Summary
Introduction
Since the majority of cancers occur as a result of modifiable risk factors, cancer is being seen more as a preventable disease. The primary objective of our study was to assess the level of awareness of environmental risk factors of cancer among the Lebanese general population. The secondary objective focused on identifying the predictors of the preventability of the disease.
Methods
We conducted a cross-sectional study between June and July 2020. An online questionnaire was used to collect data pertaining to the knowledge of environmental risk factors of cancer, source of information and personal practice of the participants. Bivariate and multivariate analyzes were performed.
Results
About 387 respondents agreed to participate in the study. The study showed low awareness regarding infectious agents, lifestyle, diet and many work exposures. The predictors of the attitude of respondents regarding the preventability of cancer were: believing that cancer has an environmental cause (p=.014), not having a healthy lifestyle (p = 0.004), not smoking waterpipe (p = 0.023), being single (p = 0.013), and having a university degree (p = 0.049).
Conclusions
Efforts should be made to improve awareness of the cancer risk factors regarding infectious agents, lifestyle, diet and many work exposures. This can also be followed by further studies assessing the impact of these community and governmental cancer prevention initiatives on cancer risk factors level of awareness.
Keywords: Awareness, Cancer, Risk factors, Lebanese, Prevention
Introduction
Cancer is the second leading cause of death globally, accounting for an estimated 9.6 million deaths, or one in six deaths in 2018 [1]. In Lebanon, the risk of being diagnosed with cancer before the age of 75 is estimated to be 17.5% and 7,100 new cases of cancer are diagnosed each year [2].
According to the World Health Organization research, 35% of deaths caused by cancer worldwide are due to potentially preventable or modifiable risk factors. These risk factors are related to lifestyle, including smoking and alcohol consumption, infections, parasites, exposure to ultraviolet (UV) light and tanning using devices that emit UV radiation, environmental exposures, dietary factors, hormone replacement therapy, as well as exposure to ionizing radiation [3-6]. Worldwide, tobacco use causes the death of around 6 million people every year [7]. Cigarette smoking is the most harmful form of tobacco use, causing the largest cancer burden. Passive smoking, like actual smoking is also carcinogenic. Substances contained in tobacco smoke sediments remains chemically active and are harmful to health [7-9]. Moreover, the international agency for research on cancer (IARC) has classified alcohol as a Class I carcinogen for liver cancer [10, 11]. It also increases the risk of cancer of the mouth, throat, larynx, esophagus, liver and breast [10-12]. Diet also plays an important role in contributing to cancer development. Indeed, the World Cancer Research Fund Report 2007 estimates that 35% of the incidences of cancer worldwide can be linked to nutrition and lack of physical activity [13]. Epidemiological studies have also shown that obese patients with oncological treatment have worse prognoses and greater morbidity and mortality than those with normal Body Mass Index (BMI) [14, 15]. According to a synthetic analysis, infections are linked to about 15.4% of cancers worldwide [16], this percentage is variable between countries and was found to be approximately equal to half of the worldwide burden in Italy [17]. Another cancer risk factor is certain workplace exposures. The Centers for Disease Control and Prevention (CDC), estimates 3 to 6% of all cancers worldwide to be caused by exposures to carcinogens in the workplace [18]. Additionally, over 120 chemical or biological agents are classified as carcinogens by the IARC [19]. The main agents found to be contributing to the workplace cancer are asbestos, shift-work involving night work, mineral oils, solar radiation, silica, Diesel Engine Exhaust (DEE), coal tars and pitches, occupation as a painter or welder, dioxins, environmental tobacco smoke, radon, tetrachloroethylene, arsenic and strong inorganic acid mists [20]. Indoor radon could explain 10% of all lung cancer deaths each year in France [21]. To add, according to a recent study done in South-Eastern Italy, areas at higher radon concentrations seem to overlap with those characterized by the highest pulmonary cancer mortality and incidence rates, thus indicating that human exposure to radon could possibly enhance other individual or environmental pro-carcinogenic risk factors (i.e. cigarette smoking, air pollution and other exposures) [22]. Other important carcinogens that are found to be linked to cancer include bisphenol A, phthalates and naphthalene [23, 24], household cleaning products, plastic containers, indoor combustion, soot and wood dust [25].
Cancer prevention is a crucial step and the most cost-effective long-term strategy for the control of cancer specially in middle and low-income countries [26]. Prevention programs are an important weapon to fight against cancer, because they can contribute to reducing both the incidence of cancer and mortality [27]. The risk of getting cancer can be also reduced by making healthy choices. Keeping a healthy weight, avoiding tobacco, limiting the amount of alcohol you drink, eating a healthy diet with plenty of fruit and vegetables, exercising regularly, limiting alcohol use, practicing safe sex, reducing exposure to UV and ionizing radiations (occupational or medical diagnostic imaging), avoiding urban air pollution and indoor smoke from household use of solid fuels can all contribute to decreasing the risk of cancer [1].
Awareness of evidence-based risk factors is considered an important part of cancer prevention. Many studies were done in the US [28], UK [29]causing an estimated 9.6 million deaths in 2018. Low cancer symptom awareness has been associated with poor cancer survival for all cancers combined. The Cancer Awareness Measure (CAM, Japan [30], Tanzania [31], Nepal [32], Iran [33], UAE [34], Oman [35], Saudi Arabia [36], India [37]) to estimate the knowledge of people about cancer and its risk factors and to implement many public health interventions to increase awareness. The knowledge level differed between these countries. Other studies suggest that awareness of specific risk factors vary for different cancer types [38].
In Lebanon, several studies estimated the knowledge of risk factors of specific types of cancer like colorectal cancer [39], breast cancer [40] and cervical cancer. However, no studies were done to assess the level of public awareness concerning the evidence-based risk factors of cancer in general among the Lebanese general population. There is a need for such studies in Lebanon in order to know how to intervene and implement a prevention strategy specially that the cancer incidence in Lebanon is among the highest in the region and is expected to remain as such over the coming decade [41, 42]. Thus, the primary objective of this study was to assess the public awareness of environmental risk factors for cancer among the Lebanese general population. The secondary objective focused on identifying the predictors of the attitude of respondents regarding the preventability of the disease.
Materials and methods
STUDY DESIGN AND PARTICIPANTS
A descriptive cross-sectional study was conducted over a period of two months from June until July 2020 to estimate the awareness about the environmental risk factors of cancer among the Lebanese general population. The inclusion criteria included: being Lebanese aged 18 or more, residing in Lebanon, and speaking Arabic or English.
SAMPLE SIZE CALCULATION
To calculate the minimum sample size needed, Epi info was used. The expected frequency was set 50% because no similar study was conducted in the region and a margin error of 5% was also considered. Accordingly, 384 participants were required and targeted.
DATA COLLECTION TOOL
The tool used in this study was an online standardized questionnaire developed using google form. The questionnaire was based on literature review [19, 28-30, 34-36]. It consisted mainly of closed-ended, dichotomous (yes/no), multiple choice questions or a 5-point Likert type scale (1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree).
The questionnaire encompasses 3 main parts. The first part is entitled “demographic and general information” and was mainly to collect sociodemographic and background information about the participants. The second part is entitled “General knowledge about cancer and its environmental risk factors” and contained questions regarding 43 environmental cancer risk factors where the answer would be in the form of 5-point Likert scale. This part also included a question about if the participant thinks cancer is preventable or not and 3 questions regarding the participant source of information. The third part is entitled “personal practice” and was mainly designed to collect some information about the participant lifestyle. This section included questions about lifestyle habits and behaviors that can somehow reflect if the participant is trying to have a healthy lifestyle or not specially that these behaviors are self-controlled like smoking, waterpipe, alcohol consumption, red meat consumption, fruits and vegetables consumption, physical activity, high sugar food consumption and excessive exposure to sunlight. The questionnaire was first written in English, translated to Arabic and then back translated to English by another person. The objective of the questionnaire was provided at the beginning of the survey in the cover letter which included the purpose of the survey and the time needed to fill the questionnaire which is 5 to 10 minutes. To ensure face and content validity, the questionnaire was pilot tested and reviewed by three experts in the field of cancer.
RECRUITMENT OF PARTICIPANTS
Questionnaires were first sent electronically as a link using Google forms through social media applications. The response rate was estimated based on the percentage of people responding by Yes to the question asking them if they accept to participate in the study that was mainly considered as a consent. Although we couldn’t track the non-responders, reminder messages were sent again. A pilot study of 14 respondents was conducted to assess the clarity of the questionnaire in both languages and the validity and reliability of the Arabic version. Even though, this study doesn’t require any definite ethical approval but a verbal consent was obtained from all participants before filling the questionnaires by asking them if they want to participate in the study. All data were collected in a manner that respects participant’s anonymity and confidentiality.
STATISTICAL ANALYSIS
Analysis of data was carried out using the Statistical Program for Social Sciences (SPSS) version 21. Descriptive analysis was first performed to evaluate the distribution of the socio-demographic characteristics of the participants, their lifestyle behaviors, their knowledge about cancer and its environmental risk factors, and their source of information. The dependent variable is a dichotomous variable: cancer preventable or not. Bivariate analysis was done for all variables related to sociodemographic, cancer history, cancer cause and practice. Since all of our variables are categorical variables, the Chi square and Fisher exact tests were used when applicable. The Cochran Armitage trend test was performed for categorical variables following a specific order such as age, BMI, income, education and variables related to practice. Differences with a two-tailed p-value < 0.05 were considered as statistically significant. Multivariate analysis using logistic regression was also performed. Since the number of participants is less than 500 the forward LR method was used. The entered variables are the variables having a p-value < 0.2 in the bivariate analysis. The adjusted odds ratio (OR) and 95% confidence intervals generated by the multiple logistic regression models were used to describe the relationship of the entered variables with the attitude of the participants toward the preventability of cancer. To test the reliability between the questions related to the same risk factor in the questionnaire, we used Cronbach alpha. To ensure construct validity of our questionnaire, a factor analysis was performed considering all the environmental risk factors. Our items were all in the form of Likert scale. Then, to ensure the reliability of the questionnaire, Cronbach alpha of the whole list of environmental risk factors was calculated.
Results
PARTICIPANTS BASELINE CHARACTERISTICS
Only 387 individuals accepted to participate in our study with 99.5% participation rate. In total, 207 participants were women (53.5%) while 180 were men (46.5%). Most of our participants were young where 52.7% of them were aged between 18 and 24 and only 3.1% were 65 years or above. Most of the participants were single (63.8%) and were from different regions in Lebanon. To note here, 56.3% of the participants were living in urban places while 43.7% lived in rural places. The majority of the participants (84.0%) completed one or more university degree. It should be noted that 80.1% of the participants didn’t work in the medical field. The majority of the participants (95.1%) didn’t undergo any cancer screening, and didn’t have cancer (97.2%) (Tab. I).
Tab. I.
The socio-demographic characteristics of the study population.
| Variable | Categories | Frequency (n = 387) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 180 | 46.5 |
| Female | 207 | 53.5 | |
| Age | 18-24 | 204 | 52.7 |
| 25-44 | 120 | 31 | |
| 45-64 | 51 | 13.2 | |
| 65 or above | 12 | 3.1 | |
| Marital | Single | 247 | 63.8 |
| Married | 128 | 33.1 | |
| Divorced | 6 | 1.6 | |
| Widowed | 6 | 1.6 | |
| Education level | Elementary/intermediate/high school | 62 | 16.1 |
| Bachelor’s degree | 215 | 55.6 | |
| Master’s or PhD degree | 110 | 28.4 | |
| PhD | |||
| Income | < 675 000 LBP | 49 | 12.7 |
| 675 000-999 000 | 46 | 11.9 | |
| 1 000 000-1 999 000 | 110 | 28.4 | |
| 2 000 000-2 999 000 | 76 | 19.6 | |
| 3 000 000 or above | 106 | 27.4 | |
| Working in the medical field | No | 310 | 80.1 |
| Yes | 77 | 19.9 | |
| Region | North | 42 | 10.9 |
| South | 65 | 16.8 | |
| Beirut | 96 | 24.8 | |
| Beqaa | 27 | 7.0 | |
| Mount Lebanon | 81 | 20.9 | |
| Nabatiyeh | 30 | 7.8 | |
| Akkar | 21 | 5.4 | |
| Baalback/hermel | 25 | 6.5 | |
| Living place | Urban | 218 | 56.3 |
| Rural | 169 | 43.7 | |
| Cancer screening | No | 368 | 95.1 |
| Yes | 19 | 4.9 | |
| Having cancer | No | 376 | 97.2 |
| Yes, I had | 2 | .5 | |
| Yes, I’m currently having | 9 | 2.3 | |
| Know someone having cancer | No | 100 | 25.8 |
| Yes | 287 | 74.2 | |
| Occupation | Unemployed | 179 | 46.3 |
| Agriculture | 9 | 2.3 | |
| Manufacturing | 4 | 1.0 | |
| Trade | 42 | 10.9 | |
| Transport, Post and telecom | 11 | 2.8 | |
| Services/Financial intermediation/insurance | 119 | 30.7 | |
| Retired | 8 | 2.1 | |
| Other/not specified | 15 | 3.9 |
KNOWLEDGE ABOUT RISK FACTORS OF CANCER AND ATTITUDE REGARDING THE PREVENTION OF THIS DISEASE
The majority of our participants have heard information about cancer (89.9%). Internet (74.2%) was the most common source of information about cancer in general. The most preferred sources identified by the participants to receive information concerning environmental risk factors of cancer were healthcare professionals (51.9%) and internet sources (43.7%).
Approximately 86 % of the respondents agreed that the cause of cancer is both genetic and environmental and 56 % agreed that cancer could be preventable (Fig. 1).
Fig. 1.
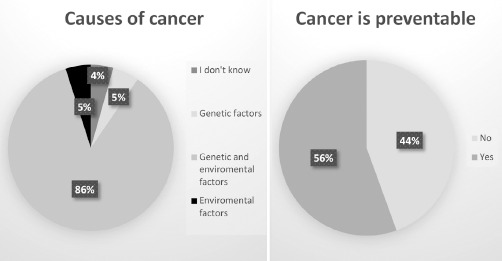
Descriptive analysis of cancer causes and preventability.
The environmental risk factors of cancer positively identified by the participants were environmental pollution (91.5%), smoking (90.4%), industrial pollution (88.3%), nuclear rays (85.5%), UV radiation (83.5%), X rays (72.6%), tobacco exposure (72.4%), processed food (72.1%), long term use of preservatives (68.8%), excessive sunlight exposure (65.9%), artificial sweeteners (65.3%), pesticides (65.4%), genetically modified food (65.2%), uranium (64.9%), high sugar diet (63.4%), living close to high voltage transmission lines (62.0%), alcohol (61.8%), stress (58.7%), plastic bottles (58.4%), hormone in beef (51.9%), red meat (50.9%), diesel exhaust (49.9%), unbalanced diet (49.8%), mobile phones (48.3%), paints (48.3%), obesity (45.5%), and hormonal treatment after menopause (45.0%).
Low awareness was found among the following factors: benzene (43.1%), low fiber diet (40.1%), low physical activity (38.2%), infections (36.6%), naphthalene (36.4%), many sexual partners (36.4%), radon (32.3%), asbestos (31.8%), arsenic (31.5%), vitamin D deficiency (31.5%), phthalates (27.6%), bisphenol A (27.1%), breastfeeding for less than 6 months (23.5%) and wood dusts (19.4%). To note, only a small percentage of participants disagreed with the fact of considering coffee and Mediterranean diet as risk factors of cancer (33.3% and 15.8% respectively) (Fig. 2).
Fig. 2.

Knowledge of the participants of the environmental cancer risk factors.
THE PARTICIPANT’S LIFESTYLE CHARACTERISTICS
Half of the participants (51.7%) considered themselves living an unhealthy lifestyle and 82.4% considered themselves living in an unhealthy environment. About 67.7% of the participants were non-smokers and 54.0% didn’t smoke waterpipe. The majority of the participants didn’t drink alcohol (83.2%) and most of the participants exercised for 30 minutes 3 times per week but with different frequencies (78.9%). About 30.2% of the participants eat five fruits and vegetables per day most of the time. Only 11.9% of the participants consume red meat more than three times per week while 75.4% consume red meat less than 3 times and 12.7% don’t consume red meat at all. In addition, 9.0% of the participants don’t consume high sugar food and only 25.1% don’t expose themselves excessively to sunlight. To note, almost half of the participants (48.3%) had a normal BMI, 35.4% were overweight, and 11.6% were obese (Tab. II).
Tab. II.
Table summarizing the lifestyle of the participants.
| Variables | Categories | Frequency (n = 387) | Percentage (%) |
|---|---|---|---|
| Healthy lifestyle | No | 200 | 51.7 |
| Yes | 187 | 48.3 | |
| Healthy environment | No | 319 | 82.4 |
| Yes | 68 | 17.6 | |
| Cigarette smoking | No | 262 | 67.7 |
| Yes, more than 20 cigarettes per day | 28 | 7.2 | |
| Yes, less than 20 cigarettes per day | 48 | 12.4 | |
| Sometimes | 21 | 5.4 | |
| Rarely | 28 | 7.2 | |
| Water pipe smoking | No | 209 | 54.0 |
| Yes, everyday | 51 | 13.2 | |
| Most of the times | 29 | 7.5 | |
| Sometimes | 41 | 10.6 | |
| Rarely | 57 | 14.7 | |
| Alcohol intake | No | 322 | 83.2 |
| Yes, not more than 1 drink per day | 5 | 1.3 | |
| Sometimes | 24 | 6.2 | |
| Rarely | 36 | 9.3 | |
| Doing at least 30 mins of physical activity 3 times per week | No | 82 | 21.2 |
| Yes, always | 79 | 20.4 | |
| Most of the times | 68 | 17.6 | |
| Sometimes | 80 | 20.7 | |
| Rarely | 78 | 20.2 | |
| Eating at least 5 fruits and vegetables per day | No | 55 | 14.2 |
| Yes, everyday | 54 | 14.0 | |
| Most of the times | 117 | 30.2 | |
| Sometimes | 112 | 28.9 | |
| Rarely | 49 | 12.7 | |
| Consuming red meat | No | 49 | 12.7 |
| Yes, more than 3 times weekly | 46 | 11.9 | |
| Yes, 3 times weekly | 120 | 31.0 | |
| Sometimes (up to 3 times/month) | 83 | 21.4 | |
| Rarely | 89 | 23.0 | |
| Consuming high sugar food | No | 35 | 9.0 |
| Yes, everyday | 28 | 7.2 | |
| Most of the times | 73 | 18.9 | |
| Sometimes | 152 | 39.3 | |
| Rarely | 99 | 25.6 | |
| Being exposed excessively to sunlight | No | 97 | 25.1 |
| Yes, everyday | 12 | 3.1 | |
| Most of the times | 44 | 11.4 | |
| Sometimes | 104 | 26.9 | |
| Rarely | 130 | 33.6 | |
| BMI | Underweight (< 18.5) | 18 | 4.7 |
| Normal (18.5 through 24.99) | 187 | 48.3 | |
| Overweight (25 through 29.99) | 137 | 35.4 | |
| Obese (30 or above) | 45 | 11.6 |
BMI: Body Mass Index; Underweight < 18.5; Normal: Between 18.5 and 24.99; Overweight: Between 25 and 29.99; Obese > 30.
SOCIODEMOGRAPHIC CHARACTERISTICS AND ATTITUDE REGARDING THE PREVENTABILITY OF THE DISEASE
Regarding the sociodemographic characteristics of the participants, the variables that were found to be significantly associated with the attitude of patients regarding the preventability of cancer were: gender (p = 0.014), age (p = 0.000), education (p = 0.001), occupation (p = 0.000), region (p = 0.000), medical field (p = 0.064), living place (p = 0.041), having cancer (p = 0.003), and knowing a family member or a friend having cancer (p = 0.015) (Tab. III).
Tab. III.
Sociodemographic characteristics and the attitude regarding preventability of cancer.
| Variable | Cancer not preventable (N = 172) | Cancer preventable (N = 215) | |||
|---|---|---|---|---|---|
| n | % | n | % | P-value | |
| Gender | 0.014† | ||||
| Male | 92 | 53.5% | 88 | 40.9% | |
| Female | 80 | 46.5% | 127 | 59.1% | |
| Marital | 0.000† | ||||
| Single | 88 | 51.2% | 159 | 74.0% | |
| Married/Divorced/Widowed | 84 | 48.8% | 56 | 26.0% | |
| Age | 0.000† 0.000‡ |
||||
| 18-24 | 76 | 44.2% | 128 | 59.5% | |
| 25-44 | 53 | 30.8% | 67 | 31.2% | |
| 45-64 | 33 | 19.2% | 18 | 8.4% | |
| 65 and above | 10 | 5.8% | 2 | 0.9% | |
| Education | 0.001† | ||||
| Elementary/intermediate/ high school | 33 | 19.2% | 29 | 13.5% | |
| Bachelor’s degree | 107 | 62.2% | 108 | 50.2% | |
| Master’s or PhD degree | 32 | 18.6% | 78 | 36.3% | |
| Occupation | 0.000¥ | ||||
| Unemployed | 79 | 45.9% | 100 | 46.5% | |
| Agriculture | 8 | 4.7% | 1 | 0.5% | |
| Manufacturing | 2 | 1.2% | 2 | 0.9% | |
| Trade | 23 | 13.4% | 19 | 8.8% | |
| Transport | 8 | 4.7% | 3 | 1.4% | |
| Services | 40 | 23.3% | 79 | 36.7% | |
| Retired | 7 | 4.1% | 1 | 0.5% | |
| Not specified/other | 5 | 2.9% | 10 | 4.7% | |
| Income | 0.303† 0.759‡ |
||||
| <675 000 LBP | 19 | 11.0% | 30 | 14.0% | |
| 675 000-999 000 | 18 | 10.5% | 28 | 13.0% | |
| 1 000 000-1 999 000 | 53 | 30.8% | 57 | 26.5% | |
| 2 000 000-2 999 000 | 40 | 23.3% | 36 | 16.7% | |
| 3 000 000 or above | 42 | 24.4% | 64 | 29.8% | |
| Region | 0.000† | ||||
| North | 19 | 11.0% | 23 | 10.7% | |
| South | 29 | 16.9% | 36 | 16.7% | |
| Beirut | 28 | 16.3% | 68 | 31.6% | |
| Beqaa | 20 | 11.6% | 7 | 3.3% | |
| Mount Lebanon | 30 | 17.4% | 51 | 23.7% | |
| Nabatiyeh | 20 | 11.6% | 10 | 4.7% | |
| Akkar | 7 | 4.1% | 14 | 6.5% | |
| Baalbeck/Hermel | 19 | 11.0% | 6 | 2.8% | |
| Working in the medical field | 0.064† | ||||
| No | 145 | 84.3% | 65 | 76.7% | |
| Yes | 27 | 15.7% | 50 | 23.3% | |
| Living place: | 0.041† | ||||
| Urban | 87 | 50.6% | 131 | 60.9% | |
| Rural | 85 | 49.4% | 84 | 39.1% | |
| Cancer screening | 0.461† | ||||
| No | 162 | 94.2% | 206 | 95.8% | |
| Yes | 10 | 5.8% | 9 | 4.2% | |
| Had cancer | 0.003¥ | ||||
| No | 162 | 94.2% | 214 | 99.5% | |
| Yes, had cancer or currently having | 10 | 5.8% | 1 | 0.5% | |
| Know a friend or family member having cancer | 0.015† | ||||
| No | 34 | 19.8% | 66 | 30.7% | |
| Yes | 138 | 80.2% | 149 | 69.3% | |
†: chi square;
‡: Cochrane;
¥: fisher.
The variables found to be significantly associated with the attitude of patients regarding the preventability of cancer were: BMI (p = 0.000), having a healthy life (p = 0.015), smoking (p = 0.000), waterpipe (p = 0.000) and alcohol (p = 0.055) (Tab. IV).
Tab. IV.
Association between lifestyle and attitude regarding preventability of cancer.
| Cancer not preventable | Cancer preventable | ||||
|---|---|---|---|---|---|
| n | % | n | % | P-value | |
| BMI | Variable | ||||
| Underweight | 3 | 1.7% | 15 | 7.0% | |
| Normal | 67 | 39.0% | 120 | 55.8% | |
| Overweight | 74 | 43.0% | 63 | 29.3% | |
| Obese | 28 | 16.3% | 17 | 7.9% | |
| Healthy life | 0.015† | ||||
| No | 77 | 44.8% | 123 | 57.2% | |
| Yes | 95 | 55.2% | 92 | 42.8% | |
| Healthy environment | 0.256† | ||||
| No | 146 | 84.9% | 173 | 80.5% | |
| Yes | 26 | 15.1% | 42 | 19.5% | |
| Smoking | 0.000† 0.000‡ |
||||
| No | 94 | 54.7% | 168 | 78.1% | |
| Rarely | 17 | 9.9% | 11 | 5.1% | |
| Sometimes | 15 | 8.7% | 6 | 2.8% | |
| Yes less than 20 cigarettes per day | 26 | 15.1% | 22 | 10.2% | |
| Yes more than 20 cigarettes per day | 20 | 11.6% | 8 | 3.7% | |
| Water pipe | 0.000† 0.000‡ |
||||
| No | 66 | 38.4% | 143 | 66.5% | |
| Rarely | 32 | 18.6% | 25 | 11.6% | |
| Sometimes | 26 | 15.1% | 15 | 7.0% | |
| Most of the times | 22 | 12.8% | 7 | 3.3% | |
| Yes everyday | 26 | 15.1% | 25 | 11.6% | |
| Alcohol | 0.055¥ 0.084‡ |
||||
| No | 137 | 79.7% | 185 | 86.0% | |
| Rarely | 4 | 2.3% | 1 | 0.5% | |
| Sometimes | 9 | 5.2% | 15 | 7.0% | |
| Not more than 1 drink per day | 22 | 12.8% | 14 | 6.5% | |
| Eating > 5 fruits and vegetables per day | 0.210† 0.023‡ |
||||
| No Rarely Sometimes Most of the times Everyday |
19 20 46 59 28 |
11.0% 11.6% 26.7% 34.3% 16.3% |
36 29 66 58 26 |
16.7% 13.5% 30.7% 27.0% 12.1% |
|
| Exercising for 30 minutes 3 times per week | 0.424† 0.479‡ |
||||
| No Rarely Sometimes Most of the times Always |
43 33 30 30 36 |
25.0% 19.2% 17.4% 17.4% 20.9% |
39 45 50 38 43 |
18.1% 20.9% 23.3% 17.7% 20.0% |
|
| Eating red meat | 0.104† 0.210‡ |
||||
| No Rarely Sometimes (up to 3 times per month) Yes, equal or less than 3 times weekly Yes, more than 3 times weekly |
22 50 30 50 20 |
12.8% 29.1% 17.4% 29.1% 11.6% |
27 39 53 70 26 |
12.6% 18.1% 24.7% 32.6% 12.1% |
|
| Eating high sugar food | 0.631† 0.195‡ |
||||
| No Rarely Sometimes Most of the times Every day |
17 48 68 27 12 |
9.9% 27.9% 39.5% 15.7% 7.0% |
18 51 84 46 16 |
8.4% 23.7% 39.1% 21.4% 7.4% |
|
| Exposed excessively to sunlight | 0.645† 0.617‡ |
||||
| No Rarely Sometimes Most of the times Everyday |
48 56 41 21 6 |
27.9% 32.6% 23.8% 12.2% 3.5% |
49 74 63 23 6 |
22.8% 34.4% 29.3% 10.7% 2.8% |
|
BMI: Body Mass Index; Underweight < 18.5; Normal: between 18.5 and 24.99; Overweight: between 25 and 29.99; Obese > 30;
†: chi square;
‡: Cochrane; ¥: fisher.
THE PREDICTORS OF THE ATTITUDE OF RESPONDENTS REGARDING THE PREVENTABILITY OF CANCER
In the multivariate model, cancer was considered more as preventable when the participants considered the cause of cancer is environmental, OR=18.648 (95% CI: 1.81-191.65, p = 0.014). People having a healthy life considered more than those who didn’t that cancer is non-preventable, OR = 0.49 (95% CI: 0.3-0.8, p = 0.004). Participants smoking waterpipe with different frequencies considered that cancer is not preventable. For rarely smokers, the OR was 0.46 (95% CI: 0.24-0.9, p = 0.023). Married participants considered that cancer is non-preventable, OR = 0.52 (95% CI: 0.31-0.87, p = 0.013). Participants having a high educational degree considered that cancer is preventable, OR = 2.18 (95% CI: 1.0-4.74, p = 0.049). Participants having cancer considered more than people who didn’t that cancer is non-preventable, OR = 0.14 (95% CI: 0.02-1.14, p = 0.066) (Tab. V).
Tab. V.
The predictors of the preventability of cancer.
| Variables | ORa | 95% CI | P-value |
|---|---|---|---|
|
Cancer cause Don’t Know Genetic Environmental Both genetic and environmental |
1 0.351 18.648 0.892 |
Ref 0.071-1.720 1.814-191.651 0.281-2.829 |
0.013 0.197 0.014 0.846 |
|
Healthy life No Yes |
1 0.485 |
Ref 0.297-0.790 |
0.004 |
|
Water pipe No Rarely Sometimes Most of the times Everyday |
1 0.462 0.268 0.114 0.362 |
Ref 0.238-0.899 0.124-0.576 0.040-0.323 0.178-0.738 |
0.000 0.023 0.001 0.000 0.005 |
|
Marital status Single Married |
1 0.520 |
Ref 0.309-0.873 |
0.013 |
|
Education Elementary/intermediate/ high school Bachelor degree Masters or PhD |
1 0.913 2.179 |
Ref 0.449-1.859 1.002-4.736 |
0.008 0.803 0.049 |
|
Have cancer No Yes |
1 0.135 |
Ref 0.016-1.141 |
0.066 |
ORa: adjusted Odds Ratio; omnibus test: significant so at least the variable is associated with the dependent variable; model summary: Nagelnerke R square 0.299 so the model was able to explain 29.9% of the variability of the dependent variable; Hosmer Lemshow was not significant (0.153) so the model is adequate; classification table showed that 71.1% of the participants had good classification; correlation matrix: all R s were < 0.8 so no variables were over correlated.
RELIABILITY AND VALIDATION OF THE SCALE
The alpha coefficient of the three following risk factors: naphthalene, phthalates and paints, the two factors sunlight and UV radiation, multiple sex partners and infections, diesel and benzene were respectively 0.697, 0.619, 0.569, 0.583. Their alpha coefficients are above 0.5 suggesting that the items have good internal consistency. The alpha coefficient of the 2 items arsenic and pesticides 0.423, bisphenol A and plastic 0.423 were low suggesting low internal consistency between the items. The results of the exploratory factor analysis suggested that our items were able to explain 62.66% of the variability of our latent variable or awareness of environmental risk factors of cancer. In this study, the Kaiser-Meyer-Olkin statistic was 0.929. This means that the data are suitable for performing factor analysis. The result of the Bartlett test was also significant. This means that the opposite assumption was confirmed and there was a significant correlation between variables (p < 0.001). Cronbach’s alpha of all scale-items was equal to 0.95.
Discussion
Cancer has a big impact on the patient’s life, physically, emotionally and financially. Thus, the most important step is the prevention of cancer occurrence when it is possible. As cancer has been linked to many preventable environmental risk factors [1], having a good knowledge about these risk factors is an essential step to help prevent and reduce the burden of this disease [26].
Our study showed that more than half of our sample had recognized the following factors as risk factors of cancer: environmental pollution, smoking, industrial pollution, nuclear rays, UV radiation, X rays, tobacco exposure, processed food, long term use of preservatives, excessive sunlight exposure, artificial sweeteners, pesticides, genetically modified food, uranium, high sugar diet, living close to high voltage transmission lines, alcohol, stress, plastic bottles, hormone in beef and red meat. On the other hand, less than 50% of the participants had recognized the following factors: diesel exhaust, unbalanced diet, mobile phones, paints, obesity, hormonal treatment after menopause, benzene, low fiber diet, low physical activity, infections, naphthalene, many sexual partners, radon, asbestos, arsenic, vitamin D deficiency, phthalates, bisphenol A, breastfeeding for less than 6 months and wood dusts.
In 2001, the American Institute for Cancer Research (AICR) commissioned its first Cancer Risk Awareness Survey to gauge Americans’ awareness of various lifestyle-related cancer risk factors. In 2019, they reported that less than half of Americans recognize that alcohol, diets high in red meat, diets low in vegetables, fruits, and fiber and insufficient physical activity all have a clear link to cancer development [28]. Our results were similar to that of the AICR 2019 survey except for alcohol and red meat where more than half of the Lebanese population did identify them as risk factors of cancer. This survey also showed that the awareness of other established cancer risk factors like obesity and processed meat is above 50% among Americans. This wasn’t the same in our study where less than half of the participants identified obesity as a risk factor for cancer. The majority of Americans correctly identified tobacco (89%) and excessive exposure to sunlight (82%) as cancer risks [28] and this was similar to our results.
Our results were not in line with a previous Japanese study that showed that the attributable fraction of cancer-causing viral and bacterial infection was considered the highest (51%), followed by that of tobacco smoking (43%), stress (39%), and endocrine-disrupting chemicals (37%) [30]. Thus, it is worth increasing awareness about infectious agents as a cause of cancer.
A study done in Iran in 2010 to assess the public awareness of cancer risk factors and its determinants showed that a small proportion of the respondents (12.2%) had high knowledge level and most of them had mixed (56.9%) and low level of awareness (30.9%). The most important determinants of knowledge level included level of education, gender, and family history [33].
Our results were also aligned with the results of a pilot study done in Emirates showing that many of the study participants were able to identify smoking, alcohol, and nuclear radiation as cancer-causing factors, but a large number of the respondents failed to identify infections, some food-related contaminants/components, and occupation-associated carcinogens as risk factor [34]. These results emphasize on the need of an awareness campaign concerning occupation-associated carcinogens.
Our results were very close to the results of a study done in Oman. Similarly to our results, the majority of respondents identified that smoking cigarettes (83.3%), passive smoking (72.7%) and excessive drinking of alcohol (69.0%) are risks factors for cancer while fewer respondents identified that eating less fruits and vegetables (21.6%), eating more red or processed meat (30.2%), being overweight (32.0%), doing less physical exercise (31.0%), having a close relative with cancer (34.9%) and getting frequent sunburn during childhood (38.8%) are risk factors contributing for the development of cancer [35].
The level of awareness is high in both western and Arab countries concerning smoking. It is important to highlight that the majority of the respondents are also aware that drinking alcohol is also a risk factor for cancer, which could be explained by the cultural stigma in these countries where smoking and alcohol are seen as unhealthy [43].
Concerning the western dietary pattern and lifestyle, the level of awareness was low in all countries and similar in Lebanon except for red meat and processed food where we had a better knowledge. Indeed, the western dietary pattern including red and processed meat and refined grains and sedentary lifestyles are associated with increase in the risk of cancer [44]. Low fruit and vegetable intake, smoking, drinking of alcohol and obesity were still the leading risk factors for death from cancer worldwide [45]. Giovannucci et al, found that a healthy lifestyle can prevent 40% of cancer cases and 50% of cancer deaths in the United States. Thus, it is important to raise awareness about the importance of adopting a healthy lifestyle [46].
Concerning the source of information of our participants, internet sources was the most common source of information followed by healthcare professionals and the most preferred sources identified were healthcare professionals (51.9%) and internet sources (43.7%). While our study population favored being educated through healthcare professionals, in the pilot study done in Emirates, respondents favored being educated via the media [34].
Concerning the attitude towards the preventability of cancer, 56% of our participants perceived that cancer is preventable and 44% considered cancer as non-preventable. Our results were similar to a study done in Mumbai where 55% of the participants perceived that cancer could be preventable [47]. However, in a study done in India, the majority of the study population (42%), perceived cancer could not be preventable, and around 30% of them did not know what to perceive about the preventive methods for cancer [48].
Concerning the predictors of the attitude of our participants toward the preventability of cancer, it is important to highlight that the main predictor is believing that cancer has an environmental cause. This is a logical result, since the environmental risk factors are usually preventable unlike the genetic ones. Participants considering cancer is preventable considered at the same time that they are not living a healthy lifestyle, which showed that they underestimate the impact of taking health precautions in preventing cancer. This result can also reflect that these participants are feeling guilty and that’s why they are considering themselves not living a healthy lifestyle. Another important result is that waterpipe remained in the multivariate model while smoking was removed, this reflects the Lebanese profile where waterpipe is a cultural habit and the prevalence of waterpipe smoking has increased extensively [49,50]. This result also shows that people smoking waterpipe are not aware that waterpipe can increase the risk of cancer. Married participants considered less that cancer is preventable this could be related to age and level of education. Participants having cancer considered more that cancer is not preventable, due to the fact that many of these patients take precautions but couldn’t stop cancer from occurring.
To our knowledge, this is the first study assessing the knowledge of the Lebanese population toward the general environmental risk factors of cancer. Another strong point in this study is that it achieved the minimum sample size needed and this increase the power of study. Concerning the questionnaire, it was strongly built based on good literature review and covered a lot of risk factors and in some cases, the question was asked in different ways to ensure that the questionnaire truly reflects what the participant knows in order to decrease the classification bias. The Cronbach alpha reflecting the reliability of the knowledge questionnaire was high (0.95). However, the calculated alpha coefficient was low for the bisphenol A and plastic and for the arsenic and pesticides. This shows that the participants are not able to identify what is the scientific name of the substance causing cancer leading to a classification bias. The questionnaire included mainly closed ended questions which makes it easier for respondents and to have fewer missing answers. Only in questions where the respondents can be frustrated because their desired answer is not a choice (like when asked about the preferred information source etc.) an option where the respondent can write a short answer was added. In questions concerning the knowledge of the participants concerning the environmental risk factors a Likert scale was used to have more precise answers thus removing the classification bias.
On the other hand, this study has some limitations. This study was done during the COVID-19 pandemic so we couldn’t fill the questionnaires face to face with the participants. First, we had difficulty reaching certain types of participants, such as those who do not have internet access and thus our sample had more young people which increase the selection bias. Second, there is no identification tool so it is impossible to know if the sample providing answers is the right person or if one person is submitting multiple responses. Third, since the questionnaire was distributed through the internet, we couldn’t control effectively its spread and we couldn’t know the exact response rate and the number of people ignoring our questionnaire. Finally, according to the Lebanese statistical Bulletin 2018 [51], 21.92% of the Lebanese population live in Akkar and the North, 14.46% in Beqaa and Baalbek, 7.81 in Nabatieh, 11.67% in the South, 34.85% in mount Lebanon and 9.3 % Beirut. While, in our study 24.8% of our participants were living in Beirut, 20.9% in Mount Lebanon, 16.8% in South, 16.3% in North and Akkar, 7.8% in Nabatieh,13.5% in Beqaa and in Baalback/Hermel. Thus, our results may overestimate the results in Beirut and South and underestimate it in Mount Lebanon. To add, our sample was selected using mostly the convenience sampling method, this can lead to selection bias and can affect the generalizability of the results.
Conclusions
Cancer is a multi-factorial disease having both environmental and genetic risk factors. Our results increase the need for more health campaigns to increase awareness on these risk factors specially those related to toxic substances and infections and lifestyle habits. This can also be followed by further studies assessing the impact of these community and governmental cancer prevention initiatives on cancer risk factors level of awareness.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any spe-cific grant from funding agencies in the public, commer-cial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
MK performed study, collected data, analyzed data and drafted the manuscript.
MEH, DK, SA, SR, AAH reviewed, edited the manuscript and approved the final version of the manuscript to be submitted.
RA designed study, analyzed data, reviewed and approved the final version of the manuscript to be submitted.
References
- [1].World Health Organization. Cancer. 2020. Available at: https://www.who.int/health-topics/cancer#tab=tab_1 (accessed July 17, 2020).
- [2].Cancerindex. Lebanon cancer oranisations and resources. 2020.Available at: http://www.cancerindex.org/Lebanon (accessed July 17, 2020).
- [3].Weiderpass E. Lifestyle and cancer risk. J Prev Med Pub Health 2010;43:459. https://doi.org/10.3961/jpmph.2010.43.6.459 10.3961/jpmph.2010.43.6.459 [DOI] [PubMed] [Google Scholar]
- [4].Chen Y-C, Hunter DJ. Molecular epidemiology of cancer. CA Cancer J Clin 2005;55:45-54. https://doi.org/10.3322/canjclin.55.1.45 10.3322/canjclin.55.1.45 [DOI] [PubMed] [Google Scholar]
- [5].Aricò M, Schrappe M, Hunger SP, Carroll WL, Conter V, Galimberti S, Manabe A, Saha V, Baruchel A, Vettenranta K, Horibe K, Benoit Y, Pieters R, Escherich G, Silverman LB, Pui C-H, Valsecchi MG. Clinical outcome of children with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia treated between 1995 and 2005. J Clin Oncol 2010;28:4755-61. https://doi.org/10.1200/JCO.2010.30.1325 10.1200/JCO.2010.30.1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Monsalve J, Kapur J, Malkin D, Babyn PS. Imaging of cancer predisposition syndromes in children. RadioGraphics 2011;31:263-80. https://doi.org/10.1148/rg.311105099 10.1148/rg.311105099 [DOI] [PubMed] [Google Scholar]
- [7].Leon ME, Peruga A, McNeill A, Kralikova E, Guha N, Minozzi S, Espina C, Schüz J. European code against cancer, 4th Edition: tobacco and cancer. Cancer Epidemiol 2015;39:S20-33. https://doi.org/10.1016/j.canep.2015.06.001 10.1016/j.canep.2015.06.001 [DOI] [PubMed] [Google Scholar]
- [8].Thomas JL, Guo H, Carmella SG, Balbo S, Han S, Davis A, Yoder A, Murphy SE, An LC, Ahluwalia JS, Hecht SS. Metabolites of a tobacco-specific lung carcinogen in children exposed to secondhand or thirdhand tobacco smoke in their homes. Cancer Epidemiol Biomarkers Prev 2011;20:1213-21. https://doi.org/10.1158/1055-9965.EPI-10-1027 10.1158/1055-9965.EPI-10-1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cogliano VJ, Baan R, Straif K, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Wild CP. Preventable exposures associated with human cancers. JNCI J Natl Cancer Inst 2011;103:1827-39. https://doi.org/10.1093/jnci/djr483 10.1093/jnci/djr483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Franceschi S, Bidoli E, Herrero R, Muñoz N. Comparison of cancers of the oral cavity and pharynx worldwide: etiological clues. Oral Oncol 2000;36:106-15. https://doi.org/10.1016/S1368-8375(99)00070-6 10.1016/S1368-8375(99)00070-6 [DOI] [PubMed] [Google Scholar]
- [11].International agency for research on cancer personal habits and indoor combustions. Available at: https://www.ncbi.nlm.nih.gov/books/NBK30439 (accessed December 1, 2020).
- [12].Chang JS, Straif K, Guha N. The role of alcohol dehydrogenase genes in head and neck cancers: a systematic review and meta-analysis of ADH1B and ADH1C. Mutagenesis 2012;27:275-86. https://doi.org/10.1093/mutage/ger073 10.1093/mutage/ger073 [DOI] [PubMed] [Google Scholar]
- [13].Lajous M. Folate, Vitamin B6, and Vitamin B12 intake and the risk of breast cancer among Mexican women. Cancer Epidemiol Biomarkers Prev 2006;15:443-8. https://doi.org/10.1158/1055-9965.EPI-05-0532 10.1158/1055-9965.EPI-05-0532 [DOI] [PubMed] [Google Scholar]
- [14].Eyre H, Kahn R, Robertson RM, Clark NG, Doyle C, Hong Y, Gansler T, Glynn T, Smith RA, Taubert K, Thun MJ, American Cancer Society; American Diabetes Association; American Heart Association . Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Stroke 2004;35:1999-2010. https://doi.org/10.1161/01.CIR.0000133321.00456.00 10.1161/01.CIR.0000133321.00456.00 [DOI] [PubMed] [Google Scholar]
- [15].Gil J, Stembalska A, Łaczmańska I, Sąsiadek M. Sporadic colorectal cancer - factors modulating individual susceptibility to cancer. Współczesna Onkol 2010;3:123-8. https://doi.org/10.5114/wo.2010.14132 10.5114/wo.2010.14132 [DOI] [Google Scholar]
- [16].Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob Health 2016;4:e609-16. https://doi.org/10.1016/S2214-109X(16)30143-7 10.1016/S2214-109X(16)30143-7 [DOI] [PubMed] [Google Scholar]
- [17].De Flora S, La Maestra S, Crocetti E, Mangone L, Bianconi F, Stracci F, Buzzoni C. Estimates of the incidence of infection-related cancers in Italy and Italian regions in 2018. J Prev Med Hyg 2019;60:E311-326https://doi.org/10.15167/2421-4248/JPMH2019.60.4.1434 10.15167/2421-4248/JPMH2019.60.4.1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Center Disease Control. Occupational cancer. Available at: https://www.cdc.gov/niosh/topics/cancer/default.html (accessed on 17 July 2020).
- [19].International Agency for Research on Cancer. IARC Monographs on the identification of carcinogenic hazards to humans. 2020. Available at: https://monographs.iarc.fr/agents-classified-by-the-iarc (accessed 17 July 2020).
- [20].Cherrie JW, Hutchings S, Gorman Ng M, Mistry R, Corden C, Lamb J, Sánchez Jiménez A, Shafrir A, Sobey M, van Tongeren M, Rushton L. Prioritising action on occupational carcinogens in Europe: a socioeconomic and health impact assessment. Br J Cancer 2017;117:274-81. https://doi.org/10.1038/bjc.2017.161 10.1038/bjc.2017.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ajrouche R, Roudier C, Cléro E, Ielsch G, Gay D, Guillevic J, Marant Micallef C, Vacquier B, Le Tertre A, Laurier D. Quantitative health impact of indoor radon in France. Radiat Environ Biophys 2018;57:205-14. https://doi.org/10.1007/s00411-018-0741-x 10.1007/s00411-018-0741-x [DOI] [PubMed] [Google Scholar]
- [22].Maggiore G, De Filippis G, Totaro T, Tamborino B, Idolo A, Serio F, Castorini IF, Valenzano B, Riccio A, Miani A, Caricato AP, Martino M, De Donno A, Piscitelli P. Evaluation of radon exposure risk and lung cancer incidence/mortality in South-Eastern Italy. J Prev Med Hyg 2020;61:E31-8. https://doi.org/10.15167/2421-4248/JPMH2020.61.1.1343 10.15167/2421-4248/JPMH2020.61.1.1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Konieczna A, Rutkowska A, Rachoń D. Health risk of exposure to Bisphenol A (BPA). Rocz Panstw Zakl Hig 2015;66:5-11. [PubMed] [Google Scholar]
- [24].Kokel D, Li Y, Qin J, Xue D. The nongenotoxic carcinogens naphthalene and para-dichlorobenzene suppress apoptosis in Caenorhabditis elegans. Nat Chem Biol 2006;2:338-45. https://doi.org/10.1038/nchembio791 10.1038/nchembio791 [DOI] [PubMed] [Google Scholar]
- [25].Espina C, Straif K, Friis S, Kogevinas M, Saracci R, Vainio H, Schüz J. European Code against Cancer, 4th Edition: Environment, occupation and cancer. Cancer Epidemiol 2015;39(Suppl. 1):S84-92. https://doi.org/10.1016/j.canep.2015.03.017 10.1016/j.canep.2015.03.017 [DOI] [PubMed] [Google Scholar]
- [26].Centers for disease control and precention. How to prevent cancer or find it early. Available at: https://www.cdc.gov/cancer/dcpc/prevention/index.htm (accessed 17 July 2020).
- [27].Valle I, Tramalloni D, Bragazzi NL. Cancer prevention: state of the art and future prospects. J Prev Med Hyg 2015;56:E21-7. [PMC free article] [PubMed] [Google Scholar]
- [28].American institute for cancer research. 2019 AICR Cancer Risk Awareness Survey.; 2020. Available at: https://www.aicr.org/assets/can-prevent/docs/2019-Survey.pdf (accessed 17 July 2020).
- [29].Connor K, Hudson B, Power E. Awareness of the signs, symptoms, and risk factors of cancer and the barriers to seeking help in the UK: comparison of survey data collected online and face-to-face. JMIR Cancer 2020;6:e14539. https://doi.org/10.2196/14539 10.2196/14539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Inoue M, Iwasaki M, Otani T, Sasazuki S, Tsugane S. Public awareness of risk factors for cancer among the Japanese general population: a population-based survey. BMC Public Health 2006;6:2. https://doi.org/10.1186/1471-2458-6-2 10.1186/1471-2458-6-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Munishi OM, McCormack V, Mchome B, Mangi G, Zullig LL, Bartlett J, Mapunda O, Nyindo P, Namwai T, Muiruri C, Kimaro F, Karia F, Mmbaga BT. Awareness of Cancer Risk Factors and Its Signs and Symptoms in Northern Tanzania: a Cross-Sectional Survey in the General Population and in People Living with HIV. J Cancer Educ 2020;35:696-704. https://doi.org/10.1007/s13187-019-01513-6 10.1007/s13187-019-01513-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Poudel K, Sumi N. Knowledge about risk factors for cancer among adults in Nepal. KnE Life Sci 2018;4:126. https://doi.org/10.18502/kls.v4i4.2270 10.18502/kls.v4i4.2270 [DOI] [Google Scholar]
- [33].Feizi A, Kazemnejad A, Babaee G, Parsayekta Z, Monjamed Z. Public awareness of risk factors for cancer and its determinants in an Iranian population. Asia Pac J Public Health 2010;22:76-88. https://doi.org/10.1177/1010539509350768 10.1177/1010539509350768 [DOI] [PubMed] [Google Scholar]
- [34].Ahmed SBM, Amer S, Hussein A, Kampani DD, Al Hasham N, Assker MM, Shawa N, Saleh D, Alfarouk KO. Assessing the knowledge of environmental risk factors for cancer among the UAE population: a pilot study. Int J Environ Res Public Health 2020;17:2984. https://doi.org/10.3390/ijerph17092984 10.3390/ijerph17092984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Al-Azri M, AL-Rasbi K, Al-Hinai M, Davidson R, Al-Maniri A. Awareness of risk factors for cancer among omani adults - a community based study. Asian Pac J Cancer Prev 2014;15:5401-6. https://doi.org/10.7314/APJCP.2014.15.13.5401 10.7314/APJCP.2014.15.13.5401 [DOI] [PubMed] [Google Scholar]
- [36].Ravichandran K, Mohamed G, Al-Hamdan NA. Public knowledge on cancer and its determinants among Saudis in the Riyadh Region of Saudi Arabia. Asian Pac J Cancer Prev 2010;11:1175-80. [PubMed] [Google Scholar]
- [37].Raj S, Piang LK, Nair KS, Tiwari VK, Kaur H, Singh B. Awareness regarding risk factors, symptoms and treatment facilities for cancer in selected states of India. Asian Pac J Cancer Prev 2012;13:4057-62. https://doi.org/10.7314/APJCP.2012.13.8.4057 10.7314/APJCP.2012.13.8.4057 [DOI] [PubMed] [Google Scholar]
- [38].Richards R, McNoe B, Iosua E, Reeder AI, Egan R, Marsh L, Robertson L, Maclennan B, Dawson A, Quigg R, Petersen A-C. Changes in awareness of cancer risk factors among adult New Zealanders (CAANZ): 2001 to 2015. Health Educ Res 2017;32:153-162. https://doi.org/10.1093/her/cyx036 10.1093/her/cyx036 [DOI] [PubMed] [Google Scholar]
- [39].Tfaily MA, Naamani D, Kassir A, Sleiman S, Ouattara M, Moacdieh MP, Jaffa MA. Awareness of colorectal cancer and attitudes towards its screening guidelines in Lebanon. Ann Glob Health 2019;85:75. https://doi.org/10.5334/aogh.2437 10.5334/aogh.2437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].El Asmar M, Bechnak A, Fares J, Al Oweini D, Al Razim A, El Achkar A, Tamim H. Knowledge, attitudes and practices regarding breast cancer amongst Lebanese females in Beirut. Asian Pac J Cancer Prev 2018;19(3). https://doi.org/10.22034/APJCP.2018.19.3.625 10.22034/APJCP.2018.19.3.625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Shamseddine A, Saleh A, Charafeddine M, Seoud M, Mukherji D, Temraz S, Sibai AM. Cancer trends in Lebanon: a review of incidence rates for the period of 2003-2008 and projections until 2018. Popul Health Metr 2014;12:4. https://doi.org/10.1186/1478-7954-12-4 10.1186/1478-7954-12-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Shamseddine A, Sibai A-M, Gehchan N, Rahal B, El-Saghir N, Ghosn M, Aftimos G, Chamsuddine N, Seoud M. Cancer incidence in postwar Lebanon: findings from the first national population-based registry, 1998. Ann Epidemiol 2004;14:663-8. https://doi.org/10.1016/j.annepidem.2003.12.002 10.1016/j.annepidem.2003.12.002 [DOI] [PubMed] [Google Scholar]
- [43].Ahmed HG. Survey on Knowledge and attitudes related to the relation between tobacco, alcohol abuse and cancer in the Northern state of Sudan. Asian Pac J Cancer Prev 2013;14:2483-6. https://doi.org/10.7314/APJCP.2013.14.4.2483 10.7314/APJCP.2013.14.4.2483 [DOI] [PubMed] [Google Scholar]
- [44].Falzon C, Chalabaev A, Schuft L, Brizzi C, Ganga M, d’Arripe-Longueville F. Beliefs about physical activity in sedentary cancer patients: an in-depth interview study in France. Asian Pac J Cancer Prev 2012;13:6033-8. https://doi.org/10.7314/APJCP.2012.13.12.6033 10.7314/APJCP.2012.13.12.6033 [DOI] [PubMed] [Google Scholar]
- [45].Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet 2005;366:1784-93. https://doi.org/10.1016/S0140-6736(05)67725-2 10.1016/S0140-6736(05)67725-2 [DOI] [PubMed] [Google Scholar]
- [46].Song M, Giovannucci E. Preventable incidence and mortality of carcinoma associated with lifestyle factors among white adults in the United States. JAMA Oncol 2016;2:1154. https://doi.org/10.1001/jamaoncol.2016.0843 10.1001/jamaoncol.2016.0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kumar YS, Mishra G, Gupta S, Shastri S. Level of cancer awareness among women of low socioeconomic status in Mumbai slums. Asian Pac J Cancer Prev 2011;12:1295-8. [PubMed] [Google Scholar]
- [48].Veerakumar AM, Kar SS. Awareness and perceptions regarding common cancers among adult population in a rural area of Puducherry, India. J Educ Health Promot 2017;6:38. https://doi.org/10.4103/jehp.jehp_152_15 10.4103/jehp.jehp_152_15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Akl EA, Gunukula SK, Aleem S, Obeid R, Jaoude PA, Honeine R, Irani J. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health 2011;11:244. https://doi.org/10.1186/1471-2458-11-244 10.1186/1471-2458-11-244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].El-Hajj M, Salameh P, Rachidi S, Al-Hajje A, Hosseini H. Cigarette and waterpipe smoking are associated with the risk of stroke in Lebanon. J Epidemiol Glob Health 2019;9:62. https://doi.org/10.2991/jegh.k.181231.002 10.2991/jegh.k.181231.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].MOPH. Statistical Bulletin. Ministry of Public Health 2020. Available at: https://www.moph.gov.lb/en/Pages/0/25192/statistical-bulletin (accessed 17 July 2020).


