Summary
Introduction
The curtailment of social gatherings and the lack of online academic engagement during the COVID-19 lockdown could have potentially damaging effects on the psychological state of university students in Nigerian public universities. This study examined the prevalence of anxiety and depression, including associated factors and coping methods, among undergraduate students.
Methods
This cross-sectional study, which involved 386 undergraduate students, was assigned approval number UI/EC/20/0242. An online questionnaire consisting mainly of the Hospital Anxiety and Depression Scale and the McMaster Family Assessment Device was circulated among the students. The results were analysed by means of descriptive statistics, chi-square, Analysis of Variance (ANOVA) and linear logistical regression, at α 0.05.
Results
Mean age was 21 ± 2.9 years, with females constituting 60.1% of the sample. The prevalence rates of anxiety and depression were 41.5 and 31.9%, respectively. Students in health-related faculties were significantly less anxious than others. Inability to afford three square meals, negative family functioning, chronic illness and living in a State/Region with a high incidence of COVID-19 were significantly associated with depression. These factors jointly accounted for 14% of depression. Coping methods included the use of social media, watching movies and participating in online skills-development programs.
Conclusion
The overall level of anxiety and depression among undergraduate students during the COVID-19 lockdown was higher than the levels previously reported. Inadequate nutrition and poor family functioning contributed significantly to this. Proactive measures ought to be taken to support undergraduate students in order to prevent the negative consequences of poor mental health.
Keywords: COVID-19, Anxiety, Depression, Family functioning, Coping
Introduction
The novel coronavirus disease (COVID-19) pandemic, which was first detected in December 2019, has continued to ravage the entire world. The outbreak started in Wuhan, China [1] and has since spread to almost all the countries in the world [2]. Six months since the first case was reported, the number of confirmed cases had risen to 9,633,157 [2]. A little less than a year later, the number of confirmed cases had risen by over 13-fold (131,487,572) [3]. Mortality from the disease is high, with the estimated death toll reaching 2,857,702 by early April 2021 [3]. Although the number of cases was slow to rise in Africa, the increase was exponential [4], placing an enormous burden on the already weak health system [5].
On March 11, 2020, the World Health Organization (WHO) declared the novel Coronavirus disease a pandemic, owing to its worldwide spread and its impact on lifestyles and social interactions [6]. It was subsequently termed a Public Health Emergency of International Concern by the WHO [7].
The first case of coronavirus in Nigeria was confirmed on February 27, 2020 [8], following which the Nigerian Centre for Disease Control (NCDC) issued several guidelines for curtailing the spread, in line with the internationally-approved standard [9]. Despite these measures, the number of cases continued to rise and was estimated to have reached 163,388 by April 7, 2021 [10]. Already by March 2020, the spread of the virus had prompted the federal and state governments and their various para-statal authorities to shut down activities in the country. By March 23, both land borders and air space had been closed and the weekly meeting of the federal executive council had been suspended, among other measures [11]. On Monday, March 23, 2020, the Nigerian University Commission (NUC) ordered the lockdown of all universities and affiliated schools [12]. This halted academic activities, causing students to go home or discontinue their industrial training - an unplanned break.
In addition, a lockdown was imposed on activities in three major states in the country from March 30, 2020, and a partial lockdown in most other states prohibited all social and religious gatherings [13]. As a result, the residents of Lagos and Ogun States and the Federal Capital Territory, where the lockdown was total, as well as those of other States, where it was partial, had to spend most of their time at home.
Many employers have since enabled their employees to work from home, while many private universities and secondary schools are taking measures to provide online tuition for their students. Unfortunately, this is not the case among students of public tertiary institutions, who form the bulk of Nigerian youths. Even before academic activities were halted because of the coronavirus pandemic, university staff across the country had already gone on strike from March 9, 2020 [14]. Hence, there was no plan in place to engage public tertiary institution students during the COVID-19 lockdown, nor was it possible to continue industrial training/internship in companies, owing to the lockdown.
A feeling of being stalled in academic progress could lead to the development of anxiety or other psychological disorders, since the period of youth is perceived as a period of opportunities [15]. It is also unclear what role youths’ family functioning may be playing in their psychological state. Given the increase in the incidence of mental disorders, particularly anxiety and depression, among young people [16], it has become crucial to examine the psychological state and coping mechanisms of undergraduate students in Nigeria. This assertion is in line with the significant function of nurses in caring for the bio-psychosocial state of individuals, whether sick or well.
Further, in 2019 the WHO reported that mental health problems accounted for 16% of the global health burden among people aged 10-19 years [17]. It also asserted that, if left undiagnosed and untreated, such disorders could lead to a myriad of physical and mental health issues, hence preventing these individuals from living fulfilling lives as adults [17]. Some authors have reported an increased prevalence of anxiety and depression among university/college students in China and Greece during the lockdown [18-21]. However, there is a dearth of information on the prevalence of anxiety and depression and their associated factors among undergraduate students in Nigeria during the COVID-19 lockdown. We therefore studied the psychological effects of the lockdown, its associated factors, family functioning and coping strategies among undergraduate students of the University of Ibadan in Nigeria.
Materials and methods
STUDY DESIGN, SETTING AND POPULATION
A descriptive study design was used, and the study was conducted among undergraduate students of the University of Ibadan between April 29th and May 5th, 2020. The University of Ibadan is the first university in Nigeria and was founded on November 17, 1948. It is located in Oyo State, south-western Nigeria. Founded and funded mainly by the federal government, the university consists of sixteen faculties [22]. Study participants were drawn from 12 faculties, which were merged into seven major faculties, namely: Social Sciences; Clinical Sciences & Public Health; Pharmacy & Basic Medical Sciences; Law & Arts; Sciences & Technology; Education; Agriculture & Veterinary medicine. Inclusion criteria were: undergraduate students attending regular courses, i.e. full-time students as opposed to those enrolled in the Open Distance Learning (ODL) mode; students who had access to a web-based method of communication, specifically Whatsapp messaging platform, and were included on the Faculty Whatsapp pages.
SAMPLE SIZE AND SAMPLING TECHNIQUE
At a confidence level of 95% and a 4.94 confidence interval (margin of error), a sample of 386 students was calculated by means of an automatic sample-size calculator to be representative of the total undergraduate population of 14,833 [23]. The representatives of students’ (sub) unions in the faculties were contacted through the university Students’ Union (SU) vice president, who is a student at the researchers’ department. The faculty executives then contacted their colleagues via an online messaging platform (Whatsapp). Information about the study (aims, benefits and study population) was provided on students’ Faculty and Department Whatsapp pages, from which a convenience sample of students chose to participate in the study.
INSTRUMENT
The study instrument consisted of a questionnaire made up of the following parts: Sociodemographic characteristics/history of chronic illness, Hospital Anxiety Depression Scale (HADS), Family Assessment Device (FAD) and coping strategies. Questions on Sociodemographic characteristics included: age, year of study, state of residence, whether there was a lockdown in the state of residence, among others. A higher level of psychological distress is associated with higher regional/state prevalence of COVID-19, as a result of perceived higher risk [24]. Hence, in this study, participants’ states of residence were categorised as low-, medium- and high-risk states on the basis of the number of cases reported in each state of the federation by the NCDC at the time of data collection. Moreover, as the closure of many businesses, due to measures to curtail the spread of the coronavirus, may have reduced family income, participants were asked if they could afford three meals a day. Also, with regard to average weekly personal income, five options were provided: less than 1,000; 1,000-5,000; 6,000-10,000; 11,000-15,000; above 15,000 naira; these were reduced to two categories, as most of the students chose the first option. These last two questions, together with questions regarding the number of cars owned by the family and whether the family owned their own house were used to roughly estimate the socioeconomic status of the students. The four questions, however, did not constitute a composite unit, but were assessed individually. To determine the presence of chronic illness(es), students were asked if they had any of the following illnesses: asthma, sickle cell disease, diabetes, hypertension, kidney disease, depression, and were instructed that they could tick more than one option. These chronic conditions are common among university students in Nigeria, to the best of the researcher’s knowledge. However, another option, ‘others’, was provided so that students could tick this option if their chronic/long-term illness was not listed. Participants were thereafter grouped into two categories according to the presence or absence of chronic illness.
The Hospital Anxiety Depression Scale (HADS) is a questionnaire made up of 14 items consisting of questions that evaluate anxiety and depression. It has been found suitable for use among psychiatric, non-psychiatric and healthy populations [25]. Specificity and sensitivity values of 80% have been reported for both sections of the questionnaire (anxiety and depression) and the subscale scores range from 0-7, which denotes ‘normal’ or no anxiety/depression; 8-10 denoting ‘suspicious’ or mild, and 11-21 which points to the presence of anxiety or depression. These categories also show that the higher the score is, the greater the anxiety or depression is. Moreover, the specificity and sensitivity values of the scales have been established to range between 85 and 92.9% among Nigerians [26]. The author of that study, which was carried out in both hospital and community settings, recommended the instrument for use in community surveys in developing countries. Another author classified the scale scores into four [27], but did not provide data on the specificity and sensitivity based on these classifications. We therefore used the three original categories in our study.
Family Assessment Device (FAD): this is based on the McMaster Family Functioning model. The FAD is a scale whereby the structural and organisational characteristics of families are assessed, together with the methods of interactions among family members. It is able to distinguish between “healthy” and “unhealthy” families, thereby guiding the possible provision of social support. It has seven [8] subscales: Problem Solving, Communication, Roles, Affective Responsiveness, Affective Involvement, Behaviour Control and General Functioning. The scale is available free of charge. The reliability α ranges from 0.72 to 0.83 for the subscales, and is 0.92 for general functioning. In a previous study [28], test-retest reliability of 0.86 on the general functioning scale was obtained among Nigerians. In the present study, we used only the general functioning section, consisting of 12 items, as it assesses the overall health or pathology of the family, since the various subscales have been incorporated into it. Moreover, including the entire scale consisting of 60 questions, which would have meant adding further sections to the questionnaire, might have reduced the response rate. Responses are marked on a four-point Likert scale: “strongly agree,” “agree,” “disagree,” and “strongly disagree. Negatively structured questions are reversed, and higher scores indicate problematic functioning. The highest obtainable score is 48, while the lowest obtainable score is 12. The higher the score, the poorer the family functioning [29].
DATA COLLECTION AND ANALYSIS
After ethical approval had been obtained from the University of Ibadan/University College Hospital ethical review board, the link to the questionnaire, which was created by means of a Google form, was sent to undergraduate students, together with an introductory message explaining the purpose of the study. The message and the link were sent through the Whatsapp messaging platform, as students were not reachable at school owing to the lockdown. The data collected were cleaned and transferred from the Google form excel spreadsheet to Statistical Package for Social Sciences (SPSS) version 20.0 for analysis. Frequencies, percentages and means were used to report the sociodemographic variables. These variables were tested by means of the chi-square test and ANOVA for their association with anxiety and depression. Those that were significant were entered into a linear regression model to determine to what degree they predicted depression. Depression and anxiety were classified into three scales: 0-7, which denotes ‘normal’ or absence of anxiety/depression; 8-10 denoting ‘suspicious’ or mild anxiety/depression, and 11-21, pointing to the presence of moderate-to-severe anxiety or depression. These two measures were also tested by means of ANOVA for their association with family functioning. Post-hoc analysis was carried out by means of Fisher’s Least Significant Difference, to determine the pair means that were statistically different. Coping methods used by the students and their willingness to be seen by a healthcare provider if they were experiencing anxiety or depression were presented as bar charts.
ETHICAL CONSIDERATIONS
The study protocol was submitted for ethical approval to the University of Ibadan/University College Hospital Ibadan (U.I. /UCH) ethical review committee, which assigned it an approval number (UI/EC/20/0242). Moreover, the questionnaire, which was circulated as a Google form, included an introduction explaining the aims and benefits of the study. Students who completed the form gave their consent implicitly.
Results
SOCIODEMOGRAPHIC CHARACTERISTICS AND THEIR ASSOCIATION WITH ANXIETY AND DEPRESSION
Respondents’ sociodemographic characteristics and their association with anxiety and depression, as evaluated by the Chi-square test, are presented in Table I. The mean age of the undergraduates was 20.8 (± 2.9) years, with a little over half (50.2%) in the 20-23 year age-range. Most were female (60.1%), and Christianity was the most prevalent religion. Almost 20% of the participants could not afford three square meals. Eight percent (8%) of the participants suffered from some form of chronic illness, and 35.2% reported that a total lockdown was in force in their state at the time of data collection. Inability to afford three square meals and being under complete lockdown in the State of Residence were associated with depression (p < 0.001 and p < 0.05, respectively). There was a significant association between students’ academic faculty and anxiety.
Tab. I.
Analysis of association between respondents’ sociodemographic characteristics and psychological state.
| Variable | F (N = 386) |
% | Anxiety | Depression | ||
|---|---|---|---|---|---|---|
| X2 | P-value | X2 | P-value | |||
|
Age (in years) 16-9: 20-23 24-27 28 & over Mean 21 ± 2.9 |
128 204 46 8 |
33.2 52.8 11.9 2.1 |
7.43 | 0.26 | 4.42 | 0.60 |
|
Gender: Female Male |
232 154 |
60.1 39.9 |
2.14 | 0.35 | 0.21 | 0.93 |
|
Faculty: Social Sciences Clinical Sciences & Public Health Pharmacy & Basic Medical Sciences Law & Arts Sciences & Technology Education Agriculture & Vet. medicine |
82 71 65 59 48 34 27 |
21.2 18.4 18.8 15.2 12.4 8.8 7.0 |
2.34 | 0.03a* | 1.01 | 0.42 |
|
Level of study: 1st year 2nd year 3rd year 4th year 5th year 6th year |
104 84 83 88 23 4 |
26.9 21.8 21.5 22.8 6.0 1.0 |
16.89 | 0.08 | 12.97 | 0.23 |
|
Religion: Christianity Islam Others |
322 57 7 |
83.4 14.8 1.8 |
8.53 | 0.13 | 3.62 | 0.68 |
|
Presence of chronic illness: Yes No |
36 355 |
8.0 92.0 |
2.57 | 0.30 | 8.29 | 0.02* |
|
Able to afford 3 meals/day: Yes No |
311 75 |
80.6 19.4 |
11.63 | 0.003* | 22.44 | 0.000* |
|
Ownership of cars: ≥ 3 0-2 |
55 331 |
14.3 85.7 |
8.71 | 0.36 | 5.70 | 0.68 |
|
Personal income: < 1,000 naira (< $2.6)/week ≥ 1,000 naira (≥ $2.6)/week |
230 156 |
59.6 40.4 |
9.21 | 0.30 | 5.67 | 0.67 |
|
Currently working part-time: Yes No |
60 326 |
15.5 84.5 |
0.52 | 0.79 | 1.71 | 0.41 |
|
Total lockdown in place of residence: Yes No |
186 250 |
35.2 64.8 |
2.74 | 0.26 | 7.47 | 0.02* |
|
Place of residence during the lockdown: Staying with family or friends Staying alone |
370 16 |
95.9 4.1 |
0.79 | 0.67 | 0.90 | 0.64 |
|
State of residence during lockdown: High-risk state (> 300 cases) Medium-risk state (50-299 cases) Low-risk state (< 50 cases) |
87 33 266 |
22.5 8.5 69 |
1.86 | 0.76 | 5.36 | 0.25 |
|
Family members exposed/on front line: Yes No |
78 308 |
20.2 79.8 |
0.41 | 0.84 | 2.09 | 0.36 |
a ANOVA test. The rest are chi-square test.
* Significant at p < 0.05.
Faculty of study and inability to afford three square meals were significantly associated with anxiety. Having a chronic illness, inability to afford three square meals and presence of lockdown in the state of residence were significantly associated with depression.
Post-hoc analysis (LSD - Least Significant Difference) of mean scores among the different faculties showed that students in the faculties of Clinical Sciences/Dentistry/Public Health displayed a significantly lower level of anxiety (5.2 ± 4.1) than their counterparts in Social Sciences and Economics (6.61 ± 4.50, p = 0.046); Science and Technology (7.4 ± 4.5, p = 0.01); Education (7.7 ± 4.1, p = 0.01) and Agriculture/Veterinary Medicine 7.9 ± 5.4, p = 0.01). However, there was no significant difference between the scores of those in Clinical Sciences/Dentistry/Public Health and Pharmacy/Basic Medical Sciences (5.7 ± 3.4), p = 0.64.
Additionally, students in the Faculty of Education had a higher mean score on depression (7.2 ± 3.9) than those in the faculties of Pharmacy/Basic Medical Sciences (5.7 ± 3.4), p = 0.04.
PREVALENCE OF ANXIETY AND DEPRESSION AND WILLINGNESS TO CONSULT A HEALTH PROFESSIONAL
Table II shows that 20.7% of the students experienced moderate-to-severe anxiety, with another 20.7% suffering from mild anxiety. Also, the prevalence of moderate-to-severe depression was 10.9%, while 21% had mild depression.
Tab. II.
Prevalence of anxiety and depression.
| Psychological state | Category | Frequency | Percent |
|---|---|---|---|
| Anxiety | No anxiety, i.e. normal | 226 | 58.5 |
| Anxiety suspected, i.e. mild | 80 | 20.7 | |
| Anxiety present, i.e. moderate-to-severe | 80 | 20.7 | |
| Total | 386 | 100 | |
| Depression | No depression, i.e. normal | 263 | 68.1 |
| Depression suspected, i.e. mild | 81 | 21 | |
| Depression present, i.e. moderate-to-severe | 42 | 10.9 | |
| Total | 386 | 100 |
More than 40% of the undergraduates had mild-to-severe forms of anxiety, while a little over 30% had some degree of depression.
A good number of students were open to discussing their mental health state with a health professional.
COPING WITH THE LOCKDOWN
As shown in Figure 2, students coped with the lockdown and the cessation of academic activities by using social media (17.9%), watching television or videos (11.1%), or engaging in online skills-building activities (15.3%). Other methods of coping included sports activities, meditation, helping at home, games and music.
Fig. 2.

Students' favourite activities for coping with the lockdown included virtual entertainment, watching television and skills acquisition.
ASSOCIATION BETWEEN FAMILY FUNCTIONING AND PSYCHOLOGICAL STATES
Table III shows a significant effect of family functioning on the presence, suspected presence or absence of anxiety at p < 0.01 [F (2, 383) = 15.49, p = 0.000], on Analysis of Variance (ANOVA).
Tab. III.
ANOVA showing association between family functioning and anxiety.
| N | Mean | Standard deviation | F | P-value | |
|---|---|---|---|---|---|
| No anxiety | 226 | 23.2 | 5.1 | 15.49 | 0.000a |
| Anxiety suspected | 80 | 24.8 | 6.0 | ||
| Anxiety present | 80 | 27.2 | 6.5 |
a significant at p < 0.01.; two-tailed.
The mean difference between undergraduate students who were anxious or had suspected anxiety was significant.
Moreover, post-hoc comparison of the mean scores of the three categories, on Fisher’s Least Significant Difference (LSD) (Tab. IV) revealed that the mean score for family functioning among students with no anxiety (23.2 ± 5.1) was significantly different from that of students in whom anxiety was suspected (24.8 ± 6.0); p = 0.03. Similarly, there was a significant difference between those with no anxiety (23.2 ± 5.1) and those in whom anxiety was present (27.2 ± 6.3, p = 0.000). Higher scores denote poor family functioning.
Tab. IV.
Post-hoc analysis of family functioning and state of anxiety.
| Anxiety Category |
Anxiety category |
Mean difference | P-value | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| No anxiety | Anxiety suspected | -1.564 | 0.03 | -2.99 | -0.13 |
| Anxiety present | -4.014 | 0.000a | -5.44 | -2.58 | |
| Anxiety suspected | No anxiety | 1.564 | 0.03 | 0.13 | 2.99 |
| Anxiety present | -2.450 | 0.01 | -4.19 | -0.71 | |
| Anxiety present | No anxiety | 4.014 | 0.000a | 2.58 | 5.44 |
| Anxiety suspected | 2.450 | 0.01 | 0.71 | 4.19 | |
a p < 0.01.
The family functioning of students who were not anxious at all was significantly different from that of students who were suspected of having anxiety at p < 0.05 and from those with anxiety, at p < 0.01. There was also a significant difference in family functioning between students in whom anxiety was suspected and those with actual anxiety.
ANOVA results on depression and family functioning (Tab. V) showed a significant association between the two variables [F (2, 383) = 14.209, p = 0.000].
Tab. V.
ANOVA showing association between depression and family functioning.
| Category | N | Mean | Standard deviation | F | P-value |
|---|---|---|---|---|---|
| No depression | 263 | 23.4 | 5.4 | 14.209 | 0.000a |
| Depression suspected | 81 | 25.9 | 5.9 | ||
| Depressed | 42 | 27.6 | 6.1 |
a significant at p < 0.01; two-tailed.
There was a significant association between family functioning and depression.
In addition, Fisher’s Least Significant Difference (LSD), in Table VI, showed that the mean score for family functioning among students without depression (23.35 ± 5.44) was significantly lower than that of students who had borderline (suspected) depression (25.88 ± 5.87); p = 0.000 and of those who were depressed (27.6 ± 6.13), p = 0.000.
Tab. VI.
Post-hoc analysis of family functioning and depression.
| Depression category | Depression category | Mean difference | P-value | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| No depression | Depression suspected | -2.527 | 0.000a | -3.93 | -1.13 |
| Depressed | -4.245 | 0.000a | -6.08 | -2.41 | |
| Depression suspected | No depression | 2.527 | 0.000a | 1.13 | 3.93 |
| Depressed | -1.719 | 0.11 | -3.82 | 0.38 | |
| Depression | No depression | 4.245 | 0.000a | 2.41 | 6.08 |
| Depression suspected | 1.719 | 0.11 | -0.38 | 3.82 | |
a p < 0.01.
However, there was no significant difference between the family functioning of those with borderline depression (25.88 ± 5.87) and those who were depressed (27.6 ± 6.13), p = 0.108.
Students who were depressed had significantly better family functioning than students who had suspected and actual depression.
MULTIPLE LINEAR REGRESSION ON VARIABLES THAT PREDICT DEPRESSION
A multiple linear regression was performed to determine to what extent some variables predicted the presence of depression, as shown in Table VII. The results indicated that the model explained 14.3% of the variance and that the model was a significant predictor of depression, F (4,381) = 15.92, p < 0.001. The results also showed that three meals/day, [Beta = 0.19, t (381) = 3.97, p < 0.01]; chronic illness [Beta = 0.123, t (381) = 2.5, p = 0.01] and family functioning [Beta = 0.264, t (381)] = 5.52, p < 0.01] significantly predicted the presence of depression. However, current residence in a state under lockdown was not statistically significant.
Tab. VII.
Multiple linear regression analysis of the relationship between selected variables and depression.
| B | Standard error | β | t | P-value | |
|---|---|---|---|---|---|
| (Constant) | -2.577 | 1.189 | -2.168 | 0.03 | |
| 3 meals/day | 1.683 | 0.424 | 0.19 | 3.97 | 0.000 |
| Lockdown in State | 0.614 | 0.35 | 0.084 | 1.752 | 0.08 |
| Chronic illness | 1.589 | 0.614 | 0.123 | 2.59 | 0.01 |
| Family functioning | 0.16 | 0.029 | 0.264 | 5.517 | 0.000 |
F (4,381) = 15.92; p < 0.001; R2 = 0.143 (14.3%); R2 Adjusted 0.134
Participants’ predicted depression score was - 2.58 + 1.68 (3 meals/day) + 0.61 (lockdown in state of residence) + 1.59 (chronic illness) + 0.16 (family functioning), where 3 meals/day and lockdown in the state of residence were coded as 2 = Yes, 1 = No; and chronic illness was coded as 2 = Yes, 1 = No. Students who were unable to afford three square meals, who had chronic illness(es) and who had poor family functioning were more depressed.
The model shows that the four factors were able to predict 14% of depression seen in the students.
Discussion
The lockdown prompted by the coronavirus pandemic was an exceptional event in Nigeria. Every sector of the country has been affected, although the Federal and State Governments have finally eased the lockdown. In January 2021, which was a few months before this report was written, the undergraduate students were able to resume their academic activities, after eight months’ interruption.
The response rate to this survey was 21.2%. Most of the participants were female (60%), although the male: female ratio in schools is usually around 53:47 [30]; hence, it was expected that a slightly higher or an equal number of male students would participate in the study. However, the higher percentage of females participants could be explained by the greater interest of women in psychology-related issues. Indeed, the dominance of women in psychology is supported by research [31], which has revealed that there are more females in the field of psychology – both in education and the workforce. Similarly, some authors [32] have found that a significantly higher number of females than males enrol in postgraduate programmes in psychology, the proportion being as high as 75% females vs 25% males; this trend has been under way for about 10 years.
Students with one or more chronic illness had a significantly higher level of anxiety and depression than those who did not have such illnesses. This finding is in line with data from Wang et al. [33], who reported a higher level of psychological distress among people with a medical history of chronic illness in a population-based study involving 1210 people in China.
Contrary to the findings of some authors [18, 19, 34], in which female participants had a significantly higher level of depression than their male counterparts during the COVID-19 pandemic, there was no significant association between gender and anxiety or depression among the participants in this study. This difference may be due to the difference in demography. Indeed, whereas the present study was carried out among university students aged 16 to 30 years, the above authors [18, 19, 34] carried out their surveys among all age-groups. Conversely, the present findings are in keeping with those of some other studies [16, 35, 36], which were all carried out among university students. Thus, it is possible that other factors, such as age, combine to make females more prone to psychological distress. However, a study [37] conducted among university students in China showed a significantly higher prevalence of depression among female students.
Although such measures of socioeconomic status as the number of cars owned by the family, the level of private income and living in one’s own house were not associated with anxiety and depression, students who could not afford three square meals/day had a significantly higher level of anxiety and depression. However, being able to provide three meals is linked to income. Hence, it can be presumed that students who could not afford three square meals were of low socioeconomic background. Cao et al. [18] also reported that poor socioeconomic status was associated with anxiety among the university students who participated in their study, with those living in poorer conditions experiencing considerably more anxiety. At the beginning of the lockdown in Nigeria, the federal government and some state governments promised to provide financial support to ease the economic burden of the lockdown. However, owing to the limited resources available, these palliative measures could only be provided for the ‘poorest of the poor’. This socioeconomic group, which constitutes 49.66% of the population, is mostly resident in the rural areas of the country [38]. Therefore, residents of urban areas, which is where most university students live, were not provided with support, hence the inability to afford three square meals a day.
Regarding the prevalence of anxiety, Cao et al. [18] reported that about 25% of Chinese university students experienced mild-to-severe forms of anxiety during the COVID-19 pandemic. In the present study, by contrast, a higher percentage of Nigerian university students (41.5%) experienced mild-to-severe forms of anxiety. The higher rate could be due to the different periods of data collection. Indeed, while Cao et al. [18] collected their data in February 2020, before the pandemic reached its peak in most parts of the world, the data for the present study were collected in May 2020, a period during which cases were increasing exponentially in Nigeria. Before the COVID-19 pandemic, some authors [39] had reported a lower rate of anxiety (14.8%) among undergraduate students in five universities in South-western Nigeria. Again, this is not surprising, since several studies conducted in Italy, the United States, China and Spain [19-21, 35, 40] have averred that the lockdown/self-quarantine associated with COVID-19 has put considerable psychological strain on college students.
Furthermore, mild-to-severe depression was detected in 31.9% of the university students who participated in this study, one-third of whom were adolescents (aged 16-19 years). Although there are no national data on the prevalence of depression among Nigerian youths, there are reports of studies carried out in the same geopolitical zone where the present study was conducted. For instance, the prevalence found in this study was higher than that reported earlier among Nigerian adolescents [41], according to which 21.2% of rural adolescents in south-western Nigeria were found to have varying degrees of depression. It is not surprising that more participants in this study experienced depression, since the COVID-19 lockdown was something that put emotional strain on many people. Likewise, in 2019, a somewhat lower prevalence rate of depression (21.6%) was reported by Ayandele et al. [39] among undergraduate students in five universities located in the same region where the present study took place.
Earlier, in 2013, Peltzer et al. [42] had documented a prevalence of 25.2% of moderate-to-severe forms of depression among undergraduate students in Western Nigeria. However, 10.9% of undergraduate students who participated in this study experienced moderate-to-severe depression. This difference could be due to the fact that, in the study by Peltzer et al. [42], other sensitive information, such as the experience of sexual abuse, physical violence or injury and substance abuse, was elicited from the participants at the same time as data on depression. This information might have brought on some negative feelings leading to a higher score on depression were collected.
Moreover, students who lived alone did not experience a significantly higher level of anxiety than those living with family or friends, a finding which is in line with Mazza et al. [19]. Since most participants were young adults, it could be that those living alone were able to fend for themselves and therefore did not suffer from a significantly higher level of anxiety. Furthermore, the results of post-hoc ANOVA showed that students in non-health-related faculties had a considerably higher level of anxiety than those in health-related fields. This inter-faculty difference is congruent with what was reported in another study among college students in China and Spain [37, 40].
Another contributory factor to depression among undergraduate students was family functioning. Participants with poor family functioning experienced mild-to-severe depression, while those with good family functioning were not depressed. As mentioned earlier, living alone or with family or friends did not significantly influence the experience of depression. Nevertheless, living with family or friends, as almost all the participants did, while at the same time experiencing poor functioning, was a significant causal factor of depression. Cao et al. [18] reported a negative correlation between social support and anxiety, with anxiety decreasing as social support increased. Furthermore, Li et al. [43] reported that good family functioning was associated with a decreased level of psychological distress among students of the health professions. This was also the position of Jianjun et al. in a study conducted among undergraduate students in China [44].
The top three coping methods used by our undergraduate students were: using social media - Whatsapp, status challenges, Instagram, among others - watching television or movies and participating in online skills-acquisition programmes or extra-curricular study activities. These methods are similar to those mostly used by university students in Jordan, as reported by Al-Tamemmi et al. [36]. Also, students in states where there was a total lockdown experienced a significantly higher level of depression. This difference is logical, since states under lockdown had a higher number of cases of COVID, and the students must have felt more exposed to coronavirus infection, as well as being deprived of social gatherings or religious interaction. This is in agreement with what has been reported by some authors of studies involving higher institution students in China [45, 46]. Another interesting finding is the students’ responses regarding their willingness to speak to a health professional if they were experiencing anxiety or depression. Almost half (48.4%) of the students answered “Yes”, while about a fifth (17.6%) answered ‘No’; the rest were undecided. Two studies, carried out in 2017 and 2018 [47, 48], showed a negative attitude towards mental illness among young people in a secondary school and a University in Nigeria, respectively. Another study reported a more positive (accepting) attitude on the part of Pharmacy students [49].
On the whole, the factors that proved significant on univariate analysis and were included in the linear regression showed that not being able to afford three meals in a day, poor family functioning, having a chronic illness and residing in a state under total lockdown accounted for 14% of the depression seen among participants in the study.
Conclusions
In conclusion, the lockdown due to COVID-19 has placed a lot of psychological stress on university students; indeed, more than a third of those who participated in this study had varying degrees of anxiety and depression. It is recommended that measures such as financial support or the provision of food for needy families, counselling for dysfunctional families, and appropriate education and support for students with chronic illnesses be put in place in order to alleviate the psychological distress of these students. There is also a need to recommence academic activities through online engagement in order to positively channel the energy of university students.
Figures and tables
Fig. 1.
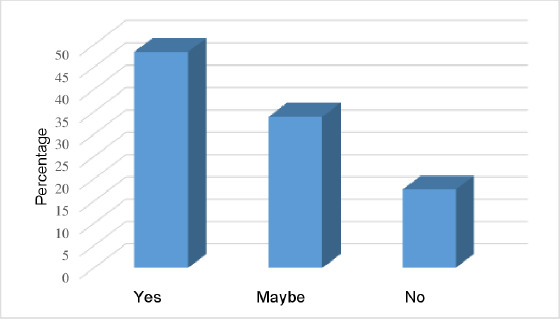
Reporting students’ willingness to speak to a health professional shows that about half of the students (48.4%) were willing to see a healthcare professional if they were feeling anxious or depressed.
Acknowledgements
Funding sources: this research did not receive any spe-cific grant from funding agencies in the public, commer-cial, or not-for-profit sectors.
The author especially thanks Professor G.O. Ademowo of the Institute for Advanced Medical Research and Training (IMRAT), College of Medicine, University of Ibadan for guidance regarding the online ethical application process. The author also acknowledges the students’ faculty representatives, who facilitated data collection. These are: Oluwatumininu Oma, Olamide Akinyemi, Temilola Akinditi, Chisom Okafor, Adanna Emeaghara, Elizabeth Okoye, Nkechi Nweya, Judith Onyekwere, Udochukwu Okeahialam, Chibueze Agwuncha, Ahmed Ajibade, Irewole Olumeyan, Adeola Olajide, Olalekan Michael Ajibola, John Fadele, Iyanuoluwa, Kene and Wole
Footnotes
Study limitations
The Hospital Anxiety and Depression scale (HADs) used in data collection does not distinguish between moderate and severe forms of the two psychological states.
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
LYO conceptualized and designed the study; reviewed literature, collected and analysed data; and wrote the manuscript
References
- [1].Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health 2020;5:e261-70. https://doi.org/10.1016/S2468-2667(20)30073-6 10.1016/S2468-2667(20)30073-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].World Health Organsation. Covid Prevalence. Available at: https://covid19.who.int (accessed 20/06/2020). [Google Scholar]
- [3].World Health Organsation. WHO Coronavirus (COVID-19) Dashboard with vaccination data. Available at: https://covid19.who.int (accessed 07/04/2021). [Google Scholar]
- [4].World Health Organsation. WHO concerned as COVID-19 cases accelerate in Africa. Available at: https://www.afro.who.int/news/who-concerned-covid-19-cases-accelerate-africa (accessed 20/06/2020). [Google Scholar]
- [5].Lone SA, Ahmad A. COVID-19 pandemic - An African perspective. Emerg Microbes Infect 2020;1-28. https://doi.org/10.1080/22221751.2020.1775132 10.1080/22221751.2020.1775132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 20/04/2020). [Google Scholar]
- [7].World Health Organization. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum. Available at: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum%0 (accessed on 20/06/2020). [Google Scholar]
- [8].Nigeria Centre for Disease Control. First case of corona virus disease confirmed in Nigeria. Available at: https://ncdc.gov.ng/news/227/first-case-of-corona-virus-disease-confirmed-in-nigeri (accessed 22/04/2020). [Google Scholar]
- [9].Nigeria Centre for Disease Control. Guideline on Social Distancing. Available: https://covid19.ncdc.gov.ng/media/files/Social_Distancing_Guide_2.pdf (accessed on 22/04/2020). [Google Scholar]
- [10].Nigeria Centre for Disease Control. COVID-19 microsite - Frequently asked questions. Available at: https://covid19.ncdc.gov.ng/faq (accessed 07/04/2021). [Google Scholar]
- [11].Premium Times. Nigeria shuts land borders. Available at: https://www.premiumtimesng.com/news/headlines/383448-just-in-coronavirus-nigeria-shuts-land-borders.html (accessed 22/05/2020). [Google Scholar]
- [12].National Universities Commision: Management of the Corona Virus (COVID-19) Pandemic. Available at: https://www.nuc.edu.ng/management-of-the-corona-virus-covid-19-pandemic (accessed 24/06/2020). [Google Scholar]
- [13].Premium Times. Lockdown Extension_ Buhari issues regulation backing action. Available at: https://www.premiumtimesng.com/news/387759-lockdown-extension-buhari-issues-regulation-backing-action.html (accessed 23/04/2020). [Google Scholar]
- [14].Sahara Reporters. Breaking: ASUU begins indefinite strike action. Available at: http://saharareporters.com/2020/03/23/breaking-asuu-begins-indefinite-strike-action (accessed 18/06/2020). [Google Scholar]
- [15].American Psychological Association. Adolescence: a unique period of challenge and opportunity for positive development. 2014. Available at: https://www.apa.org/pi/families/resources/newsletter/2014/12/adolescence-development (accessed 08/06/2020). [Google Scholar]
- [16].John A, Marchant AL, McGregor JI, Tan JOA, Hutchings HA, Kovess V, Choppin S, Macleod J, Dennis MS, Lloyd K. Recent trends in the incidence of anxiety and prescription of anxiolytics and hypnotics in children and young people: An e-cohort study. J Affect Disord 2015;183:134-41. https://doi.org/10.1016/j.jad.2015.05.002 10.1016/j.jad.2015.05.002 [DOI] [PubMed] [Google Scholar]
- [17].Adolescent mental health by Melling P. Available at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed 08/06/2020). [PubMed] [Google Scholar]
- [18].Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J.The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. A nationwide survey of psychological distress among Italian people during the covid-19 pandemic: Immediate psychological responses and associated factors. Int J Environ Res Public Health 2020;17:1-14. https://doi.org/10.3390/ijerph17093165 10.3390/ijerph17093165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang H, Xia Q, Xiong Z, Li Z, Xiang W, Yuan Y, Liu Y, Li Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS One 2020;15:1-10. https://doi.org/10.1371/journal.pone.0233410 10.1371/journal.pone.0233410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Huckins JF, Alex W, Wang W, Hedlund E, Rogers C, Wu J, Obuchi M, Murphy EI, Meyer ML, Wagner DD, Holtzheimer PE, Campbell AT. Mental Health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res 2020;22:1-13. https://doi.org/10.2196/20185 10.2196/20185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Vice Chancellor. History of the University of Ibadan. Available at: https://www.ui.edu.ng/HistoryVice%20Chancellor (accessed 24/04/2020). [Google Scholar]
- [23].American Writing Association. Sample size calculator - confidence level, confidence interval, sample size, population size, relevant population - creative research systems. Available at: https://www.surveysystem.com/sscalc.htm (accessed 28/05/2020). [Google Scholar]
- [24].Kim M, Park IH, Kang YS, Kim H, Jhon M, Kim JW, Ryu S, Lee JY, Kim JM, Lee J, Kim SW.Comparison of psychosocial distress in areas with different COVID-19 prevalence in Korea. Front Psychiatry 2020;11:1-9. https://doi.org/10.3389/fpsyt.2020.593105 10.3389/fpsyt.2020.593105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bjelland I, Dahl AA, Haug TT, ND. Hospital anxiety and depression scale - an updated literature review. J Psychosom Res 2002;52:69-77. https://doi.org/10.1016/S0022-3999(01)00296-3 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- [26].Abiodun OA. A Validity study of the hospital anxiety and depression scale in general hospital units and a community sample in Nigeria. Br J Psychiatry 1994;165:669-72. https://doi.org/10.1192/bjp.165.5.669 10.1192/bjp.165.5.669 [DOI] [PubMed] [Google Scholar]
- [27].Screening for depression in primary care. Available at: https://patient.info/doctor/screening-for-depression-in-primary-care (accessed 23/05/2020). [Google Scholar]
- [28].Bello CB, Irinoye O, Akpor OA. Health status of families: a comparative study of one-parent and two-parent families in Ondo State, Nigeria. Afr J Prm Health Care Med 2018;10:a1550. https://doi.org/10.4102/phcfm.v10i1.1550 10.4102/phcfm.v10i1.1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Duckett S. Family assessment device. Arch Phys Med Rehabil 1997;78:234. https://doi.org/10.1016/S0003-9993(97)90272-0 10.1016/S0003-9993(97)90272-0 [DOI] [PubMed] [Google Scholar]
- [30].Otekunrin O, Okon E, Otekunrin O. Analysis of candidates’ performance in Unified Tertiary Matriculation Examinations (UTME) and Post-UTME in the University of Ibadan, Nigeria. J Sci Res Reports 2017;14:1-8. https://doi.org/10.9734/JSRR/2017/34322 10.9734/JSRR/2017/34322 [DOI] [Google Scholar]
- [31].American Psychological Association. Women outnumber men in psychology, but not in the field’s top echelons. Available at: https://www.apa.org/monitor/2017/07-08/women-psychology (accessed 23/05/2020). [Google Scholar]
- [32].Graduate Study in Psychology 2017. Summary report: student demographics. 2016. Available at: https://www.apa.org/education/grad/survey-data/2017-student-demographics.pdf (accessed 26/05/2020). [Google Scholar]
- [33].Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17(5). https://doi.org/10.3390/ijerph17051729 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry 2020;33:1-4. https://doi.org/10.1136/gpsych-2020-100213 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Liu X, Liu J, Zhong X. Psychological state of college students during COVID-19 epidemic. SSRN Electron J 2020. https://doi.org/10.2139/ssrn.3552814 10.2139/ssrn.3552814 [DOI] [Google Scholar]
- [36].Al-Tammemi AB, Akour A, Alfalah L. Is it just about physical health? An online cross-sectional study exploring the psychological distress among university students in Jordan in the midst of COVID-19 pandemic. Front Psychol 2020;11:562213. https://doi.org/10.3389/fpsyg.2020.562213 10.3389/fpsyg.2020.562213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chang J, Yuan J, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 2020;40:171-6. https://doi.org/10.12122/j.issn.1673-4254.2020.02.06 10.12122/j.issn.1673-4254.2020.02.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].United Nations Department of Economics and social. Rural population - Nigeria - Data. United Nations population division’s world urbanization prospects: 2018 revision. Available at: https://data.worldbank.org/indicator/SP.RUR.TOTL?locations=NG (accessed 18/06/2020). [Google Scholar]
- [39].Ayandele O, Popoola O, Obosi A, Busari A. Depression, anxiety and smart phone addiction among young people in South West Nigeria. Covenant International Journal of Psychology 2019;4:1-14. [Google Scholar]
- [40].Odriozola-gonzález P, Planchuelo-gómez Á, Jesús M, de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res 2020;290:113108. https://doi.org/10.1016/j.psychres.2020.113108 10.1016/j.psychres.2020.113108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Fatiregun AA, Kumapayi TE. Prevalence and correlates of depressive symptoms among in-school adolescents in a rural district in southwest Nigeria. J Adolesc 2014;37:197-203. https://doi.org/10.1016/j.adolescence.2013.12.003 10.1016/j.adolescence.2013.12.003 [DOI] [PubMed] [Google Scholar]
- [42].Peltzer K, Pengpid S, Olowu S, Olasupo M. Depression and associated factors Among University students in Western Nigeria. J Psychol Africa 2013;23:459-65. https://www.tandfonline.com/doi/abs/10.1080/14330237.2013.10820652 10.1080/14330237.2013.10820652 [DOI] [Google Scholar]
- [43].Li Y, Wang Y, Jiang J, Valdimarsdóttir UA, Fall K, Fang F, Song H, Lu D, Zhang W. Psychological distress among health professional students during the COVID-19 outbreak. Psychological Medicine 2020:1-3. https://doi.org/10.1017/S0033291720001555 10.1017/S0033291720001555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Jianjun D, Tsingan L, Jiali W, Limei T. The effect of COVID-19 stress on sexual compulsivity symptom: the mediating role of perceived social support. Research Square (Preprint) 2020. https://doi.org/10.21203/rs.3.rs-17956/v1 10.21203/rs.3.rs-17956/v1 [DOI] [Google Scholar]
- [45].Huang L, Lei W, Xu F, Liu H, Yu L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: a comparative study. PLoS One 2020;15:e0237303. https://doi.org/10.1371/journal.pone.0237303 10.1371/journal.pone.0237303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, Chen S, Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord 2020;274:1-7. https://doi.org/10.1016/j.jad.2020.05.009 10.1016/j.jad.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Ogundele OA, Ogundele Y, Taha SM. Factors influencing adolescents stigmatising attitudes and perception of community reaction towards mental illness in Nigeria. Sudan J Med Sci 2017;12:240. https://doi.org/10.18502/sjms.v12i4.1355 10.18502/sjms.v12i4.1355 [DOI] [Google Scholar]
- [48].Jombo EH, Idung UA. Stigmatising Attitudes towards persons with mental illness among university students in Uyo, South-South Nigeria. Int J Heal Sci Res 2018;8:24-31. Available at: https://www.ijhsr.org/archive_ijhsr_vol.8_issue4.html [Google Scholar]
- [49].Anosike C, Ukwe CV, OA. Attitudes of pharmacy and non-pharmacy students towards mental illness in Nigeria: a comparative survey. Int J Pharm Pract 2020;28:346-54https://doi.org/10.1111/ijpp.12601 10.1111/ijpp.12601 [DOI] [PubMed] [Google Scholar]


