Abstract
Background
Exposure to childhood adversities (CA) is associated with sleep disturbances; however, evidence has largely been drawn from cross-sectional data and has not addressed the relationship across developmental stages. Also, most studies have primarily focused on non-Hispanic White cohorts with a dearth of longitudinal evidence about racial/ethnic minorities. We examined the longitudinal association between CA and sleep disturbances in Puerto Rican youth.
Method
The Boricua Youth Study is a longitudinal study of Puerto Rican youth living in San Juan, Puerto Rico, and the South Bronx, NY (N = 2491). Among youth 5–9 and 10–16 years old, sleep disturbances were assessed through three yearly interviews. Lifetime exposure to CA included parental loss, child maltreatment, parental maladjustment, and exposure to violence. Weighted generalized linear mixed models examined the longitudinal association between CA and sleep disturbances in youth adjusting for sociodemographic and contextual covariates.
Results
The prevalence of sleep disturbances was similar in both age groups (ages 5–9 and 10–16). In multivariable mixed models, CA were associated with sleep disturbance across three Waves among 10–16-year-olds. For example, having 2–3 or ≥ 4 types of CA were related to a higher prevalence of trouble falling/staying asleep in models adjusting for social context, gender, welfare status, or mother’s education. No associations were observed among 5–9-year-olds.
Conclusion
The results suggest that cumulative adversities in childhood may lead to sleep problems in adolescence. These findings highlight the utility of addressing CA during childhood to help reduce sleep-wake disorders throughout adolescence, a known risk factor for future mental and physical health problems.
Keywords: Children, Childhood adversity, Sleep-wake disorders, Puerto Rico, Hispanic Americans
Introduction
Sleep plays a critical role in child and adolescent development. Disturbances in the quality or quantity of sleep have been linked to a range of adverse health outcomes in children and adolescents, including poor school performance [1], behavioral and cognitive problems [2], obesity and increased metabolic risk [3], substance use [4], injury [5], and mental health disorders [6]. Childhood adversity is defined as childhood experiences (< 18 years old) that threaten the child’s bodily, familial, or social safety or security, and are recognized as a crucial early life environmental component influencing a range of unfavorable outcomes across the life course [7–10]. Recent evidence suggests that childhood adversities (i.e., child maltreatment, neglect, parental separation, parental substance abuse, family dysfunction) are a significant risk factor for sleep disturbances in adults [11], but less is known about the association in children and adolescents.
To date, studies examining the relationship between childhood adversities and sleep disturbances rely largely on cross-sectional data or retrospective analyses and assess the relationship between isolated adverse childhood experiences, such as exposure to abuse or neglect [12], with sleep disturbances. These studies have observed at least a 20% greater risk of problems with sleep in adults exposed to childhood maltreatment [13], with only a few studies conducted among adolescents [14] and even fewer studies among preadolescents [15]. In the literature, many studies have failed to capture the interconnectedness of childhood adversities experienced by children when only one adversity or construct of adversity is assessed. Furthermore, childhood adversities are experienced both in- and outside of the home/family setting. Therefore, studies focusing on a narrow range of adversity types limit the scope and interpretation of findings in this area of research [16]. Considerable gaps in the literature regarding childhood adversity and sleep problems among youth still exist, but understanding whether adversities impact sleep earlier in the life course is important to developing interventions as well as understanding mechanisms that may drive these associations.
Differences in sleep disturbances may vary by developmental stage. It remains unclear whether childhood adversities negatively affect sleep across all stages of childhood development or whether there are specific developmental periods [17] when the harmful effects of adversity are most heightened. Changes in sleep follow a characteristic pathway as children grow from infants into adolescents. As children transition through different developmental stages, emergence and resolution of sleep disturbances may also fluctuate. In studies of adolescents, it has been observed that exposure to adversities compared with no exposure is associated with having insomnia [17, 18], but we do not yet know if these findings are echoed in preadolescent children. We are also unaware of any longitudinal studies of childhood adversities that assessed children at different developmental stages. Identifying and treating children with sleep disturbances early in development may be essential in reducing the adverse effects of childhood adversities in later life.
Among those who are economically disadvantaged and racial/ethnic minorities, there is a higher prevalence, and a broader range of adversities experienced [19]. Certain types of adversities (i.e., exposure to violence/crime, feeling unsafe in one’s neighborhood) are more common in minority populations and have been associated with poorer sleep quality and duration [20, 21] and insomnia symptoms [22]. Relatedly, identification of risk factors for poor health in Latinos, and specifically the influence of sleep patterns, has received limited attention [23]. Of the major US Latino subgroups, Puerto Ricans carry a disproportionate burden of health consequences and more severe consequences associated with sleep disturbances such as obesity, diabetes, and hypertension [24], and have a higher prevalence of short sleep among Hispanic/Latino subgroups. Reasons for the widening gap in health disparities between Puerto Ricans and other Hispanic/Latino Americans in the USA are not well understood, but variations between subgroups based on cultural background, socioeconomic status, and care-seeking behaviors are considered to be significant contributors [25]. However, there is a dearth of information on disparities in sleep disturbances and the role of sociocultural context in these relationships [26], especially among Latinos. Limited evidence suggests that sleep duration may be shorter [27] and subjective sleep quality may be poorer for Latino adults compared with Caucasian adults [28], with even fewer studies focusing on Latino children [29].
To address limitations in past literature and increase understanding about the relationship between childhood adversities and sleep disturbances in children, our study sought to examine the prospective association between childhood adversities and indicators of sleep disturbance in a longitudinal cohort of Puerto Rican youth. Specifically, this study contributes to the research by presenting an opportunity for understanding the developmental origins of sleep disturbances given racial/ethnic disparities in sleep and the influence of childhood adversity on sleep disturbances. We modeled the effects of childhood adversity on three separate symptoms of sleep disturbance: trouble falling/stay asleep, daytime sleepiness, and having bad dreams/nightmares, and hypothesized that childhood adversities would be associated with each factor of sleep disturbance among children. The study addressed three research questions to test this hypothesis: First, what is the prospective association between childhood adversity and sleep disturbances? Second, does the prospective association between childhood adversity and sleep disturbances differ between age groups representing key developmental periods? Finally, does sex (male and female) and social context (living in Puerto Rico or the South Bronx, NY) modify the relationship between childhood adversity and sleep disturbance among Puerto Rican youth?
Methods
Data
The Boricua Youth Study (BYS) is a longitudinal study of 2491 Puerto Rican children living in the South Bronx (n = 1138) in New York and the standard metropolitan areas of San Juan and Caguas (n = 1353) in Puerto Rico. The BYS was designed to study disruptive behavior disorders in Puerto Rican youth. The study design and procedures are detailed elsewhere [30]. In brief, the study used a representative probability sample of the study sites based on the 1990 Census. Eligible households had the following inclusion criteria: families with at least one caretaker of Puerto Rican background and the presence of a child ages 5 to 16 at Wave 1. In households with more than three children, up to three children were randomly selected. All participants provided written informed consent, and assent forms for younger children. Interviews were conducted in Spanish or English; all of the participants in Puerto Rico chose Spanish interviews. Follow-ups were conducted annually for three Waves. After three Waves, the retention rate was over 85%. The study was approved by the Institutional Review Boards at the New York State Psychiatric Institute and the University of Puerto Rico Medical Sciences Campus and procedures have been performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Measures
Exposure: Cumulative Childhood Adversities
Childhood adversity was measured from a series of parent and youth responses using questions based on items from validated scales [31–34]. Lifetime exposure to childhood adversities was measured at Wave 1 using eleven items that evaluated four childhood adversity constructs (see Supplemental Table 1): (1) youth-reported parental loss (death or divorce/separation), (2) youth-reported maltreatment (neglect and physical, sexual, and emotional abuse), (3) parental maladjustment (intimate partner violence, antisocial personality, substance use problems, emotional problems) reported by parents, and (4) youth-reported exposure to violence. These constructs overlap with the ten items that are part of the original Adverse Childhood Experiences Study [35], which focused on adverse experiences in the home. A final item (exposure to violence) was added to expand on the type of experienced childhood adversity that is relevant to urban populations [36, 37] and youth who witness, are a victim, or know someone exposed to several violent acts [38]. We assessed exposure to violence through youth’s report of being a victim of one or more violent acts. Each adversity item was coded as a binary variable.
For this study, we use the accumulation of risk conceptual model to describe how exposures in early life may affect health risk over the life course. The accumulation model postulates that correlated and independent risks can build over time to cumulatively influence health outcomes later in life [39, 40]. We hypothesize that an increasing number of adverse events across childhood will be associated with a higher prevalence of sleep disturbances; in other words, with more childhood adversities, we would expect great health risk. The number of childhood adversities was categorized into four groups to capture the effects of cumulative adversities (0 adversities, 1 adversity, 2–3 adversities, 4+ adversities) for analysis. The childhood adversity measure included in the current study is a modification of a previously constructed scale used by the BYS [36].
Outcome: Sleep Disturbances
Symptoms of sleep disturbances were assessed at each of the three Waves using parent report only for participants 5–9 years old at Wave 1 and both parent and youth report for participants 10–16 years old at Wave 1, hereafter 5–9-year-olds and 10–16-year-olds. Responses to questions in the Depression and Dysthymia sections of the DISC-4 were used to assess three types of sleep disturbances in the past year: (a) trouble falling/staying asleep (Was there a time when [the child/you] had trouble sleeping—that is, trouble falling asleep, staying asleep, or waking up too early?); (b) daytime sleepiness (Was there a time when [the child/you] slept more during the day than [he/she] usually do/does?); and (c) bad dreams/nightmares (Has there been a time when [the child/you] had a lot of bad dreams or nightmares?). Response options for each question were yes/no. We recognize that each of the sleep factors used in this study are different from one another and access different underlying sleep problems. Therefore, each sleep disturbance item was used as a separate outcome measure. To assess the effects of childhood adversity on sleep disturbances among children across both developmental periods (ages 5–9 and 10–16), the primary analysis was restricted to parental report of sleep disturbances. A separate analysis was conducted using youth-reported sleep disturbances (ages 10–16) to test the robustness of our results using parent-reported data.
Demographic factors included sociocultural context (study site), child gender and age, poverty (below or above federal poverty level), and maternal education (less than high school, high school, and college/above).
Statistical Analysis
Participants were stratified by age at Wave 1 (5–9 and 10–16 years of age) based on the sleep questionnaire reporting sources and analyses were conducted separately for each age group. Univariate analyses were conducted to examine the distribution of sleep disturbances (parental report), childhood adversities, and covariates. Generalized linear mixed models (GLIMMIX [41]) were used to test the prospective associations between childhood adversities measured at Wave 1 and the likelihood of having an indicator of sleep disturbances across three Waves. We calculated prevalence ratios (PRs) and 95% confidence intervals (CI) with Poisson regression models fit to the binary response, a random intercept for each family identity, and a nested random intercept to address the nested family study design for each subject using the GLIMMIX procedure [42]. The PR is preferable to the odds ratio when the outcome is common and allows for better interpretability, among other favorable statistical properties [42]. Each model was fully adjusted for study site, participant age, gender, poverty, mother’s age at the time of assessment, and propensity score (predicted by maternal education, family income, family structure—single versus two-parent family). Models also included an interaction term for childhood adversity and time—tests for interaction between childhood adversities and time (Wave) were statistically significant in both age groups; Type III test p < 0.01. Average adjusted prevalence ratios are reported. Two sensitivity analyses were conducted. First, we examined youth- rather than parent-report of sleep disturbances among 10–16-year-old children to gauge the robustness of the data to two different reporting sources. Second, we reran multivariable analyses stratified by three age categories (5–8, 9–12, 13–16 years) to assess possible developmental differences on measures of effect. All analyses were conducted in SAS 9.4. Descriptive statistics and longitudinal regression analyses incorporate design weights that adjust for the differential probability of selection into the study and differences in the age and gender distributions between the 1990 and the 2000 Census.
Results
Descriptive Statistics
Wave 1 characteristics of the Boricua Youth Study sample (N = 2491) are presented in Table 1 by youth age group. Overall, the distribution of characteristics was similar between 5–9- and 10–16-year-olds. The majority of participants were male (52% and 50%), living in Puerto Rico (56% and 53%), living in households not receiving welfare assistance (53% and 55%), and mothers had a high school education or higher (57% each), respectively. About 50% of both 5–9- and 10–16-year-olds had 2 or more childhood adversities.
Table 1.
Descriptive statistics for sleep quality in the study sample (n = 2491), Boricua Youth Study at Wave 1
| Total sample | Youth 5–9 years old | Youth 10–16 years old | ||||
|---|---|---|---|---|---|---|
| (N = 2491) | (N = 1220) | (N = 1271) | ||||
| Characteristics | Percentage | SE | Percentage | SE | Percentage | SE |
| Youth age (mean) | 9.23 | 0.07 | 7.11 | 0.06 | 11.57 | 0.05 |
| Gender % | ||||||
| Male | 50.92 | 1.14 | 51.64 | 1.58 | 50.11 | 1.47 |
| Female | 49.08 | 1.14 | 48.36 | 1.58 | 49.89 | 1.47 |
| Site %—unweighted | ||||||
| Bronx | 45.68 | – | 44.26 | – | 47.05 | – |
| Puerto Rico | 54.32 | – | 55.74 | – | 52.95 | – |
| Welfare statusa % | ||||||
| Yes | 45.72 | 1.99 | 46.48 | 2.45 | 44.77 | 2.51 |
| No | 54.28 | 1.99 | 53.42 | 2.45 | 55.23 | 2.51 |
| Maternal education % | ||||||
| Less than high school | 42.81 | 1.92 | 43.42 | 1.96 | 42.13 | 2.24 |
| High school | 43.04 | 1.72 | 42.61 | 1.98 | 43.51 | 2.05 |
| At least some college | 14.15 | 1.30 | 13.97 | 1.38 | 14.36 | 1.48 |
| Childhood adversitiesb | ||||||
| None | 17.01 | 1.37 | 18.35 | 2.50 | 15.53 | 1.22 |
| 1 adversity | 31.64 | 1.47 | 30.73 | 2.45 | 32.65 | 1.63 |
| 2–3 adversities | 35.43 | 1.35 | 35.03 | 2.12 | 35.86 | 1.65 |
| 4 or more adversities | 15.92 | 1.20 | 15.88 | 1.90 | 15.96 | 1.43 |
Weighted data, SE, standard error
Welfare refers to whether the youth’s biological mother was currently (at the time of the interview) receiving public assistance
Eleven types of adversities were used to evaluate four constructs of childhood adversity: (1) loss of a parent (death or divorce/separation), (2) parental maltreatment (neglect and physical, sexual, and emotional abuse), (3) parental maladjustment (intimate partner violence, antisocial personality, substance use problems, and emotional problems), and (4) environmental stressors (exposure to violence)
Figure 1 shows the prevalence of having each sleep disturbance type by Wave stratified by age group. Except for bad dreams/nightmares among the younger children (14%), the most common type of sleep disturbance was trouble falling/staying asleep, present in about 10% or more of children from both age groups. The largest developmental differences were found for daytime sleepiness from 5 to 6% in 5–9-year-olds and 8–12% in older children.
Fig. 1.
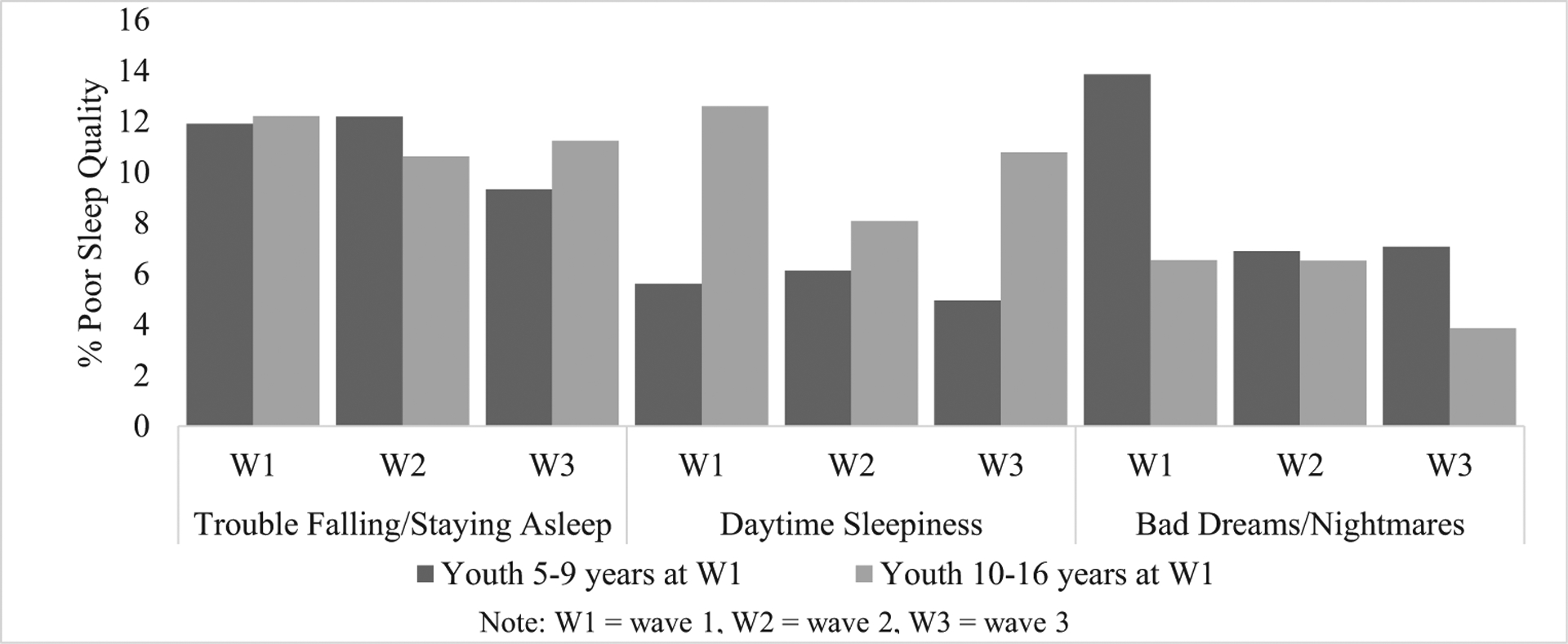
Weighted prevalence of sleep disturbances (parent report) by age group and Wave
Childhood Adversities and Sleep Disturbance
We assessed the relationship between childhood adversities and reported sleep disturbance using cross-tabulations. Table 2 shows the weighted prevalence of sleep disturbances in youth reporting on lifetime childhood adversities at Wave 1. Prevalence of trouble falling/staying asleep, daytime sleepiness, and having bad dreams/nightmares in 5–9-year-olds were not significantly different across levels of adversities. In participants 10–16 years old, those with 2 or more adversities were significantly more likely to report daytime sleepiness than experiencing bad dreams/nightmares (p < 0.01).
Table 2.
Weighted prevalence of sleep disturbances (parent report, Waves 1–3) by lifetime childhood adversities at Wave 1 (y/n)
| Childhood adversities at Wave 1 | Trouble falling/staying asleep | Daytime sleepiness | Bad dreams/nightmares |
|---|---|---|---|
| Youth age 5–9 years | |||
| 0 childhood adversities | 6.93 | 5.06 | 11.69 |
| 1 childhood adversity | 10.82 | 3.95 | 12.02 |
| 2–3 childhood adversities | 14.83 | 6.44 | 16.70 |
| 4+ childhood adversities | 13.36 | 7.59 | 13.62 |
| Rao-Scott χ2 test | p = 0.1257 | p = 0.4469 | p = 0.5200 |
| Youth age 10–16 years | |||
| 0 childhood adversities | 6.36 | 3.00 | 5.92 |
| 1 childhood adversity | 10.16 | 7.29 | 5.07 |
| 2–3 childhood adversities | 13.78 | 12.73 | 9.68 |
| 4+ childhood adversities | 16.67 | 12.48 | 10.62 |
| Rao-Scott χ2 test | p = 0.0997 | p = 0.0062 | p = 0.0963 |
In adjusted multivariable models using parent-reported sleep disturbance in youth 5–9 years old, childhood adversities were not significantly associated with higher prevalence of trouble falling/staying asleep, daytime sleepiness, or having bad dreams/nightmares (Table 3). In youth 10–16 years old, using parent-reported sleep quality, having 2–3 or ≥ 4 types of childhood adversities compared with 0 childhood adversities were related to higher prevalence of trouble falling/staying asleep across each of the three Waves in adjusted models (APR2–3CA = 3.73, 95% CI 1.52, 9.15; APR ≥4CA = 7.68, 95% CI 2.67, 22.04). Having ≥ 4 childhood adversities compared with 0 CA was related to higher prevalence of daytime sleepiness (APR≥4CA = 3.67, 95% CI 1.32, 10.23) and having bad dreams/nightmares (APR≥4CA = 3.42, 95% CI 1.04, 11.27) (Table 4). In both age groups, we tested for differences by study site and sex, but no significant differences were observed.
Table 3.
Weighted parent report of child sleep disturbance, 5–9-year-olds. Adjusted random effects longitudinal associations between childhood adversities (CA) and parent-reported sleep disturbances in youth 5–9 years, Boricua Youth Study Waves 1–3a
| Trouble falling/staying asleep | Daytime sleepiness | Bad dreams/nightmares | |||||
|---|---|---|---|---|---|---|---|
| CA at Wave 1 | APR | 95% CI | APR | 95% CI | APR | 95% CI | |
| Wave 1–3 | 0 CA | Ref. | Ref. | Ref. | |||
| 1 CA | 1.19 | 0.49–2.86 | 0.77 | 0.31–1.93 | 1.30 | 0.46–3.44 | |
| 2–3 CA | 1.35 | 0.57–3.19 | 1.04 | 0.42–2.54 | 1.39 | 0.54–3.60 | |
| 4+ CA | 1.61 | 0.57–4.54 | 1.66 | 0.58–4.77 | 1.97 | 0.64–6.08 | |
APR, adjusted prevalence ratio; models adjusted for covariates: site, gender, poverty status, and mother’s education. CA, childhood adversities; CI, confidence interval; Ref., reference group
Multivariable GLIMMIX model; binary sleep disturbance indicators. Estimates reported by Wave as CA*time were significant
Table 4.
Weighted parent report of child sleep disturbance, 10–16-year-olds. Adjusted random effects longitudinal associations between childhood adversities (CA) and parent-reported sleep disturbances in youth 10–16 years, Boricua Youth Study Waves 1–3a
| Trouble falling/staying asleep | Daytime sleepiness | Bad dreams/nightmares | |||||
|---|---|---|---|---|---|---|---|
| CA at Wave 1 | APR | 95% CI | APR | 95% CI | APR | 95% CI | |
| WAVE 1–3 | 0 CA | Ref. | Ref. | Ref. | |||
| 1 CA | 1.53 | 0.61–3.79 | 0.70 | 0.29–1.69 | 1.56 | 0.54–4.50 | |
| 2–3 CA | 3.73 | 1.52–9.15 | 2.02 | 0.85–4.80 | 2.62 | 0.94–7.34 | |
| 4+ CA | 7.68 | 2.67–22.04 | 3.67 | 1.32–10.23 | 3.42 | 1.04–11.27 | |
APR, adjusted prevalence ratio; models adjusted for covariates: site, gender, poverty status, and mother’s education. CA, childhood adversities; CI, confidence interval; Ref., reference group
Multivariable GLIMMIX model; binary sleep disturbance indicators. Estimates reported by Wave as CA*time were significant
Sensitivity Analyses
In the first sensitivity analysis, youth-reported sleep disturbances replaced parent-reported measures in multivariable models among the 10–16-year-olds. Findings were generally consistent and showed no significant differences based on informant report (Supplemental Table 2). In the second sensitivity analysis, participants were categorized into narrower age categories (5–8, 9–12, and 13–16 years) and models were reanalyzed within each age group strata to test the robustness of the results to more distinct developmental stages. The results were generally consistent with estimates reported for the broader age categories (Supplemental Table 3). Note: given the small sample size for 13–16-year-olds and response distribution for “having bad dreams/nightmares” (Wave 1 n = 19; Wave 2 n = 10; Wave 3 n = 14), the model failed to converge.
Discussion
To summarize the results, this study provides evidence that having an accumulation of childhood adversities is significantly associated with sleep disturbances (trouble falling/staying asleep, daytime sleepiness, and having bad dreams/nightmares) in youth 10–16 years of age. In general, the estimated prevalence ratios showed a dose-response relationship with increasing adversities being associated with increased risk of sleep disturbances in fully adjusted analyses. For younger children, cumulative childhood adversities were not significantly associated with any of the sleep disturbance indicators. These results extend the current knowledge on the association between adversities and sleep to a younger age group than has previously been reported [11, 18].
Sleep problems are frequent in children, and the rates observed in this study are similar to those reported in other cohort studies [17]. Our results are consistent with recent findings by Wang et al. (2016) [18], who concluded in a cross-sectional analysis that retrospective report of exposure to adversities in childhood is associated with insomnia in adolescents, a type of sleep disturbance characterized by difficulty falling or staying asleep. Our findings additionally note an association between adversities and symptoms of daytime sleepiness and having bad dreams/nightmares. Furthermore, the results are also consistent with the cumulative risk theory that constructs of childhood adversities are highly interrelated [13] and supports studying the effects of accumulation of childhood adversities on outcomes rather than focusing solely on individual childhood adversities.
We did not observe childhood adversities to be significantly associated with sleep disturbances in children 5–9 years of age. We hypothesize that the burden of sleep disturbance in youth varies by developmental stage and may contribute to our findings. Early adolescence is a developmental period marked by numerous physiological (e.g., pubertal development) and psychosocial (e.g., development of identity) changes [43], and also changes in habitual sleep patterns. Sleep duration begins to decrease from age 10 and throughout adolescence with an increased tendency to fall asleep during the day and in more severe cases, problems with insomnia [44]. These changes differ from the sleep needs and patterns of elementary school-aged children, who are commonly characterized as having fewer difficulties falling asleep or sleeping through the night compared with their sleep experiences during infancy and toddler stages, but may have an increased prevalence of parasomnias (i.e., sleepwalking, nightmares, bruxism, and enuresis) [45]. Therefore, the effect of childhood adversities on sleep disturbances may differ by age group, as has been seen in our study. Another consideration for the lack of association between childhood adversity and sleep in the younger participants may be due to the possible lack of agreement between parent report of their child’s sleep and the youth’s sleep experience. A vast literature has suggested that school-aged children may perceive their own somatic complaints very differently than their parents [46–48]. Especially as children age, parents often have less information about or lack awareness entirely of some of their child’s emotional and behavioral challenges including their child’s sleep health. Thus, considering only the parent’s perspective on sleep issues of a child may provide an incomplete assessment of the child’s experience. For participants 10 years of age and older, we were able to compare associations between childhood adversity and sleep disturbances reported by parents with sleep disturbances reported by the youth, and noted consistent findings between the two reporting sources. However, we did not ascertain self-reported sleep disturbance items among children under 10 years of age. Other possible explanations include the impact of changes in sleep architecture, hormonal changes that occur due to puberty, degree of parental involvement, and school-related stress, all of which change during early adolescence, and the role of latency or chronicity of exposure to childhood adversities [11, 48, 49]; however, we did not have the capacity to assess these factors. Finally, there may be some programming mechanism that may occur, where disruptions to sleep may result from childhood adversities when children are very young, but only appear to manifest themselves later in life (e.g., adolescence, adulthood).
A growing body of evidence from research on trauma, stress, sleep neurobiology, and psychophysiology converge to suggest that exposure to trauma in childhood evokes intense stress or fear response that causes general disruption in regular routines and ultimately sleep and circadian dysregulation [50]. There exist several plausible mechanisms that could connect childhood adversities to sleep disturbances. Substantial evidence suggests that stress due to childhood adversities elevates corticotrophin-releasing hormone (CRH), which subsequently results in hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system hyperactivity. This hyperactivity manifests itself as hyperarousal of both the physiological and neurobiological states of equilibrium, which subsequently affects homeostatic sleep quality [51]. The relationship between stress, coping strategies, and sleep remains unclear but may be crucial in understanding how older adolescents successfully transition to adulthood with regulated sleep/waking patterns despite years of dysregulated sleep during adolescence [52].
The findings from the present study must be interpreted in light of its limitations. First, sleep disturbances were assessed using three single-question survey items as opposed to a validated scale [53], and did not comprehensively measure other vital dimensions of sleep (e.g., timing, duration). Given the limited prospective data available for this topic area, we find the current indicators to be adequate to address the research questions posited in this study. Second, our indicators of sleep disturbances were taken subjectively using questionnaires and did not include objective measures (e.g., polysomnography, actigraphy). Objective measures of sleep in youth have the benefit of identifying characteristics of sleep quality and duration at different sleep stages; however, they fail at capturing the subjective sense of having a sleep problem. For example, in one study, children with depression reported sleep disturbances using sleep diaries, but these disturbances were not captured by the encephalogram measures [54]. Therefore, both forms of sleep measurements have their strengths and limitations, and our use of self-reported sleep has value in answering our research question. Other limitations include our inability to assess timing, persistence, and severity of childhood adversities as well as possible residual confounding for the associations observed between childhood adversities and sleep disturbances. For example, sharing a room with many siblings is associated with increased sleep problems [55], but we lacked data to control for these effects.
The major strengths of the present study include a large sample size selected probabilistically, the longitudinal design, and high compliance rate at follow-up. We also considered a range of sleep-related disturbances rather than a specific disorder and assessed different reporting sources, when available. The present study focused on sleep in Latinos and specifically in Puerto Rican youth, which, to our knowledge, has not been documented previously even though Puerto Ricans are the second-largest Latino minority group in the USA. While the findings need to be replicated in other settings, the results suggest that the association between childhood adversity and sleep disturbances among Puerto Rican youth emerges in early adolescence.
In conclusion, the results of this study suggest that young adolescents with a greater accumulation of childhood adversities experience sleep disturbances that persist over several years. This association is not explained by social context, gender, welfare status, and mother’s education. These early findings highlight the utility of addressing childhood adversities during early life to help reduce sleep-wake disorders throughout adolescence, a known risk factor for future mental and physical health problems. Future work may be able to build upon this evidence and help to identify factors (e.g., childhood alcohol use and depression) that may explain the relationships observed and generate targeted therapies. Intervening on the effects of childhood adversities in childhood may help to reduce or prevent sleep disturbances in later adolescence and adulthood.
Supplementary Material
Funding Information
This work is supported in part by grants from the National Institutes of Health (R01 HL125761-02S1 (April-Sanders, Suglia), MH56401 (Bird), DA033172 (Duarte), AA020191 (Duarte), MH098374 (Alegria, Canino, Duarte), HD060072 (Martins, Duarte, Canino), HL125761 (Suglia), UG3OD023328-01 (Duarte, Canino, Monk, Posner), K23 HL125748 (Alcántata)).
Abbreviations
- CA
Childhood adversities
- APR
Adjusted prevalence ratio
- CI
Confidence interval
Footnotes
The study was approved by the Institutional Review Boards at the New York State Psychiatric Institute and the University of Puerto Rico Medical Sciences Campus and procedures have been performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Conflict of Interest The authors declare that they have no conflict of interest.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s12529-020-09873-w) contains supplementary material, which is available to authorized users.
References
- 1.Titova OE, Hogenkamp PS, Jacobsson JA, Feldman I, Schioth HB, Benedict C. Associations of self-reported sleep disturbance and duration with academic failure in community-dwelling Swedish adolescents: sleep and academic performance at school. Sleep Med. 2015;16(1):87–93. [DOI] [PubMed] [Google Scholar]
- 2.James S, Hale L. Sleep duration and child well-being: a nonlinear association. J Clin Child Adolesc Psychol. 2017;46(2):258–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferranti R, Marventano S, Castellano S, Giogianni G, Nolfo F, Rametta S, et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci. 2016;9(2):117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. J Youth Adolesc. 2012;41(9):1184–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koulouglioti C, Cole R, Kitzman H. Inadequate sleep and unintentional injuries in young children. Public Health Nurs. 2008;25(2): 106–14. [DOI] [PubMed] [Google Scholar]
- 6.Sarchiapone M, Mandelli L, Carli V, Iosue M, Wasserman C, Hadlaczky G, et al. Hours of sleep in adolescents and its association with anxiety, emotional concerns, and suicidal ideation. Sleep Med. 2014;15(2):248–54. [DOI] [PubMed] [Google Scholar]
- 7.Midei AJ, Matthews KA. Interpersonal violence in childhood as a risk factor for obesity: a systematic review of the literature and proposed pathways. Obes Rev. 2011;12(5):e159–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalmakis KA, Chandler GE. Adverse childhood experiences: towards a clear conceptual meaning. J Adv Nurs. July. 2014;70(7): 1489–501. [DOI] [PubMed] [Google Scholar]
- 9.Slopen N, Koenen KC, Kubzansky LD. Cumulative adversity in childhood and emergent risk factors for long-term health. J Pediatr. 2014;164(3):631–2. [DOI] [PubMed] [Google Scholar]
- 10.Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, Danese A, et al. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation. 2018;137(5):e15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 2015;16(3):320–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poon CYM, Knight BG. Impact of childhood parental abuse and neglect on sleep problems in old age. J Gerontol Ser B Psychol Sci Soc Sci. 2011;66(3):307–10. [DOI] [PubMed] [Google Scholar]
- 13.Chapman DP, et al. Adverse childhood experiences and frequent insufficient sleep in 5 US States, 2009: a retrospective cohort study. BMC Public Health. 2013;13(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gregory AM, Caspi A, Moffitt TE, Poulton R. Family conflict in childhood: a predictor of later insomnia. Sleep. 2006;29(8):1063. [DOI] [PubMed] [Google Scholar]
- 15.Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired sleep maintenance in abused children. J Am Acad Child Adolesc Psychiatry. 1997;36(9):1236–43. [DOI] [PubMed] [Google Scholar]
- 16.Sameroff AJ, Bartko WT, Baldwin A, Baldwin C, Seifer R. Family and social influences on the development of child competence;Fam. risk,competence, Routledge; 2014, p. 171–96. [Google Scholar]
- 17.Hall Brown TS, Belcher HME, Accardo J, Minhas R, Briggs EC. Trauma exposure and sleep disturbance in a sample of youth from the National Child Traumatic Stress Network Core Data Set. Sleep Heal. 2016;2:123–8. 10.1016/j.sleh.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Raffeld MR, Slopen N, Hale L, Dunn EC. Childhood adversity and insomnia in adolescence. Sleep Med. 2016;21:12–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hale L, Hill TD, Friedman E, Nieto FJ, Galvao LW, Engelman CD, et al. Perceived neighborhood quality, sleep quality, and health status: evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simonelli G, et al. The impact of home safety on sleep in a Latin American country. Sleep Heal. 2015;1(2):98–103. [DOI] [PubMed] [Google Scholar]
- 21.Williams NJ, Knutson KL, Roberts D. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. February. 2016;18:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen-Edinboro LP, et al. Neighborhood physical disorder, social cohesion, and insomnia: results from participants over age 50 in the Health and Retirement Study. Int Psychogeriatr. 2015;27(2): 289–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel SR, Sotres-Alvarez D, Castañeda SF, Dudley KA, Gallo LC, Hernandez R, et al. Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015;38(10):1515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daviglus ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17): 1775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lucas JW, Freeman G, Adams PF. Health of Hispanic adults: United States, 2010–2014: NCHS Data Brief 2016;251:1–8. [PubMed] [Google Scholar]
- 26.Williams NJ, et al. Racial/ethnic disparities in sleep health and health care: importance of the sociocultural context. Sleep Heal. March. 2015;1(1):28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC). Perceived insufficient rest or sleep among adults-United States, 2008. MMWR Morb Mortal Wkly Rep. October. 2009;58(42):1175–9. [PubMed] [Google Scholar]
- 28.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33(7):962–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quan SF, Goodwin JL, Babar SI, Kaemingk KL, Enright PL, Rosen GM, et al. Sleep architecture in normal Caucasian and Hispanic children aged 6–11 years recorded during unattended home polysomnography: experience from the Tucson Children’s Assessment of Sleep Apnea Study (TuCASA). Sleep Med. 2003;4(1):13–9. [DOI] [PubMed] [Google Scholar]
- 30.Bird HR, Canino GJ, Davies M, Duarte CS, Febo V, Ramírez R, et al. A study of disruptive behavior disorders in Puerto Rican youth: I. Background, design, and survey methods. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1032–41. [DOI] [PubMed] [Google Scholar]
- 31.Lish JD, Weissman MM, Adams PB, Hoven CW, Bird H. Family psychiatric screening instrument for epidemiologic studies: pilot testing and validation. Psychiatry Res. 1995;57(2):169–80. [DOI] [PubMed] [Google Scholar]
- 32.Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse Negl. 1998;22(4):249–70. [DOI] [PubMed] [Google Scholar]
- 33.Finkelhor D, Dziuba-Leatherman J. Children as victims of violence: a national survey. Pediatrics. 1994;94(4):413–20. [PubMed] [Google Scholar]
- 34.Raia JA. Perceived social support and coping as moderators of effects of children’s exposure to community violence. Dissertation AbstractsInternational, 1996;56, 5181. [Google Scholar]
- 35.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–58. [DOI] [PubMed] [Google Scholar]
- 36.Ramos-Olazagasti MA, Bird HR, Canino GJ, Duarte CS. Childhood adversity and early initiation of alcohol use in two representative samples of Puerto Rican youth. J Youth Adolesc. 2017;46(1):28–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cronholm PF, et al. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. 2015;49(3):354–61. [DOI] [PubMed] [Google Scholar]
- 38.Richters JE, Martinez P. The NIMH community violence project: I. Children as victims of and witnesses to violence. Psychiatry. 1993;56(1):7–21. [DOI] [PubMed] [Google Scholar]
- 39.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–93. [PubMed] [Google Scholar]
- 40.Appleton AA, Holdsworth E, Ryan M, Tracy M. Measuring childhood adversity in life course cardiovascular research: a systematic review. Psychosom Med. 2017;79(4):434–40. [DOI] [PubMed] [Google Scholar]
- 41.Schabenberger O. Introducing the GLIMMIX procedure for generalized linear mixed models. SUGI 30 Proceedings; 2005. [Google Scholar]
- 42.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. [DOI] [PubMed] [Google Scholar]
- 43.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–84. [DOI] [PubMed] [Google Scholar]
- 44.Carskadon MA, Acebo C. Regulation of sleepiness in adolescents: update, insights, and speculation. Sleep. 2002;25(6):606–14. [DOI] [PubMed] [Google Scholar]
- 45.Pressman MR, Broughton R. NREM arousal parasomnias. Sleep Med, Springer. 2015:375–89. 10.1007/978-1-4939-2089-1. [DOI] [Google Scholar]
- 46.Owens JA, Maxim R, Nobile C, McGuinn M, Msall M. Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2000;154(6):549–55. [DOI] [PubMed] [Google Scholar]
- 47.Meltzer LJ, Avis KT, Biggs S, Amy AC, Crabtree VML, Bevans KB. The children’s report of sleep patterns (CRSP): a self-report measure of sleep for school-aged children. J Clin Sleep Med 2013;9:235–45. 10.5664/jcsm.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115(1 Suppl):241–9. [DOI] [PubMed] [Google Scholar]
- 49.Owens JA, Witmans M. Sleep problems. Curr Probl Pediatr Adolesc Health Care. April. 2004;34(4):154–79. [DOI] [PubMed] [Google Scholar]
- 50.Greenfield EA, Lee C, Friedman EL, Springer KW. Childhood abuse as a risk factor for sleep problems in adulthood: evidence from a US national study. Ann Behav Med. 2011;42(2):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.El-Sheikh M, Buckhalt JA, Keller PS, Granger DA. Children’s objective and subjective sleep disruptions: links with afternoon cortisol levels. Health Psychol. 2008;27(1):26–33. [DOI] [PubMed] [Google Scholar]
- 52.Wolfson AR. Adolescents and emerging adults’ sleep patterns: new developments. J Adolesc Health. 2010;46(2):97–9. [DOI] [PubMed] [Google Scholar]
- 53.Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33(6):781–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bertocci MA, et al. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry. 2005;44(11):1158–66. [DOI] [PubMed] [Google Scholar]
- 55.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2005;31(5):469–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


