Abstract
Background
Multiple sclerosis (MS) is a chronic inflammatory disease and acute exacerbations are also a part of the clinical course. The presence of the disease and relapses cause stress in people with MS (pwMS). For this reason, stress coping strategies of the patients are important in reducing perceived stress. Our aim in this study is to evaluate which strategies pwMS use during the COVID-19 pandemic, the effect of the strategies on perceived stress, their relationship with relapses and their role on quality of life (QoL).
Methods
An online form including Perceived Stress Scale (PSS; 10 items), Coping with Experienced Problems Scale (Brief-COPE; 28 items) and SF-12 were sent to 340 pwMS under our follow-up.
Results
During the COVID-19 pandemic, we found that the patients used the strategies of turn to religion, planning and acceptance at a high rate. PSS score was high in 23 (11.2%) of the patients. The patients with low perceived stress used the acceptance strategy more (P=0.008). We found a negative correlation between physical component summary (PCS) of SF-12 and denial (r=-0.2, p<0.001) and distraction (r =-0.1, p=0.04). A negative correlation was found between mental component summary (MCS) of SF-12 and behavioral disconnection (r=-0.2, p=0.006). There was a positive correlation between MCS and humor (r=0.1, p=0.04), use of instrumental support (r=0.2, p=0.009), planning (r=0.1, p=0.04), and positive reframing (r=0.2, p=0.002).
Conclusion
PwMS have been successful in coping with stress in the first half of the pandemic with the combination of emotional and problem-focused strategies. Acceptance strategy was highly adopted by patients with low PSS, and the tendency to use the active coping strategy together with the acceptance strategy was high in patients without relapses. Adoption to emotional strategies may have prevented the severe deterioration in QoL in this study group in the early period of Covid-19 pandemic.
Keywords: Multiple sclerosis, COVID-19 pandemic, Perceived stress, Coping strategies, Quality of life, Relapse
1. Introduction
Stress can be defined as a process created by a physical, mental, or emotional factor that exceeds the coping capacity of the individual and causes bodily or mental tension. Stress may result in some psychological or biological damage in the individual (Mohr, 2007). Stress is alleviated with cognitive and behavioral strategies or coping strategies that minimize or eliminate feelings of anxiety and discomfort (Jean et al., 1997). Coping constitutes the entirety of all the thoughts and behaviors an individual uses to manage all stressful demands (Grech et al., 2018). Stress and coping are two concepts that are often used together (Friedman, 2011). The effect of stress on the individual is measured by evaluating how the individual perceives and gets over the situations related with stress. Multiple Sclerosis (MS) is a neurodegenerative and inflammatory chronic disease of the central nervous system, characterized by relapses and disability. In MS, different neurological systems are affected due to demyelination and axonal damage. The relationship between stress and MS has been studied for many years. Most of the studies have proven that stressful life events can be risk factors for MS exacerbations and affect quality of life (QoL) in patients (Mohr et al., 2004, Brown et al., 2006, Gil-González et al., 2020).
In the literature it has been stated that traumatic, life-threatening acute stressors cause very high levels of cortisol secretion by the adrenal glands, and milder chronic stressors can cause changes in the neuroendocrine-immune system by reducing the defense against inflammation (Mohr, 2007). Persistent stress rather than acute, such as a life-threatening illness or serious marital difficulties, is defined as chronic stress, while events in overtime such as the death of a loved one or job loss are considered acute stress (McGonagle and Kessler, 1990). Clinical data have shown the importance of hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system dysregulation for the pathogenesis and progression of MS. These two main systems have known to respond to stress. At the same time, the combination of a hyporesponsive HPA axis and insensitive peripheral glucocorticoid in early MS may allow excessive inflammation. It is assumed that occurrence of HPA axis hyperactivity during the disease progression, is associated with neurological disability, brain atrophy and cognitive impairment (Heesen et al., 2007).
People with MS (pwMS) need to manage both disease-related and daily life-related stresses at every stage of their disease. It is also important in terms of QoL to control stress with appropriate stress management strategies. It is difficult to distinguish between voluntary or involuntary responses to stress (Friedman, 2011). The emotional outcome of encountering a stressful situation is related to the extent and how the individual handles this situation. Thus, particularly during uncontrollable events such as health-related crises, coping efficiency is measured by the degree of emotional stress reduction, not by the reduction of the stressful situation's degree. Efforts aimed at minimizing emotional distress are classified as emotional-focused coping strategies, while efforts to reduce or change the source of distress are categorized as problem-focused coping strategies. Most individuals use a combination of both emotional and problem-focused coping methods when handling stressful situations (Jean et al., 1997). In studies examining strategies of coping with stress in pwMS, it has been determined that emotional-focused coping strategies to manage the stress caused by attacks are mostly used in the early stages of the disease. When the illness prolongs and the disability occurs, patients tend to use problem-oriented strategies (Lode et al., 2007).
Active coping, problem solving, planning the solution of problem, cognitive positive restructuring, emotional and instrumental social support, emotional expression, and acceptance are the strategies that found to be associated with higher QoL in MS. In addition, Grech et al found a similar association with restrained coping (Grech et al., 2018) which is defined as holding on to take action until getting appropriate opportunity (Carver et al., 1989), Strober with humor (Strober, 2018) and Mikula et al with stopping unpleasant emotional coping strategies (Mikula et al., 2014). On the contrary, avoidance, behavioral disconnection, distancing, distraction, denial, emotion-focused and venting coping strategies, social withdrawal, wishful thinking, self-criticism, suppression, and self-control coping strategies are the ones reported to be associated with low QoL (Gil-González et al., 2020).
The COVID-19 infection, which was declared as a global pandemic on March 11, 2020, has become a life-threatening, traumatic stressor for all humanity (Anand et al., 2020). Therewithal, the fact that chronic diseases are poor prognostic factors, and the short and long-term effects of the virus are not fully known have led to increased levels of fear and stress in many chronic disease groups (Pedrozo-Pupo and Campo-Arias, 2020). Questions about the course of COVID -19 infection in individuals with MS, the effect of COVID -19 on the course of MS, and the side effects that may occur with the used immunomodulatory and immunosuppressant drugs in pwMS were raised as the additional stressor factors.
With the announcement of the pandemic in Turkey on March 11, 2020, it drew our attention that until June, there was a significant decrease in hospital admissions and help requests of MS patients who were regularly followed-up due to complaints and relapses. We wondered what coping strategies MS patients, who manage a chronic disease with the stress factors of life, are trying to overcome this situation in the face of an acute and serious stressor such as a pandemic. Therefore, in this study, we aimed to evaluate the coping strategies used by pwMS during the first six months of the COVID-19 pandemic. We examined the effects of perceived stress levels on disease activity and QoL together with coping strategies.
2. Material and Methods
2.1. Participants of the study
Three hundred and forty patients with definite MS diagnosis who were being followed up from the demyelinating diseases outpatient clinic of Tekirdag Namik Kemal University Training and Research Hospital were invited to the study. Contact information was obtained from the hospital database for communication. Inclusion criteria were determined as having a diagnosis of MS according to the 2010 Revised Mc Donald criteria (McDonald et al., 2001), volunteering to participate in the study, being literate, having technical equipment to answer questions online. Patients that have a major psychiatric diagnosis, have substance abuse disorder, have another chronic disease besides MS, and pregnant or in the postpartum period were excluded from the study. Approval was obtained for the study by the Ethics Committee of Tekirdag Namik Kemal University Faculty of Medicine with reference number 2020.217.09.04.
Informed consent information was available on the home page of the forms prepared in the online application and the participants were able to access the questions if they clicked the "I Approve" button.
2.2. Data Collection
PwMS filled out an online form consisting of demographic questionnaire, Perceived stress scale (PSS), Coping Orientations to Problems Experienced (Brief COPE), and Quality of Life scale (SF-12). Patients could directly reach the researchers in case of needing technical support during filling process of the form.
Demographic questionnaire was used to obtain the information about age, gender, education level, marital status (married, single, widowed etc.), employment status and drugs used.
2.3. Perceived stress scale
Stress level was measured with the 10-item PSS of which the reliability and validity of Turkish version was made by Eskin et al (Eskin et al., 2013). Participants were asked to score each item of the scale between 0 (never) and 4 (very often) according to their feelings and thoughts during the period after the COVID-19 pandemic started. Scoring results in values between 0 and 40 and higher scores were associated with increased perceived stress (Sanaeinasab et al., 2017). The patients who scored 25 and above was considered having high perceived stress (Pedrozo-Pupo and Campo-Arias, 2020).
2.4. Coping orientations to problems experienced (Brief COPE)
Brief-COPE is a 28 item self-report questionnaire designed to measure effective and ineffective ways to deal with stressful life events (Carver, 1997). This questionnaire cognitively and behaviorally assesses how a person reacts to a difficult or stressful event in his/her life (Carver et al., 1989, Carver, 1997). Brief-COPE, of which reliability and validity of Turkish version was conducted by Bacanli et al. (Bacanlı et al., 2013), consists of a total of 14 subscales (self-distribution, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disconnection, ventilation, positive reframing, planning, humor, acceptance, religion, and self-blame). This strategy determination scale created by Carver, Scheier and Weintraub was used in our study, and participants were clearly instructed to address the COVID-19 pandemic as a target stress factor. The coping score for each factor was determined as the sum of the scores of individual items, and a higher total score was considered to indicate more use of coping style (Lode et al., 2007). In the categorization model created by Cooper, coping strategies are analyzed in three categories; 1- Problem-focused (active coping, use of instrumental support, planning) 2- Emotional-focused (acceptance, use of emotional support, humor, positive reframing, religion) 3- Dysfunctional (behavioral disconnection, denial, distraction, self-blame, substance use, venting of emotions (Cooper et al., 2006). In the model presented by Meyer, two strategy categories were determined 1- adaptive (problem + emotional oriented strategies) 2- maladaptive (dysfunctional strategies) (Meyer et al., 2001). The data obtained were evaluated together with both categorization systems.
2.5. Quality of life (SF-12)
SF-12 is a short version of SF-36 currently used to assess QoL in pwMS (Ware et al., 1994). It is a self-report questionnaire consisting of 12 items that assesses two components: Physical health (physical component summary = PCS) and mental health (mental component summary = MCS) (Ataoğlu et al., 2017). In this study, the scoring of the SF-12 scale was made using certain automated algorithms (Ottoboni et al., 2017). Higher score was considered to indicate better QoL.
Disease-specific data were recorded retrospectively from hospital databases. Disease duration, age of diagnosis, type of disease, relapse status during the first six months of the COVID-19 pandemic, the treatment regimen and their disability score (Expanded Disability Status Scale (EDSS)) (Kurtzke, 1983) were recorded. Disease duration was defined as the time elapsed after diagnosis.
2.6. Evaluation of the data
Since March 11, 2020 when the first patient diagnosed with COVID-19 notification was made in Turkey, relapses of the pwMS who accepted to participate in the study, were obtained from the patient records. The occurrence of new symptoms or worsening of existing symptoms lasting more than 24 hours in the absence of fever or infection was considered as relapse (McDonald et al., 2001) Patients with and without relapses were analyzed in 2 categories.
2.7. Statistical analysis
Mean, standard deviation, percentage and minimum-maximum expressions were used to express the variables. The normality distribution of the variables was evaluated with the Kolmogorov-Smirnov test and then quantitative data were analyzed. In the evaluation of coping strategies, normally distributed groups were evaluated using Student-T test, and groups not showing were evaluated with Mann-Whitney U test. Perceived stress score and demographic and clinical characteristics were evaluated with Mann Whitney U test or Kruskal Wallis test with Bonferroni correction according to the evaluated group numbers. We analyzed the gender in two (male and female), marital status in three (married, single, widowed), education status in four (primary school graduates, secondary school graduates, high school graduates, university graduates), employment status in two (employed and unemployed), income level in three (poor, moderate, good), used disease modifying therapy (DMT) in three (oral, injectable, and intravenous) and relapse status in two (with relapse and without relapses) categories. The relation between age, age at diagnosis, disease duration and perceived stress score and between QoL and coping strategies was evaluated with the Spearman correlation test. P value less than 0.05 was considered as significant.
3. Results
The forms were sent online to 340 patients who were under follow-up with definite MS diagnosis. Two hundred forty (70.5%) patients completed the forms, but data of 35 (10.2%) patients were not analyzed due to missing data or duplicating entry or inappropriate responses. Data of 205 (60.3%) pwMS were analyzed. One hundred fifty-two (74.1%) of the patients were female and 53 (25.9%) were male and the mean age was 37.7 ± 10.0 (15–71) years. Demographic and disease specific features of the whole group summarized in Table 1 .
Table 1.
Demographic and disease specific features of the group and relationship between perceived stress are presented.
| PSS | ||||
|---|---|---|---|---|
| N (%) | Mean±SD1 (min-max) | p or r and p-value | ||
| Gender | Male | 53 (25.9%) | 0.1a | |
| Female | 152 (74.1%) | |||
| Age (years) | 37.7 ± 10.0 (15-71) | -0.08, 0.2b | ||
| Marital status | Married | 139 (67.8%) | 0.7c | |
| Single | 43 (21.0%) | |||
| Widowed | 23 (11.2%) | |||
| Educational status | Primary school graduates | 41 (20%) | 0.1c | |
| Secondary school graduates | 29 (14.1%) | |||
| High school graduates | 51 (24.9%) | |||
| University graduates | 84 (41.0%) | |||
| Employment status | Employed | 97 (47.3%) | 0.9a | |
| Unemployed | 108 (52.7%) | |||
| Income level | Good | 51 (24.9%) | 0.07c | |
| Moderate | 137 (66.8%) | |||
| Poor | 17 (8.3%) | |||
| Age at diagnosis (years) | 30.0 ± 9.1 (12-69) | -0.006, 0.9b | ||
| MS type | RRMS2 | 189 (92.2%) | ||
| SPMS3 | 12 (5.9%) | |||
| PPMS4 | 4 (2%) | |||
| Disease duration (years) | 7.4 ± 6.5 (1-34) | -0.007, 0.9b | ||
| EDSS | 2.1 ± 1.4 (0-6.5) | -0.03, 0.5b | ||
| DMT5 | Oral Injectabl Intravenous |
101 (49.3%) 65 (31.7%) 30 (14.6%) |
||
| Relapse in first six months of the pandemic | Yes No |
17 (8.3%) 188 (91.7%) |
0.6a |
Standard deviation.
Relapsing remitting multiple sclerosis.
Secondary progressive multiple sclerosis.
Primary progressive multiple sclerosis.
Disease modifying therapy.
Mann Whitney U test.
Spearman correlation.
Kruskal Wallis test.
3.1. Evaluation of data associated with perceived stress scale
It was observed that the PSS score of the whole MS group was 20.0 ± 4.4 (0–33). The PSS score was under 25 in 182 (88.8%) of the patients. Relapses occurred in 17 (8.3%) patients between March 11, 2020 and December 31, 2020. The perceived stress average score of these 17 patients was 20.8 ± 4.5 (13–29). There was no difference or relationship between perceived stress and demographic and disease-specific characteristics (Table 1).
3.2. Evaluation of the coping orientations to problems experienced (Brief COPE) related data
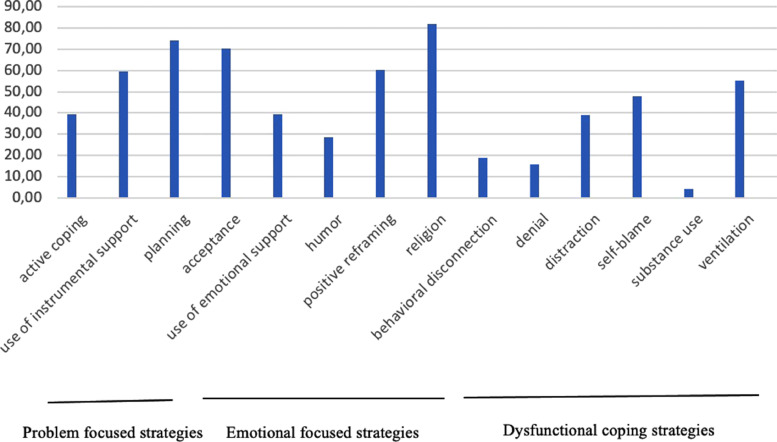
When the strategies used by the patients during the COVID-19 pandemic were evaluated, it was found that religion (6.8 ± 1.5) and acceptance (6.0 ± 1.5) from the emotional-focused strategies, planning (6.3 ± 1.4) from the problem-focused strategies were the ones mostly used and substance use (2.3 ± 1.0), denial (3.8 ± 1.5) and behavioral disconnection (3.8 ± 1.6) strategies were the ones least used in the whole group (Figure-1 ).
Fig. 1.
Coping strategies in MS patients during COVID-19 pandemic Coping strategies used by people with MS are given together with their percentages during the first half of the COVID-19 pandemic.
There was no difference between the DMT, educational status, marital status and income level groups in terms of problem, emotional focused and dysfunctional coping strategies. pwMS with low perceived scores used the acceptance strategy significantly more (P = 0.008) (Table-2 ). The usage of emotional (p < 0.001) and dysfunctional (p = 0.008) strategies were higher in women and the usage of dysfunctional strategies was statistically higher in the unemployed group (p = 0.008). There was a positive correlation between age and dysfunctional strategy scores (r = 0.1, p = 0.04). The usage of dysfunctional strategies was increasing with age. Although we couldn't find any relationship between the duration of the disease and the used strategies (p > 0.05), we saw that pwMS with the disease duration ≤ 3y were preferring to use emotional strategies more than the pwMS with the duration of disease longer than three years.
Table 2.
Comparison of Coping strategies adopted by the patients according to perceived stress scores are presented.
| Score of high perceived stress |
Score of low perceived stress |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | p-value | |
| Active coping | 5.2 | 1.4 | 2 | 8 | 5.1 | 1.4 | 2 | 8 | 0.9 |
| Use of instrumental support | 5.3 | 2.0 | 2 | 8 | 5.7 | 1.5 | 2 | 8 | 0.3 |
| Planning | 6.5 | 1.4 | 3 | 8 | 6.2 | 1.4 | 2 | 8 | 0.3 |
| Acceptance | 5.0 | 1.9 | 2 | 8 | 6.2 | 1.4 | 2 | 8 | 0.008* |
| Use of emotional support | 4.9 | 1.7 | 2 | 8 | 5.0 | 1.5 | 2 | 8 | 0.8 |
| Humor | 3.9 | 2.2 | 2 | 8 | 4.3 | 1.8 | 2 | 8 | 0.2 |
| Positive reframing | 5.9 | 1.6 | 2 | 8 | 5.7 | 1.6 | 2 | 8 | 0.7 |
| Religion | 6.7 | 2.0 | 2 | 8 | 6.8 | 1.5 | 2 | 8 | 0.8 |
| Behavioral disconnection | 3.8 | 1.4 | 2 | 7 | 3.8 | 1.6 | 2 | 8 | 0.6 |
| Denial | 4.1 | 1.9 | 2 | 8 | 3.7 | 1.5 | 2 | 8 | 0.4 |
| Distraction | 4.7 | 1.7 | 2 | 8 | 5.1 | 1.5 | 2 | 8 | 0.1 |
| Self-blame | 5.6 | 1.2 | 3 | 8 | 5.4 | 1.2 | 2 | 8 | 0.5 |
| Substance use | 2.7 | 1.6 | 2 | 7 | 2.3 | 0.8 | 2 | 7 | 0.6 |
| Ventilation | 5.3 | 1.8 | 2 | 8 | 5.3 | 1.6 | 2 | 8 | 1.0 |
p-value less than 0.05 was considered as significant. Patients with low stress levels used acceptance strategy more than the ones with high perceived stress.
3.4. Evaluation of the results according to relapses
The mean duration of disease in MSpwR group was 4.41 ± 3.9 (1–15) years, and in MSpwoR group it was 7.7 ± 6.7 (1–34) years. The duration of disease was significantly higher in MSpwoR (p = 0.04). It was determined that the perceived stress did not differ significantly between the patient groups with (MSpwR) and without relapses (MSpwoR) (p = 0.6). In the statistical analysis of the two groups with and without relapse, it was found that the usage of active coping (p = 0.01), acceptance (p = 0.04) and behavioral disconnection (p = 0.04) strategies was statistically higher in the group of patients without relapse (Table 3 ).
Table 3.
Comparison of coping strategies adopted by the patients with and without relapses are presented.
| Score of the MSpwR1 |
Score of the MSpwoR2 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | p-value | |
| Active coping | 4.3 | 1.5 | 2 | 7 | 5.2 | 1.4 | 2 | 8 | 0.01* |
| Use of instrumental support | 4.9 | 1.6 | 2 | 8 | 5.7 | 1.6 | 2 | 8 | 0.05 |
| Planning | 6.6 | 1.1 | 4 | 8 | 6.2 | 1.4 | 2 | 8 | 0.3 |
| Acceptance | 5.5 | 1.1 | 3 | 8 | 6.1 | 1.5 | 2 | 8 | 0.04* |
| Use of emotional support | 4.8 | 1.6 | 3 | 8 | 5.0 | 1.5 | 2 | 8 | 0.4 |
| Humor | 4.4 | 1.3 | 2 | 6 | 4.2 | 1.8 | 2 | 8 | 0.5 |
| Positive reframing | 6.4 | 1.3 | 4 | 8 | 5.7 | 1.6 | 2 | 8 | 0.06 |
| Religion | 7.0 | 1.6 | 3 | 8 | 6.8 | 1.5 | 2 | 8 | 0.3 |
| Behavioral disconnection | 3.0 | 1.1 | 2 | 6 | 3.8 | 1.6 | 2 | 8 | 0.04* |
| Denial | 3.6 | 1.3 | 2 | 7 | 3.8 | 1.5 | 2 | 8 | 0.8 |
| Distraction | 5.3 | 1.3 | 3 | 8 | 5.0 | 1.6 | 2 | 8 | 0.5 |
| Self-blame | 5.3 | 1.2 | 3 | 8 | 5.4 | 1.2 | 2 | 8 | 0.5 |
| Substance use | 2.1 | 0.5 | 2 | 4 | 2.3 | 1.0 | 2 | 7 | 0.5 |
| Ventilation | 5.4 | 1.8 | 2 | 8 | 5.3 | 1.6 | 2 | 8 | 0.9 |
p-value less than 0.05 was considered as significant. Active coping, acceptance and behavioral disconnection strategies were used significantly more in MSpwoR.
Multiple sclerosis patients with relapse.
Multiple sclerosis patients without relapse.
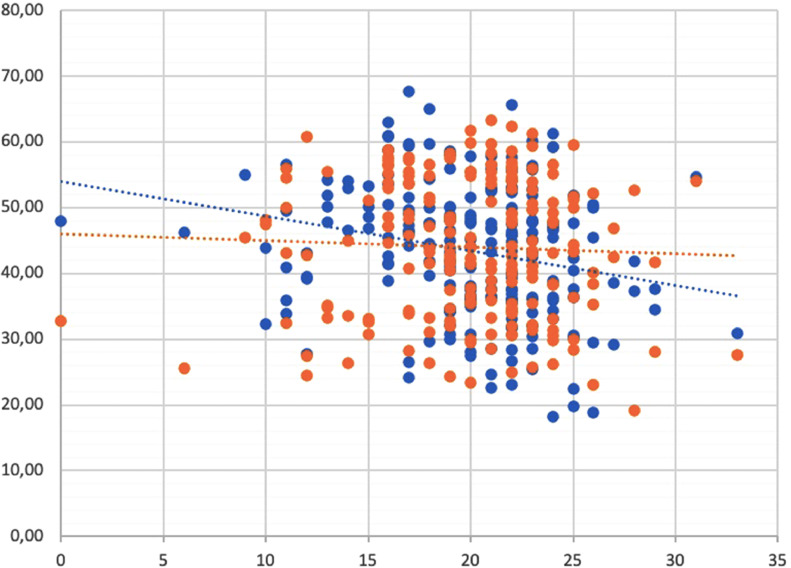
3.5. Evaluation of quality-of-life data
The mean PCS, which is the sub-scale of the SF-12 quality of life scale, was 43.9 ± 10.3 (19.1–63.2) and the mean MCS was 43.2 ± 10.4 (18.2–67.7). Although there was no significant correlation between the perceived stress score and PCS (r = -0.08, p = 0.2), we found a negative correlation between perceived stress score and MCS (r =-0.2, p < 0.001) (Figure-2 ).
Fig. 2.
The correlation between perceived stress scores and quality of life scores Relations (physical: red dots, mental: blue dots) are presented. A negative correlation between the PSS and mental quality of life, drawn as the blue dashed line, can be seen.
In the correlation analysis between coping strategies and physical / mental quality of life scores, a significant negative correlation between PCS and usage of denial (r = -0.2, p < 0.001) and distraction (r = -0.1, p = 0.04) strategies was found. Patients with poor PCS preferred to use these two dysfunctional strategies more than the ones with high PCS. A positive correlation was found between MCS scores and humor (r = 0.1, p = 0.04), use of instrumental support (r = 0.2, p = 0.009), planning (r = 0.1, p = 0.04), and positive reframing (r =0.2, p = 0.002) strategies, while a negative correlation was found between MCS scores and the use of behavioral disconnection (r =-0.2, p = 0.006) strategy.
4. Discussion
Learning the methods of coping with chronic disease and daily life related stress along with the diagnosis of the disease plays a very important role in the disease management and treatment adaptation processes in pwMS. In this study, coping strategies of pwMS against a sudden emerging, general environmental disease stressor, affecting the whole world were evaluated. We assessed the perceived stress of pwMS in a time between the acute and chronic phases of pandemic that can be considered as a transition period. Although all emotional, problem-focused and dysfunctional strategies were used by patients, it has been observed that the most frequently used strategies were emotional (religion, acceptance) and problem (planning) focused strategies (Fig. 1).
For many patients with MS, emotional distress has been reported as a persistent problem which may result, in part, from cognitive illness appraisals, coping strategies/responses and coping resources (Fisher et al., 2020). Rates of distress in the MS population during COVID-19 in reported studies were aligned with each other (Alschuler et al., 2021, Stojanov et al., 2020). Both depression and anxiety were elevated above the rates observed in the general population, but only marginally above typical levels for the MS population relative to prior studies. On the other hand, in a study conducted on pwMS during pandemic indicated increased perceived stress compared with healthy controls but in the same study, it has been observed that people with migraine were more stressful than pwMS (Bonavita et al., 2020). In our study group, the perceived stress level was found to be high only in 11.0% and perceived stress was not associated with many factors such as gender, age, marital status, education level, employment status, disease duration, disability and income level. The region where the patient group lived (Tekirdağ) during the period when the questionnaire forms were sent was one of the provinces in Turkey where the number of cases and the risk level of Covid-19 was low. With the pandemic announcement, the communication of this patient group with healthcare professionals was ensured regularly through established communication networks over the phone. Living in a region with a low COVID-19 risk level and being accessible to healthcare professionals may have reduced the perceived stress level, but it should be kept in mind that patients with low stress levels may have responded primarily to the questions we sent, and patients with high stress levels may not have participated in the study.
Along with a chronic illness, disability-related difficulties that may arise due to illness, as well as many negative situations such as affected by social relations and difficulty in obtaining a job, should be managed by the pwMS. The strategies that pwMS use to reduce their stress associated with the disease are influenced by the strategies they use in their general lives (Lode et al., 2007). Our study group used dysfunctional strategies at a low rate during the first wave of the COVID-19 pandemic (Fig. 1). Participants adopted to use mostly the emotional (religion, acceptance) and problem (planning) focused strategies to cope with stress. Considering the low perceived stress level, we can say that they were successful in reducing stress by using these strategies. It should not be forgotten that all strategies used to deal with the stress factor must be intertwined and in harmony with each other. Additionally, MS patients may have adopted more effective strategies to control the perceived level of stress during the acute COVID-19 outbreak, based on their experience of coping with a chronic disease and attacks. In our analysis, we saw that regardless of disability, female, unemployed and elderly pwMS used mostly emotional and dysfunctional coping mechanisms to reduce their stress. These results support the previous studies reporting that male pwMS use more problem-solving strategies and seek less support (Santangelo et al., 2021; Dennison et al., 2011) and dysfunctional strategies are mostly used in older and more disabled patients (Contentti et al., 2021). As we consider that the continued use of emotional-focused strategies and not being replaced by problem-focused strategies also increases the tendency to depression (Lynch et al., 2001, McCabe and McKern, 2002), we think that female, unemployed and older patients using emotional and dysfunctional strategies may have difficulty coping with the new pandemic process and will need more support.
Clinical relapse occurred in 8.3% of patients during the period between March 11 and December 31, 2020. When we evaluated the relapses according to time, we realized that during the first wave of COVID-19 pandemic (between March and June 2020), no relapse was recorded. This period was full of unknowns, it can be considered as the period with the highest perceived stress and the highest uneasiness during the acute pandemic process until today because of full closure conditions (i.e., governmental enforced lockdown). Questionnaire forms were sent to the patients in July 2020, and relapses emerged between September and December among the patients who volunteered to participate in the study. There are many studies in the literature examining the effects of stress on relapses (Mohr, 2007; Franklin et al., 1988; Artemiadis et al., 2011; Yamout et al., 2010; Xie et al., 2020). Although some of these studies reported no relation between relapses and perceived stress, most of them concluded that stress influences the number of relapses (Golan et al., 2008) or MRI activity of the disease (Yamout et al., 2010). Somer et al. evaluated the coping strategies associated with risk for relapse during war time and reported that active coping and planning strategies were used less in patients who had relapses during war time (Somer et al., 2010). In this study we observed that active coping, acceptance and behavioral dissociation strategies were mostly used by patients without relapses (Table 3). As a result of detecting the prominence of these strategies, it is thought that the risk of relapse may be low in patients who are intertwined and compatible with the use of problem, emotional-focused and dysfunctional strategies together. Another issue that we have recognized was that; duration of disease was significantly higher in MSpwoR. Although there are studies concluding that coping strategies remain stable over time if there are no interventions to change the coping pattern (Lode et al., 2010), there are also other studies that have indicated that patient's adjustment to the disease will promote more active and less avoidance coping strategies (Maes et al., 1999). During an unexpected high-risk disease pandemic pwMS with longer disease duration in our study selected mostly active coping and acceptance strategies in reducing the perceived stress, and they were the ones without relapse. Although religious beliefs were one of the frequently used strategies in our study group, there was no significant relationship between faith and relapses. Santangelo et al in their study evaluated the relationship between coping strategies and disease activity and their results revealed a less employment of emotion-based coping strategies in pwMS without depression. A scarce use of faith for support and a frequent adoption of a positive attitude were associated with an increase of MS activity in terms of annual relapse rate (Santangelo et al., 2021). It is accepted that religious beliefs and practices can play an important role in coping with stress, especially in patients with chronic diseases and poor prognosis, as they provide comfort and hope (Koenig, 2004). However, adopting to use ‘turning to religion’ strategy frequently in our study group may be related with the cultural differences.
QoL is impaired in RRMS patients for many reasons and pandemic could aggravate this. Changes in coping strategies used individually for managing the stress of new pandemic disease in pwMS also may affect the QoL (Bassi et al., 2021). In our study group, where the number of patients with high perceived stress levels was quite low, we found that mental QoL was negatively affected in patients with high perceived stress. The use of adaptive (emotional focused) strategies was associated with well-being in physical and mental QoL and maladaptive coping strategies (denial and distraction) was associated with lower physical QoL. This result was in accord with the studies reporting that QoL may be associated with the lower usage of problem-focused coping strategies and the higher usage of emotional coping strategies (Wilski et al., 2019; Roubinov et al., 2015). Usage of maladaptive strategies has also been reported as a negative factor on QoL (Contentti et al., 2021; Bassi et al., 2021). We didn't questionnaire the changes in QoL of our study group due to pandemic, but Stojanov et al reported in their study that the scores of pwMS obtained on questionnaires for QoL were lower during the pandemic compared to scores from 2019 in the same cohort of patients, but with no statistical significance (Stojanov et al., 2020). As coping is considered to be a dynamic process that takes into consideration changing characteristics of the stressor over time adoption to emotional strategies may have prevented the severe deterioration in QoL in the early period in pwMS.
4.1. Limitations of the study
Our study was conducted in a period in the first six months in which the COVID-19 pandemic became chronic. The time when patients filled out the questionnaires coincided with a period when stress became chronic and the impact of the pandemic was relatively less. Therefore, this stress factor can be considered as a chronic factor with reduced effect. At the same time, data were collected from patients under our follow-up via an online form and self-reporting. The patients were grouped as those who had relapses (n = 17) and those with high perceived stress (n = 23). We would like to state that the numbers of these patients are also relatively low. In addition, patients with high levels of depression (Jean et al., 1997; Lynch et al., 2001) and cognitive impairment (Goretti et al., 2009; Montel et al., 2012) may exhibit subtle changes in their attempts to cope particularly about the disease-related stressors. We would like to emphasize that the relationship between depression and cognition was not evaluated while coping strategies were evaluated. Also, considering that the population included in our study is limited to those with low EDSS and short disease duration, the findings cannot be generalized due to lack of representation of progressive MS subtypes.
5. Conclusion
PwMS have been successful in coping with stress in the first half of the pandemic with the combination of emotional and problem-focused strategies. It was noticed that the tendency to use the acceptance strategy was high especially in those with low perception of stress, and the tendency to use the active coping strategy together with the acceptance strategy was high in patients without relapses. Female, unemployed, and elderly PwMS adopted to use dysfunctional strategies regardless of their disability. Therefore, it can be thought that this patient group needs more support from healthcare professionals in coping with stress due to the pandemic. Since coping is a dynamic process that takes into consideration changing characteristics of the stressor over time, adoption to emotional strategies may have prevented the severe deterioration in QoL of PwMS in the early period of Covid-19 pandemic.
Sample CRediT author statement
Bengu Altunan: Conceptualization, Methodology, Formal analysis, Writing- Original draft preparation. Aysun Unal: Methodology, Conceptualization, Writing- Original draft preparation. Ayhan Bingol: Conceptualization, Investigation, Project administration. Filiz Dilek: Investigation, Visualization. Derya Girgin: Investigation, Visualization.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
Authors declare no conflicts of interest.
References
- Mohr D.C. Stress and multiple sclerosis. J. Neurol. 2007;254:1165–1168. doi: 10.1007/s00415-007-2015-4. [DOI] [PubMed] [Google Scholar]
- Jean V.M., Beatty W.W., Paul R.H., et al. Coping with general and disease-related stressors by patients with multiple sclerosis: relationships to psychological distress. Mult. Scler. 1997;3:191–196. doi: 10.1177/135245859700300304. [DOI] [PubMed] [Google Scholar]
- Grech L.B., Kiropoulos L.A., Kirby K.M., et al. Target coping strategies for interventions aimed at maximizing psychosocial adjustment in people with multiple sclerosis. Int. J. MS Care. 2018;20:109–119. doi: 10.7224/1537-2073.2016-008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman H.S. Oxford University Press; Oxford: 2011. The Oxford handbook of health psychology. [DOI] [Google Scholar]
- Mohr D.C., Hart S.L., Julian L., et al. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004;328:731. doi: 10.1136/bmj.38041.724421.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R.F., Tennant C.C., Sharrock M., et al. Relationship between stress and relapse in multiple sclerosis: Part I. Important features. Mult. Scler. 2006;12:453–464. doi: 10.1191/1352458506ms1295oa. [DOI] [PubMed] [Google Scholar]
- Gil-González I., Martín-Rodríguez A., Conrad R., et al. Quality of life in adults with multiple sclerosis: a systematic review. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle K.A., Kessler R.C. Chronic stress, acute stress, and depressive symptoms. Am. J. Community. Psychol. 1990;18:681–706. doi: 10.1007/BF00931237. [DOI] [PubMed] [Google Scholar]
- Heesen C., Mohr D.C., Huitinga I., et al. Stress regulation in multiple sclerosis: current issues and concepts. Mult. Scler. 2007;13:143–148. doi: 10.1177/1352458506070772. [DOI] [PubMed] [Google Scholar]
- Lode K., Larsen J.P., Bru E., et al. Patient information and coping styles in multiple sclerosis. Mult. Scler. 2007;13:792–799. doi: 10.1177/1352458506073482. [DOI] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: a theoretically based approach. J. Pers. Soc. Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Strober L.B. Quality of life and psychological well-being in the early stages of multiple sclerosis (MS): importance of adopting a biopsychosocial model. Disabil. Health J. 2018;11:555–561. doi: 10.1016/j.dhjo.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikula P., Nagyova I., Krokavcova M., et al. Coping and its importance for quality of life in patients with multiple sclerosis. Disabil. Rehabil. 2014;36:732–736. doi: 10.3109/09638288.2013.808274. [DOI] [PubMed] [Google Scholar]
- Anand K.B., Karade S., Sen S., et al. SARS-CoV-2: Camazotz's Curse. Med. J. Armed Forces India. 2020;76:136–141. doi: 10.1016/j.mjafi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrozo-Pupo J.C., Campo-Arias A. Depression, perceived stress related to COVID, post-traumatic stress, and insomnia among asthma and COPD patients during the COVID-19 pandemic. Chron. Respir. Dis. 2020;17 doi: 10.1177/1479973120962800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald W.I., Compston A., Edan G., et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- Eskin M., Harlak H., Demirkıran F., et al. The adaptation of the perceived stress scale into Turkish: a reliability and validity analysis. J. New Symp. 2013;51:132–140. http://yenisymposium.com/Pdf/EN-YeniSempozyum-c1d2631c.PDF [Google Scholar]
- Sanaeinasab H., Saffari M., Hashempour M., et al. Effect of a transactional model education program on coping effectiveness in women with multiple sclerosis. Brain Behav. 2017;7:e00810. doi: 10.1002/brb3.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol's too long: consider the brief COPE. Int. J. Behav. Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Bacanlı H., Sürücü M., İlhan T. An investigation of psychometric properties of coping styles scale brief form: a study of validity and reliability. Educ Sci. 2013;13:90–96. https://files.eric.ed.gov/fulltext/EJ1016675.pdf [Google Scholar]
- Cooper C., Katona C., Orrell M., et al. Coping strategies and anxiety in caregivers of people with Alzheimer's disease: the LASER-AD study. J. Affect. Disord. 2006;90:15–20. doi: 10.1016/j.jad.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Meyer B., Johnson S.L., Winters R. Responsiveness to threat and incentive in bipolar disorder: relations of the BIS/BAS scales with symptoms. J Psychopathol. Behav. Assess. 2001;23:133–143. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J.E., Kosinski M., Keller S.D. 2nd ed. The Health Institute, New England Medical Center; Boston, MA: 1994. SF-12: How to score the SF-12 physical and mental health summary scales. [Google Scholar]
- Ataoğlu S., Ankaralı H., Ankaralı S. A Comparison of the Measuring Instruments to Assess Quality of Life in Patients with Fibromyalgia Syndrome. Anadolu Klinigi Tıp Bilimleri Dergisi. 2017;22:85–94. doi: 10.21673/anadoluklin.285068. [DOI] [Google Scholar]
- Ottoboni G., Cherici A., Marzocchi M., et al. Algoritimi di Calcolo per gli Indici PCS e MSC del Questinario SF-12. AMS Acta. 2017;3:1–2. doi: 10.6092/unibo/amsacta/5751. [DOI] [Google Scholar]
- Kurtzke J.F. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33 doi: 10.1212/wnl.33.11.1444. 1444–1152. [DOI] [PubMed] [Google Scholar]
- Fisher P.L., Salmon P., Heffer-Rahn P., et al. Predictors of emotional distress in people with multiple sclerosis: A systematic review of prospective studies. J. Affect. Disord. 2020;276:752–764. doi: 10.1016/j.jad.2020.07.073. [DOI] [PubMed] [Google Scholar]
- Alschuler K.N., Roberts M.K., Herring T.E., et al. Distress and risk perception in people living with multiple sclerosis during the early phase of the COVID-19 pandemic. Mult. Scler. Relat. Disord. 2021;47 doi: 10.1016/j.msard.2020.102618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojanov A., Malobabic M., Milosevic V., et al. Psychological status of patients with relapsing-remitting multiple sclerosis during coronavirus disease-2019 outbreak. Mult. Scler. Relat. Disord. 2020;45 doi: 10.1016/j.msard.2020.102407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonavita S., Sparaco M., Russo A., et al. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID-19 pandemic. Eur. J. Neurol. 2020 doi: 10.1111/ene.14697. [DOI] [PubMed] [Google Scholar]
- Santangelo G., Corte M.D., Sparaco M., et al. Coping strategies in relapsing-remitting multiple sclerosis non-depressed patients and their associations with disease activity. Acta Neurol. Belg. 2021;121:465–471. doi: 10.1007/s13760-019-01212-5. [DOI] [PubMed] [Google Scholar]
- Dennison L., Yardley L., Devereux A., et al. Experiences of adjusting to early stage Multiple Sclerosis. J. Health Psychol. 2011;16:478–488. doi: 10.1177/1359105310384299. [DOI] [PubMed] [Google Scholar]
- Contentti E.C., López P.A., Alonso R., et al. Coping strategies used by patients with relapsing multiple sclerosis from Argentina: correlation with quality of life and clinical features. Neurol. Res. 2021;43:126–132. doi: 10.1080/01616412.2020.1831304. [DOI] [PubMed] [Google Scholar]
- Lynch S.G., Kroencke D.C., Denney D.R. The relationship between disability and depression in multiple sclerosis: the role of uncertainty, coping, and hope. Mult. Scler. 2001;7:411–416. doi: 10.1177/135245850100700611. [DOI] [PubMed] [Google Scholar]
- McCabe M.P., McKern S. Quality of life and multiple sclerosis: comparison between people with multiple sclerosis and people from the general population. J. Clin. Psychol. Med. Set. 2002;9:287–295. doi: 10.1023/A:1020734901150. [DOI] [Google Scholar]
- Franklin G.M., Nelson L.M., Heaton R.K., et al. Stress and its relationship to acute exacerbations in multiple sclerosis. J. Neurol. Rehab. 1988;2:7–11. doi: 10.1177/136140968800200102. [DOI] [Google Scholar]
- Artemiadis A.K., Anagnostouli M.C., Alexopoulos E.C. Stress as a risk factor for multiple sclerosis onset or relapse: a systematic review. Neuroepidemiology. 2011;36:109–120. doi: 10.1159/000323953. [DOI] [PubMed] [Google Scholar]
- Yamout B., Itani S., Hourany R., et al. The effect of war stress on multiple sclerosis exacerbations and radiological disease activity. J. Neurol. Sci. 2010;288:42–44. doi: 10.1016/j.jns.2009.10.012. [DOI] [PubMed] [Google Scholar]
- Xie Y., Tian Z., Han F., et al. Factors associated with relapses in relapsing-remitting multiple sclerosis: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99 doi: 10.1097/MD.0000000000020885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golan D., Somer E., Dishon S., et al. Impact of exposure to war stress on exacerbations of multiple sclerosis. Ann. Neurol. 2008;64:143–148. doi: 10.1002/ana.21409. [DOI] [PubMed] [Google Scholar]
- Somer E., Golan D., Dishon S., et al. Patients with multiple sclerosis in a war zone: coping strategies associated with reduced risk for relapse. Mult. Scler. 2010;16:463–471. doi: 10.1177/1352458509358714. [DOI] [PubMed] [Google Scholar]
- Lode K., Bru E., Klevan G., Myhr K.M., et al. Coping with multiple sclerosis: a 5-year follow-up study. Acta Neurol. Scand. 2010;122:336–342. doi: 10.1111/j.1600-0404.2009.01313.x. [DOI] [PubMed] [Google Scholar]
- Maes S., Leventhal H., de Ridder D.T.D. In: Handbook of coping. MEN Zeidner., editor. John Wiley & Sons Inc; New York: 1999. Coping with chronic diseases; pp. 221–251. [Google Scholar]
- Koenig H.G. Religion, spirituality, and medicine: research findings and implications for clinical practice. South. Med. J. 2004;97:1194–1200. doi: 10.1097/01.SMJ.0000146489.21837.CE. [DOI] [PubMed] [Google Scholar]
- Bassi M., Grobberio M., Negri L., et al. The contribution of illness beliefs, coping strategies, and social support to perceived physical health and fatigue in multiple sclerosis. J. Clin. Psychol. Med. Settings. 2021;28:149–160. doi: 10.1007/s10880-019-09692-6. [DOI] [PubMed] [Google Scholar]
- Wilski M., Gabryelski J., Brola W., et al. Health-related quality of life in multiple sclerosis: Links to acceptance, coping strategies and disease severity. Disabil. Health J. 2019;12:608–614. doi: 10.1016/j.dhjo.2019.06.003. [DOI] [PubMed] [Google Scholar]
- Roubinov D.S., Turner A.P., Williams R.M. Coping among individuals with multiple sclerosis: evaluating a goodness-of-fit model. Rehabil. Psychol. 2015;60:162–168. doi: 10.1037/rep0000032. [DOI] [PubMed] [Google Scholar]
- Goretti B., Portaccio E., Zipoli V., et al. Coping strategies, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol. Sci. 2009;30:15–20. doi: 10.1007/s10072-008-0009-3. [DOI] [PubMed] [Google Scholar]
- Montel S., Spitz E., Bungener C. Coping strategies in multiple sclerosis patients with frontal cognitive disorders. Eur. Neurol. 2012;68:84–88. doi: 10.1159/000337905. [DOI] [PubMed] [Google Scholar]