Summary
Introduction
Seasonal influenza is an annual common occurrence in cold seasons; but the COVID-19 pandemic is also currently ongoing. These two diseases can’t be distinguished from their symptoms alone; therefore, the importance of preventing influenza by vaccination is more than ever. Due to the high exposure of hospital personnel, widespread influenza vaccination of these high-risk groups seems to be a necessity. This Study conducted to determine vaccination coverage in the personnel of four tertiary referral collegiate hospitals in 2019 and to further investigate individual obstacles for Influenza vaccination.
Methods
In this cross-sectional descriptive study, 637 personnel were selected randomly from distinctive hospitals in a list-wised. Ones vaccinated filled the side effects questionnaire and who not vaccinated filled the vaccination obstacles questionnaire. The study was approved by the ethics committee of Tehran University of Medical Sciences with this reference number: IR.TUMS.IKHC.REC.1398.218
Results
The mean vaccination coverage was 29.4% and the coverage difference among centers was not statistically significant (p = 0.192). The following items had the most impact on personnel decision: confidence about one’s immune system (p < 0.05), the experience of side effects from previous vaccinations (p = 0.011), attitude about vaccination in colleagues (p = 0.021) and work experience (p < 0.05). About 23% of vaccinated individuals reported side effects following vaccination and the most common side effect was mild cold symptoms with 12.3% prevalence.
Conclusion
The results of the current study revealed that influenza vaccination coverage among HCWs is not satisfactory in Iran. Hospital authorities and infection control units should plan to remove the obstacles of influenza vaccination.
Keywords: Influenza, Vaccination, Healthcare workers
Introduction
Influenza, also known as “the flu” is an infectious disease caused by the influenza virus, leading to an acute respiratory illness affecting the upper and/or lower respiratory tract [1]. Receiving an influenza vaccination, as CDC confirms, is the major public health measure for the prevention of influenza virus infection [2] and thus, vaccination has to be considered one of the most crucial actions which have to be taken to immunize healthcare workers who are highly in exposure to various threatening viruses.
Influenza epidemics are a familiar annual event, but currently in the absence of widespread use of vaccine for novel coronavirus, the COVID-19 pandemics also circulate in parallel with seasonal influenza [3, 4]. WHO concerns many healthcare systems are already reached to their limits and may not be able to deal with influenza. Unfortunately, the two diseases can’t be distinguished from their symptoms alone, and laboratory tests are needed. Therefore, the importance of preventing influenza infection is certainty these years more than ever. The most effective way to avoid influenza infection is through vaccination [3].
Based on a rapid evidence appraisal identifying the public health need for healthcare worker (HCW) influenza immunization and the international independent expert group confirmed in 2019 the need to support policy-making for health worker vaccination to support pandemic preparedness in countries in line with the WHO global influenza vaccine strategy. However, some studies are indicating that the majority of healthcare workers are not usually immunized based on different reasons [5]. Some of the barriers to acceptance of influenza vaccination among HCWs are fear of vaccine side-effects (especially influenza-like symptoms), perceived ineffectiveness of the vaccine, insufficient time, or inconvenience [6, 7]. Other factors included perceived low likelihood of contracting influenza, perceived low threat compared to other infectious diseases, avoidance of medications, and fear of needles [8]. In response to these perceptions, healthcare facilities have adopted programmatic strategies to improve vaccination uptake in HCWs including the participation of senior personnel or opinion leaders as role models, removing administrative barriers, e.g. costs, providing on-site vaccination delivery service at convenient times that are easily accessible by HCWs [5, 9]. Several studies have highlighted that the vaccinated and non-vaccinated HCWs had opposing perceptions about the risks and benefits of the vaccination and degree of its benefits [10, 11].
Despite the importance of identifying and breaking these barriers in increasing vaccination coverage of HCWs, there have been limited studies countrywide, investigating the vaccine coverage rate among HCWs and identifying barriers to get vaccinated among them [7, 12]. Therefore, in this study, we are trying and aiming to help the governors and motivate them to work things out to define a new priority for immunizing HCWs who are highly vulnerable for transmitting the disease. The other contribution of the current paper is to analyze adverse effects of vaccination and exploiting the scope of its effectiveness in HCWs.
Methods
In this cross-sectional descriptive study, some personnel of distinctive hospitals (four tertiary referral collegiate hospitals in Tehran, Iran) were selected randomly in a list-wised fashion. Moreover, a pre-designed questionnaire was taken from listed HCWs regarding their attitude of vaccination and their confidence about their immune system capabilities, vaccination history, number of flu episodes in the past year as well as the scope and severity of symptoms if present, underlying diseases, fear from side effects and injection, side effects regarding vaccination, and their demographic data as well as their working experience.
Another questionnaire was additionally taken from vaccinated HCW regarding the side effects they have experienced following their current influenza vaccination.
RESEARCH ETHICS
In this study no intervention was done, and no cost imposed on the participants. Researchers, in all stages, were adhered to the principles of the Helsinki manifesto and the Ethics Committee of Tehran University of Medical Sciences. Ethics Code: IR.TUMS.IKHC.REC.1398.218.
Results
From 637 listed individuals as healthcare workers across four hospitals, 477 were female and 160 were males. Vaccination coverage across all hospitals was 29.4% with the median age of 36.88 and 34.15 years in vaccinated and non-vaccinated groups respectively. The vaccination coverage was significantly different between sex groups with 35.85% and 27.31% for males and females respectively (p = 0.041). Vaccination coverage in these four hospitals was 24.41, 27.51, 34.29, and 34.33%. Vaccination coverage among different centers was not statistically significant (p = 0.192).
To analyze possible etiologies for not getting vaccinated, the chi-square test was used to compare questionnaire variables between vaccinated and non-vaccinated groups. The mean work experience was 11.83 and 8.92 years for vaccinated and non-vaccinated groups respectively which was statistically significant (p < 0.05). Besides, 33.8% of individuals in the non-vaccinated group had high self-esteem about their immune system capability which was significantly higher from 12.2% in vaccinated individuals (p < 0.05). Also, 75.4% of individuals who had a history of occurrence of side effects following their previous vaccination haven’t participated in the new year’s vaccination program, which was statistically significant (p = 0.011). Moreover, 14.1% of non-vaccinated individuals were heard negative feedbacks and attitudes from their colleagues, which was significantly more from 7.5% in vaccinated individuals (p = 0.021). Interestingly, known vaccination side effects that had been occurred in an individual’s colleagues had no significant difference between vaccinated and non-vaccinated individuals (p = 0.682).
Lack of education and knowledge about vaccination benefits had no significant difference between vaccinated and non-vaccinated individuals in our study. In addition, vaccination was not significantly different regarding individuals’ occupation, which is shown in Figure 1.
Fig. 1.
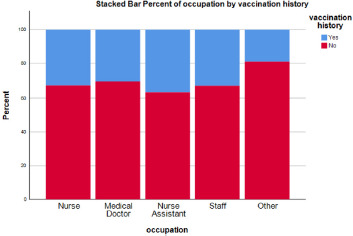
Percent of influenza vaccination by the occupation of personnel.
Moreover, vaccinated proportions were not significantly different across different wards and units (Fig. 2).
Fig. 2.
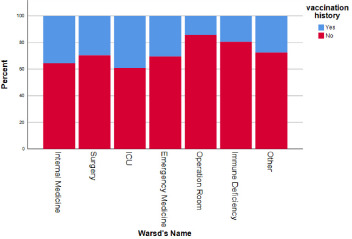
Percent of influenza vaccination by hospital wards.
The relative frequency of different side effects following influenza vaccination from 187 vaccinated individuals is summarized in Figure 3. Common cold and influenza symptoms, as well as, fever were the most common side effects following the vaccination.
Fig. 3.
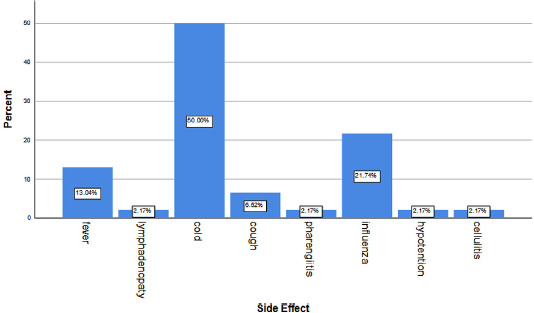
Relative frequency of side effects following influenza vaccination.
To assess vaccination efficacy in healthcare workers, the occurrence of flu symptoms in last year were compared in vaccinated and non-vaccinated individuals. Twenty percent of vaccinated individuals experienced one or more episodes of flu-like symptoms in the past year which wasn’t significantly different from 15.38% in non-vaccinated individuals; Although, vaccinated individuals had a significantly faster recovery following the onset of the symptoms (p < 0.05). This study about the duration of flu symptoms in vaccinated and non-vaccinated individuals suggested 69.76% of vaccinated individuals had a recovery duration of 3 days or less from their symptom onset, which is significantly more from 50% in the non-vaccinated group.
Discussion
Results of the current study revealed influenza vaccination coverage among healthcare centers in Iran is not satisfactory. Moreover, in this study individuals’ attitude about the probability of “getting the disease” was correlated with their willingness for vaccination. Interestingly results of the current study suggest this probability is more correlated with one’s self-esteem about his/her immune system capability as well as, his/her personal history of getting the flu rather than educational and knowledge of severity and prevalence of the illness. This effect of attitude in vaccination was previously shown in several studies [5, 6, 13].
Interestingly, more working experience had a positive impact on getting the influenza vaccine. This is coherent with several studies that showed more professional experience correlation with higher vaccination rates [14-16]. Although, in contrast to the study performed by Barbodoro which stated good awareness of influenza and influenza vaccination is positively correlated with more vaccination rates [14], here such a correlation was not present.
Findings of the present study suggested although influenza vaccination can have limited to no effects in the prevention of the flue, it significantly accelerates the recovery process and reduces the severity and shortens the course of the illness. These findings are in line with the study by Nishi et al. [17] except in our study vaccination didn’t decrease yearly flu episodes in HCWs.
The results from the current study suggested a relatively low prevalence of mostly mild side effects following the influenza vaccination. Hashemi et al. has reported similar results in a study performed in Shiraz [7].
Current years however are quite unique because the symptoms of patients may not necessarily be due to influenza but also due to the COVID-19. In addition, because of standing the receptors for both influenza and COVID-19 on human host cells one may get infected with either or both infection. Hence the scientists encourage everyone to take the vaccine and avoid this complex scenario [4]. Besides, in a conclusion by Debisarun et al, influenza vaccine can also induce trained immunity responses and may also create a relative protection against COVID-19. These data, coupled with similar reports, discuss a beneficial effect of influenza vaccination in the influenza season against both infections [18, 19].
Conclusions
Considering international recommendations on influenza vaccination for HCWs, the results of the current study revealed that influenza vaccination coverage among HCWs is not satisfactory in Iran. Hospital authorities and infection control units should plan to remove the factors correlated with not getting vaccinated in healthcare workers. Influenza vaccination is an effective way to prevent or reduce the severity of seasonal flu in healthcare workers with few and mostly mild side effects.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any spe-cific grant from funding agencies in the public, commer-cial, or not-for-profit sectors.
Special appreciation to infection control supervisors, physicians, and participants in this research in Imam Khomeini hospital, Shariati hospital, Sina hospital, and Amir Alam hospital.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
HM: senior supervisor of the study; HNG: primary analysis and preparation of manuscript draft; MM, RP, HM, GA, AA and VYB: data collecting in Sina hospital, Shariati hospital, Amir Alam hospital, Imam Khomeini hospital, Cancer Institute and Valiasr hospital respectively; ASH, ME, HA and A-AA: study supervision and confirming the data in Shariati hospital, Imam Khomeini hospital Complex, Sina hospital and Amir Alam hospital respectively; SA: designing the study, final analysis and revising the paper. MH and NGHcontributed equally to this work. All authors reviewed the results and approved the final version of the manuscript.
References
- [1].Gruneir A, Kwong JC, Campitelli MA, Newman A, Anderson GM, Rochon PA, Mor V. Influenza and seasonal patterns of hospital use by older adults in long-term care and community settings in Ontario, Canada. Am J Public Health 2014;104:e141-e7. https://doi.org/10.2105/ajph.2013.301519 10.2105/ajph.2013.301519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Talbot TR, Babcock H, Caplan AL, Cotton D, Maragakis LL, Poland GA, Septimus EJ, Tapper ML, Weber DJ. Revised SHEA position paper: influenza vaccination of healthcare personnel. Infect Control Hosp Epidemiol 2010;31:987-95. https://doi.org/10.1086/656558 10.1086/656558 [DOI] [PubMed] [Google Scholar]
- [3].World Health Organization (WHO/Europe). Influenza in the time of COVID-19. Available from: https://www.euro.who.int/en/health-topics/communicable-diseases/influenza/news/news/2020/10/influenza-in-the-time-of-covid-19 (accessed on 05/10/2010). [Google Scholar]
- [4].Grech V, Borg M. Influenza vaccination in the COVID-19 era. Early Hum Dev 2020;148:105116. https://doi.org/10.1016/j.earlhumdev.2020.105116 10.1016/j.earlhumdev.2020.105116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].To K, Lai A, Lee K, Koh D, Lee S. Increasing the coverage of influenza vaccination in healthcare workers: review of challenges and solutions. J Hosp Infect 2016;94:133-42. https://doi.org/10.1016/j.jhin.2016.07.003 10.1016/j.jhin.2016.07.003 [DOI] [PubMed] [Google Scholar]
- [6].Dedoukou X, Nikolopoulos G, Maragos A, Giannoulidou S, Maltezou HC. Attitudes towards vaccination against seasonal influenza of health-care workers in primary health-care settings in Greece. Vaccine 2010;28:5931-3. https://doi.org/10.1016/j.vaccine.2010.06.108 10.1016/j.vaccine.2010.06.108 [DOI] [PubMed] [Google Scholar]
- [7].Hashemi A, Soodejani MT, Karami M, Pordanjani SR. Adverse effects of influenza vaccination among healthcare staff in shiraz in 2014, Iran. Qom Univ MedSci J 2016;10:58-64. Available from: http://journal.muq.ac.ir/article-1-1174-fa.pdf [Google Scholar]
- [8].Parry H, Damery S, Fergusson A, Draper H, Bion J, Low A. Pandemic influenza A (H1N1) 2009 in a critical care and theatre setting: beliefs and attitudes towards staff vaccination. J Hosp Infect 2011;78:302-7. https://doi.org/10.1016/j.jhin.2011.02.009 10.1016/j.jhin.2011.02.009 [DOI] [PubMed] [Google Scholar]
- [9].Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. Hum Vaccin Immunother 2018;14:772-89. https://doi.org/10.1080/21645515.2017.1348442 10.1080/21645515.2017.1348442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Looijmans-van den Akker I, van Delden JJ, Verheij TJ, van Essen GA, van der Sande MA, Hulscher ME, Hak E. Which determinants should be targeted to increase influenza vaccination uptake among health care workers in nursing homes? Vaccine 2009;27:4724-30. https://doi.org/10.1016/j.vaccine.2009.05.013 10.1016/j.vaccine.2009.05.013 [DOI] [PubMed] [Google Scholar]
- [11].Prematunge C, Corace K, McCarthy A, Nair RC, Pugsley R, Garber G. Factors influencing pandemic influenza vaccination of healthcare workers - a systematic review. Vaccine 2012;30:4733-43. https://doi.org/10.1016/j.vaccine.2012.05.018 10.1016/j.vaccine.2012.05.018 [DOI] [PubMed] [Google Scholar]
- [12].Moghadami M, Afsar Kazeroni P, Honarvar B, Ebrahimi M, Bakhtiari H, Akbarpour MA, Tabatabaee HR, Mirahmadizadeh AR, Rezaianzadeh A, Hasanzadeh J, Zamiri N, Sabayan B, Moattari A, Emami A, Lankarani KB. Influenza A (H1N1) virus pandemic in fars province: a report from Southern Iran, July-December 2009. Iran Red Crescent Med J 2010;12:231-8. Available from: https://ircmj.kowsarpub.com/cdn/dl/b5f082ac-4adc-11e8-809d-4bdc53cc9af0 [Google Scholar]
- [13].Domínguez A, Godoy P, Castilla J, Soldevila N, Toledo D, Astray J, Mayoral JM, Tamames S, García-Gutiérrez S, González-Candelas F, Martín V, Díaz J, Torner N. Knowledge of and attitudes to influenza vaccination in healthy primary healthcare workers in Spain, 2011-2012. PLoS One 2013;8:e81200. https://doi.org/10.1371/journal.pone.0081200 10.1371/journal.pone.0081200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Barbadoro P, Marigliano A, Di Tondo E, Chiatti C, Di Stanislao F, D’Errico MM, Prospero E. Determinants of influenza vaccination uptake among Italian healthcare workers. Hum Vaccin Immunother 2013;9:911-6. https://doi.org/10.4161/hv.22997 10.4161/hv.22997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Falomir-Pichastor JM, Toscani L, Despointes SH. Determinants of flu vaccination among nurses: the effects of group identification and professional responsibility. Appl Psychol 2009;58:42-58. https://doi.org/10.1111/j.1464-0597.2008.00381.x 10.1111/j.1464-0597.2008.00381.x [DOI] [Google Scholar]
- [16].Antón-Ladislao A, García-Gutiérrez S, Soldevila N, González-Candelas F, Godoy P, Castilla J, Mayoral JM, Astray J, Martín V, Tamames S, Toledo D, Aguirre U, Domínguez A. Visualizing knowledge and attitude factors related to influenza vaccination of physicians. Vaccine 2015;33:885-91. https://doi.org/10.1016/j.vaccine.2014.12.012 10.1016/j.vaccine.2014.12.012 [DOI] [PubMed] [Google Scholar]
- [17].Nishi K, Mizuguchi M, Ueda A. Effectiveness of influenza vaccine in health-care workers. Kansenshogaku zasshi 2001;75:851-5. https://doi.org/10.11150/kansenshogakuzasshi1970.75.851 10.11150/kansenshogakuzasshi1970.75.851 [DOI] [PubMed] [Google Scholar]
- [18].Debisarun PA, Struycken P, Domínguez-Andrés J, Moorlag SJCFM, Taks E, Gössling KL, Ostermann PN, Müller L, Schaal H, Oever JT, Crevel RV, Netea MG. The effect of influenza vaccination on trained immunity: impact on COVID-19. MedRxiv 2020. https://doi.org/10.1101/2020.10.14.20212498 10.1101/2020.10.14.20212498 [DOI] [Google Scholar]
- [19].Yang MJ, Benjamin JR, Le TT, Santiago IO, Diamond J, Dorsey NL, Mainous AG. Influenza vaccination and hospitalizations among COVID-19 infected adults. J Am Board Fam Med 2021. Available from: https://www.jabfm.org/sites/default/files/COVID_20-0528.pdf [DOI] [PubMed] [Google Scholar]


