Abstract
Background:
In an effort to improve quality and reduce costs, reimbursement for total knee arthroplasty (TKA) and total hip arthroplasty (THA) is based on the value of care provided, with adjustments for some qualifying comorbidities, including diabetes in its most severe form and excluding many diabetes codes. The study aims to examine the effects of diabetes on elective TKA or THA complication and readmission risks among Medicare beneficiaries.
Methods:
Complications (N = 521,230) and readmissions (N = 515,691) data were extracted from 2013–2014 Medicare files. Diabetes status (no diabetes, controlled-uncomplicated diabetes, controlled-complicated diabetes, and uncontrolled diabetes) was identified with ICD-9 codes. TKA or THA complications and readmissions odds based on diabetes status were estimated using logistical regression and adjusted for sociodemographic and clinical characteristics including comorbidities.
Results:
Compared to no diabetes, odds ratio (OR) of TKA complications were significant for uncontrolled diabetes, OR (95% CI) = 1.29 (1.06, 1.57). Odds of THA complications were significant for controlled-uncomplicated diabetes, 1.08 (1.00, 1.17), and controlled-complicated diabetes, 1.45 (1.17, 1.80). Readmission odds were significant for all diabetes groups (TKA: ORs = 1.21 to 1.48; THA = 1.20 to 1.70).
Conclusion:
Readmission odds were higher in all diabetes categories. The uncontrolled-diabetes group had the greatest TKA readmission and complication odds. The controlled-complicated diabetes group had the greatest THA readmission and complication odds. Findings suggest that cost adjustments in alternative payment models for arthroplasty should consider including diabetes and associated systemic complications.
Level of evidence:
Level III
INTRODUCTION
Approximately 48 to 56% of patients with diabetes develop osteoarthritis (OA) that leads to functional decline, mobility risks, and early mortality1. The current standard of care for end-stage knee or hip OA is to elect a total knee arthroplasty (TKA) or a total hip arthroplasty (THA)2,3. Joint arthroplasty surgeries account for the largest proportion of Medicare spending among all in-patient procedures4. Given that the prevalence of both diabetes and OA increases with age5, these patients are often combating the co-existing pathogenesis of OA, post-arthroplasty recovery, diabetes, and senescence6.
Although the risk of arthroplasty related complications is low, the risk increases with age and comorbidities7. Complications substantially increase the costs for arthroplasty care8,9. The Centers for Medicare and Medicaid Services (CMS) are shifting from fee-for-service to alternative payment models, such as the bundled Comprehensive Care for Joint Replacement (CJR) program, to help manage arthroplasty costs10,11. However, such payment models may be incentivizing lower extremity arthroplasty providers to select patients with fewer medical comorbidities10.
The CJR bundled payment model assigns a “target price” to an episode of care that starts at hospital admission for arthroplasty surgery and extends to 90 days following discharge10. The target price covers inpatient and outpatient services, Part B medications, durable medical equipment, and any additional medical care, which can challenge the profitability of arthroplasty when managing patients with comorbidities such as diabetes12.
The current CJR model risk adjusts the target price for comorbidities using Medicare Severity-Diagnosis Related Group (MS-DRG) codes to account for potential higher risk managements of medically complex patients15. The MS-DRG code 469 includes a major joint replacement with major complications or comorbidities (MCC), while 470 includes a major joint replacement without major complications or comorbidities10,15. A limitation of this approach is that the qualifying comorbidities for MS-DRG 469 include severe diseases that are unlikely to be medically cleared for a TKA or THA. For example, while diabetes is a risk factor for arthroplasty complications16, the disease must be severe (e.g., ketoacidosis, hyperosmolarity, and/or with coma) before it is considered an MCC17. Under the current ICD-10 diagnostic codes, over 80 codes specify various forms of uncontrolled diabetes; yet, only 13 of these codes are considered an MCC17. In a study by Marchant et al.18, patients with one or more uncontrolled diabetes ICD-9 codes had increased odds of experiencing a perioperative surgical or medical complication, mortality, or prolonged hospital stay during the indexed arthroplasty admission. No studies have examined the impact of diabetes status on peri- and postoperative outcomes among Medicare beneficiaries over 90 days – the duration of the current CJR episode of care.
The objective of this study is to examine the effects of diabetes on complication and readmission outcomes over a 90-day episode of care among Medicare fee-for-service beneficiaries receiving an elective knee or hip arthroplasty. We hypothesize that higher risks of complications and readmissions within the 90-day episode of care will be related to diabetes categories: no diabetes, controlled-uncomplicated diabetes, controlled-complicated diabetes, and uncontrolled diabetes.
METHODS
Data Source
The study examined data from Medicare beneficiaries who received elective TKA or THA in 2013 and 2014. Data were extracted and linked from the following 100% CMS files, Medicare Provider Analysis and Review (MedPAR) and Beneficiary Summary, as defined in Middleton et al7. The study was reviewed by the University Institutional Review Board. A Data Use Agreement was completed following CMS requirements.
Patient Population
Medicare fee-for-service beneficiaries who received an elective TKA or THA between January 1, 2013, and August 31, 2014, were considered for the study, N=1,013,169. Figure 1 includes details on cohort selection. Cases were screened with the inclusion criteria: age 65 years and older, continuous Part A coverage for a minimum of 6-months before arthroplasty, and surgery performed within the United States (i.e., not a territory). For beneficiaries with more than one arthroplasty meeting study criteria, one randomly selected TKA or THA was included. Cases with pre-arthroplasty admittance from a long-term care nursing home, lack of continuous Part A coverage within 90 days or until death following arthroplasty, and non-planned arthroplasty were excluded.
Figure 1.
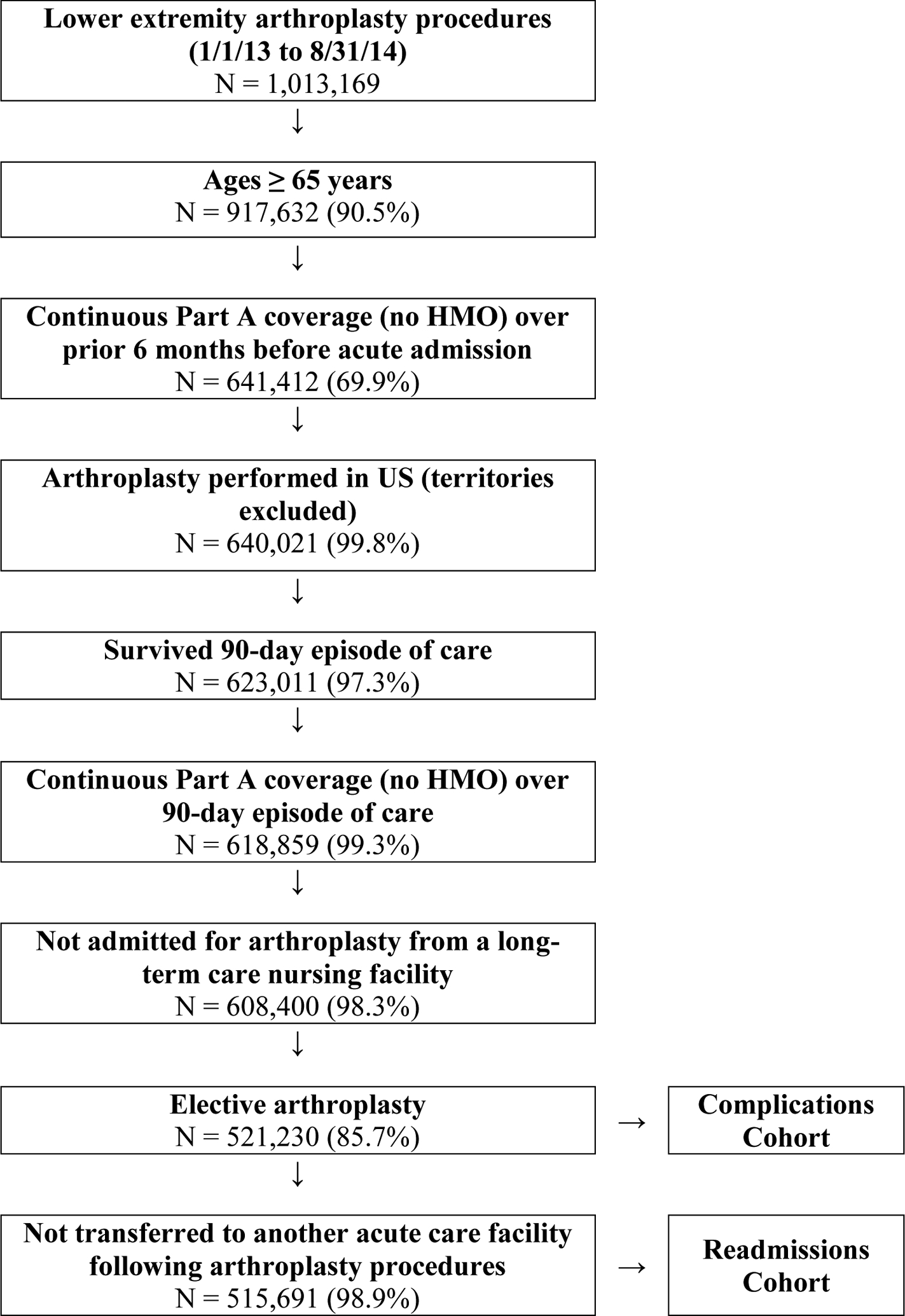
Cohort selection. Number of cases eligible per criteria applied. Percentages represent the remaining proportion from the previous criteria. HMO, health maintenance organization; US, United states.
Diabetes status were stratified into four groups (no diabetes, controlled-uncomplicated diabetes, controlled-complicated diabetes, and uncontrolled diabetes) using ICD-9 codes (Appendix A). The no diabetes group was defined by the absence of diabetes ICD-9 codes. The controlled-uncomplicated group included those having controlled diabetes without diabetic complications. The controlled-complicated group was defined as having controlled diabetes with diabetic complications. The uncontrolled group included those with uncontrolled diabetes.
A total of 521,230 beneficiaries were included in our assessment of complications within the TKA or THA episode of care (Figure 1). To examine 90-day readmissions, we excluded claims data of beneficiaries who transferred between acute settings. A total of 515,691 beneficiaries were included in our assessment of 90-day readmissions following a TKA or a THA.
Outcomes
Complications
Information on complications occurring within the TKA or THA episode of care was extracted from MedPAR files as defined by the Hospital-Level Risk-Standardized Complication Rate Following Elective Primary Total Hip Arthroplasty and/or Total Knee Arthroplasty Algorithm, Version 5.019. This measure of medical and surgical complications is a quality measure collected at medical facilities participating in the CJR program. The windows for monitoring complications differ by complication type. Providers are accountable for complications that occur from hospital admission for arthroplasty to 1) seven-days for myocardial infarction (AMI), pneumonia, and sepsis/septicemia/shock; 2) 30-days for bleeding and pulmonary embolism, and 3) 90-days for mechanical complications and periprosthetic joint infection/wound infection19. Complications were dichotomized as “yes” or “no”. Patients were marked as “yes” for experiencing a complication if one or more conditions were reported within the timeframe.
Readmission
Claims for readmissions within 90-days following hospital discharge were extracted from MedPAR files. Readmissions were dichotomized as “yes” or “no”. Reasons for the first readmission were documented based on the ICD-9 code reported for the primary diagnosis. Complications occurring after discharge resulting in rehospitalization were considered readmissions.
Patient Characteristics
Sociodemographic characteristics extracted from the Beneficiary Summary file included: age, sex (male/female), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), disability entitlement (disability original reason for Medicare, yes/no), and dual eligibility (Medicare and Medicaid eligible, yes/no).
Claims data extracted from MedPAR included: comorbidities, number of hospitalizations over the 6 months prior to arthroplasty, intensive or coronary care unit utilization (ICU/CCU) during index hospitalization, and length of stay. Non-diabetes related comorbidities were categorized and listed using the Elixhauser approach (Appendices B and C), which was developed to use with administrative datasets and accounts for 31 conditions that most likely impact healthcare utilization and/or mortality20,21.
Data Analysis
Complication and readmission rates were calculated for the TKA and THA cohorts sub-grouped by diabetes status (no diabetes, controlled-uncomplicated, controlled-complicated, and uncontrolled). Complications and readmissions of each diabetes group were compared to the no diabetes group using logistical regression that adjusted for sociodemographic and clinical characteristics including comorbidities. Odds ratios (OR) with 95% confidence intervals (CI) greater than 1.0 suggested significantly higher risks.
RESULTS
A total of 355,155 TKAs and 166,075 THAs met study criteria and were included in the complications cohort (Table 1). For TKAs, the prevalence of controlled-uncomplicated diabetes was 20.6% (n = 73,065), controlled-complicated diabetes was 1.4% (n = 5,127), and uncontrolled diabetes was 0.9% (n = 3,167) (Table 1). For THA, the complication cohort included 15.4% (n = 25,547) with controlled-uncomplicated diabetes, 1.0% (n = 1,731) with controlled-complicated diabetes, and 0.6% (n = 940) with uncontrolled diabetes (Table 1).
Table 1.
Complications by arthroplasty type
| Characteristic | Knee Arthroplasty | Hip Arthroplasty | ||
|---|---|---|---|---|
| N (%) | Complications (95% CI) | N (%) | Complications (95% CI) | |
| Overall | 355,155 | 2.1% (2.0, 2.1) | 166,075 | 3.0% (2.9, 3.0) |
| Sex | ||||
| Male | 129,242 (36.4%) | 2.3% (2.2, 2.3) | 64,459 (38.8%) | 2.8% (2.7, 2.9) |
| Female | 225,913 (63.6%) | 2.0% (1.9, 2.0) | 101,616 (61.2%) | 3.1% (3.0, 3.2) |
| Age, years | ||||
| 65–69 | 113,253 (31.9%) | 1.8% (1.7, 1.8) | 49,398 (29.7%) | 2.4% (2.3, 2.6) |
| 70–74 | 104,256 (29.4%) | 2.0% (1.9, 2.0) | 45,771 (27.6%) | 2.8% (2.6, 2.9) |
| 75–79 | 77,650 (21.9%) | 2.3% (2.2, 2.4) | 35,342 (21.3%) | 3.1% (2.9, 3.2) |
| 80–84 | 43,066 (12.1%) | 2.6% (2.4, 2.7) | 23,330 (14.0%) | 3.7% (3.4, 3.9) |
| ≥85 | 16,930 (4.8%) | 3.0% (2.7, 3.3) | 12,234 (7.4%) | 4.0% (3.7, 4.4) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 313,403 (88.2%) | 2.1% (2.0, 2.1) | 152,090 (91.6%) | 3.0% (2.9, 3.1) |
| Non-Hispanic Black | 17,956 (5.1%) | 2.4% (2.2, 2.6) | 7,363 (4.4%) | 3.0% (2.6, 3.4) |
| Hispanic | 13,466 (3.8%) | 2.1% (1.8, 2.3) | 3,067 (1.8%) | 2.6% (2.0, 3.1) |
| Other | 10,330 (2.9%) | 1.8% (1.6, 2.1) | 3,555 (2.1%) | 2.4% (1.9, 3.0) |
| Disability entitlement a | ||||
| No | 323,698 (91.1%) | 2.0% (2.0, 2.1) | 153,743 (92.6%) | 2.8% (2.7, 2.9) |
| Yes | 31,457 (8.9%) | 2.8% (2.7, 3.0) | 12,332 (7.4%) | 4.9% (4.5, 5.3) |
| Dual eligibility b | ||||
| No | 328,085 (92.4%) | 2.0% (2.0, 2.1) | 156,776 (94.4%) | 2.8% (2.8, 2.9) |
| Yes | 27,070 (7.6%) | 3.0% (2.8, 3.2) | 9,299 (5.6%) | 4.7% (4.3, 5.2) |
| Prior hospitalization | ||||
| 0 | 326,687 (92.0%) | 2.0% (2.0, 2.1) | 151,503 (91.2%) | 2.9% (2.8, 2.9) |
| 1 | 25,836 (7.3%) | 2.6% (2.4, 2.7) | 12,787 (7.7%) | 3.7% (3.4, 4.1) |
| 2 | 2,231 (0.6%) | 4.1% (3.3, 4.9) | 1,473 (0.9%) | 5.6% (4.5, 6.8) |
| 3+ | 401 (0.1%) | 4.5% (2.5, 6.5) | 312 (0.2%) | 7.7% (4.7, 10.6) |
| Hospital LOS, days c | ||||
| <4 | 299,750 (84.4%) | 1.2% (1.1, 1.2) | 141,110 (85.0%) | 2.1% (2.1, 2.2) |
| 4–7 | 52,398 (14.8%) | 5.5% (5.3, 5.7) | 23,411 (14.1%) | 6.0% (5.7, 6.3) |
| 8+ | 3,007 (0.8%) | 34.0% (32.3, 35.7) | 1,554 (0.9%) | 29.9% (27.6, 32.1) |
| ICU/CCU d | ||||
| No | 340,417 (95.9%) | 1.7% (1.7, 1.8) | 158,344 (95.3%) | 2.6% (2.5, 2.7) |
| Yes | 14,738 (4.1%) | 10.1% (9.6, 10.6) | 7,731 (4.7%) | 10.6% (9.9, 11.3) |
| Diabetes Status | ||||
| None | 273,805 (77.1%) | 2.0% (1.9, 2.0) | 137,858 (83.0%) | 2.8% (2.7, 2.9) |
| Controlled – Uncomplicated | 73,056 (20.6%) | 2.4% (2.3, 2.5) | 25,546 (15.4%) | 3.5% (3.3, 3.8) |
| Controlled – Complicated | 5,127 (1.4%) | 3.7% (3.2, 4.2) | 1,731 (1.0%) | 6.0% (4.8, 7.1) |
| Uncontrolled | 3,167 (0.9%) | 4.3% (3.6, 5.0) | 940 (0.6%) | 5.6% (4.2, 7.1) |
Abbreviations: LOS = length of stay, ICU/CCU = intensive care unit/coronary care unit
“Disability” original reason for receiving Medicare.
Eligible for Medicare and Medicaid.
LOS for hospitalization during joint arthroplasty procedure
Admitted to ICU or CCU during hospitalization for joint arthroplasty procedure.
Complications
Complication rates were 2.1% (95% CI, 2.0, 2.1) for TKA and 3.0% (2.9, 3.0) for THA (Table 1). Leading TKA complications included pulmonary embolism, pneumonia, and periprosthetic joint and wound infection (Table 2). Leading THA complication were mechanical complications, pneumonia, and infections (Table 3).
Table 2:
Total knee arthroplasty (TKA) complications stratified by diabetes status
| Complication | No Diabetes | Controlled-Uncomplicated | Controlled-Complicated | Uncontrolled |
|---|---|---|---|---|
| Any Complication | 5343 (2.0%) | 1,740 (2.4%) | 191 (3.7%) | 137 (4.3%) |
| AMI | 432 (0.2%) | 199 (0.3%) | 24 (0.5%) | 20 (0.6%) |
| Pulmonary embolism | 1,701 (0.6%) | 456 (0.6%) | 48 (0.9%) | 35 (1.1%) |
| Mechanical complications | 525 (0.2%) | 154 (0.2%) | 14 (0.3%) | * |
| Pneumonia | 1,422 (0.5%) | 454 (0.6%) | 60 (1.2%) | 34 (1.1%) |
| Sepsis/septicemia/shock | 354 (0.1%) | 129 (0.2%) | 24 (0.5%) | 23 (0.7%) |
| Surgical site bleeding | 80 (0.0%) | 24 (0.0%) | * | * |
| Joint or wound infection | 1,183 (0.4%) | 440 (0.6%) | 35 (0.7%) | 34 (1.1%) |
Represents n < 11 experiencing the complication
AMI = myocardial infarction
Values represent n (%) of each diabetes group experiencing complications from hospital admission for TKA to 7-days for AMI, pneumonia, and sepsis/septicemia/shock; 30-days for bleeding and pulmonary embolism, and 90-days for mechanical complications and periprosthetic joint infection/wound infection as defined by the Hospital-Level Risk-Standardized Complication Rate Following Elective Primary Total Hip Arthroplasty and/or Total Knee Arthroplasty Algorithm, Version 5.019
Table 3:
Total hip arthroplasty (THA) complications stratified by diabetes status
| Complication | No Diabetes | Controlled-Uncomplicated | Controlled-Complicated | Uncontrolled |
|---|---|---|---|---|
| Any Complication | 3,849 (2.8%) | 903 (3.5%) | 103 (6.0%) | 53 (5.6%) |
| AMI | 270 (0.2%) | 84 (0.3%) | 12 (0.7%) | * |
| Pulmonary embolism | 384 (0.3%) | 73 (0.3%) | * | * |
| Mechanical complications | 1,694 (1.2%) | 333 (1.3%) | 46 (2.7%) | 14 (1.5%) |
| Pneumonia | 575 (0.4%) | 166 (0.6%) | 21 (1.2%) | 14 (1.5%) |
| Sepsis/septicemia/shock | 297 (0.2%) | 61 (0.2%) | * | * |
| Surgical site bleeding | 91 (0.1%) | 26 (0.1%) | * | * |
| Joint or wound infection | 760 (0.6%) | 222 (0.9%) | 18 (1.0%) | 14 (1.5%) |
Represents n < 11 experiencing the complication
AMI = myocardial infarction
Values represent n (%) of each diabetes group experiencing complications from hospital admission for THA to 7-days for AMI, pneumonia, and sepsis/septicemia/shock; 30-days for bleeding and pulmonary embolism, and 90-days for mechanical complications and periprosthetic joint infection/wound infection as defined by the Hospital-Level Risk-Standardized Complication Rate Following Elective Primary Total Hip Arthroplasty and/or Total Knee Arthroplasty Algorithm, Version 5.019
The odds of TKA complications, when compared to the no diabetes group, were significant and the highest for those with uncontrolled diabetes, OR (95% CI) = 1.27 (1.04, 1.55) (Table 4). The odds of THA complications were significant and the highest for controlled-complicated diabetes, OR = 1.45 (1.17, 1.80) and followed by controlled-uncomplicated diabetes, OR = 1.08 (1.0, 1.17) (Table 4). The odds of TKA complications for those with controlled-uncomplicated and controlled-complicated diabetes and the odds of THA complications for uncontrolled diabetes were not significant (Table 4).
Table 4:
Odds for 90-day arthroplasty complications or readmissions stratified by diabetes status
| Knee Arthroplasty | Hip Arthroplasty | |||
|---|---|---|---|---|
| Complications OR (95% CI) | Readmission OR (95% CI) | Complications OR (95% CI) | Readmission OR (95% CI) | |
| Diabetes | ||||
| No Diabetesa | Reference | Reference | Reference | Reference |
| Controlled- Uncomplicated | 1.04 (0.98 – 1.11) | 1.21 (1.17 – 1.25)* | 1.08 (1.00 – 1.17) | 1.20 (1.14 – 1.26)* |
| Controlled- Complicated | 1.02 (0.86 – 1.20) | 1.44 (1.31 – 1.58)* | 1.45 (1.17 – 1.80)* | 1.70 (1.48 – 1.96)* |
| Uncontrolled | 1.29 (1.06 – 1.57)* | 1.48 (1.31 – 1.66)* | 1.26 (0.94 – 1.71) | 1.44 (1.17 – 1.77)* |
OR = odds ratio; CI = confidence interval
Results from multivariate, adjusted analyses.
Indicates statistically significant odds, defined as OR ≥ 1.0 and 95% CI not crossing 1.0
The no diabetes group served as the reference group for all group comparisons to calculate odds of complications and readmissions.
Readmission
The readmissions cohort included 98.9% of those receiving an elective arthroplasty (Figure 1) with a total of 351,183 TKA and 164,508 THA cases that met criteria (Table 5).
Table 5.
Unplanned readmissions over 90-days episode of care by arthroplasty type
| Characteristic | Knee Arthroplasty | Hip Arthroplasty | ||
|---|---|---|---|---|
| N (%) | Readmission (95% CI) | N (%) | Readmission (95% CI) | |
| Overall | 351,183 | 6.3% (6.2, 6.4) | 164,508 | 7.0% (6.9, 7.1) |
| Sex | ||||
| Male | 127,799 (36.4%) | 6.8% (6.7, 6.9) | 63,860 (38.8%) | 6.9% (6.7, 7.1) |
| Female | 223,384 (63.6%) | 6.1% (6.0, 6.2) | 100,648 (61.2%) | 7.1% (6.9, 7.3) |
| Age, years | ||||
| 65–69 | 112,283 (32.0%) | 4.7% (4.6, 4.9) | 49,056 (29.8%) | 5.1% (4.9, 5.3) |
| 70–74 | 103,095 (29.4%) | 5.6% (5.5, 5.7) | 45,391 (27.6%) | 6.0% (5.8, 6.2) |
| 75–79 | 76,664 (21.8%) | 7.2% (7.0, 7.3) | 34,933 (21.2%) | 7.7% (7.4, 8.0) |
| 80–84 | 42,401 (12.1%) | 8.8% (8.6, 9.1) | 23,032 (14.0%) | 9.4% (9.1, 9.8) |
| ≥85 | 16,740 (4.8%) | 11.3% (10.8, 11.8) | 12,096 (7.4%) | 12.1% (11.5, 12.7) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 310,029 (88.3%) | 6.2% (6.2, 6.3) | 150,707 (91.6%) | 7.0% (6.9, 7.2) |
| Non-Hispanic Black | 17,576 (5.0%) | 8.1% (7.7, 8.5) | 7,232 (4.4%) | 8.1% (7.5, 8.7) |
| Hispanic | 13,360 (3.8%) | 6.4% (6.0, 6.8) | 3,044 (1.9%) | 6.4% (5.5, 7.2) |
| Other | 10,218 (2.9%) | 5.7% (5.2, 6.1) | 3,525 (2.1%) | 4.9% (4.2, 5.7) |
| Disability entitlement a | ||||
| No | 320,125 (91.2%) | 6.0% (5.9, 6.1) | 152,317 (92.6%) | 6.7% (6.5, 6.8) |
| Yes | 31,058 (8.8%) | 9.5% (9.1, 9.8) | 12,191 (7.4%) | 11.3% (10.8, 11.9) |
| Dual eligibility b | ||||
| No | 324,423 (92.4%) | 6.0% (6.0, 6.1) | 155,315 (94.4%) | 6.8% (6.6, 6.9) |
| Yes | 26,760 (7.6%) | 9.8% (9.4, 10.2) | 9,193 (5.6%) | 11.2% (10.6, 11.9) |
| Prior hospitalization | ||||
| 0 | 323,093 (92.0%) | 6.0% (5.9, 6.1) | 150,112 (91.2%) | 6.6% (6.5, 6.7) |
| 1 | 25,581 (7.3%) | 9.5% (9.1, 9.8) | 12,651 (7.7%) | 10.1% (9.6, 10.7) |
| 2 | 2,124 (0.6%) | 16.3% (14.8, 17.9) | 1,439 (0.9%) | 18.7% (16.7, 20.7) |
| 3+ | 385 (0.1%) | 29.9% (25.3, 34.4) | 306 (0.2%) | 30.1% (24.9, 35.2) |
| Hospital LOS, days c | ||||
| <4 | 296,634 (84.5%) | 5.6% (5.5, 5.7) | 139,849 (85.0%) | 6.2% (6.1, 6.3) |
| 4–7 | 51,597 (14.7%) | 9.7% (9.5, 10.0) | 23,138 (14.1%) | 10.9% (10.5, 11.3) |
| 8+ | 2,952 (0.8%) | 21.0% (19.5, 22.5) | 1,521 (0.9%) | 21.7% (19.6, 23.8) |
| ICU/CCU d | ||||
| No | 336,649 (95.9%) | 6.2% (6.1, 6.2) | 156,869 (95.4%) | 6.8% (6.7, 6.9) |
| Yes | 14,534 (4.1%) | 10.0% (9.5, 10.4) | 7,639 (4.6%) | 11.9% (11.2, 12.6) |
| Diabetes Status | ||||
| None | 270,889 (77.1%) | 5.8% (5.7, 5.9) | 136,621 (83.0%) | 6.6% (6.4, 6.7) |
| Controlled – Uncomplicated | 72,137 (20.5%) | 7.6% (7.4, 7.8) | 25,244 (15.3%) | 8.8% (8.5, 9.2) |
| Controlled – Complicated | 5,031 (1.4%) | 11.5% (10.6, 12.4) | 1,712 (1.0%) | 14.7% (13.0, 16.4) |
| Uncontrolled | 3,126 (0.9%) | 10.6% (9.5, 11.7) | 931 (0.6%) | 12.0% (9.9, 14.1) |
Abbreviations: LOS = length of stay, ICU/CCU = intensive care unit/coronary care unit
“Disability” original reason for receiving Medicare.
Eligible for Medicare and Medicaid.
LOS for hospitalization during joint arthroplasty procedure
Admitted to ICU or CCU during hospitalization for joint arthroplasty procedure.
The odds of readmission were significant for all diabetes groups when compared to the no diabetes group for both TKA and THA (Table 4). For TKA, the uncontrolled diabetes group had the highest readmissions odds, OR = 1.48 (1.31, 1.66), followed by controlled-complicated diabetes, OR = 1.44 (1.31, 1.58), and then controlled-uncomplicated diabetes, OR = 1.21 (1.17, 1.25) (Table 4). For THA, the readmission odds were the highest for those with controlled-complicated diabetes, OR = 1.70 (1.48, 1.96), followed by uncontrolled diabetes, OR = 1.44 (1.17, 1.77) and then controlled-uncomplicated diabetes, OR = 1.20 (1.14, 1.26) (Table 4).
DISCUSSION
The purpose of this study was to examine elective TKA or THA complications and readmissions risks within 90-day episodes of care for Medicare beneficiaries with varying levels of diabetes severity. Compared to those without diabetes, statistically greater odds were observed for TKA and THA readmissions among all diabetes groups, TKA complications for uncontrolled diabetes, and THA complications for controlled-complicated and -uncomplicated diabetes. Although this was the first known study to examine complications and readmissions over a 90-day arthroplasty-related episode of care based on diabetes presence among Medicare beneficiaries, the findings paralleled previous results of studies that examined similar outcomes under a 30-day episode of care18. These findings support that while the CJR programs are showing promise to reduce costs, excluding certain comorbidities from cost adjustment are less appropriate for TKA and THA programs.
Consistent with our hypothesis, the results found that Medicare beneficiaries with diabetes, regardless of severity, were at higher risks for TKA or THA readmissions than the no diabetes group. This finding is consistent with previous studies that identify diabetes as an independent predictor of readmissions under the 30-day episode of care18,22. With the CJR’s, health care facilities with high rates of readmissions may experience financial penalties. These penalties may be reduced with risk adjustment for high-cost patients based on qualified comorbidities defined by the MCC list. Unfortunately, this MCC list was adopted from comprehensive care for cardiac patients and appeared to be less appropriate for elective arthroplasty procedures. The current MCC list includes diabetes in its most severe forms that would usually be medically disqualified for elective arthroplasty. Potential lack of medical clearance may explain the notably small prevalence of uncontrolled and controlled-complicated diabetes (i.e., < 2%) found in this study. The current MCC list is limited to 13 uncontrolled diabetes codes with diagnoses like glycemic coma. Perhaps revising the MCC list to account for less severe diabetes codes and associated systemic complications would be more logical.
Unexpectedly, beneficiaries with controlled-complicated diabetes had the largest odds for THA readmissions and complications of all groups, and the risks for TKA readmissions were comparable to uncontrolled diabetes. Diabetes control is primarily evaluated by blood glucose levels. Elevated preoperative blood glucose levels are of concern because surgery can induce intraoperative physiological stress responses that further tax glucose levels and increase complication risks23. For those with controlled-complicated diabetes, associated TKA or THA complications may yield similar consequences but without the same clinical monitoring and follow-ups as those with uncontrolled glucose control. Perhaps preoperative screening and peri- and postoperative management, if not already, need to extend beyond blood glucose levels and consider associated diabetic complications. The controlled-complicated DM subgroup warrants further research, careful clinical considerations, and adding this sub-group to the MCC list can help account for the increased costs associated with comprehensive TKA or THA management.
Interestingly, uncontrolled diabetes yielded odds for THA complications, but the wide 95% CI that crossed 1 suggested that such risks were not significantly greater than the no diabetes group. The lack of statistical significance may be explained by a small prevalence of uncontrolled diabetes among the THA complications cohort, the predetermined study criteria, and the complication types. The uncontrolled diabetes group made up of 0.6% of the THA complication cohort, of which 53 beneficiaries or 12% experienced a complication. The small sample may be attributed to the predetermined selection criteria for elective THAs. Patients with diabetes, especially when uncontrolled, are at high risk for fractures that require non-elective THAs24,25, which was excluded from the current study. This may limit the number of individuals with uncontrolled diabetes receiving elective THA in our cohort or pre-select healthier individuals for the uncontrolled diabetes sub-group. In fact, the leading THA complications were joint-related, including mechanical complications and infection. Unlike the THA cohort, TKA complications were highest among those with uncontrolled diabetes and included primarily medical issues, including pulmonary embolism, pneumonia, and infection. Perhaps precipitating factors of poor glycemic control combined with the physiological response of surgery may be increasing the risks of medical complications related to a TKA. Based on these findings, it would be reasonable to defer surgery for those with uncontrolled diabetes to achieve glycemic control, as this is a modifiable risk factor. Future studies would benefit from further examining precipitating factors that may increase complication risks with a larger elective arthroplasty cohort of patients with uncontrolled diabetes.
The study has several limitations. First, we included ICD-9 codes for primary (250.xx) and secondary (249.xx) diabetes, which may cause other medical conditions, and not necessarily diabetes, to be the precipitating complication or readmission mechanism. (Appendix A). To limit this potential effect, we statistically controlled for demographics, comorbidities, and other clinical factors and limited TKAs and THAs to elective procedures. Elective TKA and THA requires medical stability, severe joint arthritis, and pain related disability. Meanwhile, 249.xx codes accounted for 149 beneficiaries or 0.2% of the sample. Including both primary and secondary codes allow the full presence and effects of diabetes to be examined. The study design combined with the statistical control of comorbidities should minimize the impact of other diseases on our results.
Also, the uncontrolled diabetes group accounted for 0.6% of the sample but the highest odds for TKA complications and readmissions. The small prevalence but statistically significant odds may limit the clinical relevance of these findings. However, the prevalence of diabetes ranged between 22.9% and 17% of the elective TKA and THA cohorts, respectively, and those with diabetes accounted for at least a quarter of those with complications or readmissions. We used 95% CI that did not cross 1.0 to identify statistically significant odds ratios. A large odds ratio with a wide 95% CI, as in uncontrolled diabetes for THA complications, were not considered significant. Further, this study is clinically relevant, because it examines the effect of diabetes, as an overall diagnosis and comprehensively per diabetes severity, on elective TKA and THA outcomes.
Other limitations include not examining other subgroups, postoperative rehabilitation, or diseases that commonly cluster with diabetes. The analyses include fee-for-service beneficiaries receiving elective TKA or THA not admitted from institutional settings (e.g., long-term care facilities), which could impact the results and not reflect the entire Medicare beneficiary population. Further, Medicare beneficiaries are a subset of the United States’ population, potentially limiting the applicability of the study’s findings to non-Medicare users (i.e., non-citizens, other countries, or users of other payor sources). Although other samples are not included in this data, the results can help inform clinicians and patients of expectations. Research that targets long-term care facilities, non-elective joint arthroplasty, and/or sub-group analyses for rehabilitative protocol, co-existing diseases, different countries and/or payer sources are important factors to consider for future research. For the current study, exploring such confounding factors, while necessary and important, were beyond the scope of this project. Current findings provide the foundation for future studies to examine other high prevalence comorbidities and disease clusters in this population.
Our results indicate that the odds of hospital readmission and complications following an elective TKA and THA are increased for Medicare beneficiaries with diabetes. The findings suggest that diabetes and associated systemic complications should be included in the DRG codes used for risk adjustment in the CJR program. Additional research is needed to replicate our results and better understand how the level of diabetic control and severity are related to quality measures and performance-based outcomes associated with CJR and other value-based payment programs associated with health care reform.
Supplementary Material
GRANTS AND ACKLNOWLDGEMENTS:
This study was supported with funding from the National Institutes of Health (P2C-HD065702, R01-HD069443, P30-AG024832, K12-HD055929, KL2-TR001452, UL1-TR001450), the Agency for Healthcare Quality and Research (T32-HS26133), and the National Institute on Disability, Independent Living and Rehabilitation Research (H90AR5009).
Contributor Information
Annalisa Na, Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, Texas; Department of Physical Therapy and Rehabilitation Sciences, Drexel University, Philadelphia, Pennsylvania.
Addie Middleton, New England Geriatric Research Education and Clinical Center, VA Boston Healthcare System, Boston, Massachusetts.
Allen Haas, Office of Biostatistics, University of Texas Medical Branch (UTMB), Galveston, Texas.
James Graham, Department of Occupational Therapy, Colorado State University, Fort Collins, Colorado.
Kenneth J. Ottenbacher, Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, Texas.
References
- 1.Bolen J, Hootman J, Helmick CG, Murphy L, Langmaid G, Caspersen CJ. Arthritis as a potential barrier to physical activity among adults with diabetes -- United States, 2005 and 2007. Morb Mortaility Wkly Rep. 2008;57(18):486–489. doi:mm5718a3 [pii] [PubMed] [Google Scholar]
- 2.Gossec L, Paternotte S, JF M, et al. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthr Cartil. 2011;19(2):147–154. doi: 10.1016/j.joca.2010.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Löfvendahl S, Bizjajeva S, Ranstam J, Lidgren L. Indications for hip and knee replacement in Sweden. J Eval Clin Pract. 2011;17(2):251–260. doi: 10.1111/j.1365-2753.2010.01430.x [DOI] [PubMed] [Google Scholar]
- 4.“Centers for Disease Control and Prevention.” National hospital discharge survey: 2010 table, procedures by selected patient characteristics. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf. Published 2013. [Google Scholar]
- 5.Courties A, Sellam J. Osteoarthritis and type 2 diabetes mellitus: What are the links? Diabetes Res Clin Pract. 2016;122:198–206. doi: 10.1016/j.diabres.2016.10.021 [DOI] [PubMed] [Google Scholar]
- 6.Nielen JTH, Emans PJ, Dagnelie PC, et al. Severity of Diabetes Mellitus and Total Hip or Knee Replacement: A Population-Based Case-Control Study. Medicine (Baltimore). 2016;95(20):e3739. doi: 10.1097/MD.0000000000003739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Middleton A, Lin Y-L, Graham JE, Ottenbacher KJ. Outcomes Over 90-Day Episodes of Care in Medicare Fee-for-Service Beneficiaries Receiving Joint Arthroplasty. J Arthroplasty. 2017;32(9):2639–2647.e1. doi: 10.1016/j.arth.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis DE, Paxton ES, Maltenfort M, Abboud J. Factors affecting hospital charges after total shoulder arthroplasty: an evaluation of the National Inpatient Sample database. J shoulder Elb Surg. 2014;23(12):1860–1866. doi: 10.1016/j.jse.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 9.Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee G-C. Should All Patients Be Included in Alternative Payment Models for Primary Total Hip Arthroplasty and Total Knee Arthroplasty? J Arthroplasty. 2016;31(9 Suppl):45–49. doi: 10.1016/j.arth.2016.03.020 [DOI] [PubMed] [Google Scholar]
- 10.McLawhorn AS, Buller LT. Bundled Payments in Total Joint Replacement: Keeping Our Care Affordable and High in Quality. Curr Rev Musculoskelet Med. 2017;10(3):370–377. doi: 10.1007/s12178-017-9423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nwachukwu BU, O’Donnell E, McLawhorn AS, Cross MB. Episode of Care Payments in Total Joint Arthroplasty and Cost Minimization Strategies. HSS J ®. 2016;12(1):91–93. doi: 10.1007/s11420-015-9460-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare Program; Comprehensive Care for Joint Replacement Payment Model for Acute Care Hospitals Furnishing Lower Extremity Joint Replacement Services. Final rule. Fed Regist. 2015;80(226):73273–73554. http://www.ncbi.nlm.nih.gov/pubmed/26606762.AccessedMay 22, 2019. [PubMed] [Google Scholar]
- 13.Jubelt LE, Goldfeld KS, Blecker SB, et al. Early Lessons on Bundled Payment at an Academic Medical Center. J Am Acad Orthop Surg. 2017;25(9):654–663. doi: 10.5435/JAAOS-D-16-00626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ponnusamy KE, Naseer Z, El Dafrawy MH, et al. Post-Discharge Care Duration, Charges, and Outcomes Among Medicare Patients After Primary Total Hip and Knee Arthroplasty. J Bone Jt Surg. 2017;99(11):e55. doi: 10.2106/JBJS.16.00166 [DOI] [PubMed] [Google Scholar]
- 15.Center for Medicare & Medicaid Services. Major Joint Replacement (Hip or Knee). https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/jointreplacement-ICN909065Printfriendly.pdf.Published2017.
- 16.McGrory BJ, Weber KL, Jevsevar DS, Sevarino K. Surgical Management of Osteoarthritis of the Knee: Evidence-based Guideline. J Am Acad Orthop Surg. 2016;24(8):e87–93. doi: 10.5435/JAAOS-D-16-00159 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Draft ICD-10-CM/PCS MS-DRGv31.0 Definitions Manual. https://www.cms.gov/icd10manual/version31-fullcode-cms/P0001.html.Published2015.
- 18.Marchant MH, Viens NA, Cook C, Vail TP, Bolognesi MP. The Impact of Glycemic Control and Diabetes Mellitus on Perioperative Outcomes After Total Joint Arthroplasty. J Bone Jt Surgery-American Vol. 2009;91(7):1621–1629. doi: 10.2106/JBJS.H.00116 [DOI] [PubMed] [Google Scholar]
- 19.Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). 2016 Procedure-Specific Measure Updates and Specifications Report Hospital-Level Risk-Standardized Complication Measure: Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) – Version 5.0; 2016.
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity Measures for Use with Administrative Data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 21.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 22.Goldstein DT, Durinka JB, Martino N, Shilling JW. Effect of preoperative hemoglobin A(1c) level on acute postoperative complications of total joint arthroplasty. Am J Orthop (Belle Mead NJ). 2013;42(10):E88–90. http://www.ncbi.nlm.nih.gov/pubmed/24278910.AccessedNovember 9, 2017. [PubMed] [Google Scholar]
- 23.Akiboye F, Rayman G. Management of Hyperglycemia and Diabetes in Orthopedic Surgery. Curr Diab Rep. 2017;17(2):13. doi: 10.1007/s11892-017-0839-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dhaliwal R, Cibula D, Ghosh C, Weinstock RS, Moses AM. Bone quality assessment in type 2 diabetes mellitus. Osteoporos Int. 2014;25(7):1969–1973. doi: 10.1007/s00198-014-2704-7 [DOI] [PubMed] [Google Scholar]
- 25.Falcão FRC, Dias BAG, Wolfovitch LA, Sadigursky D. Total hip arthroplasty complications in patients with or without controlled diabetes mellitus during hospitalization. Rev Bras Ortop (English Ed.2016;51(5):589–596. doi: 10.1016/j.rboe.2016.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


