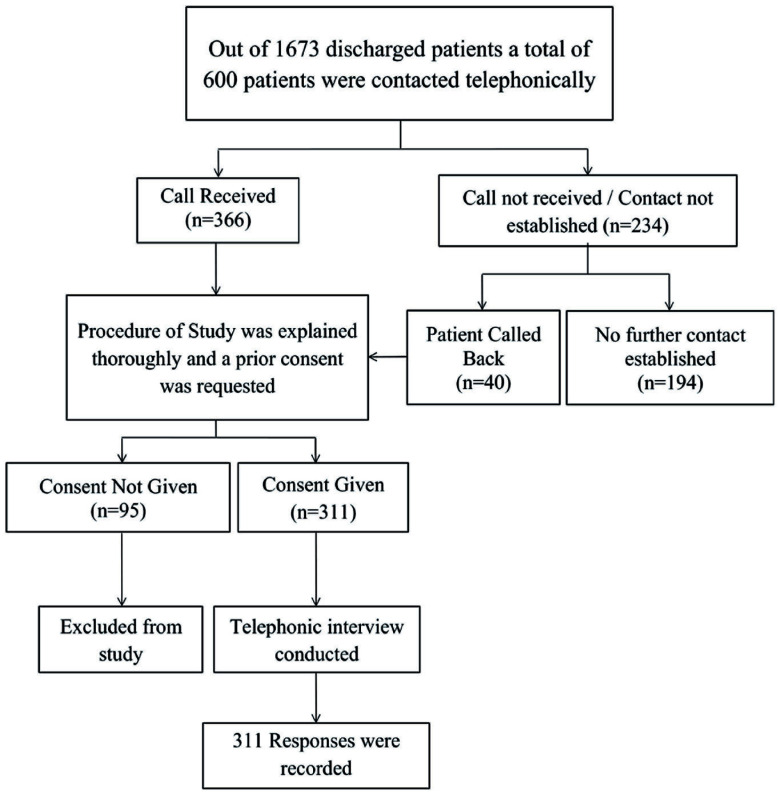
Study procedure. The survey was conducted between May 15 and June 30, 2020. Patients discharged between May 1 and June 15, 2020, who provided informed consent and were able to participate in the telephonic interview were included in the study. A total of 1,673 patients were discharged between May 1 and June 15, 2020, with around 30–40 discharges daily. Lists of discharges were collected from records, and two weeks after the discharge date, the patient was approached for a telephonic interview. From the list of discharges, 600 subjects were contacted, using convenience sampling, for interview. Two researchers contacted patients telephonically and interviewed them in either Hindi or English, as per the participant’s preference. Each interview lasted approximately half an hour. Participants’ participation and data collection are illustrated in Figure 1. We have analyzed stigma at various domains of life, perceived causes of stigma, level of stress, and QoL of these participants.
Figure 1. Protocol Followed for Data Collection.
Statistical analysis. Data were analyzed using SPSS software version 21 (IBM Corp. Armonk, New York). Associations between stigma and patient characteristics were evaluated using the chi-square test/Fisher’s exact test. The 95% confidence interval of the proportion of stigma at each level was determined using the Wald method. Chi-square for trend was performed to test the trend of stigma with age. To find the correlation between the level of stress and QoL, Spearman’s correlation was performed.
Results
A total of 1,673 COVID-19 patients were discharged between May 1 and June 15, 2020, and conveniently 600 participants were approached, of which 311 agreed to participate (response rate of 51.8%). Since stigma is associated with the sociodemographic profile, all 311 recruited participants are described based on their sociodemographic profile as depicted in Table 1.
Outcome. To analyze stigma, we considered the internal stigma as self-perceived stigma; external stigma as stigma perceived from family or friends or at place of work or marketplace.10 Responses given by participants are illustrated in Table 2.
During interviews, self-perceived stigma was recorded by asking whether participants felt dirty, ashamed, guilty, worthless, and meaningless. A total of 182 (58.52%) participants (95% CI: 53.04–64.00) agreed that they experienced self-perceived stigma. On being asked questions regarding quarantine-related stigma, 163 (52.41%) participants (95% CI: 46.86–57.96) reported having experienced discrimination during the process of managing the disease and receiving care. Regarding stigma imposed by neighbors on them and their family members, 222 (71.38%) participants (95% CI: 66.36–76.40) perceived that they and their family members were discriminated against by neighbors. A total of 207 (66.56%) participants (95% CI: 61.31–71.80) reported that their families felt hesitant, while 104 (33.1%) reported that their families felt no hesitation in revealing the disease status of the participant. Participants were asked regarding experiences at market places, including others observing unusual physical distancing or shopkeeper’s refusing to serve them. Overall, 214 (68.81%) participants (95% CI: 63.66–73.95) experienced discrimination at markets and other public places. A total of 180 (57.88%) participants (95% CI: 52.39–63.37) experienced discrimination at workplace, such as losing respect, facing a risk of losing perks, or endangering promotions and jobs.
A significant correlation was observed between age and stigma, where the age group of 46–60 years (n = 53 [17.04%]) showed the highest incidence of stigma. Self-employed participants (n = 91[29.26%]) had the highest incidence of stigma, and this association was statistically significant. While looking for the correlation between family income and stigma, it was noted that the highest stigma is in the income group of 10–20 thousand per month (n = 83 [26.69%]). Participants living in slums: daily wagers/labors/vendors (n = 92 [29.58%]) showed the highest incidence of stigma. Results were analyzed for all six domains of daily life, and their association with sociodemographic determinants is illustrated in Table 3.
Table 3.
Association of Stigma with Sociodemographic Profiles and Various Domains of Life
| Categories | Subcategories | Stigma in COVID-19 Patients at Various
Levels |
|||||||||||
| Self-perceived Stigma |
Quarantine-Related Stigma |
Neighborhood Stigma |
Stigma Experienced by Patients’ Family
Members |
Stigma Experienced at the Market |
Stigma Experienced at Work |
||||||||
| % | P Value | % | P Value | % | P Value | % | P Value | % | P Value | % | P Value | ||
| Sex | Male (246) | 59.3 | 0.229 | 54.5 | 0.097 | 73.2 | 0.128 | 69.1 | 0.058 | 69.1 | 0.575 | 59.8 | 0.078 |
| Female (62) | 53.2 | 46.8 | 62.9 | 54.8 | 66.1 | 48.4 | |||||||
| Others (3) | 100·0 | 00 | 100.0 | 100.0 | 100.0 | 100.0 | |||||||
| Age | ≤15 (4) | 00 | 0.041 | 00 | 0.031 | 50.0 | 0.454 | 50.0 | 0.117 | 50.0 | 0.372 | 00 | 0.075 |
| 16–30 (129) | 54.3 | 48.8 | 72.9 | 62.0 | 66.7 | 57.4 | |||||||
| 31–45 (107) | 60.7 | 51.4 | 71.0 | 70.1 | 70.1 | 58.9 | |||||||
| 46–60 (53) | 69.8 | 67.9 | 75.5 | 77.4 | 77.4 | 66.0 | |||||||
| >60 (18) | 55.6 | 50.0 | 55.6 | 50.0 | 55.6 | 44.4 | |||||||
| Education | Illiterate (4) | 50.0 | 0.949 | 50.0 | 0.975 | 50.0 | 0.908 | 75.0 | 0.532 | 75.0 | 0.829 | 50.0 | 0.931 |
| Up to class 5 (13) | 69.2 | 46.2 | 76.9 | 69.2 | 76.9 | 61.5 | |||||||
| 5th–10th (51) | 60.8 | 49.0 | 70.6 | 74.5 | 62.7 | 51.0 | |||||||
| 11th–12th (82) | 59.8 | 51.2 | 70.7 | 70.7 | 73.2 | 59.8 | |||||||
| Graduate (144) | 56.2 | 54.9 | 72.9 | 61.1 | 68.1 | 59.0 | |||||||
| Postgraduate (17) | 58.8 | 52.9 | 64.7 | 64.7 | 64.7 | 58.8 | |||||||
| Occupation | Unemployed (37) | 56.8 | < 1.73E-8 | 37.8 | < 1.63E-8 | 56.8 | < 1.47E-5 | 59.5 | < 4.63E-4 | 59.5 | < 3.01E-4 | 43.2 | < 4.99E-8 |
| Student (23) | 17.4 | 13.0 | 52.2 | 43.5 | 56.5 | 21.7 | |||||||
| Self employed (91) | 76.9 | 69.2 | 86.8 | 79.1 | 84.6 | 78.0 | |||||||
| Private employee (83) | 68.7 | 67.5 | 78.3 | 73.5 | 73.5 | 67.5 | |||||||
| Government employee (49) | 40.8 | 36.7 | 65.3 | 61.2 | 53.1 | 42.9 | |||||||
| Defense/ police/ security (28) | 35.5 | 32.1 | 46.4 | 42.9 | 53.6 | 39.3 | |||||||
| Family income (INR per month) | Up to 5,000 (14) | 78.6 | < 8.28E-12 | 57.1 | < 5.85E-10 | 78.6 | < 5.81E-11 | 85.7 | < 3.06E-9 | 85.7 | < 3.10E-9 | 64.3 | < 1.17E-8 |
| 5,000 to 10,000 (31) | 71.0 | 58.1 | 83.9 | 77.4 | 71.0 | 71.0 | |||||||
| 10,000 to 20,000 (83) | 77.1 | 72.3 | 88.0 | 84.3 | 86.7 | 72.3 | |||||||
| 20,000 to 30,000 (92) | 58.7 | 58.7 | 69.6 | 65.2 | 68.5 | 57.6 | |||||||
| 30,000 to 50,000 (64) | 48.4 | 35.9 | 68.8 | 56.2 | 62.5 | 54.7 | |||||||
| >50,000 (27) | 00 | 00 | 14.8 | 18.5 | 18.5 | 3.7 | |||||||
| Residence/ society | Slums: daily wagers/labors/vendors (92) | 73.9 | < 1.43E-9 | 64.1 | < 8.63E-7 | 87.0 | < 1.3E-8 | 80.4 | < 2.15E-5 | 82.6 | < 2.14E-5 | 70.7 | < 3.52E-6 |
| Private colonies (130) | 66.2 | 60.0 | 74.6 | 69.2 | 70.0 | 63.8 | |||||||
| Government colonies (57) | 40.4 | 36.8 | 61.4 | 54.4 | 61.4 | 42.1 | |||||||
| Camps (police/army/other) (32) | 15.6 | 15.6 | 31.2 | 37.5 | 37.5 | 25.0 | |||||||
From the results, it is evident that stigma affects all domains of daily life, which is also reflected in responses to the open-ended questions in which participants narrated their experiences of discrimination in various forms and formats, which varied from apprehension of getting discriminated if they disclose the information that they are infected to coronavirus, to losing business as people preferred not to make any contact with a person who was once infected. Participants reported that their interpersonal relations with friends and family members were also affected due to the infection. Participants also reported discrimination by neighbors and community members where they live and discrimination even to their family members who were living in remote villages and had no contact with the participant. Therefore, on asking participants to share their experience, a total of ten participants responded. The responses, recorded in their own language, are illustrated in Table 4.
Table 4.
Open-Ended Responses Recorded in Participants’ Own Language
| Serial No. | Response |
| 1 | I have not even informed my siblings and parents about the infection. If I do so, and people of society get to know it, they will completely outcast my family. |
| 2 | I am a sanitation worker. People always maintain unusual distancing from me, and after I contracted COVID, the situation is going to be worse. |
| 3 | It is getting difficult to run my shop now. Customers do not prefer my shop for purchases, specifically those who know me personally. |
| 4 | When someone passes by my house, they cover their face, and soon after crossing my house, they remove the cover; people clean their doorsteps if I pass by but not if somebody else passes by; people close their doors if they see me walking out of my house. |
| 5 | Vendors and shopkeepers are asking me not to come to their shops. If I go to their shops, they say that other customers won’t come. Therefore it is getting difficult for me to buy my supplies from nearby shops. |
| 6 | People have stopped visiting our houses; they do not include us for social gatherings; not inviting us to family functions; and not even letting their kids play with our kids. |
| 7 | Residents of my locality are not letting me enter in locality despite having proper discharge documents provided by the hospital |
| 8 | Residents of my village got to know about my infection. Now they have started discriminating against my parents who are living in the village. |
| 9 | When ambulance and police personals came to pick me from my home, people were watching from their windows as if I have committed some crime and I am being taken to police custody. I was scared. |
| 10 | While talking about me, people start their conversations by saying, “The person who had COVID-19….” and then they continue further. |
Stigma at multiple domains. A total of 133 (42.8%) participants faced stigma in all six domains, and more than 60% of participants experienced stigma in ≥3 domains.
Perceived causes of discrimination. While asked about the probable causes of discrimination, 184 (59.2%) participants replied that fear of getting infected was the cause, 172 (55.3%) opted for lack of education and awareness in society, and 131 (42.1%) replied that lack of proper documented information regarding rejoining the community after discharge created a confusion between the patient and the community. In total, 129 (41.5%) participants reported that people discriminated against them more because of their stay in hospital/quarantine center, and 125 (40.2%) participants opted for the state of panic fostered by news and media channels as the reason for the discrimination.
Level of stress and QoL. Spearman’s correlation was applied to find the strength of association between stress score and the QoL score, and the Spearman’s rho was –0.87 (P-value < 2.85E-96). A negative correlation was observed, which revealed that if stress is low, then the QoL is high (Table 5). Considering scores 1 and 2 as poor QOL; scores 3, 4, and 5 as good QOL; scores 1 and 2 as minimal stress; and scores of 3, 4, and 5 as significant stress, a significant positive correlation was observed between the stress and number of stigma levels (Spearman’s rho = 0.43). Those with higher levels of stigma had higher stress. The correlation between the QoL and the number of stigma levels was negative (Spearman’s rho = –0.40) indicating that more stigmatized individuals had poorer QoL.
Table 5.
Association Between the Level of Stress and QoL
| Level of Stress | Quality of Life |
||||||
| Score | 1 (Very Poor) | 2 (Poor) | 3 (Regular) | 4 (Good) | 5 (Very good) | Total | |
| 1 (No stress) | 0 | 0 | 1 | 9 | 32 | 42 | |
| 2 (Mild stress) | 0 | 3 | 16 | 105 | 3 | 127 | |
| 3 (Moderate stress) | 0 | 7 | 75 | 8 | 1 | 91 | |
| 4 (Severe stress) | 0 | 46 | 5 | 0 | 0 | 51 | |
| 5 (Very severe stress) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 0 | 56 | 97 | 122 | 36 | 311 | |
Note. Spearman’s strength of association between level of stress and quality of life illustrating a negative correlation. Spearman’s rho = –0.869, P value < 2.85E-96.
Discussion
Our study revealed a total of 263 (84.5%) participants faced stigma in some domain in their day-to-day lives and more than 60% of participants experienced stigma in ≥3 domains. The prevalence of stigma in any domain ranged from 52% to 71%. Significant associations of stigma were observed with occupation, family income, and place of residence.
Stigma is a complex, ambiguous phenomenon that depends upon various factors broadly divided into internal perception and external stimulus, also known as internal and external sociology.11,12 Stigma associated with infections such as COVID-19 occurs late in the disease trajectory.13 As the incidence of COVID-19 increased, isolated reports of stigma started coming in from various domains of Indian society.14
Middle-aged to older adults suffer a significant burden of stigma. We found that self-stigma and stigma faced due to quarantine were significant in this age group. A potential cause is the lack of social support for older adults15 translating into stigma.16 Various studies have reported that older adults with HIV-AIDS face significant stigma. This finding has been attributed to multiple factors, including ageism, homophobia, racism, substance abuse, etc.17–19 The transgender community normally suffers huge discrimination, which COVID-19 may have worsened.20
Occupation significantly contributed to stigmatization. Persons with marginal social security suffer heavily from stigma as compared to persons working in socially secured environments.21,22 But after the 2003 SARS outbreak in Hong Kong, Lee et al. found an increased level of stigma in higher-earning employed respondents. This was ascribed to employment being crucial for one’s livelihood. Fear of stigma can lead to under-confidence and may result in a poor work attitude, leading to unemployment and a vicious cycle of avoiding job interviews.23
Known social acquaintances imposed more stigma on cured individuals. Social distancing and proper hygiene measures are keys to containing COVID-19, but when distancing and hygiene gets practiced beyond advisable limits, particularly toward a COVID-19 cured individual, we believe this discrimination faced by them significantly contributes to their stigma burden.24
Significant association of education to stigma has been found in various studies.25 More educated people have better knowledge of diseases and are less likely to be stigmatized. Our study did not show any significant difference of stigma with the level of education, probably because COVID-19 has been the center of discussion right from the time it was declared a pandemic.
Patients’ trust in their family and friends plays an important role in disclosing their status. In our study, most participants were hesitant to disclose their infection to their loved ones. This may be because of the self-perceived stigma itself and the inability to trust their community. It has been seen that family members are not willing to share utensils or eat with patients suffering from infectious diseases.26
Stigma reported was not confined to patients but also extended to the family members. Mak et al. compared stigma associated with various infectious diseases (SARS, AIDS, TB) and found that stigma perceived by patients significantly affected their family members and contributed to care giver strain.10 Lack of proper information and awareness about the disease causes such discrimination.
Stigma is a difficult phenomenon to overcome. However, rational attitude and subtle changes in societal behavior with a scientific approach toward medical situations,27 diluting misinformation and misconceptions by pooling authentic and evidence-based information, placing accountability on spreaders of misinformation and fake news, and proper documentation in discharge sheet regarding patient’s fitness to rejoin the community are the immediate measures to reduce stigma. For long-term developments, schools and other educational institutions should help in mass education to the society. Volunteer participations, street plays, skits, television, and online interactive sessions will help alleviate stigma. Use of the words “COVID-19” and “coronavirus” should be avoided for infected as well as cured individuals.28
Limitations
Because stigma in COVID-19 patients has not been evaluated in India so far, we used expert-informed, team-derived items to assess stigma. However, using a conservative approach to interpretation, we found high levels of patient-perceived stigma across important domains. Because feasibility limited our ability to collect data on a matched non-COVID sample, we do not know the extent to which COVID independently contributed to the stigma we identified. Nevertheless, our qualitative comments and some of our items such as family-reported stigma support that an important aspect of the stigma we describe is COVID-related. The study being exploratory and conducted at a single center does not reflect aspects of the pandemic-associated stigma that may occur in other areas or contexts in India. Therefore, further study with a big sample size is required.
Conclusion
A high prevalence of stigma to COVID-19-cured individuals exist in Indian society. A huge proportion of these individuals face stigma at multiple domains of their daily lives. The burden of stigma further translates into stress and hampers the QoL. We found a significant association between stigma and educational status, society where the patient resides, and the age and occupation of patients. These associations will help understand the roots of stigma and the methods to fight this stigma.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Barrett R and Brown P. Stigma in the time of influenza: social and institutional responses to pandemic emergencies. J Infect Dis, 2008; 197(suppl 1): S34–S37. [DOI] [PubMed] [Google Scholar]
- 2.Waxler NE. Learning to be a leper: a case study in the social construction of illness—ABIM—an annotated bibliography of Indian medicine [Internet]. Indianmedicine.eldoc.ub.rug.nl. https://indianmedicine.eldoc.ub.rug.nl/44525/ (2020, cited 19 December 2020) [Google Scholar]
- 3.Maleche A, Citro B, Tisile P, et al. Measuring TB-related stigma. Int J Tuberc Dis, 2017; 21(11): 4–5. [DOI] [PubMed] [Google Scholar]
- 4.Cava M, Fay K, Beanlands H, et al. The experience of quarantine for individuals affected by SARS in Toronto. Public Heal Nurs, 2005; 22(5): 398–406. [DOI] [PubMed] [Google Scholar]
- 5.Hatzenbuehler M, Phelan J, and Link B. Stigma as a fundamental cause of population health inequalities. Am J Public Heal, 2013; 103(5): 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkman L and Syme S. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda county residents. Am J Epidemiol, 1979; 109(2): 186–204. [DOI] [PubMed] [Google Scholar]
- 7.Pappas G, Kiriaze I, Giannakis P, et al. Psychosocial consequences of infectious diseases. Clin Microbiol Infect, 2009; 15(8): 743–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmedani B. Mental health stigma: society, individuals, and the profession [Internet]. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3248273/2020 (2020, cited 19 December 2020). [PMC free article] [PubMed]
- 9.Ramaci T, Barattucci M, Ledda C, et al. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustain, 2020; 12(9): 3834. [Google Scholar]
- 10.Mak WW, Cheung F, Woo J, et al. A comparative study of the stigma associated with infectious diseases (SARS, AIDS, TB). Hong Kong Med J, 2009; 15(suppl 8): 34–37. [PubMed] [Google Scholar]
- 11.Pescosolido B and Martin J. The stigma complex. Annu Rev Sociol, 2015; 41(1): 87–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reidpath D and Chan K. A method for the quantitative analysis of the layering of HIV-related stigma. AIDS Care, 2005; 17(4): 425–432. [DOI] [PubMed] [Google Scholar]
- 13.Logie C. Lessons learned from HIV can inform our approach to COVID-19 stigma. J Int AIDS Soc, 2020; 23(5): e25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stigma F. Fighting the Covid stigma [Internet]. The New Indian Express. https://www.newindianexpress.com/states/kerala/2020/jun/17/fighting-the-covid-stigma-2157506.html (2020, cited 19 December 2020).
- 15.Goll J, Charlesworth G, Scior K, et al. Barriers to social participation among lonely older adults: the influence of social fears and identity. PLoS One, 2015; 10(2): e0116664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Mendonça Lima C, Levav I, Jacobsson L, et al. Stigma and discrimination against older people with mental disorders in Europe. Int J Geriatr Psychiatry, 2003; 18(8): 679–682. [DOI] [PubMed] [Google Scholar]
- 17.Emlet C. “You’re awfully old to have this disease”: experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. The Gerontol, 2006; 46(6): 781–790. [DOI] [PubMed] [Google Scholar]
- 18.Foster P and Gaskins S. Older African Americans’ management of HIV/AIDS stigma. AIDS Care, 2009; 21(10): 1306–1312. [DOI] [PubMed] [Google Scholar]
- 19.Haile R, Padilla M, and Parker E. “Stuck in the quagmire of an HIV ghetto”: the meaning of stigma in the lives of older Black gay and bisexual men living with HIV in New York City. Cult Heal Sex, 2011; 13(4): 429–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mattocks K, Sullivan J, Bertrand C, et al. Perceived stigma, discrimination, and disclosure of sexual orientation among a sample of lesbian veterans receiving care in the Department of Veterans Affairs. LGBT Heal, 2015; 2(2): 147–153. [DOI] [PubMed] [Google Scholar]
- 21.Tsai A. Socioeconomic gradients in internalized stigma among 4,314 persons with HIV in Sub-Saharan Africa. AIDS Behav, 2015; 19(2): 270–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stuart H. Stigma and work. Healthc Pap, 2004; 5(2): 100–111. [DOI] [PubMed] [Google Scholar]
- 23.Lee S, Chan L, Chau A, et al. The experience of SARS-related stigma at Amoy gardens. Soc Sci Med, 2005; 61(9): 2038–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kane J, Elafros M, Murray S, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med, 2019; 17(1): 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Des Jarlais D, Stuber J, Tracy M, et al. Social factors associated with AIDS and SARS. Emerg Infect Dis, 2005; 11(11): 1767–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Datiko D, Jerene D, and Suarez P. Stigma matters in ending tuberculosis: nationwide survey of stigma in Ethiopia. BMC Public Heal, 2020; 20(1): 190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sartorius N. Stigmatized illnesses and health care. Croat med J, 2007; 48(3): 396–397. [PMC free article] [PubMed] [Google Scholar]
- 28.National Academies of Sciences, Engineering, and Medicine. Ending discrimination against people with mental and substance use disorders: the evidence for stigma change. Washington, DC: The National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK384914/ (2016, cited 19December2020). [PubMed] [Google Scholar]