Abstract
Background:
The study is amined to correlate the voiding pattern after successful mini sling Ophira implantation with postoperative symptoms and satisfaction, in addition to identifying obstructions.
Materials and methods:
From 2012 to 2015 in a single institution, all consecutive patients who had stress urinary incontinence treated by using the mini sling Ophira had a pre- and 12 months postoperative urodynamic test. The International Consultation on Incontinence Questionnaire – Urinary Incontinence – Short Form (ICIQ-UI-SF) and the International Consultation on Incontinence Questionnaire – Overactive Bladder (ICIQ-OAB) translated into Portuguese, were given. Patients were objectively considered cured when presenting no urinary incontinence at the Valsalva test and subjectively cured when the ICIQ-UI-SF was zero.
Results:
Questionnaire scores were obtained from 29 patients and urodynamic data from 20 patients. Mini sling Ophira implantation resulted in a significant improvement of urinary symptoms evidenced by a significant mean reduction in ICIQ-UI-SF from 16 to 5 (p < 0.0001) and ICIQ-OAB from 8 to 4 (p = 0.0001). The subjective and objective cure rates were 55% and 45%, respectively. The urodynamic changes were not related to success even when adjusted for age, hormonal status, or anterior pelvic organ prolapse. The mean maximum flow decreased to 4.9 mL/s (95% CI: 0.62–10.8; p = 0.035), and the mean detrusor pressure at maximum flow increased to 11.4 cmH2O (95% CI: 4–18; p = 0.0078).
Conclusions:
Mini sling Ophira implantation decreased maximum urinary flow and increased the detrusor pressure at the maximum urinary flow and these urodynamic changes were not related to success.
Keywords: Mini sling, Single-incision sling, Stress urinary incontinence, Suburethral sling, Urodynamic
1. Introduction
Urinary incontinence is an important condition in the female population, with a lifetime estimated risk of about 40%–50%.[1] Though not a life-threatening condition, it is an important cause of work absenteeism, low self-esteem, and has a great impact on the quality of life. The retropubic mid-urethral synthetic sling was introduced in 1996 and showed results as good as traditional surgeries. However, complications such as bladder perforation, bowel and vascular injury, urethral lesions, and obstruction were not negligible.
The next sling generations were developed by attempting to keep the same success while performing less invasive procedures with fewer complications.[2] Mini slings have a shorter length, are inserted by a single incision, and fixed by a self-anchoring mechanism, and thus they are supposed to have a lower risk of complications such as viscera injury and bladder obstruction.[3,4] However, there is limited evidence about the voiding pattern after mini sling implantation.[3]
This study aimed to evaluate the urodynamic voiding pattern after mini sling Ophira implantation and to correlate it to success, postoperative symptoms, and satisfaction in addition to identify signs of obstruction.
2. Materials and methods
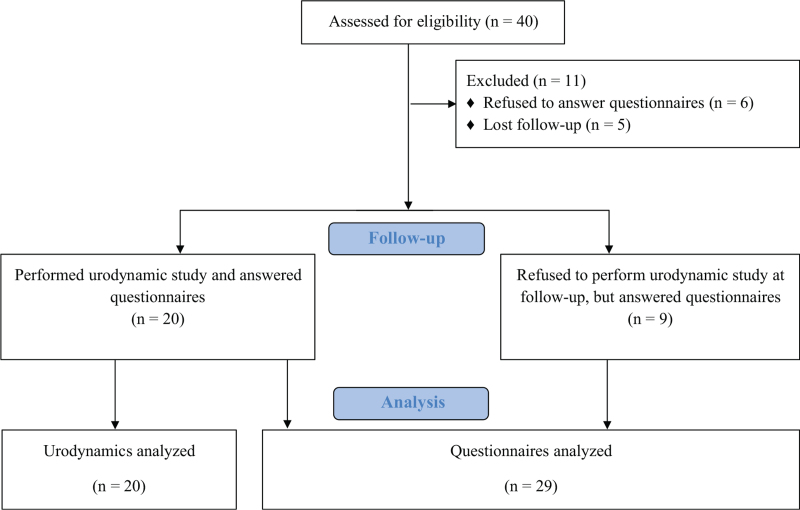
After institutional board approval number 1.111.087, the prospective single-institution study included all consecutive patients who had stress urinary incontinence (SUI) treated using mini sling Ophira® (Promedon, Cordoba, Argentina) implantation from 2012 to 2015. The surgeries took place at a teaching center, were performed by junior urologists supervised by 1 of 2 senior urologists, using the same previously described technique.[5] All patients had a pre- and 12 months postoperative urodynamic test, and were given the International Consultation on Incontinence Questionnaire – Urinary Incontinence – Short Form (ICIQ-UI-SF) and the International Consultation on Incontinence Questionnaire – Overactive Bladder (ICIQ-OAB).[6,7] Patients who refused to sign a written informed consent or to answer questionnaires were excluded. Patients who refused to repeat the urodynamic study but answered the questionnaires were included as described in Figure 1.
Figure 1.
Study diagram.
The urodynamic test was performed according to the recommendations of the International Continence Society including cystometry and pressure-flow study.[8,9] The parameters analyzed were: first desire to void, cystometric capacity, bladder compliance, presence of SUI assessed by the Valsalva leak point pressure, voided volume, maximum flow (Qmax), detrusor pressure at maximum flow (PdetQmax), and postvoid residual volume. The Valsalva leak point pressure test was performed in the standing position to objectively access continence with the bladder filled to cystometric capacity. Outlet obstruction was assessed using Qmax and PdetQmax.[10] The zero scores at the ICIQ-UI-SF questionnaire were considered as a subjective cure while the objective cure was the absence of urinary leakage during a cough or a Valsalva maneuver during the urodynamic study.
Statistical analysis was performed using Prism 7.0 for Mac (Graphpad, La Jolla, CA). Quantitative data were analyzed as mean values, maximum, minimum, and standard deviation. Results were evaluated for normality using the D’Agostino and Pearson normality test. They were compared using ANOVA, Mann-Whitney, or Wilcoxon for paired tests. Linear regression was used to relate outcomes to age, menopause, and anterior pelvic organ prolapse. Pearson and Spearman correlation coefficients were used to relate the urodynamics parameters to success and questionnaire scores. The level of significance adopted was 5%.
3. Results
From 2012 to 2015, a total of 40 patients underwent mini sling implantation, 6 did not answer preoperative questionnaires and 5 were lost during follow-up, so the final study population consisted of 29 patients. Of these, 9 did not agree to perform the follow-up urodynamic study and were assessed only with questionnaires. Finally, we had urodynamic data from 20 patients and questionnaires scores from 29 patients. The study flow diagram is shown in Figure 1.
The mean age of the population at surgery was 62 ± 10.8 years. The mean follow-up was 29 ± 14.4 months. The majority (82.5%) was postmenopausal and 27.5% had low-grade pelvic organ prolapse. Table 1 presents the ICIQ-OAB and the ICIQ-UI-SF scores and Table 2 the urodynamic results.
Table 1.
Mini sling Ophira: subjective assessment.
| Preoperative | Postoperative | p | |
|---|---|---|---|
| ICIQ-UI-SF | 16 ± 3 | 5.1 ± 5 | <0.0001 ∗ |
| ICIQ-OAB | 8 ± 4 | 4.07 ± 3.6 | 0.0001 ∗ |
| ICIQ-OAB 3a | 1.7 ± 1.25 | 0.52 ± 0.69 | <0.001 ∗ |
| ICIQ-OAB 4a | 2.07 ± 1.44 | 1.03 ± 1.09 | 0.001 ∗ |
| ICIQ-OAB 5a | 2.24 ± 1.3 | 1.28 ± 1.16 | 0.011 ∗ |
| ICIQ-OAB 6a | 1.97 ± 1.3 | 1.24 ± 1.33 | 0.025 ∗ |
ICIQ-OAB = International Consultation on Incontinence Questionnaire – Overactive Bladder; ICIQ-UI-SF = International Consultation on Incontinence Questionnaire – Urinary Incontinence – Short Form; SD = standard deviation.
Statistically significant (p < 0.05).
Table 2.
Mini sling Ophira: pressure-flow studies.
| Presling | Postsling | Variation | Wilcoxon test | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | Mean | 95% CI | p | |
| Qmax, ml/s | 18.4 ± 7.1 | 17 (9–41) | 13.5 ± 5.5 | 12 (5–25) | −4 | −8.1 to 0.16 | 0.08 |
| PdetQmax, cmH2O | 21.1 ± 11.6 | 23 (2–46) | 32.3 ± 17.4 | 28 (2–91) | 12.1 | 2.3–21.9 | 0.014 ∗ |
CI = confidence interval; PdetQmax = detrusor pressure at maximum flow; Qmax = maximum flow; SD = standard deviation.
Statistically significant (p < 0.05).
A significant improvement in urinary symptoms was noticed after the intervention, evidenced by a significant score decrease in both questionnaires. The mean ICIQ-UI-SF score decreased from 16.0 ± 3.0 to 5.1 ± 5.0 (p < 0.0001) and the ICIQ-OAB score from 8.0 ± 4.0 to 4.1 ± 3.6 (p = 0.0001). The individual analysis of ICIQ-OAB questions 4a, 5a, and 6a showed that the individual variation in each question was also significant (Table 1). There was not a single case of acute urinary obstruction requiring bladder catheterization or reoperation.
The mean PdetQmax significantly increased by 12.2 cmH2O (95% CI: 2.3–21.9; p = 0.014) and the Qmax decreased by 4 mL/s (95% CI: 0.16–8.1; p = 0.08) (Table 2). The subjective and objective cure rates were 55% and 45%, respectively. The subgroup analysis regarding success and failure showed that both groups had similar values of Qmax and PdetQmax. Table 3 shows urodynamic parameters versus the objective success rate.
Table 3.
Urodynamic parameters vs. objective success rate.
| Success mean (95% CI) | Failure mean (95% CI) | p (Mann-Whitney test) | |
|---|---|---|---|
| Qmax postoperative, mL/s | 13.2 (9.4–10.9) | 14.6 (10.4–18.7) | 0.34 |
| PdetQmax postoperative, cmH2O | 31.9 (24–39) | 33.2 (16.4–49.9) | 0.88 |
CI = confidence interval; PdetQmax = detrusor pressure at maximum flow; Qmax = maximum flow.
4. Discussion
This study presents the urodynamics parameter changes after mini sling Ophira placement. The only significant change was the increase in PdetQmax which was not followed by a significant Qmax reduction. Previous studies, although not focused on urodynamic changes, showed similar results with other mini slings.
Natale et al.[11] showed a significant decrease in Qmax and an increase in PdetQmax after implantation of the mini sling AdjustTM at 6 months, while Sun et al.[3] showed a decrease in average flow rate after MiniArcTM implantation. Studies with traditional slings also showed changes in urodynamics.
Both Qmax and PdetQmax values were quite similar between dry and failure patients, which indicated that the mini sling success does not rely upon urodynamic infravesical obstruction. Moreover, correlation studies also support this hypothesis showing no statistical correlation between Qmax and PdetQmax, nor between Qmax and scores. The increase in PdetQmax was related to an improvement in ICIQ-OAB questions 3a and 4a as showed by negative correlation coefficients. These findings confirm the proposed concept that the mini slings function relies on urethropelvic fascia reinforcement and urethral pillowing instead of urethral compression.[12]
The third-generation mid-urethral slings, also called mini slings were developed to reduce the amount of mesh and complications such as bladder perforation, bowel and vascular lesions, and groin pain. Independent of the brand, almost all of them are inserted by a single incision and fixed at the level of the internal obturator muscle tendinous arc.
The Ophira mini sling is fixed by a self-anchoring system and can be performed as an outpatient procedure under local anesthesia.[5] Due to its length and positioning, one can suppose that it may cause less obstruction than retropubic or transobturator slings. However, this study brings new data on the voiding pattern after mini sling placement and shows that the mini sling does impact on flow-pressure studies. Moreover, one can consider that these impacts are similar to traditional slings, so patients’ follow-up should be similar to the traditional slings.
Previous studies showed that mid-urethral slings are related to postoperative higher detrusor pressure at Qmax, lower Qmax, and increased residual post-voided volume.[13–16] The Burch procedure is also related to higher urethral resistance in the success group and no changes in failures.[17]
According to Qmax and Pdet (Blaivas-Groutz nomogram), we observed a trend to mild obstruction following the successful surgery in 50% of dry patients compared to only 10% in those that failed, though none of the patients presented acute urinary retention needing catheterization to pass urine nor reoperation.
The single incision slings compose a heterogeneous device group with different sizes and anchoring systems, which may explain the variety of success rates found in the literature. Thus, when evaluating mini sling studies, one should bear these differences in mind. Regarding mini sling Ophira™, a few prospective studies showed an objective success rate of 68%–85% at 1 year follow up.[5,18–20] Gon et al.[21] showed mini sling Ophira success in the long-term of 67% at 8 years follow-up.
The present study was not designed for success evaluation; therefore, success rates should be interpreted with caution. In addition, the strict success criteria, using the ICIQ-UI-SF score equal to 0, can contribute to the low success rate. Moreover, Ophira™ was related to a significant patient satisfaction and improvement in quality of life as shown by a mean decrease of 11 points in the ICIQ-UI-SF score (95% CI 6–16; p < 0.001), which is widely used to access subjective improvement and quality of life.[5,14,22]
The study limitations are the relatively small number of patients, mainly those who agreed to perform postoperative urodynamics. However, it is important to consider the difficulty to get patients’ consent to perform such an invasive procedure, even more in asymptomatic ones. To the best of our knowledge, this is the first study that focused on the urodynamic changes after mini sling surgery, correlating them to the clinical outcomes.
5. Conclusions
Mini sling Ophira™ raises the detrusor pressure at maximum urinary flow, without correlation to success, supporting the hypothesis that the mini slings mechanism of action relies on urethral support instead of obstruction. Like other techniques for SUI treatment, caregivers should keep in mind the risk of voiding dysfunction in the follow-up.
Acknowledgments
To the involved institution(s), the patients, and those that provided and cared for study patients.
Statement of ethics
Subjects have given their written informed consent and the study protocol was approved by the institute's committee on human research, approval number 1.111.087. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest statement
The authors report no conflicts of interest.
Funding source
Leonardo O. Reis: CNPq: 304747/2018-1.
Author contributions
Lucas Mira Gon: Data collection and analysis, manuscript writing;
Danilo Leite Andrade: Data Collection and analysis, manuscript writing;
Paulo Palma: Project development, manuscript review;
Leonardo O. Reis: Project development, manuscript review;
Cássio Luis Zanettini Riccetto: Project development, manuscript review.
References
- [1].Nambiar A, Cody JD, Jeffery ST. Single-incision sling operations for urinary incontinence in women. Cochrane Database Syst Rev 2014;(6):CD008709. [DOI] [PubMed] [Google Scholar]
- [2].Santos-Souza R, Rodrigues-Palma PC, Goulart-Fernandes-Dias F, Teixeira-Siniscalchi R, Zanettini-Riccetto CL. Does the design of mini slings anchoring systems really matter? A biomechanical comparison between Mini Arc and Ophira. Actas Urol Esp 2016;40(9):564–569. [DOI] [PubMed] [Google Scholar]
- [3].Sun MJ, Sun R, Li YI. A comparative study of a single-incision sling and a transobturator sling: Clinical efficacy and urodynamic changes. Int Urogynecol J 2013;24(5):823–829. [DOI] [PubMed] [Google Scholar]
- [4].Mostafa A, Lim CP, Hopper L, Madhuvrata P, Abdel-Fattah M. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: An updated systematic review and meta-analysis of effectiveness and complications. Eur Urol 2014;65(2):402–427. [DOI] [PubMed] [Google Scholar]
- [5].Palma P, Riccetto C, Bronzatto E, Castro R, Altuna S. What is the best indication for single-incision Ophira mini sling? Insights from a 2-year follow-up international multicentric study. Int Urogynecol J 2014;25(5):637–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Tamanini JT, Dambros M, D’Ancona CA, Palma PC, Rodrigues Netto N, Jr. Validation of the “International Consultation on Incontinence Questionnaire—Short Form” (ICIQ-SF) for Portuguese. Rev Saude Publica 2004;38(3):438–444. [DOI] [PubMed] [Google Scholar]
- [7].Pereira SB, Thiel Rdo R, Riccetto C, et al. Validation of the International Consultation on Incontinence Questionnaire Overactive Bladder (ICIQ-OAB) for Portuguese. Rev Bras Ginecol Obstet 2010;32(6):273–278. [DOI] [PubMed] [Google Scholar]
- [8].Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29(1):4–20. [DOI] [PubMed] [Google Scholar]
- [9].Rosier P, Schaefer W, Lose G, et al. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn 2017;36(5):1243–1260. [DOI] [PubMed] [Google Scholar]
- [10].Nitti VW. Pressure flow urodynamic studies: The gold standard for diagnosing bladder outlet obstruction. Rev Urol 2005;7Suppl 6:S14–21. [PMC free article] [PubMed] [Google Scholar]
- [11].Natale F, Dati S, La Penna C, Rombola P, Cappello S, Piccione E. Single incision sling (Adjust) for the treatment of female stress urinary incontinence: 2-year follow-up. Eur J Obstet Gynecol Reprod Biol 2014;182:48–52. [DOI] [PubMed] [Google Scholar]
- [12].Tse V, Chan L. Outlet obstruction after sling surgery. BJU Int 2011;108Suppl 2:24–28. [DOI] [PubMed] [Google Scholar]
- [13].Klutke JJ, Klutke CG, Bergman J, Elia G. Urodynamics changes in voiding after anti-incontinence surgery: An insight into the mechanism of cure. Urology 1999;54(6):1003–1007. [DOI] [PubMed] [Google Scholar]
- [14].Palma P, Riccetto C, Castro R, Altuna S, Herrmann V, Miyaoka R. Safety and efficacy of the Ophira mini-sling system: One year follow-up from a multicenter international clinical trial. UroToday IntJ 2011;4(3):art44. [Google Scholar]
- [15].Djehdian LM, Araujo MP, Takano CC, et al. Transobturator sling compared with single-incision mini-sling for the treatment of stress urinary incontinence: A randomized controlled trial. Obstet Gynecol 2014;123(3):553–561. [DOI] [PubMed] [Google Scholar]
- [16].Kraus SR, Lemack GE, Richter HE, et al. Changes in urodynamic measures two years after Burch colposuspension or autologous sling surgery. Urology 2011;78(6):1263–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Smith PP, Dhillon RK, Baptiste M, Arunkalaivanan AS. Comparison of single-incision mid-urethral tape (Ophira™) and transobturator tape (Obtryx™) suburethral sling procedures for female stress urinary incontinence. J Clin Med Res 2013;5(5):58–61. [Google Scholar]
- [18].Sharifiaghdas F, Nasiri M, Mirzaei M, Narouie B. Mini sling (Ophira) versus pubovaginal sling for treatment of stress urinary incontinence: A medium-term follow-up. Prague Med Rep 2015;116(3):210–218. [DOI] [PubMed] [Google Scholar]
- [19].Texl J, Huser M, Belkov I, et al. Efficacy of surgical treatment of stress urinary incontinence with mini-invasive single incision sling. Ceska Gynekol 2015;80(5):345–350. [PubMed] [Google Scholar]
- [20].Zengin K, Kara M, Tanik S, Sertcelik MN, Eraslan A. Comparison of transobturator tape and mini-sling tissue fixation in female patients who had stress urinary incontinence. Adv Clin Exp Med 2015;24(5):851–855. [DOI] [PubMed] [Google Scholar]
- [21].Mira Gon L, Zanettini Riccetto CL, Citatini de Campos CC, et al. Mini-sling Ophira at 8 years follow-up: Does it sustain results? Urol Int 2019;102(3):326–330. [DOI] [PubMed] [Google Scholar]
- [22].Karmakar D, Mostafa A, Abdel-Fattah M. A new validated score for detecting patient-reported success on postoperative ICIQ-SF: A novel two-stage analysis from two large RCT cohorts. Int Urogynecol J 2017;28(1):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]