Abstract
Introduction
Ivermectin is a drug with antiviral properties and has been proposed as an alternative treatment for patients with COVID-19, in some countries; however, there is limited evidence to support its clinical use. Accordingly, the aim of this review and meta-analysis is to obtain superior evidence on the effectiveness and safety of ivermectin in treatment of COVID-19.
Methods and analysis
We will search in the medical databases and International Clinical Trials Registry Platform databases for randomised clinical trials and quasi-randomised trials published from December 2019. The criteria for inclusion are that infection needs to be confirmed by a real-time PCR or serology test, and the effect of ivermectin has been compared with placebo, symptomatic treatment or no treatment. We will exclude observational studies and clinical trials that involved patients with symptoms suggestive of COVID-19, but without a laboratorial diagnosis. Outcomes of interest include mortality, time to symptom resolution, time of hospitalisation, frequency of invasive mechanical ventilation and extracorporeal membrane oxygenation, incidence of severe acute respiratory syndrome, admission to intensive care unit, viral load, PCR-negative status, percentage of infection after prophylactic use, and total incidence of adverse and side effects. Study selection will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Two reviewers will independently select the studies and assess their eligibility. Two other reviewers will independently extract data from each study. Meta-analysis will then be carried out using fixed-effects or random-effects model, using the mean difference for continuous outcomes and the relative risk for dichotomous outcomes. Bias risk will be assessed using the Cochrane risk-of-bias tool. The quality of evidence for each outcome will be assessed using GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology. Review Manager V.5.3.5 will be used for synthesis and subgroup analysis.
Ethics and dissemination
Owing to the nature of the review, ethical approval is not required. The results will be disseminated through peer-reviewed publications.
PROSPERO registration number
CRD42020197395.
Keywords: clinical pharmacology, infectious diseases, public health
Strengths and limitations of this study.
Evaluation of the efficacy and safety of ivermectin against COVID-19 using only randomised clinical trial (RCT) and quasi-RCT data.
Strict search strategy in multiple databases and references of selected studies.
Evidence quality assessment using GRADE (Grading of Recommendations Assessment, Development and Evaluation) working group methodology.
Only a small number of RCTs and quasi-RCTs have evaluated the effectiveness and safety of ivermectin in COVID-19 treatment.
Heterogeneity among patients infected with SARS-CoV-2 and treated with ivermectin can influence the results.
Introduction
In December 2019, an increase in pneumonia cases was reported in Wuhan, China, and the causative agent was subsequently identified as a new coronavirus (SARS-CoV-2) on 3 January 2020 through tests on secretions from the upper respiratory tract. With the exponential increase in cases of the disease (ultimately termed COVID-19) caused by this virus, the WHO declared a pandemic; by the end of January 2021, 102 399 513 cases of infected patients and 2 217 005 deaths due to COVID-19 have been registered worldwide.1 The scientific community has been working hard to find preventive strategies and effective treatments against SARS-CoV-2, with numerous randomised clinical trials (RCTs) already conducted and others at an advanced stage of testing in humans with medicines and vaccines.2–4 To reduce the risk of severe acute respiratory syndrome (SARS) caused by SARS-CoV-2 and to stimulate the immune system, numerous vaccines have been developed, including mRNA-1237 and CoronaVac, which have been approved for emergency use in some countries.5–8 However, to date, there is no evidence of the effectiveness of drugs for the treatment of patients infected with SARS-CoV-2, and results on the efficacy and safety of several vaccines under development are not conclusive.9
With no confirmed treatment, several countries have adopted a strategy of the off-label use of drugs with potential antiviral and immunomodulatory effects approved for the clinical management of other infections in patients with COVID-19 since the beginning of the pandemic.10 Some studies have evaluated the effectiveness of antivirals and other drugs against COVID-19, including lopinavir/ritonavir, remdesivir and chloroquine/hydroxychloroquine, with or without azithromycin and dexamethasone.11–15 Despite some medications showing positive results, such as dexamethasone, which reduced mortality among inpatients who were receiving mechanical invasive ventilation or oxygen, there is still no drug with proven efficacy for the treatment of COVID-19.15 16
Caly et al17 reported that ivermectin has antiviral activity against SARS-CoV-2 and inhibits its replication in vitro. As a result, some countries have proposed the prophylactic use of ivermectin after contact with infected people, or its therapeutic use for those who have been diagnosed with an asymptomatic, mild form of the disease or in the early stage of COVID-19. Ivermectin is an anti-parasitic agent that causes tonic paralysis of the muscles, thereby inducing the death of the parasite, along with anti-inflammatory activity.18 Other studies have indicated that ivermectin can inhibit the in vitro replication of some RNA viruses such as dengue virus, Zika virus, yellow fever virus and chikungunya virus.19–22 In addition, ivermectin was shown to regulate the immune system, suggesting that it could prevent contracting SARS-CoV-2, even after close contact with an infected individual, as a prophylactic measure.23 24 However, these results are mainly derived from in vitro or observational studies, with only a few RCTs that have evaluated the efficacy and safety of ivermectin in patients with COVID-19 conducted to date.
Brito et al9 conducted a systematic review of studies excluding RCTs and concluded that the effectiveness and safety of ivermectin in patients with COVID-19 have not yet been proven, and its use is not recommended until the results of ongoing clinical trials can be evaluated. Therefore, this protocol describes a systematic review for assessing the efficacy and safety of ivermectin in the prophylaxis and treatment of COVID-19 based on updated data, including those from RCTs.
Methods and analysis
This protocol was designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines extension for reporting systematic review protocols (PRISMA-P).25 The review protocol was registered with the International Prospective Register of Systematic Reviews.
Research question
Is ivermectin safe and effective for the prophylaxis and treatment of adults infected with SARS-CoV-2?
Inclusion criteria
Participants
This review will include studies that involved adults with SARS-CoV-2 infection confirmed by real-time PCR or serological tests, and people at risk of exposure to the virus (people having ‘high-risk’ contact with patients with confirmed COVID-19). Studies including children or patients with only suggestive symptoms of COVID-19, but without a diagnosis confirmed by any of the aforementioned tests, will be excluded.
Intervention
RCTs and quasi-RCTs, one in which participants are allocated to different arms of the trial (to receive the study medicine, or placebo, for example) using a method of allocation that is not truly random, that evaluated the efficacy and safety of ivermectin alone or in combination with other interventions will be considered for inclusion.
There will be no restriction on the dosage, start, and duration of treatment, or route of administration of ivermectin.
Comparator
RCTs and quasi-RCTs that compared ivermectin with placebo, symptomatic treatment or no treatment will be considered. In addition, studies that included treatment with ivermectin in combination with another treatment will be eligible only if the comparison groups also received a similar co-intervention as the group treated with ivermectin. The comparison groups may have received placebo, symptomatic treatment or no treatment other than the co-intervention.
Outcome measures
Primary outcome
The primary outcome will be mortality.
Secondary outcomes
Secondary outcomes will be symptom resolution, time of hospitalisation (in days), use of invasive mechanical ventilation and extracorporeal membrane oxygenation, incidence of SARS, admission to the intensive care unit, viral load, PCR-negative status, percentage of infection after prophylactic use, and total incidence of adverse and serious side effects.
Types of studies
We will consider only RCTs and quasi-RCTs.
Article exclusion criteria
Studies with the following features will be excluded: participants diagnosed based solely on symptoms; duplicate, insufficient data or data that cannot be extracted; observational studies; retrospective studies; non-randomised trials; quasi-experimental studies and animal studies.
Search strategy
Data from studies that evaluated the efficacy and safety of ivermectin against SARS-CoV-2, published as of December 2019, will be obtained from the electronic databases PubMed, Embase, CENTRAL, Web of Science, Scopus, Cochrane Library and Google Scholar, and from the clinical trials registries Clinicaltrials.gov, EU Clinical Trials Register and International Clinical Trials Registry Platform, without language restrictions. Articles will also be searched from the references of the selected studies and from grey literature databases such as OpenGrey.
The following terms with their respective synonyms will be used for database searches: (ivermectin OR stromectol OR mectizan OR MK-933 OR MK 933 OR MK933 OR eqvalan OR ivomec OR soolantra) AND (“COVID-19” OR COVID19 OR “SARS-CoV-2” OR “2019-nCoV” OR “2019-nCoV disease” OR “COVID 19” OR “2019 novel coronavirus infection” OR coronavirus) AND (“randomized clinical trial” OR “controlled clinical trial” OR ‘randomized controlled trial” OR “intervention study OR “clinical study” OR “clinical studies”). The search strategy that will be used for PubMed is presented in table 1 as an example.
Table 1.
PubMed search strategy
| Search items | |
| 1 | ivermectin |
| 2 | stromectol |
| 3 | mectizan |
| 4 | MK-933 |
| 5 | MK 933 |
| 6 | MK933 |
| 7 | eqvalan |
| 8 | Ivomec |
| 9 | Soolantra |
| 10 | OR/1–9 |
| 11 | “COVID-19” |
| 12 | COVID19 |
| 13 | “SARS-CoV-2” |
| 14 | “2019-nCoV” |
| 15 | “2019-nCoV disease” |
| 16 | “COVID 19” |
| 17 | “2019 novel coronavirus infection” |
| 18 | Coronavírus |
| 19 | OR/11–18 |
| 20 | “randomized clinical trial” |
| 21 | “controlled clinical trial” |
| 22 | “randomized controlled trial” |
| 23 | “intervention study” |
| 24 | “clinical study” |
| 25 | clinical studies |
| 26 | OR/20–25 |
| 27 | 10 AND 19 AND 26 |
Study selection
After searching the databases and references, all identified articles will be exported to the web-based tool Rayyan,26 and duplicates will be removed. In the first stage, titles and abstracts will be reviewed independently by at least two reviewers (MLdLM and ATBS) based on the inclusion criteria. The full texts of the selected studies will be independently analysed by two other reviewers (RRM and DF); only studies identified by both pairs of reviewers based on the inclusion criteria will ultimately be included in the systematic review, and a third reviewer (RNC) will make a final decision for inclusion in the case of discrepancy.
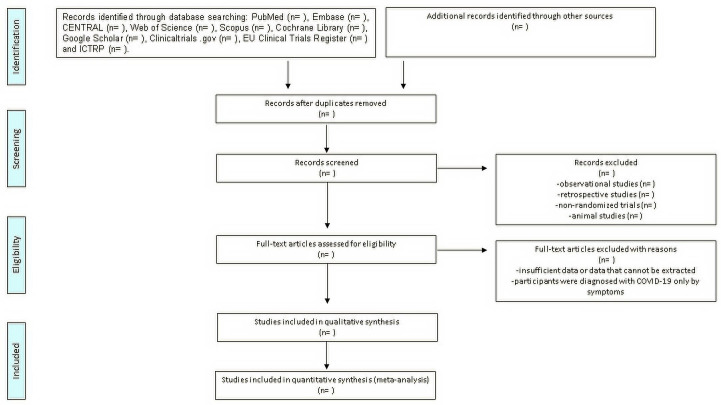
We will maintain a record of the reasons for excluding clinical trials at all stages of review. The results of the selection or exclusion of the studies will be reported using the PRISMA flow chart as shown in figure 1.
Figure 1.
PRISMA flow chart: search strategy. ICTRP, International Clinical Trials Registry Platform; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Data extraction
Using standardised forms, two reviewers (ATBS and DF) will independently extract the following data from each included study: first author; year of publication; study location (country); study design; average age of participants with SD; number of participants; and details about the intervention administered and comparison, including dose and therapeutic scheme, duration, time after diagnosis, route of administration, outcomes assessed, time of their measurement and adverse effects.
Risk of bias assessment
The risk of bias for each RCT or quasi-RCT will be assessed using the Cochrane tool to assess the risk of bias in randomised studies (RoB 2).27
Two reviewers (DF and RRM) will independently assess the following five bias domains for all reported results and time points: (1) bias due to the randomisation process, (2) deviations from intended interventions (selection and measurement bias), (3) unreported outcome data, (4) presentation of outcomes and (5) selection of reported results. Thus, the studies will be classified as having a low risk of bias, inconclusive risk or high risk of bias. Discrepancies between reviewers will be resolved by discussion to reach a consensus; if necessary, a third reviewer (RNC) will be consulted. Age, comorbidities (eg, hypertension, obesity, diabetes), disease severity and co-interventions will be considered as potential confounding factors.
Measures of treatment effect
For dichotomous variables, we will analyse the relative risk with the respective 95% CIs. For continuous variables, we will use the mean difference and SD to summarise the data with the 95% CI. In cases in which continuous variables were measured using different scales, the treatment effect will be expressed as the standardised mean difference (SMD) with 95% CI. Wherever possible, we will multiply the SMD by an SD representative of the set of studies, such as the SD of a well-known scale used by several studies included in the analysis on which the result was based. In cases where the minimally important difference (MID) was known, we will present continuous variables in MID units or will report the results as the difference in the proportion of patients who achieved an important minimum effect between intervention and control groups.
Data synthesis
In the event of inclusion of three or more RCTs, we will perform a quantitative synthesis (meta-analysis) using RevMan V.5.3.528 software with the fixed-effects or random-effects model if more than 50% heterogeneity is identified among studies. Statistical heterogeneity will be assessed using the I2 statistic. Subject to insufficient data to calculate an estimated effect, a narrative synthesis will be presented, describing the direction and size of the effects, along with any reported accuracy measures.
Missing data management
We will contact the authors to obtain missing or incomplete data; if unable to obtain the missing data, incomplete data will be excluded from the analysis.
Reporting bias assessment
We will construct funnel plots to evaluate reporting bias if more than 10 RCTs are included. In other cases, Egger’s test will be performed to assess publication bias.
Subgroup analysis
We plan to carry out the following subgroup analyses, wherever possible: respiratory failure versus SARS, adults versus elderly people over 65 years old, and prophylactic versus therapeutic use of ivermectin. If a significant difference between subgroups is identified (test for interaction p<0.05), we will report the results for individual subgroups separately. We will also perform a formal test for subgroup interactions using RevMan V.5.3.5.
Sensitivity analysis
We will perform a sensitivity analysis to explore the effects of trial bias risk on outcomes, wherever possible. The primary analysis will include only those studies that had low risk or some concerns of bias according to the RoB 2 assessment. We will include high risk of bias studies in a secondary analysis to assess the impact on the results.
In the case of a significant difference between the estimates of the effect of the primary analysis and sensitivity analysis, we will perform an adjusted sensitivity analysis.
Grading the quality of evidence
The quality of evidence for all outcomes will be assessed using the GRADE (Grading of Recommendations Assessment, Development and Evaluation)29 Working Group methodology through risk of bias, consistency, objectivity, accuracy and reported bias. The certainty of evidence will be classified as high, moderate, low or very low.
Discussion
Ivermectin is a drug with antiviral properties against a few viral infections. Owing to its considerable accessibility due to its low total cost, it has become an alternative treatment for patients with COVID-19. Studies have shown a reduction in mortality in patients hospitalised with COVID-19 who received the drug.23 30 Another study indicated that early administration of ivermectin resulted in earlier clearance of the virus compared with placebo, assessed over a 5-day course, suggesting that early intervention with ivermectin may limit viral replication in the host.31
However, there is still no concrete evidence on the efficacy of ivermectin in the prophylaxis and treatment of patients infected with SARS-CoV-2 who are in the initial stage of the disease, or who are already hospitalised after the infection worsens. Thus, it is important to summarise all of evidence, as it becomes available evidence, especially robust evidence from RCTs, to assess the effectiveness and safety of ivermectin during different phases of COVID-19.
Siemieniuk et al32 performed a systematic review to compare the effectiveness of various drugs used for the treatment of COVID-19, and concluded that corticosteroids reduced the need for mechanical ventilation; however, the effectiveness of azithromycin, remdesivir, hydroxychloroquine, interferon-beta, and tocilizumab has not been proven in the treatment of patients infected with SARS-CoV-2. They did not assess the efficacy and safety of ivermectin. A recent RCT evaluated the effect of early treatment with ivermectin on viral load, in addition to symptomatic and humoral responses in patients with COVID-19.33 Twenty-four patients were equally randomised to a group that received a single dose of ivermectin and a group that received placebo. The authors concluded that among patients without risk factors for severe COVID-19 who received a single dose of 400 mg/kg of ivermectin, there was no reduction in viral load and no difference in the proportion of a positive PCR test on the seventh day. However, patients treated with ivermectin showed earlier improvement in self-reported anosmia/hyposmia.
A possible limitation of this study is that clinical trials with low number of participants, or events, or both, leading to wide CIs and high uncertainty of the estimated effects can compromise the level of evidence generated in this meta‐analysis.
Therefore, this systematic review will be carried out using a specific approach with a meta-analysis of the results obtained if there are at least three comparable studies with available data. The current systematic review is justified because of the lack of evidence on the effectiveness and safety of ivermectin in people infected with SARS-CoV-2. The results of this study are expected to provide new insight into the potential effects of ivermectin in adults infected with this new coronavirus, and thus eliminate uncertainties about the treatment that persist despite some related published studies.
Patient and public involvement
This research is based on previously conducted studies and does not involve any patients or individuals or include new studies on human subjects performed by any of the authors.
Ethics and dissemination
Because of the nature of the review, which is a collection of data without direct human involvement, ethical approval is not required. The results will be widely disseminated through peer-reviewed publications, as well as presentations at conferences, congresses and symposia.
Supplementary Material
Footnotes
Contributors: RNC conceived of the study and provided general guidance for drafting the protocol. ATBS and DFOS designed the search strategy. ATBS, CFMF, DFOS, MLdLM, PVAL and RRM drafted the protocol. RRM and RNC reviewed and revised the manuscript. All authors have read and approved the final version of the manuscript.
Funding: This work was partially supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES) (Finance Code 001).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . Coronavirus disease 2019 (COVID-19), 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf [PubMed]
- 2.Tan W, Zhao X, Ma X, et al. A novel coronavirus genome identified in a cluster of pneumonia cases — Wuhan, China 2019−2020. China CDC Wkly 2020;2:61–2. 10.46234/ccdcw2020.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565–74. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soiza RL, Scicluna C, Thomson EC. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing 2021;50:279–83. 10.1093/ageing/afaa274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021;384:403–16. 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palacios R, Patiño EG, de Oliveira Piorelli R, et al. Double-Blind, randomized, placebo-controlled phase III clinical trial to evaluate the efficacy and safety of treating healthcare professionals with the adsorbed COVID-19 (inactivated) vaccine manufactured by Sinovac – PROFISCOV: a structured summary of a study protocol for a randomised controlled trial. Trials 2020;21:1–3. 10.1186/s13063-020-04775-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Zeng G, Pan H, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis 2021;21:181–92. 10.1016/S1473-3099(20)30843-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brito GV, Marra LP, Medeiros FC. Ivermectina para a Covid-19. Revisão sistemática rápida, 2020. Available: https://oxfordbrazilebm.com/index.php/2020/05/07/ivermectina-para-o-tratamento-de-pacientes-com-covid-19-revisao-sistematica-rapida2/
- 10.Sanders JM, Monogue ML, Jodlowski TZ. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA Netw 2020;323:1824–36. [DOI] [PubMed] [Google Scholar]
- 11.Cao B, Wang Y, Wen D, et al. A trial of Lopinavir-Ritonavir in adults hospitalized with severe Covid-19. N Engl J Med 2020;382:1787–99. 10.1056/NEJMoa2001282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2020;395:1569–78. 10.1016/S0140-6736(20)31022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fiolet T, Guihur A, Rebeaud ME, et al. Effect of hydroxychloroquine with or without azithromycin on the mortality of coronavirus disease 2019 (COVID-19) patients: a systematic review and meta-analysis. Clin Microbiol Infect 2021;27:19–27. 10.1016/j.cmi.2020.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elavarasi A, Prasad M, Seth T, et al. Chloroquine and hydroxychloroquine for the treatment of COVID-19: a systematic review and meta-analysis. J Gen Intern Med 2020;35:3308–14. 10.1007/s11606-020-06146-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horby P, Lim WS, Emberson JR, RECOVERY COLLABORATIVE GROUP . Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med 2020:NEJMoa2021436. [Google Scholar]
- 16.Cunningham AC, Goh HP, Koh D. Treatment of COVID-19: old tricks for new challenges. Crit Care 2020;24:91. 10.1186/s13054-020-2818-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caly L, Druce JD, Catton MG, et al. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res 2020;178:104787. 10.1016/j.antiviral.2020.104787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.González Canga A, Sahagún Prieto AM, Diez Liébana MJ, et al. The pharmacokinetics and interactions of ivermectin in humans--a mini-review. Aaps J 2008;10:42–6. 10.1208/s12248-007-9000-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tay MYF, Fraser JE, Chan WKK, et al. Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor ivermectin. Antiviral Res 2013;99:301–6. 10.1016/j.antiviral.2013.06.002 [DOI] [PubMed] [Google Scholar]
- 20.Wagstaff KM, Sivakumaran H, Heaton SM, et al. Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J 2012;443:851–6. 10.1042/BJ20120150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang SNY, Atkinson SC, Wang C, et al. The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer. Antiviral Res 2020;177:104760. 10.1016/j.antiviral.2020.104760 [DOI] [PubMed] [Google Scholar]
- 22.Varghese FS, Kaukinen P, Gläsker S, et al. Discovery of berberine, abamectin and ivermectin as antivirals against Chikungunya and other alphaviruses. Antiviral Res 2016;126:117–24. 10.1016/j.antiviral.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 23.Heidary F, Gharebaghi R. Ivermectin: a systematic review from antiviral effects to COVID-19 complementary regimen. J Antibiot 2020;73:593–602. 10.1038/s41429-020-0336-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rizzo E, Ivermectin RE. Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action. Naunyn Schmiedebergs Arch Pharmacol 2020;393:1153–6. 10.1007/s00210-020-01902-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile APP for systematic reviews. Syst Rev 2016;5:21. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 28.The Nordic Cochrane Centre . Review manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Cochrane Collaboration, 2014. [Google Scholar]
- 29.Guyatt G, Oxman AD, Akl EA, et al. Grade guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 30.Rajter JC, Sherman MS, Fatteh N, et al. Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ivermectin in COVID nineteen study. Chest 2021;159:85–92. 10.1016/j.chest.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmed S, Karim MM, Ross AG, et al. A five-day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Dis 2021;103:214–6. 10.1016/j.ijid.2020.11.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siemieniuk RA, Bartoszko JJ, Ge L, et al. Drug treatments for covid-19: living systematic review and network meta-analysis. BMJ 2020;370:m2980. 10.1136/bmj.m2980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaccour C, Casellas A, Matteo AB. The effect of early treatment with ivermectin on viral load, symptoms and humoral response in patients with mild COVID-19: a pilot, double-blind, placebo-controlled, randomized clinical trial. EClinicalMedicine 2020;32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.