Summary
Tobacco Consumption (TC) is one of the main causes of the deterioration of health; however, there are few studies linking its consumption with diet and nutrition among university students. The objective of this study is to test the association of smoking with anthropometry, diet and sleep quality among Chilean university students. Cross-sectional study. University students (n = 1454) from the North, South and Central parts of Chile were evaluated. A self-assessment survey was used to evaluate healthy and unhealthy eating habits. Nutritional status was evaluated by Body Mass Index (BMI). Two surveys were used to assess sleep quality: the Questionnaire of Insomnia and the Epworth Scale. Finally, participants were consulted about Tobacco Consumption: 30% of the students consume tobacco and have a higher score in unhealthy food consumption, less frequent weekly breakfast consumption (< 0.01), lower daily fruit (< 0.01) and vegetables (< 0.05) consumption, higher alcohol consumption (< 0.05) and daily junk food consumption (< 0.05) compared to non-consuming students. Men who consume tobacco present greater insomnia (< 0.001), sleep latency (< 0.001) and daytime sleepiness (< 0.05) compared to non-consumers; and women who consume tobacco have a higher weight (< 0.001) and BMI (< 0.01). When performing logistic regression, tobacco consumption is positively associated with major alcohol consumption (< 0.001), whereas fish (< 0.05) and vegetable (< 0.05) consumption was negatively associated. In conclusion, students of both sexes who smoke have more unfavorable health factors and a poorer quality of life.
Keywords: Tobacco, University students, Food, Breakfast, Health
Introduction
Between 1960 and 2000, Chile has experienced economic, social and health changes that have influenced lifestyles related to eating habits, sedentary lifestyles, and consumption of tobacco, alcohol and other drugs [1]. Many of these changes have gone hand in hand with the deterioration of the quality of life. In the last two decades an increase in malnutrition due to excess has been reported, affecting 64.5% of the population over 18 years of age [2]. Chile is now among the top countries in the Americas, surpassed only by the United States and Mexico, on the World Health Organization’s list of countries with the highest prevalence of obesity [3].
University years are a period of transition to early adulthood where lifestyles associated with risk behaviors are established and the risk of developing obesity and chronic diseases increases [4]. Lifestyle characteristics of university students include factors related to the later development of disease: low economic capital, poor eating habits, frequent skipping of meals, high fast food consumption [6], sedentary lifestyle, smoking, and stress [5-8].
Tobacco consumption is one of the main causes of health deterioration, associated with several chronic diseases and is positively correlated with a decrease in physical activity [9]. Chile has the highest prevalence of tobacco consumption in Latin America, both among youth and adult population; the 2016-2017 National Health Survey indicates that 33.3% of the population currently smokes, with rates greater in men than in women (37.8 vs 29.1%) [2]. The average age of the first cigarette is 15 (a prevalence rate that has been increasing in recent years), but the habit is established at college age. On the other hand, sleep problems have been shown to be associated with the pathophysiology of severe disorders related to smoking [10]. The university population is especially prone to develop sleep disorders due to external factors (social and environmental) and lifestyle habits that can deteriorate their quality of life.
Several recent studies have tried to relate tobacco consumption with Body Mass Index (BMI), eating habits and sleep quality; however, there are few studies, especially in Latin America, relating these 3 variables.
The objective of this study was to test the association of smoking with anthropometry, diet and sleep quality among Chilean university students.
Method
We conducted a descriptive study with 1455 students from 6 universities: University of Antofagasta (located in Northern Chile), University San Sebastian (in Central and Southern Chile), University Autónoma de Chile (in Central and Southern Chile), University Bernardo O Higgins (Central Chile), University Playa Ancha (Central Chile), and the University Católica de Temuco (Southern Chile). The sample was selected using non-probabilistic criteria. All students present at the time of the evaluations were included. Participants provided informed consent. Reasons for non-participation included: unavailability due to internships, illness, or failure to sign the informed consent. The study was developed following the Declaration of Helsinki and was approved by the Ethics Committee of the Universidad Católica de Temuco.
QUESTIONNAIRES
Eating habits survey
The Food Habits Survey created by Durán et al. [11] was used. The survey is self-administered and measures healthy and unhealthy eating habits. The frequency of health habits, such as the consumption of food groups recommended in the Chilean dietary guidelines is assessed with nine items with a minimum score of 1 (does not consume) and a maximum of 5 (suggested portion per day or week). Responses are added up together to obtain a total value between 9 to 45 points; a higher value indicates healthier eating habits. Unhealthy eating habits are assessed with six items: consumption of sugary drinks, alcohol, fried foods, fast food, snacks, and adding salt to meals without tasting them first. Available responses range from 1 (does not consume) to 5 (> 3 portions per day/week) or from 1 to 3 for the question about salt. Response values are added up and the total ranges from 6 to 28 points, with higher values indicating poorer eating habits.
Insomnia Questionnaire or Insomnia Severity Index (ISI)
The ISI is a self-report questionnaire to assess the nature, severity and impact of insomnia [12,13]. A score between 0 and 7 indicates absence of clinical insomnia, 8-14 subclinical insomnia, 15-21 moderate clinical insomnia and 22-28 clinical insomnia (severe).
Epworth Sleepiness Scale (ESE)
The ESE evaluates the propensity to fall asleep in eight different sedentary situations. This scale is self-administered and response options for each item range between 0-3. At the end, cumulative scores between 0 and 24 are obtained, where higher scores represent a greater degree of drowsiness [14].
Information on the amount of sleep and sleep latency was also asked.
Weight and height were measured. Participants were weighed in light clothing using a mechanical scale (SECA) with a maximum capacity of 220 kg and 50 g precision. Height was measured with a height rod that is incorporated in the scale. Body mass index (BMI) was calculated to categorize the nutritional status according to WHO criteria [15].
Finally, participants were asked about tobacco consumption. Participants who reported having smoked in the last week were labeled smokers.
STATISTICAL ANALYSIS
The results are presented as mean ± standard deviations and as percentages according to the type of variable. Kolmogorov-Smirnov normality test was used to determine the normality of the variables. Participants were analyzed by groups, according to their nutritional status. For categorical variables, the Chi-square test was used. For non-categorical variables the T-Test used. Logistic regression was used to assess associations with tobacco consumption. The level of significance used was α = 0.05 in all cases. STATA 12.1 was used for analyses.
Results
Out of the 1455 students surveyed, 1439 had complete data. Figure 1 shows a high overall prevalence of tobacco consumption (30.1%), with prevalence starting high in the first year of study and decreasing in the second year, before increasing again in subsequent years. However, no significant differences were observed (0.073).
Fig. 1.
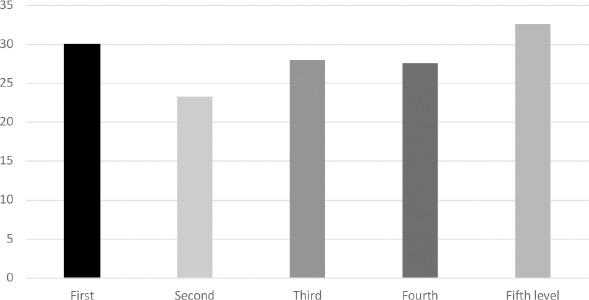
Tobacco consumption by year of university study (Chi Square = 0.073).
Among participants who exercised, 32 smoked and 29% of those who did not exercise, smoked (p > 0.05).
Table I shows that students who smoke, regardless of sex, have significant differences in BMI, height, score for unhealthy foods, greater daytime sleepiness, insomnia, sleep latency and greater sleep hours, compared to those who did not smoke.
Tab. I.
Comparison of anthropometry, food survey score, insomnia and daytime sleepiness by smoking status 1.
| Non-smokers (n = 1015) |
Smokers (n = 424) |
P-value2 | |
|---|---|---|---|
| Weight (kg) | 61.6 ± 10.5 | 64.1 ± 11.7 | 0.059 |
| Height (m) | 1.62 ± 0.07 | 1.63 ± 0.08 | 0.025 |
| BMI (k/m2) | 23.2 ± 3.1 | 23.8 ± 3.4 | 0.001 |
| Healthy foods score | 55.1 ± 7.3 | 54.7 ± 7.2 | 0.375 |
| Unhealthy foods score | 12.7 ± 3.3 | 14.3 ± 3.7 | 0.011 |
| Epworth | 7.3 ± 4.9 | 8.0 ± 5.0 | 0.033 |
| Insomnia score | 10.2 ± 4.8 | 10.9 ± 4.9 | 0.015 |
| Sleep latency (min) | 26.3 ± 30.3 | 31.4 ± 31.4 | 0.007 |
| Sleep duration (h) | 7.6 ± 1.5 | 7.8 ± 1.6 | 0.028 |
* Values are mean ± SD.
2 Student T test.
Table II shows that male smokers have a less favorable sleep quality compared to non-smokers, reflecting greater daytime sleepiness, insomnia, sleep latency and also had higher unhealthy food scores. In contrast, female smokers weighed significantly more, had a higher BMI and unhealthy food score compared to non-smoking women, with no differences observed for sleep variables.
Tab. II.
Comparison of anthropometry, food survey score, insomnia and daytime sleepiness by smoking status, stratified by sex 1.
| Men | Non-smokers (n = 231) |
Smokers (n = 111) |
P-value2 |
|---|---|---|---|
| Weight (kg) | 72.3± 10.9 | 73.7 ± 13.1 | 0.342 |
| Height (m) | 1.72 ± 0.06 | 1.72 ± 0.07 | 0.656 |
| BMI (k/m2) | 24.3 ± 3.2 | 24.5 ± 3.4 | 0.480 |
| Healthy foods score | 55.1 ± 7.3 | 54.7 ± 7.2 | 0.061 |
| Unhealthy foods score | 12.7 ± 3.3 | 14.3 ± 3.7 | 0.001 |
| Epworth | 7.3 ± 4.9 | 8.0 ± 5.0 | 0.030 |
| Insomnia score | 10.2 ± 4.8 | 10.9 ± 4.9 | 0.001 |
| Sleep latency (min) | 26.3 ± 30.3 | 31.4 ± 31.4 | 0.001 |
| Sleep duration (h) | 7.6 ± 1.5 | 7.8 ± 1.6 | 0.199 |
| Women |
Non-smokers
(n = 784) |
Smokers
(n = 313) |
P-value2 |
| Weight (kg) | 58.7 ± 8.4 | 60,9 ± 9.3 | 0.001 |
| Height (m) | 1.59 ± 0.05 | 1.60 ± 0.05 | 0.137 |
| BMI (k/m2) | 22.9 ± 3.0 | 23.6 ± 3.3 | 0.002 |
| Healthy foods score | 55.1 ± 7.2 | 55.2 ± 7.5 | 0.877 |
| Unhealthy foods score | 12.5 ± 3.2 | 14.0 ± 3.5 | 0.002 |
| Epworth | 5.1 ± 4.5 | 6.3 ± 4.9 | 0.072 |
| Insomnia score | 8.0 ± 4.8 | 8.6 ± 4.9 | 0.184 |
| Sleep latency (min) | 26.5 ± 31.7 | 29.0 ± 30.2 | 0.249 |
| Sleep duration (h) | 7.6 ± 1.4 | 7.7± 1.5 | 0.106 |
1 Values are mean ± SD.
2 Student T test.
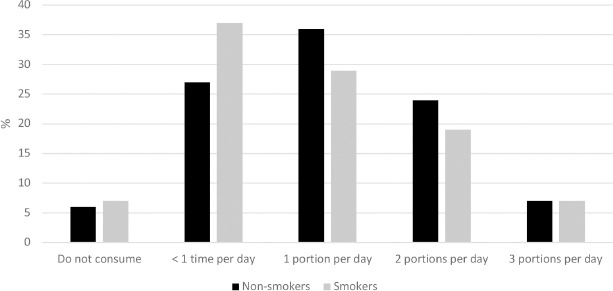
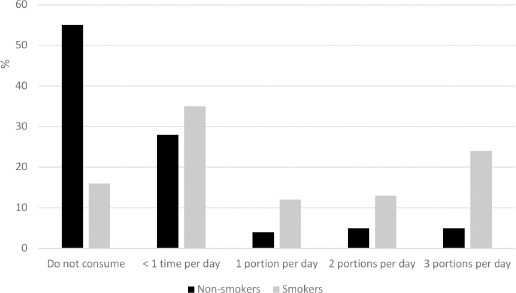
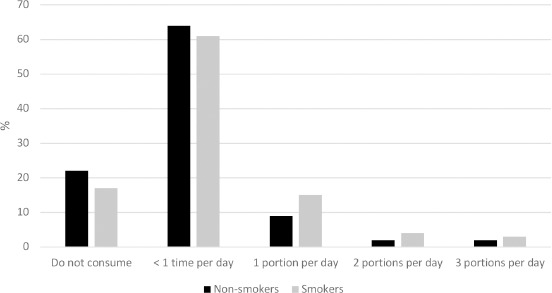
Figures 2, 3, 4 and 5 show a dependent and significant relationship between smoking and an unfavorable diet, reflected in lower frequency of breakfast during the week, lower daily fruit consumption, higher daily consumption of junk food (pizzas, hotdogs, hamburgers, fries or sopaipillas) and higher consumption of alcoholic beverages compared to non-smoking students (p < 0.05). However, as shown in Figure 6, we observed that smokers reported greater daily consumption of vegetables compared to non-smokers.
Fig. 2.
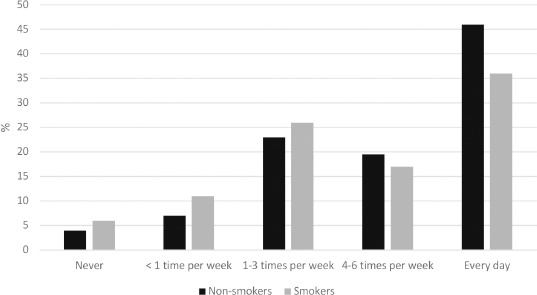
Breakfast consumption by smoking status (Chi Square = 0.004).
Fig. 3.
Daily fruit consumption by smoking status (Chi Square = 0.002).
Fig. 4.
Daily alcohol consumption by smoking status (Chi Square = 0.001).
Fig. 5.
Daily junk food consumption by smoking status (Chi Square = 0.02).
Fig. 6.

Daily vegetable consumption by smoking status (Chi Square = 0.03).
Table III shows when performing logistic regression, that the consumption of tobacco is positively associated with the consumption of alcohol, while is negatively associated with the consumption of fish and vegetables.
Tab. III.
Factors associated with tobacco consumption.
| Estimate | Std. Error | T value | P-value | |
|---|---|---|---|---|
| (Intercept) | -0.084 | 0.175 | -0.484 | 0.628 |
| Age | 0.003 | 0.005 | 0.618 | 0.536 |
| Sex | 0.052 | 0.035 | 1.461 | 0.144 |
| nutritional status | 0.023 | 0.052 | 0.442 | 0.658 |
| Breakfast | 0.045 | 0.028 | 1.617 | 0.106 |
| Dairy products | 0.010 | 0.049 | 0.208 | 0.835 |
| Fruits | -0.083 | 0.077 | -1.088 | 0.276 |
| Vegetables | -0.068 | 0.032 | -2.073 | 0.038 |
| Fish | -0.096 | 0.038 | -2.518 | 0.011 |
| Legumes | -0.034 | 0.031 | -1.092 | 0.275 |
| Bread | -0.007 | 0.033 | -0.219 | 0.826 |
| Lunch | 0.011 | 0.027 | 0.404 | 0.686 |
| Dinner | 0.033 | 0.044 | 0.752 | 0.452 |
| Health food habits | -0.015 | 0.032 | -0.464 | 0.642 |
| Soft drik | 0.001 | 0.034 | 0.045 | 0.964 |
| Alcohol | 0.307 | 0.028 | 10.68 | < 0.001 |
| Fries food | 0.034 | 0.054 | 0.64 | 0.522 |
| Salt | 0.027 | 0.027 | 1.016 | 0.309 |
| Pizza/hog-dog | -0.007 | 0.037 | -0.201 | 0.840 |
| Cookies | -0.048 | 0.033 | -1.445 | 0.147 |
| Unhealthy eating habits | 0.017 | 0.042 | 0.406 | 0.684 |
| Epworth | 0.031 | 0.031 | 1.012 | 0.311 |
| insomnia | 0.002 | 0.029 | 0.079 | 0.936 |
| Sleep duration | -0.001 | 0.001 | -0.672 | 0.501 |
| Sleep Latency | 0.016 | 0.032 | 0.517 | 0.605 |
| Physical activity | -0.001 | 0.001 | -0.852 | 0.394 |
Discussion
The main result of this study is that university students of both sexes who smoke have higher unfavorable health factors and a poorer quality of life: they present a higher unhealthy food consumption score, lower frequency of weekly breakfast consumption, lower daily fruit consumption, and higher daily consumption of alcohol and junk food compared to non-smoking students. Male smokers had greater insomnia, sleep latency and daytime sleepiness compared to non-smokers; and female smokers had higher weight and BMI.
Smoking is a chronic and addictive disease, considered by the WHO as the main cause of avoidable death in the world. It is one of the most important risk factors for disease and death in Chile and is related to chronic obstructive pulmonary disease, pulmonary emphysema, lung cancer, laryngeal cancer, and heart and cerebrovascular diseases [16]. It causes premature death (shortens life by 5-10 years) in more than 50% of smokers, affecting the respiratory and cardiovascular systems, and can cause various neoplasms in the body [17]. According to recent studies that evaluated the age at which the smoking begins, 1 in 3 smokers starts in adolescence or between 18 and 25 years old. We also note that the prevalence of smoking among female has approached that of men in recent years [18-20].
The university population modify their lifestyle to be accepted by their peers. Some studies define university students as a vulnerable group, since many of the healthy habits for adult life can be acquired and modified during this stage [1]. One of the main results obtained in this study is that smoking was associated with unhealthy eating habits. Among men, there was a tendency towards a lower score for healthy eating in non-smokers, versus smokers, although the difference was not statistically significant. An attempt has been made to evaluate the relationship between healthy eating and smoking. In a cross-sectional study, young people who consumed fruit ≥ 2 times a day were 53% less likely (RR = 0.47, p < 0.05) than those who did not normally consume fruit to be more heavy smokers. Longitudinally, the association of fruit and tobacco consumption was not significant (RR = 0.61, p = 0.28). There were no significant associations between the consumption of vegetables and smoking. The consumption of fruits, but not the consumption of vegetables, was inversely associated with the frequency of smoking cross-sectionally, but not longitudinally [21]. Another study conducted in a Japanese population, compared the consumption of food and nutrients between persons who consumed tobacco and non-tobacco users, showing that there was a lower intake of vegetables and fruits rich in antioxidants, preventive factors for many diseases, in those who consumed tobacco. In men, smoking was positively related to the consumption of rice, three alcoholic beverages (sake, beer and whiskey), carbohydrates and other eight foods/nutrients (p < 0.05) and negatively associated with consumption of animal protein, fat, fatty acids, dietary fiber, isoflavones and 36 other foods/nutrients (p < 0.05 for all foods). In contrast, in women, smoking was positively associated with the intake of 13 foods/nutrients, while being negatively associated with the consumption of rice, energy, dietary fiber and other 14 foods/nutrients (p < 0.05 for all food) [22]. These studies support the results obtained in our work, which shows that smokers have a lower nutritional value compared to non-smokers, with less frequent breakfast consumption during the week, less daily fruit consumption, and higher frequency of junk food and alcoholic beverages consumption, compared to non-smokers (p < 0.05). However, it was observed that smokers consumed more daily portions of vegetables compared to non-smokers. Attempts have been made to postulate mechanisms that explain the choice of unhealthy foods in smokers, and the explanation could be at the level of the brain. Jastreboff et al. compared responses in different regions of the brain between smokers and non-smokers during an exposure to their favorite food. Those who consumed tobacco exhibited decreased activation in the caudate, putamen, insula and thalamus [23].
In our study, smoking was associated with greater sleep latency, insomnia and daytime sleepiness. These results are in agreement with other studies [24-28]. Sleep disorders that result in insufficient sleep have been linked with negative physical, cognitive and public health outcomes. Tobacco consumption has been shown to be a predictive variable of sleep disturbances [23]. This interaction was also observed in individuals with chronic rheumatic diseases, who were more likely to report an average < 6 h of sleep per night and frequent insomnia compared to individuals with a chronic rheumatic condition that did not consume tobacco [25]. A study in US individuals also showed that smokers reported significantly less total sleep time, greater sleep latency, greater difficulty in falling asleep, maintaining sleep and waking earlier than desired compared to those who did not consume tobacco, a result similar to our study. Individuals who were former tobacco users reported alterations similar to non-smokers and smokers experienced lower quality sleep than non-smokers, compared with those who had never used tobacco, smokers had a significantly higher probability of self-reported snoring (OR = 2.0, 95% CI = 1.56-2.56) and short sleep (OR = 1.68, CI 95% = 1.35-2.10; OR = 1.38, 95% CI = 1.09-1.74). A dose-response relationship was observed between amount smoked and sleep symptoms [26]. In multivariate analysis, no significant interaction was observed between sex and smoking for snoring, short sleep or poor sleep. In a study conducted among US adults, current TC was independently associated with greater odds of snoring and sleeping poorly [27]. Sleeping is considered a healthy behavior. Within the relationships that have been described in the literature, persons with a better diet also have better sleep quality and smokers are more likely to report insomnia and insufficient sleep [28].
Although tobacco consumption has been associated with relatively thinner body mass and smoking cessation with weight gain [29], the brain mechanisms underlying these relationships are not well understood and the results have been contradictory in studies that have tried to understand these variables. Compared to non-smokers, smokers have diminished nervous system responses to non-gratifying tobacco stimuli, however, brain response to favorite foods in relation to smoking status have not been investigated. During the exposure to their favorite food, smokers exhibited decreased activations in the caudate, putamen, insula and thalamus, compared to non-smokers. Neuronal responses during stress and neutral relaxation conditions were similar between the groups that smoke versus those who do not and subjective indices of food cravings were similar between groups. Relatively diminished neural responses to favorite food signals in smokers can contribute to lower BMI [23].
Among the main metabolites associated with tobacco consumption, are nicotine, cotinine, thiocyanate, o-cresol sulfate, and hydroxycotinine, among others. Studies have postulated that nicotine could be the cause of weight gain, however it has been shown to stimulate the basal metabolic rate of smokers [30]. TC and nicotine directly affect the metabolism of glucose and body weight as a result of changes in metabolism, activating lipoprotein lipases that break triglycerides to form free fatty acids, which activates the sympathetic nervous system. These are among other changes that result in greater energy consumption and weight loss. Weight loss is associated with the direct stimulation of the melanocortin 4 receptor (MC4-R), which leads lower food consumption and lower leptin levels. It also stimulates the sympathetic nervous system, which increases adrenaline levels and noradrenaline, lipolysis among other processes [31]. Another study showed an inverse correlation between leptin concentrations and nicotine dependence in people who used tobacco [32]. In contrast, our study shows that smokers weighed more and had a higher BMI, especially in women. It is possible that these results are explained by the fact that non-smokers had healthier eating habits, which is protective for weight gain.
The weaknesses of this study include that the number of cigarettes per day was not quantified. In addition, this was a cross-sectional study, thus causality cannot be inferred. The study had several strengths. We were able to evaluate specific relationships between foods consumed, eating habits and tobacco consumption. We considered several variables - diet, physical activity, anthropometry, and sleep quality - which are not usually evaluated together.
Conclusions
University students who smoked were significantly different from non-smokers in factors related to deteriorating health: higher BMI, greater daytime sleepiness, insomnia and sleep difficulties, lower frequency of weekly breakfast consumption, lower fruit consumption, higher consumption of junk food and alcoholic beverages and a higher unhealthy food score. However, tobacco consumption was associated on a differentiated manner according to sex. In men, tobacco consumption had a negative effect on daytime sleepiness, insomnia and sleep difficulties and in women, it was associated with higher weight and BMI.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any spe-cific grant from funding agencies in the public, commer-cial, or not-for-profit sectors.
Thanks to the universities and organizations that participated in this study.
Footnotes
Abbreviations
Body Mass Index (BMI); Insomnia Severity Index (ISI); Epworth Sleepiness Scale (ESE); World Health Organization (WHO); melanocortin 4 receptor (MC4-R); Unites States (US).
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
SDA, VV; Conceptualization. Methodology, formal analysis, investigation, data curation, writing, original draft, writing, review and editing. Conceptualization. Methodology, formal analysis, investigation, data curation, writing, original draft, writing, review, editing and Project administration, GO, MF, MV, MC, VE, FM: Methodology, Investigation, Writing - Review & Editing.
References
- [1].Bastías E, Stiepovich J. Una revisión de los estilos de vida de estudiantes universitarios ibereoamericanos. Cienc Enferm 2014;20:93-101. https://doi.org/10.4067/S0717-95532014000200010 10.4067/S0717-95532014000200010 [DOI] [Google Scholar]
- [2].Ministerio de Salud. III Encuesta Nacional de Salud 2016-2017 (http://web.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf).
- [3].Global Database on Body Mass Index, WHO (http://apps.who.int/bmi/index.jsp).
- [4].Pelletier JE, Lytle LA, Laska MN. Stress, health risk behaviors, and weight status among community college students. Health Educ Behav 2016;43:139-144. https://doi.org/10.1177/1090198115598983 10.1177/1090198115598983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].García R, López F, López P, García Cantó E. Actividad físico-deportiva, gasto calórico y consumo de tabaco en adolescentes de Murcia (España). Arch Argent Pediatr 2014;112:12-18. https://doi.org/10.5546/aap.2014.12 10.5546/aap.2014.1224566776 [DOI] [Google Scholar]
- [6].Morales IG, del Valle C, Soto VÁ, Ivanovic M D. Factores de riesgo cardiovascular en estudiantes universitarios. Rev Chil Nutr 2013;40:391-396. https://doi.org/10.4067/S0717-75182013000400010 10.4067/S0717-75182013000400010 [DOI] [Google Scholar]
- [7].Güneş FE, Bekiroglu N, Imeryuz N, Agirbasli M. Awareness of cardiovascular risk factors among university students in Turkey. Prim Health Care Res Dev 2019;20:e127. https://doi.org/10.1017/S146342361900063X 10.1017/S146342361900063X [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lanuza F, Morales G, Hidalgo-Rasmussen C, Balboa-Castillo T, Ortiz MS, Belmar C, Muñoz S. Association between eating habits and quality of life among Chilean university students. J Am Coll Health 2020:1-7. https://doi.org/10.1080/07448481.2020.1741593 10.1080/07448481.2020.1741593 [DOI] [PubMed] [Google Scholar]
- [9].Nazareno N, Benavente A, Alicto M, Arceo J, Charfauros A, Dizon C, Flores E, Fontanilla J, Holm B, Johanes C, Mercado J, Perez K, Perez K, Tingson J, Paulino YC. Smoking, Nutrition, Alcohol, Physical Activity, and Obesity (SNAPO) health indicators among college students in Guam. Hawaii J Health Soc Welf 2020;79(6 Suppl 2):24-29. [PMC free article] [PubMed] [Google Scholar]
- [10].Cohrs S, Rodenbeck A, Riemann D, Szagun B, Jaehne A, Brinkmeyer J, Gründer G, Wienker T, Diaz-Lacava A, Mobascher A, Dahmen N, Thuerauf N, Kornhuber J, Kiefer F, Gallinat J, Wagner M, Kunz D, Grittner U, Winterer G. Impaired sleep quality and sleep duration in smokers - results from the German multicenter study on nicotine dependence. Addiction Biol 2014;19:486-496. https://doi.org/10.1111/j.1369-1600.2012.00487.x 10.1111/j.1369-1600.2012.00487.x [DOI] [PubMed] [Google Scholar]
- [11].Durán S, Valdez-Badilla P, Godoy-Cumillaf A, Herrera T. Eating habits and physical condition of physical education students. Rev Chil Nutr 2014;41:251-259. https://doi.org/10.4067/S0717-75182014000300004 10.4067/S0717-75182014000300004 [DOI] [Google Scholar]
- [12].Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2001;2:297-307. https://doi.org/10.1016/s1389-9457(00)00065-4 10.1016/s1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- [13].Morin C. Insomnia: psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- [14].Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-545. [DOI] [PubMed] [Google Scholar]
- [15].WHO Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- [16].Ministry of Health of Chile. Reporte impacto del tabaquismo en la salud en Chile. 2015. (http://web.minsal.cl/sites/default/files/files/2015_09_02_TABACO.pdf).
- [17].De Granda-Orive JI, De Granda-Beltrán AM, Segrelles-Calvo G, López-Padilla D, Jiménez-Ruiz CA, Solano-Reina S. Avances y líneas de investigación en el tratamiento y diagnóstico del tabaquismo. Sanid Mil 2017;73:57-65. [Google Scholar]
- [18].Ministerio del interior y seguridad pública. Décimo primer estudio nacional de drogas en población general, 2015. (http://www.senda.gob.cl/media/estudios/PG/2014_EstudioDrogas_Poblacion_General.pdf).
- [19].Nasser AMA, Geng Y, Al-Wesabi SA. The prevalence of smoking (cigarette and waterpipe) among university students in some Arab countries: a systematic review. Asian Pac J Cancer Prev 2020;21:583-591. https://doi.org/10.31557/APJCP.2020.21.3.583 10.31557/APJCP.2020.21.3.583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Font-Mayolas S, Sullman MJM, Gras ME. Sex and polytobacco use among Spanish and Turkish university students. Int J Environ Res Public Health 2019;16:5038. https://doi.org/10.3390/ijerph16245038 10.3390/ijerph16245038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Haibach J, Homish G, Collins L, Ambrosone C, Giovino G. An evaluation of fruit and vegetable consumption and cigarette smoking among youth. Nicotine Tob Res 2015;17:719-726. https://doi.org/10.1093/ntr/ntu215 10.1093/ntr/ntu215 [DOI] [PubMed] [Google Scholar]
- [22].Endoh K, Kuriki K, Kasezawa N, Tohyama K, Goda T. Association between smoking status and food and nutrient consumption in Japanese: a large-scale cross-sectional study. Asian Pac J Cancer Prev 2015;16:6527-6534. https://doi.org/10.7314/apjcp.2015.16.15.6527 10.7314/apjcp.2015.16.15.6527 [DOI] [PubMed] [Google Scholar]
- [23].Jastreboff AM, Sinha R, Lacadie CM, Balodis IM, Sherwin R, Potenza MN. Blunted striatal responses to favorite food cues in smokers. Drug Alcohol Depend 2015;146:103-106. https://doi.org/10.1016/j.drugalcdep.2014.09.006 10.1016/j.drugalcdep.2014.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Custodio L, Carlson CR, Upton B, Okeson JP, Harrison AL, de Leeuw R. The impact of cigarette smoking on sleep quality of patients with masticatory myofascial pain. J Oral Facial Pain Headache 2015;29:15-23. https://doi.org/10.11607/ofph.1266 10.11607/ofph.1266 [DOI] [PubMed] [Google Scholar]
- [25].Wang X, Li W, Zhou J, Wei Z, Li X, Xu J, Zhang F, Wang W. Smoking and sleep apnea duration mediated the sex difference in daytime sleepiness in OSA patients. Sleep Breath 2020;25:289-297. https://doi.org/10.1007/s11325-020-02109-x 10.1007/s11325-020-02109-x [DOI] [PubMed] [Google Scholar]
- [26].McNamara JP1, Wang J, Holiday DB, Warren JY, Paradoa M, Balkhi AM, Fernandez-Baca J, McCrae CS. Christina. Sleep disturbances associated with cigarette smoking. Psychol Health Med 2014;19:410-419. https://doi.org/10.1080/13548506.2013.832782 10.1080/13548506.2013.832782 [DOI] [PubMed] [Google Scholar]
- [27].Pengpid S, Peltzer K. Tobacco use and associated health risk behaviours among university students in 27 countries. Int J Adolesc Med Health 2020;June8(Online ahead of print). https://doi.org/10.1515/ijamh-2019-0268 10.1515/ijamh-2019-0268 [DOI] [PubMed] [Google Scholar]
- [28].Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med 2016;18:7-18. https://doi.org/10.1016/j.sleep.2015.01.020 10.1016/j.sleep.2015.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].El Reda D, Ström P, Sandin S, Oh JK, Adami HO, Löf M, Weiderpass E. Determinants of long-term weight change among middle-aged Swedish women. Obesity (Silver Spring) 2017;25:476-485. https://doi.org/10.1002/oby.21745 10.1002/oby.21745 [DOI] [PubMed] [Google Scholar]
- [30].Pánková A. Role of incretins in energy metabolism and weight changes after smoking cessation. Cas Lek Cesk 2016;155:41-43. [PubMed] [Google Scholar]
- [31].Harris KK, Zopey M, Friedman TC. Metabolic effects of smoking cessation. Nat Rev Endocrinol 2016;12:299-308. https://doi.org/10.1038/nrendo.2016.171 10.1038/nrendo.2016.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Suhaimi MZ, Sanip Z, Jan HJ, Yusoff HM. Leptin and calorie intake among different nicotine dependent groups. Ann Saudi Med 2016;36:404-408. https://doi.org/10.5144/0256-4947.2016.404 10.5144/0256-4947.2016.404 [DOI] [PMC free article] [PubMed] [Google Scholar]


